Abstract
Patellofemoral disorders can be divided into those that primarily cause pain and those that cause instability. Lateral tracking, malalignment, and a tight lateral retinaculum are anatomic factors that can increase joint reactive forces resulting in pain and chondral damage. Patella alta, trochlear dysplasia, lateral tracking vector, and MPFL deficiency can be associated with patella instability. Tibia tubercle osteotomy can be used to treat pain and instability in cases that demonstrate malalignment and a lateral tracking vector. This chapter will define indications for tibia tubercle transfer, review anatomic and biomechanical factors associated with the technique, and highlight important technical considerations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Anterior knee pain is a common complaint among athletes. Although the etiology of the knee pain is not always clearly delineated, it is often associated with patellofemoral anatomic abnormalities. Common examples are abnormal lateral patella tracking leading to increased joint reactive forces resulting in pain, with or without chondral wear. Traumatic patella dislocations can lead to painful and debilitating lateral laxity resulting in recurrent subluxations with a patella “jump” when entering the trochlea or even chronic instability. Chronic patella instability is not common with a single traumatic patella dislocation, but with certain risk factors, recurrent instability can occur: patella alta, trochlea dysplasia, rotational malalignment, and extensor mechanism valgus (as represented by increased Q angle or elevated TT–TG distance). In patients with “anterior knee pain,” it is very important to systematically delineate activity-related pain from patella instability as the primary complaint in order to appropriately treat the pathology. Unfortunately, it is not uncommon for the two to be found concurrently.
The tibia tubercle osteotomy has the ability to change the orientation of the extensor mechanism by which it can be a powerful tool to treat multiple complaints within the patellofemoral compartment. The power of this osteotomy is related to the ease of surgical exposure and the multi-planar corrections possible. Osteotomy cuts can be made to accommodate alignment changes within the coronal, axial, and sagittal planes. Consequently, osteotomy has a variety of functions; it can alter the area and amount of joint contact pressures, decrease the patella height to allow for earlier patella capture, and decrease the lateral displacement force vector. Understanding the effects each plan has on the function and forces within the patellofemoral joint during activity allows the surgeon to treat both pain and instability in this population. There are subtle complexities with this type of surgery that requires an understanding of the pathophysiology of the condition and knowledge of the effects of a given surgical treatment on the mechanics and biology of patellofemoral function for optimal outcomes.
Fortunately, nonoperative treatments are very effective and should be exhausted prior to surgical intervention. The described measures include quadriceps and hip flexor/external rotator strengthening, extensor mechanism stretching, core stability training, McConnell taping, and patella bracing.
The purpose of this chapter is to define the situations in which tibial tubercle transfer is indicated for anterior knee pain and/or patellar instability. In this chapter, we will attempt to present a brief overview of the anatomic and biomechanical factors important to decision-making and then present techniques for the treatment of these issues with osteotomies about the tibia tubercle.
Patient Selection and Osteotomy Selection
Patients presenting with patellofemoral pain may or may not have instability. Anterior knee pain can be generated by a variety of factors that may not be addressed by adjusting the position of the tibia tubercle. Patient selection and workup are critical to successful treatment. Quadriceps weakness is one of the most common causes of anterior knee pain as joint forces are increased in the setting of weak and/or stiff extensor mechanism that has a clear function in absorbing energy during gait [1]. In the athletic population, flexibility imbalance, iliotibial band friction syndrome, vastus lateralis tendinitis, lateral retinacular strain or contracture, patellar or quadriceps insertional tendinitis, and plica or fat pad syndrome have all been described and would need to be treated conservatively [2, 3]. The workup of patients with activity-related anterior knee pain and chronic injury to the posterior cruciate ligament must also be ruled out. Posterior tibia laxity can lead to retropatellar pain as the extensor mechanism holds the tibia from posterior subluxation and leads to increased patellofemoral contact pressures resulting in pain [4, 5]. It is important to take a rational approach to patellofemoral disorders that require an understanding that various problems may be related to combinations of articular pain, soft tissue pain, and pain resulting from lateral instability of the joint. Therefore, a careful examination is indispensable for an accurate diagnosis of patellofemoral disorders. We feel it is imperative that a diagnosis of patellofemoral pain is dependent on the physician’s ability to reproduce the patient’s complaints by physical examination. The examination can suggest or determine an underlying malalignment pattern, abnormally tight soft tissue structures, generalized ligamentous laxity, or patterns of tenderness, which are all critical to understanding the pathophysiology of each individual and thus the correct application of an osteotomy to correct a malalignment or alter the patellofemoral joint contact pressures.
Understanding the Q Angle or Lateral Force Vector
The quadriceps angle (Q angle) is a clinical assessment of the angle made by the attachment vector of the extensor mechanism and the relationship of the quadriceps tendon to the tibia tubercle (Fig. 7.1). The angle is classically measured in extension from the anterior superior iliac spine to the midpoint of the patella that forms the angle between patella tendons force vector to the tibial tuberosity (Fig. 7.1). An increased angle leads to an increase in the lateral vector of quadriceps force, which may increase tension in the medial soft tissue restraints and may lead to an increased tendency toward lateral patellar translation or subluxation, especially in the patient with a concomitant dysplasia of the trochlea [6]. Measurements of the Q angle have been made while the patient is supine and standing. We favor the standing measurement because it includes physiologic loading. Unfortunately, the Q angle also has not been proved to correlate with the incidence of pain or the results of treatment [7]. Although the importance of understanding the lateral extensor moment and its potential effects on patellar alignment is undeniable, the role of Q angle measurement is less clear. It should be noted that there is significant variability within populations and differences between males and females. Ranges have been reported to be 14–23° within a normal, asymptomatic population [3, 7–9]. There is a dynamic component, and thus, examine the patient while standing and ambulating for evidence of an increased Q angle, torsional deformities of the femur or tibia, knee varus/valgus, pronation of the hindfoot, leg length discrepancy, ankle deformity, scars, and other factors that may affect patellar alignment. One clinical test to examine function changes in Q angle related to poor proximal muscular control and hip external rotator weakness is to have the patient perform a single-leg knee bend while you watch from the front. A positive test results in the knee rolling inward, increasing valgus and suggesting weakness of external rotation at the hip, a known and important variable leading to torsional changes and anterior knee pain [10, 11].
A better estimation of the functional malalignment is measuring the distance between the tibia tubercle and the trochlea groove (TT–TG distance) on CT scan or MRI as it directly estimates the correctable static distance between the points of articulation and attachment of the extensor mechanism [12]. Dejour and associates first described this measurement and found, upon comparing normal patients with those with patellar instability, that the threshold for normal was 20 mm [13]. This measurement is done by measuring the lateral distance of the tibial tuberosity from the most posterior point in the femoral sulcus, along a line parallel to the axis of the posterior femoral condyles (Fig. 7.2). Certainly there is a spectrum of anatomic malalignment in the form of increased TT–TG distances. These increased distances have been associated and found in patients with recurrent patella instability [3, 13, 14]. A recent report looking at patients with instability or anterior knee pain associated with “pathologic” TT–TG malalignment determined to be 15 mm or greater. The authors concluded that both stability and pain were corrected with isolated anteromedialization osteotomy procedures [15]. Based on expert opinion from the Patellofemoral Society Members [16], a TT-TG distance of 20 mm or greater is considered “severely abnormal” and blue bone needs to be addressed surgically a re-adjustment osteotomy to correct the increased lateral vector. The amount of medialization needed can also be estimated from this measurement, and the most often targeted goal for postoperative TT–TG distance is less than approximately 10 mm. Measurement of the TT–TG is helpful in confirming that tuberosity medialization is appropriate in a clinical situation that otherwise warrants medial or anteromedial transfer.
Determination of the tibia tubercle to trochlea groove (TT–TG) distance on a CT scan axial in which cuts at the deepest section of the trochlea groove are measured to the highest point on the tibia tubercle. Representation of three techniques to determine distance; (a) posterior condyle axis is used as reference to ensure no rotational effect and perpendicular line is drawn in center of groove and tubercle. (b) On a free software package OsiriX© a reference point can be placed and “fixed” as the axial cuts are scrolled to the groove and distance measured. (c) During CT reformatting, the axial cuts can be superimposed to allow for a direct measurement. Note: The TT–TG distance should represent a true lateral distance and not have a rotational or radius component
Standing anteroposterior films are important to search for confounding sources of pain such as arthrosis or mechanical axis abnormalities, which need to be confirmed by measurements from a standing hip to ankle X-ray. The true lateral knee image provides the most information as it can delineate patella alta and estimate trochlea dysplasia; both are important variables in determining the need and type of tubercle osteotomy to perform. A normal ratio of patellar tendon length to patellar length of less than 1.2 has been described by Insall and Salvati [17]. However, we prefer the Blackburne and Peel [18] method as it accounts for changes in patella osteology and imperfect lateral X-rays better. The measurement represents the ratio of the articular length of the patella to the height of the lower pole of the patellar articular cartilage above the tibial articular surface (normal, <1.0). If patella alta is present, a distalization osteotomy may be considered to allow for “earlier” capture of the patella during flexion that can lead to increased stability if significant dysplasia is not present.
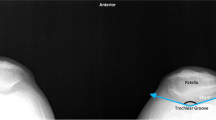
Axial tangential views of the patellofemoral joint, such the one described by Merchant et al. [19], may be used as screening tests for malalignment but can be difficult to interpret because of image overlap (unless the image is precisely tangential to the joint). Other radiographic variables that may affect the decision to perform a distal osteotomy include the congruence angle of Merchant and Mercer and the lateral patellofemoral angle of Laurin and Dussault (both are estimations of lateral subluxation and tilt, respectively). The symmetry of subchondral sclerosis of the patellar facets should also be evaluated for signs of localized sclerosis (indicating unbalanced stress) [6]. Kujala and Kormano [20] emphasized imaging of the patellofemoral joint in early flexion. They found greater magnetic resonance imaging (MRI) differences in tilt and lateral subluxation on views with less than 30° of flexion in a group of patients with recurrent patellar dislocations than in a normal control group. Computed tomography (CT) provides a fast, low-cost way of determining amount of dysplasia, flexion angle at which the patella is captured, and helps to define malalignment in the form of increased distance from the tibia tubercle to the center of the trochlea groove (TT–TG distance) which serves as a anatomic Q angle. The use of CT scans was first suggested by Delgado-Martins [21] in 1979 as he described its use in a series of 24 patients looking at patella–trochlea contact with increasing knee flexion angles. These studies are not used for diagnosis but in patients being considered for surgical correction to understand the anatomy needed to be corrected to provide stability. We are currently utilizing a CT tracking study protocol in which the patients have four sections taken at 5 mm through the patellofemoral articulation at 0, 10, 20, 30, 40, and 50° of knee flexion followed by a full scan at 1.25 mm in extension (Fig. 7.3). This provides information regarding the articulation of the patella during knee flexion and identifies the flexion angle at which the patella is fully captured and allows us to quantify the amount of trochlea dysplasia present.
An example of CT tracking images, bilateral axial cuts at 0, 10, 20, and 30° of knee flexion, in a patient with right recurrent patella instability and demonstrates Dejour C dysplasia (based on lateral X-ray, not included). Images show lateral patella tracking with incomplete patella capture even at 30° of knee flexion
Anterior Knee Pain and Chondral Pressures
Vague anterior knee pain is common in the athlete and can be associated with overuse that leads to soft tissue inflammation and pain within the peripatellar tissue or fat pad. These typically respond to activity modification in addition to stretching and strengthening of the fatigued and tight muscle groups, quadriceps. However, pain can also develop from an imbalance created from malalignment within the quadriceps–patella–tibia tubercle relationship which affects lateral facet contact pressures. This lateral malalignment, or elevated Q angle, can produce increased contact pressures within the lateral facet of the patella and degradation of the overloaded cartilage [22–26]. Through a concept of “edge” loading and repeated motion, cartilage lesions can lead to increase the pressure applied to the surrounding cartilage, which can overload the subchondral bone and activate the nociceptive fibers in the bone, causing pain [27]. By moving the tibia tubercle 10 mm medial, a reduction of 15 % of the contact pressures can be observed at knee flexion angles of 60 and 80° [24].
Approach to Distal Realignment Procedures (Fig. 7.4)
Medialization of the Tibia Tubercle
Roux in 1888 was the first to report tibia tubercle realignment osteotomy coupled with lateral release and medial plication in the treatment of recurrent patellar dislocation [3]. Later this technique to treat patella instability was adapted and described by Hauser in 1938. Medial transfer of the tubercle has the effect of decreasing the lateral extensor vector [28]. This procedure moved the tubercle distal and medial with an effective posterior displacement of the tubercle that leads to an increased incidence (~70 %) of patellofemoral arthrosis at 7.3, 16, and 18 years after the procedure [29–31]. The Roux–Elmslie–Trillat procedure is a pure distal realignment technique because it provides isolated medialization without transferring the tibial tubercle anteriorly [3]. The Roux–Elmslie–Trillat procedure involves a lateral retinacular release of the knee, medial capsular reefing, and medial displacement of the infrapatellar tendon hinged on a distal periosteal attachment. This procedure has been shown to demonstrate maintained correction of the extensor angle and has been reported with good results to control patella stability [32] especially if combined with a proximal procedure [33]. This procedure has limited use as it can only produce pure medial realignment, and there does exist the risk of painful hardware and osteotomy nonunion as the osteotomy surface area is limited.
Recommendations: Pure medialization procedure is reserved for patients with mild elevation in quadriceps angle as minimal correction can be obtained. Bone contact is minimal with more medialization as the medial cortex curves posterior.
Distalization of the Tibia Tubercle
The role for distalizing the tibia tubercle in isolation is very limited. It can be used to correct anterior knee pain associated with patella alta [34]. In patients without instability and mild grade 2 chondromalacia at greater than 2 years, there were improved Kujala scores compared to baseline or preoperative values [34]. However, in patients with higher grades of patella chondromalacia, their scores did not demonstrate significant improvement.
Patella alta is rarely an isolated finding and it is most often a symptom of a regional patellofemoral dysplasia with four major instability factors, i.e., trochlear dysplasia, patella alta, excessive TT–TG, and patellar tilt all contributing to the pain and instability. In patients with abnormal patella height leading to late trochlear capture, stability and pain are improved with a combined osteotomy to distalize and medialize the tubercle. Caton and Dejour describe having a 75 % success rate with a combined procedure to produce a stable patellofemoral articulation in a series of 50 patients with chronic instability with young age [35].
Recommendations: A pure distalization osteotomy procedure is rarely indicated. In the clinical setting of a patient with chronic patella instability and elevated Blackburne–Peel (Fig. 7.5) or Caton–Deschamps index, then a distalizing tubercle osteotomy in addition to medialization or anteromedialization should be strongly considered.
Anteriorization of the Tibia Tubercle
In 1990, Fulkerson et al. (Fulkerson JP) reported a tubercle osteotomy known as anteromedialization to achieve dual plan realignment and address some of the complications associated with the Maquet procedure [36]. Specifically this osteotomy (AMZ) technique is designed to address patellofemoral pain found in conjunction with patellar maltracking. The osteotomy is made in an oblique fashion that allows for simultaneous anteriorization and medialization of the tibial tubercle (Fig. 7.6). Additionally, it produces a large surface area for healing of the osteotomy and to accommodate multiple bi-cortical screws to be placed in compression to optimize healing of the osteotomy. One advantage of this osteotomy is the variability that can be produced by varying the angle of the osteotomy. Therefore, the tubercle can be biased to a more anterior or more medial position and be “dialed” to the patients needs. Over the last 15 years, the indications for this procedure have evolved significantly. It is now commonly used in conjunction with patellofemoral cartilage resurfacing procedures as well as improved objective measures of patellar alignment, contact area, and forces. Results combining AMZ with PF cartilage restorative procedures such as autologous chondrocyte implantation and osteoarticular grafting procedures within the PF compartment have demonstrated superior results to either procedure performed independently [37–40].
Indications for Anteromedialization of the Tibial Tubercle
Osteotomies to the tibia tubercle can be performed in isolation or in combination with a proximal procedure when patella instability or lateral patella instability is the primary patient complaint. It can produce excellent clinical results in patients with lateral tracking and arthritis wear secondary to increased contact pressures in deeper knee flexion.
For the treatment of anterior knee pain associated with lateral facet chondral wear, an anteromedialization (AMZ) of the tibial tubercle is a powerful surgical technique. It will reduce loading of the lateral and distal PF joint by transferring load medially and proximally on the patella [3, 24, 25]. Therefore, the procedure is most appropriate and beneficial for those patients with symptomatic lateral tracking of the patella, usually because the patella alignment vector is abnormally lateral; this leads to excessive loading of the distal patella cartilage. In patients with malalignment, the lateral facet strikes the lateral trochlea as the patella engages the trochlea and receives accentuated contact pressures until it becomes fully centered within the trochlea deeper knee flexion. These patients may or may not have instability, but pain is the primary complaint.
In some patients, this abnormal tracking pattern may be difficult to identify without computerized tomography with mid patella transverse images at 0, 15, 30, and 45° knee flexion to prove that the patella is entering the central trochlea late in knee flexion, thereby resulting in prolonged and excessive lateral and distal articular loading of the patella. An osteotomy that can anteriorize the tubercle reduces load on the distal and lateral facet joint that has become painful as a result of the chronic, abnormal overload [3, 24, 25].
Because of the reduced contact pressures produced with this technique, AMZ has proven useful in conjunction with articular cartilage resurfacing procedures [37–41]. The obliquity of the AMZ osteotomy should be designed to optimally unload the resurfaced area. A short, steep AMZ can provide substantial and even complete relief of pain in the patient with distal patella articular softening related to late entry of the patella into the trochlea.
Another advantage of the AMZ osteotomy is correction of extensor malalignment and secondary rotational abnormalities that can lead to increased lateral force during active knee flexion. In the patient with attenuated medial restraints and with a shorted, dysplastic trochlea, it can help to obtain stability and protect the proximal reconstruction. Typically it is indicated in the treatment of patella instability in patients in whom the TT–TG relationship is grossly abnormal (>20 mm), the Q angle is abnormally high (>20), and the distal/lateral patella will benefit from reduced load. In patients with patella alta, the patella may be moved distally by removing a predetermined amount of bone distally from the osteotomy fragment.
In patients with patella baja and infrapatellar contracture, a steep AMZ may be used to distract the released contracture and also slide the extensor mechanism proximally as needed before screw fixation of the transferred tubercle.
Case Examples
Case 1: Isolated Lateral Patellofemoral Arthrosis
This is a case very common of a 38-year-old woman who has mild malalignment and history of obesity, now 1 year out from a gastric bypass procedure with 145 lb weight loss and progressive anterior knee pain. She has attempted physical therapy for extensor mechanism stretching and strengthening with some success. She wishes to be more active but retropatellar knee pain with stairs and prolonged sitting is becoming very limiting to her. Her current weight is 190 lb. Radiographs demonstrate lateral tracking and arthrosis with large osteophyte (Fig. 7.7a, b) and MRI demonstrates bone edema from increased pressure and bone–bone articulation (Fig. 7.7c). Arthroscopy confirms the lateral compartment bone loss (Fig. 7.7d) and minimal cartilage loss in medial trochlea wall and in the medial/lateral knee compartments. Patient was treated with open osteophyte removal, lateral release and AMZ (native TT–TG was 10), and subchondral drilling of patella and lateral trochlea. Postoperative radiographs demonstrate AMZ (Fig. 7.8). Patient is allowed to immediately start motion postoperative and electrical stimulation is done for quadriceps activation. At 3 months she is almost pain free but with much improved function. This is an example of an intermediate procedure for arthrosis in a younger patient or in a patient with higher activity demands for which arthroplasty is not an option, either isolated patellofemoral or total knee arthroplasty.
Clinical case example 1: (a) lateral radiograph demonstrating isolated patellofemoral arthritis. (b) Merchant view demonstrating a lateral tracking patella with osteophyte and subchondral sclerosis but normal patella tilt angle of Laurin or congruence angle of Merchant. (c) MRI of the same patient noting the lateral facet bone edema with cystic changes present secondary to increased contact pressures and arthritis. (d) Intraoperative arthroscopic image of isolated lateral patellofemoral compartment grade IV cartilage loss and arthritis
Case 2: Recurrent Patella Instability
This is a case example of a 22-year-old college senior with multiple patella dislocations after her first dislocation at age 14. Her first dislocation occurred while running and turning while playing soccer. She currently significantly limits her activities secondary to patella instability and intermittent pain with effusions following subluxation events which occur one to two times per week. She does have decreased symptoms with lateral stabilization brace and mild obesity and has attempted physical therapy on several occasions with a focus on hip external rotators and gait training. Her exam demonstrates clear apprehension with lateral directed patella force in extension, 3+ quadrant glide before she removes your hand, J tracking, pain with patella load, and measured Q angle of 19–20 with 20° of flexion. Knee series and CT tracking studies demonstrate patella alta (ratio 1.8) and type C trochlea dysplasia (Fig. 7.9), and her TT–TG distance is measured to be 24 (Fig. 7.10). This case demonstrates the situation where a proximal MPFL procedure was done in addition to combining a distalization of 8 mm to the AMZ tibia tubercle osteotomy secondary to her dysplasia and alta (Fig. 7.11). Postoperative course was excellent with no reported instability at 6 M; repeat radiographs demonstrate correction of patella alta with distalization/AMZ osteotomy (Fig. 7.12).
Clinical case example 2: preoperative to postoperative comparison lateral radiograph demonstrating the patella alta correction and new measurement by Blackburne–Peel index. Note: The goal is not a complete or over correction, but simply to provide enough correction to affect “earlier” entrance of the patella into the trochlea
Author’s Preferred Techniques
Technique of AMZ
Preoperative planning provides the critical information needed to design an AMZ osteotomy. Since the operation involves moving the tibial tubercle medially as well as anteriorly, the preoperative indication is lateral patella tracking with excessive pressure on the lateral patella and trochlea facets. Distal patella articular damage will also benefit from unloading following and anteriorization osteotomy. Suffice it to say that the AMZ procedure should provide improved tracking of the patella (putting it into a balanced, centered, mechanically desirable relationship with the trochlea throughout flexion and extension of the knee) while optimizing articular contact in the patellofemoral joint by shifting the patella off of damaged and/or painful articular surfaces and onto better cartilage more medially and proximally on the patella.
Anteromedial tibial tubercle transfer starts with an arthroscopy using low anteromedial and lateral portals to fully examine the knee. Patellofemoral tracking and alignment, with and without fluid in the knee, dysplasia, displaceability of the patella, and documentation of location and extent of articular damage should be assessed. The surgeon may then determine how much anteriorization and medialization are appropriate when designing the osteotomy. A more oblique osteotomy will achieve anteriorization, thereby unloading or reduce the contact pressures within the distal articular cartilage; a more flat osteotomy will produce a more medial translation of the patella tendon resulting in a medial shift within the patella–trochlea articular contact. During the history, chief complaint, clinical examination, and lastly with imaging, the balance of medial and anterior transfer is considered and decided preoperatively, which is implemented by designing the osteotomy obliqueness according to each patient’s need. Of note, the concomitant problem of excessive patella alta can be addressed by planning some amount osteotomy bone removal that produced a distal displacement of the tubercle to allow for patella alta normalization.
Limited lateral release at the time of arthroscopy is helpful in many cases, particularly releasing any infrapatellar scar or abnormal tether that will restrict the desired patella displacement. Because the osteotomy will create some anteriorization, the release is distracted and therefore scarring down is very uncommon.
The skin incision placement is important and is positioned just lateral to the tubercle, so when the osteotomy is medialized, it is away from the incision site (Fig. 7.13). It extends usually for a length of 5–6 cm depending on how long the surgeon wises to make the osteotomy and should be made judiciously during the first 10–20 procedures, and a shorted skin incision places the patient at risk for damage to the skin during osteotomy creation that can impact healing or cosmetics of the wound (Fig. 7.13).
The distal patella tendon is exposed such that a hemostat may be placed behind the tendon (Fig. 7.14). The anterior compartment is then incised along its anterior edge and reflected off of the lateral tibia with a large periosteal elevator. This careful elevation should expose the junction of the lateral and posterior tibia, and then a large retractor exposes the entire lateral tibia over the extent of the planned osteotomy before starting the osteotomy itself. Thereby, the surgeon will have a complete exposure of the saw blade as it comes through the lateral tibia and avoid any possibility of neurovascular injury (the anterior tibial artery and the deep peroneal nerve run just behind the posterolateral tibia at the osteotomy level).
The obliquity of the osteotomy may be determined in several ways and guides are available for this purpose. My preferred technique however requires a free hand cut after studying the proximal tibia geometry using an oscillating saw. First the line along the anteromedial tibia where the osteotomy will be medial is defined and marked with the electrocautery. Important: the osteotomy line must be drawn such that the osteotomy is tapered to the anterior tibial cortex at the osteotomy’s distal extent (Fig. 7.15). For osteotomies intended to provide mainly medial translation with a flat cut, less obliquity, the osteotomy starts more posteriorly, often a centimeter medial to the medial patella tendon insertion. For a steeper osteotomy, the bone cut will start very close to the medial patella tendon insertion (Fig. 7.15b).
Intraoperative pictures of freehand creation of the osteotomy (a, b) with the saw blade cutting from medial to lateral in a sloped position. The more shallow the slope (a) and the more medial and less anterior the osteotomy created, the steeper the cut an increase in anterior tubercle placement is made (c). A few systems designed to help “guide” the cut angle with more precise measurement are available; the system demonstrated is the AMZ Tracker System©
The osteotomy cut is created slowly such that the surgeon visualizes the desired obliquity, watching the saw blade from above and below and assuring that the saw will exit the lateral tibia at the desired level of the lateral tibial cortex (Fig. 7.15a, b). The saw should always exit the lateral tibia first at the most distal aspect of the osteotomy which is the most anterior and therefore safest part of the bone cut. The remainder of the cut then is watched by direct vision as the saw cuts more proximally and therefore exits the lateral tibia more posteriorly at its most proximal extent. The saw blade exit must be watched at all times.
At this point, I prefer to use a large Lambotte osteotome to connect the lateral, proximal extent of the osteotomy, at its posterior extent, to a point just proximal to the lateral patella tendon insertion (Fig. 7.16).
The final cut is made with a ½ in. osteotome by retracting the patella tendon anteriorly and then cutting straight across to meet the medial proximal extent of the osteotomy.
Once these cuts have been completed, it is typically easy to complete the osteotomy by placing a large osteotome into the osteotomy. The osteotomy fragment is elevated anteriorly, thereby creating a small greenstick fracture at its distal extent so that the released osteotomy fragment may be rotated anteromedially using the distal end as the pivot point (Fig. 7.17). At this point, it is imperative to assess the patella by fixing the osteotomy transiently with a drill bit or two K-wires and taking the knee through a flexion arc. I like to use the arthroscope for this purpose to visualize under direct the improvement and more medial tracking that should be noticed in flexion ranges from 20 to 60°. The patella should never be placed into a medial tracking configuration by which the lateral trochlea wall is not contacted. The potential for over correction medial is real, especially if a medial chondral lesion is present and the procedure is being done for instability.
The osteotomy is then secured in the desired position with two fully threaded cortical screws, using lag technique (Fig. 7.18). Typically use 4.5 mm self-tapping screws, overdrilled to provide compression (lag mode) within the near cortex or entry hole to 4.5, and then drill the posterior cortex to 3.2 mm. To prevent fracture, the screws should be placed a minimum of one distal to the patella tendon insertion and a minimum of 2 cm apart from each other. If the size of the osteotomy will not accommodate this spacing, a larger screw can be used, but we would favor using smaller screw and two points of fixation to prevent rotation around a central fixation point. Assuming the fragment has been moved accurately along the osteotomy plane, the fixation of this displaced fragment is very secure. Nonunion is very rare when this is done properly.
Intraoperative image of various fixations for osteotomy after translation. (a) Smaller osteotomy with single bi-cortical 4.5 cortical screw in lag mode with countersink. (b) Two 3.5 bi-cortical screws with washer—typically used for an older patient with concerns of softer bone and need for increased surface area contact on the near cortex. (c) Typical fixation of two 3.5 bi-cortical placed with overdrilling of the near cortex to get compression of osteotomy and countersink of the near cortex to decrease the screwhead prominence
After release of the tourniquet, one should control any soft tissue bleeding and do a final evaluation of the patella tracking arthroscopically. This is a critical step as it is extremely important to avoid any medial tracking as this will lead to problems.
Following AMZ, the retinacular tissues both medially and laterally must be evaluated, and reconstruction, restoration, or release is performed as needed. In patients with trochlea dysplasia increases, the need for balanced retinacular restoration is important as the risk of recurrent instability is greater. In all cases, it is imperative to avoid excessive lateral release and to restore lateral as well as medial retinacular restraints to prevent medial as well as lateral instability. Examination on the OR table after AMZ is the ideal time to determine if the patella may be excessively displaceable as a result of deficient retinacular restraints. In some cases, all that is needed are a few imbrications sutures to restore normal balance.
Postoperative Management
Postoperatively, all patients should start a single arc of knee flexion daily within a few days of surgery. Most patients can achieve a 90 bend within 2–3 weeks. They should use a knee immobilizer for 5 weeks and crutches for 6–8 weeks in most case. Physical therapy for further motion, strength, and progressive weight bearing starts at 5–6 weeks postoperative. Many patients are off crutches by the eighth postoperative week.
References
Winter DA. Energy generation and absorption at the ankle and knee during fast, natural, and slow cadences. Clin Orthop Relat Res. 1983;175:147–54.
Fulkerson JP. Evaluation of the peripatellar soft tissues and retinaculum in patients with patellofemoral pain. Clin Sports Med. 1989;8:197–202.
Post WR, Fulkerson JP. Distal realignment of the patellofemoral joint: indications, effects, results, and recommendations, Chapter 61. In: Insall JN, Scott WN, editors. Surgery of the knee. 5th ed. Amsterdam: Elsevier; 2012.
Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21:132–6.
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, Li G. The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med. 2004;32(1):109–15.
Bicos J, Carofino B, Andersen M, Schepsis AA, Fulkerson JP, Mazzocca A. Patellofemoral forces after medial patellofemoral ligament reconstruction: a biomechanical analysis. J Knee Surg. 2006;19(4):317–26.
Post W. History and physical examination of patients with patellofemoral disorders. In: Fulkerson J, editor. Disorders of the patellofemoral joint. Baltimore, MD: Williams & Wilkins; 1997.
Insall J, Falvo KA, Wise DW. Chondromalacia patellae: a prospective study. J Bone Joint Surg Am. 1976;58:1.
Fairbank JCT, Pynsent PB, van Poortvliet JA, et al. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Am. 1984;66:685.
Piva SR, Goodnite EA, Childs JD. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801.
Willson JD, Binder-Macleod S, Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36(8):1587–96.
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13(1):26–31.
Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26.
Balcarek P, Jung K, Frosch KH, Stürmer KM. Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med. 2011;39(8):1756–61.
Koëter S, Diks MJ, Anderson PG, Wymenga AB. A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br. 2007;89(2):180–5.
Farr J, Cole B, Kercher J, Lachlan B, Sarvottam B. Anterior tibial tubercle osteotomy (Fulkerson osteotomy), Chapter 40. In: Vicente Sanchis-Alfonso, editor. Anterior knee pain and patellar instability. 2nd ed. Berlin: Springer; 2011.
Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–4.
Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241–2.
Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391–6.
Kujala UM, Kormano OK. Patellofemoral relationships in recurrent patellar dislocation. J Bone Joint Surg Br. 1979;71:788–92.
Delgado-Martins H. A study of the position of the patella using computerized tomography. J Bone Joint Surg Br. 1979;61:443–4.
Elias JJ, Kilambi S, Goerke DR, Cosgarea AJ. Improving vastus medialis obliquus function reduces pressure applied to lateral patellofemoral cartilage. J Orthop Res. 2009;27:578–83.
Ramappa AJ, Apreleva M, Harrold FR, Fitzgibbons PG, Wilson DR, Gill TJ. The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. Am J Sports Med. 2006;34:749–56.
Saranathan A, Kirkpatrick MS, Mani S, Smith LG, Cosgarea AJ, Tan JS, Elias JJ. The effect of tibial tuberosity realignment procedures on the patellofemoral pressure distribution. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2054–61.
Fulkerson JP, Shea KP. Disorders of patellofemoral alignment. J Bone Joint Surg Am. 1990;72:1424–9.
Saleh KJ, Arendt EA, Eldridge J, Fulkerson JP, Minas T, Mulhall KJ. Operative treatment of patellofemoral arthritis. J Bone Joint Surg Am. 2005;87:659–71.
Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–56.
Hauser EW. Total tendon transplant for slipping patella. Surg Gynecol Obstet. 1938;66:199–214.
DeCesare WF. Late results of Hauser procedure for recurrent dislocation of the patella. Clin Orthop Relat Res. 1979;140:137–44.
Hampson WGJ, Hill P. Late results of transfer of the tibial tubercle for recurrent dislocation of the patella. J Bone Joint Surg Am. 1975;57:209–13.
Juliusson R, Markhede G. A modified Hauser procedure for recurrent dislocation of the patella: a long-term follow-up study with special reference to osteoarthritis. Arch Orthop Trauma Surg. 1984;103:42–6.
Carney JR, Mologne TS, Muldoon M, Cox JS. Long-term evaluation of the Roux-Elmslie-Trillat procedure for patellar instability: a 26-year follow-up. Am J Sports Med. 2005;33(8):1220–3.
Barber FA, McGarry JE. Elmslie-Trillat procedure for the treatment of recurrent patellar instability. Arthroscopy. 2008;24(1):77–81.
Al-Sayyad MJ, Cameron JC. Functional outcome after tibial tubercle transfer for the painful patella alta. Clin Orthop Relat Res. 2002;396:152–62.
Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2):305–9.
Fulkerson JP, Becker GJ, Meaney JA, et al. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490–6.
Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463:187–94.
Minas T, Bryant T. The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res. 2005;436:30–9.
Peterson L, Brittberg M, Kiviranta I, et al. Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med. 2002;30:2–12.
Pascual-Garrido C, Slabaugh MA, L’Heureux DR, Friel NA, Cole BJ. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med. 2009;37 Suppl 1:33S–41.
Gomoll AH, Farr J, Gillogly SD, Kercher JS, Minas T. Surgical management of articular cartilage defects of the knee. Instr Course Lect. 2011;60:461–83.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Edgar, C., Bollier, M., Fulkerson, J.P. (2014). Tibial Tubercle Osteotomies. In: West, R., Colvin, A. (eds) The Patellofemoral Joint in the Athlete. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4157-1_7
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4157-1_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4156-4
Online ISBN: 978-1-4614-4157-1
eBook Packages: MedicineMedicine (R0)