Abstract
The global coagulation tests, prothrombin time (PT) and activated partial thromboplastin time (aPTT), are commonly used to screen for coagulation deficiencies and are usually done in preparation for surgery. Simultaneous prolongation of both times can be found in severe hepatic disease, vitamin K deficiency, and disseminated intravascular coagulation. In the absence of these disorders, one must consider inherited deficiencies or acquired inhibitors of those factors in the distal or the common portion of the coagulation pathway. While these constitute a group of rare bleeding disorders, they are important to recognize as they can result in severe bleeding, either spontaneously or with surgical procedures. This chapter reviews the pathobiology of those acquired and inherited conditions that cause concurrent prolongation of the PT and aPTT as well as specific management considerations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
The coagulation cascade is typically assessed by measurement of the prothrombin time (PT) and activated partial thromboplastin time (aPTT). While these are crude screening tests for abnormalities of coagulation, they do provide a rapid way of detecting significant deficiencies in the extrinsic, intrinsic, contact, and common pathways of coagulation which may or may not reflect an increased risk of bleeding. Unlike the already described isolated elevations in either the PT or the aPTT (Chaps. 3 and 4), a finding of prolongation of both clotting times implies a defect in the more distal or common pathway of the coagulation cascade (Fig. 5.1).
Inherited single or combined defects in this group of coagulation reactions are among the rarest coagulation disorders. Both inherited and acquired defects discussed in this chapter are listed in Table 5.1.
Congenital Fibrinogen Disorders
Clinical Vignette 1
A 52-year-old female with a PMH of diabetes, osteoarthritis, and migraine headaches referred for preoperative evaluation of prolonged clotting times. A total knee replacement was scheduled. She had had previous minor procedures (endoscopy, skin biopsy) but no major surgery. She had recurrent epistaxis as a child but no menorrhagia or any other type of excessive bleeding. There was no history of thrombosis or liver disease. Her laboratory testing revealed the following:
PT 16.5 (9–13 s)
1:1 mix with normal plasma 12.0 s
aPTT 33.2 (24.4–31.7 s)
Fibrinogen clot 66 (200–400 mg/dL)
Fibrinogen antigen 352 (149–353 mg/dL)
Thrombin time 36.2 (15.1–18.5 s)
Reptilase time >60 (18–22 s)
Factors II, V, VII, VIII, IX, X, XI, and XII were within normal limits.
She underwent knee surgery and was given cryoprecipitate postoperatively as prophylaxis against bleeding. Her fibrinogen level (activity) went up to 217 mg/dL. She experienced no perioperative bleeding.
Fibrinogen is a large glycoprotein (340 kDa) encoded by three genes located in close proximity to each other on chromosome 4. It is synthesized in the liver, and its normal plasma concentration is approximately 250 mg/dL (Marder et al. 2013). A level of 50–100 mg/dl is considered adequate to support hemostasis. Compared to most coagulation factors, it has a long half-life of 3–5 days, so that replacement with cryoprecipitate in a patient with congenital hypofibrinogenemia can be relatively infrequent. Fibrinogen is a complex molecule, consisting of three different paired polypeptide chains expressed as Aα2, Bβ2, and γ2 that are linked together by disulfide bonds (Mosesson et al. 2001). During the process of fibrin formation and stabilization these fibrinopeptides are cleaved by thrombin, forming fibrin which then polymerizes. The fibrin polymers must be cross-linked through the action of factor XIII (activated by thrombin) resulting in a stable clot at the site of a vascular injury. Remodeling of the clot then occurs through activation of tissue-bound plasminogen by tissue plasminogen activator, generation of plasmin, and cleavage of the stabilized fibrin meshwork within the clot. Besides its function in the coagulation cascade, fibrinogen facilitates platelet aggregation via binding to the platelet glycoprotein IIb/IIIa (αIIbβ3) receptor and von Willebrand factor (Marder et al. 2013).
Conversion of fibrinogen to fibrin by thrombin is the most distal step in the coagulation cascade. In the laboratory this step is measured in isolation by either the thrombin or the reptilase times. The thrombin time is sensitive to the presence of heparin, whereas heparin has no effect on the reptilase time in which the reagent used to initiate the reaction is a snake venom enzyme, reptilase. This allows assessment of fibrinogen function even in the presence of heparin. Both the thrombin time and reptilase times will be elevated in either hypofibrinogenemia or dysfibrinogenemia, but the thrombin time is more sensitive for detecting dysfibrinogenemia (Hayes, 2002). Although an absence of fibrinogen will affect both coagulation times (PT and aPTT), dysfibrinogemia appears to have a preferential effect on the prothrombin time (Hayes 2002).
Two major methods are used to quantify the level of functional fibrinogen, the PT-derived method and the Clauss assay. Both of these are clot-based methods, and the detection limit is variable (20–60 mg/dL). In a comparison study, the PT-derived method correlated with the fibrinogen antigen concentration, whereas the Clauss method correlated best with functional coagulation tests such as the reptilase time, thrombin time, and prothrombin time. It was therefore recommended that the Clauss assay be used in the management of hypofibrinogenemic patients who are bleeding (Miesbach et al. 2010).
While quantitative and qualitative abnormalities of fibrinogen are the most common heritable causes of a combined PT and aPTT elevation, they themselves are rare. Afibrinogenemia occurs with a frequency of 0.0001 % and hypo- and dysfibrinogenemia at a somewhat higher frequency (Acharya et al. 2004). The latter are difficult to quantify because many patients, especially with dysfibrinogenemia, are asymptomatic.
Afibrinogenemia, defined by the complete absence of measurable fibrinogen activity and antigen, is inherited in an autosomal recessive fashion with variable penetrance (Asselta et al. 2006). The majority of the causal mutations have been discovered in the fibrinogen Aα, or FGA gene, but others have been found in the Bβ and -γ chains resulting in either a complete loss of expression or production of abnormal proteins that are retained within the cell. The gene defects include deletions, frameshift, nonsense, or splicing mutations (de Moerloose and Neerman-Arbez 2009). Homozygous mutations usually lead to the most severe hemorrhagic tendency. However, correlations between phenotype and genotype are not always predictable. Hypofibrinogenemic patients (fibrinogen activity levels below 150 mg/dL with a proportionate decrease in fibrinogen antigen) are usually heterozygous for the same mutations found in afibrinogenemia.
Dysfibrinogenemia results from production of a qualitatively dysfunctional fibrinogen molecule. It is transmitted with an autosomal dominant mode of inheritance. Dysfibrinogenemia can also be acquired in patients with liver disease. In the inherited form, causative mutations, mostly in FGA, cause defective cellular release or abnormal fibrin polymerization and cross-linking. In typical cases the fibrinogen functional activity is low, but the immunological measurement reveals a normal amount of fibrinogen antigen, usually twice that of the activity level. Other laboratory findings include correction of the abnormal PT and aPTT in mixing studies, elevations in both the thrombin and reptilase times, and normal levels of coagulation factors in the extrinsic and intrinsic pathway.
Clinical Manifestations
The bleeding symptoms in afibrinogenemia are more severe than in either hypofibrinogenemia or dysfibrinogenemia but generally less severe than in hemophilia. The types of bleeding also differ in that there is a lower incidence of joint and muscle bleeds and a higher incidence of mucosal bleeding than in hemophiliacs. The most common kinds of bleeds in afibrinogenemic patients include umbilical cord bleeding (85 %), muscle hematoma (72 %), mucosal bleeding (including epistaxis, oral cavity, and menorrhagia) in 72 %, hemarthrosis (54 %), and CNS hemorrhage (10 %) (Lak et al. 1999). Posttraumatic hematomas are also common in these patients. This distribution of bleeding sites is similar to that of more recent series of 90 patients in Iran (Lak et al. 2010). Afibrinogenemia is also associated with thrombotic events and an increased incidence of spontaneous abortion, particularly in the first trimester.
Patients with congenital dysfibrinogenemia have a milder disease. Approximately 55 % may be asymptomatic and go undiscovered until screening coagulation testing is done in preparation for surgery. About 25 % have a bleeding tendency, and 20 % have thromboembolic complications (de Moerloose et al. 2010).
Management
Management of the patient with congenital afibrinogenemia consists of prophylactic replacement of fibrinogen. This typically consisted of regularly scheduled infusions of cryoprecipitate for both prophylaxis and at the time of a bleed or a procedure. In Europe and now the USA, a plasma-derived fibrinogen concentrate is approved for use for acute bleeding episodes in afibrinogenemic patients (RiaSTAP®). The fibrinogen concentrates are favored since dosing is more defined, extraneous coagulation proteins (factor VIII, von Willebrand factor, factor XIII) are avoided, and they are virally inactivated. However, thrombosis has been associated with the administration of such concentrates (Bornikova et al. 2011).
In general, there is a good correlation between the functional fibrinogen level and the occurrence of bleeding, with the accepted hemostatic level of 50 % (Castaman 2008). However, the optimal dosage and target level of fibrinogen for prophylaxis are unknown. The severity and frequency of bleeding must be taken into account when deciding on the need for secondary prophylactic replacement therapy. A prior CNS bleed or frequent spontaneous bleeding are the two most common indications for prophylaxis. Fibrinogen concentrate or cryoprecipitate are given with variable frequency, from every week to every 2 weeks to monthly (Peyvandi et al. 2006). In a large review of case reports of treated patients, a fibrinogen level of 50–100 mg/dL was most commonly used as a goal of replacement for nonsurgical patients and 100–200 mg/dL in surgical cases (Bornikova et al. 2011). For epistaxis or dental extractions, antifibrinolytics such as epsilon aminocaproic acid (EACA) or tranexamic acid can be used as adjunctive therapy.
There are several reports of success with fibrinogen replacement to prevent miscarriage in afibrinogenemic women (Frenkel et al. 2004). Again, the schedule and target level of fibrinogen are not well defined, although a target trough level was typically above 60 mg/dL (Bornikova et al. 2011).
Prothrombin, Factor V, and Factor X Deficiencies
Clinical Vignette 2
RT is a 64-year-old female admitted for left lower quadrant pain, nausea, and vomiting. She gave the history of multiple bleeding episodes since she was a child, including umbilical cord hemorrhage and severe bleeding when she was losing her baby teeth. She was hospitalized on several occasions and required transfusion. As an adult, she had severe bleeding after dental extraction treated with EACA and topical thrombin. She has had multiple episodes of hemarthrosis in her knees, wrists, ankles, and elbows. She was managed only with bed rest. She had severe menorrhagia from the time of menarche and had to be transfused with PRBCs and plasma in the past. Depoprovera was given to suppress her periods. Her brother had had multiple episodes of hemarthrosis and also bleeding with the loss of teeth. They were both given vitamin K as children for bleeding episodes. She is one of 12 children, but none of her siblings had a bleeding diathesis.
There was no history of cardiac, pulmonary, renal, hepatic, and thyroid disease; diabetes; or hypertension. She is G0, P0.
Laboratory testing: PT >76.9 (8.4–13 s)
1:1 mix with normal plasma, 11.9 s
aPTT 76.3 (23–32.4 s)
Fibrinogen clot 784 (200–400 mg/dL)
Thrombin time 18.3 (<18.6 s)
Factor X <1 % (73–163 %)
Factor II 70 % (71–138 %)
She received two units of FFP in preparation for colonoscopy. She did not require surgery.
Prothrombin, factor V, and factor X are all positioned in the common distal pathway of coagulation, and their deficiencies lead to combined elevations in both the PT and aPTT (see Fig. 5.1). Because of their rarity these deficiencies have been considered as part of a group of “rare bleeding disorders” (RBD) or “rare inherited coagulation disorders” (RICD). All have an autosomal recessive inheritance pattern and occur with a prevalence of <1:1,000,000 in homozygous forms, which are frequently associated with consanguinity. The gene mutations or deletions that have been identified usually lead to quantitatively defective synthesis of each corresponding factor (i.e., a type 1 deficiency). In combined factor VIII and V deficiency, however, the defect is neither of these gene sequences, but rather in a gene responsible for intracellular transport and secretion of the factors from the cell. These genes are MCFD1 or LMAN1, and the end result of the mutation is a decrease in FV and FVIII activities to approximately 5–30 % accompanied by a moderate bleeding disorder. Inherited combined deficiencies of all vitamin K-dependent (VKD) factors have also been reported. In the few patients that have been described, the molecular defects have been found in the γ-glutamyl carboxylase gene necessary for the carboxylation step in the posttranslational modification of all VKD factors and in the vitamin K epoxide reductase gene, responsible for regeneration of reduced vitamin K (Brenner 2000). Interestingly, in animal models the defect caused by defective carboxylation can be bypassed by supplemental vitamin K.
Prothrombin and factor X are synthesized in the liver and circulate as precursors to a serine protease. Factor V is also thought to be synthesized in the liver, but there is evidence of synthesis in megakaryocytes as well. Approximately 20 % of plasma factor V is stored in platelet α-granules (Tracy et al. 1982). Their activities intersect within the prothrombinase complex where factor Xa cleaves prothrombin to thrombin in the presence of factor Va, calcium, and phospholipid (Fig. 5.2). Factor Va increases the activity of factor Xa by about 5 orders of magnitude (Mann and Kalafatis 2003).
Activation of factor V and formation of the prothrombinase complex. (a) Inactive factor V binds to the phospholipid surface. (b) Factor V is activated to factor Va by thrombin (IIa). (c) Factor Va binds to factor Xa forming the prothrombinase complex which cleaves prothrombin (II) to thrombin (IIa). (d) Activated protein C (APC) cleaves at three sites of the factor Va molecule, rendering it inactive (Vai). The resulting product (factor Vai) is unable to generate thrombin (adapted from Mann and Kalafatis 2003)
Clinical Manifestations
While these factors play essential roles within the coagulation cascade, their deficiency, even when severe, is not always manifested by a bleeding diathesis. The bleeding complications are quite variable. As with afibrinogenemia, the distribution of bleeding sites varies from that of hemophilia with a lower incidence of joint, muscle, and CNS bleeding (Mannucci et al. 2004). Menorrhagia is common in women with these deficiencies as are other types of mucosal bleeding (oral cavity, epistaxis).
Factor V deficiency, initially known as “parahemophilia,” mainly presents with platelet-type bleeding such as ecchymoses, epistaxis, menorrhagia, and bleeding after surgery. This is perhaps due to the involvement of platelets as a source of factor V for the prothrombinase complex. The complete absence of factor V in mice causes severe hemorrhage, but in humans with levels of plasma factor V activity of <2 % there may be no bleeding tendency. In a registry of RBD in North America, a cohort of 18 patients with severe deficiency (median factor V level of <0.01 U/ml) had spontaneous hemorrhage including hemarthrosis and intramuscular and intracranial bleeds. In those who were heterozygous (median factor V level of 0.35 U/ml), there was a lower incidence of spontaneous skin, mucous membrane, musculoskeletal, and genitourinary bleeding (Acharya et al. 2004).
Patients who are homozygous for factor X deficiency have a median factor X level of <0.01 U/ml and have a similar incidence of cutaneous and mucous membrane bleeding (45 %) and musculoskeletal bleeding (27 %) but a slightly higher rate of CNS bleeding (15 %) compared to severely deficient factor V patients (Acharya et al. 2004). Most patients have missense mutations (Mannucci et al. 2004; Herrmann et al. 2006). This distribution of bleeding sites is based on a small number of patients. Herrmann et al. described a larger cohort correlating the clinical and laboratory phenotype with mutational analysis of the factor X gene (Herrmann et al. 2006). Spontaneous bleeding was seen in both homozygous and heterozygous patients, but severe hemorrhage (CNS, GI, hemarthrosis) occurred only in patients with factor X levels of <2 %. For heterozygous patients, factor X coagulation activity in the plasma correlates imperfectly with clinical bleeding. For example, even though the mean factor X level of the heterozygous patients was 50.7 %, 13 % of them were symptomatic with spontaneous epistaxis, menorrhagia, and bruising. However, none had the severe forms of bleeding seen in homozygous patients. This is somewhat higher than the previously reported incidence of bleeding in heterozygous patients (Uprichard and Perry 2002).
Deficiency of prothrombin is the rarest of the congenital bleeding disorders. Severe deficiency (median activity of 0.03 U/ml) resulted in either spontaneous or trauma-induced bleeding with a distribution of sites similar to that of FV deficiency: skin, mucous membrane, musculoskeletal, GI, GU, and CNS. Those with moderate deficiency (less than 0.25 U/ml) had bleeding episodes which were in the skin and mucous membranes (Acharya et al. 2004). The PT and aPTT are sensitive enough to detect factor V, factors V + VIII, and factor X deficiencies but may be normal in prothrombin deficiency.
Management
Specific replacement of the deficient factor in the rare bleeding disorders is the ideal treatment for bleeding episodes as it is in hemophilia A and B. Unfortunately, neither concentrates nor recombinant proteins are available for these rare deficiencies. The most specific replacement at this time for the VKD factors is with prothrombin complex concentrates (PCCs), containing either 3 (II, IX, and X) or 4 (II, VII, IX, and X) coagulation factors. PCCs were originally licensed for treatment of hemophilia B but are now used for warfarin reversal and as bypass agents in the treatment of factor VIII inhibitors, either acquired or in hemophiliacs. The 4-factor PCC available in North America, FEIBA®, is in an activated form, but all PCCs are thrombogenic, especially after high cumulative doses. Monitoring of the nonessential factors is recommended to avoid levels of >150 % (Mannucci et al. 2004). They have the advantage over plasma of delivering a more precise amount of either prothrombin or factor X (although labeled in units of factor IX, amounts of other factors are available from the manufacturer). Another advantage is that less volume is required compared to plasma.
Treatment dosage and schedule depend upon the type of bleeding or surgical procedure as well as the target level and projected half-life of the factor being replaced. Prothrombin and factor X deficiencies can be treated with PCCs or FFP (Mathias et al. 2010). Prothrombin has a long half-life (see Table 5.2), so dosing is less frequent. The recommended dose of PCC for major surgery is 20–30 U/kg and for FFP, 15–20 ml/kg for both prothrombin and factor X deficiencies (Mannucci et al. 2004). Factor V deficiency can only be replaced with FFP since no concentrate is available. The recommended dose is 15–20 ml/kg to raise the factor V level to >20 % (Mannucci et al. 2004). The half-life of factor V, 36 h, allows once-a-day dosing with FFP. Recombinant factor VIIa (rFVIIa) has also been used in factor V-deficient patients.
Acquired Defects Prolonging the PT and APTT
Liver Disease
Since the liver is the sole site of synthesis for all coagulation factors with the exception of factor VIII and VWF, it stands to reason that hepatic dysfunction will lead to reduced factor synthesis and prolongation of the screening coagulation tests. Despite the addition of thrombocytopenia and numerous other hemostatic abnormalities, this does not necessarily imply an increased bleeding risk. Conversely, protection from thrombosis cannot be assured because of the concomitant reductions in protein C, protein S, and antithrombin production as well as other prothrombotic changes that occur in liver failure. Indeed thrombosis is not uncommon in advanced hepatic disease, ranging in incidence from 0.5 to 1.9 % and up to 6.3 % in hospitalized patients (Dabbagh et al. 2010; Rodriguz-Castro et al. 2012).
In liver disease, either acute hepatitis or more chronic conditions, the PT is more sensitive to the effects of the coagulopathy perhaps due to the greater proportionate decrease in factor VII compared to the other VKD factors, II and X, which, in turn, are decreased to a greater degree than factor IX. This is due to alterations in synthesis as well as impaired utilization of vitamin K resulting in decreased carboxylation of factor II (Corrigan et al. 1982; Blanchard et al. 1981). Abnormalities of fibrinogen, either hypofibrinogenemia as a result of impaired synthesis or dysfibrinogenemia, are seen mainly in chronic hepatitis and cirrhosis. This form of acquired dysfibrinogenemia has been related to an abnormal sialic acid content (Marder et al. 2013). The fibrinogen level is less than normal but usually greater than 100 mg/dL. Thrombin and reptilase times will be prolonged.
Vitamin K Deficiency
Vitamin K is a critical cofactor in the synthesis of the phospholipid-dependent coagulation factors II, VII, IX, and X and the endogenous inhibitors, protein Z and protein C and its cofactor protein S. It allows for the posttranslational modification of glutamic acid residues to γ-carboxylated glutamyl or Gla residues at the N-terminal regions of these molecules through the action of γ-glutamyl carboxylase. This enables the VKD factors to bind calcium, a necessary step in their activation. Vitamin K is also important in the modification and activation of other Gla proteins important in bone metabolism (osteocalcin), inhibition of arterial calcification (matrix Gla protein or MGP), and cellular growth regulation (growth-arrest-sequence protein 6 or Gas6). Vitamin K deficiency has been implicated in postmenopausal bone loss and in atherosclerosis (Berkner and Runge 2004). In total 17 Gla proteins have been discovered at this time (Berkner and Runge 2004).
The reduced form of vitamin K (vitamin K hydroquinone or KH2) serves as the cofactor for γ-glutamyl carboxylase and is recycled to vitamin K epoxide. Vitamin K epoxide is then converted back to KH2 by vitamin K oxidoreductase or VKOR (see Fig. 5.3).
Vitamin K acts as a cofactor in the γ-carboxylation of glutamic acid residues within coagulation factors and other Gla-containing proteins. Source: Lichtman MA, Beutler E, Kipps TJ, Seligsohn U, Kaushansky K, Prchal JT: Williams Hematology, seventh Edition: http://www.accessmedicine.com. Copyright © The McGraw-Hill Companies, Inc. All Rights Reserved
Carboxylation of the glutamic acid residues in the VKD coagulation factors is necessary for binding to anionic phospholipids on whose surface the central reactions of the coagulation cascade take place, i.e., formation of the tenase and prothrombinase complexes. Without vitamin K, those factors are still present but nonfunctional and known as Proteins Induced by Vitamin K Absence, or PIVKA.
Rare combined deficiencies of the VKD factors occur with hereditary deficiency of either γ-glutamyl carboxylase or VKOR. These patients have very low levels of factors II, VII, IX, and X. Severely affected individuals have life-threatening intracranial or umbilical cord bleeding in infancy or spontaneous joint and soft tissue bleeding in childhood if factor levels are below 5 U/dL (Brenner et al. 2009). Skeletal changes and mental retardation can occur. Both the PT and PTT are prolonged without evidence of liver disease or nutritional insufficiency.
Acquired coagulopathy due to vitamin K deficiency occurs in various settings, most commonly in the hospitalized, severely ill patient who has poor nutritional intake, malabsorption, inflammatory bowel disease after extensive intestinal resection, biliary obstruction or undergoing broad-spectrum antibiotic therapy. Infants are most susceptible due to poor placental transport of vitamin K and the low concentration of the vitamin in breast milk (Lippi and Franchini 2011). However, production of vitamin K by intestinal bacteria, once thought to be an important source of the vitamin, is now felt to be insufficient for the normal requirement and possibly not available for use in hemostatic and other reactions. Moreover the normal intestinal flora does not produce enough vitamin K to replace that lost when there is a decrease in delivery of bile salts into the intestinal tract (Berkner and Runge 2004; Lippi and Franchini 2011).
Compared to the non-hemostatic functions supported by vitamin K, the amount necessary for adequate hemostasis is relatively small, and some would argue that the minimum daily requirement (100 μg per day) should be increased (Berkner and Runge 2004). This is especially true in hemodialysis patients who have high levels of non-carboxylated MGP on 140 μg vitamin K, a situation which may put them at risk of increased arterial calcification and vascular disease (Cranenburg et al. 2012).
Assessment of vitamin K status in hospitalized patients is usually by means of global coagulation tests, the PT and aPTT. However, these are very insensitive to vitamin K deficiency since the prothrombin level needs to be only 40–50 % of normal to result in a normal PT. Both increased levels of the non-carboxylated, nonfunctional form of prothrombin (PIVKA-II) and phylloquinone can be measured and used as indicators of vitamin K deficiency (Shearer 2009). In liver disease this becomes more complex since it is not possible to separate, by measurement of the PT and aPTT, defective synthesis of coagulation factors due to hepatic failure from the reduced VKD factor activity due to vitamin K deficiency. Phylloquinone levels may be useful in this circumstance but are not readily available. An easier approach is to first do mixing studies on the PT and aPTT to rule out inhibitory activity. Once an inhibitor is ruled out, measurements of representative VKD factors can be compared to factor V, a non-VKD factor synthesized in the liver. If the level of a VKD factor (II, VII, or X) is low but factor V is normal, the diagnosis is vitamin K deficiency. If both are low, deficient factor synthesis from liver failure is more likely.
Replacement of vitamin K can be done in various ways. Oral replacement is adequate provided the patient has a functional GI (and biliary) tract. In hepatic parenchymal disease, oral vitamin K was less effective than IV when assessed by phylloquinone and PIVKA-II levels (Pereira et al. 2005). Similarly, postoperative or severely ill patients in the ICU have GI absorptive defects, so vitamin K must be given parentally. Subcutaneous or intravenous dosing, 1–10 mg, is sufficient. While anaphylactic reactions have been reported after parenteral administration, these are related to the stabilizer or the emulsifier in the vitamin K preparation rather than vitamin K itself (Shearer 2009).
Lupus Anticoagulants
Although the aPTT is a relatively insensitive test for the lupus anticoagulant (LA), it is the typical laboratory presentation of this phenomenon. Unless the patient is on warfarin, the PT is usually normal. However, there are two circumstances when both the PT and aPTT will be elevated, although not necessarily proportional to each other in the presence of a lupus anticoagulant. This results from a deficiency in prothrombin, either through antibody-mediated increased prothrombin clearance or specific neutralizing antiprothrombin antibodies (Bajaj et al. 1983). This is known as lupus anticoagulant-hypoprothrombinemia syndrome (LAHS) and is a rare variant of the LA which presents with bleeding instead of clotting manifestations due to low prothrombin levels. According to a recent review, 74 cases of LAHS have been reported, with 89 % presenting with bleeding manifestations, including severe hemorrhage in the brain, GI tract, and soft tissue (Mazodier et al. 2012). Most cases are associated with autoimmune disease, particularly SLE. In children, infection is the most common cause with usual resolution of LAHS after the infection clears.
In the laboratory, the aPTT is variably elevated; the PT is increased but proportionately less. The prothrombin activity and antigen levels are severely decreased, consistent with increased clearance of antibody–antigen complexes (Mazodier et al. 2012). Antiprothrombin antibodies are common in LA-positive patients and may prolong the PT while not causing either a decrease in plasma prothrombin activity or bleeding symptoms. These antibodies were found to react in a polyspecific fashion with both negatively charged phospholipids and prothrombin (Fleck et al. 1988). It is still controversial whether these antiphospholipid/prothrombin antibodies play a significant role in the clinical manifestations of antiphospholipid syndrome (Hoxha et al. 2012; Nojima et al. 2001; Marozio et al. 2011; Pengo et al. 2010).
Unlike most cases of a typical lupus anticoagulant, significant steroid responsiveness has been reported in LAHS, with normalization of the PT and prothrombin level occurring in approximately 60 %. Other immunosuppressive therapy with azathioprine and cyclophosphamide is used in patients who have LAHS in association with SLE. There are too few cases reported to assess response to other immune-modulating treatment such as IVIG and rituximab (Mazodier et al. 2012).
Acquired Factor V Inhibitor
Acquired inhibitors to coagulation factors in the common distal pathway that lead to both PT and PTT prolongation are rare events, occurring in even lower frequency than factor VIII autoantibodies. Perhaps the best known is the inhibitor to factor V that can develop after exposure to bovine thrombin. Topical thrombins have been in use for decades, particularly in vascular, cardiac, and neurosurgical procedures. Cross-reactivity of anti-bovine thrombin antibodies with human thrombin is known to occur, causing a prolonged thrombin time, PT, and PTT but usually no significant bleeding. Serum IgG bound to thrombin and prothrombin has been demonstrated in these cases (Stricker et al. 1988). In early reports of acquired factor V inhibitors, most patients had had a major surgical procedure just prior to detection of the inhibitor, and transfusion or antibiotics were implicated. It is unknown how many of them were exposed intraoperatively to topical bovine thrombin (Feinstein 1978). A bovine thrombin-induced factor V inhibitor was first described in 1990 in a cardiac surgery patient who had severe bleeding 12 days after his surgery. The factor V activity was 1 % of normal, and mixing studies of his elevated PT, PTT, and thrombin time showed no correction with normal plasma. While his serum IgG reacted with bovine and not human thrombin, there was reactivity with both bovine and human factor V, indicating that the anti-bovine factor V antibody cross-reacts with human factor V (Zehnder and Leung 1990).
Multiple additional cases of thrombin-induced factor V inhibitors have since been reported with variable bleeding manifestations from severe fatal hemorrhage to no excessive bleeding (Rapaport et al. 1992; Spero 1993; Streiff and Ness 2002). Anti-factor V antibodies resolve over time, but if severe bleeding occurs aggressive management is necessary. Treatment with steroid, IVIG, cyclosporine, cyclophosphamide, EACA, and plasmapheresis has been attempted with variable degrees of success (Zehnder and Leung 1990; Streiff and Ness 2002). The development and FDA approval of recombinant human topical thrombin should obviate this problem. It appears to be equivalent in efficacy to bovine thrombin and is less immunogenic (Chapman et al. 2007; Singla et al. 2009).
In addition to inhibitors seen after the use of bovine thrombin, acquired factor V inhibitors have been observed after other drug exposures such as amiodarone (Shreenivas et al. 2012), in patients with malignancy (Nesheim et al. 1986), after liver transplantation (Guglielmone et al. 2011), and as spontaneous or postoperative events (Bobba et al. 2011). However, it is difficult to assign a cause of the inhibitor formation as infection, antibiotic exposure, and other autoimmune conditions are often found in the background of reported cases of factor V and other acquired inhibitors (Franchini and Lippi 2011).
These inhibitors can result in serious bleeding from the GI and GU tracts and other mucosal surfaces (Lipshitz et al. 2012), but in recent reviews, 20–30 % are discovered incidentally in the absence of hemorrhage (Franchini and Lippi 2011; Ang et al. 2009). The frequency of bleeding in spontaneous factor V inhibitor patients, however, appears to be about twice that seen in bovine thrombin-induced inhibitors (Streiff and Ness 2002).
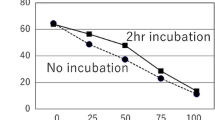
The diagnosis of a spontaneous factor V inhibitor in the laboratory is similar to bovine thrombin-induced ones—the PT and PTT will be prolonged without correction in mixing studies, and factor V levels will be low. A Bethesda assay on factor V will quantify the inhibitor and will inactivate factor V in minutes, although some inhibitors are time dependent. Two hours of incubation are recommended (Ang et al. 2009). In two reviews of acquired factor V inhibitors, the level of inhibitor titer was not predictive of bleeding. Patients with bleeding manifestations, however, had lower factor V levels—a median of 1 % in bleeding patients and 3 % in non-bleeders—and higher PT and aPTTs (Franchini and Lippi 2011; Ang et al. 2009).
As with other acquired factor inhibitors, treatment is designed in two phases—control of the bleeding and eradication of the inhibitor. Fresh frozen plasma, PCCs, rFVIIa, and platelet transfusions have been used with variable degrees of success. Plasma is not expected to be effective due to rapid factor V inactivation by the patient’s antibody. This may not be the case with platelet transfusion in which the factor V contained within platelets may be protected from the inhibitor. In some series, a fairly high rate of response to platelet concentrates is reported (Ang et al. 2009; Chediak et al. 1980), but this has not been a uniform experience (Bobba et al. 2011).
Suppression of the inhibitor can usually be accomplished by various immune-modulating agents. Corticosteroids are the most common initial therapy and result in a high response rate. As with acquired factor VIII inhibitors, rituximab has also been used successfully (Ang et al. 2009; Lebrun et al. 2008; Lian et al. 2004). Other immunosuppressant drugs such as azathioprine, cyclophosphamide, and vincristine should be used only if less toxic agents are ineffective. Factor V inhibitors have been observed to resolve spontaneously in 20–56 % of patients, particularly in those in whom an identifiable cause (e.g., antibiotic therapy) can be removed. The median time to resolution is 6–8 weeks. Although a mortality rate from bleeding complications of 12 % has been reported, the overall prognosis of a factor V inhibitor is largely dependent on that of the underlying disease (Franchini and Lippi 2011).
Acquired Factor X Deficiency and Inhibitors
Clinical Vignette 3
DH is a 37-year male who was well except for a history of hypertension. He sustained abdominal trauma playing with his daughter and developed intraperitoneal hemorrhage requiring exploratory laparotomy, splenectomy, and segmental liver resection. Subconjunctival hemorrhage was noted. Three months later he presented with spontaneous flank pain and hematemesis and had a large perinephric hematoma associated with acute renal failure. Biopsies of both the duodenum and stomach contained deposits of acellular amorphous eosinophilic material, congophilic on Congo red stain with an apple-green birefringence under polarized light. An immunohistochemical stain for P-component was reactive within the deposits confirming that the material was amyloid.
Further pathological review of the spleen also revealed Congo red-positive material confirmed to be amyloid. Immunohistochemical stains for kappa and lambda light chains showed preferential staining of the amyloid material for lambda. A bone marrow biopsy showed plasmacytosis with lambda light chain excess and aberrant cyclin D1 expression, consistent with involvement by a plasma cell neoplasm.
Laboratory testing:
PT 15.7 (8.4–13 s)
1:1 mix with normal plasma, 11.5 s
aPTT 32.7 (23–32.4 s)
Fibrinogen clot 475 (200–400 mg/dL)
Factor X 28 % (73–163 %)
Factor II 98 % (71–138 %)
Factor V 89 % (50–150 %)
Factor VII 72 % (50–150 %)
Treatment was initiated with bortezomib, dexamethasone, and EACA. His prothrombin time corrected to normal. Ultimately the kappa-lambda serum levels and ratio normalized, and a repeat bone marrow biopsy showed no evidence of myeloma. However an echocardiogram demonstrated severe LVH, stage 2 diastolic dysfunction, increased RV wall thickness, and an estimated RVSP of 43 mmHg, consistent with mild pulmonary hypertension; the overall appearance was consistent with cardiac amyloidosis. He underwent high-dose melphalan therapy followed by autologous peripheral stem cell transplantation. He has been in hematologic remission over the subsequent 2 years without further episodes of bleeding. His PT and aPTT are normal, and the factor X level has improved to 62 %.
Aside from liver disease and vitamin K deficiency, acquired factor X deficiency is usually due to systemic AL amyloidosis. In two large series, low factor X levels occurred in 8.7–14 % of amyloidosis patients (Choufani et al. 2001; Mumford et al. 2000). A significant reduction in factor X activity but not necessarily factor X antigen is found, without detectable inhibitory activity. The half-life of factor X after infusion of plasma is extremely low due to increased clearance of factor X from the circulation via binding to amyloid fibrils (Furie et al. 1977). The amount of exposed amyloid in the circulation and the particular binding characteristics of an individual patient’s type of amyloid determine how much factor X is removed and whether factor X deficiency and bleeding occur (Furie et al. 1981). Other data, showing discordance between low factor X coagulant activity and normal factor X antigen levels, suggest some other mechanism resulting in defective factor X function (Mumford et al. 2000).
Approximately a third of all patients with AL amyloidosis and 56 % of those with factor X deficiency will have bleeding symptoms. Subcutaneous and gastrointestinal bleeding are the most common sites, and splenic hemorrhage has been described. The severity of bleeding (other than in the skin) appears to parallel the level of factor X activity (Choufani et al. 2001; Mumford et al. 2000). Of the global coagulation screening tests, a prolonged thrombin time (32 %) and PT (24 %) were most commonly found, with a prolonged PTT seen in 14 % of amyloid patients; the thrombin time does not correlate with bleeding but is associated with proteinuria and hypoalbuminemia (Mumford et al. 2000).
Besides factor X deficiency, other coagulation defects have been described in amyloidosis. Included is factor V deficiency, probably due to increased factor V clearance through binding to amyloid as described with factor X. The deficiency in factor V can cause significant bleeding (Emori et al. 2002). Amyloid binds to factor IX and prothrombin (to a lesser extent than factor X), causing subnormal plasma levels (Furie et al. 1981). Increased vascular fragility, abnormal fibrin polymerization, and dysfibrinogenemia have been described (Mumford et al. 2000).
Treatment of amyloid-associated bleeding which is due to factor X deficiency is difficult. Plasma has little, if any, effect due to factor X’s rapid binding to the blood vessel-contained amyloid. Activated PCCs, rFVIIa, and plasma exchange have been used to treat bleeding and in preoperative management of amyloidosis patients (Thompson et al. 2010; Boggio and Green 2001; Ma et al. 2006). In a retrospective review of surgical outcomes in patients with amyloidosis, there was a 10 % incidence of bleeding complications, more commonly with placement of a central venous catheter. Surprisingly, the incidence of bleeding did not correlate with factor X levels, implying the presence of other hemostatic defects which modify bleeding risk. In nine patients in whom rFVIIa was used, four (44.4 %) had either bleeding or thrombotic complications, raising caution about the use of rFVIIa in this patient population (Thompson et al. 2010). Splenectomy has resulted in improved factor X levels and resolution of bleeding, perhaps due to removal of the large splenic reservoir of amyloid protein resulting in a decrease in factor X clearance (Ma et al. 2006; Rosenstein et al. 1983). However, this is a high-risk procedure in amyloidosis and should only be considered in a patient with life-threatening bleeding. Primary treatment of AL amyloidosis with chemotherapy and autologous transplantation can lead to correction of factor X deficiency if hematologic remission is achieved (Choufani et al. 2001).
References
Acharya SS, Coughlin A, Dimichele D. North American rare bleeding disorder study group. Rare bleeding disorder registry: deficiencies of factors II, V, VII, X, XIII, fibrinogen and dysfibrinogenemia. J Thromb Haemost. 2004;2:248–56.
Ang AL, Kuperan P, Ng CH. Acquired factor V inhibitor—a problem-based systematic review. Thromb Haemost. 2009;101:852–9.
Asselta R, Duga S, Tenchini ML. The molecular basis of quantitative fibrinogen disorders. J Thromb Haemost. 2006;4:2115–29.
Bajaj SP, Rapaport SI, Fierer DS, Herbst KD, Schwartz DB. A mechanism for the hypoprothrombinemia of the acquired hypoprothrombinemia-lupus anticoagulant syndrome. Blood. 1983;61:684–92.
Berkner KL, Runge KW. The physiology of vitamin K nutriture and vitamin K-dependent protein function in atherosclerosis. J Thromb Haemost. 2004;2:2118–32.
Blanchard RA, Furie BC, Jorgensen M, Kruger SF, Furie B. Acquired vitamin K-dependent carboxylation deficiency in liver disease. N Engl J Med. 1981;305:242–8.
Bobba RK, Garg P, Arya M, Freter CE. Postoperative bleeding in an elderly patient from acquired factor V inhibitor: rapid response to immunosuppressive therapy. Am J Med Sci. 2011;341:253–6.
Boggio L, Green D. Recombinant human factor VIIa in the management of amyloid-associated factor X deficiency. Br J Haematol. 2001;112:1074–5.
Bornikova L, Peyvandi F, Allen G, Bernstein J, Manco-Johnson MJ. Fibrinogen replacement therapy for congenital fibrinogen deficiency. J Thromb Haemost. 2011;9:1687–704.
Brenner B. Hereditary deficiency of vitamin K-dependent coagulation factors. Thromb Haemost. 2000;84:935–6.
Brenner B, Kuperman AA, Watzka M, Oldenburg J. Vitamin K-dependent coagulation factors deficiency. Semin Thromb Haemost. 2009;35:439–46.
Castaman G. Prophylaxis of bleeding episodes and surgical interventions in patients with rare inherited coagulation disorders. Blood Transfus. 2008;6 Suppl 2:39–44.
Chapman WC, Singla N, Genyk Y, McNeil JW, Renkens Jr KL, Reynolds TC, et al. A phase 3, randomized, double-blind comparative study of the efficacy and safety of topical recombinant human thrombin and bovine thrombin in surgical hemostasis. J Am Coll Surg. 2007;205:256–65.
Chediak J, Ashenhurst JB, Garlick I, Desser RK. Successful management of bleeding in a patient with factor V inhibitor by platelet transfusion. Blood. 1980;56:835–41.
Choufani EB, Sanchorawala V, Ernst T, Quillen K, Skinner M, Wright DG, et al. Acquired factor X deficiency in patients with amyloid light-chain amyloidosis: incidence, bleeding manifestations, and response to high-dose chemotherapy. Blood. 2001;97:1885–7.
Corrigan JJ, Jeter M, Earnest DL. Prothrombin antigen and coagulant activity in patients with liver disease. JAMA. 1982;248:1736–9.
Cranenburg EC, Schurgers LJ, Uiterwijk HH, Beulens JW, Dalmeijer GW, Westerhuis R, Magdeleyns EJ, Herfs M, Vermeer C, Laverman GD. Vitamin K intake and status are low in hemodialysis patients. Kidney Int. 2012;82:605–10.
Dabbagh O, Oza A, Prakash S, Sunna R, Saettele TM. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest. 2010;137:1145–9.
de Moerloose P, Neerman-Arbez M. Congenital fibrinogen disorders. Semin Thromb Hemost. 2009;35:356–66.
de Moerloose P, Boehlen F, Neerman-Arbez M. Fibrinogen and the risk of thrombosis. Semin Thromb Hemost. 2010;36:7–17.
Emori Y, Sakugawa M, Niiya K, Kiguchi T, Kojima K, Takenaka K, et al. Life-threatening bleeding and acquired factor V deficiency associated with primary systemic amyloidosis. Blood Coag Fibrinol. 2002;13:555–9.
Feinstein DI. Acquired inhibitors of factor V. Thrombos Haemost. 1978;39:663–73.
Fleck RA, Rapaport SI, Rao VM. Anti-prothrombin antibodies and the lupus anticoagulant. Blood. 1988;72:512–9.
Franchini M, Lippi G. Acquired factor V inhibitors: a systematic review. J Thromb Thrombolysis. 2011;31:449–57.
Frenkel E, Duksin C, Herman A, Sherman DJ. Congenital hypofibrinogenemia in pregnancy: report of two cases and review of the literature. Obstet Gynecol Surv. 2004;59:775–9.
Furie B, Greene E, Furie BC. Syndrome of acquired factor X deficiency and systemic amyloidosis: in vivo studies of the metabolic fate of factor X. N Engl J Med. 1977;297:81–5.
Furie B, Voo L, McAdam KP, et al. Mechanism of factor X deficiency in systemic amyloidosis. N Engl J Med. 1981;304:827–30.
Guglielmone H, Jarchem G, Minoldo S. Successful treatment with intravenous immunoglobulin (IVIg) in a patient with an acquired factor V inhibitor after liver transplantation. Thromb Haemost. 2011;106:985–6.
Hayes T. Dysfibrinogenemia and thrombosis. Arch Pathol Lab Med. 2002;126:1387–90.
Herrmann FH, Auerswald G, Ruiz-Saez A, Navarrete M, Pollmann H, Lopaciuk S, Batorova A, Wulff K, for the Greifswald factor X deficiency study group. Factor X deficiency: clinical manifestation of 102 subjects from Europe and Latin America with mutations in the factor 10 gene. Haemophilia. 2006;12:479–89.
Hoxha A, Ruffatti A, Pittoni M, Bontadi A, Tonello M, Salvan E, et al. The clinical significance of autoantibodies directed against prothrombin in primary antiphospholipid syndrome. Clin Chim Acta. 2012;413:911–3.
Lak M, Heihani M, Elahi F, Peyvandi F, Mannucci PM. Bleeding and thrombosis in 55 patients with inherited afibrinogenemia. Br J Haematol. 1999;107:204–6.
Lak M, Toogheh G, Keyhani M. Bleeding and thrombosis in 90 Iranian patients with inherited afibrinogenemia. Blood 2010;116: Abstract 3667.
Lebrun A, Leroy-Matheron C, Arlet JB, Bartolucci P, Michel M. Successful treatment with rituximab in a patient with an acquired factor V inhibitor. Am J Hematol. 2008;83:163–4.
Lian EC, Tzakis AG, Andrews D. Response of factor V inhibitor to rituximab in a patient who received liver transplantation for primary biliary cirrhosis. Am J Hematol. 2004;77:363–5.
Lippi G, Franchini M. Vitamin K in neonates: facts and myths. Blood Transfus. 2011;9:4–9.
Lipshitz J, Chelliah T, Aledort L. A case of factor V inhibitor with complete correction of the PT and aPTT upon mixing. Am J Hematol. 2012;87:313–5.
Ma JF, Coutre SE, Curet MJ. Refractory hematuria from amyloidosis successfully treated by splenectomy. Urology. 2006;67:1085.e13–5.
Mann KG, Kalafatis M. Factor V: a combination of Dr Jekyll and Mr Hyde. Blood. 2003;101:20–30.
Mannucci PM, Duga S, Peyvandi F. Recessively inherited coagulation disorders. Blood. 2004;104:1243–52.
Marder VJ, Aird VC, Bennett JS, Schulman S, White GC, editors. Hemostasis and thrombosis: basic principles and clinical practice. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
Marozio L, Curti A, Botta G, Canuto EM, Salton L, Tavella AM, et al. Anti-prothrombin antibodies are associated with adverse pregnancy outcome. Am J Repro Immunol. 2011;66:404–9.
Mathias M, Pollard D, Riddell A. Prophylaxis in severe prothrombin deficiency. Br J Haemotol. 2010;152:243–4.
Mazodier K, Arnarud L, Mathian A, Costedoat-Chalumeau N, Haroche J, Frances C, et al. Lupus anticoagulant-hypoprothrombinemia syndrome—report of 8 cases and review of the literature. Medicine. 2012;91:251–60.
Miesbach W, Schenk J, Alesci S, Lindhoff-Last E. Comparison of the fibrinogen Clauss assay and the fibrinogen PT derived method in patients with dysfibrinogenemia. Thromb Res. 2010;126:e428–33.
Mosesson MW, Siebenlist KR, Meh DA. The structure and biological features of fibrinogen and fibrin. Ann NY Acad Sci. 2001;936:11–30.
Mumford AD, O’Donnell J, Gillmore JD, Mannin RA, Hawkins PN, Laffan M. Bleeding symptoms and coagulation abnormalities in 337 patients with AL-amyloidosis. Br J Haematol. 2000;110:454–60.
Nesheim ME, Nichols WL, Cole TL, Houston JG, Schenk RB, Mann KG, et al. Isolation of an acquired inhibitor of human coagulation factor V. J Clin Invest. 1986;77:405–15.
Nojima J, Kuratsune H, Suehisa E. Association between the prevalence of antibodies to b2-glycoprotein I, prothrombin, protein C, protein S, and annexin V in patients with systemic lupus erythematosus and thrombotic and thrombocytopenic complications. Clin Chem. 2001;47:1008–15.
Pengo V, Denas G, Bison E, Banzato A, Padayattil Jose S, Gresele P, et al. Prevalence and significance of anti-prothrombin (aPT) antibodies in patients with lupus anticoagulant (LA). Thromb Res. 2010;126:150–3.
Pereira SP, Rowbotham D, Fitt S, Shearer MJ, Wendon J, Williams R. Pharmacokinetics and efficacy of oral versus intravenous mixed-micellar phylloquinone (vitamin K1) in severe acute liver disease. J Hepatol. 2005;42:365–70.
Peyvandi F, Haertel S, Knaub S, Mannucci PM. Incidence of bleeding symptoms in 100 patients with inherited afibrinogenemia or hypofibrinogenemia. J Thromb Haemost. 2006;4:1634–7.
Rapaport SI, Zivelin A, Minow RA, Hunter CS, Donnelly K. Clinical significance of antibodies to bovine and human thrombin and factor V after surgical use of bovine thrombin. Am J Clin Pathol. 1992;97:84–91.
Rodriguz-Castro KI, Simioni P, Burra P, Senzolo M. Anticoagulation for the treatment of thrombotic complications in patients with cirrhosis. Liver Int. 2012;32:1465–76.
Rosenstein ED, Itzkowitz SH, Penziner AS, Cohen JI, Mornaghi RA. Resolution of factor X deficiency in primary amyloidosis following splenectomy. Arch Intern Med. 1983;143:597–9.
Shearer MJ. Vitamin K in parenteral nutrition. Gastroenterology. 2009;137:S105–18.
Shreenivas AV, Lipshitz J, Patel D. A rare case of factor V inhibitor in a patient on amiodarone therapy. Blood Coag Fibrinol. 2012;23:342–4.
Singla NK, Ballard JL, Moneta G, Duane Randleman C, Renkens KL, Allan AW. A phase 3b, open-label, single-group immunogenicity and safety study of topical recombinant thrombin in surgical hemostasis. J Am Coll Surg. 2009;209:68–74.
Spero JA. Bovine thrombin-induced inhibitor of factor V and bleeding risk in postoperative neurosurgical patients-report of three cases. J Neurosurg. 1993;78:817–20.
Streiff MB, Ness PM. Acquired FV inhibitors: a needless iatrogenic complication of bovine thrombin exposure. Transfusion. 2002;42:18–26.
Stricker RB, Lane PK, Leffert JD, Rodgers GM, Shuman MA, Corash L. Development of antithrombin antibodies following surgery in patients with prosthetic cardiac valves. Blood. 1988;72:1375–80.
Thompson CA, Kyle R, Gertz M, Heit J, Pruthi R, Pardanani A. Systemic AL amyloidosis with acquired factor X deficiency: a study of perioperative bleeding risk and treatment outcomes in 60 patients. Am J Hematol. 2010;85:171–3.
Tracy PB, Eide LL, Bowie EJW, Mann KG. Radioimmunoassay of factor V in human plasma and platelets. Blood. 1982;60:59–63.
Uprichard J, Perry DJ. Factor X deficiency. Blood Rev. 2002;16:97–110.
Zehnder JL, Leung LK. Development of antibodies to thrombin and factor V with recurrent bleeding in a patient exposed to topical bovine thrombin. Blood. 1990;76:2011–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Silver, B.J. (2014). Prolongation of Both PT and aPTT. In: Lichtin, A., Bartholomew, J. (eds) The Coagulation Consult. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9560-4_5
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9560-4_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9559-8
Online ISBN: 978-1-4614-9560-4
eBook Packages: MedicineMedicine (R0)