Abstract
This chapter summarizes the surgical techniques used to reconstruct the diseased middle ear, as well as some of the basic science behind such reconstructions. The techniques include the reconstruction of the tympanic membrane and ossicular chain, as well as surgery to replace the stapes after otosclerotic stapes fixation. The importance of aeration of the middle ear is raised, and recommendations for the amount of air needed for adequate middle ear function are made. Types of passive ossicular replacement prostheses are also discussed.
Saumil N. Merchant
Deceased
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cholesteatoma
- Chronic otitis media
- Conductive hearing loss
- Mastoidectomy
- Middle ear aeration
- Middle ear reconstructive surgery
- Ossicular reconstruction
- Ossicular replacement prostheses
- Otosclerosis
- Stapedectomy
- Tympanoplasty
9.1 Introduction
A surgical procedure performed to repair or reconstruct the tympanic membrane (TM) and/or one of more of the ossicles is called tympanoplasty. As described in Sect. 9.3.1 there are many subtypes of tympanoplasty. Related terms used by otologic surgeons include myringoplasty (a simple repair of just the TM) and ossiculoplasty (repair or reconstruction of the ossicular chain only). The majority of tympanoplasty procedures are performed for defects of the TM or ossicles as a result of chronic otitis media. Tympanoplasty surgery is often performed in conjunction with mastoidectomy, which refers to surgical opening and exenteration of mastoid air cells, typically performed for eradication of infection within the middle ear and mastoid air spaces. The term stapedectomy refers to a surgical procedure consisting of removal of the stapes and its replacement by an artificial prosthesis. The main indication of a stapedectomy is to restore hearing in patients with conductive hearing loss due to fixation of the stapes bone caused by otosclerosis.
A major objective of tympanoplasty and stapedectomy procedures is restoration of hearing loss caused by middle ear diseases such as chronic otitis media and otosclerosis. These diseases often result in a conductive hearing loss, the severity of which can be quantified by the difference between air- and bone-conduction thresholds on audiometry (so-called air–bone gap). Readers are referred to Chap. 4 by Voss et al. and Chap. 8 by Popelka and Hunter for a discussion of audiometry, air–bone gap, and conductive hearing loss.
The present chapter provides an overview of chronic otitis media and otosclerosis, surgical terminology used, the acoustics and mechanics of these operative procedures, and future directions. Readers should consult clinical and surgical texts for in-depth information and details which are beyond the scope of this chapter (Nadol and McKenna 2005; Brackmann et al. 2010; Merchant and Nadol 2010).
Historically, surgery of the middle ear and mastoid evolved out of the desire of otologic surgeons to combat middle ear infections and to correct the conductive hearing loss caused by disorders such as otitis media and otosclerosis. In many instances, these procedures were developed and improved upon by empirical observations, and by trial and error, as the underlying basic science knowledge of the mechanics of the normal and diseased middle ear was not available. In the pre-antibiotic era, the vast majority of procedures consisted of different types of mastoidectomy, with the main goal being the eradication of infection to prevent meningitis and other feared intracranial complications of otitis media. There was little regard for restoration of hearing at the time. Clinical advances made possible by the introduction of antibiotics and the operating microscope, as well as availability of safe techniques of anesthesia, set the stage for the modern era of middle ear reconstruction in the 1950s when tympanoplasty and stapedectomy were described. The German otologic surgeons Horst Wullstein and Fritz Zollner were at the forefront in the development of techniques of tympanoplasty (Sismanis 2010), while American otologists John Shea and Harold Schuknecht pioneered the modern stapedectomy operation (Handzel and McKenna 2010). Subsequently, many other clinicians and surgeons modified these techniques, and tympanoplasty and stapedectomy became firmly established and adopted on a worldwide basis by the early 1960s. It is pertinent to point out that attempts at similar middle ear procedures had occurred decades earlier in the pre-antibiotic era. For instance, Berthold in Germany described a technique for TM reconstruction in 1878, and Jack and Blake in Boston described a series of patients undergoing stapedectomy in the 1890s (Sismanis 2010).
9.2 Brief Review of Common Disorders Requiring Middle Ear Reconstructive Surgery
Chronic otitis media (COM) is a chronic inflammatory disease of the middle ear and mastoid that may result in partial or total loss of the TM and/or ossicles leading to conductive hearing loss that can be as large as 60–70 dB. COM comprises a spectrum of disorders, which may be broadly classified into two categories: COM without cholesteatoma and COM with cholesteatoma (“cholesteatoma” is a term used to describe a disorder characterized by presence of skin in the middle ear).
The main clinical feature of COM without cholesteatoma is a perforation of the pars tensa of the TM (Fig. 9.1). The hallmark of cholesteatoma is a retraction pocket or a perforation of TM with retention of squamous debris within the middle ear (Fig. 9.2).
Chronic otitis media (COM) without cholesteatoma. (Left) Otoscopic images of small and large perforations of the pars tensa of the tympanic membrane (TM). (Right) shows photomicrograph of a human temporal bone showing multiple pathologic changes in the tympanic cavity including mucosal hypertrophy and inflammation, and formation of pus. Similar changes occur throughout the mastoid air spaces. These changes result in defects in the TM and erosion of the ossicles. ET Eustachian tube
COM with cholesteatoma. (Left) Otoscopic images of cholesteatoma of the pars flaccida (top) and pars tensa (bottom). In both cases, the dark areas consist of squamous debris within a retraction pocket of the TM. (Right) A photomicrograph of a human temporal bone showing a cholesteatoma of the middle ear. Note the reactive mucosal inflammation and thickening. The cholesteatoma and the reactive mucosal changes lead to erosion and resorption of the ossicles and defects of the TM, all of which result in conductive hearing loss
Both categories of COM may be accompanied by bacterial infection within the middle ear and mastoid, resulting in purulent otorrhea. Both categories are also often characterized by pathologic changes within the middle ear and mastoid air spaces (Figs. 9.1 and 9.2), including mucosal inflammation, formation of granulation tissue, resorptive osteitis, and erosion of bone, as well as healing responses characterized by deposition of fibrous tissue, formation of new bone, and deposition of hyaline plaques (called tympanosclerosis). In addition, ears with COM often demonstrate abnormalities of middle ear static pressure and dysfunction of the Eustachian tube.
The widespread tissue changes and abnormalities in ears with COM have important implications for tympanoplasty. For example, postoperative mucosal fibrosis, formation of new bone, and development of negative static pressure in the middle ear, which can occur over the course of months or years, can have a detrimental effect on the outcome of tympanoplasty. These factors are responsible for the overall modest nature of tympanoplasty results (Merchant et al. 1998a), especially in comparison to outcomes after stapedectomy for otosclerosis.
Otosclerosis is a localized genetic disorder affecting bone of the otic capsule that is characterized by disordered resorption and deposition of bone. Otosclerosis occurs at certain sites of predilection within the otic capsule, one of which is the area anterior to the oval window (Fig. 9.3). An expanding otosclerotic lesion in this location often results in fixation of the stapes, which produces a conductive hearing loss. The physiology of the middle ear and mastoid remains unaffected in patients with otosclerosis. In other words, the TM, malleus and incus, static pressure in the middle ear and mastoid, and mucosa of the middle ear all remain healthy, unlike in cases of COM. As a result, the main surgical challenge is to overcome the mechanical fixation of the stapes and once that is accomplished, long-term results are generally favorable.
Otosclerosis. Photomicrograph of temporal bone shows an otosclerotic lesion anterior to the oval window that has fixed the stapes. Middle ear structures such as the TM, malleus, incus, and the air spaces are unaffected in otosclerosis. Image in lower left corner shows otoscopic appearance of TM, which is typically normal in patients with otosclerosis
9.3 Terminology for Middle Ear Surgical Procedures
9.3.1 Tympanoplasty
Otologic surgeons have developed a large repertoire of tympanoplasty procedures, each designed to correct specific types of anatomical defects for a given disease state of the middle ear. It is common to have more than one method that has been described to correct a given anatomical defect. Wullstein classified tympanoplasty operations as types I through V, based on the concepts of sound transformation at the oval window and sound protection of the round window (Wullstein 1956). However, this classification was developed before the advent of ossicular implants; hence, other classification schemes have been developed, for example, the Schuknecht-Nadol modification of Wullstein’s classification (Merchant 2005) and the Austin classification (Sismanis and Poe 2010). For the sake of simplicity and ease of understanding, the present chapter relies on describing the reconstruction done in a tympanoplasty rather than adhering to a particular classification scheme.
TM reconstruction is performed when there is a perforation of the TM but the ossicular chain is intact (top left panel in Fig. 9.4). Many different tissue grafts have been described for repair of the TM including temporalis fascia, perichondrium, cartilage, periosteum, and adipose tissue. A large number of surgical techniques have been described for repair of perforations, depending on the size and location of the perforation, as well as presence or absence of additional middle ear pathology. Repair of just the TM is the most commonly performed tympanoplasty in otologic practice.
The ossicular chain is diseased in many cases and has to be reconstructed in a tympanoplasty. A common problem is resorption of the distal part of the long process of the incus. If the remainder of the incus is healthy, it can be removed, reshaped by a surgical drill, and placed back as an incus strut to restore the continuity of the ossicular chain; such a procedure is termed an incus interposition (top right panel in Fig. 9.4). If the ossicles are too diseased to be reused, or they are missing (resorbed) because of COM, then synthetic implants (prostheses) can be used to reconstruct the ossicular chain. If the stapes is present, then a prosthesis can be placed from the stapes capitulum to the TM or manubrium; this is termed a partial ossicular replacement prosthesis (PORP; middle left panel in Fig. 9.4). If the stapes is missing, then a prosthesis may be placed between the stapes footplate and the TM or manubrium; this is termed a total ossicular replacement prosthesis (TORP; middle right panel in Fig. 9.4). PORPs and TORPs made of hydroxyapatite or titanium are popular in contemporary otologic practice. A buffer of cartilage is often interposed between a PORP/TORP and the TM to decrease the potential for extrusion of the prosthesis.
When the ossicles are diseased, it is also possible to perform a tympanoplasty without the use of an interposed incus, PORP or TORP. In a stapes columella tympanoplasty, the reconstructed TM is advanced in a medial direction so that it is in direct contact with the capitulum of the stapes (bottom left panel in Fig. 9.4). In a type IV tympanoplasty, the stapes footplate is allowed to remain directly exposed to incoming sound from the ear canal, and a tissue graft is placed to acoustically shield the round window membrane from sound (bottom right panel in Fig. 9.4). The air space enclosed between the acoustic shield and the round window is called the cavum minor. The cavum minor is aerated via the Eustachian tube.
The choice of tympanoplasty procedure is dictated by the extent of deficiency of the TM and ossicles caused by disease, as well as by the nature of ancillary mastoid surgery, preference of the surgeon, and availability of synthetic materials.
9.3.2 Mastoidectomy
Mastoidectomy refers to a surgical procedure to open the mastoid and drill away the mastoid air cells with the objective of removing infection, or accessing sequestered anatomical areas such as the epitympanum. A common indication for mastoidectomy is COM. There are two broad types of mastoidectomy procedures (Fig. 9.5). A canal wall-up mastoidectomy consists of removal of mastoid air cells while preserving the posterior wall of the bony external auditory canal. On the other hand, a canal wall-down mastoidectomy consists of removal of the posterior bony canal wall so that the external auditory canal, mastoid, and epitympanum become one common cavity. The bony canal wall is surgically removed to the level of the facial nerve. The size of the resulting mastoid cavity (called “mastoid bowl”) is often reduced by obliterating it with tissue such as bone dust, muscle, and fat. Mastoidectomy is often combined with tympanoplasty and the two procedures may be performed at the same time or sequentially.
Mastoidectomy. Diagrammatic representation of canal wall-up and canal wall-down mastoidectomy. The uniform gray areas show the regions in which the surgeon has opened the mastoid to remove disease. In the canal-wall down procedure, this area is contiguous with the widened ear canal. See also descriptions in text
9.3.3 Stapedectomy
The term stapedectomy is used broadly to include all procedures where the stapes is removed and replaced by a prosthesis. The most common reason to perform a stapedectomy is when the stapes bone is ankylosed due to otosclerosis. Other indications include a stapes fixed by tympanosclerosis (caused by COM), or a stapes that has been compromised due to trauma. When the entire footplate is removed, the procedure is termed a total stapedectomy. When a small opening is made in a portion of the footplate only, the procedure is more accurately called a stapedotomy (Fig. 9.6). Note: In this chapter, the term stapedectomy is used to include both total stapedectomy and stapedotomy procedures. A large variety of stapes prostheses have been described; implants made of Teflon and titanium are in common use.
Schematic diagram of stapedotomy, where the superstructure has been removed, an opening made in the footplate, and sound transmission restored by placement of a stapes prosthesis from the incus to the oval window. The black area at the lower end of the prosthesis represents tissue (e.g., fat) used to seal the opening in the footplate around the piston
9.4 Acoustics and Mechanics of Reconstructed Middle Ears
9.4.1 Role of Aeration
Aeration of the middle ear (including the round window) is critical to the success of any tympanoplasty procedure. Aeration allows the TM, ossicles, and round window to move. Clinical experience has shown that nonaerated ears often demonstrate 40–60 dB air–bone gaps (Merchant et al. 1998a) because (1) ossicular coupling is greatly reduced (see Voss et al., Chap. 4 for a description of ossicular coupling), and (2) stapes motion is reduced because the round window membrane (which is coupled to the stapes by incompressible cochlear fluids) cannot move freely.
How much air is necessary behind the TM (i.e., within the middle ear and mastoid)? Model analyses of the effects of varying the volume of the middle ear and mastoid predict an increasing low frequency hearing loss as air volume is reduced (Rosowski and Merchant 1995) (Fig. 9.7). The normal, average volume of the middle ear and mastoid is 6 cc; a combined middle ear and mastoid volume of 0.5 cc is predicted to result in a 10 dB conductive hearing loss. Volumes smaller than 0.5 cc should lead to progressively larger gaps, whereas increases in volume above about 1.0 cc are predicted to provide little additional acoustic benefit. Experimental studies using a human temporal bone preparation in which the middle ear and mastoid volume was reduced progressively show results consistent with the model prediction (Gyo et al. 1986; Whittemore et al. 1998).
Model predictions of the effects of reducing the volume of the middle ear and mastoid. The normal baseline volume is taken to be 6 cc. Note that reduction of the volume to 0.4 cc is predicted to result in an air bone gap less than 10 dB. Volumes smaller than 0.4 cc are predicted to lead to progressively larger gaps (Modified from Rosowski and Merchant 1995.)
Static air pressure within the middle ear space is another parameter that can influence middle ear mechanics. Animal studies and measurements of ossicular motion in human temporal bones have demonstrated that middle ear static pressure can have different effects on sound transmission at different frequencies (Murakami et al. 1997). Generally, trans-TM static pressure differences produce decreases in sound transmission through the middle ear for frequencies less than 1,000 Hz, and have less effect at higher frequencies. Also, the effects of such static pressure differences are asymmetric, with larger decreases observed when the middle ear pressure is negative relative to that in the ear canal. The mechanisms by which pressure changes reduce middle ear sound transmission are not well defined, and possible sites of pressure sensitivity include the TM, annular ligament, incudo–malleal joint, and suspensory ligaments of the ossicles. Although some of these structures are drastically altered by tympanoplasty, the acoustic effects of negative and positive middle ear static pressure in reconstructed ears have not been characterized.
9.4.2 TM Reconstruction
Clinical observations indicate that the surgical techniques used to repair the TM can lead to good hearing results with resolution of the conductive hearing loss (Merchant et al. 2003a). However, in up to 30 % of patients there is a residual air bone gap that may vary from 5 to 35 dB even in the presence of an aerated middle ear (Merchant et al. 2000). Although clinical observations suggest that restoration or preservation of the normal TM anatomy can lead to good hearing results, research is needed to define the optimum acoustic and mechanical properties of reconstructed TM. For example: (1) although O’Connor et al. (2008) found that radial fibers are important for sound transmission greater than 4 kHz in the normal TM, little is known of the mechanical significance of the arrangements of structural fibers in reconstructed TM. (2) Although it has been argued that the conical shape of the normal TM plays an important role in middle ear function (Tonndorf and Khanna 1972; Fay et al. 2006), the possible effects of changes in TM shape on postoperative hearing results are not understood. (3) Although many existing models of TM function have been shown to fit some of the available data (Funnell and Decraemer 1996), there are wide differences in the structure of these models, and little effort has been made to compare their significant differences and similarities. With a few exceptions (Tuck-Lee et al. 2008), these models generally have not been applied to the reconstructed TM. Better understanding of the features of TM structure that are critical to its function should lead to improved methods for TM reconstruction.
9.4.3 Ossicular Reconstruction with Incus Interposition, PORPs, and TORPs
The hearing results after ossicular reconstructions vary widely with air–bone gaps ranging from 0 to 60 dB. A large number of studies have evaluated the influence of acoustical and mechanical properties of an ossicular prosthesis including its stiffness, mass, and position; the tension imposed by the prosthesis on the TM and annular ligament; and mechanical features associated with coupling of the prosthesis to the TM and stapes (Goode and Nishihara 1994; Merchant et al. 1998a).
In general, the stiffness of a prosthesis will not be a significant factor as long as the stiffness is much greater than that of the stapes footplate-cochlear impedance. For clinical purposes, prostheses made of ossicles (such as an interposed incus) and many synthetic materials generally meet this requirement.
Model analysis (Rosowski and Merchant 1995) and experimental data (Gan et al. 2001; Bance et al. 2007a) suggest that an increase in ossicular mass does not cause significant detriment in middle ear sound transmission. Increases up to 16 times the ossicle mass are predicted to cause less than 10 dB conductive loss and only at frequencies greater than 1,000 Hz.
The positioning of a prosthesis appears to be important to its function (Murugasu et al. 2005). Measurements in human temporal bone preparations suggest that the angle between the stapes and a prosthesis should be less than 45° for optimal sound transmission (Vlaming and Feenstra 1986; Nishihara and Goode 1994), and that the neck of the malleus is a good contact point for TORPs (Puria et al. 2005). There is also evidence that some variations in positioning produce only small changes. For example, while it is ideal to attach a prosthesis to the manubrium, experimental data show that acceptable results can occur with a prosthesis placed against the posterior–superior quadrant of the tympanic membrane as long as approximately 3–4 mm of the prosthesis’ diameter contacts the TM (Goode and Nishihara 1994; Bance et al. 2007b).
The tension the prosthesis creates in the middle ear, which is generally a function of prosthesis length, appears critical in determining the hearing result (Morris et al. 2004). The mechanical impedance of biological structures is inherently nonlinear, and the TM and annular ligament act as linear elements only over the range of small motions (less than 10 μm) associated with physiological sound levels. Larger displacements of the ligament and TM (by a prosthesis that is too long) would stiffen these structures, resulting in a reduction in tympano-ossicular motion and an air–bone gap. Currently, tension cannot be assessed intraoperatively in an objective fashion; a reliable objective test of the tension would be useful to the otologic surgeon.
Coupling refers to how well a prosthesis adheres to the footplate or TM, and the degree of coupling will determine whether or not there is slippage in sound transmission at the ends of a prosthesis. Thus, a prosthesis transmits sound effectively only if there is good coupling at both ends. Clinical observations indicate that it is rare to obtain a firm union between a prosthesis and the stapes footplate. Hence, inadequate coupling at the prosthesis–footplate joint may be an important cause of a persistent postoperative air–bone gap. The physical factors that control coupling have not been determined in a quantitative manner, and further study of this parameter is warranted.
9.4.4 Stapes Columella Tympanoplasty
Large air–bone gaps (40–60 dB) occur as a result of stapes fixation, nonaeration of the middle ear, or both (Mehta et al. 2003; Merchant et al. 2003b). When the stapes is mobile and the middle ear is aerated, the average postoperative air–bone gap is on the order of 20–25 dB, suggesting that there is little middle ear sound pressure gain occurring through the reconstruction. Experimental and clinical studies of the stapes columellar reconstruction have shown that interposing a thin disk of cartilage between the graft and the stapes head improves hearing in the lower frequencies by 5–10 dB. It has been hypothesized that the cartilage acts to increase the “effective” area of the graft that is coupled to the stapes, which leads to an increase in the middle ear gain of the reconstructed ear (Merchant et al. 2003b).
9.4.5 Type IV Tympanoplasty
Peake et al. (1992) described a lumped element model of the type IV reconstruction as shown in Fig. 9.8. Predictions of the model under different conditions were tested against experimental data from a cadaveric temporal bone preparation and against clinical data (Merchant et al. 1995, 1997). A good match was seen between the predictions and the data. The model suggested that an “optimum” type IV reconstruction, as defined by normal footplate mobility, a sufficiently stiff acoustic graft-shield, and adequate aeration of the round window would result in maximum acoustic coupling with a predicted residual air–bone gap of only 20–25 dB. Such an optimum result is indeed consistent with the best type IV hearing results seen clinically. The analyses also predicted that decreased footplate mobility, inadequate acoustic shielding or inadequate round window aeration can lead to hearing losses as large as 60 dB.
Model of type IV tympanoplasty described by Peake et al. (1992). Stapes velocity, VS, depends on the sound-pressure difference, PWD, between the oval window sound pressure, POW, and the round window sound pressure, PRW. PWD is determined by the acoustic impedance of four structures represented by the gray boxes: impedance of the stapes footplate and annular ligament, impedance of the cochlea, impedance of the acoustic graft-shield, and impedance of the cavum minor. See also details in the text
9.4.6 Biologic and Pathologic Considerations in Tympanoplasty
In the case of tympanoplasty, an important determinant of the hearing outcome is the mechanical and acoustical adequacy of the reconstruction. In addition, the biology and pathology of COM can have significant effects on hearing results. For example, postoperative mucosal fibrosis, neo-osteogenesis, formation of adhesions and development of negative static pressure in the middle ear can occur over the course of months or years, which in turn can have a detrimental effect on the hearing result. It is instructive to note that the few studies in the literature that assess long-term hearing results show a progressive and systematic decline in initial hearing gain as a function of time. For example, Colletti et al. (1987), in a study of 832 ossiculoplasty procedures, found that at 6 months 77% of ears had an air–bone gap of 20 dB or less, but at 5 years only 42% had such a small air–bone gap.
Proliferation of fibrous tissue and formation of adhesions are significant problems that are more prone to occur when the middle ear mucosa is diseased, removed, or traumatized. Many different materials have been placed in the middle ear in an attempt to prevent formation of adhesions and fibrous tissue (Merchant et al. 1998b). These materials include GelfoamTM, hyaluronic acid, SilasticTM, and TeflonTM. GelfoamTM elicits a host inflammatory response leading to its resorption. In some cases, this inflammatory response results in adhesions, especially when the middle ear mucosa is deficient. Further, GelfoamTM is resorbed within 2 weeks, which is probably insufficient time for mucosal regeneration to occur. Hyaluronic acid is somewhat more difficult to handle than GelfoamTM and is also absorbed before mucosal regeneration is likely to be completed. SilasticTM and TeflonTM sheeting are relatively inert but they are not resorbed and can sometimes extrude. On occasion, they become engulfed by fibrous tissue leading to a nonaerated ear. Hence, none of the currently available spacer materials is ideal. What is needed is a material that will remain in place for several weeks to allow sufficient time for mucosal regeneration and will then undergo degradation and resorption so the ear can become aerated without fibrosis.
While rates of successful closure of TM perforations are uniformly high, in excess of 90%, a small number of grafted TMs show undesirable pathological changes including proliferation of fibrous tissue and thickening, resorption and excessive thinning, and lack of epithelialization with resulting discharge. The factor or factors controlling such responses are not well understood at present. Similarly, histopathologic responses of the ear to various ossicular grafts and prostheses play an important role in determining outcome of tympanoplasty; these include a foreign body giant cell response to synthetic materials that may lead to breakdown and resorption of parts of an implant (Bahmad and Merchant 2007).
Two significant causes for long-term failure of tympanoplasty are total or partial nonaeration of the middle ear and development of negative static pressure (as previously described). Nonaeration of the middle ear is usually due to Eustachian tube dysfunction and results in TM graft atelectasis, middle ear effusion, fibrocystic sclerosis of the middle ear, or a combination of these changes. Some postoperative ears that are aerated have a tendency to develop negative static pressure in the middle ear. Over the long term, this negative pressure leads to retraction and atelectasis of the reconstructed TM and functional compromise, as well as a predisposition to displacement or extrusion of ossicular prostheses. The negative pressure can also lead to recurrent cholesteatoma. The latter problem is a disadvantage for canal-wall up procedures relative to canal-wall down mastoidectomy.
9.4.7 Mastoidectomy
In a canal-wall-down mastoidectomy, the bony tympanic annulus and much of the ear canal is removed, and the TM graft is typically placed onto the stapes head, as well as onto the facial ridge and medial attic wall. This results in a significant reduction in the size of the residual middle ear air space. However, as long as this air space is greater than or equal to 0.5 cc, the resultant loss of sound transmission should be less than 10 dB (see Sect. 9.4.1). Since the average volume of the tympanic cavity is 0.5–1.0 cc (Molvaer et al. 1978), a canal-wall down procedure should create no significant acoustic detriment (in comparison to canal wall-up procedures), so long as the middle ear is aerated. Indeed, clinical studies comparing the acoustic results of canal wall-down verses canal wall-up mastoidectomy have shown no significant differences in hearing between the two conditions (Colletti et al. 1987; Merchant et al. 2003a).
A canal wall-down procedure also results in the creation of a large air space lateral to the eardrum, that is, the air space within the mastoid bowl including the external auditory canal. This mastoid bowl and ear canal air space generates resonances that can influence middle ear sound transmission favorably or unfavorably (Goode et al. 1977). The structure–function relationships between the size and shape of the mastoid cavity, and cavity resonances have not been well defined. An improved understanding of this issue may help otosurgeons to configure mastoid cavities in ways that are acoustically beneficial.
9.4.8 Stapedectomy
The output of the middle ear can be quantified by the “volume velocity” of the stapes (Rosowski and Merchant 1995), where volume velocity is the product of stapes linear velocity and the area of the stapes footplate. After a stapedotomy, the effective area of the footplate is reduced to the area of the prosthesis, thereby reducing the volume velocity produced by a given stapes linear velocity. The reduction in effective footplate area also reduces the area of the cochlear fluid over which the force generated by the stapes is applied. Whereas the reduced footplate area leads to a local increase in pressure over the surface of the prosthesis, the average pressure at the cochlear entrance is reduced. The reduction in stapes volume velocity and cochlear sound pressure lead to a decrease in ossicular coupling and the development of an air–bone gap. The smaller the area of the stapes prosthesis is, the greater the air–bone gap. Model predictions of the relationship between piston diameter and residual air–bone gap after stapedotomy were made using a simple lumped element model of the middle ear (Rosowski and Merchant 1995). This analysis predicted the 0.8 mm piston diameter will produce 5 dB better hearing results than the 0.6 mm piston and 10 dB better results than the 0.4 mm piston. These predictions are in general agreement with (1) experimental temporal bone data (Honda and Goode 2004), (2) results of finite element modeling data (Bohnke and Arnold 2007), and (3) clinical observations (Teig and Lindeman 1999; Laske et al. 2011). The predictions made in the simple lumped element model assumed that the effective vibrating footplate surface area after a stapedotomy is no more than the area of the lower end of the prosthesis. In cases of partial or total stapedectomy with placement of a tissue graft and a stapes prosthesis, the effective vibrating surface may be greater than the area of the prosthesis alone, and the model predictions may overestimate the air–bone gap.
9.5 Results After Middle Ear Surgery
Tympanoplasty and mastoidectomy surgery for COM: Such surgery is quite successful in controlling infection and preventing recurrent disease, with success rates in excess of 80–90%. Postoperative hearing results vary widely, depending on extent of TM and ossicular lesions, mucosal disease, cholesteatoma, and Eustachian tube function. When only TM reconstruction is needed, 80–90% of patients will have an air–bone gap of 20 dB or less. When ossicular reconstruction is necessary, long-term closure of the air–bone gap to less than 20 dB occurs in 40–70% of cases when the stapes is intact, and in only 20–55% in which the stapes superstructure is missing (Merchant et al. 1998a).
Stapedectomy surgery for otosclerosis: Results are uniformly good, with long-term closure of the air–bone gap to less than or equal to 20 dB reported in more than 95% of patients.
9.6 Future Directions
There are a number of areas where future research could optimize or improve results after middle ear reconstruction. Some of these areas were mentioned in the earlier sections. These include better understanding of structure–function correlations for reconstructed TMs, better ways to deal with effects of tension in ossicular reconstruction, and improved ways of coupling TORPs to the stapes footplate.
Research efforts have focused on utilizing growth factors and similar drugs to stimulate the closure of TM perforations without the need for surgical repair (Ma et al. 2002); the goal is to be able to apply the treatment topically and induce the edges of the perforation to heal over the opening.
The recent development of real time opto-electronic laser holographic techniques to study motion of the TM offers the prospect of improving our understanding of TM reconstructions and the issue of tension (Rosowski et al. 2009; Cheng et al. 2010). Zahnert and colleagues are developing a novel technique for better coupling of TORPs to the footplate using prostheses that are impregnated with compounds such as bone morphogenetic protein that induce formation of new bone (Neudert et al. 2010). Another area for future research involves development of ossicular prostheses that would “self-adjust” to changes in position of the TM and changes in static pressure within the middle ear over time, as described by Goode and colleagues (Zhao et al. 2005; Yamada and Goode 2010).
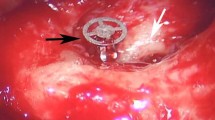
Nonaeration of the middle ear after tympanoplasty surgery is another type of problem for which optimal solutions do not exist in current otologic practice. Such nonaeration is often due to a combination of deposition of fibrous tissue and fluid related to mucosal disease and/or tubal dysfunction. Our research group has been involved in the development of a middle ear implant termed “the Boston EAiR implant” that would restore hearing in such nonaerated ears by providing a semipermanent compressible air pocket (Fig. 9.9). The EAiR implant is a small air-filled balloon with thin polymer walls. Each implant is an ovoid cylinder 3 × 2 mm in width and 5 mm in length, with a compressibility equivalent to that of an air volume of approximately 20 μL. The implant is designed for placement in the middle ear and is expected to restore hearing by introducing a compressible pocket that allows the TM, ossicles, and round window to vibrate in response to sound. A successful implant must be biocompatible (nontoxic to the tissues), bioinert (not biodegradable by the host response of the middle ear), compressible by sound vibrations, and provide a good barrier (it must be impermeable to water and body fluids and prevent loss of air from within the implant). EAiR implants meeting these criteria have been successfully developed, manufactured, and tested at a bench level. Approval from the U.S. Food and Drug Administration (FDA) to initiate prospective clinical trials is pending.
References
Bahmad, F., & Merchant, S. N. (2007). Histopathology of ossicular grafts and implants in chronic otitis media. Annals of Otology Rhinology and Laryngology, 116, 181–191.
Bance, M., Morris, D. P., & Van Wijhe, R. (2007a). Effects of ossicular prosthesis mass and section of the stapes tendon on middle ear transmission. Journal of Otolaryngology, 36, 113–119.
Bance, M., Campos, A., Wong, L., Morris, D. P., & van Wijhe, R. (2007b). How does prosthesis head size affect vibration transmission in ossiculoplasty? Otolaryngology Head and Neck Surgery, 137, 70–73.
Bohnke, F., & Arnold, W. (2007). Finite element model of the stapes-inner ear interface. Advances in Otorhinolaryngology, 65, 150–154.
Brackmann, D.E., Shelton, C., & Arriaga, M. (Eds.). (2010). Otologic Surgery, 3rd edition. Philadelphia: Saunders Elsevier.
Cheng, J. T., Aarnisalo, A. A., Harrington, E., Hernandez-Montes, M. D. S., Furlong, C., Merchant, S. N., & Rosowski, J. J. (2010). The motion of the human tympanic membrane measured with stroboscopic holography. Hearing Research, 263, 66–77.
Colletti, V., Fiorino, F. G., & Sittoni, V. (1987). Minisculptured ossicle grafts versus implants: Long term results. American Journal of Otology, 8, 553–559.
Fay, J. P., Puria, S., & Steele, C. R. (2006). The discordant eardrum. Proceedings of the National Academy of Sciences of the U S A, 103, 19743–19748.
Funnell, W. R. J., & Decraemer, W. M. (1996). On the incorporation of moiré shape measurements in finite-element models of the cat eardrum. Journal of the Acoustical Society of America, 100, 925–932.
Gan, R. Z., Dyer, R. K., Wood, M. W., & Dormer, K. J. (2001). Mass loading on the ossicles and middle ear function. Annals of Otology Rhinology and Laryngology, 110, 478–485.
Goode, R. L., & Nishihara, S. (1994). Experimental models of ossiculoplasty. In E. Monsell (Ed.), Ossiculoplasty: Otolaryngology Clinics of North America (pp. 663–675). Philadelphia: Saunders.
Goode, R. L., Friedrichs, R., & Falk, S. (1977). Effect on hearing thresholds of surgical modification of the external ear. Annals of Otology Rhinology and Laryngology, 86, 441–451.
Gyo, K., Goode, R. L., & Miller, C. (1986). Effect of middle-ear modification on umbo vibration-human temporal bone experiments with a new vibration measuring system. Archives of Otolaryngology Head and Neck Surgery, 112, 1262–1268.
Handzel, O., & McKenna, M. J. (2010). Surgery for otosclerosis. In A. J. Gulya, L. B. Minor, & D. S. Poe (Eds.), Glasscock-Shambaugh surgery of the ear, 6th edition (pp. 529–546). Shelton, CT: People’s Medical Publishing House-USA.
Honda, N., & Goode, R. L. (2004). The acoustic evaluation of stapedotomy using a temporal bone otosclerosis model. In K. Gyo, & H. Wada (Eds.), Middle ear mechanics in research and otology (pp. 203–208). Singapore: World Scientific.
Laske, R. D., Röösli, C., Chatzimichalis, M. V., Sim, J. H., & Huber, A. M. (2011). The influence of prosthesis diameter in stapes surgery: A meta-analysis and systematic review of the literature. Otology and Neurotology, 32, 520–528.
Ma, Y., Zhao, H., & Zhou X. (2002). Topical treatment with growth factors for tympanic membrane perforations: Progress towards clinical application. Acta Oto-Laryngologica, 122, 586–599.
Mehta, R. P., Ravicz, M. E., Rosowski, J. J., & Merchant, S. N. (2003). Middle-ear mechanics of type III tympanoplasty (stapes columella): I. Experimental studies. Otology and Neurotology, 24, 176–185.
Merchant, S. N. (2005). Ossiculoplasty and tympanoplasty in chronic otitis media. In J. B. Nadol & M. J. McKenna (Eds.), Surgery of the ear and temporal bone, 2nd edition (pp. 305–324). Philadelphia: Lippincott, Williams & Wilkins.
Merchant, S. N. & Nadol, J. B., Jr. (Eds.). (2010). Schuknecht’s pathology of the ear, 3rd edition. Shelton, CT: People’s Medical Publishing House-USA.
Merchant, S. N., Rosowski, J. J., & Ravicz, M. E. (1995). Middle-ear mechanics of type IV and type V tympanoplasty. II. Clinical analysis and surgical implications. American Journal of Otology, 16, 565–575.
Merchant, S. N., Rosowski, J. J, & Ravicz, M. E. (1997). Experimental investigation of the mechanics of type IV tympanoplasty. Annals of Otology Rhinology and Laryngology, 106, 49–60.
Merchant, S. N., Ravicz, M. E., Voss, S. E., Peake, W. T., & Rosowski, J. J. (1998a). Middle-ear mechanics in normal, diseased and reconstructed ears. Journal of Laryngology and Otology, 112, 715–731.
Merchant, S. N., McKenna, M. J., & Rosowski, J. J. (1998b). Current status and future challenges of tympanoplasty. European Archives of Oto-Rhino-Laryngology, 255, 221–228.
Merchant, S. N., Whittemore, K., Poon, B., Lee, C. Y., & Rosowski, J. J. (2000). Clinical measurements of tympanic membrane velocity using laser Doppler vibrometry: Preliminary results, methodological issues and potential applications. In J. J. Rosowski & S. N. Merchant (Eds.), The function and mechanics of normal, diseased and reconstructed middle ears (pp. 367–381). Amsterdam: Kugler Publications.
Merchant, S. N., Rosowski, J. J., & McKenna, M.J. (2003a). Tympanoplasty. Operative Techniques in Otolaryngology–Head and Neck Surgery, 14, 224–236.
Merchant, S. N., McKenna, M. J., Mehta, R. P., Ravicz, M. E., & Rosowski, J. J. (2003b). Middle-ear mechanics of type III tympanoplasty (stapes columella): II. Clinical studies. Otology and Neurotology, 24, 186–194.
Molvaer, O., Vallersnes, F., & Kringelbotn, M. (1978). The size of the middle ear and the mastoid air cell. Acta Oto-Larygologica, 85, 24–32.
Morris, D. P., Bance, M., van Wijhe, R. G., Kiefte, M., & Smith, R. (2004). Optimum tension for partial ossicular replacement prosthesis reconstruction in the human middle ear. Laryngoscope, 114, 305–308.
Murakami, S., Gyo, K., & Goode, R. L. (1997). Effect of middle ear pressure change on middle ear mechanics. Acta Oto-Larygologica, 117, 390–395.
Murugasu, E., Puria, S., & Roberson, J. B. (2005). Malleus-to-footplate versus malleus-to-stapes-head ossicular reconstruction prostheses: Temporal bone pressure gain measurements and clinical audiological data. Otology and Neurotology, 26, 572–582.
Nadol, J. B., & McKenna, M. J. (Eds.). (2005). Surgery of the ear and temporal bone, 2nd edition. Philadelphia: Lippincott, Williams and Wilkins.
Neudert, M., Beleites, T., Ney, M., Kluge, A., Lasurashvili, N., Bornitz, M., Scharnweber, D., & Zahnert, T. (2010). Osseointegration of titanium prostheses on the stapes footplate. Journal of the Association for Research in Otolaryngology, 11, 161–171.
Nishihara, S., & Goode, R. L. (1994). Experimental study of the acoustic properties of incus replacement prostheses in a human temporal bone model. American Journal of Otology 15, 485–494.
O’Connor, K. N., Tam, M., Blevins, N. H., & Puria, S. (2008). Tympanic membrane collagen fibers: A key to high-frequency sound conduction. Laryngoscope, 118, 483–490.
Peake, W. T., Rosowski, J. J, & Lynch, T. J. III. (1992). Middle ear transmission: Acoustic versus ossicular coupling in cat and human. Hearing Research, 57, 245–268.
Puria, S., Kunda, L. D., Roberson, J. B., & Perkins, R. C. (2005). Malleus-to-footplate ossicular reconstruction prosthesis positioning: Cochleovestibular pressure optimization. Otology and Neurotology, 26, 368–379.
Rosowski, J. J., & Merchant, S. N. (1995). A mechanical and acoustical analysis of middle-ear reconstruction. American Journal of Otology, 16, 486–497.
Rosowski, J. J, Cheng, J. T., & Ravicz, M. E., Hulli, N., Harrington, E. J., Hernandez-Montes, M. S., & Furlong, C. (2009). Computer-assisted time-averaged holography of the motion of the surface of the tympanic membrane with sound stimuli of 0.4 to 25 kHz. Hearing Research, 253, 83–96.
Sismanis, A. (2010). Tympanoplasty—tympanic membrane repair. In A. J. Gulya, L. B. Minor, & D. S. Poe (Eds.), Glasscock-Shambaugh surgery of the ear, 6th edition (pp. 465–488). Shelton, CT: People’s Medical Publishing House-USA.
Sismanis, A., & Poe, D. S. (2010). Ossicular chain reconstruction. In A. J. Gulya, L. B. Minor, & D. S. Poe (Eds.), Glasscock-Shambaugh surgery of the ear, 6th edition (pp. 489–500). Shelton, CT: People’s Medical Publishing House-USA.
Teig, E., & Lindeman, H. H. (1999). Stapedectomy piston diameter: Is bigger better? Otorhinolaryngologica Nova, 9, 252–256.
Tonndorf, J., & Khanna, S. M. (1972). Tympanic membrane vibrations in human cadaver ears studied by time-averaged holography. Journal of the Acoustical Society of America, 52, 1221–1233.
Tuck-Lee, J. P., Pinsky, P. M., Steele, C. R., & Puria, S. (2008). Finite element modeling of acousto-mechanical coupling in the cat middle ear. Journal of the Acoustical Society of America, 124, 348–362.
Vlaming, M. S. M. G., & Feenstra, L. (1986). Studies on the mechanics of the reconstructed human middle ear. Clinical Otolaryngology, 11, 411–422.
Whittemore, K. R., Merchant, S. N., & Rosowski, J. J. (1998). Acoustic mechanisms: Canal wall-up versus canal wall-down mastoidectomy. Otolaryngology Head and Neck Surgery, 118, 751–761.
Wullstein, H. (1956). The restoration of the function of the middle ear in chronic otitis media. Annals of Otology Rhinology and Laryngology, 65, 1020–1041.
Yamada, H., & Goode, R. L. (2010). A self-adjusting ossicular prosthesis containing polyurethane sponge. Otology and Neurotology, 31, 1404–1408.
Zhao, S., Hato, N., & Goode, R. L. (2005). Experimental study of an adjustable-length prosthesis in a temporal bone model. Acta Oto-Laryngologica, 125, 33–37.
Acknowledgments
This work was supported by NIH grants R01 DC 004798 and U24 DC 011943.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Merchant, S.N., Rosowski, J.J. (2013). Surgical Reconstruction and Passive Prostheses. In: Puria, S., Fay, R., Popper, A. (eds) The Middle Ear. Springer Handbook of Auditory Research. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6591-1_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6591-1_9
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6590-4
Online ISBN: 978-1-4614-6591-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)