Abstract
Both indoor and outdoor air pollution have been recognized to contribute to global health burden. The reported health effects range from cardiovascular, respiratory diseases, neuronal to cancer. This chapter aims to provide the up-to date details on the mechanisms of carcinogenesis of air pollutants; benzene, formaldehyde, polycyclic aromatic hydrocarbons, environmental tobacco smoke, while identifying common and unique molecular mechanisms of carcinogenesis. Finally, this chapter also discusses about research gaps and future research needs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Air pollution
- Formaldehyde
- Benzene
- Poly cyclic aromatic hydrocarbons
- Environmental Tobacco smoke
- Metabolism
- Carcinogenesis mechanisms
6.1 Introduction
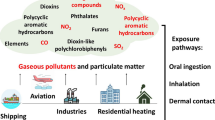
Both indoor and outdoor air pollution is a well-recognized contributory factor to the global health burden and accounts for approximately two million mortalities per year worldwide (World Health Organization (WHO) News release 2011). The exhaust emissions from automobiles, industrial vents, fossil fuel combustion, volatile organic compounds and environmental tobacco smoke (ETS) contribute to outdoor air pollution. The emissions from biomass-burning cooking stoves, radon, and tobacco smoke constitute the majority of indoor air pollution. Scientific evidence both from epidemiology and animal experimental studies over the past few decades has consistently linked exposure to air pollution, especially, the respirable particles to a wide range of health effects such as cardio-respiratory diseases, asthma and chronic obstructive pulmonary disease (COPD) (Narot et al. 2011; Shah et al. 2013; Schluger and Koppaka 2014; Ferkol and Schraufnagel 2014). Children, elderly and people with predisposed health conditions such as asthma are demonstrated to be especially vulnerable to air pollution-induced adverse health effects (Schluger and Koppaka 2014; Ferkol and Schraufnagel 2014; Zar and Ferkol 2014; Esposito et al. 2014).
Air pollution exposure related health effects aroused concern for a long time. The first large epidemiological cohort study of the American Cancer Society by Pope et al. (2002) observed association between ambient fine particulate matter and lung cancer and cardiopulmonary mortality. Current research points out to a general positive association between air pollution exposure and lung cancer etiology (Demetriou et al. 2012). Recently, the International Agency for Research on Cancer (IARC) has designated outdoor air pollution as a whole to be carcinogenic (IARC 2014).
A detailed characterization of the carcinogenic/mutagenic properties of air pollution constituents is beyond the scope of this chapter. Readers are referred to two of the recent reviews which provided an exhaustive review of literature on the genotoxicity of ambient air using in vitro assay systems (Claxton et al. 2004) and mutagenicity and rodent carcinogenicity of ambient air (Claxton and Woodall 2007). In brief, these reviews concluded that smaller particles (≤PM 2.5) contain higher percentage of extractable organic materials which were found to be more mutagenic compared to larger particles (>PM 2.5). In addition the carcinogenic activity of air was primarily attributed to its component constituents, such as polycyclic aromatic hydrocarbons (PAHs) and other aromatic compounds, whose levels may be subjected to change due to variations in atmospheric conditions (Claxton and Woodall 2007). A critical analysis of global epidemiological studies related to air pollution and air borne carcinogens is discussed elsewhere in this book (Chap. 7). The readers are also referred to Chap. 12 where genetic factors influencing disease outcomes related to air pollution exposure are outlined and to Chap. 13 where carcinogenic potential of air pollutants resulting from the recent advancements in the combustion technology, use of biofuels and engineered nanomaterial (both as additives and catalytic converters) are detailed. In addition, Chap. 13 also discusses the in vitro and in vivo studies pertaining to the carcinogenicity of emerging air pollutants.
Chemical carcinogens are believed to either initiate and/or promote carcinogenesis by a diverse number of mechanisms such as DNA adducts and DNA protein cross links formation, epigenetic alterations, regenerative cell proliferation, oxidative stress, inhibition of DNA repair and altered cell cycle regulation. Given the scope, the present chapter will attempt to provide readers with the current state of understanding on the carcinogenic mechanisms for a select set of chemicals, namely formaldehyde and benzene, and two representative mixtures – PAHs, and ETS (Environmental Tobacco Smoke), for which more detailed and significant mechanistic understanding of the carcinogenic process had been obtained over the past decade.
6.2 Formaldehyde
Formaldehyde was first described in 1855 and is ranked as one of the top 25 highest volume chemicals produced in the U.S (National Toxicology Program (NTP) 2002; Agency for Toxic Substances and Disease Registry (ATSDR) 1999; International Agency for Research on Cancer (IARC) 2006) for the past 21 years. Worldwide production of formaldehyde was estimated to be ~21.0 metric tons in the year 2000 (International Agency for Research on Cancer (IARC) 2006). The saturated aqueous solution of formaldehyde called as formalin, (37 % by weight or 40 % by volume), stabilized with 10–15 % methanol, is used in consumer products such as laundry detergent and several general purpose cleaners, as tissue preservative and as preservative in food and cosmetic products (National Toxicology Program (NTP) 2011).
In the ambient air, major sources of exposure to formaldehyde are from anthropogenic emissions, primarily from motor vehicles, power plants, and plants that produce or use formaldehyde or substances such as adhesives and coatings which release formaldehyde from curing (Agency for Toxic Substances and Disease Registry (ATSDR) 1999; International Agency for Research on Cancer (IARC) 1995). Additional sources of emission are incineration, wood burning, tobacco smoke and cooking operations (Agency for Toxic Substances and Disease Registry (ATSDR) 1999; Salthammer et al. 2010; Li et al. 1994; Health and Environment Canada 2012). In addition, endogenous formaldehyde is produced in the body through normal cellular metabolism through enzymatic or nonenzymatic reactions, and also as a detoxification product of xenobiotics during cellular metabolism (National Toxicology Program (NTP) 2011)
Population exposure to formaldehyde can occur via inhalation, ingestion and dermal routes. Ambient levels of formaldehyde in outdoor air are often significantly lower than those measured in the indoor air of workplaces or residences (National Toxicology Program (NTP) 2011; Salthammer et al. 2010). Improved manufacturing processes and construction practices have contributed to reduction in the levels of indoor formaldehyde emissions since the early to mid-1980s, yet, indoor levels of exposure of the population to formaldehyde remains a level which is still of concern to public health (National Toxicology Program (NTP) 2011).
6.2.1 Absorption, Distribution, Metabolism and Excretion (ADME)
A majority of the daily intake of formaldehyde results from inhalation exposure. Animal studies using labeled formaldehyde indicated differential ADME kinetics from oral, dermal and inhalation routes of exposure (Buss et al. 1964; Heck et al. 1983). In dogs, a majority of inhaled formaldehyde was found to be absorbed in the upper respiratory tract (Egle 1972), but deposition differed due to variability of scrubbing behavior across species (Kimbell et al. 2001). The computational modeling efforts for realistic representation of the human nasal airways from a single individual have demonstrated that approximately 90 % of inhaled formaldehyde was predicted to be absorbed in the nose at resting inspiration. This fraction decreased to about 70 % at light exercise and to 58 % at heavy exercise conditions (Kimbell et al. 2001).
Free formaldehyde exists in equilibrium (The ratio of methanediol to free formaldehyde 99.1–0.1 %) with its hydrated form, methanediol (CH2OH2) (Kd = 5.5 × 10−4) at physiological temperature and pH in the body (Fox et al. 1985). When free formaldehyde is removed from aqueous solution through covalent binding to small peptides or cellular components (Metz et al. 2004), the equilibrium is reestablished by dehydration of a fraction of methanediol to free formaldehyde for maintaining the ratio. Thus, a small pool of free formaldehyde can potentially be sustained in biological systems due to reversible nature of this hydration reaction (Fox et al. 1985).
Glutathione (GSH)-dependent formaldehyde dehydrogenase (FALDH) and mitochondrial aldehyde dehydrogenase 2 (ALDH2) are the primary enzymes that metabolize formaldehyde. Numerous studies now recognize FALDH as a member of the alcohol dehydrogenase (ADH) family, specifically ADH3 (Thompson et al. 2009; Hedberg et al. 2003; Deltour et al. 1999). Essentially, two principle pathways operate in the metabolism of formaldehyde to formate by oxidation. This involves mitochondrial ALDH2 (minor pathway) and a two-enzyme systems that involves ADH3 (major pathway) that converts glutathione-conjugated formaldehyde or S-hydroxymethyl glutathione (HMGSH) to the intermediate S-formylglutathione and subsequently metabolized to formate and GSH by S-formylglutathione hydrolase. The pharmacokinetics of formate involves: (A) formate undergoing adenosine triphosphate (ATP)-dependent addition to tetrahydrofolate (THF), by carrying either one or two; one-carbon groups. (B) Formate conjugating with THF to form N10-formyl-THF and its isomer N5-formyl-THF, both of which getting converted to N5-, N10-methenyl-THF, which undergo further metabolism. Decreased metabolisms of formaldehyde in ADH-knockout mouse studies have demonstrated that deletion of ADH3 increases the sensitivity of mice to formaldehyde (Deltour et al. 1999). Formate, the main product of formaldehyde clearance is further metabolized to CO2 and water, or incorporated into the one-carbon pool, or eliminated in the urine (National Toxicology Program (NTP) 2011).
6.2.2 Carcinogenic Effects of Formaldehyde
The International Agency for Research on Cancer (IARC) categorized formaldehyde as “known” human carcinogen based on the conclusion that nasopharyngeal cancer (NPC) was etiologically associated with formaldehyde exposure (International Agency for Research on Cancer (IARC) 2006) and that it is also a “known cause” for leukemia (International Agency for Research on Cancer (IARC) 2009). This classification is based on NCI cohort data (Beane Freeman et al. 2009), occupational exposure data on embalmers (Hauptmann et al. 2009) and studies in myeloid progenitor cells of exposed workers (Zhang et al. 2010) and meta-analysis of the epidemiology data by Zhang et al. (Zhang et al. 2009a). The conclusions of these assessments and studies are part of an on-going scientific debate which is beyond the scope of this chapter. The focus in this chapter is on a critical analysis of data from animal studies that indicate potential mechanisms of carcinogenesis.
Long-term inhalational exposure studies in diverse rat and mouse strains clearly demonstrated formaldehyde-induced tumors in nasal tissues: primarily squamous cell carcinomas, papillomas, polyploid adenoma, adenocarcinoma and fibro sarcoma (Sellakumar et al. 1985; Morgan et al. 1986; Monticello et al. 1996; Kamata et al. 1997; Soffritti et al. 1989; Soffritti et al. 2002; National Toxicology Program (NTP) 2009).
6.2.3 Carcinogenic Mechanisms
The available experimental evidence from in vitro and limited in vivo studies suggest that several mechanisms such as induction of mutations at the site of entry, decreased DNA repair function and enhanced cell proliferation are possibly involved in the formaldehyde-induced carcinogenesis process. What is known at present about how these mechanisms contribute individually or together in the development of cancer is reviewed in the following paragraphs.
6.2.3.1 Mutations
Studies have demonstrated formaldehyde-induced DNA mutations under different experimental conditions. (Snyder and Van Houten 1986; Dillon et al. 1998; Speit and Merk 2002). These mutations may occur during repair of DNA adducts, DNA-protein cross links (DPXs), and as single strand breaks (SSBs) formed through replication errors during mitosis. Investigations using diverse bacterial mutagenicity assays under varied experimental conditions such as reverse and forward mutation assays as well as use of specific strains for detecting deletions, insertions point mutations either with or without metabolic activation have clearly demonstrated formaldehyde-induced mutations (Liber et al. 1989; Speit et al. 2000; Dillon et al. 1998; Speit and Merk 2002). Formaldehyde has also been shown to induce primary DNA damage in E. coli in the form of excisions which are repairable via the R-factor plasmid to mediate the repair process. Studies in several bacterial strains indicated that AT base pairs are the primary reversion sites for the induction of mutations by formaldehyde (Dillon et al. 1998).
Studies investigating the mutagenic potential of formaldehyde in the mammalian cell culture system suggested that covalent alteration of DNA bases was not responsive to excision repair mechanisms (Liber et al. 1989; Speit et al. 2000). One study using the hypoxanthine phosphoribosyl transferase locus with high concentrations of formaldehyde reported point mutations showing a preferential AT to CG transversions (Liber et al. 1989). Speit et al. (2000) observed increased susceptibility of the repair-deficient cell lines to formaldehyde-induced micronuclei (MN) induction and proposed that more than one repair pathway may be involved in the repair of crosslinks. Also, observations in the L5178Y cell mouse lymphoma system suggest that exposure of formaldehyde in workers resulted in increased mutant P53 protein in peripheral blood lymphocytes indicating potential compromised function of p53.
6.2.3.2 Cell Proliferation
In vitro studies suggest that formaldehyde may induce cell proliferation at concentrations well below those causing cytotoxicity (Tyihák et al. 2001; Reuzel et al. 1990). Induction of this proliferation capability may be responsible for the transient cell proliferation observed in rat nasal passages and trachea following formaldehyde exposure (Ura et al. 1989; Nelson et al. 1986). Acute or short-term exposure studies in rodents indicate that the observed cell proliferation is dose-and time-dependent and varies by species and location of exposure in the nose (Cassee and Feron 1994; Monticello et al. 1990, 1991). The increased staining for proliferating cell nuclear antigen observed in respiratory epithelium in formaldehyde exposed rats may be indicative of nasal hyperplasia and squamous metaplasia (Monticello et al. 1996). Taken together accumulated scientific evidence suggests genotoxic, mutagenic and possibly cell proliferation (portal of entry) mechanisms to contribute in the development of carcinogenic effects.
6.2.3.3 Genotoxicity Mechanisms
A wide range of experimental studies, from cell-free systems to single cells and in vivo animal exposures, suggest that formaldehyde directly reacts with DNA. Initial studies using cell free systems demonstrated that direct interaction of formaldehyde with DNA results in multiple forms of DNA adducts: N6-hydroxymethyldeoxyadenosine, N4-hydroxymethyldeoxycytidine, and N2-hydroxymethyldeoxyguanosine as detected by high performance liquid chromatography (Beland et al. 1984; Kennedy et al. 1996; Cheng et al. 2003). The observation of aforementioned adducts in human nasal epithelial cells in vitro (Zhong and Que Hee 2004) further confirms the direct interaction of formaldehyde with DNA and DNA adduct formation. In vivo studies using labeled formaldehyde by a dual-isotope (3H/14C) method found that formaldehyde binds to DNA and protein resulting in DPXs and GSH depletion in the nasal mucosa of F344 rats. In addition, it also leads to oxidative stress by GSH depletion (Casanova and Heck 1987).
In vitro studies using cytotoxic concentrations of formaldehyde report that formaldehyde can induce clastogenic effects – increased MN, chromosomal aberrations, and sister chromatid exchanges (Miyachi and Tsutsui 2005; Hikiba et al. 2005). Similar observation from studies that used whole blood cultures exposed to cytotoxic concentrations (200 μM) of formaldehyde (Schmid and Speit 2007) suggest that clastogenic effects may also be implicated in the formaldehyde-induced carcinogenic process.
The initial observation of formaldehyde-induced DNA-histone cross links in isolated chromatin samples (Ohba et al. 1979) led to several in vitro studies demonstrating induction of DNA-protein crosslinks (DPX) by formaldehyde in bacteria (Wilkins and Macleod 1976), yeast (Magana-Schwencke and Ekert 1978) and mammalian cells, including diverse animal and human cells (Environment Canada 2012). In addition to DPXs, formaldehyde at higher concentrations was also found to induce SSBs, DNA-DNA cross links (DDXs) and scheduled and unscheduled DNA synthesis (UDS) in multiple mammalian cell culture systems (Speit et al. 2000; Shaham et al. 2003; Li et al. 2004; Bermudez and Allen 1984; Bermudez et al. 1989; McQueen et al. 1989). Although the in vivo experimental data points out that DPX occur at lower concentration compared to DDX, a single in vitro experiment in buccal cells reported formaldehyde induced DNA strand breaks at low concentration, and DDXs and DPXs at higher concentrations (Li et al. 2004). UDS, which represents DNA repair activity following excision of DNA damage, was reported in formaldehyde exposed nasal epithelial cells of F344 rats (Bermudez and Allen 1984), rat hepatocytes (Bermudez et al. 1989; McQueen et al. 1989) Syrian hamster embryo cells (Hamaguchi and Tsutsui 2000) and in HeLa cells (Martin et al. 1978); however, UDS was not found in human peripheral blood cells (Doolittle et al. 1985; Grafstrom et al. 1984). DNA repair inhibition was reported in human bronchial epithelial cells, skin fibroblasts or keratinocytes exposed to formaldehyde (Grafstrom et al. 1984; Emri et al. 2004). Additional studies that utilized DNA repair proficient and deficient cell lines (Liteplo and Meek 2003) observed inhibition of DNA repair at a concentration range of 0.125 mM to 10 mM. In vitro studies to understand the potential confounding interactions between formaldehyde and UV irradiation in human keratinocytes indicated DNA repair inhibition by UVB, UVC, but not UVA. The incomplete repair of irradiation-induced DNA damage in the cells that were exposed to formaldehyde post irradiation suggests that formaldehyde may enhances UV-induced carcinogenesis (Emri et al. 2004).
The experimental evidence presented above suggest that formaldehyde-induced carcinogenic effects to be mediated by multiple pathways that appear to be usually initiated by a genotoxic mechanism and associated downstream events. Though a majority of the studies in laboratory animal models were carried out in high exposure doses, they do provide biological plausibility for the multiple types of cancers associated with exposure to formaldehyde.
6.3 Benzene
Benzene, also known as benzol, is a colorless liquid with a sweet odor. Benzene evaporates into air very quickly and dissolves slightly in water. Benzene is highly flammable and ranks in the top 20 for high production volume chemicals in the United States (Agency for Toxicological Substances Disease Registry (ATSDR) 2007). It is an industrial solvent with wide use in the production of resins, synthetic fibers, polymers and in industries such as printing, shoe making, chemical manufacturing, coal-based coke production, and as a component in gasoline (Galbraith et al. 2010). Early studies in 1800 to 1900s reported adverse health effects from occupational exposure to benzene, causing significant reduction of blood elements associated with exposure in a dose and duration dependent manner (Hamilton 1931). The first comprehensive review on the acute and chronic benzene poisoning was associated with incidence of leukemia (Mallory et al. 1939).
Occupational exposure is the major route of high level human exposure to benzene; however, gasoline, cigarette smoke, gas emissions from volcanoes and forest fires also contribute to environmental benzene exposure. In general, the concentrations of benzene in ambient air have decreased steadily since 1900s and the use in consumer products has fallen off significantly (Galbraith et al. 2010; Williams et al. 2008). However, human exposure to benzene still continues to occur from ambient air due to burning of crude fossil oils, gasoline, and environmental cigarette smoke. The general population is exposed to benzene mainly through inhalation of contaminated air, particularly in areas of heavy traffic, around gas stations, and through inhalation of tobacco smoke from both active and passive smoking. It is reported that smokers have higher body burden (6–10 times) of benzene compared to non-smokers (Wallace 1996). People living in cities or industrial areas are generally exposed to higher levels of benzene in air than those living in rural areas. Measured levels of benzene in U.S in outdoor air have ranged from 0.02 to 34 ppb. Benzene levels in the home are usually higher than outdoor levels primarily because of tobacco smoke or materials stored in garages. As the average level of benzene is very low (0.1 ppb) in drinking water in the US, exposure to benzene through food, beverages, or drinking water is not a major concern, while exposure by inhalation is a major concern. Benzene exposure worldwide is of a significant concern as there are no regulatory standards for permissible exposure concentrations in gasoline in many countries.
6.3.1 Absorption, Distribution, Metabolism and Excretion (ADME)
Ingestion, inhalation and dermal routes are major routes of benzene exposure. About half of the benzene exposed by inhalation or ingestions routes was found to pass through the epithelial lining of lung and intestine and enter the blood stream. Once in the blood stream, benzene traverses throughout the body and is temporarily stored in adipose tissue and bone marrow (Agency for Toxicological Substances Disease Registry (ATSDR) 2007). Pathways of benzene metabolism are largely similar between rodents and primates. However significant differences exist in the type and quantity of the metabolites produced; indicating the species specific differences in metabolism. Primary metabolism of benzene occurs in liver and lung with secondary metabolism occurring in bone marrow.
Principally, the initial step involves cytochrome P-450 mediated oxidation of benzene to benzene oxide catalyzed by Cyp2E1. Benzene oxide, by and large, exists in equilibrium with its tautomer, oxepin, and can also spontaneously rearrange to phenol (PH), one of the intermediary metabolic products. Benzene oxide can also be hydrolyzed to catechol 1, 2 benzoquinone via benzenedihydrol, which reacts with cellular glutathione to produce S-phenyl mercapturic acid. Another toxic metabolite, hydroquinone is converted to highly reactive 1, 2, 4-benzene triol by CYP2E1. Oxepin on the other hand, also can open up its aromatic ring, yielding highly reactive muconaldehydes and E-E muconic acid. The electrophilic benzene oxide, muconaldehydes and benzoquinones react with cellular components such as proteins and interfere with normal cellular processes. Muconaldehyde is a known hematotoxicant in mice. Peroxidases also play a major role in the oxidation of benzene to produce phenolic metabolites such as quinones and semiquinones, which can bind to macromolecules and generate oxygen radicals. Benzoquinone, the major carcinogenic metabolite of benzene, is produced by catalytic activation of hydroquinone in bone marrow by myeloperoxidase (Smith et al. 1989). Recent studies demonstrate CYP2E1 and CYP2A13-, as major metabolizing enzymes, active at concentrations <1 ppm in lung, indicating that lung may be primary active site of metabolism at low exposure levels (Rappaport et al. 2009).
6.3.2 Carcinogenic Effects of Benzene
Benzene exposure, mostly occupational has been associated with various types of lympho hematopoietic cancers – acute non-lymphocytic leukemia/myelogenous leukemia and chronic myelogenous leukemia, non Hodkins lymphoma, multiple myeloma, neoplasms of kidney and cancers of lung. However, there is a large degree of variation in the association reported in many of these epidemiological studies due to multiple factors such as study design, exposure duration and dose, presence of confounders, cohort size and statistical methods employed (Galbraith et al. 2010; International Agency for Cancer Research (IARC) 2010; Sorahan 2011; Snyder 2012).
A few epidemiological studies demonstrated associations between un-metabolized benzene as a potential biomarker for exposure to benzene in gasoline attendants, urban policemen and bus drivers (Farmer et al. 2005; Fustinoni et al. 2005; Waidyanatha et al. 2001). Urinary phenol measurements have been used for monitoring occupational exposure to benzene (Smith et al. 1989), trans-, trans-muconic acid and S-phenylmercapturic acid levels have also been found to be correlated with occupational exposure to benzene (Inoue et al. 1989, 2000; Ruppert et al. 1997; Qu et al. 2005; Bechtold and Henderson 1993; Bechtold et al. 1992a). Additionally, hemoglobin and albumin adducts of the benzene metabolites, benzene oxide and 1, 4-benzoquinone, have been used as biomarkers of exposure to benzene (Bechtold et al. 1992b; Smith and Rothman 2000; Yeowell-O’Connell et al. 1998, 2001). However, ‘muconic acid’ and ‘phenyl mercapturic acid’ ‘have often shown correlation with environmental benzene exposure’ (Inoue et al. 1989, 2000; Ruppert et al. 1997).
6.3.3 Carcinogenic Mechanisms
Studies in laboratory animals (rats and mice) of both sexes either by oral or inhalational routes of exposure to benzene have been found to induce cancers such as Zymbal gland carcinomas of oral cavity, fore stomach lesions and liver adenomas in female rats (Maltoni et al. 1982, 1983, 1985, 1989), lung adenomas, squamous cell carcinomas of the Preputial and Zymbal glands in male mice (Snyder et al. 1988; Farris et al. 1993). In both sexes of mice, increased incidence of lympho- and hematopoietic cancers were observed (Snyder et al. 1980; Cronkite et al. 1984). In mice exposed by the oral route, papillomas and carcinomas of the oral cavity, skin of the lip, and papillomas of the palate were reported (National Toxicology Program (NTP) 1989). Two year cancer bioassay studies carried out by NTP also observed an increased incidence of hepato-carcinomas, pheochromocytomas, harderian gland adenomas and preputial gland squamous cell carcinomas in male mice (National Toxicology Program (NTP) toxicology and carcinogenesis studies of benzene 1989).
Several in vitro studies have demonstrated that oxy radicals generated in the metabolism of benzene induce gene mutations, DNA strand breaks and homologous recombination (Mullin et al. 1995; Rothman et al. 1995; Win 2003). In vitro and limited in vivo studies using the benzene metabolites, hydroquinone, phenol and 1, 2, 4-benzene triol observed increased levels of 8-OH-2′-deoxy guanosine (8-OH-dG) adducts (Mullin et al. 1995; Win 2003; Shen et al. 2006). Studies from several human cell lines as well as yeast also demonstrate that benzene metabolites are capable of initiating genetic recombination and defective DNA damage repair resulting in chromosomal aneuploidy (Mullin et al. 1995; Kolachana et al. 1993; Luo et al. 2008; Andreoli et al. 2012; Gowans et al. 2005; Sheltzer et al. 2011; Solomon et al. 2011). The genomic instability induced by hydroquinone was found to be similar to that resulting from ionizing radiation in the bone marrow of susceptible mice (Gowans et al. 2005).
The RecQ family of helicase genes, which play a role in the maintenance of genomic stability, are also implicated with Werner syndrome (WS), a rare autosomal premature aging syndrome associated with a predisposition to cancer (Oshima 2000). The gene coding for Werner syndrome WRN(a RecQ helicase family gene) also plays a role in sensing oxidative DNA damage caused by oxy radicals. In studies using RNA interference approach to silence endogenous WRN in HeLa cells, subsequently exposed to hydroxy quinone, a benzene metabolite an increase in the amount of DNA double-strand breaks and an elevated DNA damage was demonstrated (Ren et al. 2009). Lan et al. (2009) observed a significant association between single nucleotide polymorphisms in WRN and other genes involved in DNA repair, genomic stability and increased incidence of hematotoxicity in workers exposed to benzene. This supports the role for DNA recombination pathways in benzene carcinogenesis.
Results from human cell culture studies on cells obtained from individuals exposed to high levels of benzene and its metabolites observed chromosomal abnormalities similar to chromosomal changes observed in acute myeloid leukemia. Investigations that used conventional classic cytogenetic analysis as well as modern techniques such as chromosome wide aneuploidy have also unequivocally established benzene as a clastogen capable of inducing aneuploidy (Zhang et al. 1998). Recent pilot study that utilized in situ hybridization for chromosome wide aneuploidy analysis on peripheral lymphocytes of benzene exposed subjects demonstrated both monosomy on Chromosomes 5–7 and 10 and trisomy on Chromosomes 5–8, 10, 14, 16 and 21–22. When this study was extended to larger sample size, these increases were found to be dose-dependent and statistically significant (Zhang et al. 2005, 2011).
Several DNA repair mechanisms such as base excision, double strand repair and nucleotide excision repair continuously monitor and fix DNA adducts and apurinic sites (Ishihama et al. 2008). In vitro studies where cells are exposed to benzene metabolites have demonstrated an increased expression and nuclear translocation of the catalytic sub unit of DNA dependent protein kinase c, which regulates the non-homologous end joining in double strand DNA repair (Bi et al. 2010). This increased expression of DNA repair enzymes observed in the hematopoietic stem cells treated with benzene metabolites has been implicated in cell survival, transformation and proliferation of leukemia phenotype (Alexander and Wagner 2010).
Recent findings from the studies in patients with chronic benzene exposure observed reduced activity of Topo isomerase II (Topo II) expression due to altered histone acetylation and methylation of Topoi-alpha promoter region (Yu et al. 2011). These findings provide supportive experimental evidence for interactions of benzene metabolites with Topo II-alpha inhibition elucidated in quantitative structure activity relationship modeling studies (Eastmond et al. 2001). Further Xing et al. (2010) also reported reduced expression of P15 and 16 through DNA methylation in gas station workers exposed to low levels of benzene indicating epigenetic effects.
In summary, the experimental evidence accumulated to date suggests that benzene-induced carcinogenic effects may begin by oxy radicals generated from metabolites of benzene, which in turn elicit DNA damage and a cascade of events associated with this process. The multiple mechanisms as published and suggested to be involved in benzene-induced toxicity and cancer are depicted in Fig. 6.1.
Multiple modes of benzene-induced toxicity and leukemia (Reproduced with copyright permission from Mc Hale et al. (2012))
6.4 Polycyclic Aromatic Hydrocarbons (PAHs)
The PAHs consist of three or more fused benzene rings containing only carbon and hydrogen. A complex mixture of liquid and solid PAHs are produced in coal gasification plants, municipal incinerators, smokehouses, and some aluminum production facilities. In addition, cigarette smoking and environmental tobacco smoke, forest fires and volcanoes are additional sources of PAHs. There are approximately 100 different known PAHs in air, soil, food and water (Skupińska et al. 2004). The US EPA has designated several PAH compounds as priority pollutants (US 2009). The IARC has classified some of these compounds as carcinogenic (group 1) or likely carcinogenic (group 2A) to humans (IARC monographs on the evaluation of carcinogenic risks to humans 2010). ATSDR has grouped 17 PAHs in the ambient air as toxicants for their discussions in their toxicological profile (Agency for Toxic Substances and Disease Registry (ATSDR) 1995). Once emitted to the atmosphere, weight influences the fate of the gaseous PAH mixtures. The heavier PAHs (more than four rings) were found to adsorb to particulate matter, while lighter PAHs (less than four rings) tend to remain gaseous until removed via precipitation (Boström et al. 2002; Jenkins et al. 1996a; Table II (exposure media and potential for Children’s exposure) of USEPA BaP summary 2007; Jenkins et al. 1996b). PAHs are weakly soluble in water and this leads to their accumulation in sediments and aquatic organisms. Once in the atmosphere the PAHs are known to undergo chemical reactions with nitrogen radicals (•NO3), hydroxide radicals (•OH) and ultraviolet light and generate more active derivatives such as hydroxylated PAHs and PAH quinones (Boström et al. 2002; Jenkins et al. 1996a, b).
The most studied PAHs [e.g., benzo [a] pyrene B[a]P] is a byproduct of incomplete combustion or burning of organic material (e.g., cigarettes, gasoline, and wood). B[a]P is a ubiquitous compound in ambient (outdoor) air due to releases from multiple sources and is also a common indoor air pollutant, particularly in homes where people smoke (Table II (exposure media and potential for Children’s exposure) of USEPA BaP summary 2007). A wide range of PAHs have been identified based on chemical characterization and bioassay-directed fractionation in the particulates from diverse sources of emissions. Analysis of combustion source-specific differences in the PAHs content of emissions (Boström et al. 2002) indicated that gasoline vehicles without catalytic converters have the highest PAH emission rate for B[a]P compared to the ones with the converters. Diesel vehicles in general have lower PAH emissions than gasoline vehicles due to nitration of PAHs to nitro-PAHs. However, many of the nitro-PAHs are more carcinogenic than the parent compounds (Cook et al. 2007).
Residential combustion of wood has been estimated to be the largest source of PAH in Sweden and some areas of US (Agency for Toxic Substances and Disease Registry (ATSDR) 1995; Boström et al. 2002). Emission factors for PAH species have a wide range depending on the burning conditions. Several independent studies have reported a wide range of PAH emissions from biomass (cereal crop residues and wood fuels) burned in a combustion wind tunnel to simulate open burning. In a first study of four different cereal crop residues and four different wood fuels, the concentration range of 19 PAHs have been found to vary from 120 to 4,000 mg/kg fuel. Weakly flaming and spreading fires in the burning of cereal stubbles were observed to produce higher levels of heavier PAHs with greater partitioning of PAHs to the particulate phase (Dhammapala et al. 2007). Individual PAH species concentrations appeared correlated well within groups based primarily on molecular weight, but no single PAH species was observed to correlate with all others to serve as an indicator of PAH emission strength (Jenkins et al. 1996b). In general, these studies indicate that total PAH emissions, particle phase concentrations and fraction of PAH on particles were more strongly influenced by burning conditions than fuel type. Rogge et al. (1993) have conducted analysis of organic aerosols from road dust, tire, debris and organometallic break lining dust and reported PAHs of several species as well.
The fine particles, organic aerosols and organic carbon species generated during the cooking process make significant contributions to both indoor and outdoor air pollution. Multiple studies have reported emission rates for about 150 organic compounds emitted during residential cooking to include PAHs (Nolte et al. 1999; Kleeman et al. 1999). Though the PAHs emitted from cooking sources may be a small fraction in the urban ambient air, studies from Taiwan demonstrated that a higher proportion of carcinogenic B[a]P was emitted from cooking compared to traffic sources (Li et al. 2003). Tobacco smoke, both mainstream and secondhand contains about 50 or more carcinogens which includes PAHs and other nitrogen containing Azarenes, N-nitrosoamines, aromatic amines and heterocyclic aromatic amines (Hecht 1999).
6.4.1 Absorption, Metabolism and Excretion of PAHs
Clear qualitative similarities have been found in the distribution of certain PAHs across tissues upon inhalation exposure (IARC monographs on the evaluation of carcinogenic risks to humans polycyclic aromatic heterocarbons 2010).
The PAHs are chemically less reactive lipophilic compounds and on absorption (inhalation, ingestion, dermal) are activated to highly reactive electrophilic compounds by the classic Phase I and Phase II drug/xenobiotic enzyme systems. The metabolic activation of PAHs by Phase I enzymes result in the formation of radical cations, diol epoxides, and electrophilic and redox-active o-quinones. This is handled by three main routes: (1) Metabolic oxidation mediated by Cytochrome peroxidases leading to the formation of cationic PAH radicals; (2) Dihydrodiol dehydrogenase-catalyzed oxidation and formation of PAH-O-quinones; and (3) CYP mediated dihydrodiol epoxide formations involving epoxide hydrolase. The key cytochrome P450s involved in these metabolic conversions includes CYPs1A1, 1A2, 1B1 and 3A4. Cytochrome enzymes also play a vital role in PAH interactions with aryl hydrocarbon receptors (AhR), a key mechanism that is implicated in several of PAH-induced disease states including lung cancer. The AhR is present in the cytoplasm as a complex with several co-chaperons. When PAHs conjugates to AhR, it leads to the release of other proteins in the complex and initiates translocation of AhR-PAH complex to nucleus and subsequent formation of a hetero dimer of this complex with AhR nuclear translocator protein (ARNT). This heterodimer reacts with DNA through the xenobiotic response element (XRE) located in the promoter region of CYP1A and 1B genes (Shimada et al. 2002).
The Aldo-keto reductases (AKRs) are a superfamily of monomeric NAD(P) H-dependent oxidoreductases. AKRs catalyze the reduction of aldehydes and ketones to yield primary and secondary alcohols on a variety of endogenous substrates and xenobiotics including PAHs (Matsuura et al. 1996; Jin and Penning 2007). Several members of the AKR superfamily are able to oxidize PAH trans-dihydro diols to o-quinones (Smithgall et al. 1986, 1988). The substrate specificity of AKRs covers structurally diverse PAH trans-dihydro diols. PAH o-quinones are electrophilic and highly reactive to endogenous nucleophiles. PAH o-quinones can readily conjugate with cellular thiols to yield l-cysteine, N-acetyl-cysteine (NAC), and GSH leading to their elimination (Murty and Penning 1992a). The oxidative metabolites formed in phase I are enzymatically conjugated to small molecules by enzymes such as sulfo-transferases (SULTs), glutathione transferases (GSTs) and UDP-glucuronyl-transferases (Murty and Penning 1992b; Chou et al. 1998; Bansal et al. 1981). The oxygenated benzo[a] pyrene derivatives are common substrates of UDP-Glucuronyl transferase (UDPGT) (Bansal et al. 1981). In addition to the liver and kidneys, metabolism of PAHs occur in the adrenal glands, testes, thyroid, lungs, skin, sebaceous glands, and small intestines. The glucuronide and sulfate conjugates of epoxides, dihydro diol derivatives and phenols of these metabolites are excreted in the bile and urine. Glutathione conjugates are further metabolized to mercapturic acids in the kidney and are excreted in the urine. In humans the hydroxylated metabolites of the PAHs are excreted in urine both as free hydroxylated metabolites and as hydroxylated metabolites conjugated to glucuronic acid and sulfate (Bansal et al. 1981).
6.4.2 Carcinogenic Effects of PAHs
The ability of PAHs to cause cancer has been documented as early as 1775 by Sir Percival Pott, who demonstrated a correlation between scrotal cancers in workers exposed to chimney soot. The initial studies with residual oil fly ash, a product of fossil fuel emissions suggested role for transition metals and PAHs as contributors for cancer in occupational boiler workers with the detection of urinary 1-1-hydroxypyrene(OHP) and associated oxidative DNA injury marker, 8-hydroxy-2′-deoxyguanosine(8-OHdg) in these workers (Mukherjee et al. 2004). Reported research in PAH-induced carcinogenesis began with the isolation of BaP from coal tar in 1930 and its ability to induce mouse skin tumors upon repeated painting (Cook et al. 1933). Since then, numerous reports indicate PAHs to cause cancers of several types such as lung, bladder, breast, esophagus, digestive tract and skin. PAHs are carcinogenic in a number of animal models for multiple target organs (Nesnow et al. 1998; Arif et al. 1999; Darwiche et al. 2007; Courter et al. 2008; Wester et al. 2011; Marston et al. 2001; Yu et al. 2006a, b; Mahadevan et al. 2005; Guttenplan et al. 2012). Several laboratory studies have shown dibenzo (a) pyrene as a potent mouse carcinogen (Marston et al. 2001; Yu et al. 2006a, b), as well as capable of crossing trans-placental barriers (Yu et al. 2006a, b; Castro et al. 2008a, b; Shorey et al. 2012).
Atmospheric PAHs concentrations vary from place to place because of variation in emissions; atmospheric transport contributes to the variations by location as well. In addition, differences in respiration rate and genetic susceptibility among individuals can lead to a different risk at the same exposure level. Despite these limitations, PAH exposure from the ambient air had been demonstrated as one of the risk factors for lung cancer (Zhang et al. 2009b). Zhang et al (2009b), had reported increased risk of lung cancer in the urban population of China exposed to PAHs in outdoor ambient air. A more recent study from Brazil, which analyzed the PAH concentrations (B[a] P equivalent) in fraction of particulate matter less than 10 μm (PM10) of the ambient air at multiple sites also observed increased risk for lung cancer (Menezes and Cardeal 2012). Wickramasinghe et al. (2012) observed a significant correlation in lung cancer risk to source PAH exposure only in rural areas of Sri Lanka due to biomass fuel emission.
6.4.3 Mechanisms of Carcinogenesis
A comprehensive review of the diverse molecular mechanisms involved in PAH-induced carcinogenesis is beyond the scope of this chapter. The model PAH, B[a]P is one of the most investigated carcinogen and a vast amount of literature on the chemical carcinogenesis mechanisms of this compound is available (Rubin 2001; Siddens et al. 2012). Some of the recent findings on the PAH mediated carcinogenic mechanisms are described below.
Carcinogenic PAH compounds from particulates are taken up by the epithelial lining of tissues such as lung by binding to the cytosolic receptor AhR and its activation initiates a series of downstream events, including inflammation, DNA adduction, cell proliferation, loss of cell to cell adhesion, and eventually tumor formation. AhR is a transcription factor that plays a key role in mediating toxicity of a number of aromatic air pollutants (Denison and Nagy 2003). The nuclear translocation of AhR is dependent on Ary hydrocarbon receptor nuclear translocator (ARNT). AhR is known to interact with multiple signaling pathways: the induction of Cytochrome P450s; cell proliferation; cell-cell contact; and cell cycle regulation. The role of AhR in many types of cancers is well known (Safe et al. 2013). Figures 6.2 and 6.3 are schematic depiction of metabolism of Benzo [a] pyrene and the role of AhR in PAH mediated DNA binding respectively. Studies using AhR deficient mouse clearly demonstrated the inability of B[a]P to induce CYP1A2 and attenuation of skin carcinogenesis (Shimizu et al. 2000). In mouse strains specifically depleted for ARNT in epidermis, B[a]P failed to induce tumors (Shi et al. 2009; Kuang et al. 2013) suggesting the role or AhR and its nuclear translocation in B[a]P-induced skin tumorigenesis in this animal model.
The activation of PAHs involves metabolism by P450s to generate electrophilic metabolites. The PAH oxy quinones and epoxides generated in this activation step are highly reactive; their phase II detoxification step is elimination of these electrophilic intermediates by conjugation to cellular thiols, which may lead to oxidative stress depending on the load on cellular antioxidant machinery. Alternatively, diverse PAH-metabolites induced free radicals may directly interact with guanine causing DNA damage, resulting in the production of 8-OHdG (Lin et al. 2001).
The enantiomers generated from diol epoxides of PAH metabolism form covalent DNA adducts of varying structures and biological activity. These adducts are normally excised by DNA repair enzymes at different rates for different adducts. The diol epoxides of PAHs bind to guanine and adenine at exocyclic amino groups resulting in the formation of stable adducts with in DNA (Zienolddiny et al. 2006; Schoherr 1928). Several lines of work indicate that DNA adducts block polymerase-mediated replication activity contributing to increased damage by reducing DNA repair activity. This may modify adduct numbers and mutagenicity (Schoherr 1928). Binkova et al (2007), have suggested that polymorphisms in several DNA repair genes involved in nucleotide excision repair (NER) may modify PAH-DNA adduct levels and these adducts may be useful biomarkers to identify individual susceptibility to DNA damage resulting from carcinogenic PAH exposure.
6.5 DNA Repair Pathways
Multiple DNA damage repair pathways play a role in repairing DNA damage induced by PAHs. For example, nucleotide excision repair is the major pathway to repair PAH induced bulky lesions of DNA (Skosareva et al. 2013). Additional repair pathways such as BER homologous recombination repair were also reported under different experimental conditions for various PAHs of different structures or various PAH metabolites (Braithwaite et al. 1998; Meschini et al. 2010; Desler et al. 2009).
The HR mechanism is primarily involved in search for homology and DNA strand invasion through the Rad51-ssDNA presynaptic filament by positioning the invading 3′-end on a template duplex DNA to initiate repair synthesis. This system was found to be principally involved in repair induced by 3 PAHs: 4-nitroquinoline 1-oxide, N-acetoxy-2-acetylaminofluorine, and 1-Nitroso pyrene. When tested for their relative ability to cause intra-chromosomal homologous recombination between two identical genes that were stably integrated into a mouse cell genome, a dose-dependent increase in recombination frequency with differences among compounds was observed (Bhattacharya et al. 1989).
The mismatch repair (MMR) pathway has been found to play a role in PAH-mediated DNA adduct repair. For example, B[a]P mediated enhancement in lymphomagenisis was demonstrated in Msh2−/− mice in comparison to heterozygous (Msh2+/− mice had been demonstrated by Zienolddiny et al. (2006).
6.6 Second Hand Smoke/Environmental Tobacco Smoke
Involuntary exposure to passive smoke, commonly referred to as second hand smoke (SHS) or environmental tobacco smoke (ETS) or side stream smoke occurs frequently from being in close proximity to cigarette smokers or from exposure to smoke and its components released into the environment. The earliest record of harmful effects of SHS was reported in 1928 (Schoherr 1928). The Surgeon General’s report in 1964 classified tobacco smoke as a carcinogenic mixture and after critical evaluation of human and animal data, the US EPA in its report in 1992 classified SHS as a Group A human carcinogen (US 1992). Despite these warnings, in the US about 43.4 million adults continue to smoke, exposing approximately 126 million nonsmokers (CDC 2009) to SHS making and it’s a major public health concern. Currently, 7 % of people in high-income countries are covered by comprehensive smoke-free legislation at the national level, and an additional 8 % are covered at the regional level. However, there has been almost no implementation of smoke-free legislation at the subnational level in middle- and low-income countries, despite many of these jurisdictions having the legal authority to do so (World Health Organization 2009). About one-third of adults worldwide are exposed to SHS, which accounts for, 33 % of male and 35 % of female and 40 % of children non-smokers who are exposed to SHS (IARC 2010). The exposure was estimated to have resulted in about 1 % of worldwide mortality due to lung cancer in nonsmokers (Oberg et al. 2011). The SHS has been implicated in about 47 % deaths in women, 28 % in children, and 26 % in men worldwide (Grimmer et al. 1987). While the risk of lung cancers to SHS exposure are unequivocal (Sheldon et al. 1993), associations have also been reported for colorectal and breast cancers and very weak association for pancreatic, ovarian, and several other types of cancers (World Health Organization 2009; Oberg et al. 2011; Vineis et al. 2004). Due to space limitations, this chapter will focus only on the origin, association and molecular mechanisms implicated in lung cancer from SHS.
Tobacco smoke consists of >2,500 constituents several of which are known human carcinogens (NTP 2005). Both mainstream and side stream smoke are comprised of a vapor phase containing volatile agents, including benzene, vinyl chloride, acrolein, etc., a particulate phase containing semi-volatile and non-volatile agents, such as alkaloids, nicotine and its derivatives, aromatic amines and PAHs. The chemical composition of side stream smoke and mainstream smoke are qualitatively similar, due to difference in the burning temperatures, ageing of smoke and dilution in ambient air; the quantities differ in vapor and particulate phases. However, certain carcinogens, such as aromatic amines have been found to be richer in SHS. Along with these carcinogens, both mainstream and side stream smoke contain a high concentration of reactive organic radicals (RORs) that form on the top of the cigarette at high temperatures. SHS contains not only the gas phase of exhaled smoke, but also the products of combustion of a cigarette. In people, SHS exposure results in up to 50× higher concentration of some of the toxicants than in smokers themselves (A report of the Surgeon General 2006). SHS contains a majority of the IARC group 1 carcinogens benzene, cadmium, 2-aminonaphthalene, nickel, chromium, arsenic and 4-aminobiphenyl; IARC group 2A carcinogens formaldehyde, 1, 3-butadiene and benzo(a) pyrene; the IARC group 2B carcinogens acetaldehyde, isoprene, catechol, acrylonitrile, styrene, NNK, NNN, Lead; and many other carcinogens and genotoxicants (IARC 2004). It has also been observed that the particulate phase of the SHS contains tenfold higher amounts of PAHs than mainstream smoke (Grimmer et al. 1987; Lodovici et al. 2004; Kalaitzoglou and Samara 2006) and is the major source of PAHs in indoor ambient air (Sheldon et al. 1993; Georgiadis et al. 2001; Garfinkel 1981).
One of the first major epidemiologic studies carried out in 1980s indicated a positive association for second hand smoke exposure to a higher risk of developing lung cancer in nonsmoking women married to smokers compared to women married to nonsmokers (Hirayama 1981; Trichopoulos et al. 1981; Apelberg et al. 2013). These three initial studies were followed by numerous investigations that were specifically conducted to evaluate SHS exposure and the risk of lung cancer among nonsmokers. As many as 40 case-control studies and a total of 25 epidemiological studies carried out across the globe confirmed the positive association for workplace secondhand smoke exposure and the risk of lung cancer among lifetime nonsmokers, despite geographic differences in exposure prevalence (A report of the Surgeon General 2006). These epidemiological studies used diverse measurements such as airborne respirable particles and nicotine content to associate the relationship between exposure to SHS and cancer outcomes (Klepeis et al. 2007). The airborne concentration depends on diverse physical factors, such as the volume of the environment measured and ventilation. It has generally been observed that SHS levels remained relatively stable and decayed over time until ventilation patterns changed indoors, where as in outdoor environments SHS levels dropped immediately to background levels once the source was extinguished (Weaver et al. 1998). In the environments with low SHS exposure, airborne nicotine was non-detectable in the absence of tobacco smoke, while background levels of PM-2.5 from other sources are always present, suggesting that assessment of SHS outdoors cannot be based solely on PM-2.5 measurements, given the limited correlation observed, while both measures can be used indoors when other sources of combustion are absent (Weaver et al. 1998).
Studies relating to urinary trans-, trans-muconoic acid (a marker of benzene exposure) and uptake from SHS has given mixed results (Hecht 2004; Anderson et al. 2001). The urinary metabolites of PAHs, pyrene and phenanthrenone (1-hydroxy pyrene, and hydroxy phenanthranone) respectively were not found to be increased in persons exposed to SHS. The urinary metabolites of tobacco specific markers such as 4 (methyl-nitrasoamine)-1-(3-pyridal)-1-butanone (NNK), which is normally low in smokers is often detected and found elevated in persons exposed to SHS. One study reported about six times higher levels of NNK in women who lived with smokers than who lived with nonsmokers (Anderson et al. 2001; Yamamoto et al. 2013). NNAL-Gluc (4-(methylnitrosoamino)-1-(3-pyridyl)-1-(o-beta-d-glucopyranuronosyl) butane Plus NNAL (4-(methylnitrosamino)-1-3-Pyridyl-1 butanol), is more directly related to cancer risk in SHS than cotinine (Report of the Surgeon general 2006).
Typically, animal studies of second hand smoke often involve exposure to side stream smoke produced by smoking machines. Though these experimental exposures do not fully simulate human exposures, the animals develop tumors. Nevertheless, the animal data provide valuable insights regarding the carcinogenic potential of secondhand tobacco smoke (Coggins 2007; Witschi 2003; Hecht 2005; Toh et al. 2006). Each of the animal model studies with different routes of smoke exposure Viz. nose only or whole body, have their own limitations. These include, difficulty in the accuracy of the dose delivered due to pain and discomfort accompanied with former route and dermal and gastro intestinal absorption of smoke material with the latter. Another inherent issue is that the rodents are obligatory nose breathers with complex nasal turbinates, which filter smoke efficiently and forced smoke exposure in animals leads to a shallow breathing pattern, resulting in scant deposition in lower airways making the rodent a less than ideal model for human exposure (Hecht 2005). In spite of these limitations, animal studies have provided potential biological plausibility for the carcinogenicity of second hand/side stream smoke. These experimental studies in laboratory animals have observed that the exposure to SHS causes biological effects that include: (i) increases or decreases in the activity of phase I enzymes involved in carcinogen metabolism; (ii) increased expression of nitric oxide synthase, xanthine oxidase and various protein kinases; (iii) the formation of smoke-related DNA adducts in several tissues, and (iv) the presence of urinary biomarkers of exposure to tobacco smoke (Coggins 2007; Witschi 2003; Hecht 2005). Studies using condensates of side stream or mainstream cigarette smoke have produced a spectrum of benign and malignant skin tumors in mice following topical application, and the side stream condensate exhibited higher carcinogenic activity. Side stream smoke condensate was shown to produce a dose-dependent increase in lung tumors in rats following implantation into the lungs (Hecht 2005). In mice, SHS induced tumors primarily occur in peripheral lung as hyperplasia, growing into adenomas and eventually becoming adenocarcinomas. This observation is consistent with the development of non-small cell lung cancer, and particularly of adenocarcinoma in never smokers (Coggins 2007; Witschi 2003; Hecht 2005). Smoke exposure to Hamsters almost exclusively produces laryngeal tumors but not tumors in the deep airways (Witschi 2003; Hecht 2005).
6.6.1 Mechanisms of SHS-Induced Carcinogenesis
It’s well known that SHS qualitatively contains essentially the same toxicants and carcinogens in primary tobacco smoke and many of these carcinogens are known to be genotoxicants and induce cancer through genotoxic mechanisms. However, the major difference is that carcinogenic dose resulting from SHS tends to be generally low compared to primary tobacco smoke inhalation. Though small in quantity, the carcinogens in SHS such as NNK undergo detoxification. This results in electrophilic intermediaries that can bind to nucleophilic macromolecules resulting in DNA adducts, subsequently this leads to gene mutations due to DNA mis repair. A significant amount of urinary metabolites of NNK [4-(methyl nitrosamino)-1-(3-Pyridyl)-1-butanol];(NNAL) and its glucuronide conjugate [(NNAL-Gluc)] have been found in the urine of SHS exposed subjects (Hecht 1999; Toh et al. 2006; Wakelee et al. 2007; Meger et al. 2002) suggesting detoxification of NNK, but there is no measureable data on their potential to form adducts with macromolecules. Similarly there is no clear experimental data to support a role for PAHs in the SHS in the mutagenic or carcinogenic process.
Primary tobacco smoke induced lung carcinogenesis has been known to be mediated through mutations in p53 tumor suppressor gene and k-ras oncogenes (Husgafvel-Pursiainen et al. 2000). Epidemiological studies that explored the potential role for these genes in SHS-induced lung tumors failed to find any association due to small number of cases. But, these studies observed that G: C to A: T transitions are the most common mutations among lifetime nonsmokers (Kim et al. 2012) and it was also observed that exposure to SHS doubled the risk of TP53 mutation in never-smokers. In animal models, Transgenic Big Blue mice exposed to side stream smoke for duration of 2–4 months, demonstrated that SHS elicits significant mutagenic response in the lung, trachea and bladder (Kim et al. 2012; Tao et al. 2010). Additional comparative DNA sequencing analysis of lung cellular DNA from SHS exposed Big Blue mouse with lung cancer DNA from known nonsmokers revealed an identical mutation spectrum for TP53 gene and this was significantly different from lung cancer samples of smokers. Also, the ratio of G: C to A: T transitions and G: C to T: A transversions in the SHS exposed mouse lung and lung cancer from nonsmokers were significantly elevated compared to lung cancer from smokers (Kim et al. 2012). The high incidence of mutations in the bladder tissue of Big Blue mice also provide some experimental support to increased bladder cancer risk observed in lifelong-nonsmokers exposed to SHS (Tao et al. 2010). Additional experimental analysis that investigated overall hypermethylation pattern of tumor suppressor genes on 216 lung cancer patients that includes both smokers and never smokers (Wu et al. 2008) revealed interesting specific patterns of gene expression. The authors indicated increased hypermethylation of these genes including DNA repair gene, O6-methylguanine–DNA methyl transferase (MGMT). This coincides with the fact that the inactivation of MGMT in non-small cell lung cancer, the most frequent cancer in never smokers has been associated with increased occurrence of TP53 mutation, especially the G:C to A:T transition (Wu et al. 2008). The hypermethylation pattern and increased TP53 observed in never smokers due to SHS exposure indirectly suggest that similar mechanisms may be operating in SHS induced lung cancer. Thus far, the accumulated experimental evidence from studies carried out in laboratory animals (usually at a high dose exposure to SHS rather than in human exposure scenarios) indicate multiple pathways to be implicated in the carcinogenesis process and suggests the need to develop better experimental models and design for future studies to gain realistic and relevant knowledge to understand this process in a more cognizant manner.
6.7 Summary
Epidemiological studies point to associations between exposure to air pollution (that contains many well recognized carcinogens) and increase in the incidence of various cancers in population studies. The evidence is stronger in the case of occupational exposure to individual constituents of air pollutants suggesting a potential relationship for carcinogenic effects of air pollution mixtures. The available experimental evidence from laboratory studies for selective air pollutants (viz. formaldehyde, benzene, PAHs and second hand smoke reviewed here), suggest involvement of multiple, but possible common biological pathways. These carcinogenic compounds in the air may enter into humans by inhalation, ingestion or dermal routes. Once these compounds have entered into different organs/portals of entry, they are metabolized/activated to radical/electrophilic moieties by phase I xenobiotic system or chemical specific metabolizing enzymes and conjugated and eliminated by phase II enzymes in liver, lung and other organ systems. The electrophilic/oxidative metabolites generated in this process are capable of initiating carcinogenic process by either genotoxic/mutagenic or non-genotoxic pathways. The former pathways include generation of DNA adducts and DNA-protein adducts. The DNA damage leads to activation of DNA repair machinery to fix damaged DNA. Misrepair of DNA and subsequent error-prone replication may potentially lead to mutagenesis. In addition, these airborne carcinogens may also perturb the cellular homeostasis processes resulting in: (a) oxidative stress; (b) inflammatory responses; and (c) epigenetic and gene expression alterations leading to enhanced cell proliferation. These pathways either independently; or together are implicated in the initiation and or promotion of carcinogenic process and contribute to diverse cancers observed in the population studies. The potential role of multiple pathways implicated in the carcinogenic process mediated by these chemicals is depicted in Fig. 6.4. These diverse pathways may act alone or in different combinations resulting in cancer. Similarly, how specific genotoxic/mutagenic or carcinogenic compounds in the air act alone or together in a synergic or additive way to induce one or more mechanistic pathways referred above, leading to cancer is still largely unknown. Future research efforts to elucidate molecular pathways involved in air- pollution induced carcinogenesis studies may have to develop more integrated approaches that include a combination of high throughput systems biology and to identify specific drivers of cancer that may aid in providing scientific basis for their mode of action to aid in hazard identification and or risk assessment.
References
A report of the Surgeon General (2006) The health consequences of involuntary exposure to tobacco smoke. pp 1–23, 423–485
Agency for Toxic Substances and Disease Registry (ATSDR) Toxicological profile for formaldehyde (1999) Public Health Service, U.S. Department of Health and Human Services, Atlanta. http://www.atsdr.cdc.gov/toxprofiles/tp111.html
Agency for Toxic Substances and Disease Registry (ATSDR) Toxicological profile for polycyclic aromatic hydrocarbons (1995) Public Health Service, U.S. Department of Health and Human Services, Atlanta. http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=122&tid=25
Agency for Toxicological Substances Disease Registry (ATSDR) (2007) Toxicological profile for Benzene. www.atsdr.cdc.gov/toxprofiles/tp3.pdf
Alexander DD, Wagner ME (2010) Benzene exposure and non-Hodgkin lymphoma: a meta-analysis of epidemiologic studies. J Occup Environ Med 52(2):169–189
Anderson KE, Steven G, Carmella C et al (2001) Metabolites of a tobacco-specific lung carcinogen in nonsmoking women exposed to environmental tobacco smoke. J Natl Cancer Inst 93(5):378–381
Andreoli R, Protano C, Manini P et al (2012) Association between environmental exposure to benzene and oxidative damage to nucleic acids in children. Med Lav 103(5):324–337
Apelberg BJ, Hepp LM, Avila-Tang E et al (2013) Environmental monitoring of secondhand smoke exposure. Tob Control 22(3):147–155
Arif JM, Smith WA, Gupta RC (1999) DNA adduct formation and persistence in rat tissues following exposure to the mammary carcinogen dibenzo [a, l]pyrene. Carcinogenesis 20(6):1147–1150
Bansal SK, Zaleski J, Gessner T (1981) Glucuronidation of oxygenated benzo (a) pyrene derivatives by UDP-glucuronyl transferase of nuclear envelope. Biochem Biophys Res Commun 98(1):131–139
Beane Freeman LE, Blair A et al (2009) Mortality from lymphohematopoietic malignancies among workers in formaldehyde industries: the National Cancer Institute Cohort. J Natl Cancer Inst 101(10):751–761
Bechtold WE, Henderson RF (1993) Biomarkers of human exposure to benzene. J Toxicol Environ Health 40(2–3):377–386
Bechtold WE, Willis JK, Sun JD et al (1992a) Biological markers of exposure to benzene: S-phenylcysteine in albumin. Carcinogenesis 13(7):1217–1220
Bechtold WE, Sun JD, Birnbaum LS et al (1992b) S-phenylcysteine formation in hemoglobin as a biological exposure index to benzene. Arch Toxicol 66(5):303–309
Beland FA, Fullerton NF, Heflich RH (1984) Rapid isolation, hydrolysis and chromatography of formaldehyde-modified DNA. J Chromatogr 308:121–131
Bermudez E, Allen PF (1984) The assessment of DNA damage and repair in rat nasal epithelial cells. Carcinogenesis 5(11):453–458
Bermudez E, Smith-Oliver T, Delehanty LL (1989) The induction of DNA-strand breaks and unscheduled DNA synthesis in F-344 rat hepatocytes following in vivo administration of caprolactam or benzoin. Mutat Res 224(3):361–364
Bhattacharya NP, Maher VC, McCormic JJ (1989) Ability of structurally related polycyclic aromatic carcinogens to induce homologous recombination between duplicated chromosomal sequences in mouse L cells. Mutat Res 211(2):205–214
Bi Y, Li Y, Kong M, Xiao X et al (2010) Gene expression in benzene-exposed workers by microarray analysis of peripheral mononuclear blood cells: induction and silencing of CYP4F3A and regulation of DNA-dependent protein kinase catalytic subunit in DNA double strand break repair. Chem Biol Interact 184(1–2):207–211
Binkova B, Chvatalova I, Lnenickova Z et al (2007) PAH-DNA adducts in environmentally exposed population in relation to metabolic and DNA repair gene polymorphisms. Mutat Res 620(1–2):49–61
Boström CE, Gerde P, Hanberg A et al (2002) Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environ Health Perspect 110(Suppl 3):451–488
Braithwaite E, Wu X, Wang Z (1998) Repair of DNA lesions induced by polycyclic aromatic hydrocarbons in human cell-free extracts: involvement of two excision repair mechanisms in vitro. Carcinogenesis 19(7):1239–1246
Buss J, Kuschinsky K, Kewitz H et al (1964) Enteric resorption of formaldehyde. Naunyn Schmiedebergs Arch Pharmacol 247:380–381
Casanova M, Heck H’A (1987) Further studies of the metabolic incorporation and covalent binding of inhaled [3H]- and [14C]formaldehyde in Fischer-344 rats: effects of glutathione depletion. Toxicol Appl Pharmacol 89(1):105–121
Cassee FR, Feron VJ (1994) Biochemical and histopathological changes in nasal epithelium of rats after 3-day intermittent exposure to formaldehyde and ozone alone or in combination. Toxicol Lett 72(1–3):257–268
Castro DJ, Löhr CV, Fischer KA et al (2008a) Lymphoma and lung cancer in offspring born to pregnant mice dosed with dibenzo[a, l]pyrene: the importance of in utero vs. lactational exposure. Toxicol Appl Pharmacol 233(3):454–458
Castro DJ, Baird WM, Pereira CB (2008b) Fetal mouse Cyp1b1 and transplacental carcinogenesis from maternal exposure todibenzo(a, l)pyrene. Cancer Prev Res (Phila) 1(2):128–134
CDC (2009) Tobacco use targeting the nation’s leading killer at a glance. Available at http://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/tobacco.pdf
Cheng G, Shi Y, Sturla SJ et al (2003) Reactions of formaldehyde plus acetaldehyde with deoxyguanosine and DNA: formation of cyclic deoxyguanosine adducts and formaldehyde cross-links. Chem Res Toxicol 16(2):145–152
Chou HC, Ozawa S, Fu PP et al (1998) Metabolic activation of methyl-hydroxylated derivatives of 7,12-dimethylbenz[a]anthracene by human liver dehydroepiandrosterone-steroid sulfotransferase. Carcinogenesis 19(6):1071–1076
Claxton LD, Woodall GMJR (2007) A review of the mutagenicity and rodent carcinogenicity of ambient air. Mutat Res 636(1–3):36–94
Claxton LD, Mathew PP, Warren SH (2004) The genotoxicity of ambient outdoor air, a review: Salmonella mutagenicity. Mutat Res 567(2–3):347–349
Coggins CR (2007) An updated review of inhalation studies with cigarette smoke in laboratory animals. Int J Toxicol 26(4):331–338
Cook JW, Hewett CL, Hieger I (1933) The isolation of a cancer-producing hydrocarbon from coal tar. Parts I, II, and III. J Chem Soc 0:395–405
Cook R, Strum M, Touma JS et al (2007) Inhalation exposure and risk from mobile source air toxics in future years. J Expo Sci Environ Epidemiol 17:95–105
Courter LA, Luch A, Musafia-Jeknic T et al (2008) The influence of diesel exhaust on polycyclic aromatic hydrocarbon-induced DNA damage, gene expression, and tumor initiation in Sencar mice in vivo. Cancer Lett 265(1):135–147
Cronkite EP, Bullis J, Inoue T et al (1984) Benzene inhalation produces leukemia in mice. Toxicol Appl Pharmacol 75(2):358–361
Darwiche N, Ryscavage A, Perez-Lorenzo R, Wright L et al (2007) Expression profile of skin papillomas with high cancer risk displays a unique genetic signature that clusters with squamous cell carcinomas and predicts risk for malignant conversion. Oncogene 26(48):6885–6895
Deltour L, Foglio MH, Duester G (1999) Metabolic deficiency in alcohol dehydrogenase Adh1, Adh3 and Adh4 null mutant mice: Overlapping roles in Adh1 and Adh4 in ethanol clearance and metabolism of retinol to retinoic acid. J Biol Chem 274(24):16796–16801
Demetriou CA, Raascou-Nielsen O, Loft S et al (2012) Biomarkers of ambient air pollution and lung cancer: a systematic review. Occup Environ Med 69(9):619–627
Denison MS, Nagy SR (2003) Activation of the aryl hydrocarbon receptor by structurally diverse exogenous and endogenous chemicals. Annu Rev Pharmacol Toxicol 43:309–334
Desler C, Johannessen C, Rasmussen LJ et al (2009) Repair of DNA damage induced by anthanthrene, a polycyclic aromatic hydrocarbon (PAH) without bay or fjord regions. Chem Biol Interact 177(3):212–217
Dhammapala R, Claiborn C, Jimenez J et al (2007) Emission factors of PAHs, methoxyphenols, levoglucosan, elemental carbon and organic carbon from simulated wheat and Kentucky bluegrass stubble burns. Atmos Environ 41(12):2660–2669
Dillon D, Combes R, Zeiger E (1998) The effectiveness of Salmonella strains TA100, TA102 and TA104 for detecting mutagenicity of some aldehydes and peroxides. Mutagenesis 13(1):19–26
Doolittle DJ, Furlong JW, Butterworth BE (1985) Assessment of chemically induced DNA repair in primary cultures of human bronchial epithelial cells. Toxicol Appl Pharmacol 79(1):28–38
Eastmond DA, Schuler M, Frantz C et al (2001) Characterization and mechanisms of chromosomal alterations induced by benzene in mice and humans. Res Rep Health Eff Inst 103:1–68; discussion 69–80
Egle JL Jr (1972) Retention of inhaled formaldehyde, propionaldehyde, and acrolein in the dog. Arch Environ Health 25:119–124
Emri G, Schaefer D, Held B et al (2004) Low concentrations of formaldehyde induce DNA damage and delay DNA repair after UV irradiation in human skin cells. Exp Dermatol 13(5):305–315
Health and Environment Canada (2012) Report on formaldehyde: indoor air quality. Available at: http://cfpub.epa.gov/ncea/iris_drafts/recorddisplay.cfm?deid=223614
Esposito S, Tenconi R, Lelii M et al (2014) Possible molecular mechanisms linking air pollution and asthma in children. BMC Pulm Med 14(31):1471–1474
Farmer PB, Kaur B, Roach J (2005) The use of S-phenylmercapturic acid as a biomarker in molecular epidemiology studies of benzene. Chem Biol Interact 153–154:97–102
Farris GM, Everitt JI, Irons RD et al (1993) Carcinogenicity of inhaled benzene in CBA mice. Fundam Appl Toxicol 20(4):503–507
Ferkol T, Schraufnagel D (2014) The global burden of respiratory disease. Ann Am Thorac soc 11(3):404–406
Fox CH, Johnson FB, Whiting J et al (1985) Formaldehyde fixation. J Histochem Cytochem 33(8):845–853
Fustinoni S, Consonni D, Campo L et al (2005) Monitoring low benzene exposure: comparative evaluation of urinary biomarkers, influence of cigarette smoking, and genetic polymorphisms. Cancer Epidemiol Biomarkers Prev 14(9):2237–2244
Galbraith D, Gross SA, Paustenbach D (2010) Benzene and human health: a historical review and appraisal of associations with various diseases. Crit Rev Toxicol 40(Suppl 2):1–46
Garfinkel L (1981) Time trends in lung cancer mortality among nonsmokers and a note on passive smoking. J Natl Cancer Inst 66(6):1061–1066
Georgiadis P, Topinka J, Stoikidou M et al (2001) Biomarkers of genotoxicity of air pollution (the AULIS project): bulky DNA adducts in subjects with moderate to low exposures to airborne polycyclic aromatic hydrocarbons and their relationship to environmental tobacco smoke and other parameters. Carcinogenesis 22(9):1447–1457
Gowans ID, Lorimore SA, McIlrath JM et al (2005) Genotype-dependent induction of transmissible chromosomal instability by gamma-radiation and the benzene metabolite hydroquinone. Cancer Res 65(9):3527–3530
Grafstrom RC, Fornace A Jr, Harris CC (1984) Repair of DNA damage caused by formaldehyde in human cells. Cancer Res 44(10):4323–4327
Grimmer G, Brune H, Dettbarn G et al (1987) Contribution of polycyclic aromatic compounds to the carcinogenicity of sidestream smoke of cigarettes evaluated by implantation into the lungs of rats. Cancer Lett 43(3):173–177
Guttenplan JB, Kosinska W, Zhao ZL et al (2012) Mutagenesis and carcinogenesis induced by dibenzo[a, l]pyrene in the mouse oral cavity: a potential new model for oral cancer. Int J Cancer 130(12):2783–2790
Hamaguchi F, Tsutsui T (2000) Assessment of genotoxicity of dental antiseptics: ability of phenol, guaiacol, p-phenolsulfonic acid, sodium hypochlorite, p-chlorophenol, m-cresol or formaldehyde to induce unscheduled DNA synthesis in cultured Syrian hamster embryo cells. Jpn J Pharmacol 83(3):273–276
Hamilton A (1931) Benzene (Benzol) poisoning: general review. Arch Pathol 11:601–637
Hauptmann M, Stewart PA, Lubin JH et al (2009) Mortality from Lymphohematopoietic malignancies and brain cancer among embalmers exposed to formaldehyde. J Natl Cancer Inst 101(24):1696–1708
Hecht SS (1999) Tobacco smoke carcinogens and lung cancer. J Natl Cancer Inst 91(14):1194–1210
Hecht SS (2004) Carcinogen derived biomarkers: applications in studies of human exposure to secondhand tobacco smoke. Tob Control 13:i48–i56
Hecht SS (2005) Carcinogenicity studies of inhaled cigarette smoke in laboratory animals: old and new. Carcinogenesis 26(9):1488–1492
Heck HD, Chin TY, Schmitz MC (1983) Distribution of [14C] formaldehyde in rats after inhalation exposure. In: Gibson JE (ed) Formaldehyde toxicity. Hemisphere Publishing Corporation, Washington, DC, pp 26–37
Hedberg JJ, Griffiths WJ, Nilsson SJ et al (2003) Reduction of s-nitroso glutathione by human alcohol deghydrogenase 3 is an irreversible reaction as analyzed by electrospray mass spectrometry. Eur J Biochem 270(6):1249–1256
Hikiba H, Watanabe E, Barrett JC et al (2005) Ability of fourteen chemical agents used in dental practice to induce chromosome aberrations in Syrian hamster embryo cells. J Pharmacol Sci 97(1):46–52
Hirayama T (1981) Non-smoking wives of heavy smokers have a higher risk of lung cancer: a study from Japan. Bull World Health Org 78(7):940–942
Husgafvel-Pursiainen K, Boffetta P, Kannio A et al (2000) p53 mutations and exposure to environmental tobacco smoke in a multicenter study on lung cancer. Cancer Res 60(11):2906–2911
IARC (2004) Monograph on evaluating carcinogen risks. Tobacco smoke and involuntary smoking. Lyon. 83:1–1438
IARC (2010) Table 1.5. Monograph on second hand tobacco smoke, Lyon, France 100E:213–255. http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-7.pdf. Referenced to Öberg M, Jaakkola MS, Prüss-Üstün A, Schweizer C, Woodward A (2010) Second-hand smoke: assessing the environmental burden of disease at national and local levels. World Health Organization, Geneva (WHO Environmental Burden of Disease Series, No. 18). http://www.who.int/quantifying_ehimpacts/publications/SHS.pdf
IARC (2014) http://www.iarc.fr/en/publications/books/sp161/index.php. In: Kurt Straif, Aaron Cohen, Jonathan Samet (eds) Air pollution and cancer. IARC Scientific Publication No. 161
IARC (2010) monographs on the evaluation of carcinogenic risks to humans vol 92. Some non-heterocyclic polycyclicaromatic hydrocarbons and some related exposures. Available at monographs.ionc.fr/EVG/monographs/vol92/mono92.pdf
Inoue O, Seiji K, Nakatsuka H et al (1989) Urinary t, t-muconic acid as an indicator of exposure to benzene. Br J Ind Med 46(2):122–127
Inoue O, Kanno E, Kakizaki M et al (2000) Urinary phenylmercapturic acid as a marker of occupational exposure to benzene. Ind Health 38(2):195–204
International Agency for Cancer Research (IARC) (2010) Benzene – IARC monographs on the evaluation of carcinogenicity of Benzene. 100F:257–262. monographs.iarc.fr/ENG/Monographs/vol100F/mono100F-24.pdf
International Agency for Research on Cancer (IARC) Monographs (2009) Vol 100: A review and update on occupational carcinogens – a review of human carcinogens – part C: metals, arsenic, dusts and fibres. Lyon, pp 87–89. http://monographs.iarc.fr/ENG/Publications/techrep42/TR42-11.pdf
International Agency for Research on Cancer (IARC) monographs on the evaluation of carcinogenic risks to humans (1995), Wood dust and formaldehyde, vol 62. Lyon. http://www.inchem.org/documents/iarc/vol62/wood.html and http://www.inchem.org/documents/iarc/vol62/formal.html
International Agency for Research on Cancer (IARC) Monographs on the evaluation of carcinogenic risks to humans (2006) Formaldehyde, 2-Butoxyethanol and 1-tert-Butoxy-2-propanol, vol 88. IARC, Lyon. http://monographs.iarc.fr/ENG/Monographs/vol88/volume88.pdf
Ishihama M, Toyooka T, Ibuki Y (2008) Generation of phosphorylated histone H2AX by benzene metabolites. Toxicol In Vitro 22(8):1861–1868
Jenkins BM, Jones AD, Turn QT et al (1996a) emission factors for polycyclic aromatic hydrocarbons from biomass burning. Environ Sci Technol 30(8):2462–2469
Jenkins BM, Jones AD, Turn SQ et al (1996b) Particle concentrations, gas-particle partitioning, and species inter correlations for polycyclic aromatic hydrocarbons (PAH) emitted during biomass burning. Atmos Environ 30(22):3825–3835
Jin Y, Penning TM (2007) Aldo-keto reductases and bioactivation/detoxication. Annu Rec Pharmacol Toxicol 47:263–292
Kalaitzoglou M, Samara C (2006) Gas/particle partitioning and yield levels of polycyclic aromatic hydrocarbons and n-alkanes in the mainstream cigarette smoke of commercial cigarette brands. Food Chem Toxicol 44(8):1432–1442
Kamata E, Nakadate M, Uchida O et al (1997) Results of a 28 month – chronic inhalation toxicity study of formaldehyde in male Fisher 344 rats. J Toxicol Sci 22(3):239–254
Kennedy G, Slaich PK, Golding BT et al (1996) Structure and mechanism of formation of a new adduct from formaldehyde and guanosine. Biol Interact 102(2):93–100
Kim SI, Yoon JI, Tommasi S et al (2012) New experimental data linking secondhand smoke exposure to lung cancer in nonsmokers. FASEB J 26(5):1845–1854
Kimbell JS, Overton JH, Subramaniam RP et al (2001) Dosimetry modeling of inhaled formaldehyde: binning nasal flux predictions for quantitative risk assessment. Toxicol Sci 64:111–121
Kleeman MJ, Schauer JJ, Cass GR (1999) Size and composition distribution of fine particulate matter emitted from wood burning, meat charbroiling, and cigarettes. Environ Sci Tech 33:3516–3523
Klepeis NE, Ott WR, Switzer P (2007) Real-time measurement of outdoor tobacco smoke particles. J Air Waste Manage Assoc 57(5):522–534
Kolachana P, Subrahmanyam VV, Meyer K et al (1993) Benzene and its phenolic metabolites produce oxidative DNA damage in HL60 cells in vitro and in the bone marrow in vivo. Cancer Res 53(5):1023–1026
Kuang D, Zhang W, Deng Q, Zhang X et al (2013) Dose–response relationships of polycyclic aromatic hydrocarbons exposure and oxidative damage to DNA and lipid in coke oven workers. Environ Sci Technol 47(13):7446–7456
Lan Q, Zhang L, Shen M (2009) Large-scale evaluation of candidate genes identifies associations between DNA repair and genomic maintenance and development of benzene hematotoxicity. Carcinogenesis 30(1):50–58
Li SM, Anlauf KG, Wiebe HA et al (1994) Estimating primary and secondary production of HCHO in eastern North America based on gas-phase measurements and principal component analysis. Geophys Res Lett 21:669–672
Li CT, Lin YC, Lee WJ (2003) Emission of polycyclic aromatic hydrocarbons and their carcinogenic potencies from cooking sources to the urban atmosphere. Environ Health Perspect 111(4):483–487
Li R, Lu ZS, Qiao Y et al (2004) Study on the formaldehyde-induced DNA damage with comet assay. Shi Yan Sheng Wu Xue Bao 37(4):262–268
Liber HL, Benforado K, Crosby RM, Simpson D et al (1989) Formaldehyde-induced spontaneous alterations in human hprt DNA sequence and m-RNA expression. Mutat Res 226(1):31–37
Lin CH, Huang X, Kolbanovskii A, Hingerty BE et al (2001) Molecular topology of polycyclic aromatic carcinogens determines DNA adduct conformation: a link to tumorigenic activity. J Mol Biol 306(5):1059–1080
Liteplo RG, Meek ME (2003) Inhaled formaldehyde: exposure estimation, hazard characterization, and exposure-response analysis. J Toxicol Environ Health B Crit Rev 6(1):85–114
Lodovici M, Akpan V, Evangelisti C et al (2004) Side stream tobacco smoke as the main predictor of exposure to polycyclic aromatic hydrocarbons. J Appl Toxicol 24(4):277–281
Luo L, Jiang L, Geng C et al (2008) Hydroquinone-induced genotoxicity and oxidative DNA damage in HepG2 cells. Chem Biol Interact 173(1):1–8
Magana-Schwencke N, Ekert B (1978) Biochemical analysis of damage induced in yeast by formaldehyde. II. Induction of cross-links between DNA and protein. Mutat Res 51(1):11–19
Mahadevan B, Luch A, Bravo CF et al (2005) Dibenzo [a, l]pyrene induced DNA adduct formation in lung tissue in vivo. Cancer Lett 227(1):25–32
Mallory TB, Gall EA, Brickley WJ et al (1939) Chronic exposure to benzene (benzol). III. The pathologic results. J Ind Hyg Toxicol 21:355–377
Maltoni C, Cotti G, Valgimigli L et al (1982) Hepatocarcinomas in Sprague–Dawley rats, following exposure to benzene by inhalation: First experimental demonstration. Med Lav 73(4):446–450
Maltoni C, Conti B, Cotti G (1983) Benzene: a multipotential carcinogen. Results of long-term bioassays performed at the Bologna Institute of Oncology. Am J Ind Med 4(5):589–630
Maltoni C, Conti B, Cotti G et al (1985) Experimental studies on benzene carcinogenicity at the Bologna Institute of Oncology: current results and ongoing research. Am J Ind Med 7(5–6):415–446
Maltoni C, Ciliberti A, Cotti G et al (1989) Benzene, an experimental multipotential carcinogen: results of the long-term bioassays performed at the Bologna Institute of Oncology. Environ Health Perspect 82:109–124
Marston CP, Pereira C, Ferguson J et al (2001) Effect of a complex environmental mixture from coal tar containing polycyclic aromatic hydrocarbons (PAH) on the tumor initiation, PAH-DNA binding and metabolic activation of carcinogenic PAH in mouse epidermis. Carcinogenesis 22(7):1077–1086
Martin CN, McDermid AC, Garner RC (1978) Testing of known carcinogens and non-carcinogens for their ability to induce unscheduled DNA synthesis in HeLa cells. Cancer Res 38(8):2621–2627
Matsuura K, Deyashiki Y, Bunai Y et al (1996) Aldose reductase is a major reductase for isocaproaldehyde, a product of side-chain cleavage of cholesterol, in human and animal adrenal glands. Arch Biochem Biophys 328(2):265–271
Mc Hale CM et al (2012) Current understanding of the mechanism of benzene-induced leukemia in humans: implications for risk assessment. Carcinogenesis 33(2):240–252
McQueen CA, Rosado RR, Williams GM (1989) Effect of nalidixic acid on DNA repair in rat hepatocytes. Cell Biol Toxicol 5(2):201–206
Meger M, Meger-Kossien I, Schuler-Metz A et al (2002) Simultaneous determination of nicotine and eight nicotine metabolites in urine of smokers using liquid chromatography – tandem mass spectrometry. J Chromatogr B 778:251–261
Menezes HC, Cardeal ZL (2012) Study of polycyclic aromatic hydrocarbons in atmospheric particulate matter of an urban area with iron and steel mills. Environ Toxicol Chem 31(7):1470–1471
Meschini R, Berni A, Marotta E et al (2010) DNA repair mechanisms involved in the removal of DBPDE-induced lesions leading to chromosomal alterations in CHO cells. Cytogenet Genome Res 128(1–3):124–130
Metz B, Kersten GF, Hoogerhout P et al (2004) Identification of formaldehyde-induced modifications in proteins: reactions with model peptides. J Biol Chem 279:6235–6243
Miyachi T, Tsutsui T (2005) Ability of 13 chemical agents used in dental practice to induce sister-chromatid exchanges in Syrian hamster embryo cells. Odontology 93(1):24–29
Monticello TM, Morgan KT, Hurtt ME (1990) Unit length as the denominator for quantitation of cell proliferation in nasal epithelia. Toxicol Pathol 18(1):24–31
Monticello TM, Renne R, Morgan KT (1991) Chemically induced cell proliferation in upper respiratory tract carcinogenesis. Prog Clin Biol Res 369:323–335
Monticello TM, Swenberg JA, Gross EA et al (1996) Correlation of regional and non-linear formaldehyde-induced nasal cancer with proliferating populations of cells. Cancer Res 56(5):1012–1022
Morgan KT, Gross EA, Patterson DL (1986) Distribution, progression and recovery of acute formaldehyde – induced inhibition of nasal mucociliary function in F-344 rats. Toxicol Appl Pharmacol 86(3):448–456
Mukherjee S, Palmer LJ, Kim JY et al (2004) Smoking status and occupational exposure affects oxidative DNA injury in boilermakers exposed to metal fume and residual oil fly ash. Cancer Epidemiol Biomarkers Prev 13(3):454–460
Mullin AH, Rando R, Esmundo F et al (1995) Inhalation of benzene leads to an increase in the mutant frequencies of a lacI transgene in lung and spleen tissues of mice. Mutat Res 327:121–129
Murty VS, Penning TM (1992a) Polycyclic aromatic hydrocarbon (PAH) ortho-quinone conjugate chemistry: kinetics of thiol addition to PAH ortho-quinones and structures of thioether adducts of naphthalene-1, 2- dione. Chem Biol Interact 84(2):169–188
Murty VS, Penning TM (1992b) Characterization of mercapturic acid and glutathionyl conjugates of benzo[a]pyrene-7, 8-dione by two-dimensional NMR. Bioconjug Chem 3(3):218–224
Narot TS, Perez L, Kunzli N et al (2011) Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 377:732–740
National Toxicology program (NTP) Formaldehyde: Report on carcinogens, 12th edn (2011) National Institute of Environmental Health Sciences, Public Health Service, U.S. Department of Health and Human Services, Research Triangle Park. http://ntp.niehs.nih.gov/ntp/roc/twelfth/profiles/formaldehyde.pdf
National Toxicology Program (NTP) Report on carcinogens (2002) 10th edn. National Institute of Environmental Health Sciences, Public Health Service, U.S. Department of Health and Human Services, Research Triangle Park. http://ehp.niehs.nih.gov/roc/tenth/profiles/s089form.pdf
National Toxicology Program (NTP) Report on carcinogens (2009) Back ground document for formaldehyde. http://ntp.niehs.nih.gov/ntp/roc/twelfth/2009/…/formaldehyde_bd_final.pdf
National Toxicology Program (NTP) toxicology and carcinogenesis studies of benzene (1989) CAS No. 71-43-2 in F344/N Rats and B6C3F1 Mice (Gavage Studies). Natl Toxicol Program Tech Rep Ser 289:1–277
Nelson N, Levine RJ, Albert RE et al (1986) Contribution of formaldehyde to respiratory cancer. Environ Health Perspect 70:23–35
Nesnow S, Mass MJ, Ross JA et al (1998) Lung tumorigenic interactions in strain A/J mice of five environmental polycyclic aromatichydrocarbons. Environ Health Perspect 106(Suppl 6):1337–1346
Nolte CG, Schauer JJ, Cass GR (1999) Highly polar organic compounds present in meat smoke. Environ Sci Technol 33(19):3313–3316
NTP (2005) 12th Report on carcinogens. U.S. Department of Health and Human Services, Public Health Service. http://ntp.niehs.nih.gov/go/roc12
Oberg M, Jaakkola MS, Woodward A et al (2011) Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 377(9760):139–146
Ohba Y, Morimitsu Y, Watarai A (1979) Reaction of formaldehyde with calf-thymus nucleohistone. Eur J Biochem 100(1):285–293
Oshima J (2000) Comparative aspects of the Werner syndrome gene. In Vivo 14(1):165–172
Pope CA 3rd, Burnett RT, Thun MJ et al (2002) Lung cancer, cardiopulmonary mortality, and long term exposure to fine particulate air pollution. JAMA 287(9):1132–1141
Qu Q, Shore R, Li G et al (2005) Biomarkers of benzene: urinary metabolites in relation to individual genotype and personal exposure. Chem Biol Interact 153–154:85–89
Rappaport SM, Kim S, Lan Q et al (2009) Evidence that humans metabolize benzene via two pathways. Environ Health Perspect 117(6):946–952
Ren X, Lim S, Smith MT et al (2009) Werner syndrome protein, WRN, protects cells from DNA damage induced by the benzene metabolite hydroquinone. Toxicol Sci 107(2):367–375
Reuzel PG, Wilmer JW, Woutersen RA et al (1990) Interactive effects of ozone and formaldehyde on the nasal respiratory lining epithelium in rats. J Toxicol Environ Health 29(3):279–292
Rogge WF, Hildemann LM, Mazurek MA et al (1993) source of fine organic aerosol. 3. Road dust, tire debris and organo metallic break lining dust: Roads as sources and sinks. Environ Sci Technol 27:1892–1904
Rothman N, Haas R, Hayes RB et al (1995) Benzene induces gene-duplicating but not gene-inactivating mutations at the glycophorin A locus in exposed humans. Proc Natl Acad Sci U S A 92(9):4069–4073
Rubin H (2001) Synergistic mechanisms in carcinogenesis by polycyclic aromatic hydrocarbons and by tobacco smoke: a bio-historical perspective with updates. Carcinogenesis 22(12):1903–1930
Ruppert T, Scherer G, Tricker AR et al (1997) trans, trans-muconic acid as a biomarker of non-occupational environmental exposure to benzene. Int Arch Occup Environ Health 69(4):247–251
Safe S, Lee SO, Jin UH (2013) Role of the aryl hydrocarbon receptor in carcinogenesis and potential as a drug target. Toxicol Sci 135(1):1–16
Salthammer T, Mentese S, MarutZky R (2010) Formaldehyde in the indoor environment. Chem Rev 110(4):2536–2572
Schluger NW, Koppaka R (2014) Lung disease in a global context a call for public health action. Ann Am Thorac Soc 11(3):407–416
Schmid O, Speit G (2007) Genotoxic effects induced by formaldehyde in human blood and implications for the interpretation of biomonitoring studies. Mutagenesis 22(1):69–74
Schoherr E (1928) Second hand smoke contribution to the statistical and clinical features of lung tumors (in German). Z Krebsforsch 27:436–450
Sellakumar AR, Snyder CA, Solomon JJ et al (1985) Carcinogenicity of formaldehyde and hydrogen chloride in rats. Toxicol Appl Pharmacol 81(3):401–406
Shah ASV, Langrish JP, Nair H et al (2013) Global association of air pollution and heart failure: a systematic review and meta analysis. Lancet. doi: http://dx.doi.org/10.1016/ S0140-6736(13)60898-3
Shaham J, Bomstein Y, Gurvich R et al (2003) DNA- protein cross links and P53 protein expression In relation to occupational exposure to formaldehyde. Occup Environ Med 60(6):403–409
Sheldon L, Clayton A, Keever J et al (1993) Indoor concentrations of polycyclic aromatic hydrocarbons in California residences. California Air Resources Board, Report A033-132. http://www.arb.ca.gov/research/apr/reports/l3041.pdf
Sheltzer JM, Blank HM, Pfau SJ et al (2011) Aneuploidy drives genomic instability in yeast. Science 333(6045):1026–1030
Shen M, Lan Q, Zhang L et al (2006) Polymorphisms in genes involved in DNA double-strand break repair pathway and susceptibility to benzene-induced hematotoxicity. Carcinogenesis 27:2083–2089
Shi S, Yoon DY, Hodge-bellK C et al (2009) The aryl hydro carbon receptor nuclear translocator(ARNT)is required for tumor initiation by Benzo(a) pyrene. Carcinogenesis 30(11):1956–1961
Shimada T, Inoue K, Suzuki Y et al (2002) Arylhydrocarbon receptor-dependent induction of liver and lung cytochromes P450 1A1, 1A2, and 1B1 by polycyclic aromatic hydrocarbons and polychlorinated biphenyls in genetically engineered C57BL/6 J mice. Carcinogenesis 23(7):1199–1207
Shimizu Y, Nakatsura Y, Takahasi Y et al (2000) Benzo(a) pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor. Proc Natl Acad Sci 97(2):779–782
Shorey LE, Castro DJ, Baird WM et al (2012) Transplacental carcinogenesis with dibenzo[def, p]chrysene (DBC): timing of maternal exposures determines target tissue response in offspring. Cancer Lett 317(1):49–55
Siddens LK, Larkin A, Krueger SK et al (2012) Polycyclic aromatic hydrocarbons as skin carcinogens: comparison of benzo[a] pyrene, dibenzo [defp] Chrysene and three environmental mixtures in the FVB/N mouse. Toxicol Appl Pharmacol 264(3):377–386
Skosareva LV, Lebedeva NA, Lavrik OI et al (2013) Repair of bulky DNA lesions deriving from polycyclic aromatic hydrocarbons. Mol Biol 47(5):634–644
Skupińska K, Misiewicz I, Kasprzycka-Guttman T (2004) Polycyclic aromatic hydrocarbons: physicochemical properties, environmental appearance and impact on living organisms. Acta Pol Pharm 61(3):233
Smith MT, Rothman N (2000) Biomarkers in the molecular epidemiology of benzene-exposed workers. J Toxicol Environ Health A 61(5–6):439–445
Smith MT, Yager JW, Steinmetz KL, Eastmond DA (1989) Peroxidase-dependent metabolism of benzene’s phenolic metabolites and its potential role in benzene toxicity and carcinogenicity. Environ Health Perspect 82:23–29
Smithgall TE, Harvey RG, Penning TM (1986) Regio- and stereospecificity of homogeneous 3 alpha-hydroxysteroid-dihydrodiol dehydrogenase for trans-dihydrodiol metabolites of polycyclic aromatic hydrocarbons. J Biol Chem 261(14):6184–6691
Smithgall TE, Harvey RG, Penning TM (1988) Oxidation of the trans-3,4-dihydrodiol metabolites of the potent carcinogen 7,12-dimethylbenz(a)anthracene and other benz(a)anthracene derivatives by 3 alpha-hydroxysteroid-dihydrodiol dehydrogenase: effects of methyl substitution on velocity and stereochemical course of trans-dihydrodiol oxidation. Cancer Res 48(5):1227–1232
Snyder R (2012) Leukemia and benzene. Int J Environ Res Public Health 9(8):2875–2893
Snyder RD, Van Houten B (1986) Genotoxicity of formaldehyde and an evaluation of its effects on the DNA repair process in human diploid fibroblasts. Mutat Res 165(1):21–30
Snyder CA, Goldstein BD, Sellakumar AR et al (1980) The inhalation toxicology of benzene: incidence of hematopoietic neoplasms and hematotoxicity in ARK/J and C57BL/6 J mice. Toxicol Appl Pharmacol 54(2):323–331
Snyder CA, Sellakumar AR, James DJ et al (1988) The carcinogenicity of discontinuous inhaled benzene exposures in CD-1 and C57Bl/6 mice. Arch Toxicol 62(5):331–335
Soffritti M, Maltoni C, Maffei F et al (1989) Formaldehyde: an experimental multipotential carcinogen. Toxicol Ind Health 5(5):699–730
Soffritti M, Belpoggi F, Lambertin L et al (2002) Results of long-term experimental studies on the carcinogenicity of formaldehyde and acetaldehyde in rats. Ann N Y Acad Sci 982:87–105
Solomon DA, Kim T, Diaz-Martinez LA et al (2011) Mutational inactivation of STAG2 causes aneuploidy in human cancer. Science 333:1039–1043
Sorahan T (2011) Occupational benzene exposure and lymphoma risk. Environ Health Perspect 119(11):A468–A469
Speit G, Merk O (2002) Evaluation of mutagenic effects of formaldehyde in vitro: detection of cross links and mutations in mouse lymphoma cells. Mutagenesis 17(3):183–187
Speit G, Schütz P, Merk O (2000) Induction and repair of formaldehyde-induced DNA cross links in repair deficient human cell lines. Mutagenesis 15(1):85–90
Table II (exposure media and potential for Children’s exposure) of USEPA BaP summary (2007) Available at http://www.epa.gov/teach/chem_summ/B[a]P_summary.pdf (compilation of Information reflecting the statement in the text described in this table was derived from several resources including studies listed in the TEACH Database (http://www.epa.gov/teach)
Tao L, Xiang YB, Wang R (2010) Environmental tobacco smoke in relation to bladder cancer risk–the Shanghai bladder cancer study [corrected]. Cancer Epidemiol Biomarkers Prev 19(12):3087–3095
Thompson CM, Sonawane B, Grafström RC (2009) The ontogeny, distribution, and regulation of alcohol dehydrogenase 3: implications for pulmonary physiology. Drug Metab Dispos 37(8):1565–1571
Toh CK, Gao F, Lim WT et al (2006) Never-smokers with lung cancer: epidemiologic evidence of a distinct disease entity. J Clin Oncol 24(15):2245–2251
Trichopoulos D, Kalandidi A, Sparros L et al (1981) Lung cancer and passive smoking. Int J Cancer 27(1):1–4
Tyihák E, Bocsi J, Timár F et al (2001) Formaldehyde promotes and inhibits the proliferation of cultured tumour and endothelial cells. Cell Prolif 34(3):135–141
Ura H, Nowak P, Litwin S et al (1989) Effects of formaldehyde on normal xenotransplanted human tracheobronchial epithelium. Am J Pathol 134(1):99–106
US EPA (1992) Respiratory health effects of passive smoking: lung cancer and other disorders. EPA, Washington, DC. oaspub.epa.gov/eims/eimscomm.getfile?p_download_id=36793
US EPA (2009) List of priority chemicals in united states. Available at http://www.epa.gov/oSW/hazard/wastemin/priority.htm
Vineis P, Alavanja M, Garte S et al (2004) Dose–response relationship in tobacco-related cancers of bladder and lung: a biochemical interpretation. Int J Cancer 108(1):2–7
Waidyanatha S, Rothman N, Fustinoni S et al (2001) Urinary benzene as a biomarker of exposure among occupationally exposed and unexposed subjects. Carcinogenesis 22(2):279–286
Wakelee HA, Chang ET, Gomez SL et al (2007) Lung cancer incidence in never smokers. J Clin Oncol 25(5):472–478
Wallace L (1996) Environmental exposure to benzene: an update. Environ Health Perspect 104(Suppl 6):1129–1136
Weaver VM, Buckley TJ, Groopman JD et al (1998) Approaches to environmental exposure assessment in children. Environ Health Perspect 106(Suppl 3):827–832
Wester PW, Muller JJ, Slob W et al (2011) Carcinogenic activity of benzo[a]pyrene in a 2 year oral study in Wistar rats. Food Chem Toxicol 50(3–4):927–935
Wickramasinghe AP, Karunaratne DG, Sivakanesan R (2012) M(10)-bound polycyclic aromatic hydrocarbons: biological indicators, lung cancerrisk of realistic receptors and ‘source-exposure-effect relationship’ under different source scenarios. Chemosphere 87(11):1381–1387
Wilkins RJ, Macleod HD (1976) Formaldehyde induced DNA-protein crosslinks in Escherichia coli. Mutat Res 36(1):11–16
Williams PR, Panko JM, Unice K et al (2008) Occupational exposures associated with petroleum-derived products containing trace levels of benzene. J Occup Environ Hyg 5(9):565–574
Win LM (2003) Homologous recombination initiated by benzene metabolites: potential role of oxidative stress. Toxicol Sci 72:143–149
Witschi H (2003) Induction of lung cancer by passive smoking in an animal model system. Methods Mol Med 74:441–455
World Health Organization (2009) Report on the global tobacco epidemic, implementing smoke-free environments. http://whqlibdoc.who.int/publications/2009/9789241563918_eng_full.pdf
World Health Organization (WHO) News release (2011) Tackling the global clean air challenge. http://www.who.int/mediacentre/news/releases/2011/air_pollution_20110926/en/index.html
Wu JY, Wang J, Lai JC et al (2008) Association of O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation with p53 mutation occurrence in non-small cell lung cancer with different histology, gender, and smoking status. Ann Surg Oncol 11:3272–3277
Xing C, Wang QF, Li B, Tian H et al (2010) Methylation and expression analysis of tumor suppressor genes p15 and p16 in benzene poisoning. Chem Biol Interact 184(1–2):306–309
Yamamoto ML, Chapman AM, Schiest RH (2013) Effects of side stream tobacco smoke and smoke extract on glutathione- and oxidative DNA damage repair-deficient mice and blood cells. Mutat Res 749(1–2):58–65
Yeowell-O’Connell K, Rothman N, Smith MT et al (1998) Hemoglobin and albumin adducts of benzene oxide among workers exposed to high levels of benzene. Carcinogenesis 19(9):1565–1571
Yeowell-O’Connell K, Rothman N, Waidyanatha S et al (2001) Protein adducts of 1,4-benzoquinone and benzene oxide among smokers and nonsmokers exposed to benzene in China. Cancer Epidemiol Biomarkers Prev 10(8):831–838
Yu Z, Loehr CV, Fischer KA et al (2006a) In utero exposure of mice to dibenzo[a, l]pyrene produces lymphoma in the offspring: role of the aryl hydrocarbon receptor. Cancer Res 66(2):755–762
Yu Z, Mahadevan B, Löhr CV et al (2006b) Indole-3-carbinol in the maternal diet provides chemoprotection for the fetus against transplacental carcinogenesis by the polycyclic aromatic hydrocarbon dibenzo[a, l]pyrene. Carcinogenesis 27(10):2116–2123
Yu K, Shi YF, Yang KY et al (2011) Decreased topoisomerase IIα expression and altered histone and regulatory factors of topoisomerase IIα promoter in patients with chronic benzene poisoning. Toxicol Lett 203(2):111–117
Zar HL, Ferkol TW (2014) The global burden of respiratory disease-impact on child health. Pediatr Pulmonol 49(5):430–434
Zhang L, Rothman N, Wang Y et al (1998) Increased aneusomy and long arm deletion of Chromosomes 5 and 7 in the lymphocytes of Chinese workers exposed to benzene. Carcinogenesis 19(11):1955–1961
Zhang L, Lan Q, Guo W et al (2005) Use of octochrome fluorescence in situ hybridization to detect specific aneuploidy among all 24 chromosomes in benzene-exposed workers. Chem Biol Interact 153–154:117–122
Zhang L, Steinmaus C, Eastmond DA et al (2009a) Formaldehyde exposure and leukemia: a new meta-analysis and potential mechanisms. Mutat Res 681:150–168
Zhang Y, Tao S, Shen H et al (2009b) Inhalation exposure to ambient polycyclic aromatic hydrocarbons and lung cancer risk of Chinese population. Proc Natl Acad Sci U S A 106(50):21063–21067
Zhang L, Tang X, Rothman N et al (2010) Occupational exposure to formaldehyde, hematotoxicity, and leukemia-specific chromosome changes in cultured myeloid progenitor cells. Cancer Epidemiol Biomarkers Prev 19:80–88
Zhang L, Lan Q, Guo W et al (2011) Chromosome-wide aneuploidy study (CWAS) in workers exposed to an established leukemogen benzene. Carcinogenesis 32(4):605–612
Zhong W, Que Hee SS (2004) Formaldehyde-induced DNA adducts as biomarkers of in vitro human nasal epithelial cell exposure to formaldehyde. Mutat Res 563(1):13–24
Zienolddiny S, Ryberg D, Svendsrud DH et al (2006) Msh2 deficiency increases susceptibility to benzo[a]pyrene-induced lymphomagenesis. Int J Cancer 118(11):2899–2902
Acknowledgements
The author expresses sincere appreciation to Drs. George Woodall, Sury Vulimiri, Jason Fitz, Kathleen Newhouse, Yu-Sheng Lin and Bob Sonawane of NCEA, EPA for their critical review and helpful suggestions during the preparation of the manuscript. Sincere appreciation is also for NCEA management for allowing me to take up this task and helping me throughout the agency clearance process.
Disclaimer
The views expressed in this Chapter are those of the author and do not necessarily reflect the views or policies of the U.S. Environmental Protection Agency.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag London
About this chapter
Cite this chapter
Mudipalli, A. (2015). Airborne Carcinogens: Mechanisms of Cancer. In: Nadadur, S., Hollingsworth, J. (eds) Air Pollution and Health Effects. Molecular and Integrative Toxicology. Springer, London. https://doi.org/10.1007/978-1-4471-6669-6_6
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6669-6_6
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6668-9
Online ISBN: 978-1-4471-6669-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)