Abstract
The most critically ill patients can now be treated with life saving mechanical circulatory support. The development of databases to track the outcomes of patients with critical illness has been ongoing for much of the last two decades. Clinicians who engage in the use of mechanical circulatory support are interested in the analysis of outcomes of patients treated with Extracorporeal Membrane Oxygenation (ECMO) and Ventricular Assist Devices (VAD), with the ultimate aim of improvement in the quality of care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ventricular assist device
- Extracorporeal Membrane Oxygenation
- ECMO
- VAD
- Database
- Registry
- Quality improvement
Introduction
The most critically ill patients can now be treated with mechanical circulatory support. Extracorporeal life support using Extracorporeal Membrane Oxygenation (ECMO) is used to provide cardiopulmonary support in patients with life threatening cardiorespiratory failure unresponsive to conventional medical therapies. Mechanical circulatory support using Ventricular Assist Devices (VAD) is used to provide cardiovascular support in patients with end stage heart failure refractory to conventional medical therapies. The development of databases to track the outcomes of patients with critical illness has been ongoing for much of the last two decades, paralleled by the increasing awareness of the impact on outcomes of patients obtained from programs designed to improve quality and enhance the safety of patients. Clinicians who engage in the use of mechanical circulatory support are interested in the analysis of outcomes of patients treated with ECMO and VAD with the ultimate aim of improvement in the quality of care provided to these patients.
The Extracorporeal Life Support Organization (ELSO) is an international consortium of health care professionals and scientists who are dedicated to the development and evaluation of novel therapies for support of failing organ systems. Since 1989, ELSO has maintained a registry of the use of ECMO in active ELSO centers. The Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) is a national registry in the United States of America for patients who are receiving mechanical circulatory support device therapy to treat advanced cardiac failure. This registry was devised as a joint effort of the National Heart, Lung and Blood Institute (NHLBI), the Centers for Medicare and Medicaid Services (CMS), the Food and Drug Administration (FDA), clinicians, scientists, and industry representatives in conjunction with the University of Alabama at Birmingham (UAB) and United Network for Organ Sharing (UNOS).
This Chapter will focus on databases used to track outcomes of critically ill patients treated with ECMO and VAD. This review discusses the historical aspects, current state of analysis of outcomes, and the potential for transitioning from acquisition of data to improvement of quality and enhanced safety in the care of these patients.
ELSO Registry
Extracorporeal Membrane Oxygenation
Extracorporeal life support using Extracorporeal Membrane Oxygenation (ECMO) is used to provide cardiopulmonary support in patients with life threatening cardiorespiratory failure unresponsive to conventional medical therapies [1]. ECMO can be lifesaving in these patients as they face imminent mortality without mechanical circulatory and/or respiratory support. Although lifesaving for many patients, ECMO does not treat primary illness that caused cardiopulmonary failure and is merely a modality of cardiopulmonary support for providing perfusion to end-organs while awaiting recovery of the primary condition or disease causing cardiopulmonary failure. Thus, outcomes following ECMO use are largely influenced by the prognosis for the primary disease (Table 16.1) [2]. Use of ECMO, indications for ECMO, and number of centers providing ECMO support have increased over the last decade. Even though ECMO offers potentially lifesaving support for many patients, many issues exist regarding the use of ECMO that require careful consideration:
-
First, despite increasing use, greater experience, and newer and improved equipment and technology, mortality following ECMO support is high and has largely remained unchanged over decades.
-
Second, considerable variability exists in many areas in the clinical practice of ECMO [3]. These areas include selection of patients for ECMO, timing of ECMO deployment, equipment used to provide ECMO, practice of anticoagulation while on ECMO, management of patients on ECMO, and weaning from ECMO.
-
Third, safe and efficient use of ECMO requires easy availability of equipment and personnel to deploy and manage ECMO 24 hours a day, resulting in the need for a large amount of resources and expenditure [4].
-
Finally, growing evidence shows that survival after ECMO is related to the characteristics of the center providing ECMO, such as volume of patients managed in the center [5, 6].
These issues have raised the need for tools to assess the quality of care provided to patients supported with ECMO and to evaluate of “best” ECMO practices. One resource available for improving care provided to ECMO patients is the ECMO registry of the Extracorporeal Life Support Organization (ELSO). The following paragraphs describe the history, details of the registry, and potential for its use for purposes of assessment of quality.
ECMO Registry of ELSO
The ECMO registry of ELSO is a data registry that collects information about ECMO across all age groups and for all ECMO indications. ELSO was formed in 1989 to improve knowledge and clinical use of Extracorporeal Life Support therapies [7, 8]. The organization’s data registry contains data on patients dating as far back as 1976 and has played a pivotal role in our current understanding and practice of ECMO support. Currently over 200 International centers submit data to the registry. Membership in ELSO is required for submitting data to the registry. Data collected include:
-
demographics of patients supported with ECMO,
-
condition of the patient prior to ECMO,
-
support of the patient prior to ECMO,
-
diagnosis (using International classification of Disease; ICD-9 codes),
-
procedures performed prior to and during ECMO (Common Procedural Terminology; CPT and Unique ELSO registry codes),
-
details about ECMO equipment,
-
duration of ECMO support,
-
complications acquired during ECMO (using unique ELSO Registry codes), and
-
Information about survival including survival to weaning off ECMO and survival to discharge from the hospital.
Data are submitted using standardized data collection forms. Recent changes to the process of submission of data include using a secure, web-based system of entry of data. As with other databases and registries, submission of data to ELSO requires approval by the local institutional review board at member centers. A data user agreement allows release of de-identified data to member centers for purposes of benchmarking and scientific research.
Uses for ECMO Registry Data
An important function of ELSO is maintaining a data registry for purposes of
-
improving outcomes of patients supported with ECMO,
-
reducing morbidity associated with ECMO, and
-
fostering innovations both in the care of patients supported with ECMO and the technology associated with ECMO.
The following paragraphs describe the uses of data from the ELSO registry of these purposes.
-
(a)
Registry Report: The Registry provides a yearly summary report of data contained in the registry and has periodically published a registry report containing detailed information on trends in use of ECMO and outcomes associated with ECMO (Table 16.1) [2]. These reports serve as valuable resources for providers of ECMO and ECMO centers for
-
assessment of need,
-
programmatic planning, and
-
identifying areas for improvement related to ECMO.
-
-
(b)
Scientific Research: The registry provides investigators limited de-identified datasets for purposes of scientific inquiry and research. Areas of scientific research [9–15] have included
-
indications for ECMO,
-
analysis of outcomes stratified by specific disease or procedure,
-
complications associated with ECMO, and
-
assessment of outcomes associated with various technologies (e.g. type of pump and outcomes).
Many examples of these publications can be searched using commonly available search engines such as PubMed.
-
-
(c)
Data for regulatory use: The registry collects detailed information on the various types of equipment associated with ECMO. These data can be used to serve as preliminary data for planning clinical trials, or used as comparative data for studying safety and efficacy of devices related to ECMO. One recent example is the use of data from the ELSO registry as a comparative cohort for the recently concluded trial of the Berlin Heart EXCOR Pediatric Ventricular Assist Device conducted by the Food and Drug Administration (FDA) of the United States of America [16].
-
(d)
Benchmarking and Assessment of Quality: In addition to the detailed international summary containing a summarized data from all centers, member centers contributing data to ELSO are provided with a center specific data describing specific information on use of ECMO, complications associated with ECMO, and outcomes. These center specific reports categorize outcomes and complications based on indications for ECMO. Given that rates of survival after ECMO vary widely by indication for ECMO, the availability of outcomes and complications categorized by indications in the international summary and center specific reports allows center specific benchmarking of outcomes and complications without detailed risk adjustment. Center specific reports provide opportunities for a specific ECMO program to set goals for future improvement in performance.
-
(e)
Limitations of the ELSO registry data: Several limitations of the data reported to the registry should be carefully considered when using these data for purposes of research and benchmarking.
-
The registry does not have a robust process of verification of data to ensure the completeness and accuracy of the submitted data. The move towards web-based submission of data has allowed implementation customization of fields of data that can help assure the integrity of the submitted data and improve the validity of the submitted data.
-
A robust and detailed methodology of risk adjustment is not available to facilitate comparison of center specific outcomes. Even though comparability is improved based on categorization by indication for ECMO, outcomes associated with ECMO vary widely based on diagnosis within a category, and a more advanced and detailed methodology of risk adjustment may provide improved comparability of programmatic performance (Table 16.2).
Table 16.2 The impact of diagnosis category on survival for neonates using ECMO for respiratory indications from the International Summary of the Extracorporeal Life Support Organization’s ECMO Registry, July 2013 -
Functional outcome after ECMO and data about quality of life are not available to improve our understanding of these important issues in survivors of ECMO.
-
In summary, the ECMO registry of ELSO has played an important role in our understanding of use of ECMO and outcomes associated with ECMO. It remains an important resource for benchmarking and improvement of quality for ECMO programs worldwide.
Ventricular Assist Device Database
The Food and Drug Administration (FDA) entered into the arena of mechanical circulatory support devices (MCSDs) in the late 1970s with the intention to create methods of regulation of devices. The development use of MCSDs flourished, and the Institute of Medicine issued a report in 1991 stating that patients implanted with MCSDs should be followed through a registry for the remainder of their lives, recommending that this initiative be spearheaded by the National Heart, Lung & Blood Institute (NHLBI). In June of 2006, the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) was established as a joint effort between the NHLBI, Centers for Medicare and Medicaid Services (CMS), FDA, representatives from industry, scientists, and clinicians. The goal of this partnership was to provide contemporary data for patients who are receiving mechanical circulatory support device therapy as a treatment of advanced cardiac failure. This collaboration established a concerted effort by physicians and partners from industry
-
to define adverse events precisely,
-
to provide information that would allow optimal MCSD-patient matching,
-
to move devices from investigational device exemption (IDE) trials into post-market approval for clinical use, and
-
to create a meaningful system of classification relevant to selection of patients for support with MCSDs.
INTERMACS is the North American prospective registry utilized to collect clinical data to demonstrate outcomes over time to [17]:
-
1.
Facilitate the refinement of selection of patients to maximize outcomes with current and new devices
-
2.
Identify predictors of good outcomes as well as risk factors for adverse events after implantation of devices
-
3.
Develop consensus “best practice” guideline to improve clinical management by reducing short-term and long-term complications of therapy with mechanical circulatory support devices
-
4.
Utilize information from the INTERMACS Registry to guide improvements in technology, particularly as next generation devices evolve
-
5.
Guide clinical testing and approval of new devices.
Information in the database includes
-
data about the profile of patients,
-
data about the implantation of devices,
-
defined follow-up information at scheduled intervals, and
-
event-driven data.
Key details that are captured by the INTERMACS registry include
-
the quality of life of the patient,
-
the level of function of the patient,
-
death,
-
occurrence of explantation of the device,
-
occurrence of transplantation, and
-
adverse events as defined by the registry.
These indices have become essential to the evaluation of therapy with MCSDs and the improvement of survival and functional status of the patients.
The treatment and management of advanced cardiac failure has matured over the past several years with the increased use of second and third generation mechanical circulatory support devices and subsequent crossover into the realm of pediatrics. Accordingly, a multidisciplinary team of clinicians with expertise in pediatric cardiac failure, including cardiac surgeons led the development of the pediatric arm of the INTERMACS registry. This pediatric arm of INTERMACS, entitled pediMACS, was launched in September of 2012 with the aim to mirror the goals and expected analyses of the main INTERMACS registry, but in patients less than 19 years old at the time of implant. This new registry would contain broader data about implants, to include both durable and temporary support devices. Other subtle variances include modifications to the existing definitions of adverse events and expansion of the instruments utilized to assess quality of life. PediMACS will additionally evaluate therapy with MCSDs in the pediatric population by focusing on
-
the differences in devices available for implantation, and
-
the complexity surrounding the selection of both the types of devices and the appropriate children for therapy with these devices.
These data are essential for measuring outcomes of patients and evaluating new cutting edge pediatric-specific devices.
Adverse events are clearly defined by INTERMACS and pediMACS and are captured by two mechanisms:
-
1.
The occurrence of infection, device failure, neurological injury, death (INTERMACS only) and bleeding (pediMACS only) trigger additional elements of data to be obtained; and
-
2.
Other adverse events that have been identified are routinely collected at defined follow-up intervals. Other adverse events captured include.
-
cardiac arrhythmias,
-
failure of the right heart,
-
arterial thromboembolic events outside of the central nervous system,
-
hypertension,
-
pericardial fluid collection,
-
myocardial infarction,
-
venous thromboembolism,
-
wound dehiscence,
-
renal dysfunction,
-
hemolysis,
-
hepatic dysfunction, and
-
respiratory failure.
Quality of life assessments are also obtained from patients, parents, and caregivers at pre-determined intervals (pre-implant, 3 months, 6 months, and every 6 months thereafter), with both registries utilizing uniform tools (i.e. EQ-5d and the Kansas City Cardiomyopathy Questionnaire [KCCQ]).
The acquisition of timely data is the driving force behind the pediMACS and INTERMACS registries. This information has been utilized in
-
obtaining approval from the FDA,
-
providing comparison arms in clinical trials,
-
comparing medical therapy and therapy with MCSDs as treatment for cardiac failure, and
-
creating a true venue for debate.
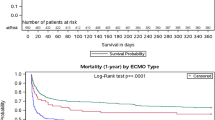
As the registry moves forward, these pertinent data will continue to identify risk stratifying factors and predictors for morbidity and mortality and then aid in the formulation of novel methods and strategies of care to minimize these risks. INTERMACS completed an analysis of the first full year of data on FDA-approved durable VADs in 2008 that represented 511 patients from 75 institutions [17]. Comparably, the fifth annual report was published in 2013, which summarizes and analyzes the first 6 years of collection of data, with more than 6,000 patients enrolled.
Since the inception of the INTERMACS database, it has generated useful information for a multitude of centers and has provided data for
-
publications about MCSDs,
-
review of outcomes, and
-
programs to improve quality.
The data learned from the registry has been essential in addressing several key questions in the field and providing risk stratification (i.e. device related infection, pump thrombosis, failure of the right heart, etc.) as well as publishing rates of survival of patients having been implanted with durable VADs. The futures for the INTERMACS and pediMACS databases are to not be geographically limited. The leadership of the International Society for Heart and Lung Transplantation (ISHLT) is aiming to collaborate and consolidate European and Asian databases (i.e.: EuroMACS, J-MACS) into a single database named the ISHLT Mechanical Assisted Circulatory Support Registry (IMACS) [18].
Conclusions
A great deal has already been accomplished to standardize and improve methodologies for the analysis of outcomes following the treatment of patients with ECMO and VAD. While these achievements have laid the groundwork, much remains to be accomplished. We can, and should, rise to the challenge, by more effectively:
-
defining and measuring outcomes,
-
setting standards to benchmark results, and
-
using these data to change and improve upon our current practice and these results.
International efforts to standardize definitions of complications relating to perfusion and extracorporeal circulation associated with the treatment of patients with congenital cardiac disease has led to the publication of “Consensus Definitions from the Multi-Societal Database Committee for Pediatric and Congenital Heart Disease” [19, 20]. These publications define multiple terms related to ECMO and VAD:
-
“Cardiopulmonary bypass is defined as the process of diverting venous blood from a patient’s heart and lungs to a gas exchange system for the addition of oxygen, removal of carbon dioxide, and subsequent re-infusion to the patient’s arterial system.”
-
“Extracorporeal membrane oxygenation is defined as the process of diverting venous blood from a patient to a gas exchange system for the addition of oxygen, removal of carbon dioxide, and subsequent re-infusion to the patient’s arterial or venous system.”
-
“A mechanical circulatory support device is defined as a pump or apparatus that augments or replaces the function of the failing heart. Two types of mechanical circulatory support devices are ventricular assist devices and intra-aortic balloon pumps.”
A non-comprehensive listing of areas in need of future development includes:
-
1.
Standardizing and unifying the tools for stratification of complexity
-
2.
Improving the tools for stratification of complexity in order to account for patient-specific variables
-
3.
Creating methodologies for analysis beyond mortality as an endpoint
-
4.
Improving methodologies for verification of data
-
5.
Establishing links between databases
-
6.
Standardizing long term follow-up
Only through a commitment to transitioning from data collection and analysis to continuous quality improvement can we leverage these data to achieve the optimal outcomes for our patients and their families.
References
Gaffney AM, Wildhirt SM, Griffin MJ, et al. Extracorporeal life support. BMJ. 2010;341:c5317.
International Summary of The Extracorporeal Life Support Organization. [www.elsonet.org].
Bembea MM, Annich G, Rycus P, et al. Variability in anticoagulation management of patients on extracorporeal membrane oxygenation: an international survey. Pediatr Crit Care Med. 2013;14(2):e77–84.
Vats A, Pettignano R, Culler S, Wright J. Cost of extracorporeal life support in pediatric patients with acute respiratory failure. Crit Care Med. 1998;26(9):1587–92.
Freeman CL, Bennett TD, Casper TC, et al. Pediatric and neonatal extracorporeal membrane oxygenation: does center volume impact mortality? Crit Care Med. 2013;42(3):1–8.
Karamlou T, Vafaeezadeh M, Parrish AM, et al. Increased extracorporeal membrane oxygenation center case volume is associated with improved extracorporeal membrane oxygenation survival among pediatric patients. J Thorac Cardiovasc Surg. 2013;145(2):470–5.
Conrad SA, Rycus PT. The Registry of the Extracorporeal Life Support Organization. In: Annich GM, Lynch WR, Maclaren G, Wilson JM, Bartlett RH, editors. ECMO: extracorporeal cardiopulmonary support in critical care. 4th ed. Ann Arbor: The Extracorporeal Life Support Organization; 2012. p. 87–104.
Paden ML, Conrad SA, Rycus PT, Thiagarajan RR. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2012;59(3):202–10.
Barrett CS, Jaggers JJ, Cook EF, et al. Outcomes of neonates undergoing extracorporeal membrane oxygenation support using centrifugal versus roller blood pumps. Ann Thorac Surg. 2012;94(5):1635–41.
Barrett CS, Jaggers JJ, Cook EF, et al. Pediatric ECMO outcomes: comparison of centrifugal versus roller blood pumps using propensity score matching. ASAIO J. 2013;59(2):145–51.
Fleming GM, Gurney JG, Donohue JE, et al. Mechanical component failures in 28,171 neonatal and pediatric extracorporeal membrane oxygenation courses from 1987 to 2006. Pediatr Crit Care Med. 2009;10(4):439–44.
Polito A, Barrett CS, Wypij D, et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. An analysis of ELSO registry data. Intensive Care Med. 2013;39(9):1594–601.
Rollins MD, Hubbard A, Zabrocki L, et al. Extracorporeal membrane oxygenation cannulation trends for pediatric respiratory failure and central nervous system injury. J Pediatr Surg. 2012;47(1):68–75.
Zabrocki LA, Brogan TV, Statler KD, et al. Extracorporeal membrane oxygenation for pediatric respiratory failure: survival and predictors of mortality. Crit Care Med. 2011;39(2):364–70.
Thiagarajan RR, Laussen PC, Rycus PT, et al. Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation. 2007;116(15):1693–700.
Fraser Jr CD, Jaquiss RD, Rosenthal DN, et al. Prospective trial of a pediatric ventricular assist device. N Engl J Med. 2012;367(6):532–41.
Kirklin JK, Naftel DC, Stevenson LW, et al. INTERMACS database for durable devices for circulatory support: first annual report. J Heart Lung Transplant. 2008;27(10):1065–73.
Holman WL. Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS): what have we learned and what will we learn? Circulation. 2012;126(11):1401–6.
Shann KG, Giacomuzzi CR, Harness L, Myers GJ, Paugh TA, Mellas N, Groom RC, Gomez D, Thuys CA, Charette K, Ojito JW, Tinius-Juliani J, Calaritis C, McRobb CM, Parpard M, Chancy T, Bacha E, Cooper DS, Jacobs JP, Likosky DS, on behalf of the International Consortium for Evidence-Based Perfusion. Complications relating to perfusion and extracorporeal circulation associated with the treatment of patients with congenital cardiac disease: consensus definitions from the Multi-Societal Database Committee for Pediatric and Congenital Heart Disease. In: 2008 supplement to Cardiology in the Young: databases and the assessment of complications associated with the treatment of patients with congenital cardiac disease, prepared by: The Multi-Societal Database Committee for Pediatric and Congenital Heart Disease, Jeffrey P. Jacobs, MD, editor. Cardiol Young. 2008;18(Suppl 2):206–14.
Jacobs JP, editor. 2008 Supplement to Cardiology in the Young: databases and the assessment of complications associated with the treatment of patients with congenital cardiac disease, prepared by: The Multi-Societal Database Committee for Pediatric and Congenital Heart Disease. Cardiol Young. 2008;18(Suppl S2):1–530.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag London
About this chapter
Cite this chapter
Cooper, D.S., Morales, D.L.S., del Corral, M., Paden, M.L., Thiagarajan, R.R. (2015). Databases for Extracorporeal Membrane Oxygenation and Ventricular Assist Devices. In: Barach, P., Jacobs, J., Lipshultz, S., Laussen, P. (eds) Pediatric and Congenital Cardiac Care. Springer, London. https://doi.org/10.1007/978-1-4471-6587-3_16
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6587-3_16
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6586-6
Online ISBN: 978-1-4471-6587-3
eBook Packages: MedicineMedicine (R0)