Abstract
Currently, the use of medications is the standard and most common method of biological treatment in psychiatry. However, sometimes pharmacotherapy does not lead to remission, so research is being carried out into other, non-pharmacological strategies of treatment.
There is a need for developing new therapies such as cryostimulation that can be used as adjunct psychiatric therapy. The mechanisms of action of hypothermic protection are not entirely understood. The response of the human body to cold occurs through the changes in the endocrine, circulatory, nervous–muscular, and immunological systems. Cryostimulation has been found useful in neurological and psychiatric disorders, especially depression. It seems that cryostimulation may be used as adjuvant therapy in the treatment of diseases with oxidative stress background since it improves the antioxidant capacity of organism.
In this study, the physiology and neuroprotection of hypothermia and influence of cryostimulation on oxidative stress in psychiatric disorders especially depression are presented. The effects of cryostimulation in multiple sclerosis depressive patients are shown.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Multiple Sclerosis
- Multiple Sclerosis Patient
- Complementary Medicine
- Hamilton Anxiety Rate Scale
- Magnetic Seizure Therapy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Currently, the use of medications is the standard and most common method of biological treatment in psychiatry. However, sometimes pharmacotherapy does not lead to remission, so research is being carried out into other, non-pharmacological strategies of treatment (Wayne et al. 2003; Werneke et al. 2006).
Many persons with psychiatric disorders turn to non-pharmacologic and nonconventional interventions (Olivieri et al. 2011; Cabral et al. 2011; Sánchez González et al. 2009), including cryostimulation. There is increasing scientific interest in the potential effectiveness of these interventions for the treatment of anxiety and depression, especially for mild to moderate levels of disorder severity (van der Watt et al. 2008). There is a need for developing new therapies such as cryostimulation that can be used as adjunct psychiatric therapy. The mechanisms of hypothermic protection are not entirely understood. It is known that lower temperature protects tissues against hypoxia by slowing down the rate of cellular damage due to formation of free radicals, chemical metabolites, and tissue edema (Gordon 2001; Miller et al. 2010b). According to increasing evidence, hypothermia can significantly improve outcomes of diseases with oxidative stress background such as neonatal hypoxic–ischemic encephalopathy (Perrone et al 2010; Fatemi et al. 2009), brain injury (Varon et al. 2011), multiple sclerosis (Miller et al. 2010a), depression (Miller et al. 2011b), and cerebral ischemia (Varon et al. 2011). Treatment with the total immersion of the body at extremely low temperatures was first introduced in Japan towards the end of the 1970s by Toshiro Yamauchi (Yamauchi 1989) who constructed the first cryogenic chamber and successfully used cryotherapy to treat rheumatism (Lange et al. 2008). At present, cryostimulation is recommended not only for inflammatory diseases of the locomotor system, degenerative joint and spine diseases, or soft tissue rheumatic diseases but also for psychiatric disorders especially for anxiety-depressive disorders (Rymaszewska et al. 2000).
2 Non-pharmacological Treatments in Psychiatry
Currently, a variety of supplementary therapies for treatment psychiatric disorders are used worldwide. Complementary medicines are either used as an alternative or in addition to conventional medicine (Cabral et al. 2011; Lavretsky 2009; Olivieri et al. 2011). Their use by those with chronic disorders such as cancers, with their associated physical and psychological problems, is well documented (Ernst and Cassileth 1998; Schraub 2000). In psychiatric patients, estimates of their use range from 8 to 57 %, with the most frequent use being in depression and anxiety. Acupuncture, aromatherapy, enzyme therapy, homeopathy, hypnotherapy, massage, reflexology, relaxation techniques, and spiritual healing were frequently used forms of treatment (Cabral et al. 2011; Edzard 2001; Shapiro et al. 2007). Phototherapy is one of the most popular and effective methods that was used in treating the seasonally occurring mood disorder occurring in bipolar disorders at the beginning of the 1980s. Electroconvulsive therapy is also still applied therapy in psychiatric disorders (Sánchez González et al. 2009). Other modern biological treatment methods such as cryostimulation are constantly being developed. Methods involving neurostimulation include repetitive transcranial magnetic stimulation (Rau et al. 2007; Lavretsky 2009), magnetic seizure therapy, vagus nerve stimulation (Rush et al. 2000), deep brain stimulation, and also transcranial direct current stimulation (Grunhaus et al. 2000). These methods may be effective in treating depression and have minimal side effects.
A population-based study from the USA found that 9 % of respondents had anxiety attacks, 57 % of whom used complementary medicines, and that 7 % of respondents reported severe depression, with 54 % of these using complementary medicines (Kessler et al. 2001). Another survey from the USA reported mental disorders in 14 % of respondents, 21 % of whom used complementary medicines. People with mental health problems may take complementary medicines to treat anxiety and depression or to counter side effects of conventional treatments, for example, late occurring dyskinesia and weight gain (Unger et al. 1992).
Some patients with chronic anxiety and depression use complementary medicine which seems to be more holistic treatment with no side effects especially when ineffectiveness of conventional treatment became evident (van der Watt et al. 2008; Berchtold et al. 2010).
3 Hypothermia as a Neuroprotective Therapy
Nowadays, hypothermia seems to be the most promising neuroprotective therapy that has been implemented to clinical practice (Shintani et al. 2011; Ceulemans et al. 2010; Dietrich and Bramlett 2010; Fatemi et al. 2009).
The first clinical studies of brain cooling in the 1960s showed decrease of O2 consumption, CO2 production, and other indicators of metabolism (Adelson 2009: Dietrich and Bramlett 2010). Even small fluctuations in the temperature of the brain alter hemodynamic, calcium-dependent intercellular signaling, excitotoxicity, inflammation and edema, apoptosis, as well as molecular makers (Adelson et al. 2005; Ceulemans et al. 2010; Kuo et al. 2011). Excitotoxicity is one of the most important processes in the brain. Many studies reported that extracellular levels of the excitatory amino acid glutamate and other neurotransmitters after brain injury were reduced following mild posttraumatic hypothermia. Additionally, hypothermia inhibits generation of oxygen free radicals involved in the secondary damage, associated with reperfusion (Christian et al. 2008; Perrone et al. 2010; Adelson 2009).
Mild to moderate hypothermia was also reported to reduce abnormal blood–brain barrier permeability after both ischemic and traumatic insults (Katz et al. 2004; Ji et al. 2007). Another mechanism of hypothermic cytoprotection is reducing inflammatory processes including trauma-induced increases in the pro-inflammatory cytokines interleukin (IL)-1β and tumor necrosis factor (TNF α) (Ceulemans et al. 2010; Jorgensen 2008). Current research lead to use the temperature modifications to discover the critical ligand/receptor and cellular signaling specific responsible foranti-inflammatory effect (Bayir et al. 2009), although the precise way of neuroprotection by hypothermia is not known (Gordon et al. 2003).
Apoptotic cell death also participates in the vulnerability of different cell types after neurotrauma. Several clinical studies suggest that posttraumatic hypothermia can significantly reduce levels of caspase 3, an important initiator of apoptotic cell death, and reduce cytochrome C release from dysfunctional mitochondria (Hasegawa et al. 2009; Bayir et al. 2009). Hypothermia may affect signaling cascades associated with hippocampal-dependent learning and memory. It may represent a molecular mechanism by means of which hypothermia improves psychological aspects of neurotrauma (Dietrich and Bramlett 2010). Additionally, hypothermia decreases the global cerebral metabolic rate for glucose and oxygen but maintains a slightly better energy level by reducing ATP breakdown (Bayir et al. 2009).
4 Physiological Effect of Cryotherapy
Cryostimulation is an exposure of whole human body to extremely low temperatures (−130 °C) in a cryogenic chamber. The cryogenic chamber (usually liquid nitrogen is a coolant) is consists of two rooms: the vestibule, with the temperature of (−60 °C), and the main chamber, with temperature (−130 °C). Sessions in the cryochamber last 3 min (Bauer and Skrzek 1999; Zagrobelny et al. 1993). During cryostimulation, the subjects wear bathing suits, surgical masks, caps, gloves, socks, and shoes. Cryostimulation sessions are usually applied every day. The participants are entered to the main chamber in groups of five or four persons. In the cryogenic chamber, subjects are instructed to keep walking in a circle, moving slowly, one behind another, without verbal contact. Just before each session of cryostimulation, systolic and diastolic blood pressures are measured, because arterial hypertension is one of the main contraindication to this therapy (Gregorowicz and Zagrobelny 2007; Lubkowska et al. 2010).
The maintenance of a constant body temperature in human body during cold stress occurs through changes in the endocrine, circulatory, neuromuscular, and immunological systems (Kellogg 2006). The major effector of human thermoregulation is cutaneous circulation. In the dermis, there are tenfold more cold receptors than heat receptors. Experimental evidence indicates that the early phase of vasoconstriction due to cooling is mainly dependent on neural regulation and that late-phase vasoconstriction relies mainly on nonneural mechanisms (Hampl et al. 2006).
Shivering is a form of thermogenesis, which consumes large amounts of energy but is not effective during severe cold (Silva 2006) such as cryostimulation. It is the earliest and most primitive response to increase heat production. Humans have evolved a more efficient and long-lasting form of non-shivering facultative thermogenesis that uses pure metabolic mechanisms to generate heat. The non-shivering thermogenesis has two categories: obligatory and facultative (Kellogg 2006). The facultative thermogenesis is regulated mainly by catecholamines released from adrenals and the sympathetic nervous system (Hampl et al. 2006). The most important endocrine factors modulating obligatory thermogenesis are thyroid hormones, which increase metabolic rate and thermogenesis. Obligatory thermogenesis proceeds continuously in all organs and tissues of the body (Silva 2006).
Currently cryostimulation is one of the most promising adjunct therapies in psychiatric disorders especially in anxiety-depressive disorders. Cryogenic temperatures induce vasoconstriction followed by vasodilation after 4 min which is connected with increasing blood flow seen as skin hyperemia and return to normal skin temperatures (after about 14 min). Vasodilation appears about 4 min after whole-body cryotherapy (WBCT) and achieves fourfold higher value than before cryostimulation and can last a few hours (Bauer and Skrzek 1999) increasing blood flow and stimulating elimination of metabolic products. There are a variety of individual responses to cold due to such factors as body size, fitness level, amount of subcutaneous fat, and sex (Gordon 2001). Cooling the skin below 20 °C causes a marked reduction in the production of acetylcholine and in the rate of conduction along cooling nerves, which varies according to the size of fibers, thus producing asynchrony of impulses (Woźniak et al. 2007). Females have a reduced cold temperature tolerance compared to men because of their lower aerobic capacity (Gordon 2010).
Cryostimulation treatment resulted in decreased levels of testosterone and estradiol in football players, although there were no changes in the concentration of luteinizing hormone and dehydroepiandrosterone (DHEA-S) (Korzonek-Szlacheta et al. 2007). After cryostimulation, decreased hemoglobin and iron in erythrocytes were observed (Banfi et al. 2009a) which probably cause decreased testosterone. Smolander et al. (2009) reported that ten sessions of WBCT in healthy females did not lead to disorders related to altered secretions of growth hormone, prolactin, thyrotropin, or thyroid hormone. The mechanisms of action of hypothermic protection are not entirely understood. It seems that lower temperature protects tissues against hypoxia by slowing the rate of cellular damage due to formation of free radicals, chemical metabolites, and tissue edema. In addition to protection from ischemic damage, hypothermia has been show to ameliorate the toxicity of various drugs and environmental toxicants as well as to protect against other disorders such as hemorrhage, hypergravity, and hypoglycemia (Gordon 2001).
5 Cryostimulation and Oxidative Stress
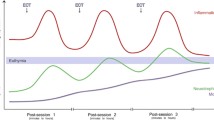
Acute cold temperature represents an obvious stress, which could lead to some adaptive mechanisms, which increase in body resistance against cold. It has been suspected that an adaptation to cold stimuli and the improvement in the body hardening could be related to an increase in the protection against oxidative stress by significant augmentation of antioxidant levels (Fig. 1) (Miller et al. 2011a). Since oxidative stress is very important factor of many psychiatric disorders, it is important to find therapy that could improve the protection of the body against oxidative stress and could have some practical applications in the development of therapies for a large numbers of individuals. Siems et al. (1999) reported a higher enzymatic protection (i.e., in the increased activity of red blood cell enzymes) for those who regularly practice winter swimming activities or after heavy endurance physical exercise in comparison with control. Recent data suggest that cold stress increases antioxidant defenses in human body (Miller et al. 2010a, b; Siems and Brenke 1992). Activation of the antioxidant system can be an adaptive defensive mechanism to cope with increased oxidative stress especially in immunoactive disorders. Cold exposure elicits substantial alterations both in metabolic and physiological aspects. Firstly, free radical formation is increased during cold stress (Armario et al. 2008). Further, cold stress activates stress responses and induces shivering and muscle movement to maintain body temperature, and this action increases production of reactive oxygen species (ROS) (Fig. 1). The ratio of oxidized glutathione to glutathione is increased after short-term whole-body cold exposure in human (Teramoto and Ouchi 1999). However, winter swimmers have a higher concentration of glutathione and greater activities of glutathione peroxidase and catalase than do healthy controls (Siems et al. 1999). These findings indicate that glutathione metabolism and function might be impaired during acute cold-water immersion but can be preserved during chronic or repeat immersion.
Thermoregulation induced by low temperatures is associated with an increase in lipid metabolism (Westerlund et al. 2003). The human body uses energy derived mainly from the conversions of carbohydrates and lipids (Vallerand and Jacobs 1989). The release of norepinephrine from the terminal endings of sympathetic neurons during non-shivering thermogenesis leads to the mobilization of fatty acids from intracellular stores of triglycerides and their oxidation in the mitochondria (Florez-Duquet and McDonald 1998).
In the course of normal human activity – energy production, detoxification of pollutants, and immunologic defense mechanisms – free radicals are produced. Dietary antioxidants (such as proanthocyanidins found in blueberries and bioflavonoids found in citrus fruits) as well as the human antioxidant enzymes and nonenzymatic provide critical protection against free radical formation and reduce damage induced by their action.
In depression, oxidative stress is increased (Kodydkvo et al. 2009; Cumurcu et al. 2009). There is a need for developing new therapies such as cryostimulation which can be used as adjuvant antioxidative therapy. After 10 sessions of cryostimulation, total antioxidative status (TAS) level in plasma was distinctly higher (p < 0.001) (Miller et al. 2011a). These observations that presented the suppression of oxidative stress by cryostimulation are consistent with other reports (Duqué et al. 2005; Siems et al. 1999; Miller et al. 2010a, b). Woźniak et al. (2007) showed that cryostimulation induces an increase in the activity of superoxide dismutase (SOD) by 36 % (P < 0.001) and glutathione peroxidase (GPx) by 68 % (P < 0.01) in the human erythrocytes.
Siems et al. (1999) reported a higher enzymatic protection (i.e., in the increased activity of red blood cells, catalase (CAT), GPx, SOD) for those who regularly practice winter swimming activities or after heavy endurance physical exercise in comparison with control. This activation can be viewed as an adaptive defensive mechanism to cope with increased oxidative stress.
Cryostimulation stimulates the antioxidative response of organism via augmentation of SOD activities (p < 0.001) and increase of uric acid (UA) level (p < 0.001) compared to non-WBCT subjects. In humans, over half the antioxidant capacity of blood plasma comes from UA. UA can scavenge superoxide, the hydroxyl radical, and singlet oxygen and may assist in the removal of superoxide by preventing the degradation of SOD, the enzyme that is responsible for clearing superoxide from the cell (Miller et al. 2011c). Uric acid like ascorbic acid is a strong reducing agent and a potent antioxidant responsible for TAS level in plasma (Kutzing and Firestein 2008; Miller et al. 2011c).
Longitudinal measurement of uric acid level in plasma after ten sessions of cryostimulation showed an increase of uric acid concentration for 3 months after therapy. Therefore, cryostimulation could be a therapy elevating uric acid concentration in plasma. It is very important because low level of uric acid is suggested as characteristic of depression and may be normalized after antidepressant pharmacologic treatment (Wen et al. 2011).
Taking into account the above data, it has been suspected that an adaptation to cold stimuli and the increase in body resistance could be related to an increase in the protection against oxidative stress (Duqué et al. 2005).
6 Cryostimulation in Psychiatric Disorders
Most pharmacological treatments of anxiety and other mental disorders rely on the hypothesis that there are underlying neurochemical or neurophysiological abnormalities that can be corrected with pharmacological treatment (Werneke et al. 2006; Unger et al. 1992). However, there may also be a component of some mental disorders that responds to the environmental factors that occurs with some forms of temperatures stimulus, such as cryotherapy.
Recent data point at a positive role of cryostimulation in affective and anxiety disorders, particularly in depression. The study of Rymaszewska et al. (2008) on 26 patients with affective and anxiety disorders reported significant reduction of 13 from 14 Hamilton Anxiety Rating Scale (HARS) items after 15 exposures of WBCT. Only gastrointestinal symptoms did not improve significantly. Concerning the Hamilton Depression Rating Scale (HDRS) items, it was the reduction in most of the items at the level of 0.001 except guilt feelings, early waking, psychomotor retardation, and hypochondrias on the level below 0.01 (gastrointestinal symptoms and body mass did not change within 3 weeks). So, after 15 (2–3 min) exposures of WBCT (1 exposure per day), a decrease of at least 50 % from the baseline HDRS-17 scores in 34.6 % of the study group and 2.9 % of the control group and a decrease of at least 50 % from the baseline HARS score in 46.2 % of the study group and in none of the control group were noted.
The next study of Rymaszewska et al. (2003) reported that the HDRS sum score for each patient (n = 33) after ten exposures of WBCT was lower than that of the baseline and reached statistical significance. Recent results (Miller et al. 2011b) demonstrate that ten exposures of cryostimulation significantly increased not only TAS level in 15 patients with mild to moderate depression (13–18 BDI) but also reduced 19 from 21 items in Beck Depression Inventory (BDI) self-report rating scale (17 items: p < 0.001).
Cryostimulation is a relatively new therapeutic method of physical medicine with a history of about 20 years. Thus, research works on mechanisms of therapeutic action of cryogenic temperatures are still carried on.
6.1 Cryostimulation and Aerobic Training
Persons with severe psychiatric disabilities in addition to their mental illness also frequently suffer the adverse effects of poor physical fitness, including weight problems, sleeplessness, poor cardiovascular fitness, fatigue syndrome, and low self-assessment. These conditions represent serious barriers to the treatment and rehabilitation (Tkachuk and Garry 1999).
Cryostimulation is often connected with exercise, especially aerobic training to increase acceleration of body temperature to normal value.
Voluntary physical activity affects brain plasticity by facilitating neurodegenerative, neuroadaptive, and neuroprotective processes (Daley 2002; Greenwood and Fleshner 2011; Lafenetre et al. 2011; Hortobgyi and Maffiuletti 2011).
At least some of the processes are mediated by neurotrophic factors (Dishman et al. 2006). Motor skill training and regular exercise concomitant with cryostimulation enhance executive functions of cognition and some types of learning. Chronic physical activity increases the expression of brain-derived neurotrophic factor (BDNF) (Heyman et al. 2011; Ding et al. 2011). In vitro and vivo studies showed that chronic exercises can increase the expression of genes that encode several brain neurotrophins such as BDNF, nerve growth factor, and galanin. BDNF supports the survival and growth of many neuronal subtypes, including glutamatergic neurons, and emerged as a key mediator of synaptic efficacy, neuronal connectivity, and use-dependent plasticity (Berchtold et al. 2010). IGF-1 levels increase in both the periphery and brain after exercise, and at least part of the increase in the brain reflects increased transport from the periphery across the blood–brain barrier (Cotman and Berchtold 2002).
Chronic training may also have neurodegenerative and neuroprotective effects on the brain by stimulating the growth and development of new cells and protecting against ischemic damage in the hippocampal formation and neurotoxic damage in the neostriatum ( Helmich et al. 2010; Pajonk et al. 2010; Sacerdote et al. 2000). The neural consequence of chronic cold stress and aerobic training is that it may contribute to these stress protective effects including alterations in serotonergic 5-hydroxytryptamine and splenic norepinephrine systems (Dishman et al. 2006).
6.2 Endorphin Hypothesis of Cryostimulation
Low temperature activates not only thermoregulation system but also hormonal response, which changes cellular metabolism and the concentrations of epinephrine, norepinephrine, adrenocorticotropic hormone (ACTH), cortisone, pro-opiomelanocortin (POMC), and β-endorphins in blood plasma as well as testosterone levels (Campeau et al 2004; Belda et al. 2008).
POMC is the source of several important biologically active substances, such as ACTH in the anterior pituitary gland and melanocyte-stimulating hormone (α-MSH) and β-endorphin. α-MSH has a role in the regulation of appetite and sexual behavior. One neurobiological hypothesis of depression is based on dysregulation of the hypothalamic–pituitary–adrenal axis (Stranahan et al. 2008). The brain’s opioid peptide systems are known to play an important role in motivation, emotion, attachment behavior, response to stress and pain, and the control of food intake (Droste et al. 2003; Sharp et al. 1998).
The physical and psychological stress such as cryostimulation coordinates the adaptive responses of the organism to stressors (Teramoto and Ouchi 1999). Activation of the stress system leads to behavioral and peripheral changes that improve the ability of the organism to adjust homeostasis. The main components of the stress system are the corticotropin-releasing hormone (CRH) and autonomic systems with their peripheral effectors and the hypothalamic–pituitary–adrenal axis (HPA) (Mellon and Bayer 1998; Sacerdote et al. 2000).
On the basis of available data, it seems that during the period of hypothermic stress, the brain releases a number of chemical mediators, including opioid peptides such as β-endorphin, which stimulate an inhibitory effect on the immune system (Carr et al. 1996; Guan et al. 1995; Shavit et al. 1986).
The activation of the HPA starts the production of adrenocorticotropin from the pituitary that in turn causes the release of glucocorticoids that could suppress the immune system (Freier and Fucks 1993; Van Den Eede and Moorkens 2008). Circulating ACTH is the key regulator of glucocorticoid secretion by the adrenal cortex. Other hormones or cytokines, either originating from the adrenal medulla or coming from the systemic circulation, as well as neuronal information from the autonomic innervation of the adrenal cortex may also participate in the regulation of cortisol secretion. Glucocorticoids play main regulatory role in the activity of the HPA axis and in the termination of the stress response by acting at extra-hypothalamic centers, the hypothalamus and the pituitary gland. The inflammatory cytokines TNF α, IL-1β and IL-6 can cause stimulation of the HPA axis alone, or in synergy with each other. It is unclear how repeated cryostimulation influences the level of pro-inflammatory and anti-inflammatory mechanisms. There is a report of increased anti-inflammatory cytokine IL-10 and decreased pro-inflammatory IL-2 and IL-8 after five systemic cryostimulation sessions (Banfi et al. 2009b). On the other hand, another report shows increased levels of IL-6 in response to ten cryostimulation sessions (Lubkowska et al. 2009). Some authors report that cryostimulation leads to an increase in plasma ACTH and cortisol, epinephrine, and norepinephrine (Zagrobelny et al. 1993), while others have not observed any stimulation of traditional stress hormones (Leppäluoto et al. 2008) (Fig. 2).
Further studies are required to explain the mechanisms of multisystem cold stress reaction in humans and determine the possible role of cryostimulation in the treatment mental disorders.
6.3 Cryostimulation in Depressive Multiple Sclerosis Patients
Multiple sclerosis (MS) is a complex disease with several pathophysiological processes: inflammation, demyelination, oxidative stress, axonal damage, and repair mechanisms that participate in this disorder (Peterson and Fujinami 2007). These processes are not uniformly represented in patient populations but can selectively predominate in individual patients (Bielekova and Martin 2004). Therefore, there is a need for developing new antioxidative pathways such as cryostimulation especially in progressive phase of MS that are more process specific and can be used in specific patient subpopulations (Miller et al. 2011b, c). There are three main types of MS: relapsing-remitting (RRMS), secondary progressive (SPMS) and primary-progressive (PPMS) with progressive-relapsing (PRMS) recently distinguished as an additional subtype (Miller et al 2011c). SPMS patients have irreversible disability with a wide range of ameliorative symptoms. MS is variable in onset and progression. First, the most common symptoms are impaired vision due to optic neuritis (inflammation of the optic nerve) and deficits in sensation (or over-sensation as burning or prickling). In the mature form of MS appear other symptoms including paresis and paralysis, ataxia, fatigue, spasticity, and incontinence. Cognitive impairment (difficulties with memory, concentration, and other mental skills), depression, and fatigue also occur frequently. Initially, more than 80 % of individuals with MS have a RRMS disease course with defined clinical exacerbations of neurologic symptoms, followed by complete or incomplete remission (Miller 2011). RRMS is dominated by multifocal inflammation, edema, and the physiologic actions of cytokines (Miller 2011; Racke 2009). After 10–20 years, about half of those with RRMS gradually accumulate irreversible neurological deficits in the absence of clinical relapses or new white matter lesions by magnetic resonance image (MRI). This stage is known as SPMS characterized by progression of clinical symptoms (Tullman et al. 2004 ; Liguori et al. 2000). Disability levels in SPMS patients often worsen despite a stable MRI T(2) lesion burden. Oxidative stress and brain atrophy in the absence of measurable inflammation are possible explanations for this phenomenon (Koch et al. 2007). It is difficult to predict the clinical course of this disease. Progression of disability seems to be increased in patients with higher number of relapses during the first and second year of the disease (Lublin and Reingold 1996; Bashir and Whitaker 1999). A higher incidence of depressive symptoms and major depressive disorder in patients with MS is well documented and reported in both large community surveys and studies of persons with MS. Depressive symptoms in MS patients are associated with reduced quality of their lives (Sollom and Kneebone 2007).
Accumulating data indicate that oxidative stress (OS) plays a crucial role in the pathogenesis of MS and depression (Miller et al. 2011b; Gilgun-Sherki et al. 2004). Reactive oxygen and nitrogen species (ROS/RNS), leading to oxidative stress, generated in excess primarily by macrophages, have been implicated as mediators of demyelination and axonal damage in MS (Gonsette 2008). Excessive release of ROS causes damage to main cellular structures and components such as lipids, proteins, and nucleic acids (e.g., RNA, DNA) and promotes transendothelial leukocyte migration as well as contributes to oligodendrocyte damage and axonal degeneration. Additionally, weakened cellular antioxidant defense systems in CNS in MS and its vulnerability to ROS effects may ameliorate damage (Miller 2011). Therefore, treatment with antioxidants might theoretically prevent propagation of tissue damage and improve both survival and neurological outcome. Cryostimulation in MS patients with neurological deficits has increased not only muscle strength, decreased spasticity, and reduced disability in EDSS (Expanded Disability Status Scale),but also higher level of antioxidative status has been observed (Miller et al. 2010b). During hypothermia, reduced demand for oxygen slows the rate of lipid peroxidation and protects ischemic cell membranes by stabilizing potassium efflux. Recent clinical studies showed that the level of TAS was distinctly reduced (p < 0.0003) in depressive MS patients in comparison with MS patients without depression (Miller et al. 2011b). Treatment with cryostimulation caused significant increase of TAS level in plasma of depressive MS patients compared to untreated patients and reached the values of healthy controls. It is unclear exactly how exactly cryostimulation might reduce depression in non-MS populations; however, several theories have been proposed to suggest a possible role for cryogenic treatment for mood and anxiety disorders including regulation of the hypothalamic–pituitary–adrenal axis (HPA), increased β-endorphin levels, normalization of hippocampal brain-derived neurotrophic factor (BDNF), regulation of monoamines, and improved perceptions of self-efficacy. The HPA, BDNF, and serotonin have all been implicated in MS pathology (Miller et al. 2011a). If cryostimulation like exercise affects HPA function, BDNF concentration, or serotonin concentration in persons with MS, this provides a possible explanation for the decreased incidence of depression observed in persons with MS who regularly participate in physical activity. Alternatively, depression etiology in MS may have a psychological rather than neurobiological explanation. Clinically significant depression can affect up to 50 % of patients with multiple sclerosis over the course of their lifetime (Feinstein 2011). Therefore, the etiology and the influence of cryostimulation on depression are areas that warrant further investigation. Cryostimulation could be an effective aid to psychopharmaceutical treatment of MS patients. Results (Miller et al. 2010a) demonstrate that ten exposures of cryostimulation significantly increased the level of TAS (p < 0.002) in MS patients. It seems that the lower level of TAS observed in plasma of MS patients is dependent on the low concentrations of endogenous antioxidants, mainly uric acid. The results suggest that cryotherapy may play an important role by suppressing oxidative stress and ROS production especially in MS patients with depression.
7 Conclusions
It seems that cryostimulation may be used as adjuvant therapy in the treatment of psychiatric diseases with oxidative stress background since it improves the antioxidant capacity of organism.
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- BDI:
-
Beck Depression Inventory
- BDNF:
-
Brain derived neurotrophic factor
- CAT:
-
Catalase
- CRH:
-
Corticotropin-releasing hormone
- DHEA:
-
Dehydroepiandrosterone
- EDSS:
-
Expanded Disability Status Scale
- GPx:
-
Glutathione peroxidase
- HARS:
-
Hamilton anxiety rating scale
- HDRS:
-
Hamilton depression rating scale
- HPA:
-
Hypothalamic–pituitary–adrenal axis
- IGF:
-
Insulin-like growth factor
- IL:
-
Interleukin
- MRI:
-
Magnetic resonance image
- MS:
-
Multiple sclerosis
- POMC:
-
Pro-opiomelanocortin
- PPMS:
-
Primary-progressive multiple sclerosis
- PRMS:
-
Progressive-relapsing multiple sclerosis
- RNS:
-
Reactive nitrogen species
- ROS:
-
Reactive oxygen species
- RRMS:
-
Relapsing-remitting multiple sclerosis
- SOD:
-
Superoxide dismutase
- SPMS:
-
Secondary-progressive multiple sclerosis
- TAS:
-
Total antioxidative status
- TNF:
-
Tumor necrosis factor
- UA:
-
Uric acid
- WBCT:
-
Whole-body cryotherapy
References
Adelson PD (2009) Hypothermia following pediatric traumatic brain injury. J Neurotrauma 26:429–436
Adelson PD, Ragheb J, Kaney P et al (2005) Phase II clinical trial of moderate hypothermia after severe traumatic brain injury in children. Neurosurgery 56:740–754
Armario A, Vallés A, Dal-Zotto S et al (2008) A single exposure to severe stressors causes long-term desensitisation of the physiological response to the homotypic stressor. Ann N Y Acad Sci 1148:165–173
Banfi G, Melegati G, Barassi A (2009a) Beneficial effects of whole body cryotherapy on sport haemolysis. J Hum Sport Exerc 24:189–193
Banfi G, Melegati A, Barassi A et al (2009b) Effects of whole-body cryotherapy on serum mediators of inflammation and serum muscle enzymes in athletes. J Therm Biol 34:55–59
Bashir K, Whitaker JN (1999) Clinical and laboratory features of primary progressive and secondary progressive MS. Neurology 53:765–771
Bauer J, Skrzek A (1999) Physiological basis of cryotherapy. Med Sport 15:3–7
Bayir H, Adelson PD, Stephen R et al (2009) Therapeutic hypothermia preserves antioxidant defenses after severe traumatic brain injury in infants and children. Crit Care Med 37:689–695
Belda X, Rotllant D, Fuentes S et al (2008) Exposure to severe stressors causes long-lasting dysregulation of resting and stress-induced activation of the hypothalamic-pituitary-adrenal axis. Psychosomatics 49:450
Berchtold NC, Castello N, Cotman CW (2010) Exercise and time-dependent benefits to learning and memory. Neuroscience 167:588–597
Bielekova B, Martin R (2004) Development of biomarkers in multiple sclerosis. Brain 127:1463–1478
Cabral P, Meyer HB, Ames D (2011) Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Prim Care Companion CNS Disord 13:4–16
Campeau S, Nyhuis TJ, Sasse SK et al (2004) Hypothalamic pituitary adrenal axis responses to low-intensity stressors are reduced after voluntary wheel running in rats. Stress 7:157–172
Carr DJ, Rogers TJ, Weber RJ (1996) The relevance of opioid receptors on immunocompetence and immune homeostasis. Proc Soc Exp Biol Med 213:248–257
Ceulemans A, Zgavc A, Kooijman R et al (2010) The dual role of the neuroinflammatory response after ischemic stroke: modulatory effects of hypothermia. J Neuroinflammation 7:74
Christian E, Zada G, Sung G et al (2008) A review of selective hypothermia in the management of traumatic brain injury. Neurosurg Focus 25:E9
Cotman CW, Berchtold NC (2002) Exercise: a behavioral intervention to enhance brain health and plasticity. Trends Neurosci 6:295–301
Cumurcu BE, Ozycurt H, Etikan I et al (2009) Total antioxidant capacity and total antioxidative status in patients with major depression: impact of antidepressant treatment. Psychiatry Clin Neurosci 63:639–645
Daley AJ (2002) Exercise therapy and mental health in clinical populations: is exercise therapy a worthwhile intervention? Adv Psychiatr Treat 8:262–270
Dietrich WD, Bramlett HM (2010) The evidence for hypothermia as a neuroprotectant in traumatic brain injury. Neurotherapeutics 7:43–50
Ding Q, Ying Z, Gómez-Pinilla F (2011) Exercise influences hippocampal plasticity by modulating brain-derived neurotrophic factor processing. Neuroscience 192:773–780
Dishman RK, Berthoud HR, Booth FW et al (2006) Neurobiology of exercise. Obesity 14:345–356
Droste SK, Gesing A, Ulbricht S et al (2003) Effects of long-term voluntary exercise on the mouse hypothalamic-pituitary-adrenocortical axis. Endocrinology 144:3012–3023
Duqué B, Smolander J, Westerlund T et al (2005) Acute and long-term effects of winter swimming and whole-body cryotherapy on plasma antioxidative capacity in healthy women. Scand J Clin Lab Invest 65:395–402
Edzard E (2001) Complementary therapies in palliative cancer care. Cancer 91:2181–2185
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 83:777–782
Fatemi A, Wilson MA, Johnston MV (2009) Hypoxic-ischemic encephalopathy in the term infant. Clin Perinatol 36:835–858
Feinstein A (2011) Multiple sclerosis and depression. Mult Scler 17:1276–1281
Florez-Duquet M, McDonald RB (1998) Cold-induced thermoregulation and biological aging. Physiol Rev 78:339–358
Freier DO, Fucks BA (1993) A mechanism of action for morphine induced immunosuppression: corticosterone mediates morphine induced suppression of NK cell activity. J Pharmacol Exp Ther 270:1127–1133
Gilgun-Sherki Y, Melamed E, Offen D (2004) The role of oxidative stress in the pathogenesis of multiple sclerosis. The need for the effective antioxidant therapy. J Neurol 251:261–268
Gonsette R (2008) Oxidative stress and excitotoxicity: a therapeutic issue in multiple sclerosis? Mult Scler 14:22–34
Gordon CJ (2001) The therapeutic potential of regulated hypothermia. Emerg Med J 18:81–89
Gordon CJ (2010) Response of the thermoregulatory system to toxic insults. Front Biosci (Elite Ed) 2:293–311
Gordon CJ, Fogarty AL, Greenleaf JE et al (2003) Direct and indirect methods for determining plasma volume during thermoneutral and cold-water immersion. Eur J Appl Physiol 89:471–474
Greenwood BN, Fleshner M (2011) Exercise, stress resistance, and central serotonergic systems. Exerc Sport Sci Rev 39:140–149
Gregorowicz H, Zagrobelny Z et al (2007) Systemic cryotherapy. Indications and contraindications, its course, and physiological and clinical results. In: Acta biomedical engineering, Whole body cryotherapy. Indygo Zahir Media, Wrocław, pp 4–16
Grunhaus L, Dannon PN, Schreiber S et al (2000) Repetitive transcranial magnetic stimulation is as effective as electroconvulsive therapy in the treatment of nondelusional major depressive disorder: an open study. Biol Psychiatry 47:314–324
Guan L, Towsend R, Eisenstein TK et al (1995) The cellular basis for opioid induced immunosuppression. Adv Exp Med Biol 373:57–64
Hampl R, Stárka L, Janský L (2006) Steroids and thermogenesis. Physiol Res 55:123–131
Hasegawa M, Ogihara T, Tamai H et al (2009) Hypothermic inhibition of apoptotic pathways for combined neurotoxicity of iron and ascorbic acid in differentiated PC12 cells: reduction of oxidative stress and maintenance of the glutathione redox state. Brain Res 1283:1–13
Helmich I, Latini A, Sigwalt A et al (2010) Neurobiological alterations induced by exercise and their impact on depressive disorders [corrected]. Clin Pract Epidemiol Ment Health 6:115–125, Erratum in: Clin Pract Epidemiol Ment Health 7:106
Heyman E, Gamelin FX, Goekint M et al (2011) Intense exercise increases circulating endocannabinoid and BDNF levels in humans-possible implications for reward and depression. Psychoneuroendocrinology 37:844–851
Hortobgyi T, Maffiuletti NC (2011) Neural adaptations to electrical stimulation strength training. Eur J Appl Physiol 111:2439–2449
Ji X, Luo Y, Ling F et al (2007) Mild hypothermia diminishes oxidative DNA damage and pro-death signaling events after cerebral ischemia: a mechanism for neuroprotection. Front Biosci 12:1737–1747
Jorgensen SL (2008) Hypothermia: a cool intervention for hypoxic-ischemic encephalopathy. JAAPA 21:44–47
Katz LM, Young AS, Frank JE et al (2004) Regulated hypothermia reduces brain oxidative stress after hypoxic-ischemia. Brain Res 1017:85–91
Kellogg DL (2006) In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges. J Appl Physiol 100:1709–1718
Kessler CR, Soukup J, Davis RB et al (2001) The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry 158:289–294
Koch J, Mostest AV, Arutjungan M et al (2007) Plasma lipid peroxidation and progression of disability in multiple sclerosis. Eur J Neur 14:529–533
Kodydkvo J, Vawvrova L, Zeman M et al (2009) Antioxidative enzymes and increased oxidative stress in depressive women. Clin Biochem 42:1368–1374
Korzonek-Szlacheta I, Wielkoszyński T, Stanek A et al (2007) Effect of whole body cryotherapy on the levels of some hormones in professional soccer players. Endokrynol Pol 58:27–32
Kuo JR, Lo CJ, Chang CP et al (2011) Attenuation of brain nitrostative and oxidative damage by brain cooling during experimental traumatic brain injury. J Biomed Biotechnol 16:145–214
Kutzing MK, Firestein BL (2008) Altered uric acid levels and diseases status. J Pharmacol Exp Ther 324:1–12
Lafenetre P, Leske O, Wahle P et al (2011) The beneficial effects of physical activity on impaired adult neurogenesis and cognitive performance. Front Neurosci 5:51
Lange U, Uhlemann C, Muller-Ladner U (2008) Serial whole body cryotherapy in the criostream for inflammatory rheumatic diseases pilot study. Med Klin 103:383–388
Lavretsky H (2009) Complementary and alternative medicine use for treatment and prevention of late-life mood and cognitive disorders. Aging Health 5:61–78
Leppäluoto J, Westerlund T, Huttunen P et al (2008) Effects of long-term whole-body cold exposures on plasma concentrations of ACTH. Beta-endorphin, cortisol, catecholamines and cytokines in healthy females. Scand J Clin Lab Invest 68:145–153
Liguori M, Marrosu MG, Pugliatti M (2000) Age at onset in multiple sclerosis. Neurol Sci 21:825–829
Lubkowska A, Szygula Z, Klimek AJ et al (2009) Do sessions of cryostimulation have influence on white blood cell count, level of IL6 and total oxidative and antioxidative status in healthy men? Eur J Appl Physiol 109:67–72
Lubkowska A, Banfi G, Dołęgowska B et al (2010) Changes in lipid profile in response to three different protocols of whole-body cryostimulation treatments. Cryobiology 61:22–26
Lublin FD, Reingold SC (1996) Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in multiple sclerosis. Neurology 46:907–911
Mellon RD, Bayer BM (1998) Evidence for central opioid receptors in the immunomodulatory effects of morphine: review of potential mechanisms of action. J Neuroimmunol 83:19–28
Miller E (2011) Multiple sclerosis. In: Ahmad SI (ed) Neurodegenerative diseases. Springer Lands Bioscience, Berlin, pp 222–238
Miller E, Mrowicka M, Malinowska K et al (2010a) Effects of whole body cryotherapy on total antioxidative status and activities of antioxidative enzymes in blood of patients with multiple sclerosis. J Med Invest 57:168–173
Miller E, Mrowicka M, Malinowska K et al (2010b) Effects of whole body cryotherapy on oxidative stress in multiple sclerosis patients. J Therm Biol 35:406–410
Miller E, Markiewicz Ł, Saluk J et al (2011a) Effects of short-term cryostimulation on antioxidative status and clinical applications in humans. Eur J Appl Physiol 112:1645–1652
Miller E, Mrowicka M, Malinowska K et al (2011b) Effects of whole body cryotherapy on a total antioxidative status and activity of antioxidant enzymes in blood of depressive multiple sclerosis patients. World J Biol Psychiatry 12:223–227
Miller E, Mrowicka M, Saluk-Juszczak J, Majsterek I (2011c) The level of isoprostanes as a non-invasive marker for in vivo lipid peroxidation in secondary progressive multiple sclerosis. Neurochem Res 36:1012–1016
Olivieri EB, Vecchiato C, Ignaccolo N et al (2011) Radioelectric brain stimulation in the treatment of generalized anxiety disorder with comorbid major depression in a psychiatric hospital: a pilot study. Neuropsychiatr Dis Treat 7:449–455
Pajonk FG, Wobrock T, Gruber O et al (2010) Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry 67:133–143
Perrone S, Szabó M, Bellieni CV et al (2010) Whole body hypothermia and oxidative stress in babies with hypoxic-ischemic brain injury. Pediatr Neurol 43:236–240
Peterson LK, Fujinami RS (2007) Inflammation, demyelination, neurodegeneration and neuroprotection in the pathogenesis of multiple sclerosis. J Neuroimmunol 184:37–44
Racke MK (2009) Immunopathogenesis of multiple sclerosis. Ann Indian Neurol 12:215–220
Rau A, Grossheinrich N, Palm U, Pogarell O et al (2007) Transcranial and deep brain stimulation approaches as treatment for depression. Clin EEG Neurosci 38:105–115
Rush AJ, George MS, Sackeim HA et al (2000) Vagus nerve stimulation (VNS) for treatment-resistant depressions: a multicenter study. Biol Psychiatry 47:276–286
Rymaszewska J, Tulczyński A, Zagrobelny Z et al (2000) The influence of whole body cryotherapy on mental health of the human. In: Zagrobelny Z (ed) Local and whole body cryotherapy. Wydawnictwo Medyczne Urban & Partner, Wrocław, pp 177–185
Rymaszewska J, Tulczyński A, Zagrobelny Z et al (2003) Influence of whole body cryotherapy on depressive symptoms – preliminary report. Acta Neuropsychiatr 15:122–128
Rymaszewska J, Ramsey D, Chladzinska-Kiejna S (2008) Whole body cryotherapy as adjunct treatment of depressive and anxiety disorders. Arch Immunol Ther Exp 56:63–68
Sacerdote P, Limiroli E, Gaspani L (2000) Experimental evidence for immunomodulatory effects of opioids. Landes Biosci, Bookshelf ID: NBK6402
Sánchez González R, Alcoverro O et al (2009) Electrophysiological mechanisms of action of electroconvulsive therapy. Actas Esp Psiquiatr 37:343–351
Schraub S (2000) Unproven methods in cancer: a worldwide problem. Support Care Cancer 8:10–15
Shapiro D, Cook IA, Davydov DM et al (2007) Yoga as a complementary treatment of depression: effects of traits and moods on treatment outcome. Evid Based Complement Alternat Med 4:493–502
Sharp BM, Roy S, Bidlack JM (1998) Evidence for opioid receptors on cells involved in host defense and the immune system. J Neuroimmunol 83:45–56
Shavit Y, Depaulis A, Martin FC et al (1986) Involvement of brain opiate receptors in the immune suppressive effect of morphine. Proc Natl Acad Sci U S A 83:7114–7117
Shintani Y, Terao Y, Ohta H (2011) Molecular mechanisms underlying hypothermia-induced neuroprotection. Stroke Res Treat 2011:809874
Siems W, Brenke R (1992) Changes in glutathione system of erythrocytes due to enhanced formation of oxygen free radicals during short-term whole body cold stimulus. Arch Med Res 51:3–9
Siems W, Brenke R, Sommerburg O et al (1999) Improved antioxidative protection in winter swimmers. QJM 99:193–198
Silva JE (2006) Thermogenic mechanisms and their hormonal regulation. Physiol Rev 86:435–464
Smolander J, Leppäluoto J, Westerlund T et al (2009) Effects of repeated whole-body cold exposures on serum concentrations of growth hormone, thyrotropin, prolactin and thyroid hormones in healthy women. Cryobiology 58:275–278
Sollom AC, Kneebone N (2007) Treatment of depression in people who have multiple sclerosis. Mult Scler 13:632–635
Stranahan AM, Lee K, Mattson MP (2008) Central mechanisms of HPA axis regulation by voluntary exercise. Neuromolecular Med 10:118–127
Teramoto S, Ouchi Y (1999) A swimming in cold water. Lancet 9191:1733
Tkachuk GA, Garry ML (1999) Exercise therapy for patients with psychiatric disorders: Research and clinical implications. Prof Psychol Res Pract 30:275–282. doi:10.1037/0735-7028.30.3.275
Tullman MJ, Oshinsky RJ, Lublin FD et al (2004) Clinical characteristics of progressive relapsing multiple sclerosis. Mult Scler 10:451–454
Unger KV, Skinar GS, Hutchinson DS et al (1992) Fitness: a viable adjunct to treatment for young adults with psychiatric disabilities. Psychosoc Rehabil J 15:20–28
Vallerand AL, Jacobs I (1989) Rates of energy substrates utilization during human cold exposure. Eur J Appl Physiol Occup Physiol 58:873–878
Van Den Eede F, Moorkens G (2008) HPA-axis dysfunction in chronic fatigue syndrome: clinical implications. Psychosomatics 49:450
van der Watt G, Laugharne J, Janca A (2008) Complementary and alternative medicine in the treatment of anxiety and depression. Curr Opin Psychiatry 21:37–42
Varon J, Marik PE, Einav S (2011) Therapeutic hypothermia: a state-of-the-art emergency medicine perspective. Am J Emerg Med 30:800–810
Wayne TP, Kiernan M, Abby CK (2003) Physical activity as a nonpharmacological treatment for depression: a review. Compl Health Pract Rev 8:139–152
Wen S, Cheng M, Wang H et al (2011) Serum uric acid levels and the clinical characteristics of depression. Clin Biochem 45:49–53
Werneke U, Turner T, Priebe S (2006) Complementary medicines in psychiatry. Review of effectiveness and safety. Br J Psychiatry 118:109–121
Westerlund T, Oksa J, Smolander J, Mikkelsson M (2003) Thermal responses during and after whole body cryotherapy (−110 °C). J Therm Biol 28:601–608
Woźniak A, Wozniak B, Drewa G et al (2007) The effect of whole-body cryostimulation on lysosomal enzyme activity in kayakers during training. Eur J Appl Physiol 100:137–142
Yamauchi T (1989) Whole body cryotherapy is method of extreme cold −175 °C treatment initially used for rheumatoid arthritis. Z Phys Med Baln Med Klin 15:311
Zagrobelny ZB, Halawa C, Niedzielski Z et al (1993) The influence of a single whole body cryostimulation on selected hemodynamic indices and hormone concentrations in the serum of healthy individuals. Pol Tyg Lek 48:303–305
Acknowledgments
I would like to thank all staff of the Department of General Biochemistry at the University of Lodz in Poland, especially Professor Barbara Wachowicz, for support and very useful comments.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Miller, E. (2015). Cryostimulation as Adjunct Treatment in Psychiatric Disorders. In: Dietrich-Muszalska, A., Chauhan, V., Grignon, S. (eds) Studies on Psychiatric Disorders. Oxidative Stress in Applied Basic Research and Clinical Practice. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-0440-2_29
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0440-2_29
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-0439-6
Online ISBN: 978-1-4939-0440-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)