Abstract
The CD1 system is composed of five types of human CD1 proteins, CD1a, CD1b, CD1c, CD1d, and CD1e, and their mammalian orthologs. Each type of CD1 protein has a distinct antigen binding groove and shows differing patterns of expression within cells and in different tissues. Here we review the molecular mechanisms by which CD1a, CD1b, and CD1c capture distinct classes of self- and mycobacterial antigens. We discuss how CD1-restricted T cells participate in the immune response, emphasizing new evidence for mycobacterial recognition in vivo in human and non-human models.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The discoverers of the CD1 locus originally separated CD1 proteins into group 1 (CD1a, CD1b, and CD1c) and group 2 (CD1d), based on amino acid sequence homology [1]. The cellular expression pattern of CD1a, CD1b, CD1c, and CD1d also supports grouping into group 1 and group 2 CD1 because the expression of group 1 CD1 molecules is limited to CD4 and CD8 double-positive thymocytes and professional antigen presenting cells, while group 2 CD1 has a more extensive distribution pattern that also includes non-hematopoietic cells. Group 1 proteins are more likely to be constitutively expressed on cells, and recent studies show inverse expression of group 1 and group 2 protein surface density when encountering bacterial stimuli [2].
Published research on CD1 function strongly emphasizes the role of NKT cells in mice, which are defined by the expression of a nearly invariant T cell receptor (TCR) and recognition of CD1d. Through germline deletion of murine CD1d or the invariant TCR, as well as the use of CD1d tetramers, invariant NKT cells have been shown to function in mycobacterial, bacterial, fungal and protozoal infections, as well as mouse models of cancer, atherosclerosis, diabetes, multiple sclerosis, and fat maintenance [3, 4]. Much of this research has emphasized the invariant nature of CD1d-restricted TCRs and a stereotyped function relating to rapid secretion of cytokines, especially Interferon-γ. However, invariant NKT cells are only part of the CD1d system, and CD1d-restricted responses are in turn only part of the much larger system of CD1-reactive T cells that respond to human CD1a, CD1b, and CD1c, as well as their mammalian orthologs. Antigen presentation by CD1a, CD1b, and CD1c is recently gaining a broader interest [5]. Because mice lack group 1 CD1 proteins, studies of CD1a, CD1b and CD1c use human T cells in vitro or ex vivo, non-murine animal models, or human CD1 proteins expressed in mice, and they are now revealing the functions of T cells that normally respond to CD1a, CD1b, and CD1c. It has become clear that many of the most well known features of invariant NKT cells, including strict TCR conservation, liver homing, α-galactosylceramide specificity, and an Interferon-γ dominated immunophenotype, are not broadly shared among the larger CD1-restricted repertoire.
Here we emphasize that the group 1 CD1 versus group 2 CD1 classification lumps CD1a, CD1b, and CD1c together in ways that obscure the distinctiveness of the individual group 1 CD1 isoforms, each of which has different patterns of expression and mechanism of antigen presentation. Here we review the data on the separate functions of the CD1a, CD1b, and CD1c isoforms and describe how different or similar they are, with an emphasis on their roles in recognizing foreign, mycobacterial antigens during infection. Further, we review CD1 genes and function among non-human mammals. Both functional and evolutionary data support the idea that CD1a, CD1b, and CD1c are remarkably different from each other.
2 Cellular Expression and Intracellular Trafficking of CD1
Human CD1a, CD1b, and CD1c vary in size of their antigen binding grooves, patterns of expression across different tissues and cell types [6], and subcellular trafficking patterns, leading to presentation of different types of antigens presented in different tissues. Whereas CD1d is abundantly expressed in the liver and gastrointestinal tract, CD1a proteins are expressed in the skin at high density on the surface of Langerhans cells. Accordingly, CD1d-restricted invariant NKT cells home to and accumulate to large numbers in the liver, whereas CD1a autoreactive T cells home to the skin [7]. CD1b expression in the periphery is limited to the surface of dendritic cells and its inducible appearance on monocytes, and under those conditions CD1a and CD1c are also expressed. In addition, CD1c is expressed on marginal zone B cells in lymph nodes and peripheral blood. These clearly different, inducible, or constitutive patterns of each type of CD1 protein represent the first line of evidence that each CD1 gene likely plays a distinct role in immune response.
The subcellular trafficking of each type of CD1 molecule to differing steady-state distribution among endocytic compartments is mainly determined by motifs in the CD1 cytoplasmic tail, which bind to adaptor protein complexes [8–10]. Whereas CD1a lacks AP binding sequences and is found on the cell surface and sorting endosomes, human CD1c and CD1d bind to AP2, which mediates recycling and antigen capture in endosomes. Mouse CD1d and human CD1b bind both AP2 and AP3, driving their trafficking and steady-state accumulation in late endosomes and lysosomes. Therefore, human and mouse CD1 proteins differ and can be ranked as to the extent of penetration into the endosomal compartment with huCD1a < huCD1c < huCD1d < huCD1b and muCD1d. These differing trafficking patterns influence their function in T cell activation because endocytic compartments differ in their antigenic content. Also, the presence of endosomal lipid transfer proteins and low pH promote antigen loading onto CD1, yet highly acidic compartments can degrade some antigens so that they are not recognized [11–16]. These data provide clear evidence that each type of CD1 protein differs with regard to the type of cell on which it is expressed, and the cellular subcompartment to which it most strongly localizes.
3 Antigen Presentation by CD1a, CD1b, and CD1c
Complementing another review on CD1d in this same edition, this review focuses on the group 1 CD1 proteins, CD1a, CD1b, and CD1c. Even though CD1a, CD1b, and CD1c are able to present mammalian self-lipids and lipids from several types of bacteria, mycobacterial lipids are the focus of this section. Here we review mycobacterial antigens, which were the first described antigens for the CD1 system [17] and for which the most information is available, including ex vivo studies of human patients. The molecular interactions of each type of CD1 groove with differing antigens are considered separately.
3.1 CD1a
Of all the human group 1 CD1 molecules, CD1a has the smallest antigen binding groove (~1,350 Å3) and apparently the least stringent conditions for loading antigens [18, 19]. Upon de novo synthesis, all CD1 molecules appear on the cell surface and subsequently undergo multiple rounds of internalization via the endocytic route. In contrast to all other human CD1 proteins, human CD1a lacks discernable AP binding motifs and only cycles through early endosomes, bypassing late endosomes, before returning to the cell surface (Fig. 1) [14, 20]. CD1a may bind its antigens in the endoplasmic reticulum in the case of endogenous phospholipids, but also egresses to the cell surface and recycles through early endosomes, where it has access to exogenously added antigens and serum lipids. However, CD1a is not known to have requirements for low pH to capture antigens, and there is no clear evidence that early endosomes provide antigen loading factors, like activated saposins, which are preferentially located and activated in late endosomes and lysosomes. As contrasted with other CD1 proteins, which have mechanisms for preferential antigen capture in endosomes, these findings suggest that CD1a may have the most promiscuous mechanisms for binding endogenous lipids or exogenous lipids encountered at or near the cell surface.
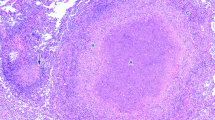
Sources of CD1a-, CD1b-, and CD1c-presented antigens. Group 1 CD1-expressing antigen presenting cells internalize mycobacterial lipids via the endocytic route in the form of bacteria or bacterial debris, debris of infected cells, as free lipids, or lipid-protein complexes. Lipids are loaded into the CD1 molecules in the early or late endocytic compartments to which CD1 isoforms differentially traffic. The structures of representative mycobacterial antigens that are presented are shown. R is glucose in glucose monomycolate, glycerol in glycerol monomycolate, or hydrogen in mycolic acid
The potential of CD1a to contribute to anti-mycobacterial immunity is demonstrated by its ability to present dideoxymycobactin (Fig. 1), a precursor molecule in the biosynthesis of mycobactin [21, 22]. The mycobactin siderophores are essential in mycobacterial iron acquisition and survival of the bacterium in vivo [23, 24]. Mycobactins and related molecules have peptidic backbones that are synthesized by non-ribosomal protein synthases. The crystal structure of CD1a bound to a mycobactin shows that the acyl chain is bound deeply within the A’ pocket in the antigen binding groove of the CD1a molecule, and the peptidic part is folded into a U-shaped conformation, so that it descends into the C’ pocket with its’ termini near the predicted plane of TCR contact. In contrast to the extended conformation of MHC I-presented peptides, for which the center of the peptide provides the key surface for TCRs, the structure of CD1a-dideoxymycobactin complexes predicts that only the termini of peptides are presented to the TCR [25]. However, unlike for CD1b- and CD1c-restricted anti-mycobacterial responses, which have been directly observed among polyclonal T cells ex vivo, published evidence for dideoxymycobactin recognition is limited to detailed studies of one clone so that broader studies of polyclonal responses ex vivo are needed.
CD1a also activates T cells in the absence of exogenous antigen, suggesting that self-antigens for CD1a exist [7, 26–29]. The antigens recognized by these clones are unknown, but most likely represent cellular lipids. Using purified or commercially available lipids to prime human T cells ex vivo, it is possible to detect responses against molecules like gangliosides and sulfatides [30] and unknown ligands possibly originating from serum [18]. The very high expression of CD1a by Langerhans cells and the recognition of CD1a in the absence of exogenously added antigen by T cell clones and polyclonal T cell populations with skin homing phenotype strongly suggests that there is a relevant physiologic function of CD1a in the skin, independent from a role in antimycobacterial immunity, possibly related to skin homeostasis [7]. For CD1d-restricted NKT cells the phenomenon of self-reactivity and reactivity to exogenously added foreign antigens is well described, including the physiologic relevance of this dual reactivity [31]. It seems that CD1a represents a comparable situation in that foreign bacterial ligands certainly exist and are capable of stimulating the immune system in a CD1a-dependent manner, but self-antigens also importantly contribute to its normal function.
3.2 CD1b
Among all CD1 isoforms, the size and shape of the CD1b groove stands out as having the largest volume (~2.200 Å3). The CD1b groove is nearly twice as large as the CD1a groove, and compared to other CD1 isoforms, CD1b binds correspondingly larger lipids, including mycolyl lipids and sulfoglycolipids that are up to C80 in length [32–37]. Because the volume of the groove is estimated to accommodate optimally C76 [38] and the fact that mycobacterial mycolyl lipids are amongst the longest hydrocarbon chains known in biology, CD1b likely plays a biological role in presenting particularly large foreign lipids. The crystal structure of human CD1b bound to glucose monomycolate shows that the very long meromycolate chain is twisted through the combined length of the A’, T’, and F’ pockets, which are oriented end to end, creating a superchannel in the CD1b molecule. The shorter α-branch lies in the C’ pocket [32]. The large volume of the CD1b groove may represent an evolved adaptation by which CD1b particularly focuses on presentation of foreign lipids. Supporting this speculation, CD1b autoreactive T cells are rarely observed among studies of autoreactive T cell populations or clones [7, 26]. Also, ~C76–C80 lipids that are commonly found in mycobacteria are generally absent in mammalian cells and were not detected in studies that broadly measured cellular CD1b ligands in eluents [39].
Considering all antigens known for all CD1 isoforms, CD1b shows the greatest flexibility for capture of lipids of different size, ranging from C12 to C80, including glucose monomycolate [37], glycerol monomycolate [36], free mycolic acid [33], diacylated sulfoglycolipids [40] and phosphatidylinositol mannosides (Fig. 1) [41, 42]. Long chain self-lipids in the range of C80 are not yet known and may not exist, begging the question of how smaller ~C40 self-lipids can bind to CD1b.
This question has been recently solved by showing that deeply seated scaffold lipids and antigenic lipids simultaneously bind to CD1b, so that their combined length fills the complete antigen binding groove of CD1b [34, 39, 43]. Crystallographic and functional studies now show that small self-antigens, like phosphatidyl ethanolamines with approximately ~C40 alkyl chains, are seated in the ‘upper’ region of the groove so that their head groups protrude for TCR contact. These antigens bind simultaneously with ~C32–40 scaffold lipids. Scaffold lipids derive their name from their deep seating within the ‘bottom’ of the groove, where provide upward support to position antigens near the A’ portal for TCR contact from the ‘bottom’ of the groove to support antigens. Scaffold lipids were originally suggested to exist based on co-crystallization of detergents in the groove [43], and naturally occurring spacer lipids have been recently identified as diacylglycerols and deoxyceramides [39, 43, 44]. It has been known for more than a decade that CD1b can present glucose mycolate antigens with either C80 or C32 tails, and the latter finding is likely explained by binding a diacylglycerol spacer beneath the short chain mycolic acid [37, 39].
Thus, CD1b has evolved specific mechanisms for sampling antigens greatly vary in length. A general structural formula of mycolyl lipids is provided in Fig. 1. CD1b also presents big non-mycolyl lipids, such as mycobacterial diacylated sulfoglycolipids (Fig. 1) and phosphatidylinositol mannosides, which have both been reported to bind CD1b and activate T cell clones [35, 40, 41]. Last, CD1b is known to present the ganglioside self-lipids GM1, GalNac GD1a, GD1b, and GQ1b [45].
For the presentation of long chain glucose monomycolate and mycolic acid, as well as diacylated sulfoglycolipid, trafficking of CD1b to low pH lysosomal compartments is necessary for antigen loading (Fig. 1) [13, 17, 40, 41, 46]. The low pH causes release of interdomain tethers that are present at neutral pH and normally connect the α1 helix across to the α2 helix and to a loop located at the end of the groove. Acidic pH at levels found in lysosomes protonates negatively charged residues that from ionic bonds within tethers, so interdomain contacts located immediately adjacent to the antigen entry portal are dissolved, providing greater access to the groove, as well as unloading of prebound self-lipids [47]. Because antigens with small alkyl chains would be less affected by this proposed dilation of the antigen entry portal, this mechanism might explain how smaller self-antigens are initially captured in the secretory pathway at neutral pH, whereas larger mycobacterial antigens strictly require low pH found in endosomes.
In addition, late endosomes and lysosomes are likely enriched for exogenous or foreign antigens by the action of the mannose receptor, DC-SIGN, Langerin, LDL, or scavenger receptor-mediated endocytosis of bacteria and bacterial debris [48–52]. CD1b expressing cells that are infected with mycobacteria present lipids to T cells, but whether antigens can gain direct access from the bacterium that resides in the cytoplasm or phagolysosome to the lysosome where CD1b loads its antigens, or whether antigens need to be shed and endocytosed has not yet been solved. Supporting the notion that CD1b is of specific relevance to the immune responses against antigens with long alkyl chains, CD1b-mediated T cell responses have not only been detected among T cell clones, but also polyclonal CD1b-restricted T cell responses from infected humans and bovines against mycolic acid, glucose monomycolate, glycerol monomycolate, and sulfoglycolipid have been described by independent research groups and will be discussed in more detail in Sect. 4 [36, 40, 53–56].
3.3 CD1c
CD1c shows interaction with both αβ or γδ T cells [28, 57]. CD1c molecules broadly survey the endocytic compartments, trafficking into early and late endosomes, an observation suggesting CD1c may have a larger antigen sampling pool than other isoforms [58, 59]. A role for CD1c in mediating T cell responses against M. tuberculosis was first demonstrated by the successful derivation of human T cell clones recognizing mycobacterial lipid extracts [60, 61]. Several CD1c-restricted T cell lines have been successfully derived against mycobacterial lipid extracts and patients infected with M. tuberculosis have CD1c-restricted immune responses [61].
Identification of the antigenic compounds that are recognized by these T cell clones revealed that CD1c presents structurally related branched chain lipids to clones and polyclonal T cells, the first description of which defined a new class of mycobacterial lipid, mycoketides (Fig. 1). Using the CD1c-restricted T cell line CD8-1, mannosyl phosphomycoketide was identified from mycobacterial lipid extracts. Mycoketides were found in lipid extracts of various medically important mycobacterial species, including M. avium, M. bovis BCG, and M. tuberculosis [61, 62]. The methyl branching pattern of mycoketides is important in positioning the lipid within CD1c for optimal T cell activation. More specifically, comparisons of synthetic mycoketide analogs demonstrate that optimal T cell activation occur with all five methyl branches with S-stereocenters [63]. In addition, T cell clones can show specificity for the presence and linkage of carbohydrate moieties within dolichyl or mycoketide phosphoglycolipids [61, 63].
The crystal structure of CD1c in complex with all-S mannosyl-phosphomycoketide reveals the second largest binding groove amongst all CD1 isoforms, at 1780 Å3. CD1c has two hydrophobic binding pockets, called A’ and F’. The CD1c A’ pocket has a toroidal shape, which is large enough to accommodate the bulky alkyl chain of mycoketides and binds the branched lipid with a hand in glove fit. The complex also highlighted the importance of the all-S configuration of methyl branches, which allows for the favorable clockwise rotation of the lipid, an orientation that may not occur with stereorandom methyl branching [64]. Thus the lipid tail helps to orient interactions within the CD1c A’ pocket to position the glycan headgroup for recognition by T cell. The short length (C30–36), saturation, and methyl branching of mycoketides differ from that seen in mammalian isoprenoid structures and may represent a pathogen-associated pattern that specifically binds to CD1c and supports recognition. Although less studied than CD1b-restricted T cell responses, CD1c-restricted T cells recognizing synthetic mycoketide homologs, mannosyl-phosphodolichols, have been observed to be expanded in number in the blood of human M. tuberculosis infected patients as compared to uninfected controls, providing evidence for an in vivo immune response to this phospholipid antigen during natural human infections [61].
4 Function of Group 1 CD1 In Vivo
The in vitro generated data discussed above suggest a possible function of group 1 CD1 in mycobacterial infection by providing proof of principle that mycobacterial lipids can be recognized by T cells and by identifying many such examples through the study of T cell clones. New data for presentation of mycobacterial lipids to polyclonal T cells in vivo or ex vivo provide direct evidence for a function of group 1 CD1 during mycobacterial infection in animal models and humans.
Guinea pigs (Cavia porcellus), a species in which group 1 CD1 is represented by multiple CD1b and CD1c orthologs, have been used in immunization experiments with M. bovis Bacille Calmette-Guérin (BCG) or with partially purified lipid extracts of M. tuberculosis, and were shown to develop strong proliferative and cytolytic T cell responses restricted by CD1b and CD1c [65, 66]. Guinea pigs are naturally highly sensitive to infection with M. tuberculosis, but immunization with M. tuberculosis lipids resulted in significantly smaller lung lesion size upon aerosol challenge with M. tuberculosis than vehicle only immunized animals. The level of protection was comparable to BCG vaccinated animals [67].
Cattle (Bos taurus) express multiple CD1a and CD1b proteins, but lack a gene for CD1c. Cattle are sensitive to natural infection with M. bovis, causing bovine tuberculosis that shares many clinical and pathological characteristics with human tuberculosis. Also, M. avium paratuberculosis causes bovine paratuberculosis, also known as Johne’s disease. Polyclonal T cells of naturally infected animals have been stimulated with lipid antigens, and despite considerable overlap in lipid content, lipid extracts from M. bovis and M. avium paratuberculosis could specifically stimulate T cells from cattle infected with M. bovis and M. avium paratuberculosis respectively, with very little crossreactivity [56]. The immunodominant lipid in M. avium paratuberculosis is glucose monomycolate [56]. In uninfected animals, immunization experiments with pure glucose monomycolate demonstrated that a CD1b-restricted T cell response against glucose monomycolate was generated and could be detected until 4 months after the last immunization, but no antibody response was induced [68].
Working with guinea pigs, cattle, or any other animal species that naturally expresses group 1 CD1 is much more cumbersome than working with mice. To create the possibility to study group 1 CD1 mediated immunity in mice, a mouse that is transgenic for the human group 1 CD1 molecules has been created [69]. The expression pattern of the individual human CD1 proteins in this mouse reflects the pattern in humans. This mouse gave rise to multiple T cell lines that were reactive to human CD1 proteins in the absence of exogenous antigens. Upon immunization with M. tuberculosis lipids or infection with M. tuberculosis, T cells that recognize M. tuberculosis lipids presented by human CD1 proteins could also be detected. An alternative way to create mouse models for human CD1 proteins is the humanized SCID mouse [70]. An important difference between the human CD1 transgenic mice and the humanized SCID mice is that the latter also has a human T cell compartment, while the human group 1 CD1 transgenic mouse uses its endogenous murine TCR gene segments.
Working with T cells from M. tuberculosis exposed human subjects provides the most physiologically relevant data on function of group 1 CD1 but in the past was mainly limited to studies of human clones in vitro. However analysis of fresh polyclonal T cells is feasible and is becoming more widespread with the recent invention of new tools. One approach is to stimulate ex vivo human T cells with group 1 CD1-expressing antigen presenting cells and M. tuberculosis lipids followed by detection of polyclonal T cell proliferation or the release of Interferon-γ directly. This approach has been taken to demonstrate the recognition of CD1c-restricted T cells recognizing phosphomycoketides selectively expanded in human M. tuberculosis infected patients, providing evidence for an in vivo immune response [61]. Also, CD1b-restricted responses against glycerol monomycolate were detected ex vivo in latent tuberculosis patients and BCG vaccinated individuals, but not in healthy controls or patients with active tuberculosis [36]. Glucose monomycolate was recognized by ex vivo T cells from latent tuberculosis patients, but not by T cells from healthy donors, patients with active tuberculosis, or BCG vaccinated individuals [55]. CD1b-restricted responses against mycobacterial sulphoglycolipid have been demonstrated in both latent and active M. tuberculosis infected patients, but not in healthy controls [40]. Finally, responses to mycolic acid were detected in active tuberculosis patients but not in healthy controls. During treatment, the mycolic acid-specific T cell population contracted and became mostly undetectable at 6 months after initiation of treatment, but T cells specific for the mycobacterial proteins ESAT-6 and CFP10 were still detectable [54].
An alternative approach to demonstrate group 1 CD1 T cell responses during mycobacterial infections in human subjects is the use of tetramers made from group 1 CD1 proteins. Two advantages of using tetramers is that CD1-restricted, antigen specific T cells can be visualized directly ex vivo without stimulation, and antigen specific cells can be physically captured in a live state after flow cytometric sorting. Tetramer studies of human group 1 reactive T cells were first reported last year using a glucose monomycolate-loaded CD1b tetramer. A small CD4+ T cell population was clearly detectable in tuberculosis patients, while no such population could be detected using unloaded CD1b tetramer. Sorting of this population confirmed the CD1b restriction and antigen specificity of these cells in an Interferon-γ ELISPOT assay and provides new avenues of research into TCR diversity and natural effector functions [53].
5 Characteristics of Group1 CD1-Restricted T Cells
The different mammalian group 1 CD1 genes and the chemical diversity of the antigens that can be presented by the group 1 CD1 proteins can only exert an effect on the course of an infectious disease, if there are also group 1 CD1 responsive immune cells. The evidence that T cells respond to antigen presentation by CD1 is very strong, but interactions of CD1 with a receptors other than the TCR were recently demonstrated in reports that showed that Ig-like transcript 4 (ILT4) expressed on monocytes can bind CD1c and CD1d [71, 72]. Binding of molecules other than TCR has also been demonstrated for classical MHC class I molecules and is by no means inconsistent with the activation of T cells as the main function of these molecules.
Very low precursor frequency MHC class I- and II-restricted T cells expand upon primary exposure to their cognate antigen, and this forms the basis of immunological memory. Therefore it was a surprise that invariant NKT cells, a subset of T cells that are restricted by CD1d, exist as a population with a very high precursor frequency with an activated phenotype. Immunization with their cognate antigen does not durably change their precursor frequency and phenotype. It is unknown whether CD1a-, CD1b-, and CD1c-restricted T cells behave like MHC class I- and class II-restricted cells, or rather like NKT cells. Pathogen-specific CD1a-, CD1b-, and CD1c-restricted T cell responses are virtually undetectable in blood in naïve individuals, and they appear upon priming with antigen either by infection in vivo with CD1-presented antigen-producing pathogens or by experimental immunization with CD1-presented antigens. These responses can be detected several months after the initial exposure with antigen or immunization, but it is unknown how long they persist in the absence of antigen. Thus, the question whether group 1 CD1-restricted T cells generate years-long durable memory responses like conventional MHC-restricted T cells has not yet been resolved.
Double-negative (CD4-CD8-) cells were among the first CD1a-, CD1b-, and CD1c-restricted T cells that were described [27]. This observation is likely attributable to the fact that early studies of CD1 specifically deleted CD4+ cells from cultures to reduce alloreactivity rather than the lack of naturally occurring CD4 cells that recognize group 1 CD1 proteins. More recent studies have detected many CD4+ CD1b-restricted clones, and T cells sorted with CD1b tetramers bound to glucose monomycolate are predominantly or exclusively CD4 positive [26, 36, 53, 73, 74].
The early in vitro studies on reactivity of CD1a-, CD1b-, and CD1c-restricted T cell clones and also polyclonal T cell responses have emphasized assays that determine cell proliferation, cytotoxicity, or Interferon-γ release, which are anti-mycobacterial effector mechanisms. Indeed, most known mycobacterial lipid-specific T cells can efficiently kill infected cells, which is a phenotype that suggests that these cells might contribute to immunity against mycobacteria [27, 46, 73, 75]. Interestingly, the release of granulysin, a mycobactericidal peptide, in cytolytic granules been described and has been shown to be able to kill M. tuberculosis bacteria [76]. However, T cell clones may show functional drift during in vitro culture. Therefore, candidate effector functions previously identified in clones must now be tested using new methods to survey fresh polyclonal T cells.
A conceptual problem with a primary cytotoxic and mycobactericidal role is that CD1a, CD1b, and CD1c are not expressed on macrophages, which form the bulk of the infected cells during tuberculosis. Also, arguing against a mainly cytotoxic and mycobactericidal function in vivo are the low percentages of circulating CD1b-restricted cells that have been detected compared to the percentages of cytotoxic MHC class I-restricted T cells during acute viral infection [53, 54]. The relatively low absolute precursor frequency in the blood raises the question as to whether these cells might migrate from the blood toward infected sites. CD1-restricted T cells might have helper functions by which the effect of a small number of antigen-specific T cells might be amplified through other effector cells, a concept that is well established for NKT cells.
It must be noted that our view of the T cell response is determined by the choice of the T cell assays. Because release of Interferon-γ is thought to be beneficial to the host during mycobacterial infection, and sensitive reagents for its detection have been widely available, it may have been the preferred readout for T cell function for convenience sake rather than the dominant natural effector function of cells in vivo. Whether CD1a-, CD1b-, and CD1c-restricted T cells perform other tasks in vivo, including regulatory, Th1, Th2, Th17-like helper-like functions, or have completely novel functions, remains to be established. These questions could be addressed with more unbiased and descriptive techniques like gene expression profiling. The recently described technology of detecting CD1-restricted T cells using antigen-loaded tetramers should help in the elucidation of the function of these cells because the Th1 biasing effects of in vitro culture can be avoided and diverse effector functions might be detected.
Another piece of information about a T cell subset lies in the TCR itself. The available TCR sequences of T cells that recognize CD1a-, CD1b-, and CD1c-presented antigens show diverse variable region usage, incorporate non-template encoded amino acids, and otherwise do not contain any features that stand out that distinguish these TCRs from the TCRs of conventional peptide specific MHC class I- or II-restricted T cells. Due to the limited number of available TCR sequences from group 1 CD1-restricted T cell clones with known antigen specificity, little is known about whether subpopulations with invariant characteristics exist. With the advance of tetramer technology and discovery of novel group 1 CD1-presented antigens, more TCR sequences will become available and invariant group 1 CD1-restricted T cells may be identified. However, the possibilities of diverse and invariant group 1 CD1-restricted are not mutually exclusive. In fact, CD1d presents lipid antigens to invariant NKT cells, but also to T cells that do not fit the criteria of invariant T cells [77–79].
6 Concluding Remarks
The CD1 family of antigen presenting molecules is a varied group of molecules that is unevenly spread among mammalian species. The functions of the CD1a, CD1b, and CD1c isoforms might be as different from each other as from CD1d. Although all the CD1 isoforms can present mycobacterial lipids to T cell clones, data suggest that for CD1a self-antigen reactive T cells are very common. In contrast, CD1b has most convincingly and repeatedly shown to present mycobacterial antigens in physiologically relevant settings. It is the right time now to to focus on animal models and study of fresh human T cells in the ex vivo setting to expand the knowledge of group 1 CD1-restricted T cells, bringing it to a level that equals our extensive knowledge of classical MHC- and CD1d-restricted T cells, and prepare the road for application of lipids in vaccines against tuberculosis.
References
Calabi F, Jarvis JM, Martin L, Milstein C (1989) Two classes of CD1 genes. Eur J Immunol 19:285–292
Roura-Mir C, Wang L, Cheng TY, Matsunaga I, Dascher CC, Peng SL, Fenton MJ, Kirschning C, Moody DB (2005) Mycobacterium tuberculosis regulates CD1 antigen presentation pathways through TLR-2. J Immunol 175:1758–1766
Matsuda JL, Mallevaey T, Scott-Browne J, Gapin L (2008) CD1d-restricted iNKT cells, the ‘Swiss-Army knife’ of the immune system. Curr Opin Immunol 20:358–368
Stronge VS, Salio M, Jones EY, Cerundolo V (2007) A closer look at CD1d molecules: new horizons in studying NKT cells. Trends Immunol 28:455–462
Young MH, Gapin L (2011) Group 1 CD1-restricted T cells take center stage. Eur J Immunol 41:592–594
Dougan SK, Kaser A, Blumberg RS (2007) CD1 expression on antigen-presenting cells. Curr Top Microbiol Immunol 314:113–141
de Jong A, Pena-Cruz V, Cheng TY, Clark RA, van Rhijn I, Moody DB (2010) CD1a-autoreactive T cells are a normal component of the human alphabeta T cell repertoire. Nat Immunol 11:1102–1109
Dascher CC, Brenner MB (2003) Evolutionary constraints on CD1 structure: insights from comparative genomic analysis. Trends Immunol 24:412–418
Jackman RM, Stenger S, Lee A, Moody DB, Rogers RA, Niazi KR, Sugita M, Modlin RL, Peters PJ, Porcelli SA (1998) The tyrosine-containing cytoplasmic tail of CD1b is essential for its efficient presentation of bacterial lipid antigens. Immunity 8:341–351
Moody DB, Porcelli SA (2003) Intracellular pathways of CD1 antigen presentation. Nat Rev Immunol 3:11–22
Kang SJ, Cresswell P (2002) Regulation of intracellular trafficking of human CD1d by association with MHC class II molecules. EMBO J 21:1650–1660
Kaser A, Hava DL, Dougan SK, Chen Z, Zeissig S, Brenner MB, Blumberg RS (2008) Microsomal triglyceride transfer protein regulates endogenous and exogenous antigen presentation by group 1 CD1 molecules. Eur J Immunol 38:2351–2359
Moody DB, Briken V, Cheng TY, Roura-Mir C, Guy MR, Geho DH, Tykocinski ML, Besra GS, Porcelli SA (2002) Lipid length controls antigen entry into endosomal and nonendosomal pathways for CD1b presentation. Nat Immunol 3:435–442
Sugita M, Grant EP, van Donselaar E, Hsu VW, Rogers RA, Peters PJ, Brenner MB (1999) Separate pathways for antigen presentation by CD1 molecules. Immunity 11:743–752
van Rhijn I, Young DC, de Jong A, Vazquez J, Cheng TY, Talekar R, Barral DC, Leon L, Brenner MB, Katz JT, Riese R, Ruprecht RM, O’Connor PB, Costello CE, Porcelli SA, Briken V, Moody DB (2009) CD1c bypasses lysosomes to present a lipopeptide antigen with 12 amino acids. J Exp Med 206:1409–1422
Zeissig S, Dougan SK, Barral DC, Junker Y, Chen Z, Kaser A, Ho M, Mandel H, McIntyre A, Kennedy SM, Painter GF, Veerapen N, Besra GS, Cerundolo V, Yue S, Beladi S, Behar SM, Chen X, Gumperz JE, Breckpot K, Raper A, Baer A, Exley MA, Hegele RA, Cuchel M, Rader DJ, Davidson NO, Blumberg RS (2010) Primary deficiency of microsomal triglyceride transfer protein in human abetalipoproteinemia is associated with loss of CD1 function. J Clin Invest 120:2889–2899
Porcelli S, Morita CT, Brenner MB (1992) CD1b restricts the response of human CD4-8-T lymphocytes to a microbial antigen. Nature 360:593–597
Manolova V, Kistowska M, Paoletti S, Baltariu GM, Bausinger H, Hanau D, Mori L, de Libero G (2006) Functional CD1a is stabilized by exogenous lipids. Eur J Immunol 36:1083–1092
Zajonc DM, Elsliger MA, Teyton L, Wilson IA (2003) Crystal structure of CD1a in complex with a sulfatide self antigen at a resolution of 2.15 A. Nat Immunol 4:808–815
Barral DC, Cavallari M, McCormick PJ, Garg S, Magee AI, Bonifacino JS, de Libero G, Brenner MB (2008) CD1a and MHC class I follow a similar endocytic recycling pathway. Traffic 9:1446–1457
Madigan CA, Cheng TY, Layre E, Young DC, McConnell MJ, Debono CA, Murry JP, Wei JR, Barry CE 3rd, Rodriguez GM, Matsunaga I, Rubin EJ, Moody DB (2012) Lipidomic discovery of deoxysiderophores reveals a revised mycobactin biosynthesis pathway in Mycobacterium tuberculosis. Proc Natl Acad Sci U S A 109:1257–1262
Moody DB, Young DC, Cheng TY, Rosat JP, Roura-Mir C, O’Connor PB, Zajonc DM, Walz A, Miller MJ, Levery SB, Wilson IA, Costello CE, Brenner MB (2004) T cell activation by lipopeptide antigens. Science 303:527–531
de Voss JJ, Rutter K, Schroeder BG, Su H, Zhu Y, Barry CE 3rd (2000) The salicylate-derived mycobactin siderophores of Mycobacterium tuberculosis are essential for growth in macrophages. Proc Natl Acad Sci U S A 97:1252–1257
Siegrist MS, Unnikrishnan M, McConnell MJ, Borowsky M, Cheng TY, Siddiqi N, Fortune SM, Moody DB, Rubin EJ (2009) Mycobacterial Esx-3 is required for mycobactin-mediated iron acquisition. Proc Natl Acad Sci U S A 106:18792–18797
Zajonc DM, Crispin MD, Bowden TA, Young DC, Cheng TY, Hu J, Costello CE, Rudd PM, Dwek RA, Miller MJ, Brenner MB, Moody DB, Wilson IA (2005) Molecular mechanism of lipopeptide presentation by CD1a. Immunity 22:209–219
de Lalla C, Lepore M, Piccolo FM, Rinaldi A, Scelfo A, Garavaglia C, Mori L, de Libero G, Dellabona P, Casorati G (2010) High-frequency and adaptive-like dynamics of human CD1 self-reactive T cells. Eur J Immunol 41:602–610
Porcelli S, Brenner MB, Greenstein JL, Balk SP, Terhorst C, Bleicher PA (1989) Recognition of cluster of differentiation 1 antigens by human CD4-CD8-cytolytic T lymphocytes. Nature 341:447–450
Vincent MS, Leslie DS, Gumperz JE, Xiong X, Grant EP, Brenner MB (2002) CD1-dependent dendritic cell instruction. Nat Immunol 3:1163–1168
Vincent MS, Xiong X, Grant EP, Peng W, Brenner MB (2005) CD1a-, b-, and c-restricted TCRs recognize both self and foreign antigens. J Immunol 175:6344–6351
Shamshiev A, Donda A, Carena I, Mori L, Kappos L, de Libero G (1999) Self glycolipids as T-cell autoantigens. Eur J Immunol 29:1667–1675
Brigl M, Tatituri RV, Watts GF, Bhowruth V, Leadbetter EA, Barton N, Cohen NR, Hsu FF, Besra GS, Brenner MB (2011) Innate and cytokine-driven signals, rather than microbial antigens, dominate in natural killer T cell activation during microbial infection. J Exp Med 208:1163–1177
Batuwangala T, Shepherd D, Gadola SD, Gibson KJ, Zaccai NR, Fersht AR, Besra GS, Cerundolo V, Jones EY (2004) The crystal structure of human CD1b with a bound bacterial glycolipid. J Immunol 172:2382–2388
Beckman EM, Porcelli SA, Morita CT, Behar SM, Furlong ST, Brenner MB (1994) Recognition of a lipid antigen by CD1-restricted alpha beta+ T cells. Nature 372:691–694
Garcia-Alles LF, Collmann A, Versluis C, Lindner B, Guiard J, Maveyraud L, Huc E, Im JS, Sansano S, Brando T, Julien S, Prandi J, Gilleron M, Porcelli SA, de la Salle H, Heck AJ, Mori L, Puzo G, Mourey L, de Libero G (2011) Structural reorganization of the antigen-binding groove of human CD1b for presentation of mycobacterial sulfoglycolipids. Proc Natl Acad Sci U S A 108:17755–17760
Guiard J, Collmann A, Garcia-Alles LF, Mourey L, Brando T, Mori L, Gilleron M, Prandi J, de Libero G, Puzo G (2009) Fatty acyl structures of mycobacterium tuberculosis sulfoglycolipid govern T cell response. J Immunol 182:7030–7037
Layre E, Collmann A, Bastian M, Mariotti S, Czaplicki J, Prandi J, Mori L, Stenger S, de Libero G, Puzo G, Gilleron M (2009) Mycolic acids constitute a scaffold for mycobacterial lipid antigens stimulating CD1-restricted T cells. Chem Biol 16:82–92
Moody DB, Reinhold BB, Guy MR, Beckman EM, Frederique DE, Furlong ST, Ye S, Reinhold VN, Sieling PA, Modlin RL, Besra GS, Porcelli SA (1997) Structural requirements for glycolipid antigen recognition by CD1b-restricted T cells. Science 278:283–286
Moody DB, Zajonc DM, Wilson IA (2005) Anatomy of CD1-lipid antigen complexes. Nat Rev Immunol 5:387–399
Huang S, Cheng TY, Young DC, Layre E, Madigan CA, Shires J, Cerundolo V, Altman JD, Moody DB (2011) Discovery of deoxyceramides and diacylglycerols as CD1b scaffold lipids among diverse groove-blocking lipids of the human CD1 system. Proc Natl Acad Sci U S A 108:19335–19340
Gilleron M, Stenger S, Mazorra Z, Wittke F, Mariotti S, Bohmer G, Prandi J, Mori L, Puzo G, de Libero G (2004) Diacylated Sulfoglycolipids are novel mycobacterial antigens stimulating CD1-restricted T Cells during infection with mycobacterium tuberculosis. J Exp Med 199:649–659
de la Salle H, Mariotti S, Angenieux C, Gilleron M, Garcia-Alles LF, Malm D, Berg T, Paoletti S, Maitre B, Mourey L, Salamero J, Cazenave JP, Hanau D, Mori L, Puzo G, de Libero G (2005) Assistance of microbial glycolipid antigen processing by CD1e. Science 310:1321–1324
Ernst WA, Maher J, Cho S, Niazi KR, Chatterjee D, Moody DB, Besra GS, Watanabe Y, Jensen PE, Porcelli SA, Kronenberg M, Modlin RL (1998) Molecular interaction of CD1b with lipoglycan antigens. Immunity 8:331–340
Gadola SD, Zaccai NR, Harlos K, Shepherd D, Castro-Palomino JC, Ritter G, Schmidt RR, Jones EY, Cerundolo V (2002) Structure of human CD1b with bound ligands at 2.3 A, a maze for alkyl chains. Nat Immunol 3:721–726
Garcia-Alles LF, Versluis K, Maveyraud L, Vallina AT, Sansano S, Bello NF, Gober HJ, Guillet V, de la Salle H, Puzo G, Mori L, Heck AJ, de Libero G, Mourey L (2006) Endogenous phosphatidylcholine and a long spacer ligand stabilize the lipid-binding groove of CD1b. EMBO J 25:3684–3692
de Libero G, Mori L (2007) Structure and biology of self lipid antigens. Curr Top Microbiol Immunol 314:51–72
Sieling PA, Chatterjee D, Porcelli SA, Prigozy TI, Mazzaccaro RJ, Soriano T, Bloom BR, Brenner MB, Kronenberg M, Brennan PJ (1995) CD1-restricted T cell recognition of microbial lipoglycan antigens. Science 269:227–230
Relloso M, Cheng TY, Im JS, Parisini E, Roura-Mir C, Debono C, Zajonc DM, Murga LF, Ondrechen MJ, Wilson IA, Porcelli SA, Moody DB (2008) pH-dependent interdomain tethers of CD1b regulate its antigen capture. Immunity 28:774–786
Hunger RE, Sieling PA, Ochoa MT, Sugaya M, Burdick AE, Rea TH, Brennan PJ, Belisle JT, Blauvelt A, Porcelli SA, Modlin RL (2004) Langerhans cells utilize CD1a and langerin to efficiently present nonpeptide antigens to T cells. J Clin Invest 113:701–708
Prigozy TI, Sieling PA, Clemens D, Stewart PL, Behar SM, Porcelli SA, Brenner MB, Modlin RL, Kronenberg M (1997) The mannose receptor delivers lipoglycan antigens to endosomes for presentation to T cells by CD1b molecules. Immunity 6:187–197
Schaible UE, Winau F, Sieling PA, Fischer K, Collins HL, Hagens K, Modlin RL, Brinkmann V, Kaufmann SH (2003) Apoptosis facilitates antigen presentation to T lymphocytes through MHC-I and CD1 in tuberculosis. Nat Med 9:1039–1046
Tailleux L, Schwartz O, Herrmann JL, Pivert E, Jackson M, Amara A, Legres L, Dreher D, Nicod LP, Gluckman JC, Lagrange PH, Gicquel B, Neyrolles O (2003) DC-SIGN is the major Mycobacterium tuberculosis receptor on human dendritic cells. J Exp Med 197:121–127
van den Elzen P, Garg S, Leon L, Brigl M, Leadbetter EA, Gumperz JE, Dascher CC, Cheng TY, Sacks FM, Illarionov PA, Besra GS, Kent SC, Moody DB, Brenner MB (2005) Apolipoprotein-mediated pathways of lipid antigen presentation. Nature 437:906–910
Kasmar AG, van Rhijn I, Cheng TY, Turner M, Seshadri C, Schiefner A, Kalathur RC, Annand JW, de Jong A, Shires J, Leon L, Brenner M, Wilson IA, Altman JD, Moody DB (2011) CD1b tetramers bind {alpha} {beta} T cell receptors to identify a mycobacterial glycolipid-reactive T cell repertoire in humans. J Exp Med 208:1741–1747
Montamat-Sicotte DJ, Millington KA, Willcox CR, Hingley-Wilson S, Hackforth S, Innes J, Kon OM, Lammas DA, Minnikin DE, Besra GS, Willcox BE, Lalvani A (2011) A mycolic acid-specific CD1-restricted T cell population contributes to acute and memory immune responses in human tuberculosis infection. J Clin Invest 121:2493–2503
Ulrichs T, Moody DB, Grant E, Kaufmann SH, Porcelli SA (2003) T-cell responses to CD1-presented lipid antigens in humans with Mycobacterium tuberculosis infection. Infect Immun 71:3076–3087
van Rhijn I, Nguyen TK, Michel A, Cooper D, Govaerts M, Cheng TY, van Eden W, Moody DB, Coetzer JA, Rutten V, Koets AP (2009) Low cross-reactivity of T-cell responses against lipids from Mycobacterium bovis and M. avium paratuberculosis during natural infection. Eur J Immunol 39:3031–3041
Spada FM, Grant EP, Peters PJ, Sugita M, Melian A, Leslie DS, Lee HK, van Donselaar E, Hanson DA, Krensky AM, Majdic O, Porcelli SA, Morita CT, Brenner MB (2000) Self-recognition of CD1 by gamma/delta T cells: implications for innate immunity. J Exp Med 191:937–948
Briken V, Jackman RM, Watts GF, Rogers RA, Porcelli SA (2000) Human CD1b and CD1c isoforms survey different intracellular compartments for the presentation of microbial lipid antigens. J Exp Med 192:281–288
Sugita M, van Der WN, Rogers RA, Peters PJ, Brenner MB (2000) CD1c molecules broadly survey the endocytic system. Proc Natl Acad Sci USA 97:8445–8450
Beckman EM, Melian A, Behar SM, Sieling PA, Chatterjee D, Furlong ST, Matsumoto R, Rosat JP, Modlin RL, Porcelli SA (1996) CD1c restricts responses of mycobacteria-specific T cells. Evidence for antigen presentation by a second member of the human CD1 family. J Immunol 157:2795–2803
Moody DB, Ulrichs T, Muhlecker W, Young DC, Gurcha SS, Grant E, Rosat JP, Brenner MB, Costello CE, Besra GS, Porcelli SA (2000) CD1c-mediated T-cell recognition of isoprenoid glycolipids in Mycobacterium tuberculosis infection. Nature 20(404):884–888
Matsunaga I, Bhatt A, Young DC, Cheng TY, Eyles SJ, Besra GS, Briken V, Porcelli SA, Costello CE, Jacobs WR Jr, Moody DB (2004) Mycobacterium tuberculosis pks12 produces a novel polyketide presented by CD1c to T cells. J Exp Med 200:1559–1569
de Jong A, Arce EC, Cheng TY, van Summeren RP, Feringa BL, Dudkin V, Crich D, Matsunaga I, Minnaard AJ, Moody DB (2007) CD1c presentation of synthetic glycolipid antigens with foreign alkyl branching motifs. Chem Biol 14:1232–1242
Scharf L, Li NS, Hawk AJ, Garzon D, Zhang T, Fox LM, Kazen AR, Shah S, Haddadian EJ, Gumperz JE, Saghatelian A, Faraldo-Gomez JD, Meredith SC, Piccirilli JA, Adams EJ (2010) The 2.5 a structure of CD1c in complex with a mycobacterial lipid reveals an open groove ideally suited for diverse antigen presentation. Immunity 33:853–862
Hiromatsu K, Dascher CC, Leclair KP, Sugita M, Furlong ST, Brenner MB, Porcelli SA (2002) Induction of CD1-restricted immune responses in guinea pigs by immunization with mycobacterial lipid antigens. J Immunol 169:330–339
Watanabe Y, Watari E, Matsunaga I, Hiromatsu K, Dascher CC, Kawashima T, Norose Y, Shimizu K, Takahashi H, Yano I, Sugita M (2006) BCG vaccine elicits both T-cell mediated and humoral immune responses directed against mycobacterial lipid components. Vaccine 24:5700–5707
Dascher CC, Hiromatsu K, Xiong X, Morehouse C, Watts G, Liu G, McMurray DN, Leclair KP, Porcelli SA, Brenner MB (2003) Immunization with a mycobacterial lipid vaccine improves pulmonary pathology in the guinea pig model of tuberculosis. Int Immunol 15:915–925
Nguyen TK, Koets AP, Santema WJ, van Eden W, Rutten VP, van Rhijn I (2009) The mycobacterial glycolipid glucose monomycolate induces a memory T cell response comparable to a model protein antigen and no B cell response upon experimental vaccination of cattle. Vaccine 27:4818–4825
Felio K, Nguyen H, Dascher CC, Choi HJ, Li S, Zimmer MI, Colmone A, Moody DB, Brenner MB, Wang CR (2009) CD1-restricted adaptive immune responses to Mycobacteria in human group 1 CD1 transgenic mice. J Exp Med 206:2497–2509
Lockridge JL, Chen X, Zhou Y, Rajesh D, Roenneburg DA, Hegde S, Gerdts S, Cheng TY, Anderson RJ, Painter GF, Moody DB, Burlingham WJ, Gumperz JE (2011) Analysis of the CD1 antigen presenting system in humanized SCID mice. PLoS ONE 6:e21701
Li D, Hong A, Lu Q, Gao GF, Jin B, Screaton GR, Xu XN (2012) A novel role of CD1c in regulating CD1d-mediated NKT cell recognition by competitive binding to Ig-like transcript 4. Int Immunol 24(11):729–737
Li D, Wang L, Yu L, Freundt EC, Jin B, Screaton GR, Xu XN (2009) Ig-like transcript 4 inhibits lipid antigen presentation through direct CD1d interaction. J Immunol 182:1033–1040
Ochoa MT, Stenger S, Sieling PA, Thoma-Uszynski S, Sabet S, Cho S, Krensky AM, Rollinghoff M, Nunes Sarno E, Burdick AE, Rea TH, Modlin RL (2001) T-cell release of granulysin contributes to host defense in leprosy. Nat Med 7:174–179
Sieling PA, Ochoa MT, Jullien D, Leslie DS, Sabet S, Rosat JP, Burdick AE, Rea TH, Brenner MB, Porcelli SA, Modlin RL (2000) Evidence for human CD4+ T cells in the CD1-restricted repertoire: derivation of mycobacteria-reactive T cells from leprosy lesions. J Immunol 164:4790–4796
Stenger S, Mazzaccaro RJ, Uyemura K, Cho S, Barnes PF, Rosat JP, Sette A, Brenner MB, Porcelli SA, Bloom BR, Modlin RL (1997) Differential effects of cytolytic T cell subsets on intracellular infection. Science 276:1684–1687
Stenger S, Hanson DA, Teitelbaum R, Dewan P, Niazi KR, Froelich CJ, Ganz T, Thoma-Uszynski S, Melian A, Bogdan C, Porcelli SA, Bloom BR, Krensky AM, Modlin RL (1998) An antimicrobial activity of cytolytic T cells mediated by granulysin. Science 282:121–125
Behar SM, Podrebarac TA, Roy CJ, Wang CR, Brenner MB (1999) Diverse TCRs recognize murine CD1. J Immunol 162:161–167
Jahng A, Maricic I, Aguilera C, Cardell S, Halder RC, Kumar V (2004) Prevention of autoimmunity by targeting a distinct, noninvariant CD1d-reactive T cell population reactive to sulfatide. J Exp Med 199:947–957
van Rhijn I, Young DC, Im JS, Levery SB, Illarionov PA, Besra GS, Porcelli SA, Gumperz J, Cheng TY, Moody DB (2004) CD1d-restricted T cell activation by nonlipidic small molecules. Proc Natl Acad Sci U S A 101:13578–13583
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Van Rhijn, I., Ly, D., Moody, D.B. (2013). CD1a, CD1b, and CD1c in Immunity Against Mycobacteria. In: Divangahi, M. (eds) The New Paradigm of Immunity to Tuberculosis. Advances in Experimental Medicine and Biology, vol 783. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-6111-1_10
Download citation
DOI: https://doi.org/10.1007/978-1-4614-6111-1_10
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-6110-4
Online ISBN: 978-1-4614-6111-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)