Abstract
The hand is a common site of peripheral joint involvement in osteoarthritis (OA) and, although often underestimated as a cause of disability, the effect on the quality of life, from limitations in performing activities of daily living such as dressing and feeding, may be considerable. One longitudinal radiographic study of 751 patients over a 24 year period, showed that in those without OA at baseline, women had more incident disease than men in almost all hand joints, but the joints most frequently affected were the same in both sexes: the distal interphalangeal (DIP), followed by the base of the thumb, proximal interphalangeal (PIP) and metacarpophalangeal (MP) joints [1]. In another radiographic study of 3,327 men and women between the ages of 40–80+, the DIP joint demonstrated the highest OA prevalence, while the PIP joint showed the lowest. Joint-specific hand OA prevalence rates for the second DIP, third PIP and trapeziometacarpal (TM) joint were 35, 18 and 21 %, respectively. Women demonstrated higher hand OA prevalence rates for the three sites examined [2]. The age adjusted prevalence of CMC arthritis based on radiographic evidence has been reported to be 15 % for the female population and 7 % for the male population [3]. The prevalence increases to 33 % for the postmenopausal female population. This predilection for the thumb axis makes it one of the most expensive and debilitating diseases in terms of cost of diagnosis, treatment and lost productivity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Osteoarthritis
- Carpometacarpal
- Trapeziometacarpal
- Scaphotrapezial
- Thumb
- Interphalangeal joint
- Metacarpophalangeal joint
- Fusion
- Arthrodesis
- Arthroplasty
- Arthroscopic
- Outcomes
- Complications
Introduction
The hand is a common site of peripheral joint involvement in osteoarthritis (OA) and, although often underestimated as a cause of disability, the effect on the quality of life, from limitations in performing activities of daily living such as dressing and feeding, may be considerable. One longitudinal radiographic study of 751 patients over a 24 year period, showed that in those without OA at baseline, women had more incident disease than men in almost all hand joints, but the joints most frequently affected were the same in both sexes: the distal interphalangeal (DIP), followed by the base of the thumb, proximal interphalangeal (PIP) and metacarpophalangeal (MP) joints [1]. In another radiographic study of 3,327 men and women between the ages of 40–80+, the DIP joint demonstrated the highest OA prevalence, while the PIP joint showed the lowest. Joint-specific hand OA prevalence rates for the second DIP, third PIP and trapeziometacarpal (TM) joint were 35, 18 and 21 %, respectively. Women demonstrated higher hand OA prevalence rates for the three sites examined [2]. The age adjusted prevalence of CMC arthritis based on radiographic evidence has been reported to be 15 % for the female population and 7 % for the male population [3]. The prevalence increases to 33 % for the postmenopausal female population. This predilection for the thumb axis makes it one of the most expensive and debilitating diseases in terms of cost of diagnosis, treatment and lost productivity.
Osteoarthritis is not merely a wear and tear or age related phenomenon, but it is a common disease of articular cartilage that becomes more prevalent with advancing age. The biomechanical loads are of importance. In a biomechanical study, Cooney and Chao demonstrated that a pinch force of 1 kg at the thumb tip was amplified to 3.68 kg at the IP joint, 6.61 kg at the MCP joint and up to 13.42 kg at the TM joint. The typical joint compression forces averaged three kilograms of force at the interphalangeal joint, 5.4 kg at the metacarpophalangeal joint and 12.0 kg at the TM joint during simple pinch. Compression forces of as much as 120 kg may occur at the TM joint during strong grasp [4]. The alterations in the contact forces that may occur after injury or surgery to the TM joint due to ligamentous insufficiency, can lead to even higher forces, which can accentuate the wear on the articular cartilage. In this chapter the discussion will focus on OA affecting the thumb interphalangeal (IP) joint, the MP and the trapeziometacarpal (TM) joints.
History and Examination
IP and MP Joints
Similar to other joints, underlying OA of the thumb joints may be asymptomatic. The symptomatic patient, however, will typically present with complaints of joint stiffness, possible instability and pain. With IP involvement, one sees joint enlargement (Heberdens node) and possibly joint subluxation with flexion/extension or varus/valgus deformities due to collateral ligament incompetence. A palpable joint effusion is not common as compared to an inflammatory arthritis. There may be crepitus with motion and/or loading, but this is not always painful. A mucoid cyst, with or without a nail groove, is a frequent association and may require separate treatment. With MP joint involvement, one will also see joint enlargement (Bouchards node), loss of motion and possibly instability. An MP joint hyperextension deformity is often associated with the lateral subluxation of the thumb metacarpal that occurs with TM OA and must be addressed separately. A flexion deformity seems to be more common in primary MP OA. Stress testing of the radial and ulnar collateral ligaments in extension and flexion may reveal a chronic ulnar or radial collateral ligament tear, which can be a primary cause of isolated post traumatic OA.
The radiographic evaluation of the IP and MP joint of the thumb includes posteroanterior, lateral and oblique views. Radiographically, the features of OA include joint space narrowing due to the erosion of the articular cartilage, the development of periarticular osteophytes and subchondral cysts.
Trapeziometacarpal Joint
The patient who presents with basal joint arthritis may complain of palmar-sided pain, which is frequently localized to the thenar eminence and may radiate up the radial wrist. Complaints of thumb weakness and clumsiness with fine manipulation tasks are common. On inspection, one may see a prominent TM joint, due to lateral subluxation of the thumb metacarpal base with or without marginal osteophytes and synovitis. There is often a loss of joint motion, especially thumb retropulsion and there may be a contracted first web space which interferes with grasping large objects. MP joint hyperextension may occur as an adaptive response to increase the first web span. There may be thenar muscle weakness and atrophy due to misuse. A concomitant carpal tunnel syndrome, however, should be sought by history of a sensory loss in the median nerve distribution, as well as through physical findings, which include a tinels sign over the carpal tunnel and a positive Phalen’s test or median nerve compression test. On palpation, the patient will often have tenderness localized to the TM joint and the scaphoid tuberosity as well as a positive scaphoid shift test, but this may also occur with scapholunate instability or scaphotrapeziotrapezoidal (STT) OA, which should be ruled out. Flexor carpi radialis tendinitis can also present with tenderness over the scaphoid tuberosity. The trapeziometacarpal grind test will be positive in the face of TM OA and can help to distinguish these entities. The test is performed by applying an axial load to the thumb metacarpal, combined with manipulation of the metacarpal in a dorsal and volar direction. A positive test will produce variable degrees of crepitus and pain, depending on the stage of the arthritis. Alterations in grip and pinch strengths are documented in order to gauge the effects of treatment, but are nonspecific findings.
The radiographic evaluation of the thumb carpometacarpal joint includes a true anteroposterior view, which is performed by placing the forearm in maximum pronation, with the dorsal aspect of the thumb resting on the x-ray table and a true lateral view. A radial stress view of the thumb can be performed by asking the patient to push the radial borders of their thumbs together. This can demonstrate the degree of joint laxity by the amount of lateral subluxation of the metacarpal base. Littler and Eaton described a radiographic staging classification of TM OA, which is in wide use (Table 5.1) [5]. Stage I comprises normal articular surfaces without joint space narrowing or sclerosis. There is less than 1/3 subluxation of the metacarpal base. Stage II reveals mild joint space narrowing, mild sclerosis or osteophytes < 2 mm in diameter. Instability is evident on stress views with > 1/3 subluxation. The STT joint is normal. In stage III there is significant joint space narrowing, subchondral sclerosis and peripheral osteophytes > 2 mm in diameter, but a normal STT joint. In stage IV there is pantrapezial OA with narrowing, sclerosis and osteophytes involving both the TM and STT joints. Burton modified this classification by incorporating the clinical findings [6]. Stage I includes ligamentous laxity and pain with forceful and/or repetitive pinching. The joint is hypermobile, which can be seen on stress views, but the x-rays are normal. In stage II crepitus and instability can be demonstrated clinically, whereas x-rays reveal a loss of the joint space. Stage III and IV are similar to Eaton’s classification.
Etiology
MP and IP Joints
Although mechanical stress has been postulated to play a role in the development of thumb IP and MP joint OA, handness has not been shown to have a clear association with either [7]. Post traumatic OA, following an intra-articular fracture, can occur at either joint, in addition to MP joint OA joint can occur as a sequelae of long standing radial and ulnar collateral ligament instability.
Trapeziometacarpal Joint
Primary thumb osteoarthritis typically presents at the TM joint. Women are affected more frequently than men, which may be the result of anatomic variations between the sexes [8] or repetitive activities, but an occupational causation has been hard to prove. The deep anterior oblique ligament, or volar beak ligament and the dorsal radial ligament have been shown to be the principal checkreins to dorsal subluxation during physiologic motion of the trapeziometacarpal joint. During key pinch, the incongruity of the articular surfaces causes apex loading on the volar articular surface of the trapezium, which transmits loads that are as high as 13 times the joint reactive force [9]. Because of the repeated eccentric loading, osteoarthritic changes begin volarly. Any laxity or incompetence to the anterior oblique ligament allows this fulcrum to move dorsally and adds to the eccentric force concentration. Post traumatic OA can also be seen after mal-reduced intra-articular fractures or sepsis.
Treatment
IP Joint
Save for historical reports [10], implant arthroplasty for the IP joint is not common. The mainstay of treatment consists of activity modification with the use of assistive devices and removable static IP joint splints. NSAIDs and selected cortisone injections are often beneficial, provided medical monitoring is instituted with chronic use. With unrelieved pain or disabling joint instability an IP joint fusion is the procedure of choice. The techniques are straightforward. Most consist of a dorsal capsulotomy, followed by removal of the joint surfaces and immobilization of the joint with percutaneous k-wires or a headless compression screw. Cobb has described an arthroscopic assisted procedure using a headless screw [11].
IPJ Arthrodesis
A longitudinal or S-shaped incision is made, centered over the IP joint. The extensor mechanism and dorsal capsule are divided in the midline, keeping the tissue planes separate for soft tissue closure over any exposed hardware. The collateral ligaments are released by sliding a scalpel blade underneath the insertion of the ligament on the neck of the proximal phalanx and cutting upwards to prevent injury to the neurovascular bundles. It is my preference to use a cup and cone arthrodesis, which allows one to adjust the amount of rotation and varus/valgus without increasing the risk of joint incongruity. The joint can be fused in neutral or 15–25° of flexion (Fig. 5.1a, b). A rongeur is used to gently remove any cartilage remnants on the head of the proximal phalanx, while preserving the normal convexity of the condyles since the metaphyseal bone is often quite soft, which can lead to excessive bone removal. The cartilage and subchondral bone is removed from the base of the distal phalanx matching the curve of the head of the proximal phalanx and preserving a circumferential rim of cortical bone. Two convergent double ended 0.035 (0.9 mm) or 0.045 in. (1.1 mm) K-wires are advanced in a retrograde fashion through the base of the distal phalanx and out through the thumb tip. Ideally the k-wires should be placed immediately underneath the nail plate. The joint surfaces are then manually compressed in the desired degree of rotation and in neutral angulation or mild flexion, while the k-wires are advanced down the intramedullary canal of the proximal phalanx, until they abut the cortex or subchondral bone plate of the phalangeal base. The k-wire position is checked fluoroscopically and adjusted as necessary. Any defects at the fusion site can be packed with local bone graft or bone substitute. The capsule and extensor mechanism are closed in layers, followed by tourniquet release and skin closure.
When a headless screw is used, the joint is fused in neutral to prevent screw cut out and to permit adequate insertion down the intramedullary canal of the proximal phalanx. One of the k-wires is used as a guide wire to allow screw insertion in a retrograde fashion through the distal pulp. Due to the small canal size, caution is needed to prevent screw cut out in the distal phalanx or interference with the nail matrix. The screw head should be buried in the distal tuft to prevent tenderness with tip pinch, while insuring there are adequate numbers of screw threads (at least 4) crossing the fusion site. Post operatively, the IP joint is immobilized for 6–8 weeks until there are radiographic signs of union at which time a home program of gradual strengthening is instituted.
Outcomes
Most series are concerned mostly with the results of DIP arthrodesis and include but a few cases of thumb IPJ arthrodesis. Sieber and Segmuller, however, reported a series of 32 IP joint fusions using a figure-of-eight tension band wire and two crossed K-wires. They adapted the angle of fusion based on the patient needs: for instrument grip, the IP joint was fused in 5–10° of flexion, while for precision grip a larger angle of 20–30° was preferred. They believed tactile gnosis was best preserved when pronation of 5–10° and slight ulnar deviation of 5° of the distal phalanx, in relation to the proximal phalanx, was achieved. They also switched from an H-shaped incision to a fork shaped incision to better preserve distal sensation [12]. Stern and Fulton reviewed 131 patients (61 with OA) who underwent a distal joint fusion, 37 of whom had an IP joint fusion. Techniques included crossed K-wires with and without cerclage wires or Herbert screws, but the breakdown by joint was not listed. There were 4/37 IPJ non-unions as compared to 17/144 DIP non-unions. Time to union was not specified by joint, but averaged 9 weeks for k-wires, 7 ½ weeks with cerclage wires and 10 weeks with screws. There were two thumb infections vs. four finger infections [13]. Clearly the data is lacking to recommend one type of fixation method over another with IP joint OA, hence surgeon preference largely dictates the technique.
MP Joint
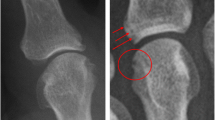
The MP joint can be adequately splinted using a custom palmar based thumb spica splint. NSAIDs and activity modification, with avoidance of repetitive pinching exercises, will provide adequate pain control in many cases. One or two selected cortisone injections can provide temporary relief, but should not be used as a chronic form of treatment. Thumb metacarpophalangeal joint arthroscopy can be of use for staging the degree of articular involvement, synovectomy and removal of loose bodies in early OA (Fig. 5.2a, b). Thumb MP arthroplasty for OA is not commonly performed. Historically, a few investigators have attempted this with mixed results. Brannon and Klein reported the first prosthetic MP joint in 1959. This early prosthesis was a hinged replica of the MP joint and was constructed of stainless steel initially and then titanium [14]. Moreover, these implants were shown to corrode after some time and the bone was unable to tolerate the metal.
Swanson popularized the use of Silastic arthroplasty using a silicone dioxide elastomer, which was used as an elastic spacer for the treatment of rheumatoid arthritis in the finger MP joints. Swanson and Herndon reported on their experience, with its use for rheumatoid thumb deformities (mostly Boutonniere) in 44 rheumatoid thumb MP joint, with good to excellent results at a 2–6 years follow up [15]. In a longer term study of 38 patients with 43 implants, good pain relief and function was noted with only one revision at a mean follow up of 6 1/2 years (3–13 years) [16].
In 1981, Beckenbaugh and Steffee reported their experience with a two-part metal and polyethylene prosthesis that were snap locked together. Their series included 8/42 MP joint replacements in patients with MP OA. Due to the limited arc of motion (16°) and equal functional and aesthetic outcomes, as compared to an MP fusion, this prosthesis was largely abandoned [17]. Pyrocarbon implants are currently in vogue for treatment of MP OA in the finger joints, but studies on their use in the thumb MP joint are lacking.
MP Joint Arthroscopy
The procedure is often done under tourniquet control with the 10 lbs. of thumb distraction using a wrist tower and a 1.9 mm, 30° angle arthroscope. A 2.0-mm shaver is useful, but a thermal probe can be used sparingly and with caution due to the risk of thermal injury to the articular cartilage and/or tendon in a small joint. The two portals are localized with a 22 gauge needle on either side of the extensor hood, followed by a shallow skin incision and insertion of the cannula and scope. The volar aspect of the joint is poorly seen, but the volar plate can be elevated with percutaneous insertion of a freer elevator. A synovectomy and removal of loose bodies can provide symptomatic comfort. Small chondral defects can be drilled to stimulate fibrocartilage formation. Following portal closure a bulky dressing is used for the first week, followed by thumb mobilization.
MP Fusion
The most popular form of treatment for painful MP joint OA or instability is an arthrodesis. There are a number of options including K-wire fixation, with and without adjuvant tension band fixation, screw and plate fixation. According to Inglis et al. the MP joint of the thumb should be fused in approximately 15° of flexion, along with mild pronation and abduction of the proximal phalanx to facilitate tip pinch with the fingers [18].
Most procedures begin with a straight or S-shaped incision centered over the MP joint, followed by a midline incision through the extensor hood and capsule. A cup and cone technique is my preference, similar to the IP joint, with the thumb flexed approximately 15°. With severe deformity or bone loss, matching bone cuts can be made, but it is more difficult to achieve congruity at the fusion site if the MP joint is placed in flexion. The articular cartilage and subchondral bone is removed, preserving the matching convexity/concavity of the joint surfaces. The joint is held in mild flexion and two convergent 0.035 or 0.045 in. Kirschner wires are inserted through the dorsal neck of the thumb metacarpal neck and advanced distally down the intramedullary canal of the proximal phalanx to the subchondral bone at the IP joint, or alternatively engaging the palmar cortex at the midportion of the proximal phalanx. A transverse bone tunnel is drilled dorsal to the neutral axis at least 5 mm from the fusion site, with a 0.045 in. k-wire to prevent cut out. A 22- gauge wire strand is passed through the bone tunnel, looped in a figure of eight fashion over the longitudinal pins and simultaneously twisted on the radial and ulnar sides just until the point of deformation of the twisted loop is seen. The K-wires are then withdrawn 5 mm, bent 90° using a needle holder and suction tip and then tamped back in to place capturing the tension band loop with the hooked ends, which are buried in bone. Bone graft substitute is used to fill any gaps at the fusion site. All sharp metal ends are trimmed and the capsule is closed over the exposed hardware (Fig. 5.3a, b). The extensor mechanism and skin are repaired, followed by a thumb spica splint for 6–8 weeks, until there is radiographic evidence of fusion.
One large diameter or two smaller diameter headless screws can be used in lieu of k-wire fixation, provided there is adequate bone stock. A dorsally applied 1.5–2.0 mm nonlocking/locking plate can be used in cases with bone loss or for revision surgery.
OA of the IP and MP joints can be treated with fusion.
Outcomes
Stanley et al. reviewed 42 cases of MP arthrodesis using a chevron arthrodesis. Most of the cases were for inflammatory arthritis with an 83 % patient satisfaction rate. Seven patients had continued pain or instability [19]. Schmidt et al. used a cup and cone technique, using a 3.0 mm cannulated AO screw and threaded washer in 26 patients. The indications included instability (12), osteoarthritis (6), inflammatory arthritis (7) and paralytic boutonniere (1). Twenty-five of 26 joints went on to fusion at an average time of 10 weeks. There were no infections and no need for hardware removal [20]. Bicknell, MacDermid and Roth performed a retrospective review of an interesting method of MP fusion used by Roth. This consisted of bone excision creating two flat surfaces, followed by the use of a single 0.062 in. k-wire inserted in a retrograde manner across the IP and MP joints with the MP in 10° of flexion and neutral deviation. The average age of the 28 patients was 49 ± 17 years. The indications included instability (9), inflammatory arthritis (18), OA (5), trauma (5) and skeletal dysplasia (1). The patients were casted for 4 weeks and splinted until there was radiographic union, followed by pin removal at an average of 78 ± 32 days. Older patients took longer to unite, 209 days in one case! Although the mean DASH score was 28 ± 24, dexterity, hand function and pinch was not significantly different from the opposite side and patient satisfaction was high. There were three complications consisting of pin loosening (1) and superficial infection (2). Twenty-five patients (89 %) were able to return to their previous occupations. There were no radiographic malunions or nonunions [21].
Treatment: Trapeziometacarpal Joint
Non-operative
Similar to other joints, the radiographic severity of osteoarthritic changes at the trapeziometacarpal joint does not correlate with the severity of clinical symptoms. The main thrust of treatment is pain management. A trial of activity modification and splinting should in general be undertaken in any patient prior to any surgical consideration. This involves avoidance of any repetitive pinching or grasping activities and the use of assistive devices as needed. Therapy may be useful for retaining range motion and augmenting thumb stability, whereas strengthening exercises are generally avoided while the patient has pain. NSAIDs are commonly used in addition to a limited number of selected cortisone injections in the trapeziometacarpal joint for flare-ups or persistent pain that is unresponsive to conservative measures. Hyaluronic acid injections are still investigational, but do not appear to be superior to steroid injections. The use of splints can provide pain relief and help enforce activity modification. In general a forearm based thumb spica splint, with the thumb held in palmar abduction, can be used on a full-time basis until the pain has been controlled and then intermittently as needed. Whether the IP joint is immobilized is largely dependent upon patient and surgeon preference. A palmar based thumb spica splint which immobilizes the trapeziometacarpal joint by abducting the thumb, can provide pain relief but may be more functional.
Surgical
There are a myriad of techniques for the open treatment of trapeziometacarpal osteoarthritis. There has been a step wise evolution in these procedures over time, which has created a bewildering number of surgical choices. It is therefore instructive to discuss these options in light of the stage of the disease. In the early stages, the treatment options have included a volar ligament reconstruction without bony resection or an extension osteotomy of the thumb metacarpal. A variety of less invasive arthroscopic resection techniques have recently emerged. In more advanced stages, various authors have advocated for a partial or complete trapezium excision with or without ligament reconstruction and with or without either tendon or an artificial interposition substance. Joint resurfacing arthroplasty or total joint replacement will not be specifically discussed, due to the paucity of long-term clinical data.
Stage I – II Disease
Volar Ligament Reconstruction
This procedure is mostly indicated in patients with painful symptomatic laxity of the trapeziometacarpal joint, or stage I disease. The joint surfaces are typically normal, but there may be trapeziometacarpal synovitis. An incision is made along the radial border of the thumb metacarpal, curving proximally to the radial border of the FCR tendon preserving any sensory nerve branches. The thenar muscles are elevated from the metacarpal, along with an exposure of the TM and STT joints. A volar to dorsal drill hole of progressively larger diameters is created using a cannulated 3.0 mm drill guide across the metacarpal base, parallel to the TM joint and perpendicular to the metacarpal long axis. The TM joint is reduced and temporarily pinned in abduction with a 0.045-in. K wire. The FCR tendon is identified in the proximal extent of the incision. A number of small transverse incisions are made proximally along the course of the tendon up to its musculotendinous junction. The tendon is then split in to a radial and ulnar half at the wrist incision. The tendon is split into two halves at the wrist and a 26 gauge wire loop is used to split the tendon proximally by grasping the loop with a needle holder and then pulling the wire proximally through each transverse incision. Since the FCR tendon rotates 180° as it courses distally, the ulnar half of the FCR is released at the musculotendinous junction since it lies radially at the wrist incision. The volar portion of the transverse carpal ligament is split and the superficial communicating branch of the radial artery is either retracted or ligated and divided. If there is an associated carpal tunnel syndrome, a carpal canal can be decompressed by dividing the dorsal leaf of the transverse carpal ligament which is also the floor of the FCR sheath. The FCR graft is then pulled in to the TM incision, while preserving its attachment onto the base of the index metacarpal. A suture retriever is used to pass the free end of the FCR graft through the drill hole from volar to dorsal, where it is sutured to the periosteum with a 3-0 non-absorbable suture. The remaining end of the graft is passed through the abductor pollicis longus tendon insertion and across the volar capsule and sutured at both places. The tendon graft is then looped around the remaining FCR tendon and sutured to itself. The thenar muscles are repaired and the K-wire is removed. The thumb is immobilized in a spica splint, or cast for 3 weeks followed by mobilization and strengthening.
Stage I TM OA can be treated with a volar ligament reconstruction or a metacarpal extension osteotomy.
Outcomes
Eaton et al. had one of the largest long-term series, reviewing 50 patients with an average follow-up of 7 years. Intractable pain was the primary indication for surgery. Ninety-five percent of the patients with stage I or II disease achieved good or excellent pain relief. All stage I cases and 82 % of stage II cases showed no x-ray evidence of osteoarthritis up to 13 years postoperatively. Only 74 % of patients with stage III and IV disease achieved good or excellent results [22]. Lane and Henley included some of these patients in their review of 37 operations in 35 patients with an average follow-up of 5.2 years (range 1–17 years). Sixty-seven percent had excellent results and 30 % had good results, with almost universal partial or complete pain relief. All patients had a stable trapeziometacarpal joint and an improvement in pinch strength. There was no clinical or x-ray evidence of osteoarthritis in any patient at the final follow-up [23].
Thumb Metacarpal Extension Osteotomy
Pellegrini et al. demonstrated in a biomechanical study that the volar contact area of the trapeziometacarpal joint was unloaded and shifted more dorsally, as long as the location of the OA did not extend more dorsal than the midpoint of the trapezium, which provides the rationale for this procedure [24]. It is indicated in symptomatic Eaton stage I and II disease, for both pain relief and to restore thumb stability. A 3 cm dorsal incision is made from the base of the thumb metacarpal, moving distally. Sensory nerve branches are protected and retracted. A subperiosteal dissection is performed and a dorsally based 30° wedge of bone is resected 1 cm distal to the metacarpal base. The wedge of bone is removed and the distal metacarpal is extended to close the wedge, and then the osteotomy is held in place with k- wires, staples or a plate.
Outcomes
There are no large series on this procedure. Tomaino prospectively evaluated 12 patients who were treated with an extension osteotomy, with an average follow-up of 2.1 years (range: 6–46 months). Eleven patients were satisfied with the outcome and the grip and pinch strength increased by an average of 8.5 and 3 kg, respectively. Parker reviewed Amadio’s experience with 8 patients who were treated with this procedure, with stage I (3 patients), stage II (3 patients) and stage III (2 patients) TM osteoarthritis at a mean follow-up of 9 years (range, 6–13 years). The average lateral pinch strength was 5 kg or 129 %, oppositional pinch strength 3 kg or 103 % and grip strength 19 kg or 108 % of the opposite side. There was no radiographic progression of the arthritis in 5 of the 8 patients. Gwynne–Jones and colleagues reviewed the results of thumb extension osteotomies without internal fixation in 28 patients with a mean age 54 years (range, 30–69 years). At a mean follow-up of 34 months (range, 12–73 months), 21 patients with 22 procedures had good or excellent results, 2 had fair and one had a poor result. Three patients required further surgery for persistent pain. Key pinch, pulp pinch and tripod pinch were 22–32 % lower, but there was no decrease in grip strength. The Michigan Hand Outcomes Questionnaire scores increased by an average of 28 points (range, 1–56) points, with a significant improvement in pain (44 points), activities of daily living (41 points) and satisfaction (35 points) [25].
Stage II – IV Disease
Ligament Reconstruction Interposition Arthroplasty (LRTI)
This procedure, described by Burton and Pellegrini in 1986, is typically used for more advanced stage II – IV disease (Fig. 5.4a–h) [26]. An 8 cm dorsoradial incision is made along the radial border of the thumb metacarpal, curving down to the FCR tendon at the wrist. Branches of the superficial radial nerve and radial artery are identified and protected throughout the procedure. A longitudinal incision is made through the TM joint capsule. An oscillating saw is used to remove the base of the thumb metacarpal and the medullary canal is enlarged with a curette. A trapeziectomy is then performed by inserting a 0.62 in. K-wire to act as a joy stick, by sequentially elevating soft tissue restraints until the trapezium can be removed in one piece. Alternatively, the trapezium can be osteotomized into four sections and removed piecemeal, while taking care to avoid injury to the FCR tendon which is in the volar depths of the wound. Caution is needed to prevent injury to the radial artery in the snuffbox, which is just proximal to the STT joint. A 6 mm bony window is made with a power burr along the dorsal aspect of the thumb metacarpal, 1 cm distal to the base.
LRTI. (a) Clinical appearance of advanced TM OA with contracted 1st web space. (b) AP x-ray view revealing obliteration of the joint space at the TM and STT joints (Eaton stage IV). (c) Harvesting of FCR tendon which is left attached to the index metacarpal base. (d) Creation of a tendon anchovie after suspensionplasty with the FCR strip. (e) immediate postoperative AP x-ray. (f) Maintenance of arthroplasty space at the 1 year follow. (g) Improved thumb abduction at I year. (h) preserved thumb opposition at 1 year (Published with the permission of David J Slutsky MD)
One half of the FCR tendon is harvested and pulled into the thumb incision as described above. Some authors prefer to use the entire FCR, without any apparent deleterious effects. The free end of the tendon slip is passed into the medullary canal of the thumb metacarpal and out the dorsal cortical window, where it is sutured to the periosteum. It is then looped around the metacarpal base and sutured to itself, while longitudinal traction is applied until the metacarpal base is even with the index CMC joint. Proper tensioning of the FCR graft helps prevent proximal migration and radial subluxation of the thumb. A percutaneous 0.045 in. k-wire can be inserted through the metacarpal base and into the distal scaphoid with the thumb in abduction to maintain the arthroplasty space. Two 2-0 non-absorbable sutures are then placed in the deep volar capsular. One of the sutures is left attached to the deep capsule and threaded through the distal end of the FCR tendon slip to create an anchovy interposition, which is then tied down to the capsule. The remaining deep suture is used to repair the capsule over the anchovy, in a vest over pants fashion. In the original surgical description, the extensor pollicis brevis is released from its insertion and tenodesed to the metacarpal shaft proximal to the metacarpophalangeal joint, to eliminate the hyperextension moment acting on the proximal phalanx. The subcutaneous tissue and skin are closed in layers and a thumb spica splint is applied. Post-operatively, a thumb spica splint is maintained until 4 weeks at which time the k-wire is removed and thumb abduction and extension exercises are instituted. Opposition is started at 6 weeks, followed by progressive strengthening exercises.
Variants of the LRTI have included the following: tendon interposition alone, ligament reconstruction alone, a partial or complete trapeziectomy with tendon interposition but no ligament reconstruction, a limited trapeziectomy with tendon interposition and volar ligament reconstruction, a trapezial resection suspensionplasty using the abductor pollicis longus tendon and a partial trapeziectomy with implantation of a synthetic biological implant. A double interposition resurfacing arthroplasty was described for stage IV disease and involves a TM joint and STT joint resection and interposition [27].
Stage II – IV TM OA can be treated with a variety of methods including implant arthroplasty, excisional arthroplasty with or without ligament reconstruction and with or without tendon interposition
Trapeziectomy
This procedure is used in stage III and IV disease. A simple trapeziectomy has been complicated by metacarpal subsidence, which can theoretically weaken the pinch strength and, in extreme cases, lead to metacarpal scaphoid impingement (Fig. 5.5). This procedure has largely been supplanted by a haematoma distraction arthroplasty, which consists of a trapeziectomy and temporary distraction pinning of the thumb metacarpal. This procedure relies on the development of a stable pseudarthrosis, that develops from the ingrowth of fibrous tissue which replaces the initial hematoma. The trapeziectomy is performed as described above. The thumb is then grasped and held in a position of wide palmar abduction, slight opposition, distraction and one or two 0.062 in. percutaneous K-wires are inserted from the base of the thumb metacarpal in a transverse orientation into the base of the index metacarpal or the trapezoid. Pinning the thumb metacarpal base to the index for 5–6 weeks is integral to the procedure, but tendon interposition or reconstruction of the TM joint capsule is not.
Outcomes
Froimson described the use of a rolled up tendon anchovy for an interposition arthroplasty in 1970 [28]. Although he reported pain relief in 80 procedures and 72 patients, the long-term follow-up showed a 30 % reduction in pinch strength, in addition to a 50 % decrease in the arthroplasty space. Eaton and Littler introduced the concept of a beak ligament reconstruction in 1973 [5]. Although they removed any osteophytes, no trapeziectomy was performed. They reported that all the patients with stage II disease and 63 % with stage III disease had excellent results at 1 year. They subsequently modified their procedure by adding a resection of the second metacarpal base and distal trapezium with 92 % good or excellent results reported in 1985 [29]. In 1986 Burton and Pellegrini published their technique of a ligament reconstruction interposition arthroplasty (LRTI) [26]. They used 1/2 of the FCR tendon to reconstruct the volar oblique ligament combined with a partial or complete trapeziectomy and interposition of the remaining tendon as an anchovy. In a retrospective series of 25 thumbs, treated with an LRTI and hemitrapeziectomy (stage II and III), or complete trapeziectomy (stage IV, pantrapezial disease) at an average follow-up of 2 years, 92 % of the patients had excellent pain relief and an average increase in pinch and grip strength of 19 %.
De Smet et al. compared the outcomes of 22 patients who underwent a trapeziectomy and 34 patients were treated with an LRTI at a follow-up of 26–34 months. They found that the trapezial arthroplasty space was better maintained in the LRTI group with a loss of height of 32 % (compared to the preoperative level) as compared to a 57.5 % decrease in height in the trapeziectomy group. Despite this finding there were no statistically significant differences for pain relief, patient satisfaction, DASH score or grip strengths, but the key-pinch strength was correlated with the amount of metacarpal subsidence.
Mahoney and Meals believed that the poor results following a simple trapeziectomy reported by Gervis in 1949 [30] could be improved by adding k-wire immobilization of the thumb in a distracted position for 5–6 weeks, to allow the post-operative hematoma to organize and the surrounding capsular remnants to consolidate to sufficiently anchor the metacarpal base. They reported their results with this procedure in 26 patients, with a minimum 2 year follow-up. Ninety-two percent of the patients were pain free and the majority recovered normal thumb motion. They noted a 47 % improvement in grip and a 33 % increase in key pinch and 23 % improvement in tip pinch over the preoperative values. They did note, however, that there was more metacarpal subsidence as compared to a more formal ligament reconstruction, but this did not correlate with outcomes.
Davis et al. performed a prospective, randomized, controlled study on 183 patients with trapeziometacarpal osteoarthritis. They were randomized to either a simple trapeziectomy, trapeziectomy with palmaris longus interposition, or trapeziectomy with ligament reconstruction and tendon interposition using one half of the FCR tendon. K-wire fixation was used for 4 weeks in all patients [31]. At the 1-year follow-up, 82 % achieved good pain relief and good range of motion. This result was independent of the type of procedure that was performed. They concluded that the outcomes of these three variations of trapeziectomy were very similar at 1 year and that there appeared to be no benefit to tendon interposition or ligament reconstruction in the short term.
Wajon et al. performed a meta-analysis of the Cochrane database of seven studies, with 384 patients having Stage II or III disease who had undergone a trapeziectomy, trapeziectomy with interpositional arthroplasty, trapeziectomy with ligament reconstruction, trapeziectomy with ligament reconstruction and tendon interposition (LRTI) and joint replacement. No procedure demonstrated any superiority over another in terms of pain, function, range of motion or strength. However, participants who underwent trapeziectomy had 16 % fewer adverse effects (p = 0 < .001) [32].
Associated MP Joint Hyperextension
MP joint hyperextension often accompanies advanced trapeziometacarpal osteoarthritis, which produces a dorsal subluxation stress at the TM joint arthroplasty site and may lead to recurrent subluxation. Correction of this MP hyperextension reverses the metacarpal collapse and improves the force transmission along the thumb ray. If there is MP joint OA, an MP joint fusion is indicated. In cases where there is a mild MCP joint hyperextension (20–30°), Eaton has recommended transferring the EPB to the base of the thumb metacarpal, which eliminates the extension force on the MP joint and augments abduction of the thumb metacarpal [33]. The joint is pinned or casted in flexion for 4 weeks postoperatively. For MP joint hyperextension of 30° or more, an MP joint volar capsulodesis or a sesamoidesis is added. In their series of MP capsulodesis of 13 patients with an average follow-up of 39 months, 10 patients had complete correction of the MP hyperextension deformity, with 9 excellent results, 3 good results, and 1 fair result.
MP joint hyperextension > 30° with TM OA should be treated with a capsulodesis or fusion.
Trapeziometacarpal Fusion
Trapeziometacarpal fusion has been advocated for patients with stage II and III disease with strong functional demands, such as manual laborers and patients younger than 40 years with post-traumatic osteoarthritis, since it provides a stable thumb ray with no risk of instability. The TM joint is exposed and the joint surfaces are denuded of cartilage and subchondral bone to create two parallel surfaces. The thumb is positioned in 35–45° of palmar abduction and 20–30° of radial abduction and pronation, so that the thumb pulp rests on the radial aspect of the index finger middle phalanx in mild opposition. K-wire, staple or plate fixation can be used. In cases of revision or if there is bone loss with a small trapezial remnant, a minicondylar blade plate is ideal. A short arm thumb spica cast is used for 6 weeks, followed by a splint, until there are signs of fusion.
Outcomes
Rizzo and co-workers examined the Mayo clinic experience of TM fusion for OA in 114 patients/126 thumbs at an average follow up of 11.2 years (range 3–28 years). The average patient age was 57 years (range 32–77). Supplemental bone graft was used in 90 thumbs. There were 17 nonunions, 9 of them requiring re-operation. The appositional pinch increased to 5.9 kg vs. 3.0 kg preoperatively, oppositional pinch 5.4 kg vs. 2.7 kg and grip strengths 23 kg vs. 14 kg. The average pain score decreased to 0.4 vs. 6.6 preoperatively (p < .01). Thirty-nine patients developed radiographic signs of STT OA, but only 8 patients were symptomatic. MP joint OA occurred in 16 patients, but no additional treatment was needed [34].
There are many published case series that examined the results of these disparate procedures. Taylor et al. performed a retrospective study of 83 patients with trapeziometacarpal joint osteoarthritis who were treated with a TM fusion (36), trapeziectomy with and without ligament reconstruction (25) or a Silastic replacement (22) [35]. The follow-up ranged from 1 to 5 years. There was a higher rate of complications and reoperation in the fusion group, but otherwise no significant differences in terms of patient satisfaction, range of movement, tip and key pinch.
Raven et al. reviewed 54 patients (74 thumbs) with TM OA who were treated with a trapeziectomy (18 thumbs), trapeziectomy with tendon interposition (17 thumbs) or trapeziometacarpal arthrodesis (28 thumbs). The average follow-up was 13 years for the resection group, 8 years for the trapeziectomy group and 9 years for the arthrodesis group. Patients in the trapeziectomy group had significantly less pain and better radial abduction as compared to the arthrodesis group. There was no difference among the three groups in grip and tip pinch strength. None of the patients in the trapeziectomy group needed a re-operation, one patient in the resection arthroplasty group had a re-operation and 22 patients in the arthrodesis group had one or more re-operations for hardware removal or because of a complication [36].
Arthroscopic Treatment
The good results that have been obtained with an open trapeziectomy provided the impetus for the development of arthroscopic techniques. Arthroscopic techniques for evaluating and treating trapeziometacarpal disease surfaced in 1994 [37, 38]. As a general rule, any patient who is an appropriate candidate for a hemiresection arthroplasty of the TM joint is also suitable for an arthroscopic hemi-trapeziectomy. This would typically include patients in Eaton stage II and stage III who have unremitting pain, despite appropriate conservative measures. This form of treatment does not preclude an open trapeziectomy and/or ligament reconstruction at a later date as a salvage procedure for failed arthroscopic surgery. The presence of Eaton Stage IV disease is a relative contraindication, although an arthroscopic hemitrapeziectomy, combined with an arthroscopic debridement or limited resection of the distal scaphoid, is an option. Badia proposed an arthroscopic classification of TM OA that is based upon the arthroscopic changes [39]. Stage I included intact articular cartilage, Stage II included eburnation on the ulnar 1/3 of the metacarpal base and central trapezium and Stage III comprised widespread full thickness cartilage loss on both surfaces. Based upon the intraoperative findings he recommended debridement for stage I, with thermal capsulorraphy in the presence of dorsal subluxation, extension/abduction osteotomy of the metacarpal base ± thermal shrinkage for stage II and an arthroscopic interposition arthroplasty for Stage III. He recommended an open arthroplasty in the presence of associated severe STT joint OA.
A 1.9 mm 30° angled scope, along with a camera attachment is used. A larger 2.7 mm scope may be substituted after the space has been partially decompressed. A 3 mm hook probe is needed for palpation of intracarpal structures. The use of an overhead traction tower greatly facilitates instrumentation. A motorized shaver is needed for debridement. Some type of diathermy unit is required if a capsular shrinkage is contemplated. Intraoperative fluoroscopy is employed to assess the adequacy of bone resection and for locating the portals as needed. The patient is positioned supine on the operating table with the arm extended on a hand table. The thumb is suspended by Chinese finger traps with 5 lb of counter traction, which forces the wrist into ulnar deviation. The relevant landmarks are outlined, including the proximal and dorsal edge of the thumb metacarpal base, the tendons of the abductor pollicus longus (APL) and the extensor pollicus longus (EPL) and the radial artery in the snuff box. The procedure is performed with a tourniquet elevated to 250 mmHg. Saline inflow irrigation is provided through the arthroscope and a small joint pump or pressure bag. To establish the 1-R portal, the thumb metacarpal base is palpated and the joint is identified with a 22 gauge needle just radial to the APL, followed by injection of 1–2 cc of saline. A small skin incision is made, followed by wound spread technique with tenotomy scissors. The capsule is pierced and a cannula and blunt trocar are inserted, followed by insertion of the arthroscope. An identical procedure is used to establish the 1-U portal, just ulnar to the EPB tendon, followed by insertion of a 3 mm hook probe. The portals are used interchangeably to systematically inspect the joint, which is facilitated by expedient use of a 2.0 mm synovial resector.
Access to the medial trapezial osteophytes may sometimes be difficult, hence I have found the use of a distal – dorsal (D-2) accessory portal to be of some value [40]. Its main utility is that it allows one to look down on the trapezium rather than across it, which facilitates resection of any medial osteophytes (Fig. 5.6a–c). This accessory portal allows views of the dorsal capsule with rotation of the scope and facilitates triangulation of the instrumentation. It is situated in the dorsal aspect of the 1st web space. An anatomical study of 5 cadaver hands revealed that the D-2 portal surface landmark is ulnar to the EPL tendon and 1 cm distal to V-shaped cleft at the juncture of the index and thumb metacarpal bases. The portal lies just distal to the dorsal intermetacarpal ligament (DIML). To establish the D-2 portal, the intersection of the base of the index and thumb metacarpal are identified just distal and ulnar to the extensor pollicus longus (EPL) tendon. The course of the radial artery can be outlined by palpation or doppler prior elevation of the tourniquet. A 22 gauge needle is inserted 1 cm distal to this juncture and angled in a proximal, radial and palmar direction, hugging the thumb metacarpal. A small skin incision is made and tenotomy scissors are used to spread the soft tissue and pierce the joint capsule. This is followed by insertion of a blunt trocar and cannula and then the arthroscope, or alternatively a hook probe, motorized shaver or 2.9 mm burr.
(a) Surface landmarks for TM and STT portals. APL abductor pollicus longus, EPB extensor pollicus brevis, EPL extensor pollicus longus, RA radial artery (b) Direction scope in 1-R portal with needle placement for the D-2 portal (c) Fluoroscopic view of scope and needle (Published with the permission of David J Slutsky MD)
Arthroscopic hemi-trapeziectomy is an option in Stage II and III TM OA
Arthroscopic Debridement and Capsular Shrinkage Interposition
The essence of arthroscopic capsular shrinkage is akin to that of an anterior oblique ligament reconstruction. It relies on thermal heating of the collagenous fibers in the surrounding ligaments and capsule, followed by a period of joint immobilization in a reduced position. A motorized shaver is used to debride any synovitis and to expose the capsular ligaments. A diathermy probe is then employed to paint the anterior oblique ligament and surrounding capsule, taking care to leave bands of tissue in between. The probe is kept away from the joint surfaces to prevent cartilage necrosis. In light of the meager joint volume, the outflow fluid temperature is frequently monitored to prevent overheating. Use of an 18 gauge needle as an accessory portal enhances fluid circulation, which minimizes this risk.
Arthroscopic Partial or Complete Trapeziectomy Without Tendon Interposition
The 1-R and 1-U portals are established as described. The anterior oblique ligament (AOL) is identified and preserved. After joint debridement a 2.9 mm burr is applied in a to and fro manner to resect the distal trapezium (Fig. 5.7a–c). The diameter of the burr, along with fluoroscopy, provide a gauge as to the amount of bony resection. A larger burr may be substituted, as the space between the metacarpal base and distal trapezium enlarges. It is crucial to remove any medial osteophytes, which will lead to impingement and possibly persistent pain. The D-2 portal is useful for this step since it allows one to debride the medial trapezium from above rather than from across the joint. Culp has recommended resecting at least 1/2 of the distal trapezium [41], although I have found that excising 3–4 mm is sufficient, provided that all of the medial osteophytes are removed. After the bony resection is complete, the thumb is k-wired in a pronated and abducted position (Fig. 5.8a–e). If there is lateral subluxation of the metacarpal base, thermal shrinkage of the anterior oblique ligament can be performed at this time. The thumb is immobilized in abduction by cast or splint for 4 weeks, at which time the k-wire is removed. In more recent years, I have abandoned k-wire immobilization and thermal shrinkage and start protected home motion exercises as pain permits at 1–2 weeks, without any deterioration in the outcomes. Thumb abduction and extension exercises are instituted, followed by adduction and opposition after 6 weeks. Strengthening ensues once motion has been restored. The rehabilitation protocol is modified as necessary if concomitant surgery on the MP joint has been performed.
(a) View of the distal trapezium from the 1-R portal. Probe is in the 1-U portal. AOLs superficial anterior oblique ligament. (b) 2.9 mm burr in the 1-U portal as seen from the 1-R portal. (c) Scope placement to check resection of medial osteophytes (Published with the permission of David J Slutsky MD)
(a) Fifty-five years of male with left TM OA. Note the large medial osteophyte arising from the trapezium. (b) Arthroscopic TM arthroplasty. Arthroscope is in the D-2 portal, burr is in the 1-R portal. (c) X-ray after partial trapeziectomy. (d) X-ray at 2 ½ years postoperative. (e) Clinical appearance (Published with the permission of David J Slutsky MD)
Arthroscopic Partial or Complete Trapeziectomy with Interposition
After a partial or complete resection of the trapezium, autogenous tendon graft such as the palmaris longus, 1/2 of the flexor carpi radialis or a slip of the APL is harvested through multiple transverse incisions. Alternatively, some form of synthetic interposition material can be substituted. An absorbable suture is placed in the leading end of the tendon graft and swedged onto a large curved needle, which is used to pass the graft through the joint. The needle is passed through the 1-U portal and brought out through the volar capsule and bulk of the thenar eminence. Traction on the suture pulls the graft into the joint. The remaining graft is packed in with forceps and the portals are closed. The thumb is k-wired in abduction for 4 weeks.
Outcomes
Menon reported his results on performing a partial arthroscopic resection of the trapezium and an interposition arthroplasty in 31 patients (33 hands) [37]. The mean age was 59 years (48–81 years) with an average follow up of 37.6 months (24–48 months). Gortex was used in 19 patients and autogenous tendon or allograft in 14. Complete pain relief was obtained in 25 patients/hands (75.7 %). Three patients had mild pain (4 hands) and 4 patients had persistent pain that required conversion to an open trapeziectomy and ligament reconstruction. All patients maintained their pre-operative motion. Pinch strength improved from 6 p.s.i. preoperatively to 11.1 p.s.i. postoperatively. Because of osteolysis in 3 patients/4 hands, the use of Gortex as an interpositional substance was not recommended.
Hofmeister et al. reviewed the long term results in 18 patients following an arthroscopic hemitrapeziectomy, thermal capsular shrinkage and temporary K-wire fixation. At an average follow-up of 7.6-years they noted a subjective improvement in pain, pinch activities, strength and range of motion in all patients. No patient required further surgery on their thumb. No patient had a first carpal-metacarpal grind or laxity by exam. The total thumb range of motion decreased by 20 %, but all patients could oppose to the fifth finger. Grip strength remained unchanged, key pinch improved from 8 to 11 lbs., and tip pinch improved from 4 to 5 lbs. Radiographs showed a metacarpal subsidence of 1.8 mm (0–4 mm). Four complications were noted: two cases of dorsal radial nerve neuritis, one rupture of the flexor pollicis longus and one prolonged hematoma [42].
Edwards and Ramsey reported similar findings. They prospectively evaluated 23 patients with stage III OA at a minimum follow-up of 4 years, who were treated with pan arthroscopic hemitrapeziectomy and thermal capsular shrinkage, without interposition, plus k-wire fixation for 3–4 weeks. At 3 months postoperatively the average DASH score improved from 61 to 10 and pain scores decreased from 8.3 to 1.5. Grip and key pinch strength improved 6.8 and 1.9 kg respectively and the wrist and finger motion were unchanged. Proximal migration of the first metacarpal averaged 3 mm and translation decreased from 30 to 10 %. These findings remained unchanged at 4 years or more [43].
Pegoli et al. performed an arthroscopic hemitrapeziectomy and tendon interposition using the palmaris longus tendon in 16 patients with Stage I and II disease. At 12 months there were 6 excellent, 6 good, 3 fair and 1 poor result using the modified Mayo score [44]. Adams and Steinmann treated 17 patients with an arthroscopic debridement and interposition arthroplasty for stage II and III disease, using a folded acellular dermal matrix allograft. The average age was 61.7 (range 47–86) and the follow-up averaged 17 (range, 6–39) months. Eighty-eight per cent of the patients reported no pain, or only occasional pain, on activities with an average pain score of 1.125 out of 10. The average grip strength was 18.3 vs. 22.6 kg pre-operatively and the average pinch strength was 4.0 kg vs. 4.8 kg. Only two patients had limited range of motion, as assessed by the palm flat test and the ability to oppose the thumb to the 5th metacarpal head. None of the patients required revision surgery and there were no instances of graft reaction [45].
Complications
The incidence and nature of the complications that may occur following TM joint surgery vary, depending upon whether the procedure is open or arthroscopic, whether temporary k-wire fixation is used and whether or not there is an interposition substance. Possible complications that are common to all of the procedures include injury to branches of the superficial radial nerve, infection metacarpal subsidence and subluxation of the thumb metacarpal. The use of autogenous tendon carries the risk of neurovascular injury during harvest of the graft. The use of a synthetic implant carries the risk of a foreign body reaction which was seen with silastic trapezial implants, has also been reported following the use of Gortex, polyurethane urea and acellular dermal grafts. Wound healing is less of a problem with arthroscopic techniques vs. open procedures, but residual trapeziometacarpal impingement or inadequate bone resection is more of a risk.
Conclusion
From the above discussion it is apparent that osteoarthritis of the IP and MP joints are commonly treated with fusion rather than arthroplasty, with generally favorable outcomes. The profusion of procedures for the treatment of trapeziometacarpal OA is a testament to the fact that most procedures provide satisfactory pain relief and function, whether performed arthroscopically or open. The type of procedure is largely dependent upon the surgeon’s preference and the patient’s needs. Similar to the hunt for the perfect mousetrap, innovative surgeons will no doubt continue to search for the ideal procedure, even though the simplest methods often suffice.
References
Chaisson CE, Zhang Y, McAlindon TE, Hannan MT, Aliabadi P, Naimark A, Levy D, Felson DT. Radiographic hand osteoarthritis: incidence, patterns, and influence of pre-existing disease in a population based sample. J Rheumatol. 1997;24:1337–43.
Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14:953–7.
Xu L, Strauch RJ, Ateshian GA, Pawluk RJ, Mow VC, Rosenwasser MP. Topography of the osteoarthritic thumb carpometacarpal joint and its variations with regard to gender, age, site, and osteoarthritic stage. J Hand Surg Am. 1998;23:454–64.
Cooney 3rd WP, Chao EY. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 1977;59:27–36.
Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655–66.
Burton RI. Basal joint arthrosis of the thumb. Orthop Clin North Am. 1973;4:347–8.
Fontana L, Neel S, Claise JM, Ughetto S, Catilina P. Osteoarthritis of the thumb carpometacarpal joint in women and occupational risk factors: a case-control study. J Hand Surg Am. 2007;32:459–65.
Barron OA, Glickel SZ, Eaton RG. Basal joint arthritis of the thumb. J Am Acad Orthop Surg. 2000;8:314–23.
Bettinger PC, Linscheid RL, Berger RA, Cooney 3rd WP, An KN. An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint. J Hand Surg Am. 1999;24:786–98.
Wilgis EF. Distal interphalangeal joint silicone interpositional arthroplasty of the hand. Clin Orthop Relat Res. 1997;(342):38–41.
Cobb TK. Arthroscopic distal interphalangeal joint arthrodesis. Tech Hand Up Extrem Surg. 2008;12:266–9.
Sieber HP, Segmuller G. Arthrodesis of the interphalangeal joint of the thumb: indication, technic, results. Handchir Mikrochir Plast Chir. 1983;15:11–6.
Stern PJ, Fulton DB. Distal interphalangeal joint arthrodesis: an analysis of complications. J Hand Surg Am. 1992;17:1139–45.
Brannon EW, Klein G. Experiences with a finger-joint prosthesis. J Bone Joint Surg Am. 1959;41-A:87–102.
Swanson AB, Herndon JH. Flexible (silicone) implant arthroplasty of the metacarpophalangeal joint of the thumb. J Bone Joint Surg Am. 1977;59:362–8.
Figgie MP, Inglis AE, Sobel M, Bohn WW, Fisher DA. Metacarpal-phalangeal joint arthroplasty of the rheumatoid thumb. J Hand Surg Am. 1990;15:210–6.
Beckenbaugh RBSA. Total joint arthroplasty for the metacarpophalangeal joint of the thumb -a preliminary report. J Bone Joint Surg Am. 1981;4:295–7.
Inglis AE, Hamlin C, Sengelmann RP, Straub LR. Reconstruction of the metacarpophalangeal joint of the thumb in rheumatoid arthritis. J Bone Joint Surg Am. 1972;54:704–12.
Stanley JK, Smith EJ, Muirhead AG. Arthrodesis of the metacarpo-phalangeal joint of the thumb: a review of 42 cases. J Hand Surg Br. 1989;14:291–3.
Schmidt CC, Zimmer SM, Boles SD. Arthrodesis of the thumb metacarpophalangeal joint using a cannulated screw and threaded washer. J Hand Surg Am. 2004;29:1044–50.
Bicknell RT, MacDermid J, Roth JH. Assessment of thumb metacarpophalangeal joint arthrodesis using a single longitudinal K-wire. J Hand Surg Am. 2007;32:677–84.
Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9:692–9.
Lane LB, Henley DH. Ligament reconstruction of the painful, unstable, nonarthritic thumb carpometacarpal joint. J Hand Surg Am. 2001;26:686–91.
Pellegrini Jr VD, Parentis M, Judkins A, Olmstead J, Olcott C. Extension metacarpal osteotomy in the treatment of trapeziometacarpal osteoarthritis: a biomechanical study. J Hand Surg Am. 1996;21:16–23.
Gwynne-Jones DP, Penny ID, Sewell SA, Hughes TH. Basal thumb metacarpal osteotomy for trapeziometacarpal osteoarthritis. J Orthop Surg (Hong Kong). 2006;14:58–63.
Burton RI, Pellegrini Jr VD. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324–32.
Barron OA, Eaton RG. Save the trapezium: double interposition arthroplasty for the treatment of stage IV disease of the basal joint. J Hand Surg Am. 1998;23:196–204.
Froimson AI. Tendon arthroplasty of the trapeziometacarpal joint. Clin Orthop Relat Res. 1970;70:191–9.
Eaton RG, Glickel SZ, Littler JW. Tendon interposition arthroplasty for degenerative arthritis of the trapeziometacarpal joint of the thumb. J Hand Surg Am. 1985;10:645–54.
Gervis WH. Excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint. J Bone Joint Surg Br. 1949;31B:537–9, illust.
Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069–77.
Wajon A, Ada L, Edmunds I. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2005;(4):CD004631.
Eaton RG, Floyd 3rd WE. Thumb metacarpophalangeal capsulodesis: an adjunct procedure to basal joint arthroplasty for collapse deformity of the first ray. J Hand Surg Am. 1988;13:449–53.
Rizzo M, Moran SL, Shin AY. Long-term outcomes of trapeziometacarpal arthrodesis in the management of trapeziometacarpal arthritis. J Hand Surg Am. 2009;34:20–6.
Taylor EJ, Desari K, D’Arcy JC, Bonnici AV. A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg Br. 2005;30:45–9.
Raven EE, Kerkhoffs GM, Rutten S, Marsman AJ, Marti RK, Albers GH. Long term results of surgical intervention for osteoarthritis of the trapeziometacarpal joint: comparison of resection arthroplasty, trapeziectomy with tendon interposition and trapezio-metacarpal arthrodesis. Int Orthop. 2007;31:547–54.
Menon J. Arthroscopic management of trapeziometacarpal joint arthritis of the thumb. Arthroscopy. 1996;12:581–7.
Menon J. Arthroscopic evaluation of the first carpometacarpal joint. J Hand Surg Am. 1998;23:757.
Badia A. Trapeziometacarpal arthroscopy: a classification and treatment algorithm. Hand Clin. 2006;22:153–63.
Slutsky DJ. The use of a dorsal-distal portal in trapeziometacarpal arthroscopy. Arthroscopy. 2007;23:1244 e1241–1244.
Culp RW, Rekant MS. The role of arthroscopy in evaluating and treating trapeziometacarpal disease. Hand Clin. 2001;17:315–9, x–xi.
Hofmeister EP, Leak RS, Culp RW, Osterman AL. Arthroscopic hemitrapeziectomy for first carpometacarpal arthritis: results at 7-year follow-up. Hand (N Y). 2009;4:24–8.
Edwards SG, Ramsey PN. Prospective outcomes of stage III thumb carpometacarpal arthritis treated with arthroscopic hemitrapeziectomy and thermal capsular modification without interposition. J Hand Surg Am. 2010;35:566–71.
Pegoli L, Parolo C, Ogawa T, Toh S, Pajardi G. Arthroscopic evaluation and treatment by tendon interpositional arthroplasty of first carpometacarpal joint arthritis. Hand Surg. 2007;12:35–9.
Adams JE, Merten SM, Steinmann SP. Arthroscopic interposition arthroplasty of the first carpometacarpal joint. J Hand Surg Eur Vol. 2007;32:268–74.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag London
About this chapter
Cite this chapter
Slutsky, D.J. (2015). Osteoarthritis of the Thumb. In: Trail, I., Fleming, A. (eds) Disorders of the Hand. Springer, London. https://doi.org/10.1007/978-1-4471-6557-6_5
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6557-6_5
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6556-9
Online ISBN: 978-1-4471-6557-6
eBook Packages: MedicineMedicine (R0)