Abstract
The liver is the major organ responsible for the elimination of endogenous and exogenous compounds via metabolism and/or excretion. Hepatocytes, the predominant cell type in the liver, are polarized cells with discrete basolateral and apical membranes. In this chapter, localization and function of hepatic transport proteins responsible for hepatobiliary drug disposition in humans are introduced. Hepatic transport proteins on the basolateral membrane mediate influx of compounds from sinusoidal blood into hepatocytes (i.e., NTCP, OATPs, OATs, OCTs) or efflux from hepatocytes back to sinusoidal blood (i.e., MRP3-6, OSTα/β). Canalicular transport proteins such as BSEP, MDR3, P-gp, BCRP, MRP2, and MATE1 are responsible for biliary excretion of compounds. Furthermore, in vitro (i.e., membrane vesicles, transfected cell systems, hepatocytes, isolated perfused liver) and in vivo (i.e., biliary excretion studies, hepatobiliary imaging techniques) model systems and methods that are used to investigate hepatic transport proteins are discussed, and their applications, advantages, and disadvantages are considered.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
9.1 Introduction
The liver is one of the major organs responsible for the metabolism and excretion of endogenous and exogenous compounds. Hepatocytes contain transport proteins that facilitate the influx of many compounds from sinusoidal blood. Once inside the hepatocyte, compounds may be biotransformed by metabolizing enzymes and/or excreted. Hepatocytes are polarized cells with distinct apical and basolateral domains (Fig. 9.1); transport proteins on the apical membrane are responsible for excretion of compounds into the bile canaliculus, whereas basolateral transport proteins mediate influx into hepatocytes and efflux back to sinusoidal blood. Biliary excretion of drugs and metabolites is an active process that requires energy, usually in the form of adenosine triphosphate (ATP); the multidrug and toxin extrusion (MATE) transporter is one exception that does not require ATP for drug transport into the bile canaliculus. ATP-dependent transport proteins also are located on the basolateral membrane and are able to efflux drugs and metabolites from hepatocytes into sinusoidal blood.
In vivo architecture of polarized hepatocytes with distinct apical and basolateral domains facing respectively the bile canaliculus and bloodstream (Köck and Brouwer 2012)
In this chapter, the hepatic transport proteins important for drug disposition in humans are introduced based on their localization and function. The nomenclature and substrate specificity of hepatic transport proteins are summarized in Tables 9.1 and 9.2. In vitro and in vivo model systems and tools used to answer questions related to hepatic transport proteins are discussed, and more sophisticated approaches under development are introduced as future directions.
9.2 Hepatic Transport Proteins
9.2.1 Hepatic Influx Transport Proteins
The solute carrier (SLC) and solute carrier organic anion (SLCO) gene families are two representative families of transport proteins that mediate the hepatic influx of xenobiotics across the basolateral hepatocyte membrane (Fig. 9.1). The list of hepatic influx transporters and example substrates is included in Table 9.1.
NTCP ( SLC10A1 ). The sodium taurocholate cotransporting polypeptide (NTCP) is expressed exclusively in hepatocytes and plays a major role in the Na+-dependent hepatic influx of conjugated bile acids such as glycocholate and taurocholate (Stieger 2011). NTCP also is capable of transporting bromosulfophthalein (BSP), estrone 3-sulfate (E1S), and drugs such as pitavastatin and rosuvastatin, although the contribution of NTCP to the uptake of drug substrates into hepatocytes in vivo remains to be determined (Table 9.1). In rats, Ntcp also may be capable of transporting the thyroid hormones and the mushroom toxin α-amanitin (Gundala et al. 2004).
OATPs ( SLCO , previously SLC21A ). The family of organic anion transporting polypeptides (OATPs) plays an essential role in sodium-independent influx of endogenous and exogenous compounds into hepatocytes and may be the rate-limiting step in the hepatobiliary clearance of some drugs, such as statins. OATPs exhibit broad and overlapping substrate specificity; the spectrum of OATP substrates includes organic anions, bulky organic cations (previously referred to as type II cations), and neutral steroids. Some OATP isoforms have been hypothesized to function as glutathione or bicarbonate antiporters (Briz et al. 2006; Li et al. 2000; Satlin et al. 1997), employing the high intracellular glutathione or bicarbonate concentrations as a driving force for hepatic influx of substrates with high efficiency.
Eleven human OATP isoforms have been identified so far; OATP1B1, OATP1B3, and OATP2B1 are the major human OATPs that play an important role in the hepatic influx of drugs across the basolateral membrane domain. OATP1B1 and 1B3 are liver-specific, whereas OATP2B1 is widely expressed (e.g., in intestine, brain, and kidney). OATP1B1 exhibits the largest diversity of substrates including bilirubin, BSP, bile salts, many antibiotics, angiotensin receptor antagonists, 3-hydroxy-3-methyl-glutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins), and anticancer drugs (Table 9.1). OATP1B1 is the major human liver transport protein that is involved in sodium-independent bile salt and bilirubin influx. Inhibition of OATP1B1-mediated influx by drugs has been correlated with the incidence of hyperbilirubinemia (Campbell et al. 2004). OATP1B1 is important in the hepatic influx of statins; genetic polymorphisms in SLCO1B1 have been shown to be associated with increased systemic exposure of statins and increased risk of statin-induced myopathy (Link et al. 2008). While OATP1B3 has overlapping substrate specificity with OATP1B1, distinct substrate specificity has been reported; repaglinide and troglitazone sulfate are more selective substrates for OATP1B1, while digoxin, cholecystokinin-8, and paclitaxel show selectivity for OATP1B3 (Table 9.1). Bile acids are known to be transported by OATP1A2, OATP1B1, and OATP1B3, but OATP2B1-mediated bile acid transport has not been investigated.
OATs ( SLC22A ). Organic anion transporters (OATs) mediate transport of small anionic compounds in exchange for dicarboxylate ions. Among six human OATs that have been functionally characterized, OAT2 (SLC22A7) is expressed in the basolateral membrane of hepatocytes and renal proximal tubule cells, while OAT7 (SLC22A9) is expressed exclusively in the liver (Hagenbuch 2010). The known substrates for human OAT2 include prostaglandins, dehydroepiandrosterone sulfate (DHEAS), E1S, and anticancer drugs such as 5-fluorouracil and methotrexate (Table 9.1). OAT7, a recently characterized OAT, has been shown to transport sulfated hormones such as E1S and DHEAS when expressed in X. laevis oocytes (Shin et al. 2007). Interestingly, typical OAT substrates such as para-aminohippurate, α-ketoglutarate, prostaglandins, cyclic nucleotides, and salicylic acid were not transported by OAT7, while OAT7 could transport the short-chain fatty acid butyrate (Shin et al. 2007).
OCTs ( SLC22A ). Organic cation transporters (OCTs) are electrogenic uniporters that primarily mediate the transport of small cations (previously referred to as type I cations) in a sodium-independent fashion. Human OCT1 (SLC22A1) is expressed exclusively at the basolateral membrane of the hepatocytes (Soroka et al. 2010). OCT1 is known to transport antiviral drugs such as acyclovir and ganciclovir, as well as the H2-receptor antagonists famotidine and ranitidine (Table 9.1). OCT3 (SLC22A3) and OCTN2 (SLC22A5) also are expressed in the liver, but expression levels are relatively low compared to OCT1 and the functional role of these proteins in hepatic drug transport remains to be elucidated (Hagenbuch 2010).
OSTα/β ( SLC51A / 51B ). Organic solute transporter (OST) α/β is a heteromeric transporter that is expressed widely in the liver, small intestine, kidney, testis, and adrenal gland. In hepatocytes, OSTα/β is expressed in the basolateral membrane and is able to transport bile acids, E1S, and DHEAS. Since OSTα/β mediates substrate transport by facilitated diffusion, OSTα/β-mediated transport is bidirectional depending on the substrate’s electrochemical gradient (Soroka et al. 2010). Gene expression levels of SLC51A and SLC51B are positively regulated by bile acids through farnesoid X receptor (FXR), and it has been shown that hepatic OSTα/β is up-regulated in patients with chronic cholestatic disease such as primary biliary cirrhosis (PBC) (Boyer et al. 2006).
9.2.2 Hepatic Canalicular Efflux Transport Proteins
Biliary excretion is an important elimination pathway for many endogenous and exogenous substances. Canalicular transport proteins responsible for biliary excretion of substances primarily belong to the ATP-binding cassette (ABC) family of proteins that mediate ATP-dependent transport of solutes.
P-glycoprotein (MDR1, ABCB1 ). P-glycoprotein (P-gp) was first identified in multidrug-resistant (MDR) tumor cells (Juliano and Ling 1976) and is the most well-characterized ABC transport protein. P-gp is widely distributed in liver, intestine, kidney, and brain. In hepatocytes, P-gp is expressed in the canalicular membrane and is responsible for biliary excretion of bulky hydrophobic and cationic substrates including many chemotherapeutic agents (e.g., daunorubicin, doxorubicin, etoposide, paclitaxel, vinblastine, vincristine), cardiac glycosides (e.g., digoxin), rhodamine 123, cyclosporine A, and protease inhibitors (e.g., amprenavir, indinavir, nelfinavir, ritonavir, saquinavir). Substrate specificity of P-gp largely overlaps with that of CYP3A4, resulting in synergistic defense mechanisms against xenobiotics. The ABCB1 gene is highly polymorphic, and hepatic expression levels of P-gp are highly variable between different individuals.
MDR3 ( ABCB4 ). MDR3, a phospholipid flippase, is involved in the biliary secretion of phospholipids and cholephilic compounds that form micelles with bile acids. Biliary excretion of phospholipids protects the lumen of the bile canaliculus by solubilizing toxic bile acids (Oude Elferink and Paulusma 2007). A deficiency in the ABCB4 gene leads to progressive familial intrahepatic cholestasis type 3 (PFIC3), a disease that is characterized by increased γ-glutamyltranspeptidase levels, ductular proliferation, and inflammatory infiltrate that can progress to biliary cirrhosis. Individuals with decreased MDR3 activity are susceptible to cholesterol gallstone formation, which is known as low-phospholipid-associated cholelithiasis (Rosmorduc et al. 2003). Inhibition of MDR3-mediated biliary phospholipid excretion is one proposed mechanism of hepatotoxicity induced by drugs such as itraconazole.
BSEP ( ABCB11 ). The bile salt export pump (BSEP) is the major transport protein that mediates the biliary excretion of conjugated and unconjugated bile acids. Some drugs such as pravastatin may be substrates for BSEP based on membrane vesicle studies (Hirano et al. 2005); however, the relative role of BSEP vs. other canalicular transport proteins in the biliary excretion of pravastatin in hepatocytes or the intact liver remains to be determined (Kullak-Ublick et al. 2000). PFIC2 patients do not express BSEP protein due to a genetic polymorphism in the ABCB11 gene; this leads to hepatocellular injury and necrosis caused by increased intracellular concentrations of detergent-like bile acids (Kullak-Ublick et al. 2004). Inhibition of BSEP-mediated bile acid transport is purported to be one mechanism of drug-induced liver injury (DILI) associated with hepatotoxic drugs such as troglitazone, bosentan, and cyclosporine.
MRP2 ( ABCC2 ). Multidrug resistance-associated protein (MRP) 2 plays an important role in the biliary excretion of organic anions, including bilirubin-diglucuronide, glutathione conjugates, sulfated bile acids, and divalent bile acid conjugates, as well as numerous drugs such as sulfopyrazone, indomethacin, penicillin, vinblastine, methotrexate, and telmisartan (Table 9.2). The absence of functional MRP2 due to genetic mutations in ABCC2 results in Dubin–Johnson syndrome (DJS), which is characterized by decreased biliary excretion of bilirubin conjugates and hyperbilirubinemia (Tsujii et al. 1999).
BCRP ( ABCG2 ). Breast cancer resistance protein (BCRP) is highly expressed in the canalicular membrane of hepatocytes as well as in the intestine, breast, and placenta. BCRP is a half-transport protein that forms a functional homodimer and is responsible for transport of glucuronide and sulfate conjugates (e.g., E1S, estradiol-17β-D-glucuronide (E217G), SN38-glucuronide), anticancer drugs (e.g., irinotecan, SN-38, methotrexate, daunorubicin, doxorubicin), and some statins (e.g., pitavastatin, rosuvastatin) (Table 9.2).
MATE1 ( SLC47A1 ). Human MATE1 is expressed predominantly in the canalicular membrane of hepatocytes and the luminal membrane of renal tubular cells. MATE1 has been shown to transport organic cations across the membrane in a bidirectional manner dependent on the proton gradient. Substrate specificity of MATE1 primarily overlaps with the OCTs; MATE1 substrates include acyclovir, N-methylpyridinium, and tetraethylammonium (Table 9.2).
9.2.3 Hepatic Basolateral Efflux Transport Proteins
Xenobiotics in the liver also may be excreted across the basolateral membrane into sinusoidal blood. MRP1, 3, 4, 5, and 6 are involved in cellular transport of both hydrophobic uncharged molecules and hydrophilic anionic compounds. OATPs also may function as basolateral efflux transport proteins under certain conditions, although the in vivo role of OATPs in basolateral efflux remains to be elucidated (Li et al. 2000).
MRP3 ( ABCC3 ). MRP3 was first localized in human and rat hepatocytes and is also expressed widely in kidney, pancreas, enterocytes, cholangiocytes, and the gallbladder (Keppler 2011). The expression level of MRP3 in hepatocytes is low in normal liver, but markedly increased in patients with DJS who lack functional MRP2, and in patients with cholestatic liver disease, consistent with the important compensatory role of MRP3 when the function of biliary transport proteins is impaired (Konig et al. 1999; Wagner et al. 2009; Hirohashi et al. 1999). MRP3 is responsible for the basolateral efflux of glutathione and glucuronide conjugates (e.g., acetaminophen glucuronide), methotrexate, and E217G.
MRP4 ( ABCC4 ). MRP4 is localized in many different tissues including liver, kidney, brain, and prostate (Keppler 2011). The expression level of MPR4 in normal hepatocytes is low, but is markedly induced under cholestatic conditions. MRP4 is responsible for the basolateral efflux of bile acids when the normal vectorial transport of bile acids from the hepatocyte into bile is compromised (Wang et al. 2011). MRP4-mediated bile acid transport requires glutathione, because bile acids and glutathione are co-transported by MRP4 (Rius et al. 2003). MRP4 also transports cyclic nucleotides (e.g., cAMP and cGMP), nucleoside analogs (e.g., zidovudine, lamivudine, and stavudine), purine analogs (e.g., 6-mercaptopurine and 6-thioguanine), and non-nucleotide substrates such as methotrexate (Sampath et al. 2002).
Other MRPs. MRP1 (ABCC1) is expressed in several tissues including liver, lung, testis, kidney, skeletal and cardiac muscle, placenta, and macrophages (Keppler 2011). MRP1 is responsible for the efflux of various organic anions, such as glucuronide, glutathione, and sulfate conjugates of drugs. MRP5 (ABCC5) transports cyclic nucleotides (e.g., cAMP and cGMP) and purine analogs (e.g., 6-mercaptopurine and 6-thioguanine). The expression levels of MRP1 and MRP5 in healthy liver are relatively low, but protein levels of hepatic MRP1 and MRP5 were significantly increased in patients with PBC (Barnes et al. 2007). Protein expression of hepatic MRP5 also was increased in acetaminophen-induced liver failure, suggesting a protective role for this protein in hepatic injury (Barnes et al. 2007). MRP6 (ABCC6) is localized in the basolateral membrane of hepatocytes and transports glutathione conjugates and the endothelin receptor antagonist BQ-123. Expression of MRP6 was not altered in patients with PBC or acetaminophen-induced liver failure, and the functional roles of MRP6 remain to be explored (Barnes et al. 2007).
9.3 In Vitro Models and Methods to Study Hepatobiliary Drug Transport
9.3.1 Membrane Vesicle System
With the development of membrane vesicle assays, it became possible to perform functional studies to identify and characterize distinct efflux transport systems. Historically, vesicle transport assays were performed using membranes isolated from hepatic tissue from the relevant species. Functional studies of hepatic efflux transporters in either canalicular liver plasma membrane (cLPM) or basolateral liver plasma membrane (bLPM) vesicles were enabled by the development of a method to separate these two membrane leaflets in the early 1980s (Meier et al. 1984; Blitzer and Donovan 1984). This assay system was used to identify and characterize bile acid and bilirubin glucuronide transport across the canalicular membrane and led to the discovery of BSEP and MRP2 (Jedlitschky et al. 1997; Gerloff et al. 1999). The isolation of high-purity apical and basolateral membranes from tissue is labor-intensive and technically challenging. Since inside-out and right-side-out vesicles coexist, ATP-dependent basolateral efflux data generated with bLPMs may be confounded by influx transporters. Naturally, these membranes contain multiple transport proteins; therefore, it is impossible to identify specific substrates for ABC efflux proteins.
Due to evolving molecular biology techniques and identification of individual transport proteins, this tissue-based assay system has been replaced by vector-transfected and virus-infected cell lines expressing a single ABC-transporter. In the early 1990s, baculovirus-infected insect cells (Spodoptera frugiperda, Sf9) were used widely to generate membrane vesicles containing the transport protein of interest because this system allowed high expression of transport proteins (Germann et al. 1990). Disadvantages of these membrane vesicles are the different glycosylation pattern and a lower cholesterol content in Sf9 cells compared to mammalian cell lines (Pal et al. 2007), which may affect the localization and function of transporters. For example, MRP2-mediated transport and ATPase activity were altered by membrane cholesterol content (Pal et al. 2007). Therefore, either transiently or stably transfected mammalian cell lines from human embryonic kidney (HEK) 293, Madin–Darby canine kidney (MDCK) II, or porcine kidney epithelial (LLC-PK1) cells are now used more frequently for preparation of membrane vesicles for transporter studies. These systems are suitable for high-throughput screening of substrates and inhibitors for a single transport protein.
The most commonly used membrane system for efflux transporters is the vesicular transport system that detects direct translocation of substrates into inside-out vesicles (Fig. 9.2). Substrates taken up into inside-out vesicles are separated from the incubation solution using rapid filtration and quantified by high-performance liquid chromatography (HPLC), liquid chromatography mass spectrometry (LC/MS), scintillation counting, or fluorescence detection. ATP-dependent transport is calculated by subtracting the transport of substrate in the presence of AMP from that in the presence of ATP; endogenous transporter-mediated transport is excluded by subtracting ATP-dependent transport of substrate in control vesicles from that in transporter-expressing vesicles. This method detects direct transport of substrate, and kinetic parameters such as the Michaelis–Menten constant (K m) and the maximal transport velocity (V max) can be calculated. This method is ideal for the detection of drug–drug interactions (DDIs) or drug–endogenous compound interactions using a probe substrate. However, it is difficult to detect the transport of highly permeable compounds due to passive diffusion out of the membrane vesicles.
The ATPase method, which detects the hydrolysis of ATP in the presence of an interacting compound, is more suitable for determining the transport of highly permeable compounds. The ATPase method is based on the principle that ABC transporters utilize the chemical energy of ATP cleavage to mediate the transport of substrates across membranes. The inorganic phosphate produced during this process is directly proportional to the activity of the transporter and can, for example, be monitored by colorimetric detection. This method is most commonly used for high-throughput screening for P-gp and BCRP, although it also is available commercially for other ABC efflux transporters. However, ATPase systems are indirect measures of transport, and are not always suitable for distinguishing between potential substrates, inhibitors or modulators. Major applications of the membrane vesicle systems as well as their advantages and disadvantages when used to study hepatobiliary drug transport are summarized in Table 9.3.
9.3.2 Transfected Cells
Bacterial, insect, and mammalian cells have been transfected with vector constructs allowing over-expression of transport proteins for identification of transport processes. The transfected cell model is illustrated in Fig. 9.2. Nonpolarized cells such as Sf9 and HEK293 cells have been used for over-expression of a single transport protein, while polarized cells have been employed for the over-expression of one or more basolateral proteins in concert with apical protein(s). Transfected cell models can be used for high-throughput screening of substrates and inhibitors of a specific over-expressed transport protein. The major limitation of this model is that generally it is not suitable for the study of efflux transporters. Hypothetically, in transfected cells expressing a single efflux protein, transported substrates should demonstrate lower cellular accumulation, and inhibitors should increase drug accumulation compared to the parental cell line. However, substrates of drug efflux transporters are usually organic anions that do not easily penetrate into the cell in the absence of influx transport proteins. To overcome this limitation, polarized mammalian cells (e.g., MDCKII, LLC-PK1) have been used for transfection of one or more influx and/or efflux transport proteins. Depending on the transporter, the protein will be routed to the apical or basolateral membrane in polarized cells; expression of influx transporters allows import of the substrates transported by the ABC efflux transporters. Furthermore, the combined expression of influx and efflux proteins enabled the analysis of vectorial transport, which is a key step in hepatobiliary elimination (Sasaki et al. 2002; Cui et al. 2001). These double-transfected polarized cell lines were first developed by Cui et al. in the early 2000s (Cui et al. 2001) and are now valuable tools to study transcellular transport. Using MDCKII cells expressing both Oatp1b2 and Mrp2, Sasaki et al. demonstrated a good correlation between the clearance values obtained from in vitro transcellular transport and in vivo biliary clearance (Sasaki et al. 2004). Triple and quadruple transfected cell lines OATP1B1/MRP2/MRP3 or MRP4, as well as OATP1B1/OATP1B3/OATP2B1/MRP2 have been developed to better predict hepatobiliary processes (Kopplow et al. 2005; Hirouchi et al. 2009). Recently, a triple-transfected cell line expressing influx and efflux transporters as well as the drug-metabolizing enzyme uridine diphosphate glucuronosyl transferase (UGT) 1A1 has been described to study transporter-metabolism interplay (Fahrmayr et al. 2012). As our understanding of the role of influx and efflux transporters in facilitating the vectorial transport of xenobiotics across the hepatocyte has evolved, the use of polarized mammalian cells has become more popular to identify substrates and inhibitors of hepatic transport proteins. However, protein trafficking or localization in transfected cells may differ from human hepatocytes, depending on the species or type of transfected cells. Also, it is difficult to standardize the relative expression levels of transporters, and the relative contribution of a particular transport protein to overall transport of the substrate cannot be determined. The major applications of transfected cells together with their advantages and disadvantages when used to study hepatobiliary drug transport are summarized in Table 9.3.
9.3.3 Hepatocytes
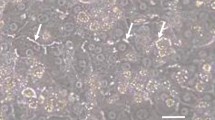
Freshly isolated hepatocytes are the most comprehensive cell-based model to study hepatic drug transport and remain the gold standard. However, the scarcity of fresh, healthy human liver tissue suitable for hepatocyte isolation is a significant limitation, and isolation of human hepatocytes is technically challenging. Recent advances in technology have made good-quality cryopreserved human hepatocytes commercially available at the user’s convenience. Cryopreserved human hepatocytes have been used widely to study drug metabolism (Lau et al. 2002) and substrate influx in suspension (Houle et al. 2003; Shitara et al. 2003a; De Bruyn et al. 2011); cryopreserved hepatocytes cultured in a sandwich configuration repolarize and form bile canalicular networks (Bi et al. 2006). Both the suspended and sandwich-cultured hepatocyte models are illustrated in Fig. 9.2. However, not all batches of cryopreserved hepatocytes are qualified for sandwich-culture due to limitations in cell attachment and the loss of expression, localization, and/or function of transport proteins and metabolizing enzymes. Thus, further research is needed to improve the cryopreservation process.
Suspended hepatocytes. Fresh or cryopreserved suspended hepatocytes are a useful tool to characterize hepatic influx and metabolism processes, and inhibition studies can be performed with this system. However, suspended hepatocytes cannot be used for induction studies because the viability of hepatocytes in suspension cannot be maintained longer than several hours. Additionally, hepatocytes lose their cellular polarity during isolation and internalization of canalicular transport proteins has been demonstrated, which precludes the use of suspended hepatocytes to predict biliary clearance (Bow et al. 2008).
Sandwich-cultured hepatocytes. In contrast to conventionally plated hepatocytes, hepatocytes cultured between two layers of gelled collagen (“sandwich-configuration”) develop functional canalicular domains with proper localization of transport proteins and metabolic enzyme expression (Swift et al. 2010). Liu et al. demonstrated that rat sandwich-cultured hepatocytes (SCH) could be used to investigate the hepatobiliary disposition of substrates using Ca2+ depletion methods (Liu et al. 1999a, b). This method involves pre-incubation of SCH with Hanks’ balanced salt solution (HBSS) containing Ca2+ (standard HBSS) or Ca2+-free HBSS for 10 min. Ca2+-free HBSS disrupts tight junctions and opens the bile canalicular networks, while incubation with standard HBSS maintains tight junction integrity. Subsequently, cells are rinsed and incubated with substrate in standard HBSS for a predetermined period of time. Accumulation of substrate in cells + bile vs. cells can be determined in standard and Ca2+-free HBSS buffers, respectively. The amount of substrate excreted into the bile canaliculi can be estimated as the difference in accumulation in standard and Ca2+-free HBSS buffers, and in vitro biliary clearance may be obtained by dividing the amount of drug in the bile compartment by the area under the concentration–time curve (AUC) in the dosing medium. This system has been applied to hepatocytes from many species and has been used extensively to assess biliary clearance as a measure to improve hepatic clearance predictions (Swift et al. 2010). Biliary clearance values scaled from in vitro intrinsic biliary clearance measurements obtained in SCH have been shown to correlate well with in vivo biliary clearance data in rats (Abe et al. 2008; Fukuda et al. 2008; Liu et al. 1999c; Li et al. 2010, Nakakariya et al. 2012) and humans (Abe et al. 2009; Ghibellini et al. 2007).
To determine the contribution of a specific transport protein to the disposition of a substrate, a transporter-specific reference compound can be employed in hepatocytes as well as transport protein over-expressing cells (Kouzuki et al. 1999). Basically, this method compares the ratio of influx clearances of the test and the reference compound in both systems. However, the results are based on the assumption that the reference compound is specific for the respective transport protein, which—due to the overlapping substrate spectrum of transport proteins—is hardly ever the case.
SCH from naturally occurring, genetically deficient rodents lacking a specific transport protein, such as the Mrp2-deficient Wistar (TR−) and Eisai-hyperbilirubinemic Sprague–Dawley (SD) rats (EHBR), and the Mdr1a-deficient CF-1 mice, have been useful tools to evaluate the role of a transporter in the disposition of substrates (Abe et al. 2008). Also, genetically modified animals that lack specific transporter(s) can be used to assess the potential involvement of specific transport protein(s) in DDIs or polymorphisms that impair the function of drug transport proteins. However, care must be taken in interpreting the results of these studies because compensatory changes in drug-metabolizing enzymes and/or other transport proteins may exist. Also, species difference in the expression, localization, and function of transport proteins between humans and genetically modified animals may limit clinical applicability of the data.
RNA interference (RNAi) of single or multiple transport proteins is a powerful tool to explore the consequences of loss of transport protein function. Synthetic small interfering RNA (siRNA) was transfected into rat SCH to specifically knock down Mrp2 and Mrp3 (Tian et al. 2004). Infection of rat SCH with adenoviral vectors expressing short hairpin RNA (shRNA) targeting Bcrp showed a significant decrease in protein expression and activity of this canalicular transport protein (Yue et al. 2009). Recently, Liao et al. successfully knocked down OATP1B1, 1B3, and 2B1 in sandwich-cultured human hepatocytes using special delivery media containing siRNA (Liao et al. 2010). These studies have demonstrated the utility of knock down of specific transport proteins in SCH. However, careful optimization is required because knock down of one transport protein may alter the expression/function of metabolic enzymes and other transport proteins.
Other hepatocyte models. Limited exposure of liver tissue to collagenase results in hepatocyte couplets preserving closed canalicular vacuoles and hepatocyte polarity (Milkiewicz et al. 2002). Hepatocyte couplets have been used to study hepatobiliary transport mechanisms underlying bile secretion (Boyer 1997; Coleman et al. 1995). HepaRG cells, a human hepatoma cell line, maintain specific liver functions such as drug-metabolizing enzymes and transport proteins. In HepaRG cells, mRNA expression levels and functional activity of basolateral and canalicular transport proteins were comparable to those of human hepatocytes (Le Vee et al. 2006). Also, expression levels of transport proteins were up-regulated by known inducers, indicating that HepaRG cells maintain transactivation pathways that regulate expression of transport proteins (Le Vee et al. 2006). Since HepaRG cells are readily available compared to human hepatocytes, they may be a useful system to study hepatobiliary transport of compounds. However, HepaRG cells differentiate into biliary epithelial cells as well as hepatocytes, and the fraction of cells that differentiate into hepatocytes varies among different cultures and plates. In addition, more characterization is warranted including cell polarity and polarized expression of relevant transport proteins. Human inducible pluripotent stem (iPS) cells have been successfully differentiated into hepatocyte-like cells that exhibit human hepatocyte function such as inducible CYP450 activity (Song et al. 2009). Although the expression and function of transport proteins still needs to be characterized, hepatocytes derived from individual-specific iPS cells may serve as a novel tool to study hepatobiliary transport of compounds in specific individuals. Newer three-dimensional microfluidic models (e.g., liverchip, Hμrel) that more closely resemble in vivo liver physiology are currently under development. Further investigations are needed to explore the utility of these more complex models. The major applications of hepatocytes as well as their advantages and disadvantages when used to study hepatobiliary drug transport are summarized in Table 9.3.
9.3.4 Isolated Perfused Liver Models
For decades, in situ or isolated perfused liver (IPL) studies have been used to investigate the physiology and pathophysiology of the liver. The model is illustrated in Fig. 9.2. Publications regarding the use of IPLs date back to the 1950s, when the metabolism of drugs and endogenous compounds was first studied using this approach. In contrast to in vitro models such as isolated hepatocytes and liver slices, the IPL preserves hepatic architecture, cell polarity, and bile flow. Furthermore, this model enables simultaneous sampling of bile as well as inflow and outflow perfusate; liver tissue may be obtained at the end of the study. Thus, the IPL provides a rich dataset amenable to pharmacokinetic modeling and makes this system useful for mechanistic studies of hepatobiliary transport.
In IPL studies, the liver may be perfused in a single-pass or recirculating mode. A single-pass perfusion system is used to determine directly the steady-state hepatic extraction ratio of a compound. In the single-pass system, outflow perfusate from the liver does not re-enter the system, and the perfusion medium is pumped into the liver at a constant rate. Thus, steady-state conditions can be achieved readily, and drug and metabolite disposition can be examined at different dose levels in a single preparation. Also, experiments can be designed so that each liver serves as its own control. Hemoglobin-free oxygenated perfusate often is used in the single-pass perfusion system because a large volume of perfusate is required. Furthermore, flow rates that are 2–3 times higher than physiologic blood flow are required to maintain adequate oxygen delivery. In recirculating systems, blood-containing perfusate is oxygenated and recirculated through the liver at a constant flow rate that is similar to liver blood flow in vivo. The hepatic clearance of the drug can be determined from the dose introduced into the reservoir and the AUC in the reservoir. In recirculating systems, the only route of metabolite elimination is via biliary excretion, and metabolites usually accumulate in hepatocytes or in the perfusate, if they are able to flux across the hepatic basolateral membrane. Accumulation of metabolites may be advantageous in mass-balance determination of metabolite formation and kinetic evaluation of hepatic influx of metabolites. However, potential drug–metabolite interactions may be magnified in the recirculating system compared with the single-pass IPL.
The IPL model can be applied to transporter knock-out animals in combination with chemical inhibitors to investigate the contribution of specific hepatic drug efflux transporters (Hoffmaster et al. 2004; Zamek-Gliszczynski et al. 2005). However, these experiments are relatively expensive and low throughput. Furthermore, species-specific differences between human and rodent transport proteins may significantly limit the clinical applicability of information generated using this approach. Whether or not the results obtained from IPL analyses can be extrapolated to in vivo findings in humans remains compound-dependent. The major applications of the IPL model, as well as advantages and disadvantages when applied to studying hepatobiliary drug transport, are summarized in Table 9.3.
9.4 In Vivo Models and Methods to Study Hepatobiliary Drug Transport
In vivo pharmacokinetic/pharmacodynamic studies in humans are the gold standard for investigating the role of hepatic transporters. However, the complexity of the hepatobiliary system, and considerable substrate overlap for many of the transporters, makes it difficult to identify the function of specific transport proteins based on in vivo studies. Genetically modified animals and patients with polymorphisms in transporter genes are valuable in evaluating the function of transport proteins, but species differences in transport protein function, and compensatory up-regulation of other transport proteins, may confound the translation of in vivo data generated in preclinical species to humans.
9.4.1 In Vivo Biliary Excretion Studies
Biliary excretion is an important route of elimination for some drugs and a potential site of drug interactions that may alter hepatic and/or systemic drug exposure. Accurate measurement of biliary clearance and understanding the mechanism(s) of biliary excretion are very important in evaluating the contribution of biliary clearance to total systemic clearance, predicting DDIs, identifying the contribution of enterohepatic recirculation to overall systemic and intestinal exposure, and elucidating potential mechanisms of hepatobiliary toxicity.
Bile duct-cannulation. Animals, primarily rodents, often are used to determine the extent and the mechanisms of biliary excretion in vivo. Complete collection of bile is possible in bile duct-cannulated animals, which generates information about the extent of biliary excretion and the potential involvement of enterohepatic recirculation in overall systemic exposure. Proper study design is critical to obtain useful information from bile duct-cannulated animals. For example, if bile flow is exteriorized for extended periods of time to obtain complete bile collection, intravenous or intestinal supplementation with bile acids should be considered to replenish the bile acid pool. In vivo biliary clearance data has been used to assess the accuracy of in vitro methods of estimating biliary clearance; reasonable in vitro-in vivo correlations have been obtained (Fukuda et al. 2008; Li et al. 2010; Abe et al. 2009; Nakakariya et al. 2012). Genetically modified animals that are deficient in specific transport proteins has improved our understanding of the complex molecular processes involved in excretion of endogenous and exogenous compounds into bile. However, significant interspecies differences in substrate specificity and regulation of transport proteins have been reported, which complicates the direct extrapolation of animal data to humans (Ishizuka et al. 1999).
Aspiration of duodenal fluids. Determining the biliary clearance of drugs in vivo in humans is challenging because it is difficult to access bile for sample collection from healthy human subjects. Bile samples can be collected in postsurgical patients with underlying hepatobiliary disease via a T-tube or nasobiliary tube (Brune et al. 1993; Verho et al. 1995). However, it is difficult to rule out the effects of underlying hepatobiliary disease (e.g., altered protein expression, function, localization, and/or bile flow) in these patients. In healthy subjects, feces often are used as a surrogate to quantify the amount of drug excreted via non-renal pathways. However, this method cannot distinguish between biliary excretion, intestinal secretion, and unabsorbed drug following oral administration. Moreover, unstable drugs may not be recovered in feces due to the long exposure to the intestinal contents and colonic flora. Furthermore, drugs that are reabsorbed in the intestine and undergo enterohepatic recycling will not be recovered completely in the feces.
Oroenteric tube. Sampling duodenal fluids in healthy volunteers using an oroenteric tube alleviates some of the above-mentioned problems. Duodenal bile is representative of gallbladder bile in terms of bile composition, and collecting bile upon discharge from the biliary tract into the small intestines excludes the contribution of intestinal excretion and minimizes loss associated with metabolism and/or reabsorption. Oroenteric tubes have been used commonly to withdraw pancreatico-biliary secretions from the duodenum in medical practice and have been used to study the biliary excretion of drugs (Galatola et al. 1991; Northfield and Hofmann 1975). Use of an occlusive balloon can facilitate more complete bile collection, and incomplete bile collection can be corrected by perfusing nonabsorbable markers. The most challenging part of this method is incomplete and highly variable recovery of compounds excreted into bile. Cholecystokinin 8 (CCK-8) may be administered intravenously to pharmacologically stimulate gall bladder empting, but interindividual response is variable. Ghibellini et al. introduced a novel method to evaluate the degree of gallbladder contraction and to detect any leakage of bile due to partial occlusion of the intestine (Ghibellini et al. 2004). Subjects were administered a hepatobiliary imaging agent (e.g., 99mTc-mebrofenin), and the gall bladder ejection fraction was calculated from the abdominal gamma images of the study participants during gallbladder contraction. Incorporation of the ejection fraction as a correction factor in the calculation of the amount of drug excreted into the duodenum accounted for the variability in biliary excretion of the drug (Ghibellini et al. 2006). This type of study provides direct evidence for biliary excretion and more precise quantification of biliary clearance, but is not used widely due to requirements for a gamma camera and personnel with expertise in gamma scintigraphy. The major applications of the in vivo biliary excretion models, as well as advantages and disadvantages when used to study hepatobiliary drug transport, are summarized in Table 9.4.
9.4.2 Hepatobiliary Imaging Techniques
Although techniques are available to study genetic polymorphisms and the expression of drug transporters at the mRNA and protein level, these data do not necessarily correlate with transporter function. Thus, there continues to be considerable interest in studying transporter function noninvasively. Pharmacokinetic analyses based on plasma concentrations in clinical studies provide information on overall hepatic clearance; however, differentiation between influx and canalicular efflux is not possible. While variations in influx activity of transporters might have a profound influence on systemic concentrations, altered canalicular efflux might significantly affect liver concentrations without having measureable effects upon systemic exposure. This is especially relevant for drugs where the target site for effect or toxicity is within the hepatocyte. Therefore, quantitative estimations of tissue concentrations in vivo are necessary to investigate variations in efflux caused by DDIs or transporter polymorphisms. Furthermore, assessing the functional transport activity of P-gp, MRP2, or BCRP in the human liver might benefit the diagnosis of transporter deficiency-related diseases (e.g., PFIC3 and DJS). Several noninvasive imaging techniques such as magnetic-resonance imaging (MRI), single-photon emission computed tomography (SPECT) using 99mTc-labeled compounds, and positron emission tomography (PET) using short-lived 11C, 13N, 15O or 18F isotopes have been employed to visualize and measure hepatic transporter activity in vivo.
Magnetic-resonance imaging. The first MRI contrast agents were developed in the early 1980s (e.g., gadopentetate dimeglumine, gadodiamide, gadoteridol). These extremely hydrophilic compounds distributed primarily into the extracellular fluid and were excreted predominantly via the kidney. Because of this distribution pattern, these contrast agents have been used primarily for angiography and to detect lesions in the brain. The development of gadobenate dimeglumine (Gd-BOPTA) and gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid (GD-EOB-DPTA, gadoxetic acid) allowed liver imaging and facilitated the distinction between normal and pathological tissue. Using these imaging agents, most hepatic tumors appear as hypointense lesions because they do not possess functional hepatocytes, while positive hepatocyte-enhancement may be observed in patients with tumors of hepatocellular origin (e.g., hepatocellular carcinoma, HCC). Hepatocyte influx of gadolinium compounds is thought to be mediated by OATPs (Narita et al. 2009; Leonhardt et al. 2010), while MRP2 mediates biliary excretion (Pascolo et al. 2001). Indeed, studies indicated that the degree of expression and localization of OATP1B1/1B3 and MRP2 affect the degree of hepatocyte-specific enhancement in HCC (Narita et al. 2009; Tsuboyama et al. 2010).
SPECT and PET imaging. For quantitative determination of drug transporters, the radionucleotide-based molecular imaging techniques SPECT and PET hold great promise. Initially, PET was used to quantify P-gp function in the blood–brain-barrier; several 11C-labeled tracers have been developed for this purpose (verapamil, carvedilol, N-desmethyl-loperamide, daunorubicin, paclitaxel). However, PET imaging also can be employed to study influx and excretion in other tissues. In 1995, Guhlmann et al. determined the hepatobiliary and renal excretion of N-[11C] acetyl-leukotriene E4 in rats and monkeys by PET analysis. In rats, cholestasis due to bile duct obstruction as well as Mrp2 deficiency (TR− rats) led to prolonged organ storage, metabolism, transport back into the blood, and subsequently enhanced renal elimination compared to wild-type rats (Guhlmann et al. 1995). Currently, compounds are being developed to evaluate hepatobiliary transport (Takashima et al. 2010). In order to be useful clinically, such probes will need to be metabolically stable in humans, and ideally, the probes should be a substrate for a specific hepatic influx and/or efflux transport protein.
SPECT tracers directly emit gamma radiation, whereas PET tracers emit positrons, which annihilate on contact with electrons, resulting in emission of gamma photons. Cholescintigraphy studies with 99mTc-N(2,6-dimethylphenyl carbamoylmethyl) iminodiacetic acid (99mTc-HIDA) were performed in patients with liver disease in the late 1970s/early 1980s for diagnostic imaging of hepatobiliary disorders (Stadalnik et al. 1981). Furthermore, 99mTc-mebrofenin has been used widely to diagnose cholestasis, gallbladder function, and bile duct leakage. In 2004, Hendrikse et al. proposed that both compounds were useful tools to evaluate the function of Mrp1, Mrp2, and P-gp in vivo (Hendrikse et al. 2004). Another compound, 99m Tc-sestamibi, has been suggested to be a probe for P-gp function (Luker et al. 1997). This compound originally was developed for imaging of myocardial ischemia and is a positively charged, lipophilic compound that readily enters cells and accumulates in mitochondria. In vivo studies with 99mTc-sestamibi showed that this substance is retained in the liver and kidneys after P-gp inhibition with PSC833, suggesting that inhibition of P-gp transport in these organs can be imaged with 99mTc-sestamibi (Luker et al. 1997). However, 99mTc-sestamibi is also a substrate for MRP1 (Gomes et al. 2009). In vivo biliary clearance values for 99mTc-sestamibi and 99mTc-mebrofenin were determined in healthy volunteers using an oroenteric catheter, which was designed to aspirate pancreatico-biliary secretions from the duodenum (Ghibellini et al. 2004, Ghibellini et al. 2007). The DDI between ritonavir and 99mTc-mebrofenin was evaluated in humans using this technique combined with a semi-physiologically-based pharmacokinetic modeling approach (Pfeifer et al. 2013). The major applications of in vivo imaging together with advantages and disadvantages when used to study hepatobiliary drug transport are summarized in Table 9.4.
9.5 Conclusions
Hepatic transport proteins play important roles in the hepatic influx and biliary excretion of drugs and metabolites, thus affecting the therapeutic efficacy and toxicity of many drugs. Therefore, it is important to understand the roles of hepatic transport proteins in the disposition of drugs and metabolites during the drug development process. Table 9.5 summarizes preferred approaches that can be used to answer specific questions regarding hepatobiliary drug transport. It is relatively straightforward to determine which transport proteins are capable of transporting drugs and metabolites by using membrane vesicle systems or cell lines expressing a single transport protein. However, determining the contribution of each transport protein to the hepatic influx or efflux of a specific compound in the whole cell/intact organ is not as straightforward and may require the use of several model systems (e.g., transfected cell lines and SCH) and scaling factors (e.g., relative activity factor) (Hirano et al. 2004). Moreover, reference compounds used to obtain the scaling factor between different systems are often not specific to a single transporter, which makes it difficult to determine the precise contribution of a single transporter to overall disposition.
Accurate predictions of clinically relevant drug interactions in hepatobiliary transport [either DDIs, drug–endogenous compound interactions (e.g., competition with bilirubin for influx or excretion) or drug–transporter interactions] are critical in drug development. Direct competitive interactions with a single protein can be predicted from membrane vesicle or transfected cell assays; however, accurate extrapolation to the in vivo setting requires an understanding of the unbound concentration at the site of transport. The ability of other transport proteins or drug-metabolizing enzymes to compensate for drug interactions cannot be predicted accurately from these simplistic systems, and intact hepatocytes (suspended for influx studies; sandwich-cultured for hepatic efflux and overall hepatobiliary disposition) or whole organ and/or in vivo studies are required. More complex drug-transporter interactions involving signaling cascades and/or regulatory mechanisms or interactions that involve generated drug metabolites require the complex machinery of the intact cell.
DILI is one of the most common reasons for withdrawal of drugs from the market, or failure of new drugs in clinical trials. Inhibition of canalicular BSEP, which leads to elevated hepatic exposure of detergent-like bile acids, has been reported as one mechanism of DILI. Some hepatotoxic drugs also are potent inhibitors of NTCP and/or MRPs. Thus, determining whether the drug and/or generated metabolite(s) inhibit(s) bile acid transport would provide key information about the drug’s potential for DILI. High-throughput screening is possible to determine the inhibitory effects of a specific compound on bile acid transport in membrane vesicles expressing a single transporter. However, model systems that enable the generation of metabolites and allow for direct measurement of bile acids accumulated in hepatocytes (e.g., SCH or IPL) provide more information to determine the potential for DILI. Hepatic exposure of the drug is important in predicting efficacy and toxicity, but this cannot be measured directly in vivo in humans nor predicted based on systemic exposure. Human SCH will provide invaluable information about the hepatic accumulation potential of drugs and generated metabolites, and how hepatic exposure changes when the function of transport proteins is altered due to disease states, drug interactions, or changes associated with genetic polymorphisms in transport proteins. Because only unbound drugs are available to interact with transporters, it is important to determine the intracellular unbound concentration. However, our current knowledge about intracellular unbound concentrations is limited, and development of in vitro systems to characterize hepatocellular binding/sequestration and the unbound concentration in the intact cell is needed.
Many tools and model systems are available to analyze the role of hepatic transport proteins in drug development. Current efforts are focused on assessing which tools should be appropriately used at defined steps in the drug development process, as well as how the resulting information can be used most efficiently to answer the key questions before the compound reaches the clinic. Important work continues to focus on mathematical modeling and simulation based on data generated from the various in vitro and in vivo models to accurately predict the role of hepatic transport proteins in drug disposition, and how alterations in hepatic transport could alter efficacy and/or toxicity.
Abbreviations
- 99mTc-HIDA:
-
99mTc-N(2,6-dimethylphenyl carbamoylmethyl) iminodiacetic acid
- ABC:
-
ATP-binding cassette
- AMP:
-
Adenosine monophosphate
- ATP:
-
Adenosine triphosphate
- AUC:
-
Area under the concentration–time curve
- BCRP:
-
Breast cancer resistance protein
- bLPM:
-
Basolateral liver plasma membrane
- BSEP:
-
Bile salt export pump
- BSP:
-
Bromosulfophthalein
- CF-1 mice:
-
Mdr1a-deficient mice
- cLPM:
-
Canalicular liver plasma membrane
- CYP450:
-
Cytochrome P450
- DDI:
-
Drug–drug interaction
- DHEAS:
-
Dehydroepiandrosterone sulfate
- DILI:
-
Drug-induced liver injury
- DJS:
-
Dubin–Johnson syndrome
- E1S:
-
Estrone 3-sulfate
- E217G:
-
Estradiol-17β-D-glucuronide
- EHBR:
-
Eisai-hyperbilirubinemic Sprague–Dawley rats
- FXR:
-
Farnesoid X receptor
- Gd-BOPTA:
-
Gadobenate dimeglumine
- Gd-EOB-DPTA:
-
Gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid
- HBSS:
-
Hanks-balanced salt solution
- HCC:
-
Hepatocellular carcinoma
- HEK cells:
-
Human embryonic kidney cells
- HMG-CoA:
-
3-Hydroxy-3-methyl-glutaryl coenzyme A
- HPLC:
-
High-performance liquid chromatography
- IPL:
-
Isolated perfused liver
- iPS cells:
-
Inducible pluripotent stem cells
- K m :
-
Michaelis–Menten constant
- LC/MS:
-
Liquid chromatography mass spectrometry
- LLC-PK1 cells:
-
Porcine kidney epithelial cells
- MATE:
-
Multidrug and toxin extrusion
- MDCK cells:
-
Madin–Darby canine kidney cells
- MDR:
-
Multidrug resistance
- MRI:
-
Magnetic-resonance imaging
- MRP:
-
Multidrug resistance-associated protein
- NCE:
-
New chemical entity
- NTCP:
-
Sodium taurocholate cotransporting polypeptide (human)
- Ntcp:
-
Sodium taurocholate cotransporting polypeptide (other species than human)
- OAT:
-
Organic anion transporter
- OATP:
-
Organic anion transporting polypeptide
- OST:
-
Organic solute transporter
- PBC:
-
Primary biliary cirrhosis
- PET:
-
Positron emission tomography
- PFIC2:
-
Progressive familial intrahepatic cholestasis type 2
- PFIC3:
-
Progressive familial intrahepatic cholestasis type 3
- Pgp:
-
P-glycoprotein
- RNA:
-
Ribonucleic acid
- RNAi:
-
RNA interference
- SCH:
-
Sandwich-cultured hepatocytes
- SD rat:
-
Sprague–Dawley rat
- shRNA:
-
Short hairpin RNA
- siRNA:
-
Small interfering RNA
- SLC:
-
Solute carrier
- SLCO:
-
Solute carrier organic anion
- SPECT:
-
Single-photon emission computed tomography
- TR− rat:
-
Mrp2-deficient Wistar rat
- UGT:
-
Uridine diphosphate glucuronosyl transferase
- V max :
-
Maximal transport velocity
References
Abe K et al (2008) In vitro biliary clearance of angiotensin II receptor blockers and 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors in sandwich-cultured rat hepatocytes: comparison with in vivo biliary clearance. J Pharmacol Exp Ther 326(3):983–990
Abe K, Bridges AS, Brouwer KLR (2009) Use of sandwich-cultured human hepatocytes to predict biliary clearance of angiotensin II receptor blockers and HMG-CoA reductase inhibitors. Drug Metab Dispos 37(3):447–452
Barnes SN et al (2007) Induction of hepatobiliary efflux transporters in acetaminophen-induced acute liver failure cases. Drug Metab Dispos 35(10):1963–1969
Bi YA, Kazolias D, Duignan DB (2006) Use of cryopreserved human hepatocytes in sandwich culture to measure hepatobiliary transport. Drug Metab Dispos 34(9):1658–1665
Blitzer BL, Donovan CB (1984) A new method for the rapid isolation of basolateral plasma membrane vesicles from rat liver. Characterization, validation, and bile acid transport studies. J Biol Chem 259(14):9295–9301
Bourdet DL, Pritchard JB, Thakker DR (2005) Differential substrate and inhibitory activities of ranitidine and famotidine toward human organic cation transporter 1 (hOCT1; SLC22A1), hOCT2 (SLC22A2), and hOCT3 (SLC22A3). J Pharmacol Exp Ther 315(3):1288–1297
Bow DA, Perry JL, Miller DS, Pritchard JB, Brouwer KLR (2008) Localization of P-gp (Abcb1) and Mrp2 (Abcc2) in freshly isolated rat hepatocytes. Drug Metab Dispos 36(1):198–202
Boyer JL (1997) Isolated hepatocyte couplets and bile duct units—novel preparations for the in vitro study of bile secretory function. Cell Biol Toxicol 13(4–5):289–300
Boyer JL et al (2006) Upregulation of a basolateral FXR-dependent bile acid efflux transporter OSTalpha-OSTbeta in cholestasis in humans and rodents. Am J Physiol Gastrointest Liver Physiol 290(6):G1124–G1130
Briz O et al (2006) OATP8/1B3-mediated cotransport of bile acids and glutathione: an export pathway for organic anions from hepatocytes? J Biol Chem 281(41):30326–30335
Brune K, Nuernberg B, Schneider HT (1993) Biliary elimination of aspirin after oral and intravenous administration in patients. Agents Actions Suppl 44:51–57
Campbell SD, de Morais SM, Xu JJ (2004) Inhibition of human organic anion transporting polypeptide OATP 1B1 as a mechanism of drug-induced hyperbilirubinemia. Chem Biol Interact 150(2):179–187
Coleman R et al (1995) Hepatobiliary function and toxicity in vitro using isolated hepatocyte couplets. Gen Pharmacol 26(7):1445–1453
Cui Y, Konig J, Keppler D (2001) Vectorial transport by double-transfected cells expressing the human uptake transporter SLC21A8 and the apical export pump ABCC2. Mol Pharmacol 60(5):934–943
Cvetkovic M et al (1999) OATP and P-glycoprotein transporters mediate the cellular uptake and excretion of fexofenadine. Drug Metab Dispos 27(8):866–871
De Bruyn T et al (2011) Determination of OATP-, NTCP- and OCT-mediated substrate uptake activities in individual and pooled batches of cryopreserved human hepatocytes. Eur J Pharm Sci 43(4):297–307
Fahrmayr C et al (2012) Identification of drugs and drug metabolites as substrates of MRP2 using triple-transfected MDCK-OATP1B1-UGT1A1-MRP2 cells. Br J Pharmacol 165(6):1836–1847
Fischer WJ et al (2005) Organic anion transporting polypeptides expressed in liver and brain mediate uptake of microcystin. Toxicol Appl Pharmacol 203(3):257–263
Floren LC et al (1997) Tacrolimus oral bioavailability doubles with coadministration of ketoconazole. Clin Pharmacol Ther 62(1):41–49
Fromm MF et al (1999) Inhibition of P-glycoprotein-mediated drug transport: a unifying mechanism to explain the interaction between digoxin and quinidine [see comments]. Circulation 99(4):552–557
Fukuda H et al (2008) Effect of plasma protein binding on in vitro-in vivo correlation of biliary excretion of drugs evaluated by sandwich-cultured rat hepatocytes. Drug Metab Dispos 36(7):1275–1282
Galatola G et al (1991) Direct measurement of first-pass ileal clearance of a bile acid in humans. Gastroenterology 100(4):1100–1105
Gerloff T et al (1999) Differential expression of basolateral and canalicular organic anion transporters during regeneration of rat liver. Gastroenterology 117(6):1408–1415
Germann UA et al (1990) Expression of the human multidrug transporter in insect cells by a recombinant baculovirus. Biochemistry 29(9):2295–2303
Ghibellini G et al (2004) A novel method for the determination of biliary clearance in humans. AAPS J 6(4):e33
Ghibellini G et al (2006) Determination of the biliary excretion of piperacillin in humans using a novel method. Br J Clin Pharmacol 62(3):304–308
Ghibellini G et al (2007) In vitro-in vivo correlation of hepatobiliary drug clearance in humans. Clin Pharmacol Ther 81(3):406–413
Gomes CM et al (2009) P-glycoprotein versus MRP1 on transport kinetics of cationic lipophilic substrates: a comparative study using [99mTc]sestamibi and [99mTc]tetrofosmin. Cancer Biother Radiopharm 24(2):215–227
Gorboulev V et al (1997) Cloning and characterization of two human polyspecific organic cation transporters. DNA Cell Biol 16(7):871–881
Grube M et al (2006) Modification of OATP2B1-mediated transport by steroid hormones. Mol Pharmacol 70(5):1735–1741
Grundemann D et al (1998) Molecular identification of the corticosterone-sensitive extraneuronal catecholamine transporter. Nat Neurosci 1(5):349–351
Grundemann D et al (1999) Selective substrates for non-neuronal monoamine transporters. Mol Pharmacol 56(1):1–10
Grundemann D et al (2003) Agmatine is efficiently transported by non-neuronal monoamine transporters extraneuronal monoamine transporter (EMT) and organic cation transporter 2 (OCT2). J Pharmacol Exp Ther 304(2):810–817
Guhlmann A et al (1995) Noninvasive assessment of hepatobiliary and renal elimination of cysteinyl leukotrienes by positron emission tomography. Hepatology 21(6):1568–1575
Gundala S et al (2004) The hepatocellular bile acid transporter Ntcp facilitates uptake of the lethal mushroom toxin alpha-amanitin. Arch Toxicol 78(2):68–73
Hagenbuch B (2010) Drug uptake systems in liver and kidney: a historic perspective. Clin Pharmacol Ther 87(1):39–47
Hayer-Zillgen M, Bruss M, Bonisch H (2002) Expression and pharmacological profile of the human organic cation transporters hOCT1, hOCT2 and hOCT3. Br J Pharmacol 136(6):829–836
Hendrikse NH et al (2004) In vivo imaging of hepatobiliary transport function mediated by multidrug resistance associated protein and P-glycoprotein. Cancer Chemother Pharmacol 54(2):131–138
Hirano M et al (2004) Contribution of OATP2 (OATP1B1) and OATP8 (OATP1B3) to the hepatic uptake of pitavastatin in humans. J Pharmacol Exp Ther 311(1):139–146
Hirano M et al (2005) Bile salt export pump (BSEP/ABCB11) can transport a nonbile acid substrate, pravastatin. J Pharmacol Exp Ther 314(2):876–882
Hirohashi T, Suzuki H, Sugiyama Y (1999) Characterization of the transport properties of cloned rat multidrug resistance-associated protein 3 (MRP3). J Biol Chem 274(21):15181–15185
Hirouchi M et al (2009) Construction of triple-transfected cells [organic anion-transporting polypeptide (OATP) 1B1/multidrug resistance-associated protein (MRP) 2/MRP3 and OATP1B1/MRP2/MRP4] for analysis of the sinusoidal function of MRP3 and MRP4. Drug Metab Dispos 37(10):2103–2111
Ho RH et al (2006) Drug and bile acid transporters in rosuvastatin hepatic uptake: function, expression, and pharmacogenetics. Gastroenterology 130(6):1793–1806
Hoffmaster KA et al (2004a) P-glycoprotein expression, localization, and function in sandwich-cultured primary rat and human hepatocytes: relevance to the hepatobiliary disposition of a model opioid peptide. Pharm Res 21(7):1294–1302
Hoffmaster KA et al (2004) Hepatobiliary disposition of the metabolically stable opioid peptide [D-Pen2, D-Pen5]-enkephalin (DPDPE): pharmacokinetic consequences of the interplay between multiple transport systems. J Pharmacol Exp Ther 311(3):1203–1210
Houle R et al (2003) Retention of transporter activities in cryopreserved, isolated rat hepatocytes. Drug Metab Dispos 31(4):447–451
Ishizuka H et al (1999) Species differences in the transport activity for organic anions across the bile canalicular membrane. J Pharmacol Exp Ther 290(3):1324–1330
Ismair MG et al (2001) Hepatic uptake of cholecystokinin octapeptide by organic anion-transporting polypeptides OATP4 and OATP8 of rat and human liver. Gastroenterology 121(5):1185–1190
Janvilisri T et al (2003) Sterol transport by the human breast cancer resistance protein (ABCG2) expressed in Lactococcus lactis. J Biol Chem 278(23):20645–20651
Jedlitschky G et al (1997) ATP-dependent transport of bilirubin glucuronides by the multidrug resistance protein MRP1 and its hepatocyte canalicular isoform MRP2. Biochem J 327(pt 1):305–310
Juliano RL, Ling V (1976) A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim Biophys Acta 455(1):152–162
Kajosaari LI et al (2005) Cyclosporine markedly raises the plasma concentrations of repaglinide. Clin Pharmacol Ther 78(4):388–399
Kameyama Y et al (2005) Functional characterization of SLCO1B1 (OATP-C) variants, SLCO1B1*5, SLCO1B1*15 and SLCO1B1*15+C1007G, by using transient expression systems of HeLa and HEK293 cells. Pharmacogenet Genomics 15(7):513–522
Kawabata S et al (2001) Breast cancer resistance protein directly confers SN-38 resistance of lung cancer cells. Biochem Biophys Res Commun 280(5):1216–1223
Kawabe T et al (1999) Enhanced transport of anticancer agents and leukotriene C4 by the human canalicular multispecific organic anion transporter (cMOAT/MRP2). FEBS Lett 456(2):327–331
Keppler D (2011) Multidrug resistance proteins (MRPs, ABCCs): importance for pathophysiology and drug therapy. Handb Exp Pharmacol (201):299–323
Khamdang S et al (2002) Interactions of human organic anion transporters and human organic cation transporters with nonsteroidal anti-inflammatory drugs. J Pharmacol Exp Ther 303(2):534–539
Kim RB et al (1998) The drug transporter P-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest 101(2):289–294
Kobayashi Y et al (2005) Transport mechanism and substrate specificity of human organic anion transporter 2 (hOat2 [SLC22A7]). J Pharm Pharmacol 57(5):573–578
Köck K, Brouwer KLR (2012) A perspective on efflux transport proteins in the liver. Clin Pharmacol Ther 92(5):599–612
Koike K et al (1997) A canalicular multispecific organic anion transporter (cMOAT) antisense cDNA enhances drug sensitivity in human hepatic cancer cells. Cancer Res 57(24):5475–5479
Konig J et al (1999) Characterization of the human multidrug resistance protein isoform MRP3 localized to the basolateral hepatocyte membrane. Hepatology 29(4):1156–1163
Kopplow K et al (2005) Human hepatobiliary transport of organic anions analyzed by quadruple-transfected cells. Mol Pharmacol 68(4):1031–1038
Kouzuki H et al (1999) Contribution of organic anion transporting polypeptide to uptake of its possible substrates into rat hepatocytes. J Pharmacol Exp Ther 288(2):627–634
Kullak-Ublick GA et al (2000) Hepatic transport of bile salts. Semin Liver Dis 20(3):273–292
Kullak-Ublick GA et al (2001) Organic anion-transporting polypeptide B (OATP-B) and its functional comparison with three other OATPs of human liver. Gastroenterology 120(2):525–533
Kullak-Ublick GA, Stieger B, Meier PJ (2004) Enterohepatic bile salt transporters in normal physiology and liver disease. Gastroenterology 126(1):322–342
Lau YY et al (2002) Development of a novel in vitro model to predict hepatic clearance using fresh, cryopreserved, and sandwich-cultured hepatocytes. Drug Metab Dispos 30(12):1446–1454
Le Vee M et al (2006) Functional expression of sinusoidal and canalicular hepatic drug transporters in the differentiated human hepatoma HepaRG cell line. Eur J Pharm Sci 28(1–2):109–117
Leonhardt M et al (2010) Hepatic uptake of the magnetic resonance imaging contrast agent Gd-EOB-DTPA: role of human organic anion transporters. Drug Metab Dispos 38(7):1024–1028
Li L, Meier PJ, Ballatori N (2000) Oatp2 mediates bidirectional organic solute transport: a role for intracellular glutathione. Mol Pharmacol 58(2):335–340
Li N et al (2010) Improved extrapolation of hepatobiliary clearance from in vitro sandwich cultured rat hepatocytes through absolute quantification of hepatobiliary transporters. Mol Pharm 7(3):630–641
Liao M et al (2010) Inhibition of hepatic organic anion-transporting polypeptide by RNA interference in sandwich-cultured human hepatocytes: an in vitro model to assess transporter-mediated drug-drug interactions. Drug Metab Dispos 38(9):1612–1622
Link E et al (2008) SLCO1B1 variants and statin-induced myopathy—a genomewide study. N Engl J Med 359(8):789–799
Liu X et al (1999a) Biliary excretion in primary rat hepatocytes cultured in a collagen-sandwich configuration. Am J Physiol 277(1 pt 1):G12–G21
Liu X et al (1999b) Use of Ca2+ modulation to evaluate biliary excretion in sandwich-cultured rat hepatocytes. J Pharmacol Exp Ther 289(3):1592–1599
Liu X et al (1999c) Correlation of biliary excretion in sandwich-cultured rat hepatocytes and in vivo in rats. Drug Metab Dispos 27(6):637–644
Luker GD et al (1997) Modulation of the multidrug resistance P-glycoprotein: detection with technetium-99m-sestamibi in vivo. J Nucl Med 38(3):369–372
Maliepaard M et al (1999) Overexpression of the BCRP/MXR/ABCP gene in a topotecan-selected ovarian tumor cell line. Cancer Res 59(18):4559–4563
Marie JP et al (1992) In vitro effect of P-glycoprotein (P-gp) modulators on drug sensitivity of leukemic progenitors (CFU-L) in acute myelogenous leukemia (AML). Exp Hematol 20(5):565–568
Matsushima S et al (2005) Identification of the hepatic efflux transporters of organic anions using double-transfected Madin-Darby canine kidney II cells expressing human organic anion-transporting polypeptide 1B1 (OATP1B1)/multidrug resistance-associated protein 2, OATP1B1/multidrug resistance 1, and OATP1B1/breast cancer resistance protein. J Pharmacol Exp Ther 314(3):1059–1067
Meier PJ et al (1984) Structural and functional polarity of canalicular and basolateral plasma membrane vesicles isolated in high yield from rat liver. J Cell Biol 98(3):991–1000
Meier-Abt F, Faulstich H, Hagenbuch B (2004) Identification of phalloidin uptake systems of rat and human liver. Biochim Biophys Acta 1664(1):64–69
Milkiewicz P et al (2002) Pathobiology and experimental therapeutics in hepatocellular cholestasis: lessons from the hepatocyte couplet model. Clin Sci (Lond) 102(6):603–614
Muller J et al (2005) Drug specificity and intestinal membrane localization of human organic cation transporters (OCT). Biochem Pharmacol 70(12):1851–1860
Nakakariya M et al (2012) In vivo biliary clearance should be predicted by intrinsic biliary clearance in sandwich-cultured hepatocytes. Drug Metab Dispos 40(3):602–609
Narita M et al (2009) Expression of OATP1B3 determines uptake of Gd-EOB-DTPA in hepatocellular carcinoma. J Gastroenterol 44(7):793–798
Niemi M et al (2005) Polymorphic organic anion transporting polypeptide 1B1 is a major determinant of repaglinide pharmacokinetics. Clin Pharmacol Ther 77(6):468–478
Northfield TC, Hofmann AF (1975) Biliary lipid output during three meals and an overnight fast. I. Relationship to bile acid pool size and cholesterol saturation of bile in gallstone and control subjects. Gut 16(1):1–11
Nozawa T et al (2004) Involvement of organic anion transporting polypeptides in the transport of troglitazone sulfate: implications for understanding troglitazone hepatotoxicity. Drug Metab Dispos 32(3):291–294
Nozawa T et al (2005) Role of organic anion transporter OATP1B1 (OATP-C) in hepatic uptake of irinotecan and its active metabolite, 7-ethyl-10-hydroxycamptothecin: in vitro evidence and effect of single nucleotide polymorphisms. Drug Metab Dispos 33(3):434–439
Oude Elferink RP, Paulusma CC (2007) Function and pathophysiological importance of ABCB4 (MDR3 P-glycoprotein). Pflugers Arch 453(5):601–610
Ozvegy C et al (2001) Functional characterization of the human multidrug transporter, ABCG2, expressed in insect cells. Biochem Biophys Res Commun 285(1):111–117
Pal A et al (2007) Cholesterol potentiates ABCG2 activity in a heterologous expression system: improved in vitro model to study function of human ABCG2. J Pharmacol Exp Ther 321(3):1085–1094
Pascolo L et al (2001) Abc protein transport of MRI contrast agents in canalicular rat liver plasma vesicles and yeast vacuoles. Biochem Biophys Res Commun 282(1):60–66
Pauli-Magnus C et al (2000) Characterization of the major metabolites of verapamil as substrates and inhibitors of P-glycoprotein. J Pharmacol Exp Ther 293(2):376–382
Payen L et al (2000) Characterization and inhibition by a wide range of xenobiotics of organic anion excretion by primary human hepatocytes. Biochem Pharmacol 60(12):1967–1975
Pfeifer ND et al (2013) Effect of ritonavir on 99mTc-mebrofenin disposition in humans: a semi-PBPK modeling and in vitro approach to predict transporter-mediated DDIs. CPT pharmacomet syst pharmacol 2:e20
Polli JW et al (1999) Role of P-glycoprotein on the CNS disposition of amprenavir (141W94), an HIV protease inhibitor. Pharm Res 16(8):1206–1212
Rius M et al (2003) Cotransport of reduced glutathione with bile salts by MRP4 (ABCC4) localized to the basolateral hepatocyte membrane. Hepatology 38(2):374–384
Rosmorduc O et al (2003) ABCB4 gene mutation-associated cholelithiasis in adults. Gastroenterology 125(2):452–459
Sampath J et al (2002) Role of MRP4 and MRP5 in biology and chemotherapy. AAPS PharmSci 4(3):E14
Sandhu P et al (2005) Hepatic uptake of the novel antifungal agent caspofungin. Drug Metab Dispos 33(5):676–682
Sasaki M et al (2002) Transcellular transport of organic anions across a double-transfected Madin-Darby canine kidney II cell monolayer expressing both human organic anion-transporting polypeptide (OATP2/SLC21A6) and multidrug resistance-associated protein 2 (MRP2/ABCC2). J Biol Chem 277(8):6497–6503
Sasaki M et al (2004) Prediction of in vivo biliary clearance from the in vitro transcellular transport of organic anions across a double-transfected Madin-Darby canine kidney II monolayer expressing both rat organic anion transporting polypeptide 4 and multidrug resistance associated protein 2. Mol Pharmacol 66(3):450–459
Satlin LM, Amin V, Wolkoff AW (1997) Organic anion transporting polypeptide mediates organic anion/HCO3- exchange. J Biol Chem 272(42):26340–26345
Schuetz JD et al (1999) MRP4: a previously unidentified factor in resistance to nucleoside-based antiviral drugs. Nat Med 5(9):1048–1051
Shin HJ et al (2007) Novel liver-specific organic anion transporter OAT7 that operates the exchange of sulfate conjugates for short chain fatty acid butyrate. Hepatology 45(4):1046–1055
Shitara Y et al (2003a) Function of uptake transporters for taurocholate and estradiol 17beta-D-glucuronide in cryopreserved human hepatocytes. Drug Metab Pharmacokinet 18(1):33–41
Shitara Y et al (2003b) Inhibition of transporter-mediated hepatic uptake as a mechanism for drug-drug interaction between cerivastatin and cyclosporin A. J Pharmacol Exp Ther 304(2):610–616
Smith AJ et al (2000) MDR3 P-glycoprotein, a phosphatidylcholine translocase, transports several cytotoxic drugs and directly interacts with drugs as judged by interference with nucleotide trapping. J Biol Chem 275(31):23530–23539
Soldner A et al (1999) Grapefruit juice activates P-glycoprotein-mediated drug transport. Pharm Res 16(4):478–485
Song Z et al (2009) Efficient generation of hepatocyte-like cells from human induced pluripotent stem cells. Cell Res 19(11):1233–1242
Soroka CJ, Ballatori N, Boyer JL (2010) Organic solute transporter, OSTalpha-OSTbeta: its role in bile acid transport and cholestasis. Semin Liver Dis 30(2):178–185
Spahn-Langguth H et al (1998) P-glycoprotein transporters and the gastrointestinal tract: evaluation of the potential in vivo relevance of in vitro data employing talinolol as model compound. Int J Clin Pharmacol Ther 36(1):16–24
Stadalnik RC et al (1981) Clinical experience with 99mTc-disofenin as a cholescintigraphic agent. Radiology 140(3):797–800
Stieger B (2011) The role of the sodium-taurocholate cotransporting polypeptide (NTCP) and of the bile salt export pump (BSEP) in physiology and pathophysiology of bile formation. Handb Exp Pharmacol (201):205–259
Stieger B et al (2000) Drug- and estrogen-induced cholestasis through inhibition of the hepatocellular bile salt export pump (Bsep) of rat liver. Gastroenterology 118(2):422–430
Sun W et al (2001) Isolation of a family of organic anion transporters from human liver and kidney. Biochem Biophys Res Commun 283(2):417–422
Swift B, Pfeifer ND, Brouwer KLR (2010) Sandwich-cultured hepatocytes: an in vitro model to evaluate hepatobiliary transporter-based drug interactions and hepatotoxicity. Drug Metab Rev 42(3):446–471
Tahara H et al (2005) A species difference in the transport activities of H2 receptor antagonists by rat and human renal organic anion and cation transporters. J Pharmacol Exp Ther 315(1):337–345
Takashima T et al (2010) Positron emission tomography studies using (15R)-16-m-[11C]tolyl-17,18,19,20-tetranorisocarbacyclin methyl ester for the evaluation of hepatobiliary transport. J Pharmacol Exp Ther 335(2):314–323
Takeda M et al (2002) Human organic anion transporters and human organic cation transporters mediate renal antiviral transport. J Pharmacol Exp Ther 300(3):918–924
Tamai I et al (2000) Molecular identification and characterization of novel members of the human organic anion transporter (OATP) family. Biochem Biophys Res Commun 273(1):251–260
Thomas J et al (2004) Active transport of imatinib into and out of cells: implications for drug resistance. Blood 104(12):3739–3745
Tian X et al (2004) Modulation of multidrug resistance-associated protein 2 (Mrp2) and Mrp3 expression and function with small interfering RNA in sandwich-cultured rat hepatocytes. Mol Pharmacol 66(4):1004–1010
Tsuboyama T et al (2010) Hepatocellular carcinoma: hepatocyte-selective enhancement at gadoxetic acid-enhanced MR imaging—correlation with expression of sinusoidal and canalicular transporters and bile accumulation. Radiology 255(3):824–833
Tsujii H et al (1999) Exon-intron organization of the human multidrug-resistance protein 2 (MRP2) gene mutated in Dubin-Johnson syndrome. Gastroenterology 117(3):653–660
Ueda K et al (1992) Human P-glycoprotein transports cortisol, aldosterone, and dexamethasone, but not progesterone. J Biol Chem 267(34):24248–24252
van Montfoort JE et al (2001) Comparison of “type I” and “type II” organic cation transport by organic cation transporters and organic anion-transporting polypeptides. J Pharmacol Exp Ther 298(1):110–115
Verho M et al (1995) Pharmacokinetics, metabolism and biliary and urinary excretion of oral ramipril in man. Curr Med Res Opin 13(5):264–273
Wagner M, Zollner G, Trauner M (2009) New molecular insights into the mechanisms of cholestasis. J Hepatol 51(3):565–580
Wang R, Sheps JA, Ling V (2011) ABC transporters, bile acids, and inflammatory stress in liver cancer. Curr Pharm Biotechnol 12(4):636–646
Wu X et al (2000) Structure, function, and regional distribution of the organic cation transporter OCT3 in the kidney. Am J Physiol Renal Physiol 279(3):F449–F458
Xiong H et al (2000) Altered hepatobiliary disposition of acetaminophen glucuronide in isolated perfused livers from multidrug resistance-associated protein 2-deficient TR(−) rats. J Pharmacol Exp Ther 295(2):512–518
Yamaguchi H et al (2000) Secretory mechanisms of grepafloxacin and levofloxacin in the human intestinal cell line caco-2. J Pharmacol Exp Ther 295(1):360–366
Yue W, Abe K, Brouwer KLR (2009) Knocking down breast cancer resistance protein (Bcrp) by adenoviral vector-mediated RNA interference (RNAi) in sandwich-cultured rat hepatocytes: a novel tool to assess the contribution of Bcrp to drug biliary excretion. Mol Pharm 6(1):134–143
Zamek-Gliszczynski MJ et al (2005) Multiple mechanisms are involved in the biliary excretion of acetaminophen sulfate in the rat: role of Mrp2 and Bcrp1. Drug Metab Dispos 33(8):1158–1165
Zhang L et al (1999) The interaction of n-tetraalkylammonium compounds with a human organic cation transporter, hOCT1. J Pharmacol Exp Ther 288(3):1192–1198
Acknowledgements
The authors are grateful for the helpful advice of Drs. Hoffmaster and Swift in the preparation of this chapter. This work was supported, in part, by a grant from the National Institute of General Medical Sciences of the National Institutes of Health under award number R01 GM41935 [K.L.R.B] and the German Research Foundation under award number Ko4186/1-1 [K.K]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Yang, K., Köck, K., Brouwer, K.L.R. (2013). Analysis of Hepatic Transport Proteins. In: Sugiyama, Y., Steffansen, B. (eds) Transporters in Drug Development. AAPS Advances in the Pharmaceutical Sciences Series, vol 7. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-8229-1_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-8229-1_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-8228-4
Online ISBN: 978-1-4614-8229-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)