Abstract
Distal femur fractures in children include physeal fractures (Salter-Harris I–IV) and isolated epiphyseal fractures, which are intra-articular knee injuries occurring most commonly in association with lateral patellar dislocations. Adolescents and preadolescents sustain both categories of distal femur fractures more commonly than younger children.
Distal femoral fractures generally involve high-energy mechanisms of injury, such as motor vehicle accidents and sports injuries. A common mechanism is a direct varus blow or direct valgus blow to the knee, with the foot planted. Alternatively, osteochondral shear injuries to the lateral aspect of the lateral femoral condyle are caused by lateral patellar dislocations, stemming from twisting injuries to the knee.
A thorough neurovascular exam of the affected limb and meticulous secondary survey should be performed for all suspected distal femoral fractures, as concomitant injuries are common. Plain AP and lateral radiographs of the femur and the knee are generally diagnostic, though MRI or CT scan may be necessary to identify intra-articular osteochondral fragments or Salter-Harris III and IV fractures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Distal femur
- Physeal fractures
- Pediatric and adolescent femur fractures
- Sports medicine injuries
- Intra-articular knee fractures
Introduction and Epidemiology
Distal femur fractures that do not involve the diaphysis can generally be divided into three categories, consisting of (1) those that involve the distal femoral physis, either with (i.e., Salter-Harris II) or without (i.e., Salter-Harris I) extension into the metaphysis; (2) physeal fractures that extend into the epiphysis (Salter-Harris III or IV); and (3) those that are limited to the epiphyseal region, which generally consist of lateral femoral condylar osteochondral shear fractures following lateral patellar dislocation.
Distal femoral physeal fractures are relatively rare, representing approximately 2 % of all physeal fractures [1–3], but have a relatively high complication rate, the most common of which is growth disturbance due to partial or complete premature physeal closure (i.e., bony “bar” formation). Such sequelae, which may occur in up to half of cases [4], make close monitoring of these fractures in the post-injury or postoperative period through skeletal maturity critical to avoid clinically significant angular deformities or leg length discrepancies. Due to the high energy required to cause these fractures, displacement and instability are common, and in general, nonoperative treatment is pursued less commonly than fixation, the principles of which are described in a below section. Adolescents and preadolescents are the most affected age group for distal femoral physeal injuries [5], in part because of increases in sports participation and sports-related injuries , which represents a common mechanism of injury for these fractures.
The treatment of Salter-Harris III or IV fractures of the distal femur, or osteochondral fractures that involve significant portions of the weight-bearing zones of the articular surface, should consist of anatomic reduction and fixation so as to optimize the long-term outcome and avoid degenerative joint disease. While Salter-Harris III or IV fractures are relatively rare, the prevalence of osteochondral fractures associated with acute patella dislocation ranges from 19 to 50 % [6–8]. Osteochondral fracture fragments may range from small incidental loose bodies to large portions of the articular surface. While osteochondral fractures occur in the patella even more commonly than the lateral femoral condyle, the treatment of patellar lesions is beyond the scope of this chapter, so the focus will be on treatment of condylar fractures, the principles of which are nearly identical to those of the patella. Treatment of intra-articular osteochondral fractures generally involves an initial arthroscopy and includes removal of small loose bodies, but fixation for larger osteochondral fragments. The underlying or resulting patellar instability is sometimes addressed with concurrent stabilization surgery, in the form of medial retinacular repair or reefing, medial patellofemoral ligament (MPFL) reconstruction, lateral retinacular release, and/or distal realignment techniques, such as tibial tubercle osteotomy for skeletally mature adolescents, and soft-tissue tendon transfers in the skeletally immature.
Mechanism of Injury
Fractures of the distal femoral physis are often high-energy injuries, such as from motor vehicle accidents, sports-related injuries, or, occasionally, falls from height. Fracture patterns relate to the underlying anatomical changes of the growing child. The collateral ligaments and their bony attachments in an adolescent or a child are actually relatively stronger than the cartilaginous growth plate. Therefore, the classically described mechanisms that lead to high-grade medial collateral ligament (MCL) or lateral collateral ligament (LCL) /posterolateral corner (PLC) tears in an adult—lateral or medial direct blows to the knee, respectively, with a planted/fixed foot—will instead cause a distal femur Salter-Harris fracture in a skeletally immature patient. Hyperflexion or hyperextension injuries can lead to fracture patterns with displacement in the sagittal plane.
Distal femoral osteochondral fractures , on the other hand, stem from either a direct blow to the knee with a shearing force applied to either the medial or lateral femoral condyle (LFC) or more commonly a flexion-rotation injury in which internal rotation at the knee is paired with a strong quadriceps contraction. When the patella dislocates in this scenario, the medial edge of the patella impacts the prominent edge of the LFC before it slides back into the trochlear groove due to pull of the quadriceps. Either the dislocation or the relocation phase of this injury can cause an osteochondral fracture to the LFC, the medial facet of the patella, or both.
Other mechanisms of injury are less common. Newborns can sustain distal femoral physeal fractures from birth trauma, with identified risk factors including prolonged labor, macrosomia, and breech presentation [9]. Child abuse, sometimes identified through the presence of a subtle metaphyseal fragment or “corner fracture,” most commonly occurs in infants and toddlers [10]. As with all types of fractures, pathologic fractures can occur with lower energy mechanisms due to underlying metabolic bone disease or osteopenia, and nonambulatory patients with cerebral palsy and other neuromuscular disorders may sustain distal femoral physeal injuries from falls or direct blows .
Evaluation and Diagnosis
Presentation and Physical Examination
Due to the high-energy mechanisms that often cause distal femur physeal fractures, awareness of concomitant fractures and other injuries is essential in the initial evaluation. A thorough secondary survey should be performed, particularly in the setting of a motor vehicle accident or a fall from height. In approximately 10–15 % of cases of distal femur fractures [11, 12], other long bone fractures or ligamentous disruptions about the knee will be present, such as cruciate ligament tears. A standard orthopedic trauma workup, including assessment of the spine and pelvis and neurovascular assessment of the involved distal extremities, should be performed. While open fractures and major arterial injuries are rare, occurring in 3 % of cases, the initial evaluator should carry a low threshold to perform Doppler ultrasound and/or assess ankle-brachial indices (ABI) , particularly with severely displaced fractures or following severe hyperextension knee injuries. Compartment syndrome following distal femoral fractures is rare, occurring in 1.2 % of cases in one series [11], and will typically arise in the hours or day after the initial injury. The peroneal nerve may be injured in up to 7 % of displaced distal femoral fractures [11]. Concomitant injuries are rare with patellar dislocations, though ligament tears (other than MPFL tears, which are an inherent component of virtually every patellar dislocation, to varying degrees), such as MCL and anterior cruciate ligament (ACL) ruptures, can occur. Most cases of distal femoral physeal injuries or patellar dislocations occur in isolation, however, particularly when presenting as sports injuries.
Children with distal femur fractures will usually refuse to bear weight, and deformity may be obvious, even before radiographs are obtained. Swelling and ecchymosis are often present about the knee, and severe effusions are common, particularly with Salter-Harris III or IV fractures and osteochondral shear fractures of the condyles. Lower energy Salter-Harris I or II fractures can be more subtle, however, with children able to bear weight, albeit with discomfort, and differentiation from other knee injuries, such as meniscal or ligament injuries, is important. Varus and valgus stress exams should be performed , which may show instability due to the compromised distal femoral physis. Lateral or medial tenderness in the region of the distal femoral physis may also direct the diagnosis. A stable knee with tenderness to palpation over the medial patella, medial epicondylar region (Bassett’s sign), and lateral aspect of the lateral femoral condyle are most common in association with lateral patellar dislocation. Late exam findings in such cases may reveal signs of a loose body, with locking or catching of the knee. Early splinting with long leg plaster splints or knee immobilizers is warranted for early stabilization and to improve comfort.
A thorough imaging assessment, with plain radiographs and possibly computed tomography (CT) and/or magnetic resonance imaging (MRI), is the next step in the diagnostic workup, once concurrent limb-threatening injuries have been ruled out and the affected lower extremity stabilized.
Diagnostic Imaging and Classification
Anteroposterior (AP) and lateral femur radiographs should be obtained in all cases of suspected distal femur fractures. Radiographic assessment of the proximal femur and femoral head is critical, particularly for high-energy injuries, as concomitant femoral neck fractures can occur with femoral shaft and distal femoral fractures, and failing to diagnose such fractures, even when non-displaced, can have catastrophic sequelae. When the injury is localized to the knee, dedicated AP and lateral knee radiographs should be obtained, with lateral and medial oblique knee radiographs added at times to better elucidate subtle fractures or in the face of diagnostic uncertainty. Dedicated tibia/fibula radiographs may be warranted at times, especially in patients with concurrent leg or ankle complaints.
Findings typical of the radiographs in a distal femoral physeal fracture include physeal widening that may be seen in isolation (suggesting a Salter-Harris I fracture), or in association with extension of the fracture line into the metaphysis (Salter-Harris II) , epiphysis (Salter-Harris III) , or both metaphysis and epiphysis (Salter-Harris IV ). Salter-Harris V fractures, which represent an axial compression phenomenon on the distal femoral physis, or Salter-Harris VI fractures [13, 14], in which a collateral ligament avulses a condylar fragment of bone containing a segment of peripheral physis, have been described but are rare. SH-V injuries have been described most commonly following a fall from height and will generally have negative radiographs, but may be picked up on MRI, due to the presence of bone marrow edema on one or both sides of the physis [15]. These have a high rate of premature closure of the physis. Interestingly, in most anatomic locations, the Salter-Harris system is fairly predictive of rates of premature physeal closure, with the higher grades (SH-III and SH-IV) having higher rates of closure. However, the distal femoral physis is particularly sensitive to even minor disruptions, with all Salter-Harris types having high rates of premature physeal closure, which has been described even in tibial shaft injuries [15–18]. In these cases, occult SH-V injuries to the distal femoral physis may have been present .
For a possible osteochondral fracture of the condyle, a skyline plain radiograph should be added to the knee series, though patients may not be able to achieve the degree of knee flexion necessary for this view. Because osteochondral fragments may involve large portions of cartilage with only a sliver of bone, radiographs should be carefully assessed for even the smallest ossific fragment. One study suggested that radiographs failed to identify osteochondral fracture in 36 % of children who had such injuries found during arthroscopy [19]. MRI should therefore be considered in all cases of lateral patellar dislocation with an associated effusion. For suspected distal femoral physeal fractures not clearly identifiable with radiographs, MRI can show a subperiosteal hematoma about the physis and adjacent metaphysis, though comparison radiographs of the contralateral knee may also allow for elucidation of subtle physeal widening characteristic of Salter-Harris I fractures. One series reported seven cases of such fractures clearly seen on MRI, but with negative radiographs [20].
While “stress views” of the knee or distal femur were historically recommended to identify non-displaced Salter-Harris I or II fractures, this approach is rarely used today, given the pain and potential fracture displacement associated with the involved varus or valgus stress maneuver, and the greater availability of advanced imaging modalities. Modern CT scan sequences have been developed to decrease the amount of radiation used in children compared to historical techniques, and can be obtained more quickly than MRI. Because decisions regarding surgical stabilization often relate to the degree of displacement or stepoff across an articular surface, a CT scan may be indicated for Salter-Harris III or IV fractures, or osteochondral fractures about the knee [21, 22].
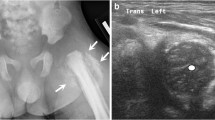
The role of ultrasonography (US) is limited to physeal fractures in infants and newborns, but may help assess displacement of a distal femoral fracture in which there is minimal developmental ossification [23].
Treatment Options and Outcomes
Nonoperative Treatment: Salter-Harris I and II Fractures
Non-displaced or minimally displaced Salter-Harris I or II distal femoral physeal fractures may be treated with long leg casts or even long leg braces, such as locked hinged braces or knee immobilizers, provided that they are utilized like casts. However, casting is generally more likely to optimize stability of the healing fracture in the first 2 weeks post-injury and thereby minimize discomfort. Moreover, a circumferential fiberglass cast, with or without inclusion of the foot, eliminates concerns related to noncompliance with brace wear, which can be an issue in the pediatric and adolescent patient populations. Because some of these fractures are relatively stable, transitioning after 2–4 weeks from a cast to hinged brace—which can be unlocked when not ambulating to work on range of motion, thereby helping to combat stiffness and deconditioning of the periarticular musculature—can be considered if there is a truly stable pattern and/or early signs of healing are present.
It is important to remember that more displacement may have occurred at the time of injury than the presenting radiographs demonstrate, and that severe soft-tissue swelling and ecchymosis may be an indication of an unstable fracture, which should prompt consideration of fixation to optimize stability and healing. One study demonstrated that over one-third of a series of 82 patients with distal femoral physeal fractures treated with closed reduction and casting progressed to redisplacement in the first 2 weeks, only one-quarter of which were to be remanipulated later [11, 12]. This and other studies underscore the dangers of pursuing less treatment than may be necessary, given the considerable energy associated with femur fracture injuries. For the truly stable fractures, however, serial radiographs, which may demonstrate subperiosteal and/or periphyseal new bone formation, will inform considerations of transitioning from casting to bracing .
Salter-Harris III and IV Fractures
Salter-Harris III and IV fractures of the distal femur are rarely non-displaced enough to warrant nonoperative treatment. Because radiographs may not show subtle degrees of subchondral stepoff that could have significant long-term implications on the development of degenerative joint disease, advanced imaging should be obtained before management decisions concluded (Fig. 12.1a–c). Even for minimally displaced fractures, there may be a role for minor reductions and stabilization to insure maintenance of anatomic subchondral surfaces with minimal stepoff at the level of the articular cartilage. Moreover, the earlier range-of-motion exercises allowed by such stabilization have been shown to be beneficial for healing cartilage and preventing stiffness.
Intra-articular Osteochondral Fractures
Nonoperative treatment of intra-articular condylar osteochondral fractures associated with patellar dislocation is reserved only for small fragments, 5–8 mm or less, that are unlikely to cause symptoms associated with loose body fragments. Occasionally, larger fragments will adhere to the soft tissues in a non-weight-bearing region of the joint, such as the medial or lateral gutter or the posterior intercondylar notch. In such cases, particularly when presenting in delayed fashion (>2–4 weeks), non-operative management can be considered, but the risk of future displacement with intra-articular injury to the joint surfaces by the fragment should be discussed with the patient and family.
Operative Treatment: Salter-Harris I and II Fractures
Displaced distal femoral physeal fractures warrant restoration of the physeal anatomy, periphyseal alignment, and a form of stabilization that respects the presence of the still biologically active physis, the normal future function of which is in question with all distal femoral fractures. While fracture tables involving traction constructs may be reasonable, they are usually not necessary, and a simple radiolucent table is favored by most authors. The first step for displaced fractures is achieving a perfect reduction, which should be performed under general anesthesia or adequate intravenous sedation to minimize further shear forces across the chondral tissue of the physis. Understanding of the fracture pattern and which sleeve of periosteum about the physis remains intact and can be utilized as a tether to achieve the reduction is critical. For example, a Salter-Harris II fracture sustained by a direct valgus blow to the lateral aspect of the knee will generally have an intact lateral periosteum against which varus stresses can be applied to achieve anatomic approximation of the medial physis.
While closed techniques are usually sufficient to obtain an anatomic reduction, if one cannot be obtained, an open incision on the side that the fracture originated (most commonly, the medial physis for Salter-Harris II fractures) should be made to assess for periosteal interposition and optimization of the physeal approximation. Following anatomic reduction, choice of fixation depends on the fracture pattern. For Salter-Harris II fractures that have an adequately sized Thurston-Holland fragment to accommodate one to three large screws (6.5 or 7.3 mm), good stability can be achieved with cannulated, partially threaded screws placed parallel and just proximal to the physis from the fragment side to the unfractured metaphyseal side. Generally, washers on the fracture fragment side are also advisable to prevent breakthrough of the screw head through the relatively thin metaphyseal cortical bone during compression. However, when multiple screws are placed on relatively smaller metaphyseal fragments, it is not uncommon to have insufficient room for multiple washers, in which case a single washer can be used to achieve compression and optimize the reduction, while additional screws reinforce the construct without washers. Smaller sized screws, such as one or two 4.5 mm screws, can also complement a single larger screw that achieves the reduction. Bicortical purchase may be pursued, but given the large size of the screws, it is often not necessary, and care should be taken to prevent screw tip protrusion beyond 1–2 mm. Because most Salter-Harris II fractures have a lateral metaphyseal fragment, medial soft-tissue irritation just above the epicondyle is not an uncommon complaint when the screw tips are placed beyond the cortex. The best way to appreciate the exact position of the screw tips is to use live fluoroscopy while rotating the knee at least 30° in either direction from the anteroposterior plane. Removal of hardware is not necessary in most cases, but in children with significant growth remaining the screws often “migrate” proximally toward the diaphyseal segment over time, making any extruded screw tips longer relative to the metaphysis. Some authors favor empiric screw removal, but this remains an evolving concept within all of pediatric orthopedic surgery .
For Salter-Harris I fractures or S-H II fractures with metaphyseal fragments too small to safely accommodate a screw, transphyseal smooth k-wires are placed in a crossed, X-shaped construct to optimize stability. Authors have described pin sizes between 2.4 and 3.2 mm. These can be placed in anterograde fashion from metaphysis to epiphysis, with the pin tips advanced to just short of the subchondral bone, or in retrograde fashion from epiphysis to metaphysis [24]. With this latter approach, care is taken to place the epiphyseal entry point at least 1–2 mm off of the articular surface to avoid chondral injury. However, because this approach necessarily leaves segments of the hardware within the knee joint, two strategies are pursued to avoid bacterial seeding of the intra-articular k-wires and minimize the risk of septic arthritis. One technique is advancing the k-wires all the way out of the skin proximally in the thigh, and pulling the k-wires further proximally, so that the trailing tip of the pin sits in the subchondral bone and the leading tip is cut and bent at the level of the skin of the thigh, to be removed manually weeks later in the office setting [25]. The second technique is placing the trailing tip of the retrograde-placed k-wire deep to the skin, thereby protected from external microbes and bacterial skin flora that would otherwise potentially migrate down the pin into the joint, with a plan to remove the wires with a secondary surgery after sufficient healing has been achieved. Due to several studies demonstrating cases of septic arthritis, leaving retrograde-placed pins out of the skin at the level of the knee is no longer routinely favored.
Rarely, plating of distal femoral physeal fractures is pursued, with the plate spanning the physis, screws placed parallel to the physis, proximal and distal, and optimal stability achieved. While this technique has the distinct disadvantage of larger incisions, even when minimally invasive submuscular plating techniques with percutaneous proximal screw placement are used, good outcomes have been reported in one series [25].
Salter-Harris III and IV Fractures
Salter-Harris III and IV fractures warrant anatomic reduction and stable fixation. Occasionally this can be achieved without performing an arthrotomy, which may decrease the chances of knee stiffness that comes with the extra dissection and disruption of the joint capsule. However, due to the importance of optimally restoring articular congruity in a young, active patient, surgeons should have a low threshold to open the joint (Fig. 12.2) or use arthroscopy (Fig. 12.3a–c) to confirm an anatomic reduction. Moreover, radiographs should show normal physeal thickness at all levels, and similar to Salter-Harris II fractures, periosteal interposition should not be overlooked as a potential block to an anatomic reduction [26]. Screw constructs and directionality vary according to the fracture pattern, but in skeletally immature patients, screws must often be placed very exactly, just below the physis, but just above the roof of the intercondylar notch to avoid iatrogenic cruciate ligament injury (Fig. 12.4a–d). However, in patients with closing growth plates, screw constructs may cross the growth plates to optimize the reduction and fixation construct (Fig. 12.5a–c).
(a) Fluoroscopic image of the same patient from Fig. 12.1 demonstrating arthroscopic assistance of reduction. (b) Arthroscopy image of the same patient from Fig. 12.1 demonstrating minimal persistent displacement following reduction of stepoff and provision wire fixation. (c) Arthroscopy image of the same patient from Fig. 12.1 demonstrating optimization of the trochlear articular surface, with no stepoff and no displacement following compression screw fixation
(a–d) AP and lateral radiograph images from the same patient as in Fig. 12.2 demonstrating screw fixation just distal to physis and proximal to intercondylar notch
Intra-articular Osteochondral Fractures
Large osteochondral fragments of the lateral femoral condyle, 1 cm and above, warrant operative treatment. Generally these contain cartilage that is lateral to the central weight-bearing surface of the lateral femoral condyle, but may also extend to include it. While each fragment is different, with regard to its shape, its condition, and the amount of bone that it may contain, even those fragments with minimal subchondral bone or no bone, which is more common in younger patients, may heal with appropriate fixation, if pursued early enough after injury. The first 2 weeks is the optimal time for fixation, but fragments with substantial portions of bone can be successfully fixated up to 6 weeks or so, provided that there is not excessive cartilage degradation. Synovial fluid intravasation into the chondral tissue can cause swelling of the size of the fragment, so steps may need to be taken to trim down a fragment to fit into the native condylar bed off of which it sheared, with the understanding that future contraction of the fragment back toward its original, native size is likely to occur, and any final implant position should be decided with this possibility in mind.
Fixation can be performed through arthroscopic or open techniques. Implant options include k-wires, cannulated or solid metal screws, variable pitch headless screws, or bioabsorbable pins [27–29], tacks, or screws, which have the advantage of not requiring implant removal but the disadvantage of being radiolucent, which means that MRI may be necessary in certain cases to confirm implant position in the postoperative period [30]. For non-bioabsorbable implants, hardware removal is usually performed at some point after fracture healing, though headless compression screws may be buried beneath the superficial level of the cartilage and may be retained [31]. Whereas fixation of chondral-only fragments was not traditionally pursued due to concerns about getting cartilage to heal to bone, newer evidence supports the notion that chondral-only fragments may be able to heal in children or adolescents if early refixation is pursued [32, 33].
Complications
Complications associated with distal femoral fractures are not uncommon, with those related to premature physeal arrest being the most common. More physeal arrest cases are incomplete, or partial, than complete arrests across the entire physis, so angular deformity is more common than frank leg length discrepancies. A large study of over 550 fractures reported a 52 % chance of growth disturbance [4], with other studies quantifying the rates based on Salter-Harris types I (36 %), II (58 %), III (49 %), and IV (64 %). While non-displaced fractures also have surprisingly high rates of growth disturbance, it is around 1/4th as likely as displaced fractures. While infants under 2 years old are an at-risk group, due to the flat shape of the physis at this age, the highest risk group are preadolescents with more than 2 years of growth remaining, in whom even minor growth disturbances can manifest themselves clinically through the peak period of pubertal growth. Older adolescents may have similar degrees of arrest that do not progress due to the limited continued growth.
Close follow-up through skeletal maturity is the best way to ensure early diagnosis and timely management of physeal disturbances. Hips-to-ankles alignment radiographs or assessments with modern, low-radiation, EOS CT imaging may be helpful to detect abnormalities, sometimes before clinically apparent on physical exam. When physeal bridging or “bony bars” are suspected and confirmed with CT or MRI, management depends on the size and the amount of growth remaining. Those that are less than 50 % of the physeal surface area in a child with more than 2 years of growth remaining should likely undergo excision and fat- or soft-tissue interposition to attempt to restore physeal function on that side of the distal femur. Restoration of growth is achievable, sometimes with spontaneous correction following bar excision to an acceptable degree of improvement of angular deformities and leg length discrepancies. Interestingly, there is a significant range of reported success rates with such techniques, with the literature suggesting that anywhere from 25 to 80 % will regain physeal function following bar excision [34–36]. However, staged or concurrent hemi-epiphysiodesis may need to be performed to optimize angular alignment, as may contralateral epiphysiodesis at a later juncture to restore equal leg lengths. More severe physeal arrests that are more than 50 % of the surface area may require contralateral epiphysiodesis or, in a younger child, consideration of leg-lengthening techniques to address more severe projected discrepancies. Older adolescents who present in delayed fashion with closing or closed growth plates may also require lengthening to address clinically significant leg length discrepancies (usually over 2–3 cm) or distal femoral osteotomies to address clinically significant angular deformity (usually 10–15°). However, the exact amount of angulation and/or discrepancy that may be “clinically significant” may be different for different children, and care should be individualized to the patient and family. The topic of treatment of growth arrests and deformity represents a huge area of study unto itself, and is not done justice with the above oversimplification of some basic principles. Awareness of the high potential for such clinical sequelae is the key takeaway, with a number of treatment options available to optimize long-term lower extremity function in the young patient .
Another common complication of Salter-Harris fractures of the distal femur is knee stiffness, which is best prevented with early range-of-motion exercise, usually best pursued through physical therapy within 4 weeks of the injury or fixation surgery. If detected later as a complication, it can often be overcome with an aggressive therapy regimen and dynamic splinting during the first 3–4 months after injury. Beyond this time frame, consideration should be made toward arthroscopic lysis of adhesions and manipulation under anesthesia, particularly in the older adolescent. Increasing flexion can sometimes be achieved over the course of up to 6 months in younger children, such as those under 12 years old or so. Should arthroscopy, lysis, and manipulation need to be pursued in this age group, care must be taken to avoid distal femoral physeal injury through excessive manipulation in skeletally immature patients [20, 37].
Other, less common complications include infection, which is best avoided by burying k-wires for later removal or removing them within 4 weeks, as well as loss of reduction, which is rare with the use of adequate pin sizes and achieving anatomic reduction. Vascular injuries are uncommon, but can occur in association with severely displaced fractures, particularly in the anterior direction, in which the metaphyseal fragment can kink or tear the popliteal artery which is stretched anteriorly or draped over a bony spike. Early detection, appropriate workup, expeditious involvement of vascular surgery consultation services, and careful monitoring for compartment syndrome of the leg, if not prophylactic fasciotomies (indicated in the setting of more than 4–6 h of ischemia time), are all essential to avoiding catastrophic sequelae. Nerve injuries are also rare, with the peroneal nerve being the most commonly affected, also with anterior epiphyseal displacement, specifically anteromedial. Direct trauma to the peroneal nerve may occur as well, in the typical valgus knee direct blow phenomenon. Either mechanism tends to warrant the use of an ankle foot orthosis and/or multi-podus boot (if the motor branches are affected) and observation, with spontaneous resolution in most cases within 3 months. If no recovery is seen within this time, an electromyogram and potentially further treatment is warranted, depending on the findings .
Complications following osteochondral fracture fixation include stiffness, implant-related complications, such as migration or prominence, and local degenerative joint disease at the site of chondral fissures or on the margin of chondral defects in cases of removed fragments. Of course, if the fracture occurred in association with a dislocation event, recurrent patellar instability may be the most common complication, with the possibility of further osteochondral injury. Some studies have shown that concomitant medial patellofemoral ligament repair decreases the risk of recurrent instability [38, 39]. However, other studies have disputed this notion, which remains controversial [40–44].
References
Kawamoto K, Kim WC, Tsuchida Y, Tsuji Y, Fujioka M, Horii M, et al. Incidence of physeal injuries in Japanese children. J Pediatr Orthop B. 2006;15(2):126–30.
Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Orthop. 1990;10(6):713–6.
Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton III LJ. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423–30.
Basener CJ, Mehlman CT, DiPasquale TG. Growth disturbance after distal femoral growth plate fractures in children: a meta-analysis. J Orthop Trauma. 2009;23(9):663–7.
Riseborough EJ, Barrett IR, Shapiro F. Growth disturbances following distal femoral physeal fracture-separations. J Bone Joint Surg Am. 1983;65(7):885–93.
Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14(4):513–5.
Stanitski CL, Paletta Jr GA. Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med. 1998;26(1):52–5.
Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717–21.
Krosin MT, Lincoln TL. Traumatic distal femoral physeal fracture in a neonate treated with open reduction and pinning. J Pediatr Orthop. 2009;29(5):445–8.
Loder RT, Bookout C. Fracture patterns in battered children. J Orthop Trauma. 1991;5(4):428–33.
Eid AM, Hafez MA. Traumatic injuries of the distal femoral physis. Retrospective study on 151 cases. Injury. 2002;33(3):251–5.
Thomson JD, Stricker SJ, Williams MM. Fractures of the distal femoral epiphyseal plate. J Pediatr Orthop. 1995;15(4):474–8.
Ogden JA. Injury to the growth mechanisms of the immature skeleton. Skeletal Radiol. 1981;6(4):237–53.
Rang M, Wenger D. The physis and skeletal injury. In: Rang’s children’s fracture. Philadephia: Lippincott Williams & Wilkins; 2005. p. 11–25.
Sferopoulos NK. Type v physeal injury. J Trauma. 2007;63(6):E121–3.
Beals RK. Premature closure of the physis following diaphyseal fractures. J Pediatr Orthop. 1990;10(6):717–20.
Hresko MT, Kasser JR. Physeal arrest about the knee associated with non-physeal fractures in the lower extremity. TJ Bone Joint Surg Am. 1989;71(5):698–703.
Navascues JA, González-López JL, López-Valverde S, Soleto J, Rodriguez-Durantez JA, García-Trevijano JL. Premature physeal closure after tibial diaphyseal fractures in adolescents. J Pediatr Orthop. 2000;20(2):193–6.
Matelic TM, Aronsson DD, Boyd Jr DW, LaMont RL. Acute hemarthrosis of the knee in children. Am J Sports Med. 1995;23(6):668–71.
Chung SM, Batterman SC, Brighton CT. Shear strength of the human femoral capital epiphyseal plate. J Bone Joint Surg Am. 1976;58(1):94–103.
Patino M, Fuentes JM, Singh S, Hahn PF, Sahani DV. Iterative reconstruction techniques in abdominopelvic CT: technical concepts and clinical implementation. AJR Am J Roentgenol. 2015;205(1):W19–31.
Seibert JA. Iterative reconstruction: how it works, how to apply it. Pediatr Radiol. 2014;44 Suppl 3:431–9.
Hubner U, Schlicht W, Outzen S, Barthel M, Halsband H. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg Br. 2000;82(8):1170–3.
Herman M, Smith B. Fractures of the distal femoral physis. In: Flynn JM, Skaggs DL, Waters PM, editors. Rockwood and Wilkins’ fractures in children. 8th ed. Philadelphia: Wolters Kluwer; 2014.
Blasier R. Distal femoral physeal fractures. In: Wiesel SW, editor. Operative techniques in orthopaedic surgery. Philadelphia: Lippincott Williams & Wilkins; 2011. p. 1116–21.
Lee YS, Jung YB, Ahn JH, Shim JS, Nam DC. Arthroscopic assisted reduction and internal fixation of lateral femoral epiphyseal injury in adolescent soccer player: a report of one case. Knee Surg Sports Traumatol Arthrosc. 2007;15(6):744–6.
Gkiokas A, Morassi LG, Kohl S, Zampakides C, Megremis P, Evangelopoulos DS. Bioabsorbable pins for treatment of osteochondral fractures of the knee after acute patella dislocation in children and young adolescents. Adv Orthop. 2012;2012:249687.
Chotel F, Knorr G, Simian E, Dubrana F, Versier G, French Arthroscopy Society. Knee osteochondral fractures in skeletally immature patients: French multicenter study. Orthop Traumatol Surg Res. 2011;97(8 Suppl):S154–9.
Walsh SJ, Boyle MJ, Morganti V. Large osteochondral fractures of the lateral femoral condyle in the adolescent: outcome of bioabsorbable pin fixation. J Bone Joint Surg Am. 2008;90(7):1473–8.
Dines JS, Fealy S, Potter HG, Warren RF. Outcomes of osteochondral lesions of the knee repaired with a bioabsorbable device. Arthroscopy. 2008;24(1):62–8.
Lewis PL, Foster BK. Herbert screw fixation of osteochondral fractures about the knee. Aust N Z J Surg. 1990;60(7):511–3.
Uchida R, Toritsuka Y, Yoneda K, Hamada M, Ohzono K, Horibe S. Chondral fragment of the lateral femoral trochlea of the knee in adolescents. Knee. 2012;19(5):719–23.
Nakamura N, Horibe S, Iwahashi T, Kawano K, Shino K, Yoshikawa H. Healing of a chondral fragment of the knee in an adolescent after internal fixation. A case report. J Bone Joint Surg Am. 2004;86-A(12):2741–6.
Broughton NS, Dickens DR, Cole WG, Menelaus MB. Epiphyseolysis for partial growth plate arrest. Results after four years or at maturity. J Bone Joint Surg Br. 1989;71(1):13–6.
Hasler CC, Foster BK. Secondary tethers after physeal bar resection: a common source of failure? Clin Orthop Relat Res. 2002;405:242–9.
Williamson RV, Staheli LT. Partial physeal growth arrest: treatment by bridge resection and fat interposition. J Pediatr Orthop. 1990;10(6):769–76.
Simonian PT, Staheli LT. Periarticular fractures after manipulation for knee contractures in children. J Pediatr Orthop. 1995;15(3):288–91.
Bassett FI. Acute dislocation of the patella, osteochondral fractures, and injuries to the extensor mechanism of the knee. Instr Course Lect. 1976;25:40–9.
Rorabeck CH, Bobechko WP. Acute dislocation of the patella with osteochondral fracture: a review of eighteen cases. J Bone Joint Surg Br. 1976;58(2):237–40.
Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38(11):2248–54.
Christiansen SE, Jakobsen BW, Lund B, Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24(8):881–7.
Nikku R, Nietosvaara Y, Aalto K, Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76(5):699–704.
Nikku R, Nietosvaara Y, Kallio PE, Aalto K, Michelsson JE. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand. 1997;68(5):419–23.
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–70.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Heyworth, B.E., Glotzbecker, M.P., Kramer, D.E. (2016). Physeal, Epiphyseal, and Intra-articular Fractures of the Distal Femur. In: Hedequist, D., Heyworth, B. (eds) Pediatric Femur Fractures. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7986-5_12
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7986-5_12
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7984-1
Online ISBN: 978-1-4899-7986-5
eBook Packages: MedicineMedicine (R0)