Abstract
Femoral neck fractures are uncommon injuries in children often associated with high-energy mechanisms. An increased risk for osteonecrosis and long-term morbidity associated with these injuries requires heightened suspicion in any high-energy lower extremity trauma scenario. Children are at an increased risk for osteonecrosis after femoral neck fractures due to injury of the medial femoral circumflex and/or retinacular vessels. The Delbet classification system is reliable and prognostic for the risk of osteonecrosis after femoral neck fractures, where Delbet Type I or II fractures are associated with the highest incidence of osteonecrosis. The majority of femoral neck fractures require operative management and treatment is tailored according to age and fracture pattern. Fracture displacement, urgent treatment within 24 h, and fracture type are all significant predictors for the development of osteonecrosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Femoral neck fractures are fortunately uncommon in children. Overall femur fractures account for 2.3 % of children’s fractures, however femoral neck fracture account for less than <1 % [1]. The majority of femoral neck fractures occur secondary to high-energy mechanisms and it is unclear if the incidence of this injury has changed in the last decade, since no specific epidemiological studies have been published. According to the most recent pediatric epidemiology studies, fracture incidence appears to have decreased in the last few decades secondary to less physical activity, improved protective equipment, and increased traffic safety [2, 3]. However, this is unclear, as other studies have shown an increased overall fracture incidence which may be related to increased motor vehicle speeds and increased participation in contact sports [4].
Femoral neck fractures are usually seen in patients after high-energy trauma (i.e. motor vehicle accidents), but pathologic and stress fractures may occur after lower-energy trauma or repetitive impact activities, and one must also be aware of these clinical scenarios in the setting of hip pain in the adolescent patient. Significant complex long-term morbidity can be generated from the injury and/or the treatment of a femoral neck fracture in a child; for this reason, these fractures require sharp recognition and careful examination. The major complication of this injury is due to the tenuous blood supply of the femoral head leading to a high incidence of osteonecrosis (ON) . In the presence of an open physis malunion, nonunion, delayed union, coxa vara , or growth abnormalities can occur after treatment of femoral neck fractures. Development of ON significantly impacts long-term functional outcomes in this population, so efforts to minimize this complication need to be employed. Thus, diminishing the risks of ON and all other complications during treatment of femoral neck fractures in children is of paramount importance to improve functional outcomes.
Clinical Presentation
Femoral neck fractures in children commonly occur after high-energy trauma and adherence to pediatric ATLS protocols must occur during all trauma scenarios. During the musculoskeletal survey, the orthopedic surgeon or emergency medicine physician must suspect a femoral neck fracture when the child is unable to weight bear on the affected lower extremity and presents with a shortened and/or externally rotated limb. Detailed neurovascular evaluation must be performed for all trauma patients; however, in the setting of an open fracture or associated hip dislocation, high suspicion of neurovascular injury must be suspected. Ankle brachial index (ABI) measurements should be obtained when pulses are equivocal, by measuring systolic blood pressure in one upper extremity and comparing that with the ankle systolic blood pressure. An ABI of <0.9 will mandate further vascular assessment with a vascular surgeon consult and/or advanced imaging. Historically, conventional radiology suite arteriography or surgeon-performed arteriography in the emergency or operating room has been used to evaluate such patients. In recent years, advances have included the introduction of mobile digital subtraction angiography (DSA) in the trauma resuscitation room and multi-detector computed tomography arteriography (MDCTA) [5]. Ipsilateral pelvis, knee, and ankle evaluation should be performed when a femoral neck fracture is detected because of the potential associated injury with a femoral neck fracture.
Patients will present with painful range of motion (ROM) and a positive log roll test on the affected hip. Multiple examinations and manipulation of the fractured hip should be avoided to decrease the risk of further fracture displacement. Upon presentation some of the patients will present with immobilization devices; these should be promptly removed in the emergency room because of the significant risk for skin sloughing over the dorsum of the ankle, and pressure over the sciatic nerve [6]. The patient’s limb should be immobilized, and the preferred method for this is with the use of “Bucks” skin traction immobilization with 10 % body-weight traction with a maximum weight of 10 pounds (Fig. 5.1). Alternative immobilization with the use of a posterior splint from the ilium to the ankle will also facilitate easier mobilization, improve pain control, and limit the risk of further fracture displacement. However, skin traction immobilization has demonstrated superior pain control in the setting of femur fractures compared to simple splinting [7]. Readily available skin traction kits allow for gentle traction/immobilization or can be done in the emergency room with ace wrap and Coban (3M™ Self-Adherent wrap), being careful to avoid significant traction over the skin that can increase soft tissue problems.
In the initial hospital setting, it is prudent to counsel parents and patients regarding the potential risk and consequences of the injury and its treatment [8]. Early parent education on the potential risk of ON and need for further treatment will help generate expectations regarding the potential complications associated with this injury.
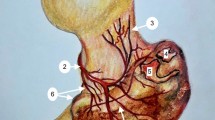
Relevant Surgical Anatomy
The anatomy of the proximal femur has been reported in multiple studies [9–11]. Blood flow to the femoral head is mainly supplied by the retinacular branches (posterosuperior and posteroinferior) of the medial femoral circumflex artery (MFCA). The lateral femoral circumflex artery (LFCA) contributes blood flow to the greater trochanter, small areas of the medial physis, and the anteromedial metaphysis. The artery of the ligamentum teres and the LFCA begin a process of regression after 4 years of age that is completed by age 10. During this period the MFCA progressively becomes the predominant nutrient provider. The end arterial blood flow of the posterosuperior retinacular branch supplies the anterior and lateral femoral head and is the main contributor to femoral head blood flow until skeletal maturity [9]. The exact location of the main vessels is of significant importance when approaching the hip and performing a capsulotomy. It is believed that an anterior capsulotomy avoiding the superolateral ascending branches will not damage the blood supply to the femoral head, as proposed by Ganz et al. [12].
The higher risk of ON after a femoral neck fracture in a growing child can be attributed to the tenuous blood supply illustrated above. At skeletal maturity the retinacular, ligamentum teres, and metaphyseal vessels establish a definitive anastomotic system that improves femoral head circulation and decreases the risk for ON in adults with femoral neck fractures [13]. Proximal femur development is also important to understand when facing a femoral neck fracture. The proximal femoral epiphysis begins to ossify at age 4–6 months in females and at age 5–7 months in males. The trochanteric apophysis begins to ossify at age 4 years. The fusion of the trochanteric apophysis and the femoral epyphysis occurs at age 14 in girls and 16 in boys [14]. Injury to these regions due to the initial trauma or subsequent osteonecrosis potentially may result in a growth disturbance.
Diagnostic Imaging
Diagnostic imaging should always begin with an anteroposterior (AP) pelvic radiograph. The AP pelvis should be obtained with the hips extended and internally rotated (15°) as tolerated by the patient. This view will serve as a comparative view with the contralateral side to assess displacement. The lateral view should be obtained with a cross-table technique to avoid displacement and increased pain with the mobilization of the injured limb required for a frog-leg lateral film. For completion of skeletal assessment, an AP of the femur and lateral radiographs should be obtained.
In the very young child under 2 years of age, ultrasound can be useful to evaluate for occult fractures in a child with post-traumatic hip pain where standard plain films are non-conclusive. An expert radiologist and technician can evaluate the proximal femur with ultrasonography and clear signs of fracture can be found in up to 92 % of confirmed occult fractures, as per previous reports [15]. Ultrasound findings include cortical discontinuity (direct sign of a fracture), epiphyseal mobility, step-off deformities, tiny avulsed bone fragments, double-line appearance of cortical margins, and diffuse irregularity of bone surfaces [15].
Femoral Neck Stress Fractures
Stress fractures of the femoral neck can be difficult to diagnose on plain radiography alone, but important to treat since they carry a risk of becoming complete fractures and subsequently displacing. Although the prevalence in the pediatric population is fortunately infrequent, some patient populations require discussion. Specifically in patients with the female athlete triad (eating disorder, amenorrhea, and decreased bone mineral density), a thorough workup should be undertaken to avoid missing these injuries in a patient with hip pain [16, 17]. When regular X-rays are not diagnostic, the clinician should remain suspicious, and further imaging with a CT scan has been used in the past. This imaging modality will give an excellent outline of the bony anatomy, but could miss an injury that only generates bony edema. For this reason, MRI is preferred for the evaluation of an occult fracture. A linear dark line will be present in all sequences if a fracture is present, and the surrounding marrow edema will be more noticeable in T2 sequences even within the first 24 h after injury. Recently, an algorithm has been proposed for the evaluation and treatment of the child with a stress femoral neck fracture (Fig. 5.2) [17]. Although there is some variation regarding treatment for femoral neck stress fractures, it is suggested that non-displaced fractures on the tension side of the femoral neck should undergo internal fixation [18]. Fractures on the compression (medial) aspect of the femoral neck can be initially treated non-operatively with restricted weight bearing or non-weight bearing. The length of time for weight-bearing restriction can vary between 4 and 8 weeks. Weight bearing can be advanced once the patient is asymptomatic and has full range of motion of the affected hip. If there is concern about the patient’s ability to maintain the restricted weight-bearing status, then percutaneous internal fixation should be considered.
Classification
Femoral neck fractures were originally classified by Delbet in 1907 and reported by Colonna [19]. The classification is commonly used and has proven to be useful and applicable since it not only allows for an accurate morphological assessment, but it also has prognostic significance (Fig. 5.3). In 2006, Moon et al. [20] demonstrated that the risk for development of osteonecrosis increases with the complexity of the fracture and progressively correlates with the Delbet type of injury. Types I, II, and III fractures were 15, 6, and 4 times more likely to develop ON than type IV fractures, respectively. ON rate by Delbet class was I = 38 %, II = 28 %, III = 18 %, and IV = 5 %; this rate of ON has been corroborated in more recent reports [20].
Type I: Transphyseal Fractures
Overall rare, Type I transepiphyseal fractures (Fig. 5.4) constitute 8 % of femoral neck fractures. An isolated injury through the proximal femoral physis is labeled -IA. Type IB has an associated femoral head dislocation from the acetabulum, and it can be present in up to 50 % of Type I fractures. Type IB fractures usually present in young children involved in high-energy trauma. It has also been reported as iatrogenic physeal fracture during closed reduction of a dislocated hip [21]. It is unclear if injury to the growth plate occurs during trauma or with forceful reduction maneuvers thereafter. For this reason, we recommend that closed reduction of a hip dislocation in a child with open proximal physis should be performed under sedation with fluoroscopic guidance in the operating room. The surgeon should consider percutaneous pin fixation of the physis prior to reduction if fluoroscopic views suggest instability of the physis as evidenced by displacement or abnormal separation of the ossific nucleus from the metaphysis compared to the normal contralateral hip. Injuries with femoral head dislocation have a poor prognosis in children. High rates of ON have been described, and premature physeal closure has been reported to be as high as 100 % [1].
Type II: Transcervical Fractures
Transcervical fractures (Fig. 5.5) are the most common type of hip fracture, accounting for half of proximal femur fractures in children. Fortunately, a non-displaced fracture has a low incidence of ON. However, with displaced Type II fractures, the rate of ON has been reported to be 28 % [20]. ON most commonly develops in older children and different etiologies have been proposed, including vessel kinking, and disruption secondary to displacement, as well as increased intracapsular pressure after the fracture.
Type III: Cervicotrocanteric Fractures
Type III fractures (Fig. 5.6) have similar outcomes to type II fractures. Type III injuries are distal on the neck and have an incidence of ON reported from 18 to 30 % in displaced fractures. Appropriate anatomic reduction and fracture site compression can decrease the incidence of this complication [22].
Type IV: Intertrochanteric Fractures
Type IV fractures (Fig. 5.7) have the lowest complication rates, and generally good outcomes secondary to its extracapsular nature. ON rates are reported to be close to 5 %; reports of physeal closure and coxa vara are rare, but have been published.
Treatment
Non-operative Management
Type I non-displaced physeal neck fractures in patients under 2 years of age can be managed with spica casting and close observation to assure no displacement. In patients with mild displacement, a gentle attempt of closed reduction can be performed. If the reduction is anatomic, then stable casting can be performed without fixation. Spica casting should be done with the limb abducted and in neutral rotation to avoid varus and external rotation displacement. Serial radiographs should be obtained 3–5 days after initial casting and then weekly for 3–4 weeks to confirm maintained alignment and healing. Early fracture displacement should warrant immediate fracture reduction and fixation. Spica cast should be utilized for 6 weeks until the fracture is healed.
Non-displaced Type IV fractures in children under 4 years of age can be treated with 12 weeks of spica casting . Again, close observation should be employed, with a low threshold for operative fixation in the setting of displacement. Weekly radiographs for the initial 3–4 weeks are recommended. If the castradiographs are difficult to interpret and displacement is questionable, a limited hip CT scan should be performed to confirm reduction [1].
Operative Management
Closed Reduction and Percutaneous Pinning
Closed reduction and pinning can be performed for certain anatomically reducible neck fractures and in certain physeal separations.
In very young infants and toddlers (under age 2) with unstable physeal separations (Type I) or unstable neck fractures Types II and III, smooth 2 mm Kirschner wires can provide sufficient fixation (Fig. 5.8a, b). For older children above ages 4–6 years with displaced unstable fractures including Type I physeal separations, II and III fractures, cannulated screw fixation is necessary [1]. Respect for fracture stability is of utmost importance, and crossing the physis to obtain stability is more important than potentially creating a minor leg length discrepancy from a premature physeal arrest. Inadequate fixation of the proximal fragment because of fixation short of the physes often results in late displacement and a high rate of ON. In children up to age 8 years, 4.0–4.5 mm cannulated screws can be used; in older children, 6.5 mm cannulated systems are indicated.
Technique
The patient is positioned supine on a flat radiolucent table; a fracture table can also be used depending on the surgeon’s preference and institution’s availability. C-arm fluoroscopy is brought in from the contralateral side; AP and lateral frog views should be obtained prior to starting the procedure to confirm appropriate visualization, without moving the leg to obtain these images.
If fluoroscopy imaging demonstrates fracture displacement, traction internal rotation and abduction are usually necessary to obtain anatomic alignment. If reduction is not anatomic, the surgeon should change plans and perform an open reduction. The greater trochanter (GT) is marked on the skin laterally and percutaneous fixation is inserted laterally through the tensor fasciae latae (TFL) just below the GT but not distal to the lesser trochanter, to prevent the creation of a “stress riser.” K wires or guide wires for cannulated screws are passed through the femoral neck under direct fluoroscopic visualization.
Two or three wires provide enough stability. Wires should be placed across the physis in a parallel fashion. Once appropriate X-ray confirmation of reduction and pin placement is confirmed, wires should be cut and bent over the lateral femoral cortex under the skin. This requires a second procedure for removal of hardware, but avoids migration or risk of infection. In older children, over age 3, reaming can be performed over the pins and appropriate-length cannulated screws placed. Screws should be placed across the physeal scar to prevent torsion stress transfer to the physis. AP and lateral views should confirm adequate screw/pin placement; a total of two screws are sufficient in young children and in older adolescents, three screws give excellent fixation but sometimes are difficult to insert due to the size. Screws should be drilled and tapped to avoid rotational fracture displacement during screw insertion. Some authors recommend hip joint aspiration to relieve the hemarthrosis that can theoretically decrease flow of the retinacular vessels to the femoral head [23].
Open Reduction
Open reduction of a femoral neck fracture is indicated when anatomic closed reduction cannot be attained by gentle manipulation. The fractures that require this type of procedure should be treated in an urgent manner (<24 h) since this potentially decreases the risk of developing ON [23].
Approaches
An anterolateral (Watson-Jones) is a useful approach for Delbet Types Ia, II, and III femoral neck fractures. The patient is positioned supine with the greater trochanter on the edge of a flat radiolucent table.
A 5–8 cm straight longitudinal incision is centered on the tip of the greater trochanter. With this approach there is no true internervous plane; gluteus medius and the tensor fasciae latae (TFL) are both innervated by the superior gluteal nerve.
The interval between TFL and gluteus medius is developed bluntly and retractors placed to expose gluteus medius and vastus lateralis distally. The anterior border of gluteus medius is identified and retracted posterior/superiorly or, if necessary, a third of its insertion is elevated from the GT. This will expose the femoral neck and the hip capsule and allow for open reduction of a femoral neck fracture and or decompression of the hip joint [24].
A lateral (Hardinge) approach is useful for Delbet Type Ib and IV femoral neck fractures. The patient is positioned supine with greater trochanter on edge of flat radiolucent table. The incision is 5–8 cm straight longitudinal centered on the tip of the greater trochanter.
There is no true internervous plane; gluteus medius and the tensor fasciae latae (TFL) are innervated by the superior gluteal nerve. The dissection is between the interval between TFL and gluteus medius , is developed bluntly, and retractors placed to expose gluteus medius and vastus lateralis distally. The gluteus medius is identified and split, starting in the midpoint of the insertion on the GT and continuing proximally for a maximum of 3 cm. Injury to SGN can be caused if dissection is carried further proximally.
The anterior part of the gluteus medius muscle with its underlying gluteus minimus and the anterior part of the vastus lateralis muscle are elevated from the GT and retracted anteriorly. After this is done, the femoral neck and the anterior hip joint capsule will be exposed [24].
Once adequate exposure of the fracture site is achieved, anatomic reduction of the fragments is performed with the help of bone-reduction clamps. The femoral neck can be brought anteriorly with the help of a bone hook placed anteriorly over the medial neck, and after reduction is achieved, this is confirmed with fluoroscopy and palpation. Fixation with cannulated screws or pins is performed as described above.
Occasionally, it is useful to perform an anterior Smith-Peteresen approach combined with a lateral approach. This allows optimal visualization of the fracture and assurance of a decompression with anatomic reduction, as the anterior approach will bring the exposure directly down onto the fracture site. This approach should be familiar to most orthopedic surgeons and utilizes the interval between the tensor and sartorius superficially, and exposing and retracting the rectus at the deep layer. This exposes the capsule which can be opened directly on the neck. The concomitant lateral approach will allow for further control of the fracture and for optimal exposure for implant placement.
Plate Fixation
There are a variety of implants available for fractures amenable to plate fixation , which are usually Delbet Type III and IV fractures. The available implants include standard dynamic hip screw constructs, which are sized for children, adolescents, and adults (Fig. 5.9). There are also newer generation pediatric locking plates which allow for locking screw placement into the femoral neck. These come in sizes of small (3.5 mm) or larger (5.00 mm) and have varying degrees of fixed screw-plate angles. There are no surgeon-specific guidelines for which size implant to use, and having a couple of sizes available will allow for intraoperative decision given the size of the femur.
A pediatric plate and screw device provides excellent fixation for Type III and IV fractures, as failures of cannulated screws can occur (Fig. 5.10a–c).
Technique
Incision is made starting at the base of the GT and carried on distally. Usually 6–8 cm is sufficient for plate fixation. Subcutaneous tissue is divided with the use of eletrocautery and TFL is exposed and incised in line with its fibers. The vastus lateralis is then visualized and an “L” type incision over its fascia is performed, detaching it vertically 1 cm distal from its insertion on the GT, and then in line with its fibers longitudinally on the posterior border. Leaving a 5 mm posterior cuff of vastus fascia can aid in later closure. The sub-vastus approach is carried out elevating vastus anteriorly and exposing the lateral femoral cortex.
Once reduction is confirmed, a guide wire is drilled through the center of the femoral neck. This can be drilled with a device guide, achieving the appropriate femoral neck-shaft angle (most commonly a 135° device is utilized). The guide wire does not need to transfix the femoral physis for Type IV fractures; position is confirmed with AP and lateral fluoroscopic views. Before drilling, an anti-torque wire can be placed parallel and superior to the hip screw guidewire to avoid rotational displacement. The appropriate screw length is measured with a depth gauge and the screw hole is drilled over the guide wire. The lag screw is placed and a three-hole side plate is passed over the screw. The plate is secured with bicortical screws and final hardware positioning is checked under fluoroscopy.
Newer generation locking-plate fixation is performed in a similar manner with cannulated techniques, to allow for optimal locking screw placement via placement of correctly placed guide wires through plate-specific guides. These plate–screw constructs allow potentially greater fixation in osteopenic bone than a dynamic hip screw, giving the locking technology and the ability to place multiple screws into the femoral neck.
Postoperative Management
A spica cast should be used in patients who have risk of displacement after operative management , because of limited fixation (k-wires), uncontrollable behavior, or poor bone biology. In general, most children under age 8 will tolerate a one-legged spica appropriately. The spica can be maintained for 6 weeks in patients under 8 years of age with Delbet I, II, and III fractures. For patients requiring spica cast immobilization after a closed reduction, weekly radiographic follow-up should be maintained for 3–4 weeks until callus formation is present. Older patients as well as Delbet Type IV fractures should receive stable fixation, and they will likely be stable enough to allow for progressive weight bearing.
A gradual return to weight-bearing activities is instituted after evidence of callus formation and fracture healing, usually at a minimum of 6 weeks. However, most families should be counseled regarding non-weight bearing for up to 3 months. Return to regular activities can be allowed at 3–6 months after injury if clinical and radiographic healing is evident and appropriate rehab has been performed. Return to full sports can be allowed after return of painless range of motion and full strength. Follow-up should be done on a regular basis approximately every third month for the first year to monitor for ON, and then yearly until maturity in order to evaluate for femoral neck fracture complications.
Complications and Outcomes
Due to the fact that femoral neck fractures have high rates of complications, operative management has increased in the last few decades. It is well known that anatomic reduction will improve outcomes and avoid malunions. Outcomes after femoral neck fractures have been studied, and recent reports have demonstrated good outcomes in approximately 60 %, fair in 20 %, and poor results in 20 % of patients with this injury [23].
Osteonecrosis (ON)
Osteonecrosis is the most severe complication following femoral neck fractures in the pediatric population, and also the most difficult to manage. Greater rates of ON and nonunion are seen with higher energy fractures such as Delbet I and II fractures. Recent reviews have reported a 23 % average of ON after femoral neck fractures ranging from 40 % in Delbet I (a rate of 100 % was for IB fx) to 5 % in Type IV fractures. Rates of ON in fractures treated with open reduction are 2.5 times higher than with closed reduction, but it is unclear if this is due to the surgical treatment or more likely to the severity of the injury requiring an open reduction. Urgency of surgical reduction is also relevant when treating femoral neck fractures, as the risk of ON is four times higher when definitive treatment is delayed greater than 24 h after injury. Decompression of the hip joint after a femoral neck fracture remains controversial. Some studies have supported joint decompression, but others have failed to find differences in risk of ON [23–27]. The authors believe that when an open reduction is required, a routine decompression can be performed with low morbidity, and hence recommend decompressing the joint in displaced femoral neck fractures. Review of 72 femoral neck fractures at the authors’ institution has demonstrated that displacement, treatment within 24 h, and fracture type are significant predictors of a patient developing ON. Odds of developing ON after suffering a displaced femoral neck fracture are 9.4 times the odds of a subject without a displaced fracture (95 % CI 1.3–69.5). Delbet Type I had 14 times the odds of developing ON (95 % CI: 1.08–175.58) and Type II fractures had four times the odds of developing ON (95 % CI: 1.09–16.41) when compared to Type III fractures [28].
The treatment of femoral head ON should take into consideration the patient factors such as age, activity level, and medical comorbidities, along with the clinical and radiological findings. The size and location of the necrotic segment, degree of femoral head depression, presence of acetabular involvement, and the morbidity of the surgical procedure planned are the major factors in deciding the treatment plan.
Treatment options for ON can be categorized as: non-surgical/medical treatment, joint-preserving procedures, and prosthetic replacements. The role of medications in osteonecrosis is still experimental and limited. Proposed medications include low-molecular-weight heparins, statins, and bisphosphonates. Many joint-preserving procedures have been described for the management of precollapse and early stages of ON. There is no single procedure that has produced reproducible and satisfactory long-term results. Some of the commonly used joint-preserving surgical procedures include:
-
Core decompression
-
Vascularized bone grafting
-
Non-vascularized bone grafting
-
Bone marrow and bone morphogenic protein injection
-
Acetabular and femoral osteotomies
Nonunion
Femoral neck nonunion is defined as a failure of fracture healing greater than 6 months after initial treatment, and is a complication which occurs in approximately 11 % of pediatric femoral neck fractures. Delbet Type II fractures have an increased risk of nonunion, while Type IV present a smaller risk, which is related to the anatomical blood supply. Mechanical forces related to non-stable fixation can be implicated in the majority of cases. The presentation of a nonunion requires further operative treatment to decrease the shear forces at the fracture site; commonly this is facilitated with a subtrochanteric valgus femoral osteotomy.
Infection
Infection is a rare complication following pediatric femoral neck fracture fixation. Irrigation and debridement should be performed; implant retention is usually necessary until fracture healing has occurred. Appropriate cultures should be obtained and intravenous antibiotics should be used according to the results of the cultures. Femoral neck infection can progress into a nonunion, malunion, or osteonecrosis, thus further complicating the patient’s outcome, as such early aggressive treatment can minimize these potential complications.
Malunion/Coxa Vara and Premature Physeal Closure (PPC)
Coxa vara is defined as a femoral neck-shaft angle of <120° and is the second most common complication of hip fractures in children. In a recent meta-analysis, coxa vara was reported to be present in 153 of 828 patients (18.5 %) with femoral neck fractures. Review of the literature demonstrates that the risk of coxa vara is decreased in patients treated operatively, and is a clear risk factor for development of hip osteoarthritis (OA). Epyphysiodesis of the greater trochanter is a treatment option for children younger than age 8 years to prevent further variation. PPC has been reported to develop in 22 % of patients with this injury [23]. Closure of the physis will affect patients differently depending on the age of presentation. Secondary angular deformity and leg length discrepancy on occasions will require further surgical treatment.
Conclusions
-
Femoral neck fractures are rare in the pediatric population, but the potential complications are severe, and pediatric orthopedic surgeons must be familiar with management of each type of injury appropriately in order to minimize risk of developing complications.
-
The Delbet classification is reliable and prognostic, and currently the preferred classification for femoral neck fractures.
-
Anatomic reduction can decrease deformity and should be the goal of operative intervention. Displaced femoral neck fractures should be treated urgently (<24 h) to decrease risk of ON.
-
Patients under age 8 with risk of displacement after operative management should be considered for immobilization with a one-legged spica.
-
Incidences for ON, nonunion, coxa vara , and PPC are 23 %, 8 %, 17 %, and 22 %, respectively. Incidence of complications rises according to severity of injury.
-
Displacement, treatment within 24 h, and fracture type are significant predictors of a patient developing ON.
References
Beaty JH, Kasser JR. Rockwood and Wilkins’ fractures in children. Philadelphia, PA: Wolters Kluwer/Lippincott, Williams & Wilkins; 2010. p. 769–96.
Tiderius CJ, Landin L, Duppe H. Decreasing incidence of fractures in children: an epidemiological analysis of 1,673 fractures in Malmo, Sweden, 1993-1994. Acta Orthop Scand. 1999;70(6):622–6.
Randsborg PH, Gulbrandsen P, Saltytė Benth J, Sivertsen EA, Hammer OL, Fuglesang HF, et al. Fractures in children: epidemiology and activity-specific fracture rates. J Bone Joint Surg Am. 2013;95(7):e42.
Omori G. Bone and joint diseases in children. Epidemiology of childhood fractures. Clin Calcium. 2010;20(6):881–6.
Feliciano DV. Management of peripheral arterial injury. Curr Opin Crit Care. 2010;16(6):602–8.
Daugherty MC, Mehlman CT, Moody S, LeMaster T, Falcone Jr RA. Significant rate of misuse of the hare traction splint for children with femoral shaft fractures. J Emerg Nurs. 2013;39(1):97–103.
Irajpour A, Kaji NS, Nazari F, Azizkhani R, Zadeh AH. A comparison between the effects of simple and traction splints on pain intensity in patients with femur fractures. Iran J Nurs Midwifery Res. 2012;17(7):530–3.
Skaggs DL, Flynn JM, Price CT. Trauma about the pelvis/hip/femur. In: Flynn JM, Skaggs DL, editors. Staying out of trouble in pediatric orthopaedics. Philadelphia: Lippincott Williams & Wilkins; 2006.
Chung SM. The arterial supply of the developing proximal end of the human femur. J Bone Joint Surg Am. 1976;58(7):961–70.
Johnson EO, Soultanis K, Soucacos PN. Vascular anatomy and microcirculation of skeletal zones vulnerable to osteonecrosis: vascularization of the femoral head. Orthop Clin North Am. 2004;35(3):285–91. viii.
Trueta J, Harrison MH. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br. 1953;35-B(3):442–61.
Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–24.
Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip fractures in children. J Am Acad Orthop Surg. 2009;17(3):162–73.
Hansman CF. Appearance and fusion of ossification centers in the human skeleton. Am J Roentgenol Radium Ther Nucl Med. 1962;88:476–82.
Cho KH, Lee SM, Lee YH, Suh KJ. Ultrasound diagnosis of either an occult or missed fracture of an extremity in pediatric-aged children. Korean J Radiol. 2010;11(1):84–94.
Haddad FS, Bann S, Hill RA, Jones DH. Displaced stress fracture of the femoral neck in an active amenorrhoeic adolescent. Br J Sports Med. 1997;31(1):70–2.
Er MS, Eroglu M, Altinel L. Femoral neck stress fracture in children: a case report, up-to-date review, and diagnostic algorithm. J Pediatr Orthop B. 2014;23(2):117–21.
Lehman Jr RA, Shah SA. Tension-sided femoral neck stress fracture in a skeletally immature patient. A case report. J Bone Joint Surg Am. 2004;86-A(6):1292–5.
Colonna PC. Fracture of the neck of the femur in childhood: a report of six cases. Ann Surg. 1928;88(5):902–7.
Moon ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma. 2006;20(5):323–9.
Herrera-Soto JA, Price CT, Reuss BL, Riley P, Kasser JR, Beaty JH. Proximal femoral epiphysiolysis during reduction of hip dislocation in adolescents. J Pediatr Orthop. 2006;26(3):371–4.
Morrissy RT, Weinstein SL. Management of fractures. In: Morrissy RT, Weinstein SL, editors. Lovell & Winter’s pediatric orthopaedics. Philadelphia, PA: Lippincott, Williams & Wilkins; 2005.
Yeranosian M, Horneff JG, Baldwin K, Hosalkar HS. Factors affecting the outcome of fractures of the femoral neck in children and adolescents: a systematic review. Bone Joint J. 2013;95-B(1):135–42.
Hoppenfeld S, deBoer P, BuckleyHoppenfeld R. Surgical exposures in orthopaedics: the anatomic approach. 4th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2009.
Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS. Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br. 2002;84(1):108–12.
Ng GP, Cole WG. Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury. 1996;27(6):419–21.
Song KS. Displaced fracture of the femoral neck in children: open versus closed reduction. J Bone Joint Surg Br. 2010;92(8):1148–51.
Spence D, DiMauro JP, Miller PE, Glotzbecker MP, Hedequist DJ, Shore BJ. Osteonecrosis after femoral neck fractures in children and adolescents: analysis of risk factors. J Pediatr Orthop. 2016;36(2):111–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Gomez, J.A., Shore, B.J., Hresko, M.T. (2016). Fractures of the Femoral Neck in Children. In: Hedequist, D., Heyworth, B. (eds) Pediatric Femur Fractures. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7986-5_5
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7986-5_5
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7984-1
Online ISBN: 978-1-4899-7986-5
eBook Packages: MedicineMedicine (R0)