Abstract
Among the many signaling pathways related to cancer initiation and progression, the Hippo pathway has emerged recently as a mediator of tumor suppression that is evolutionarily conserved from flies to humans and plays a key role in normal organ development. Genetic engineering of the Hippo pathway in mice has provided important insights into its tumor suppression function. These mouse models have also revealed both canonical and noncanonical modes of action for pathway components in tumor suppression. In this chapter, we first discuss genetic and epigenetic changes identified for Hippo pathway components in human cancers. We then describe established mouse models of cancer related to the Hippo pathway, dividing them into those in which the canonical pathway functions through inhibition of the transcriptional co-activator YAP and those in which noncanonical functions of individual pathway components contribute to tumor suppression.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Canonical Hippo pathway
- Noncanonical Hippo pathway
- liver cancer
- Oval cell
- Intestine cancer
- Tissue regeneration
- Lymphoma
- Genomic instability
1 Introduction
Cancer develops as a result of dysregulation of multiple genes and associated signaling pathways. The accumulation of genetic and epigenetic changes that favor uncontrolled cell proliferation and spread is the driving force that advances tumor development, from initial tumor formation to escape from surrounding local tissue, angiogenesis, and the acquisition of resistance to detrimental elements of the tumor environment such as anticancer agents (Hanahan and Weinberg 2000, 2011). It is thus important to characterize these changes for all stages of cancer development and for all types of cancer.
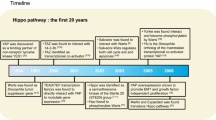
The Hippo signaling pathway, first discovered a decade ago by genetic screening in Drosophila (Saucedo and Edgar 2007; Harvey and Tapon 2007; Zhao et al. 2010a), has recently been found to mediate tumor suppression in mammals. The molecular roles of this signaling pathway have been described in detail in other chapters of this book. According to the current simplified model, upstream components of the Hippo pathway include Kibra, Merlin, and Expanded. The core complex of the pathway consists of the protein kinase Hippo (MST1 and MST2 in mammals), Salvador (SAV1 or WW45 in mammals), Mats (MOB1 in mammals), and the protein kinase Warts (LATS1 and LATS2 in mammals). On activation by unknown signals, Hippo phosphorylates and thereby activates Warts with the help of Salvador. Mats binds to Warts and enhances its kinase activity. Activated Warts, in turn, phosphorylates and inactivates the transcriptional co-activator Yorkie (YAP and TAZ in mammals). The mammalian counterparts of the Hippo signaling pathway in Drosophila are both molecularly and functionally well conserved.
2 Dysregulation of Hippo Pathway Components in Human Cancer
Inactivation or reduced expression of upstream regulators of YAP has been identified in human cancers, as has activation of YAP. Hippo pathway components whose expression has been found to be dysregulated in human cancers and the mechanistic basis for such altered expression are summarized in Table 11.1.
The gene for NF2 (Merlin) is the most frequently mutated of the genes for Hippo pathway components. It is thus mutated in individuals with familial neurofibromatosis type 2 (NF2) (Trofatter et al. 1993), which is characterized by the development of multiple tumors of the nervous system such as schwannoma, meningioma, and ependymoma. Mutations in NF2 often result in the generation of truncated proteins, although several missense mutations have been associated with less aggressive forms of the disease (Ahronowitz et al. 2007; Baser 2006). NF2 mutations have also been found in sporadic neuronal tumors. Importantly, both familial and sporadic cancers manifest loss of heterozygosity (LOH) for NF2, which is often seen with tumor suppressor genes, therefore suggesting that NF2 is indeed an authentic tumor suppressor. Epigenetic changes for NF2 have not been detected in human tumors to date. Direct mutation therefore appears to be the major mechanism for disruption of NF2 function in cancer. In addition to neuronal tumors, a high frequency of NF2 mutations has been detected in mesothelioma, a metastatic type of cancer originating from epithelial cells that line the abdominal cavity (Bianchi et al. 1995).
Mutational inactivation of MST1 or MST2 has not been identified to date in human cancer, possibly because their functional redundancy would necessitate disruption of both genes. Indeed, Mst1-null and Mst2-null mice are viable, appear to develop normally, and rarely manifest spontaneous tumors, indicative of the functional redundancy of the two proteins (Oh et al. 2009; Zhou et al. 2009). It is therefore unlikely that mutational inactivation of both MST1 and MST2 would serve as the initiating lesion for tumorigenesis. Nevertheless, reduced expression of MST1 and MST2 may promote tumor progression, as suggested by the frequent methylation of both gene promoters in soft tissue sarcoma (Seidel et al. 2007).
The promoters of LATS1 and LATS2 also undergo extensive methylation in various types of cancer. In the case of T-cell acute lymphoblastic leukemia (T-ALL), breast cancer, and astrocytoma, more than 50 % of tumors manifest LATS1 or LATS2 promoter methylation (Jimenez-Velasco et al. 2005; Morinaga et al. 2000; Jiang et al. 2006), with the extent of methylation correlating negatively with LATS1/2 expression and prognosis. Of note, LOH at chromosome 13q12, a locus that includes LATS2, has also been detected in T-ALL (3–6 %), lung cancer (67 %), mesothelioma, and cancers of the liver and ovary (Jimenez-Velasco et al. 2005; Yokota et al. 1987; De Rienzo et al. 2000). Rare inactivating mutations of LATS2 have also been identified in lung cancer and mesothelioma (Strazisar et al. 2009; Murakami et al. 2011). The fact that loss of LATS1 or LATS2 expression (or both) is frequently observed in human tumors suggests that the two proteins may perform distinct tumor suppressor functions in different contexts. Indeed, in contrast to Mst1 and Mst2 single-knockout mice, Lats1 and Lats2 single-knockout mice have distinct phenotypes characterized by the spontaneous formation of soft tissue sarcomas and embryonic lethality, respectively (St John et al. 1999; McPherson et al. 2004).
YAP and TAZ are the main downstream targets of the Hippo pathway in mammals and function as oncogenic proteins. Both YAP and TAZ are inactivated as a result of LATS-mediated phosphorylation, leading to their cytoplasmic sequestration or degradation (Zhao et al. 2010b; Dong et al. 2007; Lee et al. 2008). However, no activating missense mutations of YAP or TAZ have been identified in human cancer to date. Instead, the activity of YAP is increased as a result of its increased expression and nuclear localization in certain cancers. For example, amplification of chromosome 11q22, which harbors the genes for YAP and the anti-apoptotic protein cIAP1, has been detected in 5–10 % of glioblastomas, oral squamous cell carcinomas, mesotheliomas, and cancers of the cervix, pancreas, breast, lung, and liver (Baldwin et al. 2005; Li et al. 2012; Hermsen et al. 2005; Imoto et al. 2001, 2002; Snijders et al. 2005; Weber et al. 1996). Moreover, immunohistochemical studies indicate that overexpression of YAP or TAZ occurs in a much higher proportion of tumors (Zhao et al. 2007). Amplification of the 11q22 locus may thus account for YAP activation in only a subset of tumors, with other mechanisms of YAP accumulation, such as those mediated at the transcriptional or translational level, waiting to be identified.
3 Tumor Suppression by the Canonical Hippo Pathway in Mouse Models
Among the first mouse models to suggest the importance of the Hippo pathway in cancer were YAP transgenic mice generated by two independent groups (Dong et al. 2007; Camargo et al. 2007). These transgenic mice provided insight into two in vivo functions of the Hippo pathway in mammals: (1) Control of organ size. The two groups thus both found a marked increase in organ size in the transgenic animals. The size of the liver returned to normal when expression of the YAP transgene was eliminated. (2) Control of stem or progenitor cell proliferation and differentiation. The size of stem/progenitor cell compartments in various organs including the intestine and skin was thus increased in YAP transgenic mice, suggesting that the Hippo pathway limits stem or progenitor cell proliferation and promotes cell differentiation (Camargo et al. 2007; Schlegelmilch et al. 2011).
Subsequent studies focused on the precise roles of individual Hippo pathway components with regard to these two functions. Knockout mice with mutations in the genes for each component have thus been generated (Oh et al. 2009; McPherson et al. 2004; Lee et al. 2008; McClatchey et al. 1997). However, embryonic mortality of mice lacking Nf2, Sav1, Lats2, or both Mst1 and Mst2 has hampered investigations into the roles of the Hippo pathway in tumorigenesis. Tissue-specific knockout mice have been generated to overcome such mortality. Studies that have linked loss of Hippo signaling to liver, intestinal, and other types of cancer will be discussed.
3.1 The Hippo Pathway in Liver Cancer
The liver serves as an ideal system for studies of the control of organ size. Each individual maintains a constant size of the liver; even after severe insults such as partial hepatectomy of up to two-thirds of the tissue, the liver undergoes rapid regeneration to regain its original size. This unique feature of the liver has prompted many studies into the potential role of the Hippo pathway in this organ.
The mammalian liver is composed of two major differentiated cell types: hepatocytes and cholangiocytes (Roskams 2006). In a typical epithelial tissue, increased proliferation of stem or progenitor cells (but not of differentiated cells) is largely responsible for tissue regeneration associated with the replacement of old or damaged cells. In contrast, even though hepatocytes usually remain quiescent and rarely divide under normal conditions, they are able to undergo massive proliferation to replace damaged cells after extensive tissue injury. Only if replication of hepatocytes is blocked by hepatotoxins or if the extent of tissue damage exceeds the regenerative capacity of these cells do hepatic stem/progenitor cells, the so-called oval cells, become activated and divide to give rise to both hepatocytes and cholangiocytes. Oval cells normally reside in peripheral regions of the biliary tree known as the canals of Hering, and they rarely proliferate in the absence of severe liver damage. Importantly, many risk factors for human liver cancer, including infection with hepatitis B or C viruses as well as alcoholic or nonalcoholic steatohepatitis, can lead to oval cell activation, suggesting that oval cells are a candidate cell-of-origin for some liver cancers (Roskams 2006; Farazi and DePinho 2006).
The two most common types of liver cancer are hepatocellular carcinoma (HCC) and cholangiocarcinoma (CC). A mixed type (having both HCC and CC characteristics) and an intermediate type (having ill-defined characteristics) of liver cancer also exist and are thought to originate from liver stem/progenitor cells. Some individuals with HCC also have transformed hepatocytes that express classic oval cell markers such as CK19, with such expression correlating with poor prognosis, suggesting that these cancers could originate from either oval cells or dedifferentiated transformed hepatocytes.
The Hippo pathway was first implicated in liver cancer by an unbiased genome-wide screen for new cancer genes (Zender et al. 2006). In this study, combinations of human oncogenes were introduced into hepatoblasts isolated from mouse embryos and the cells were then transplanted into the liver of normal mice. The locus including the Yap and cIAP1 genes was found to be recurrently amplified in tumors induced by the c-MYC oncogene. This locus is syntenic to human chromosome 11q22, which is also amplified in a subset of human cancers (as described above). Transgenic mice that overexpress YAP specifically in the liver were subsequently found to develop hepatomegaly followed by HCC (Dong et al. 2007; Camargo et al. 2007). These studies thus provided direct evidence for an oncogenic function of YAP in the liver. In addition, recurrent amplification of the genomic locus containing Yap was identified in breast tumors of Brca1 +/−;p53 +/− mice, providing further support for such a function of YAP in another system (Overholtzer et al. 2006).
Can ablation of upstream negative regulators of YAP also induce liver cancer in the absence of exogenous YAP? So far, the genes for Nf2, Sav1, and both Mst1 and Mst2 have been deleted in the liver to address this question (Zhou et al. 2009; Zhang et al. 2010; Benhamouche et al. 2010; Lee et al. 2010; Song et al. 2010; Lu et al. 2010). All three mouse strains exhibited hepatomegaly and ultimately developed liver cancer with a time course similar to or slower than that for liver-specific YAP transgenic mice. The extent of Yap phosphorylation in the liver was markedly reduced in these models, and, as a result, Yap accumulated to high levels in the nucleus. Importantly, deletion of one allele of Yap in mice lacking Nf2 in the liver abolished hepatomegaly and tumor formation (Zhang et al. 2010). Control mice with only one Yap allele showed no defect in liver development or homeostasis. Similarly, growth of HCC cell lines derived from mice lacking both Mst1 and Mst2 in the liver was also inhibited by knockdown of Yap (Zhou et al. 2009). These genetic studies thus demonstrated that inactivation of upstream components of the Hippo pathway can initiate liver tumorigenesis via YAP activation.
Ablation of Nf2 or Sav1 specifically in the liver resulted in the selective overproliferation of immature cells that were likely oval cells, without any marked effect on differentiated hepatocytes (Benhamouche et al. 2010; Lee et al. 2010). Oval cell hyperplasia is also induced by hepatocyte damage, but the knockout mice exhibited no apparent defects in hepatocytes, suggesting that the oval cell proliferation in these animals was not due to liver damage. The liver tumors that developed in these Nf2- or Sav1-deficient mice with age were the mixed type, with characteristics of both HCC and CC. In recent, however, many more analysis of the liver tumors derived from Sav1-deficient mice had let us notice that Sav1-null mice also frequently developed only HCC with some progenitor expansion (T.-S.K. and D.-S.L., personal observation). Nonetheless, these findings, together with the preceding oval cell hyperplasia, suggested that the tumors could be derived from oval cells. NF2 and SAV1 in the Hippo pathway thus appear to inhibit liver tumorigenesis by restricting liver stem/progenitor cell proliferation.
The liver-specific Nf2-null and Sav1-null mice have also provided evidence that liver damage is linked to tumorigenesis through oval cell activation. Oval cell activation in these mice was thus enhanced further by hepatocyte damage induced either by a diet containing the hepatotoxin 3,5-diethoxycarbonyl-1,4-dihydrocollidine (DDC) or by partial hepatectomy. Liver-specific Sav1 knockout mice thus responded to short-term consumption of a DDC diet with excessive oval cell expansion. More dramatic results were obtained with Nf2 knockout mice. When deletion of Nf2 in the liver was induced postnatally by injection of an adenoviral vector for Cre recombinase or by interferon-driven Cre expression, only mild periportal hyperplasia ensued and macroscopic tumors did not develop. These findings thus contrasted with the pronounced oval cell hyperplasia and subsequent tumor development observed in the mice in which Nf2 was deleted during early liver development in embryos as a result of Cre expression controlled by the albumin gene promoter. However, surgical removal of two-thirds of the liver to induce liver regeneration in the two former mouse models resulted in marked overproliferation of oval cells and development of mixed HCC-CC tumors, as observed in the albumin-Cre model without hepatectomy. The acceleration of tumor development by regenerative stimuli thus again highlighted the importance of regulation of liver stem/progenitor cells by the Hippo pathway. Moreover, these findings are also clinically relevant given that, as mentioned above, risk factors for liver cancer in humans (hepatitis B or C virus infection, steatohepatitis) are linked to chronic liver damage or inflammation and ultimately to oval cell activation (Roskams 2006; Farazi and DePinho 2006). Although oval cell reactions are observed in some human liver tumors, few animal models have been available to examine their impact on actual tumorigenesis. Liver-specific Nf2 or Sav1 knockout mice thus represent important tools to study the role of oval cells in liver cancer.
Deletion of Mst1 and Mst2 in the liver also led to tumor formation (Zhou et al. 2009; Song et al. 2010; Lu et al. 2010), which was more rapid than that in liver-specific Nf2 or Sav1 knockout mice (Fig. 11.1). Strikingly, unlike these latter mice, most liver tumors formed in mice with only one copy of Mst1 or Mst2 were classified as HCC, with only a minor fraction being classified as CC or mixed HCC-CC. Complete inactivation of Mst1 and Mst2 by expression of Cre recombinase under the control of the albumin gene promoter resulted in overproliferation of both hepatocytes and oval cells followed by the development of large liver tumors. Again, most of these tumors exhibited histological characteristics of HCC, with a smaller proportion of mixed HCC-CC tumors also being detected. These Mst1/2 knockout mice also appeared to have liver damage, as evidenced by high levels of alanine and aspartate aminotransferases in their serum and inflammatory gene expression profile in their liver (Song et al. 2010; Lu et al. 2010). This liver damage might explain why tumor initiation in these Mst1/2 knockout mice was more rapid than that in Sav1 knockout mice. These observations suggested that, unlike NF2 and SAV1, MST1 and MST2 function as potent tumor suppressors in the hepatocyte compartment. Although it remains possible that MST1 and MST2 regulate oval cell homeostasis, liver damage or inflammation in animals with liver-specific ablation of these proteins may also contribute to and accelerate liver tumorigenesis. Notably, Mst1- and Mst2-deficient hepatocytes showed a markedly reduced level of Yap phosphorylation on serine-127, the residue targeted by Lats1/2 kinases, likely resulting in up-regulation of Yap’s oncogenic activity. Whereas Yap’s transgenic mice develop HCC, whether these animals also show expansion of the oval cell compartment has not been described (Dong et al. 2007; Camargo et al. 2007). In the future, it will be important to determine the relative contributions of hepatocytes and oval cells to liver tumorigenesis in liver-specific Mst1 and Mst2 double-knockout mice.
Liver cancer in albumin Cre; Mst1flox/flox; Mst2−/− mice. H&E-stained liver sections from the mice deficient for liver Mst1 and Mst2. Liver-specific gene deletion was achieved by mating with albumin-Cre transgenic mice. (a) A picture of liver from 9-week-old knockout mice showing abnormal architecture with increased progenitor-like cells around portal triads. (b) A representative picture of an HCC node developed in 6-month-old knockout mice. The progenitor-like cells were set aside the tumor node. (c) High magnification view of (b). Scale bars indicate 500 μm for (a) and (b), and 200 μm for (c)
3.2 The Hippo Pathway in Intestinal Cancer
The intestine harbors relatively well-characterized stem cells, which are located at the base of intestinal crypts and turn over rapidly to compensate for the abrasion-induced loss of epithelial cells in the lumen and thereby maintain homeostasis (van der Flier and Clevers 2009). YAP transgenic mice rapidly develop severe intestinal dysplasia with the near complete loss of differentiated cells (Camargo et al. 2007), whereas systematic Sav1 knockout embryos exhibit expansion of progenitors and defects in cell differentiation in the intestine (Lee et al. 2008). These observations implicate the Hippo pathway in intestinal stem cell regulation and intestinal cancer.
Conditional knockout mice lacking Mst1 and Mst2 in the intestine manifest a phenotype essentially corresponding to that of the liver-specific double-knockout mice (Zhou et al. 2011). Similar to the effects of YAP overexpression, deletion of Mst1 and Mst2 in the intestinal epithelium thus induced enlargement of crypts in the small intestine and dysplasia of the colon (Fig. 11.2). At the molecular level, both Wnt and Notch signaling pathways (which drive proliferation of stem and progenitor cells, respectively) were activated in the intestine of these mice. The expansion of stem and progenitor cell compartments was accompanied by a marked reduction in the number of differentiated cells in the intestine of the mutant animals. The extent of Yap phosphorylation was also reduced in association with the nuclear accumulation of Yap in intestinal cells of the double-mutant mice. Furthermore, deletion of one Yap allele in these animals rescued the cell proliferation–differentiation phenotype, confirming the role for the canonical Hippo pathway in stem-progenitor cell regulation.
Small and large intestine in Villin Cre; mice; Mst1flox/flox; Mst2−/− mice. H&E-stained colon and small intestine sections from the mice deficient for intestine Mst1 and Mst2. Intestine-specific gene deletion was achieved by mating with Villin-Cre transgenic mice. (a–c) Adenomas developed in 2-week-old Mst1/2 intestine-specific knockout mice. (a) Polyp type adenoma formed in colon of Villin Cre; Mice; Mst1flox/flox; Mst2−/− mouse. The enlarged image of inset is shown in (c), an aggressive part with high proliferation at the base and loss of differentiated cells. Right part of the polyp is relatively less transformed, which maintains differentiated villi structure. (b) Flat type adenoma formed. Dashed line indicates regions maintaining normal architecture of the colon. Left to the indicate region, the normal columnar architecture of colon is lost, accompanied by proliferation at the base and loss of differentiated goblet cells. (d, e) Small intestine of control (d) and Villin Cre; Mice; Mst1flox/flox; Mst2−/− mouse (e) at 2-weeks of age. The small intestine maintains normal architecture at this age. However, the size of the crypt compartments, which contains the stem/progenitor cells, is extremely enlarged in Villin Cre; Mice; Mst1flox/flox; Mst2−/− mouse
In contrast to Mst1/2 deletion, deletion of Sav1 in the intestine had no impact on intestinal homeostasis, with the exception that aged mice developed mild hyperplasia in the colon (Cai et al. 2010). However, treatment of these Sav1-deficient mice with dextran sulfate sodium (DSS), which damages the colonic epithelium, resulted in an exaggerated regenerative response and subsequent polyp formation. Again, deletion of one Yap allele abolished this hyper-regenerative response. DSS treatment in the wild-type mice also resulted in the rapid accumulation of Yap in the intestinal epithelium followed by normalization of Yap expression as regeneration was completed. This finding suggests that YAP contributes to the regenerative response to tissue damage. Furthermore, the absence of SAV1 or of MST1/2 likely results in the constitutive activation of YAP, which leads to continuous tissue regeneration and the consequent development of hyperplasia and cancer. The central role of YAP in intestinal regeneration was confirmed by the production of mice lacking Yap in the intestine, which failed to replace damaged tissue and died soon after DSS treatment (Cai et al. 2010). Of note, these animals showed no developmental defects in the intestine, indicating that YAP is dispensable for intestinal development but indispensable for regeneration of the intestine after injury.
4 Tumor Suppression by Noncanonical Functions of Hippo Pathway Components
4.1 Role of the MST1-SAV1-NDR1 Signaling Axis in Maintenance of Genomic Stability
In addition to their role in regulation of cell proliferation and differentiation through YAP, the core Hippo pathway components are implicated in regulation of the cell cycle. The LATS-MOB1 complex thus has an evolutionarily conserved role in mitotic exit and centrosome maintenance (Bothos et al. 2005; Brace et al. 2011). Recent studies also indicate that the MST1-SAV1-NDR1 axis performs multiple cell cycle functions. The protein kinase NDR1 is a paralog of LATS1/2, and MST1-NDR1 signaling promotes stable kinetochore-microtubule attachment by restraining Aurora B activity and centrosome duplication, whereas the MST1-SAV1 complex regulates centrosome disjunction via Nek2A (Oh et al. 2010; Hergovich et al. 2009; Mardin et al. 2010). Defects in any of these cell cycle events ultimately lead to incorrect chromosome segregation to daughter cells and aneuploidy. Although still controversial, increasing evidence suggests that aneuploidy and chromosomal instability contribute to tumor initiation and progression (Kops et al. 2005). Analysis of the hematopoietic system of Mst1-null mice has provided support for MST1 function in maintenance of chromosome integrity. These mice were thus found to be highly susceptible to the development of N-ethyl-N-nitrosourea (ENU)-induced T-ALL (Kim et al. 2012). Interestingly, Mst1-deficient lymphocytes from these mice showed a normal proliferation rate and susceptibility to pro-apoptotic stimuli. Moreover, Mst1 deficiency did not affect mouse lymphocyte developmental programs, even though naïve mouse Mst1-null T cells or human MST1-null lymphocytes undergo spontaneous apoptosis (Choi et al. 2009; Nehme et al. 2012). Rather, mouse Mst1-deficient lymphocytes manifested an increased frequency of abnormal mitosis and genomic instability, and ENU-induced lymphomas in Mst1-null mice therefore also exhibited a high incidence of genomic instability. Most Mst1-null lymphocytes that undergo abnormal mitosis would be expected to be eliminated as a result of activation of the p53-dependent cell death pathway. Consistent with this notion, Mst1 deficiency and p53 deletion induced a markedly synergistic increase in the incidence of T cell lymphoma.
Ndr1 knockout mice, similar to Mst1 knockout mice, show an increased susceptibility to ENU-induced lymphoma (Cornils et al. 2010). Although ablation of Ndr1 conferred a subtle protection from apoptosis, defective mitosis in lymphocytes is likely to contribute to the increased tumor incidence in this model. In this regard, whereas overexpression of either wild-type or a constitutively active form of YAP in epithelial tissues resulted in tumor development, that in the hematopoietic system had no apparent effect on the size, proliferation, or differentiation of the stem cell population (Jansson and Larsson 2012). The MST1-NDR1 axis thus appears to execute a tumor suppressor function independent of YAP in the hematopoietic system.
Like their paralog NDR1, LATS1 and LATS2 play an essential role during mitosis. Lats2-deficient mouse embryonic fibroblasts are characterized by cytokinesis failure, increased ploidy, and an accelerated exit from mitosis (McPherson et al. 2004). The rapid proliferation of these cells likely contributes to the generation of progeny with abnormal ploidy. The failure of cytokinesis and increased proliferation rate are even more pronounced in Lats1/2 double-knockout cells (M.-C.K. and D.-S.L, unpublished data). It remains to be determined whether Lats1 and Lats2 single-knockout or Lats1/2 double-knockout mice manifest an increased frequency of aneuploidy, and if so whether such aneuploidy might contribute to tumorigenesis. Furthermore, determination of the relative contributions of two different outcomes of Lats1/2 deletion—mitosis failure and YAP activation—to tumorigenesis in vivo will be important for a full understanding of the tumor suppressor function of LATS.
4.2 Other Knockout Mouse Models of Cancer
Even though NF2 acts as a classic tumor suppressor gene, such a role has not yet been linked to the Hippo pathway in certain tissues. For example, Nf2 heterozygous mice show an increased susceptibility to asbestos-induced mesothelioma (Fleury-Feith et al. 2003). It is possible that dysregulation of the Hippo pathway is responsible for this sensitivity, given that mutations in various Hippo pathway components are associated with mesothelioma. In human mesothelioma, NF2 mutation, 13q12 deletion, or one of several inactivating mutations of LATS2, or 11q22 amplification and associated YAP activation are found (Murakami et al. 2011; Bianchi et al. 1995; Thurneysen et al. 2009; Mizuno et al. 2012). In vitro studies indicate that reconstitution of the canonical Hippo pathway suppresses the tumorigenic potential of mesothelioma cell lines harboring mutations in Hippo pathway components (Mizuno et al. 2012). The generation of mouse models of mesothelioma with mutations of Hippo pathway components should provide insight into the tumor suppressor function of this pathway in mesothelioma development.
Mice lacking Nf2 in the intestine and kidney have been generated by expression of Cre recombinase under the control of the Villin gene promoter. However, these animals were found to develop only renal cell carcinoma (Morris and McClatchey 2009). It will be of interest to examine further whether Nf2 deletion in the intestine has any impact on intestinal homeostasis and tissue regeneration after injury.
Additional mouse models with genetic modification of Hippo pathway components and their phenotypes are listed in Table 11.2. Many such models develop various tumors, the mechanisms of which require further clarification. For example, Lats1 knockout mice develop soft tissue sarcomas with a high penetrance as well as ovarian stromal cell tumors (St John et al. 1999). RASSF family proteins, putative activators or inhibitors of MST, also serve as tumor suppressors. Rassf1A-null mice develop various tumors including lung adenoma, lymphoma, and breast adenocarcinoma at advanced ages (Tommasi et al. 2005; van der Weyden et al. 2005), whereas Rassf5-null mice did not show any substantial increase in the frequency of spontaneous tumor development (Park et al. 2010). The mechanisms underlying tumorigenesis in these RASSF knockout mice, including whether it depends on YAP or TAZ, await further investigation.
5 Future Directions
The establishment of various mouse models with genetic modifications of the Hippo pathway has revealed that the pathway exerts tumor suppressor activity through inhibition of YAP as well as that pathway components exert such activity independently of YAP, as in the maintenance of genomic integrity by the MST1-SAV1-NDR1 axis. We have focused mostly on models of liver/intestine cancer and lymphoma, respectively, in our discussion of these canonical and noncanonical roles of Hippo pathway components.
The first decade of research into the Hippo pathway has yielded many mechanistic and genetic insights. However, analysis of the role of Hippo pathway components in many genetic models of cancer, especially liver cancer, has led us to as many questions as answers. Characterization of the tumor suppressor role of Hippo pathway components in vitro has complemented the work with mouse models of cancer in vivo. We envision two key directions for future research into the role of the Hippo pathway in cancer development: (1) refinement of mouse models of cancer, and (2) discovery of novel mechanisms of tumor suppression by Hippo pathway components in vivo.
5.1 Refinement of Mouse Models of Cancer
Although mice deficient in individual Hippo pathway components, together with YAP transgenic mice, have been invaluable for modeling Hippo pathway dysregulation in human cancer, these mice have limitations that necessitate further refinement of the models to render them more clinically relevant. For example, in human cancer, the YAP locus is amplified as part of the 11q22 amplicon. This amplicon contains another putative oncogene, that for cIAP1, which has been suggested to have a synergistic effect with YAP in tumorigenesis. The accuracy of the YAP transgenic model would thus be increased by adjustment of the expression of other genes located in the 11q22 amplicon in addition to YAP to levels similar to those observed in human tumors with this amplicon. Activation of YAP or ablation of upstream regulators in a target tissue in a chimeric manner would also provide a more accurate model of human cancer, given that most such changes occur postnatally and in only a few cells within a tissue. Such models would also allow analysis of communication between mutant cells and surrounding normal cells. In addition, it will be important to examine whether Lats2 deletion in mice can initiate tumorigenesis in organs in which 13q22 LOH is found in humans.
In addition to modeling the genetic alterations associated with human cancer, it should prove valuable to examine the role of the Hippo pathway in clinically relevant cancer-predisposing conditions. The finding that dysregulation of the Hippo pathway induces oval cell activation provides an opportunity to examine this issue in the liver. Given that most of the agents known to cause liver cancer induce oval cell activation and that the extent of this response is predictive of disease outcome, it will be of interest to establish mouse models that mimic tumor-promoting situations and then to test the role of the Hippo pathway.
5.2 Discovery of Novel Mechanisms of Tumor Suppression In Vivo
Liver cancer models with genetic alterations of the Hippo pathway have shown mechanistically and histologically distinct phenotypes. Deletion of Nf2 generated mixed-type tumors with both HCC and CC characteristics. Also, deletion of Sav1 generated either mixed-type HCC-CC or HCC with less expansion of progenitor cells, whereas deletion of Mst1 and Mst2 generated mainly HCC with more expansion of progenitor cells. These observations suggest that these genes differ in their actions in different cell lineages. A more thorough examination of the various knockout mice, together with specific ablation of Hippo pathway components in specific cell lineages (such as differentiated hepatocytes or oval cells), may provide an explanation for this difference. As described above, unlike deletion of Sav1 or Nf2, the deletion of Mst1 and Mst2 appears to induce liver damage. Given that most human HCC tumors are thought to develop subsequent to liver damage or chronic inflammation, it will be of interest to test whether or how liver damage and inflammation accelerate HCC development in Mst1/2-null mice.
Apoptosis and senescence are the two principal mechanisms of cellular protection against tumorigenesis (Hanahan and Weinberg 2000). Excessive oncogenic signaling such as that mediated by RAS induces senescence (permanent withdrawal from the cell cycle) in otherwise normal cells, and many studies have implicated senescence as a critical tumor suppression mechanism in both human cancers and mouse models (Collado et al. 2005; Braig et al. 2005). Disruption of the senescence pathway often triggers tumor development in cancer models such as those based on RAS activation or loss of the tumor suppressor PTEN (Sarkisian et al. 2007; Chen et al. 2005). Studies have suggested a role for LATS1/2 in the promotion of senescence. LATS2 is thus a target of the oncogenic microRNAs miR372 and miR373, which allow cells to bypass oncogene-induced senescence (Voorhoeve et al. 2006). LATS2 has also been shown to be important for the inhibition of cell proliferation and the induction of senescence markers by the retinoblastoma protein (pRB) (Tschop et al. 2011), and partial ablation of LATS2 suppressed pRB-dependent induction of senescence markers. It will therefore be important to generate Lats1 and Lats2 knockout models in order to test whether senescence mediated by these kinases contributes to their tumor suppressor functions in vivo.
Mice with genetic disruption of the Hippo pathway manifest two key features: expansion of tissue-specific stem or progenitor cell populations, and a hyper-regenerative response and increased cancer incidence after tissue damage. These phenotypes appear to result from YAP activation, given that deletion of one Yap allele can prevent their development. These findings highlight the functions of YAP in stem/progenitor cell proliferation and survival and in tissue regeneration. Which target genes of YAP are responsible for these functions? The functional importance of YAP target genes such as those for connective tissue growth factor (CTGF), cysteine-rich angiogenic inducer 61 (CYR61), and amphiregulin has been demonstrated in vitro (Zhang et al. 2009, 2011). The importance of these downstream targets and partners of YAP in the Hippo pathway has not been examined with regard to carcinogenesis in vivo, however. Future studies to validate the functions of YAP or TAZ target genes and to identify the transcriptional machinery engaged by these proteins are warranted. Given that inhibition of the epidermal growth factor receptor (EGFR), similar to Yap deletion, has been shown to abolish the phenotype associated with NF2 loss (Benhamouche et al. 2010), the mechanism by which the activities of EGFR and YAP might be linked is also worthy of investigation. In addition, the substrates of MST1/2 and LATS1/2 that contribute to the noncanonical functions suggested for these kinases need to be identified and characterized.
Characterization of crosstalk between the Hippo pathway and other cancer-related or developmental pathways will also be important. In vitro studies have implicated YAP and TAZ in diverse developmental pathways such as those mediated by transforming growth factor-β and Smad, by Sonic Hedgehog, or by Wnt and β-catenin (Varelas et al. 2008; Alarcon et al. 2009; Fernandez et al. 2009; Heallen et al. 2011). Systematic analysis of the requirement for YAP or TAZ and for loss of Hippo pathway components in various cancer models will be necessary to examine the role of such cross talk in vivo.
Finally, upstream activating cues for the Hippo pathway in vivo need to be characterized. Studies to date suggest that, unlike other developmental pathways, the Hippo pathway is activated by mechanical cues rather than by soluble factors (Dupont et al. 2011; Schroeder and Halder 2012). This notion, together with the universal effect of disruption of the Hippo pathway on stem or progenitor cell populations, suggests the possible existence of a “physical niche” for such cells. Mechanical forces have been shown to control developmental programs and homeostasis in lower organisms such as Drosophila and Xenopus (Wozniak and Chen 2009). However, this concept has rarely been tested in higher organisms. Identification of the nature of the niche signals that activate the Hippo pathway in stem or progenitor cells will provide insight into how this pathway restricts the proliferation of these cells.
The Hippo pathway has attracted the attention of many scientists over the course of the last decade. The relevance of this pathway to tumor suppression in vivo has only just begun to emerge. Examination of the importance of the Hippo pathway in more clinically relevant settings, together with refinement and expansion of the mechanistic details of this pathway in mammals, is expected to highlight its conserved central role in tumor suppression from flies to humans over the next decade.
References
Ahronowitz I, Xin W, Kiely R, Sims K, MacCollin M, Nunes FP. Mutational spectrum of the NF2 gene: a meta-analysis of 12 years of research and diagnostic laboratory findings. Hum Mutat. 2007;28(1):1–12.
Alarcon C, Zaromytidou AI, Xi Q, Gao S, Yu J, Fujisawa S, et al. Nuclear CDKs drive Smad transcriptional activation and turnover in BMP and TGF-beta pathways. Cell. 2009;139(4):757–69.
Baldwin C, Garnis C, Zhang LW, Rosin MP, Lam WL. Multiple microalterations detected at high frequency in oral cancer. Cancer Res. 2005;65(17):7561–7.
Baser ME. The distribution of constitutional and somatic mutations in the neurofibromatosis 2 gene. Hum Mutat. 2006;27(4):297–306.
Benhamouche S, Curto M, Saotome I, Gladden AB, Liu CH, Giovannini M, et al. Nf2/Merlin controls progenitor homeostasis and tumorigenesis in the liver. Genes Dev. 2010;24(16):1718–30.
Bianchi AB, Mitsunaga SI, Cheng JQ, Klein WM, Jhanwar SC, Seizinger B, et al. High frequency of inactivating mutations in the neurofibromatosis type 2 gene (NF2) in primary malignant mesotheliomas. Proc Natl Acad Sci U S A. 1995;92(24):10854–8.
Bothos J, Tuttle RL, Ottey M, Luca FC, Halazonetis TD. Human LATS1 is a mitotic exit network kinase. Cancer Res. 2005;65(15):6568–75.
Brace J, Hsu J, Weiss EL. Mitotic exit control of the Saccharomyces cerevisiae Ndr/LATS kinase Cbk1 regulates daughter cell separation after cytokinesis. Mol Cell Biol. 2011;31(4):721–35.
Braig M, Lee S, Loddenkemper C, Rudolph C, Peters AHFM, Schlegelberger B, et al. Oncogene-induced senescence as an initial barrier in lymphoma development. Nature. 2005;436(7051):660–5.
Cai J, Zhang N, Zheng Y, de Wilde RF, Maitra A, Pan D. The Hippo signaling pathway restricts the oncogenic potential of an intestinal regeneration program. Genes Dev. 2010;24(21):2383–8.
Camargo FD, Gokhale S, Johnnidis JB, Fu D, Bell GW, Jaenisch R, et al. YAP1 increases organ size and expands undifferentiated progenitor cells. Curr Biol. 2007;17(23):2054–60.
Chen ZB, Trotman LC, Shaffer D, Lin HK, Dotan ZA, Niki M, et al. Crucial role of p53-dependent cellular senescence in suppression of Pten-deficient tumorigenesis. Nature. 2005;436(7051):725–30.
Choi J, Oh S, Lee D, Oh HJ, Park JY, Lee SB, et al. Mst1-FoxO signaling protects naive T lymphocytes from cellular oxidative stress in mice. PLoS One. 2009;4(11):e8011.
Collado M, Gil J, Efeyan A, Guerra C, Schuhmacher AJ, Barradas M, et al. Tumour biology: senescence in premalignant tumours. Nature. 2005;436(7051):642.
Cornils H, Stegert MR, Hergovich A, Hynx D, Schmitz D, Dirnhofer S, et al. Ablation of the kinase NDR1 predisposes mice to the development of T cell lymphoma. Sci Signal. 2010;3(126):ra47.
De Rienzo A, Jhanwar SC, Testa JR. Loss of heterozygosity analysis of 13q and 14q in human malignant mesothelioma. Genes Chromosomes Cancer. 2000;28(3):337–41.
Dong J, Feldmann G, Huang J, Wu S, Zhang N, Comerford SA, et al. Elucidation of a universal size-control mechanism in Drosophila and mammals. Cell. 2007;130(6):1120–33.
Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, Cordenonsi M, et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474(7350):179–83.
Farazi PA, DePinho RA. Hepatocellular carcinoma pathogenesis: from genes to environment. Nat Rev Cancer. 2006;6(9):674–87.
Fernandez LA, Northcott PA, Dalton J, Fraga C, Ellison D, Angers S, et al. YAP1 is amplified and up-regulated in hedgehog-associated medulloblastomas and mediates Sonic hedgehog-driven neural precursor proliferation. Genes Dev. 2009;23(23):2729–41.
Fleury-Feith J, Lecomte C, Renier A, Matrat M, Kheuang L, Abramowski V, et al. Hemizygosity of Nf2 is associated with increased susceptibility to asbestos-induced peritoneal tumours. Oncogene. 2003;22(24):3799–805.
Giovannini M, Robanus-Maandag E, Niwa-Kawakita M, van der Valk M, Woodruff JM, Goutebroze L, et al. Schwann cell hyperplasia and tumors in transgenic mice expressing a naturally occurring mutant NF2 protein. Genes Dev. 1999;13(8):978–86.
Giovannini M, Robanus-Maandag E, van der Valk M, Niwa-Kawakita M, Abramowski V, Goutebroze L, et al. Conditional biallelic Nf2 mutation in the mouse promotes manifestations of human neurofibromatosis type 2. Genes Dev. 2000;14(13):1617–30.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Harvey K, Tapon N. The Salvador-Warts-Hippo pathway—an emerging tumour-suppressor network. Nat Rev Cancer. 2007;7(3):182–91.
Heallen T, Zhang M, Wang J, Bonilla-Claudio M, Klysik E, Johnson RL, et al. Hippo pathway inhibits Wnt signaling to restrain cardiomyocyte proliferation and heart size. Science. 2011;332(6028):458–61.
Hergovich A, Kohler RS, Schmitz D, Vichalkovski A, Cornils H, Hemmings BA. The MST1 and hMOB1 tumor suppressors control human centrosome duplication by regulating NDR kinase phosphorylation. Curr Biol. 2009;19(20):1692–702.
Hermsen M, Guervos MA, Meijer G, van Diest P, Nieto CS, Marcos CA, et al. Chromosomal changes in relation to clinical outcome in larynx and pharynx squamous cell carcinoma. Cell Oncol. 2005;27(3):191–8.
Hossain Z, Ali SM, Ko HL, Xu J, Ng CP, Guo K, et al. Glomerulocystic kidney disease in mice with a targeted inactivation of Wwtr1. Proc Natl Acad Sci U S A. 2007;104(5):1631–6.
Imoto I, Yang ZQ, Pimkhaokham A, Tsuda H, Shimada Y, Imamura M, et al. Identification of cIAP1 as a candidate target gene within an amplicon at 11q22 in esophageal squamous cell carcinomas. Cancer Res. 2001;61(18):6629–34.
Imoto I, Tsuda H, Hirasawa A, Miura M, Sakamoto M, Hirohashi S, et al. Expression of cIAP1, a target for 11q22 amplification, correlates with resistance of cervical cancers to radiotherapy. Cancer Res. 2002;62(17):4860–6.
Jansson L, Larsson J. Normal hematopoietic stem cell function in mice with enforced expression of the Hippo signaling effector YAP1. PLoS One. 2012;7(2):e32013.
Jiang Z, Li X, Hu J, Zhou W, Jiang Y, Li G, et al. Promoter hypermethylation-mediated down-regulation of LATS1 and LATS2 in human astrocytoma. Neurosci Res. 2006;56(4):450–8.
Jimenez-Velasco A, Roman-Gomez J, Agirre X, Barrios M, Navarro G, Vazquez I, et al. Downregulation of the large tumor suppressor 2 (LATS2/KPM) gene is associated with poor prognosis in acute lymphoblastic leukemia. Leukemia. 2005;19(12):2347–50.
Kalamarides M, Niwa-Kawakita M, Leblois H, Abramowski V, Perricaudet M, Janin A, et al. Nf2 gene inactivation in arachnoidal cells is rate-limiting for meningioma development in the mouse. Genes Dev. 2002;16(9):1060–5.
Katagiri K, Ohnishi N, Kabashima K, Iyoda T, Takeda N, Shinkai Y, et al. Crucial functions of the Rap1 effector molecule RAPL in lymphocyte and dendritic cell trafficking. Nat Immunol. 2004;5(10):1045–51.
Katagiri K, Katakai T, Ebisuno Y, Ueda Y, Okada T, Kinashi T. Mst1 controls lymphocyte trafficking and interstitial motility within lymph nodes. EMBO J. 2009;28(9):1319–31.
Katagiri K, Ueda Y, Tomiyama T, Yasuda K, Toda Y, Ikehara S, et al. Deficiency of Rap1-binding protein RAPL causes lymphoproliferative disorders through mislocalization of p27kip1. Immunity. 2011;34(1):24–38.
Kim TS, Lee DH, Kim SK, Shin SY, Seo EJ, Lim DS. Mammalian sterile 20-like kinase 1 (Mst1) suppresses lymphoma development by promoting faithful chromosome segregation. Cancer Res. 2012;72(20):5386–95.
Kops GJPL, Weaver BAA, Cleveland DW. On the road to cancer: aneuploidy and the mitotic checkpoint. Nat Rev Cancer. 2005;5(10):773–85.
Larsson J, Ohishi M, Garrison B, Aspling M, Janzen V, Adams GB, et al. Nf2/merlin regulates hematopoietic stem cell behavior by altering microenvironmental architecture. Cell Stem Cell. 2008;3(2):221–7.
Lee JH, Kim TS, Yang TH, Koo BK, Oh SP, Lee KP, et al. A crucial role of WW45 in developing epithelial tissues in the mouse. EMBO J. 2008;27(8):1231–42.
Lee KP, Lee JH, Kim TS, Kim TH, Park HD, Byun JS, et al. The Hippo-Salvador pathway restrains hepatic oval cell proliferation, liver size, and liver tumorigenesis. Proc Natl Acad Sci U S A. 2010;107(18):8248–53.
Li N, Kaur S, Greshock J, Lassus H, Zhong XM, Wang YL, et al. A combined array-based comparative genomic hybridization and functional library screening approach identifies mir-30d as an oncomir in cancer. Cancer Res. 2012;72(1):154–64.
Lu L, Li Y, Kim SM, Bossuyt W, Liu P, Qiu Q, et al. Hippo signaling is a potent in vivo growth and tumor suppressor pathway in the mammalian liver. Proc Natl Acad Sci U S A. 2010;107(4):1437–42.
Makita R, Uchijima Y, Nishiyama K, Amano T, Chen Q, Takeuchi T, et al. Multiple renal cysts, urinary concentration defects, and pulmonary emphysematous changes in mice lacking TAZ. Am J Physiol Renal Physiol. 2008;294(3):F542–53.
Mardin BR, Lange C, Baxter JE, Hardy T, Scholz SR, Fry AM, et al. Components of the Hippo pathway cooperate with Nek2 kinase to regulate centrosome disjunction. Nat Cell Biol. 2010;12(12):1166–76.
Matsui Y, Nakano N, Shao D, Gao SM, Luo WT, Hong C, et al. Lats2 is a negative regulator of myocyte size in the heart. Circ Res. 2008;103(11):1309–18.
McClatchey AI, Saotome I, Ramesh V, Gusella JF, Jacks T. The Nf2 tumor suppressor gene product is essential for extraembryonic development immediately prior to gastrulation. Genes Dev. 1997;11(10):1253–65.
McClatchey AI, Saotome I, Mercer K, Crowley D, Gusella JF, Bronson RT, et al. Mice heterozygous for a mutation at the Nf2 tumor suppressor locus develop a range of highly metastatic tumors. Genes Dev. 1998;12(8):1121–33.
McPherson JP, Tamblyn L, Elia A, Migon E, Shehabeldin A, Matysiak-Zablocki E, et al. Lats2/Kpm is required for embryonic development, proliferation control and genomic integrity. EMBO J. 2004;23(18):3677–88.
Mizuno T, Murakami H, Fujii M, Ishiguro F, Tanaka I, Kondo Y, et al. YAP induces malignant mesothelioma cell proliferation by upregulating transcription of cell cycle-promoting genes. Oncogene. 2012.
Morinaga N, Shitara Y, Yanagita Y, Koida T, Kimura M, Asao T, et al. Molecular analysis of the h-warts/LATS1 gene in human breast cancer. Int J Oncol. 2000;17(6):1125–9.
Morin-Kensicki EM, Boone BN, Howell M, Stonebraker JR, Teed J, Alb JG, et al. Defects in yolk sac vasculogenesis, chorioallantoic fusion, and embryonic axis elongation in mice with targeted disruption of Yap65. Mol Cell Biol. 2006;26(1):77–87.
Morris ZS, McClatchey AI. Aberrant epithelial morphology and persistent epidermal growth factor receptor signaling in a mouse model of renal carcinoma. Proc Natl Acad Sci U S A. 2009;106(24):9767–72.
Murakami H, Mizuno T, Taniguchi T, Fujii M, Ishiguro F, Fukui T, et al. LATS2 is a tumor suppressor gene of malignant mesothelioma. Cancer Res. 2011;71(3):873–83.
Nehme NT, Schmid JP, Debeurme F, Andre-Schmutz I, Lim A, Nitschke P, et al. MST1 mutations in autosomal recessive primary immunodeficiency characterized by defective naive T-cell survival. Blood. 2012;119(15):3458–68.
Nishioka N, Inoue K, Adachi K, Kiyonari H, Ota M, Ralston A, et al. The Hippo signaling pathway components Lats and Yap pattern Tead4 activity to distinguish mouse trophectoderm from inner cell mass. Dev Cell. 2009;16(3):398–410.
Odashima M, Usui S, Takagi H, Hong C, Liu J, Yokota M, et al. Inhibition of endogenous Mst1 prevents apoptosis and cardiac dysfunction without affecting cardiac hypertrophy after myocardial infarction. Circ Res. 2007;100(9):1344–52.
Oh S, Lee D, Kim T, Kim TS, Oh HJ, Hwang CY, et al. Crucial role for Mst1 and Mst2 kinases in early embryonic development of the mouse. Mol Cell Biol. 2009;29(23):6309–20.
Oh HJ, Kim MJ, Song SJ, Kim T, Lee D, Kwon SH, et al. MST1 limits the kinase activity of aurora B to promote stable kinetochore-microtubule attachment. Curr Biol. 2010;20(5):416–22.
Overholtzer M, Zhang J, Smolen GA, Muir B, Li W, Sgroi DC, et al. Transforming properties of YAP, a candidate oncogene on the chromosome 11q22 amplicon. Proc Natl Acad Sci U S A. 2006;103(33):12405–10.
Park J, Kang SI, Lee SY, Zhang XF, Kim MS, Beers LF, et al. Tumor suppressor Ras association domain family 5 (RASSF5/NORE1) mediates death receptor ligand-induced apoptosis. J Biol Chem. 2010;285(45):35029–38.
Roskams T. Liver stem cells and their implication in hepatocellular and cholangiocarcinoma. Oncogene. 2006;25(27):3818–22.
Sarkisian CJ, Keister BA, Stairs DB, Boxer RB, Moody SE, Chodosh LA. Dose-dependent oncogene-induced senescence in vivo and its evasion during mammary tumorigenesis. Nat Cell Biol. 2007;9(5):493–505.
Saucedo LJ, Edgar BA. Filling out the Hippo pathway. Nat Rev Mol Cell Biol. 2007;8(8):613–21.
Schlegelmilch K, Mohseni M, Kirak O, Pruszak J, Rodriguez JR, Zhou D, et al. Yap1 acts downstream of alpha-catenin to control epidermal proliferation. Cell. 2011;144(5):782–95.
Schroeder MC, Halder G. Regulation of the Hippo pathway by cell architecture and mechanical signals. Semin Cell Dev Biol. 2012;23(7):803–11.
Seidel C, Schagdarsurengin U, Blumke K, Wurl P, Pfeifer GP, Hauptmann S, et al. Frequent hypermethylation of MST1 and MST2 in soft tissue sarcoma. Mol Carcinog. 2007;46(10):865–71.
Snijders AM, Schmidt BL, Fridlyand J, Dekker N, Pinkel D, Jordan RCK, et al. Rare amplicons implicate frequent deregulation of cell fate specification pathways in oral squamous cell carcinoma. Oncogene. 2005;24(26):4232–42.
Song H, Mak KK, Topol L, Yun K, Hu J, Garrett L, et al. Mammalian Mst1 and Mst2 kinases play essential roles in organ size control and tumor suppression. Proc Natl Acad Sci U S A. 2010;107(4):1431–6.
Song H, Kim H, Lee K, Lee DH, Kim TS, Song JY, et al. Ablation of Rassf2 induces bone defects and subsequent haematopoietic anomalies in mice. EMBO J. 2012;31(5):1147–59.
St John MA, Tao W, Fei X, Fukumoto R, Carcangiu ML, Brownstein DG, et al. Mice deficient of Lats1 develop soft-tissue sarcomas, ovarian tumours and pituitary dysfunction. Nat Genet. 1999;21(2):182–6.
Strazisar M, Mlakar V, Glavac D. LATS2 tumour specific mutations and down-regulation of the gene in non-small cell carcinoma. Lung Cancer. 2009;64(3):257–62.
Thurneysen C, Opitz I, Kurtz S, Weder W, Stahel RA, Felley-Bosco E. Functional inactivation of NF2/merlin in human mesothelioma. Lung Cancer. 2009;64(2):140–7.
Tommasi S, Dammann R, Zhang Z, Wang Y, Liu L, Tsark WM, et al. Tumor susceptibility of Rassf1a knockout mice. Cancer Res. 2005;65(1):92–8.
Trofatter JA, MacCollin MM, Rutter JL, Murrell JR, Duyao MP, Parry DM, et al. A novel moesin-, ezrin-, radixin-like gene is a candidate for the neurofibromatosis 2 tumor suppressor. Cell. 1993;72(5):791–800.
Tschop K, Conery AR, Litovchick L, Decaprio JA, Settleman J, Harlow E, et al. A kinase shRNA screen links LATS2 and the pRB tumor suppressor. Genes Dev. 2011;25(8):814–30.
van der Flier LG, Clevers H. Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annu Rev Physiol. 2009;71:241–60.
van der Weyden L, Tachibana KK, Gonzalez MA, Adams DJ, Ng BL, Petty R, et al. The RASSF1A isoform of RASSF1 promotes microtubule stability and suppresses tumorigenesis. Mol Cell Biol. 2005;25(18):8356–67.
Varelas X, Sakuma R, Samavarchi-Tehrani P, Peerani R, Rao BM, Dembowy J, et al. TAZ controls Smad nucleocytoplasmic shuttling and regulates human embryonic stem-cell self-renewal. Nat Cell Biol. 2008;10(7):837–48.
Voorhoeve PM, le Sage C, Schrier M, Gillis AJ, Stoop H, Nagel R, et al. A genetic screen implicates miRNA-372 and miRNA-373 as oncogenes in testicular germ cell tumors. Cell. 2006;124(6):1169–81.
Weber RG, Sommer C, Albert FK, Kiessling M, Cremer T. Clinically distinct subgroups of glioblastoma multiforme studied by comparative genomic hybridization. Lab Invest. 1996;74(1):108–19.
Wozniak MA, Chen CS. Mechanotransduction in development: a growing role for contractility. Nat Rev Mol Cell Biol. 2009;10(1):34–43.
Xin M, Kim Y, Sutherland LB, Qi X, McAnally J, Schwartz RJ, et al. Regulation of insulin-like growth factor signaling by Yap governs cardiomyocyte proliferation and embryonic heart size. Sci Signal. 2011;4(196):ra70.
Yabuta N, Okada N, Ito A, Hosomi T, Nishihara S, Sasayama Y, et al. Lats2 is an essential mitotic regulator required for the coordination of cell division. J Biol Chem. 2007;282(26):19259–71.
Yokota J, Wada M, Shimosato Y, Terada M, Sugimura T. Loss of heterozygosity on chromosomes-3, chromosome-13, and chromosome-17 in small-cell carcinoma and on chromosome-3 in adenocarcinoma of the lung. Proc Natl Acad Sci U S A. 1987;84(24):9252–6.
Zender L, Spector MS, Xue W, Flemming P, Cordon-Cardo C, Silke J, et al. Identification and validation of oncogenes in liver cancer using an integrative oncogenomic approach. Cell. 2006;125(7):1253–67.
Zhang J, Ji JY, Yu M, Overholtzer M, Smolen GA, Wang R, et al. YAP-dependent induction of amphiregulin identifies a non-cell-autonomous component of the Hippo pathway. Nat Cell Biol. 2009;11(12):1444–50.
Zhang N, Bai H, David KK, Dong J, Zheng Y, Cai J, et al. The Merlin/NF2 tumor suppressor functions through the YAP oncoprotein to regulate tissue homeostasis in mammals. Dev Cell. 2010;19(1):27–38.
Zhang H, Pasolli HA, Fuchs E. Yes-associated protein (YAP) transcriptional coactivator functions in balancing growth and differentiation in skin. Proc Natl Acad Sci U S A. 2011;108(6):2270–5.
Zhao B, Wei X, Li W, Udan RS, Yang Q, Kim J, et al. Inactivation of YAP oncoprotein by the Hippo pathway is involved in cell contact inhibition and tissue growth control. Genes Dev. 2007;21(21):2747–61.
Zhao B, Li L, Lei QY, Guan KL. The Hippo-YAP pathway in organ size control and tumorigenesis: an updated version. Genes Dev. 2010a;24(9):862–74.
Zhao B, Li L, Tumaneng K, Wang CY, Guan KL. A coordinated phosphorylation by Lats and CK1 regulates YAP stability through SCF(beta-TRCP). Genes Dev. 2010b;24(1):72–85.
Zhou D, Conrad C, Xia F, Park JS, Payer B, Yin Y, et al. Mst1 and Mst2 maintain hepatocyte quiescence and suppress hepatocellular carcinoma development through inactivation of the Yap1 oncogene. Cancer Cell. 2009;16(5):425–38.
Zhou D, Zhang Y, Wu H, Barry E, Yin Y, Lawrence E, et al. Mst1 and Mst2 protein kinases restrain intestinal stem cell proliferation and colonic tumorigenesis by inhibition of Yes-associated protein (Yap) overabundance. Proc Natl Acad Sci U S A. 2011;108(49):E1312–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Kim, MC., Kim, TS., Kim, T., Lim, DS. (2013). Hippo and Mouse Models for Cancer. In: Oren, M., Aylon, Y. (eds) The Hippo Signaling Pathway and Cancer. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6220-0_11
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6220-0_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6219-4
Online ISBN: 978-1-4614-6220-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)