Abstract
Transgender people may wish to transition to the other sex, usually to the fullest extent possible. Part of that transition is enabled by the administration of cross-sex hormones and part by surgical adaptation. The treatment of male-to-female transgender people consists of blocking androgen action and allowing estrogens to feminize the body. For virilization of female-to-male transgender people, androgens usually suffice. In adulthood, certain features of the sex hormone-induced body shape cannot be undone (such as the larger size of bones in males, the hip configuration in females). After about 2–3 years, the maximally attainable effects of cross-sex hormones have been reached. With competent endocrinological advice, cross-sex hormone treatment is usually uneventful. The estrogen ethinyl estradiol is to be avoided in view of the risks of venous thrombosis and cardiovascular disease. Androgen administration does not lead to an increase in cardiovascular disease. Hormone-dependent cancers have been observed in transgender people but not to an alarming degree. The relative rarity of transsexualism and the scattering of endocrine treatment over many centers is an impediment to build a solid body of knowledge with regard to efficacy and safety of cross-sex hormone treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
As elsewhere elaborately described in this Festschrift, transsexualism is the condition in which a person with apparently normal somatic sexual differentiation is convinced that he or she is actually a member of the other sex and believes she/he is trapped in the wrong body. This conviction is accompanied by the irresistible urge to live in that self-experienced gender, with a body that is not only anatomically as close as possible to that of the other gender but also psychologically, socially, and legally. According to current scientific evidence, transsexualism is an unalterable condition. For the affected individual, it represents a source of chronic suffering and disability. In this contribution, the principles of hormonal treatment of transsexual people will be discussed.
The indication for cross-sex hormone treatment is the result of psychological assessment that concludes that sex reassignment will bring relief to an individual suffering from gender dysphoria, the extreme feeling often described as being “trapped in the wrong body.” Although endocrine treatment is recommended by a mental health professional, it is the prescribing physician who retains responsibility for the intervention and the quality of care. It is of utmost importance, then, that there is a close collaboration between the physician and the mental health professional. Sex reassignment (social, hormonal, surgical, and legal) is an ameliorative and rehabilitative treatment (Money, 1971). It is not a complete makeover of one’s life. The only benefit sex reassignment can confer is relief of gender dysphoria; all human problems outside the area of gender dysphoria will remain, though overall well-being usually improves. Persons may harbor unrealistic expectations of hormonal and surgical treatment for transitioning to the other gender that must be addressed. Also, the limitations of cross-sex hormone administration on sex-typical body features in adult, and certainly elderly transsexuals, should be frankly discussed. After years of silent suffering and loneliness, fantasy often supersedes reality. Contact with others who are already in the process of transition, or who have completed this process, can be quite helpful in shaping a person’s expectations of what can be reasonably achieved with hormonal and surgical treatment. Likewise, it will help the individual cope with the problems of transitioning (personal, professional, and social) that may arise, both initially and long term.
1.1 Cross-Sex Hormone Treatment
The administration of cross-sex hormones to transsexuals is, from the viewpoint of endocrinology, unorthodox. Therefore, cross-sex hormone treatment has for a long time met with reservation in professional medical circles, though acceptance is growing rapidly. Major textbooks such as Endocrinology (editors De Groot & Jameson, 2010), The Oxford Textbook of Endocrinology and Diabetes, and Andrology for the Clinician (editors Wass & Shalet, 2011) now each have a chapter dealing with the issue of transsexual medicine.
The indication for hormone use is not based on standard technical endocrine grounds familiar to the endocrinologist, such as a deficiency or excess of hormone action. The endocrinological treatment was and is not standardized, and each attending endocrinologist has devised her/his own treatment schemes, usually based on principles of treating subjects with sex hormone deficiencies but now applied to the other sex. Both males and females have measurable levels of androgens and estrogens. In females, administration of testosterone is usually sufficient to induce virilization. In males, the high levels of testosterone block the biological actions of circulating estrogens, and in order to arrive at efficacious estrogen treatment, blood testosterone levels have to be suppressed or blocked in their biological action to almost nil.
The first reports detailing cross-sex hormone treatment of transsexuals appeared 40–50 years ago (Benjamin, 1966; Hamburger, 1969; Migeon, Rivarola, & Forest, 1968). In 1981, Meyer et al., (1981) published a survey of transsexual hormonal treatment in 20 gender-treatment centers and concluded:
“No systematic study has been published of the effects of hormonal therapy in the transsexual; specifically, its effect on physical changes, its suppression of endogenous hormones, or its side effects. With the growing number of transsexual treatment centers, it seemed timely to survey these programs and attempt to determine if a standard hormonal treatment exists. Twenty centers for transsexual treatment responded to a survey concerning their current hormonal treatment plan before and after removal of the gonads as sources of sex hormones. At least nine different male-to-female transsexual therapy programs and 11 different female-to-male transsexual testosterone therapy programs were reported. The typical program utilized, for male-to-female transsexuals, 2.5–5.0 mg/day of conjugated estrogen and, for female-to-male transsexuals, 200–400 mg of intramuscular long-acting conjugates of testosterone once a month. However, less than half of the centers are in agreement and the great diversity of therapies highlights the need for systematic studies of the effects of hormonal therapy to determine the optimal program for transsexuals.”
In 2009, a task force of The Endocrine Society formulated guidelines for the endocrine treatment of transsexual people (Hembree et al., 2009), which is a major step forward. The guidelines specified dosage schemes of hormones, contraindications, recommendations for clinical follow-up, and warnings for short- and long-term side effects. The presently available knowledge about cross-sex hormone treatment did not allow evidence-based recommendations. The guidelines are based on clinical experience and general expertise in the area of sex hormone treatment (Wierckx, Mueller, et al., 2012; Wierckx, Stuyver, et al., 2012; Wierckx, Van Caenegem, et al., 2012).
1.2 General Aspects of Cross-Sex Hormone Treatment
Hormonal reassignment of adult persons has two aims: (1) to eliminate to the best degree possible the hormonally induced secondary sex characteristics of the natal sex and (2) to induce those of the new sex to the fullest extent possible. Secondary sex characteristics are contingent upon sex steroids. There is no known fundamental difference in sensitivity to the biological action of sex steroids on the basis of genetic configurations or gonadal status. Adult transsexuals undergoing sex reassignment have the disadvantage that, at that advanced age, a normal average degree of hormonal somatic masculinization or feminization has already irreversibly taken place. Unfortunately, the elimination of the hormonally induced sex characteristics of the natal sex is, therefore, rarely complete. In male-to-female transsexuals, the previous effects of androgens on the skeleton (the average greater height than women; the size and shape of the hand, feet, jaws, and male-type pelvis) cannot be reversed. Conversely, the relatively lower height of female-to-male transsexuals compared to men and the broader hip configuration will not change under androgen treatment. These features show a degree of overlap between the sexes, so, in some transsexuals, characteristics of the natal sex will be more visible than in others. Also, race is a significant determinant of sex differences in body configuration in adulthood, and, generally speaking, Asians transition physically more smoothly to the other sex than Caucasians, since Asians do have less pronounced secondary sex characteristics than Caucasians.
1.3 Male-to-Female Transsexual Subjects
For male-to-female transsexuals, elimination of sexual hair growth and induction of breast formation are essential. To attain both, an almost complete reduction of the effects of androgens is required. Administration of estrogens alone will suppress gonadotropin output and, consequently, androgen production, but dual therapy with one compound suppressing androgen action and another introducing estrogen is probably more effective. Several agents are available to inhibit androgen action. In Europe, the most widely used drug is cyproterone acetate (50–100 mg/day), a progestational compound with antiandrogenic properties. If not available, medroxyprogesterone acetate (5–10 mg/day), probably somewhat less effective, is an alternative. Nonsteroidal antiandrogens, such as flutamide (50–75 mg/day) and nilutamide (150 mg/day), are also used, but they increase gonadotropin output with a rise of testosterone and estradiol; the rise of estradiol is a desirable effect in this context. Spironolactone, a diuretic with antiandrogenic properties, widely used in the USA, has androgen receptor-blocking properties and also decreases testosterone production. Also luteinizing hormone-releasing hormone (LHRH) agonists, blocking LHRH receptors on the pituitary and decreasing LH production and therewith testosterone production, can be used as monthly injections. Finasteride 1 mg, which inhibits the conversion of testosterone to the much more biopotent 5α-dihydrotestosterone, now marketed for alopecia androgenetica (male-type hair loss), might also be considered.
There are a wide range of estrogens to choose from. Oral ethinyl estradiol (50–100 μg/day), the estrogen used in oral contraceptives, is a potent and cheap estrogen. It may increase the risk of venous thrombosis, particularly in subjects over 40 years (Toorians et al., 2003), and is associated with a threefold increase in cardiovascular mortality (Asscheman et al., 2011) and should therefore be avoided. Transdermal estrogens (100 μg 17β-estradiol/day) as a patch twice a week or oral estradiol esters (2–4 mg/day) are preferred. They are, however, less potent than ethinyl estradiol. Many transsexuals favor injectable estrogens; however, they generate high levels of circulating estrogens, with possible disadvantages, and they carry a higher risk of overdosing, which some transsexuals do.
As to the effects of this dual regimen of antiandrogens and estrogens, adult male beard growth is very resilient to the described hormonal intervention, and in Caucasian subjects additional measures (electrolysis, photothermolysis, laser light treatment) to eliminate facial hair are almost always necessary. Postpubertal sexual hair growth on other parts of the body responds more favorably, usually only waxing is required. Removal of sexual hair growth on the male genital structures, serving as tissue for the construction of female genitalia (vaginoplasty) by plastic surgery, may require additional measures, such as laser treatment. Breast formation starts almost immediately after initiation of cross-sex hormone administration and goes through periods of growth and standstill. Clinical experience shows that after 2 years of hormone administration, no further development can be expected. It is quantitatively satisfactory in 40–50 % of the subjects; the remaining 50–60 % judge their breast formation as insufficient. The attained size, only in 35 % cup B, is often disproportional to the existing male dimensions of the chest and height, and surgical breast augmentation may be desired. In the remaining 65 %, breast development is lower. Higher age may also impede full breast formation, though data are not very solid. Androgen deprivation leads to decreased activity of the sebaceous glands which may result in dry skin or brittle nails. There is an increase in subcutaneous fat deposits, and, following androgen deprivation, there is a loss of approximately 4 kg of lean body mass, but most of the time body weight increases. Testes, lacking gonadotropic stimulation, will become atrophic and may enter the inguinal canal which may cause discomfort.
After reassignment surgery, including orchiectomy, hormone therapy must be continued. Some subjects still experience an increased growth of male type of sexual hair, and antiandrogens appear to be effective, though their dose may be reduced compared to presurgery. Continuous estrogen therapy is required to avoid symptoms of hormone deprivation, most importantly, to prevent osteoporosis.
1.4 Female-to-Male Transsexuals
Androgen administration may decrease glandular activity of the breasts, but it usually does not reduce their size. The objectives of androgen administration are to stop menstrual activities, experienced as improper, and to induce a male pattern of sexual hair and male physical contours. Usually, this can be attained with administration of injections of testosterone enanthate or cypionate at a dose of 200–250 mg per 2 weeks or of late testosterone undecanoate 1,000 mg per 12 weeks. Occasionally, menstrual bleeding does not cease upon this regimen, and addition of a progestational agent is necessary. If other types of androgens are used (oral or transdermal), addition of a progestational agent is nearly always needed. The development of sexual hair essentially follows the pattern observed in pubertal boys: first the upper lip, then chin, then cheeks, etc. The degree of hairiness can usually be predicted from the degree and pattern in male members of the same family. The same applies to the occurrence of male pattern baldness. Deepening of the voice already occurs after 8–10 weeks of androgen administration and is irreversible. Androgen administration leads to a reduction of subcutaneous fat but increases abdominal fat storage. The increase in lean body mass, as a result of the muscle-promoting effects of androgens, amounts to 4 kg, but the increase in body weight is usually greater. Side effects are minor. In approximately 40 %, acne is observed, predominantly on the back, as is also the case in hypogonadal men starting androgen treatment past the age of normal puberty. Clitoral enlargement occurs in all, but to a varying degree; in a small number of subjects, the size becomes sufficient for vaginal intercourse with a partner. Most subjects will note an increase in libido. The ovaries show changes which are indistinguishable from polycystic ovaries. After surgical sex reassignment, including ovariectomy, androgen therapy must be continued to prevent symptoms of hormone deprivation, such as osteoporosis.
2 Concerns of Cross-Sex Hormone Administration
2.1 Bone Health
The evidence that adequate serum levels of sex steroids are required for formation of adult bone mass in the pubertal years and maintenance of bone mineral density in adulthood is overwhelming. Postmenopausal women, subjects with sex steroid deficiencies like Turner syndrome in women, Klinefelter syndrome in men, and prostate cancer patients treated with androgen deprivation treatment testify to the above. Therefore, bone health in people undergoing sex reassignment deserves attention. Since loss of bone mass (osteopenia/osteoporosis) is often perceived as a disease of women, there was a concern that FtM subjects receiving testosterone treatment would be at risk of developing loss of bone mineral density and, as a result, bone fractures. However, studies have indicated that testosterone administered in adequate doses is capable of maintaining bone mass in FtM persons (Turner et al., 2004; van Kesteren et al., 1996; van Kesteren, Lips, Gooren, Asscheman, & Megens, 1998). The protective effect of testosterone is likely, at least in part, mediated by peripheral conversion to estradiol both systemically and locally in the bone. But testosterone itself also has anabolic effects on bone mineral density, as demonstrated by a recent study. This study found larger radial cortical bone size and lower cortical volumetric bone mineral density at the radius and tibia in FtM subjects on testosterone therapy, compared to women (Van Caenegem et al., 2012). With regard to MtF persons, the question was whether estrogens-only were capable of maintaining bone mineral density. It was reassuring that studies in natal males suggest that serum estradiol more positively correlates with bone mineral density than testosterone and is more important for peak bone mass (Khosla, 2010). Studies have shown that estrogen adequately preserves bone mineral density in MtF persons who continue on estrogen and antiandrogen therapies (Mueller et al., 2005; Ruetsche, Kneubuehl, Birkhaeuser, & Lippuner, 2005), but a later study expressed some concern (T’Sjoen et al., 2009).
A very significant finding was that the adequacy of dosing of cross-sex hormone treatment can be estimated from serum levels of luteinizing hormone. The latter hormone, of which the levels are suppressed by the amounts of circulating sex steroids, should be in the range of eugonadal subjects (Turner et al., 2004; van Kesteren et al., 1998). Transsexual persons who discontinue cross-sex hormones are at risk of developing osteoporosis (van Kesteren et al., 1996). Transsexual subjects with risk factors for osteoporosis should be more intensively followed up. In the absence of specific recommendations for transsexual people, the guidelines for the general population may be used (Ballantyne, Kayser, & Grootegoed, 2011; Watts et al., 2012).
2.2 Venous Thromboembolic Disease
A major side effect of cross-sex hormone treatment in MtF subjects is the increased risk of venous thromboembolism (VTE). Thrombotic events in MtF subjects on estrogen therapy such as pulmonary embolism and cerebral thrombosis have been reported from early on. In 1989, the VU university gender identity clinic reported a 45-fold increase in the incidence of VTE among 303 MtF subjects treated with oral ethinyl estradiol 0.1 mg/day + cyproterone acetate 100 mg/day compared to nonusers (Asscheman, Gooren, & Eklund, 1989). In the subjects of this study, no other known risk factors, such as surgery or immobilization, were found in 13 out of the 19 cases of VTE. The risk appeared clearly associated with age (2.1 % <40 years and 12 % >40 years of age). In a second study with a larger number of MtF subjects (n = 816) and longer follow-up (mean 9.5 years), drawing lessons from the earlier study, incidence of VTE had become lower after the introduction of transdermal estrogen as standard therapy in all MtF subjects >40 years of age, but the VTE incidence was still 20-fold increased (n = 45), and 36 VTE events (35 on ethinyl estradiol, 1 on transdermal estradiol) occurred in the absence of other known risk factors (van Kesteren, Asscheman, Megens, & Gooren, 1997). Remarkably, in both studies, the majority of VTE cases were diagnosed in the first year of estrogen treatment. Postoperative VTE prevalence was 1.7 % in the 1989 study (Asscheman et al., 1989) and <1.0 % in the 1997 study (van Kesteren et al., 1997), probably due to the introduction of postoperative thrombosis prevention with low molecular weight heparin for all surgery in the 1980s. In a third study of the VU university gender identity clinic, it could be demonstrated that oral ethinyl estradiol 0.1 mg/day combined with cyproterone acetate 100 mg/day caused a large increase in activated protein C (APC) resistance (nAPCsr increased from 1.2 ± 0.8 to 4.1 ± 1.1), thus increasing the risk of thrombosis, but transdermal estradiol 100 μg patch 2×/week + cyproterone acetate 100 mg/day or cyproterone acetate alone had only a small effect on APC resistance (1.3 ± 0.6 to 2.0 ± 2.0 and 1.4 ± 0.6 to 1.8 ± 0.9, respectively). Moreover, ethinyl estradiol + cyproterone acetate also decreased protein S levels, an inhibitor of coagulation. In a group of 20 subjects on oral estradiol-17β 4 mg/day + cyproterone acetate 100 mg/day, APC resistance was not different from the values on oral cyproterone acetate, with or without transdermal estradiol. It was concluded that the prothrombotic effect of ethinyl estradiol is due to its molecular structure rather than to the first-pass liver effect which ethinyl estradiol shares with all oral estrogens (Toorians et al., 2003).
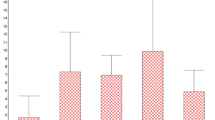
A recent literature search in PubMed resulted in nine papers that mentioned VTE as a complication of cross-sex hormone treatment mainly with estrogen-only treatment and reported on numbers and period of follow-up in estrogen-treated MtF subjects. We found only two studies with a relatively large number of user-years, the one from Amsterdam 1997 (van Kesteren et al., 1997) [which is an extension of the 1989 study (Asscheman et al., 1989) as described above and a study from Vienna (Ott, Kaufmann, Bentz, Huber, & Tempfer, 2010)]. All other studies had small numbers of user-years and few thromboembolic events resulting in very wide confidence intervals, precluding firm conclusions about the VTE risk in these populations.
In 2010, we sent questionnaires to nine European Gender Centers that treat large numbers of MtF people. These questionnaires enquired about the number of confirmed cases of VTE in MtF subjects treated with cross-sex hormone treatment and about the type of cross-sex hormone treatment. Cases of VTE had been diagnosed in all centers. Prevalence rates of any VTE during the whole follow-up period varied from 0.3 to 3.5 % of MtF subjects treated with cross-sex hormone therapy per center. Incidence rates of VTE varied from 4.8 to 35.7 per 10,000 user-years. The summary statistics with the random effects model yielded a weighted mean incidence rate of 13 per 10,000 user-years (95 %CI, 4–22), much higher than among users of oral contraceptives.
Remarkably, at least four VTE events out of 21 occurred in MtF subjects on oral contraceptives containing ethinyl estradiol + cyproterone acetate (19 %), three on transdermal estradiol with cyproterone acetate, four on oral estradiol (one on 2 mg/day, one on 4 mg/day after immobilization, and two on the high dose of 6 mg/day), and one on conjugated estrogens 0.625 mg/day (rarely used in Europe). In six cases, the type of hormone treatment at the time of the thrombotic event could not be assessed, but use of oral contraceptives was probable in four. Presuming the last four did use oral contraceptives, this would imply that ethinyl estradiol was the main culprit in eight (38 %) of the 21 confirmed events of VTE, but, of course, the latter presumption cannot be confirmed.
Postoperative VTE was rarely reported in our questionnaire, but many clinics had data on less than 100 cases of sex reassignment surgery (SRS) and all used low molecular weight heparin thrombosis prophylaxis during about 30 days postoperatively.
It was concluded that prevalence and incidence rates of VTE in estrogen-treated MtF persons have decreased considerably but are still elevated compared to the general population and also compared to women using oral contraceptives and estrogen replacement treatment (6–8/10,000 user-years). The data allowed some recommendations to be made: The use of ethinyl estradiol (and ethinyl estradiol containing oral contraceptives) is to be avoided. Use of transdermal patches or gel (the latter carries some risk of overdosing) or low to intermediate doses of oral estradiol (2–4 mg/day) or conjugated equine estrogens (up to 2.5 mg/day) is recommended. Cross-sex hormones should probably be discontinued before elective surgery for at least 2 weeks and resumed after 3 weeks and full mobilization.
2.3 Metabolic Aspects of Cross-Sex Hormone Administration and Cardiovascular Health
Cardiovascular disease is more common in males and the risk in women increases only after menopause with its cessation of estrogen production. The skewed sex ratio in cardiovascular disease has been interpreted to indicate that estrogens are cardioprotective and that androgens might increase cardiovascular disease. However, the large randomized trials (Heart and Estrogen/Progestin Replacement Study (HERS) and the Women’s Health Initiative) have refuted the protective effect of exogenous estrogens in women (Grady & Barrett-Connor, 2007). Cross-sex hormone administration in both MtF and FtM persons both improves and impairs profiles of cardiovascular risk factors. It remains difficult to determine how much weight should be attributed to these alterations in risk factors and whether these changes are of clinical significance. With these reservations in mind, the overall impression is that inducing androgen deprivation and an estrogen milieu in MtF subjects has a larger deleterious effect on risk factors than inducing an androgenic milieu in FtM subjects (Gooren & Giltay, 2008; Gooren, Giltay, & Bunck, 2008).
Data on clinical endpoints from the morbidity and mortality study in 1997 (van Kesteren et al., 1997) showed no elevated (cardiovascular) morbidity and/or mortality in the cohort of transsexuals treated at the Amsterdam clinic. More recently, two cohort studies on mortality in hormone-treated MtF persons with much longer follow-up reported an increased cardiovascular mortality. In the Amsterdam cohort, standardized mortality from ischemic heart disease was clearly increased (SMR 1.64) and associated with ethinyl estradiol use, more smoking, and hyperlipemia (Asscheman et al., 2011). In androgen-treated FtM subjects, no increased cardiovascular mortality was observed. In a Swedish cohort, the hazard ratio of cardiovascular death was 2.5 (Dhejne et al., 2011).
To reduce the risk of cardiovascular death, use of ethinyl estradiol should be avoided, and, for all transsexual persons’ lifestyle behaviors, healthy diets, smoking cessation, and regular exercise are recommended.
2.4 Partial Sex Reassignment
The World Professional Association for Transgender Health (WPATH) has updated the Standards of Care (SOC) (7th edition, July 2012) (www.wpath.org/documents). The overall goal of the SOC is to provide clinical guidance for health professionals to assist transsexual, transgender, and gender nonconforming people with safe and effective pathways to achieving lasting personal comfort with their gendered selves, in order to maximize their overall health, psychological well-being, and self-fulfillment. The scope of SOC has widened to those subjects who need and wish only partial sex reassignment treatment, which may consist of blocking the action of sex hormones of their natal sex (with hormone-blocking agents or surgery) without using cross-sex hormones. Endocrinologically speaking, a functional status of hypogonadism is induced. Prominent symptoms to arise are loss of bone mass (osteopenia, osteoporosis), loss of muscle mass, obesity, and lipid disorders increasing cardiovascular risks. These interventions must not be undertaken without medical supervision to mitigate the consequences of the induced hypogonadism. In particular, the group seeking limited adaptation to the other sex may fall outside the established categories in gender identity clinics and may be inclined to self-medicate.
2.5 Illicit Use of Cross-Sex Hormones
It is not rare that transgender individuals face harassment, discrimination, and rejection, not only in society but also in the medical system. Lack of awareness, knowledge, and sensitivity in healthcare communities eventually leads to inadequate access to, underutilization of, and disparities within the healthcare system for this population. The Institute of Medicine has published a book detailing the health needs of, among others, transgender people (Institute of Medicine, 2011), highlighting the significance of minority stress on health. Transgendered individuals may be frustrated with the standards of care that most recognized gender identity clinics observe, and there may be long delays before cross-sex hormone treatment is actually initiated. There may be financial barriers to undergo treatment in these centers. It is, therefore, not rare that transsexuals self-medicate with cross-sex hormones. Cross-sex hormones are affordable and relatively easily obtainable from peers or from the Internet. Many individuals in these situations receive advice on the use of hormones from peer groups. There is little documentation of illicit use of cross-sex hormones. In one Spanish study, there were several medical side effects that needed medical interventions (Becerra Fernandez, De Luis Roman, & Piedrola Maroto, 1999). Another study from Thailand found that about 50 % of subjects use hormones in overdose (Gooren, Sungkaew, & Giltay, 2012).
2.6 Tumors in Transsexuals Receiving Cross-Sex Hormones
A large number of transsexuals receive cross-sex hormone treatment from a relatively young age, and over their lifetime, they are exposed to cross-sex hormones for several decades. The dose taken is most of the times higher than the standard sex hormone replacement treatment in hypogonadal people. There is no evidence that men and women differ in sensitivity to the hormone action of sex steroids. Relationships exist between exposure to sex hormones and tumors of the reproductive organs, but a number of other tumors of nonreproductive organs appear to be sensitive to the action of sex steroids also. These tumors and the organs from which they originate sometimes have receptors for sex steroids. Examples are tumors of the lung (adenocarcinoma, small cell carcinoma) (Dougherty et al., 2006), of the colon (Slattery et al., 2006), of the bladder (but the latter mainly in animal models), and of the brain, particularly meningiomas (Wigertz et al., 2006).
After a successful transition to the new sex, transsexuals may not always be forthright with physicians about their past sex change, and this can lead to delays in diagnosing cancers of organs specific to the former sex. Hormone-dependent tumors appear to be rare in transsexual persons, but there may be an increase in the future. Aging may be a factor in their development, and, also, the increasingly longer duration of sex hormone administration in people having undergone sex reassignment at a young age may lead to an increase of tumors in the near future. It is difficult to reliably assess the prevalence of tumors in transsexuals. As indicated above, these tumors are relatively rare, as is transsexualism. Establishing a (potentially causal) relationship would require case–control analyses in large population cohort studies. For a review on tumors in transsexual persons receiving cross-sex hormones, see Mueller & Gooren, 2008.
In most European countries, transsexual persons receive surgical sex reassignment usually 18–36 months after start of cross-sex hormone treatment, thanks to the fact that surgical sex reassignment is covered by their health insurance. But in other parts of the world, including the USA, this may not be the case. There is no documentation of complications arising from this situation, but on the basis of insights into the pathogenesis of certain malignancies, some concern seems to be justified.
2.6.1 Tumors in Male-to-Female Transsexual Subjects
-
Lactotroph adenoma of the pituitary gland (prolactinoma)
There are several reports on prolactinomas in transsexual people in the literature. Initially, the impression was given that they occurred following very high dosages of estrogens (Gooren, Assies, Asscheman, de Slegte, & van Kessel, 1988; Kovacs, Stefaneanu, Ezzat, & Smyth, 1994; Serri, Noiseux, Robert, & Hardy, 1996), but later reports document that this need not be the case (Garcia-Malpartida, Martin-Gorgojo, Rocha, Gomez-Balaguer, & Hernandez-Mijares, 2010). Prolactinomas may present themselves after long-term estrogen administration, stressing the importance of prolactin levels being checked over the long term, be it with low frequency (Bunck et al., 2009). Hearsay suggests that prolactinomas may be more prevalent than have been reported.
-
Breast cancer
Breast cancer has been reported in six cases (Ganly & Taylor, 1995; Pritchard, Pankowsky, Crowe, & Abdul-Karim, 1988; Symmers, 1968). It is remarkable that these cases occurred more than 15 years ago, but there are also more recent cases (Dhand & Dhaliwal, 2010; Grabellus et al., 2005). The number of transsexual people receiving cross-sex hormones has increased substantially; however, there remains a relative paucity of breast cancer in MtF subjects, which may have a parallel with sufferers of Turner’s syndrome who are receiving estrogen treatment; the risk of breast cancer in these subjects is also very low (Schoemaker, Swerdlow, Higgins, Wright, & Jacobs, 2008).
-
Prostate cancer
Against expectations, prostate carcinoma was found in five cases of MtF subjects receiving estrogen treatment. In three cases, cross-sex hormone treatment only started after the age of 50 years, and the carcinoma may already have been present without generating clinical complaints (Dorff, Shazer, Nepomuceno, & Tucker, 2007; Thurston, 1994; van Haarst, Newling, Gooren, Asscheman, & Prenger, 1998). In two other subjects, this appeared not to be the case, however (Miksad et al., 2006; Molokwu, Appelbaum, & Miksad, 2008).
-
Meningioma
After the one case mentioned in the literature (Gazzeri, Galarza, & Gazzeri, 2007) occurring after 3 years of antiandrogen and estrogen treatment, two others have been reported. One in an MtF subject developed after initiation of hormone therapy (Deipolyi, Han, & Parsa, 2010), one that regressed after discontinuation of cyproterone acetate treatment (Cebula, Pham, Boyer, & Froelich, 2010).
2.6.2 Tumors in Female-to-Male Transsexual Subjects
-
Vaginal carcinoma
One case was reported 18 years after surgical sex reassignment treatment with partial removal of the vagina (Schenck et al., 2010).
-
Ovarian cancer
There have been three instances of this cancer (Dizon, Tejada-Berges, Koelliker, Steinhoff, & Granai, 2006; Hage, Dekker, Karim, Verheijen, & Bloemena, 2000). In testosterone-treated FtMs, the ovaries usually increase in volume and display characteristics of polycystic ovaries (Grynberg et al., 2010; Pache & Fauser, 1993). It is not certain whether these changes carry a higher risk for malignant development (Galazis, Olaleye, Haoula, Layfield, & Atiomo, 2012).
-
Endometrial cancer
Endometrial atrophy has been noted in 45 % of testosterone-treated FtMs (Grynberg et al., 2010). Although endometrial cancer has never been reported in FtMs, it could occur in those who have not undergone surgical sex reassignment, including hysterectomy. Administered testosterone is partially aromatized to estrogens, and estrogen action on the endometrium unopposed by progesterone increases the risk of cancer development. Addition of a progestin may be useful, though that may increase the risk of breast cancer (Ito, 2007) if the breasts have not been removed. The role of testosterone in the pathogenesis of endometrial cancer is not clear (Mueller & Gooren, 2008). A case of a preinvasive cervical carcinoma after performed hysterectomy has been reported (Driak & Samudovsky, 2004).
-
Breast carcinoma
In testosterone-treated FtMs, there is usually a marked reduction of glandular tissue and an increase of fibrous connective tissue (Slagter, Gooren, Scorilas, Petraki, & Diamandis, 2006). However, as previously indicated, administered testosterone is partially aromatized to estradiol, and this can be a risk factor for FtMs who have not undergone mastectomy. Two cases of breast cancers have been diagnosed in FtM persons who have been treated with supraphysiological doses of testosterone, suggesting the possible role of testosterone in the development of breast cancer (Shao, Grossbard, & Klein, 2011).
Even those who have undergone mastectomy may still retain some vulnerability, and one case of cancer has been reported in residual breast tissue 10 years after the breasts were removed (Burcombe, Makris, Pittam, & Finer, 2003). It appeared that there was a strong positive family history of breast cancer in this case. A recent study has also found an association between testosterone administration to FtMs and breast cancer-related gene expression signatures (Bentz et al., 2010). It is not yet clear what the role of testosterone is in the pathogenesis of breast cancer. It may certainly have a role, especially in postmenopausal women (Baglietto et al., 2010), though there is not yet general agreement on this (Dimitrakakis & Bondy, 2009).
3 Reproductive Health
When sex reassignment of transsexual people became a more accepted practice in medicine, it was almost axiomatic that, with the hormonal and surgical transition to the other sex, the procreative potential was irreversibly lost. This was “the price to pay” for becoming a member of the other sex (De Sutter, 2001).
Over the last two decades, there have been profound changes in the thinking about the ethics of reproduction, and it is now widely accepted that every person has the fundamental right to procreate. With regard to transsexual people, it has been argued that opting for the treatment they undergo, they forfeit the right to procreation. But the thinking about transsexualism has progressed, and it is now well understood that sex reassignment of transsexual people is not optional and is vital for their well-being. Presently, it is felt that transsexual individuals are in the same position as others whose procreative potential is jeopardized by their medical treatment, such as people with malignancies undergoing treatment with cytotoxic drugs or radiation. All these categories need to be counseled on the consequences of their medical interventions, and they must receive information on options to preserve their procreative potential, well before the interventions take place. For MtFs, this involves banking of spermatozoa and, for FtMs, the banking of oocytes, embryos, and ovarian tissue (Wierckx, Mueller, et al., 2012; Wierckx, Stuyver, et al., 2012; Wierckx, Van Caenegem, et al., 2012).
4 Transsexual People and Competitive Sports
After sex reassignment, transsexual people like to merge with the general population and lead the lives of ordinary men and women. Competition in sports may be part of that life. Sex segregation in competitive sports is regarded as fair. Boys and girls hardly differ before puberty in physique: Height, muscle, and bone mass are similar. In boys, exposure to testosterone during puberty produces an ultimate average greater height in men of 12–15 cm, larger bones, greater muscle mass, increased strength, and higher hemoglobin levels. Androgen ablation in postpubertal life reverses, at least in part, previous anabolic effects of testosterone on muscle (Mauras et al., 1998), bone mineral density, and hemoglobin, but the bones remain longer and have a wider diameter. It has been shown that treatment with testosterone produces a dose-dependent increase in muscle mass and maximal voluntary strength (Choong, Lakshman, & Bhasin, 2008; Storer et al., 2003), and therefore, sport organizations have banned androgens being performance-enhancing drugs (Handelsman & Heather, 2008). If men suffer from testosterone deficiency, testosterone replacements are permissible provided they do not raise blood testosterone levels above the normal male range (Gooren & Behre, 2008; Handelsman & Gooren, 2008).
Before the year 2000, genetic markers were used to determine sex for competition in sports. Chromosomal criteria of sex alone are not good indicators for differences in strength to ensure fair competition. In humans, there is no evidence that the pattern of sex chromosomes has a direct effect on muscle mass and strength. It is mainly testosterone that determines muscle mass and strength in a linear fashion. Therefore, in sports, exposure to androgens, previous and present, is a reasonable criterion for deducing unfair competition, not only between men and women but also between men.
Of late, sport organizations have addressed the issue of the participation in competitive sports of people with errors of sexual differentiation and particularly transsexual people who have been sex-reassigned. First of all, it is relevant, in view of the effects of testosterone, whether sex (re)assignment occurred before or after hormonal puberty. People who have had sex reassignment before puberty are still rare but their number will grow. Studies in the rat have shown that genetic configuration and gonadal status have no known significant effect on receptor-medicated actions of testosterone (Bentvelsen et al., 1995). During puberty, testosterone has a profound effect on bone and muscle mass and strength. Upon withdrawal of testosterone, the effects of testosterone are certainly in part reversible, but the precise extent is unknown (Gooren & Bunck, 2004). When muscle surface areas, measured by magnetic resonance imaging of male-to-female transsexuals and female-to-male transsexuals, were compared, there was a significant difference in the mean values, but there was also a considerable overlap between the two groups before any hormonal intervention had taken place. Androgen deprivation in MtF persons reduced muscle surface area, but still, after 1 year, the mean muscle surface area in male-to-female transsexuals remained significantly greater than in untreated female-to-male transsexuals; again, the two groups showed substantial overlap. As expected, testosterone administration to female-to-male transsexuals produced a significant increase in muscle surface areas. There was a large overlap with untreated male-to-female transsexuals, but the mean was significantly lower (Gooren & Bunck, 2004). Cross-sex hormones had effects on insulin-like growth factor and hemoglobin levels, both relevant for sports, in the same direction as the changes in muscle surface area.
It seems appropriate to place the effects of hormonal interventions in transsexuals in the perspective of naturally occurring differences in sporting capability between members of the same sex. While unfair competition should be prevented as much as possible, ultimately nature is unfair in her endowments of talents for all walks of life.
The International Olympic Committee (IOC) has drawn a necessarily arbitrary line which, based on present information, is reasonable with regard to participation of sex-reassigned transsexuals: Sex reassignment must have taken place at least 2 years earlier. In our aforementioned study, it could be shown that changes in muscle surface area were not greater after 3 years of cross-sex hormone administration than after 1 year (Gooren & Bunck, 2004). As is the case with hypogonadal men, doses of testosterone administered to female-to-male transsexuals must be in normal male range. Further, the reassigned sex must be legally recognized. The IOC policy is not binding for other sports organizations.
5 Thoughts About Past, Present, and Future of Cross-Sex Hormone Therapy
As indicated above, clinics offering cross-sex hormone treatment have largely developed their own treatment schedules, usually based on personal experience and personal insights into the workings of cross-sex hormones on persons of one sex wishing to transition to the other sex. It is not realistic to believe that the situation has greatly improved in 2012, although the guidelines of The Endocrine Society formulated by a panel of experts signify a step forward (Hembree et al., 2009). It is unrealistic to believe that studies with a rigorous design that can arrive at evidence-based guidelines can be performed. Second best are large cohort studies of hormone-treated transsexual people. Prospective studies with hormonal interventions based on treatment protocols and safety measurements would be desirable but are still in an early phase of development, and results are not expected for many years. Moreover, specific knowledge about effects of treatment in older subjects (>50 years of age) and long-term effects (>15 years of hormone use) or the risk of different hormone regimens will not be available in the near future. Retrospective cohort studies could bridge this gap: Transgender persons have been treated and followed up in multidisciplinary gender teams which have come into existence over the last 20 years. A number of them have published some of their results, but the comparatively low numbers of subjects relative to other conditions (with rough estimates of prevalence around 1:10,000 MtF persons and 1:25,000 FtM persons), different (hormonal) treatment protocols, and low number of exposure-years preclude firm conclusions. A strategy dubbed as “incremental validity” may be that of combining the existing data of those gender teams, a dataset with sufficient numbers of hormone-treated subjects with different hormonal regimens and longer follow-up time, resulting in a large number of treatment-years. Analysis of this dataset can ascertain the incidence of side effects and comorbidity by type of hormone therapy, period of follow-up (especially after more than 15 years of hormone use), age groups (in particular those over 50 years of age), and the relation with (cardiovascular) risk factors. The authors are involved in a study aiming to fill the gaps in knowledge about side effects, bone health, and cardiovascular risk factors which could be extended to other domains of health of people receiving cross-sex hormones.
Side effects in the short and medium term have been charted, and cross-sex hormone treatment seems acceptably safe (Asscheman et al., 2011; Gooren, 2011; Gooren et al., 2008; Gooren & Giltay, 2008; Hembree et al., 2009). There is no substantial information of long-term use of cross-sex hormones. The question is whether findings in natal men and women can reliably be extrapolated to the transsexual population. Elderly men with testosterone deficiency have a high risk of mortality due to, for instance, metabolic syndrome (Haring et al., 2009; Yeap, 2009; Yeap et al., 2009). Is the lesson that FtMs should continue testosterone until a very advanced age? Conversely, what should be the recommendation for aging MtF persons? The sudden decision by the National Heart, Lung, and Blood Institute of the National Institutes of Health to terminate the estrogen-progesterone therapy arm of the Women’s Health Initiative (WHI) study a decade ago gave rise to major concerns about safety (Grady & Barrett-Connor, 2007). They are, however, now pleased to reconsider this abrupt decision (Utian, 2012). A recent Cochrane review concluded that hormone therapy is not indicated for primary or secondary prevention of cardiovascular disease or dementia nor for preventing deterioration of cognitive function in postmenopausal women. Although hormone therapy is considered effective for the prevention of postmenopausal osteoporosis, it is generally recommended as an option only for women at significant risk, for whom non-estrogen therapies are unsuitable (Marjoribanks, Farquhar, Roberts, & Lethaby, 2012). With regard to MtF persons, careful follow-up should guide hormone treatment of aging MtF persons.
Most providers of cross-sex hormone treatment will agree that a substantial part of the transsexual population will act as shareholders with an activist attitude with regard to their treatment. It is probably an expression of the deep suffering these people have gone through and the big stakes they have in a better future life in the new sex. Naturally, this cannot be divorced from the profound changes patient–doctor relationships have undergone in the past decade. Doctors are not infallible and there should be no problem in publicly acknowledging this. Patients have access to medical information available on the Internet and may attribute greater significance to this information than warranted. The information is as reliable as those who put the information on the Internet, some of whom have an activist attitude that privileges personal opinion over scientific facts. It is regrettable and detrimental when the patient–doctor relationship becomes adversarial. An example is the use of progesterone-like drugs in the treatment of MtF persons. While progesterone is an essential hormone for reproductive functioning of women (preparing the uterus for implantation of the fertilized egg and the breasts for lactation, therefore a “female” hormone), it has, on the basis of present knowledge, no meaning for the feminization of MtF persons and may have detrimental effects on general health (Zitzmann, Erren, Kamischke, Simoni, & Nieschlag, 2005). Yet, it is not rare that MtF persons insist on taking the second female hormone, progesterone, in addition to estrogens.
References
Asscheman, H., Giltay, E. J., Megens, J. A., de Ronde, W. P., van Trotsenburg, M. A., & Gooren, L. J. (2011). A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. European Journal of Endocrinology, 164(4), 635–642.
Asscheman, H., Gooren, L. J., & Eklund, P. L. (1989). Mortality and morbidity in transsexual patients with cross-gender hormone treatment. Metabolism, 38(9), 869–873.
Baglietto, L., Severi, G., English, D. R., Krishnan, K., Hopper, J. L., McLean, C., et al. (2010). Circulating steroid hormone levels and risk of breast cancer for postmenopausal women. Cancer Epidemiological Biomarkers Prevention, 19(2), 492–502.
Ballantyne, K. N., Kayser, M., & Grootegoed, J. A. (2011). Sex and gender issues in competitive sports: Investigation of a historical case leads to a new viewpoint. British Journal of Sports Medicine, 46(8), 614–617.
Becerra Fernandez, A., De Luis Roman, D., & Piedrola Maroto, G. (1999). Morbilidad en pacientes transexuales con autotratamiento hormonal para cambiar de sexo. Medicine Clinic (Barcelona), 113, 481–483.
Benjamin, H. (1966). The transsexual phenomenon. New York, NY: Julian Press.
Bentvelsen, F. M., Brinkmann, A. O., van der Schoot, P., van der Linden, J. E., van der Kwast, T. H., Boersma, W. J., et al. (1995). Developmental pattern and regulation by androgens of androgen receptor expression in the urogenital tract of the rat. Molecular and Cellular Endocrinology, 113(2), 245–253.
Bentz, E. K., Pils, D., Bilban, M., Kaufmann, U., Hefler, L. A., Reinthaller, A., et al. (2010). Gene expression signatures of breast tissue before and after cross-sex hormone therapy in female-to-male transsexuals. Fertility and Sterility, 94(7), 2688–2696.
Bunck, M. C., Debono, M., Giltay, E. J., Verheijen, A. T., Diamant, M., & Gooren, L. J. (2009). Autonomous prolactin secretion in two male-to-female transgender patients using conventional oestrogen dosages. BMJ Case Reports. pii: bcr02.2009.1589.
Burcombe, R. J., Makris, A., Pittam, M., & Finer, N. (2003). Breast cancer after bilateral subcutaneous mastectomy in a female-to-male trans-sexual. Breast, 12(4), 290–293.
Cebula, H., Pham, T. Q., Boyer, P., & Froelich, S. (2010). Regression of meningiomas after discontinuation of cyproterone acetate in a transsexual patient. Acta Neurochirurgica, 152(11), 1955–1956.
Choong, K., Lakshman, K. M., & Bhasin, S. (2008). The physiological and pharmacological basis for the ergogenic effects of androgens in elite sports. Asian Journal of Andrology, 10(3), 351–363.
De Sutter, P. (2001). Gender reassignment and assisted reproduction: Present and future reproductive options for transsexual people. Human Reproduction, 16(4), 612–614.
Deipolyi, A. R., Han, S. J., & Parsa, A. T. (2010). Development of a symptomatic intracranial meningioma in a male-to-female transsexual after initiation of hormone therapy. Journal of Clinical Neuroscience, 17(10), 1324–1326.
Dhand, A., & Dhaliwal, G. (2010). Examining patient conceptions: A case of metastatic breast cancer in an African American male to female transgender patient. Journal of General Internal Medicine, 25(2), 158–161.
Dhejne, C., Lichtenstein, P., Boman, M., Johansson, A. L., Langstrom, N., & Landen, M. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study in Sweden. PLoS One, 6(2), e16885.
Dimitrakakis, C., & Bondy, C. (2009). Androgens and the breast. Breast Cancer Research, 11(5), 212.
Dizon, D. S., Tejada-Berges, T., Koelliker, S., Steinhoff, M., & Granai, C. O. (2006). Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient. Gynecologic and Obstetric Investigation, 62(4), 226–228.
Dorff, T. B., Shazer, R. L., Nepomuceno, E. M., & Tucker, S. J. (2007). Successful treatment of metastatic androgen-independent prostate carcinoma in a transsexual patient. Clinical Genitourinary Cancer, 5(5), 344–346.
Dougherty, S. M., Mazhawidza, W., Bohn, A. R., Robinson, K. A., Mattingly, K. A., Blankenship, K. A., et al. (2006). Gender difference in the activity but not expression of estrogen receptors alpha and beta in human lung adenocarcinoma cells. Endocrine-Related Cancer, 13(1), 113–134.
Driak, D., & Samudovsky, M. (2004). Cervical cancer in a female-to-male trans-sexual. European Journal of Cancer, 40(11), 1795.
Galazis, N., Olaleye, O., Haoula, Z., Layfield, R., & Atiomo, W. (2012). Proteomic biomarkers for ovarian cancer risk in women with polycystic ovary syndrome: A systematic review and biomarker database integration. Fertility and Sterility, 98(6), 1590–1601.
Ganly, I., & Taylor, E. W. (1995). Breast cancer in a trans-sexual man receiving hormone replacement therapy. The British Journal of Surgery, 82(3), 341.
Garcia-Malpartida, K., Martin-Gorgojo, A., Rocha, M., Gomez-Balaguer, M., & Hernandez-Mijares, A. (2010). Prolactinoma induced by estrogen and cyproterone acetate in a male-to-female transsexual. Fertility and Sterility, 94(3), 1097. e1013–e1095.
Gazzeri, R., Galarza, M., & Gazzeri, G. (2007). Growth of a meningioma in a transsexual patient after estrogen-progestin therapy. The New England Journal of Medicine, 357(23), 2411–2412.
Gooren, L. J. (2011). Clinical practice. Care of transsexual persons. The New England Journal of Medicine, 364(13), 1251–1257.
Gooren, L. J., Assies, J., Asscheman, H., de Slegte, R., & van Kessel, H. (1988). Estrogen-induced prolactinoma in a man. The Journal of Clinical Endocrinology and Metabolism, 66(2), 444–446.
Gooren, L. J., & Behre, H. M. (2008). Testosterone treatment of hypogonadal men participating in competitive sports. Andrologia, 40(3), 195–199.
Gooren, L. J., & Bunck, M. C. (2004). Transsexuals and competitive sports. European Journal of Endocrinology, 151(4), 425–429.
Gooren, L. J., & Giltay, E. J. (2008). Review of studies of androgen treatment of female-to-male transsexuals: Effects and risks of administration of androgens to females. The Journal of Sexual Medicine, 5(4), 765–776.
Gooren, L. J., Giltay, E. J., & Bunck, M. C. (2008). Long-term treatment of transsexuals with cross-sex hormones: Extensive personal experience. The Journal of Clinical Endocrinology and Metabolism, 93(1), 19–25.
Gooren, L. J., Sungkaew, T., & Giltay, E. J. (2012). Exploration of functional health, mental well-being and cross-sex hormone use in a sample of Thai male-to-female transgendered persons (kathoeys). Asian Journal of Andrology. doi:10.1038/aja.2012.139.
Grabellus, F., Worm, K., Willruth, A., Schmitz, K. J., Otterbach, F., Baba, H. A., et al. (2005). ETV6-NTRK3 gene fusion in a secretory carcinoma of the breast of a male-to-female transsexual. Breast, 14(1), 71–74.
Grady, D., & Barrett-Connor, E. (2007). Postmenopausal hormone therapy. BMJ, 334(7599), 860–861.
Grynberg, M., Fanchin, R., Dubost, G., Colau, J. C., Bremont-Weil, C., Frydman, R., et al. (2010). Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reproductive Biomedicine Online, 20(4), 553–558.
Hage, J. J., Dekker, J. J., Karim, R. B., Verheijen, R. H., & Bloemena, E. (2000). Ovarian cancer in female-to-male transsexuals: Report of two cases. Gynecologic Oncology, 76(3), 413–415.
Hamburger, C. (1969). Endocrine treatment of male and female transsexualism (pp. 291–307). Baltimore, MD: Johns Hopkins Press.
Handelsman, D. J., & Gooren, L. J. (2008). Hormones and sport: Physiology, pharmacology and forensic science. Asian Journal of Andrology, 10(3), 348–350.
Handelsman, D. J., & Heather, A. (2008). Androgen abuse in sports. Asian Journal of Andrology, 10(3), 403–415.
Haring, R., Volzke, H., Felix, S. B., Schipf, S., Dorr, M., Rosskopf, D., et al. (2009). Prediction of metabolic syndrome by low serum testosterone levels in men: Results from the study of health in Pomerania. Diabetes, 58(9), 2027–2031.
Hembree, W. C., Cohen-Kettenis, P., Delemarre-van de Waal, H. A., Gooren, L. J., Meyer, W. J., III, Spack, N. P., et al. (2009). Endocrine treatment of transsexual persons: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism, 94(9), 3132–3154.
Institute of Medicine (Ed.). (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press.
Ito, K. (2007). Hormone replacement therapy and cancers: The biological roles of estrogen and progestin in tumorigenesis are different between the endometrium and breast. The Tohoku Journal of Experimental Medicine, 212(1), 1–12.
Khosla, S. (2010). Update on estrogens and the skeleton. The Journal of Clinical Endocrinology and Metabolism, 95(8), 3569–3577.
Kovacs, K., Stefaneanu, L., Ezzat, S., & Smyth, H. S. (1994). Prolactin-producing pituitary adenoma in a male-to-female transsexual patient with protracted estrogen administration. A morphologic study. Archives of Pathology and Laboratory Medicine, 118(5), 562–565.
Marjoribanks, J., Farquhar, C., Roberts, H., & Lethaby, A. (2012). Long term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database of Systematic Reviews (Online), 7, CD004143.
Mauras, N., Hayes, V., Welch, S., Rini, A., Helgeson, K., Dokler, M., et al. (1998). Testosterone deficiency in young men: Marked alterations in whole body protein kinetics, strength, and adiposity. The Journal of Clinical Endocrinology and Metabolism, 83(6), 1886–1892.
Meyer, W. J., Walker, P. A., & Suplee, Z. R. (1981). A survey of transsexual hormonal treatment in twenty gender-treatment centers. Journal of Sex Research, 17(4), 344–349.
Migeon, C. J., Rivarola, M. A., & Forest, M. G. (1968). Studies of androgens in transsexual subjects. Effects of estrogen therapy. The Johns Hopkins Medical Journal, 123(3), 128–133.
Miksad, R. A., Bubley, G., Church, P., Sanda, M., Rofsky, N., Kaplan, I., et al. (2006). Prostate cancer in a transgender woman 41 years after initiation of feminization. JAMA: The Journal of the American Medical Association, 296(19), 2316–2317.
Molokwu, C. N., Appelbaum, J. S., & Miksad, R. A. (2008). Detection of prostate cancer following gender reassignment. BJU International, 101(2), 259. author reply 259–260.
Money, J. (1971). Transexualism and the philosophy of healing. The Journal of the American Society of Psychosomatic Dentistry and Medicine, 18, 25–26.
Mueller, A., Dittrich, R., Binder, H., Kuehnel, W., Maltaris, T., Hoffmann, I., et al. (2005). High dose estrogen treatment increases bone mineral density in male-to-female transsexuals receiving gonadotropin-releasing hormone agonist in the absence of testosterone. European Journal of Endocrinology, 153(1), 107–113.
Mueller, A., & Gooren, L. (2008). Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. European Journal of Endocrinology, 159(3), 197–202.
Ott, J., Kaufmann, U., Bentz, E. K., Huber, J. C., & Tempfer, C. B. (2010). Incidence of thrombophilia and venous thrombosis in transsexuals under cross-sex hormone therapy. Fertility and Sterility, 93(4), 1267–1272.
Pache, T. D., & Fauser, B. C. (1993). Polycystic ovaries in female-to-male transsexuals. Clinical Endocrinology, 39(6), 702–703.
Pritchard, T. J., Pankowsky, D. A., Crowe, J. P., & Abdul-Karim, F. W. (1988). Breast cancer in a male-to-female transsexual. A case report. JAMA: The Journal of the American Medical Association, 259(15), 2278–2280.
Ruetsche, A. G., Kneubuehl, R., Birkhaeuser, M. H., & Lippuner, K. (2005). Cortical and trabecular bone mineral density in transsexuals after long-term cross-sex hormonal treatment: A cross-sectional study. Osteoporosis International, 16(7), 791–798.
Schenck, T. L., Holzbach, T., Zantl, N., Schuhmacher, C., Vogel, M., Seidl, S., et al. (2010). Vaginal carcinoma in a female-to-male transsexual. The Journal of Sexual Medicine, 7(8), 2899–2902.
Schoemaker, M. J., Swerdlow, A. J., Higgins, C. D., Wright, A. F., & Jacobs, P. A. (2008). Cancer incidence in women with Turner syndrome in Great Britain: A national cohort study. The Lancet Oncology, 9(3), 239–246.
Serri, O., Noiseux, D., Robert, F., & Hardy, J. (1996). Lactotroph hyperplasia in an estrogen treated male-to-female transsexual patient. The Journal of Clinical Endocrinology and Metabolism, 81(9), 3177–3179.
Shao, T., Grossbard, M. L., & Klein, P. (2011). Breast cancer in female-to-male transsexuals: Two cases with a review of physiology and management. Clinical Breast Cancer, 11(6), 417–419.
Slagter, M. H., Gooren, L. J., Scorilas, A., Petraki, C. D., & Diamandis, E. P. (2006). Effects of long-term androgen administration on breast tissue of female-to-male transsexuals. The Journal of Histochemistry and Cytochemistry, 54(8), 905–910.
Slattery, M. L., Sweeney, C., Murtaugh, M., Ma, K. N., Caan, B. J., Potter, J. D., et al. (2006). Associations between vitamin D, vitamin D receptor gene and the androgen receptor gene with colon and rectal cancer. International Journal of Cancer, 118(12), 3140–3146.
Storer, T. W., Magliano, L., Woodhouse, L., Lee, M. L., Dzekov, C., Dzekov, J., et al. (2003). Testosterone dose-dependently increases maximal voluntary strength and leg power, but does not affect fatigability or specific tension. The Journal of Clinical Endocrinology and Metabolism, 88(4), 1478–1485.
Symmers, W. S. (1968). Carcinoma of breast in trans-sexual individuals after surgical and hormonal interference with the primary and secondary sex characteristics. British Medical Journal, 2(5597), 83–85.
Thurston, A. V. (1994). Carcinoma of the prostate in a transsexual. British Journal of Urology, 73(2), 217.
Toorians, A. W., Thomassen, M. C., Zweegman, S., Magdeleyns, E. J., Tans, G., Gooren, L. J., et al. (2003). Venous thrombosis and changes of hemostatic variables during cross-sex hormone treatment in transsexual people. The Journal of Clinical Endocrinology and Metabolism, 88(12), 5723–5729.
T’Sjoen, G., Weyers, S., Taes, Y., Lapauw, B., Toye, K., Goemaere, S., et al. (2009). Prevalence of low bone mass in relation to estrogen treatment and body composition in male-to-female transsexual persons. Journal of Clinical Densitometry, 12(3), 306–313.
Turner, A., Chen, T. C., Barber, T. W., Malabanan, A. O., Holick, M. F., & Tangpricha, V. (2004). Testosterone increases bone mineral density in female-to-male transsexuals: A case series of 15 subjects. Clinical Endocrinology, 61(5), 560–566.
Utian, W. H. (2012). A decade post WHI, menopausal hormone therapy comes full circle—Need for independent commission. Climacteric, 15(4), 320–325.
Van Caenegem, E., Wierckx, K., Taes, Y., Dedecker, D., Van de Peer, F., Toye, K., et al. (2012). Bone mass, bone geometry, and body composition in female-to-male transsexual persons after long-term cross-sex hormonal therapy. The Journal of Clinical Endocrinology and Metabolism, 97(7), 2503–2511.
van Haarst, E. P., Newling, D. W., Gooren, L. J., Asscheman, H., & Prenger, D. M. (1998). Metastatic prostatic carcinoma in a male-to-female transsexual. British Journal of Urology, 81(5), 776.
van Kesteren, P. J., Asscheman, H., Megens, J. A., & Gooren, L. J. (1997). Mortality and morbidity in transsexual subjects treated with cross-sex hormones. Clinical Endocrinology, 47(3), 337–342.
van Kesteren, P., Lips, P., Deville, W., Popp-Snijders, C., Asscheman, H., Megens, J., et al. (1996). The effect of one-year cross-sex hormonal treatment on bone metabolism and serum insulin-like growth factor-1 in transsexuals. The Journal of Clinical Endocrinology and Metabolism, 81(6), 2227–2232.
van Kesteren, P., Lips, P., Gooren, L. J., Asscheman, H., & Megens, J. (1998). Long-term follow-up of bone mineral density and bone metabolism in transsexuals treated with cross-sex hormones. Clinical Endocrinology, 48(3), 347–354.
Watts, N. B., Adler, R. A., Bilezikian, J. P., Drake, M. T., Eastell, R., Orwoll, E. S., et al. (2012). Osteoporosis in men: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology and Metabolism, 97(6), 1802–1822.
Wierckx, K., Mueller, S., Weyers, S., Van Caenegem, E., Roef, G., Heylens, G., et al. (2012). Long-term evaluation of cross-sex hormone treatment in transsexual persons. The Journal of Sexual Medicine, 9(10), 2641–2651. doi:10.1111/j.1743-6109.2012.02876.x.
Wierckx, K., Stuyver, I., Weyers, S., Hamada, A., Agarwal, A., De Sutter, P., et al. (2012). Sperm freezing in transsexual women. Archives of Sexual Behavior, 41(5), 1069–1071.
Wierckx, K., Van Caenegem, E., Pennings, G., Elaut, E., Dedecker, D., Van de Peer, F., et al. (2012). Reproductive wish in transsexual men. Human Reproduction, 27(2), 483–487.
Wigertz, A., Lonn, S., Mathiesen, T., Ahlbom, A., Hall, P., & Feychting, M. (2006). Risk of brain tumors associated with exposure to exogenous female sex hormones. American Journal of Epidemiology, 164(7), 629–636.
Yeap, B. B. (2009). Are declining testosterone levels a major risk factor for ill-health in aging men? International Journal of Impotence Research, 21(1), 24–36.
Yeap, B. B., Chubb, S. A., Hyde, Z., Jamrozik, K., Hankey, G. J., Flicker, L., et al. (2009). Lower serum testosterone is independently associated with insulin resistance in non-diabetic older men: The health in men study. European Journal of Endocrinology, 161(4), 591–598.
Zitzmann, M., Erren, M., Kamischke, A., Simoni, M., & Nieschlag, E. (2005). Endogenous progesterone and the exogenous progestin norethisterone enanthate are associated with a proinflammatory profile in healthy men. The Journal of Clinical Endocrinology and Metabolism, 90(12), 6603–6608.
Acknowledgements
Financial support was received from Stichting Reproductieve Geneeskunde, Amsterdam, the Netherlands.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Gooren, L., Asscheman, H. (2014). Sex Reassignment: Endocrinological Interventions in Adults with Gender Dysphoria. In: Kreukels, B., Steensma, T., de Vries, A. (eds) Gender Dysphoria and Disorders of Sex Development. Focus on Sexuality Research. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-7441-8_14
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7441-8_14
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-7440-1
Online ISBN: 978-1-4614-7441-8
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)