Abstract
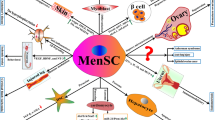
Stem cells can be opportunely used to modulate inflammation, abrogate cell death, and preserve tissue function. Today, stem cells are being extensively studied for the treatment of diverse diseases, including central nervous system disorders, although mostly in the laboratory and in limited clinical trials. Cerebrovascular diseases are the third leading cause of death and the primary cause of long-term disability in the United States. The only approved therapy for stroke is tPA, but its widespread application severely diminished by the short therapeutic window and hemorrhagic complications, therefore excluding most patients from its benefits. Parkinson’s and Huntington’s disease are the other two most studied basal ganglia diseases and, as stroke, are plagued with limited treatment options. Inflammation is a key feature in central nervous system disorders and it plays a dual role, either improving injury in early phases or impairing neural survival at later stages. In this chapter, the role of stem cells as restorative treatments for stroke and other basal ganglia disorders is discussed. The recently investigated menstrual blood stem cells are specially emphasized, and their present and future experimental and clinical applications are explored.
Disclosures
CVB and PRS serve as consultants, and PRS is a cofounder of Saneron-CCEL Therapeutics, Inc., and CVB, PRS, and JGA have a patent application in this area, owned jointly by Cryo-Cell International, Inc. and Saneron-CCEL Therapeutics, Inc. Cryo-Cell International, Inc. provided the foundational menstrual stem cell technology in the patent applications of M.A. Walton and JGA wholly owned by Cryo-Cell International, Inc.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Cell-based therapy has evolved over the years as a robust experimental treatment for regenerative medicine, but the extension of its potential entry into clinical application is still being explored. Bone marrow transplantation is one of the first and most frequently studied applications of stem cells, and replacement of diseased bone marrow by healthy cells has improved survival of thousands of patients. Following the knowledge provided by hematopoietic stem cell transplantation, other cell sources have been investigated, including embryonic, fetal, and adult tissues. In addition, different applications for stem cell therapy have been studied, not only aiming replacement but also targeting inflammation and tissue repair.
Several diseases are marked by inflammatory responses, either as etiopathogenic events or as a consequence of disease progression. In stroke, for instance, the inflammatory reaction that follows ischemia may increase the injured area to limits beyond those caused by the ischemic insult itself, providing an opportunity to a much far-ranging therapeutic application of stem cells. These cells have the ability to modulate the immune system, establishing a less inflammatory environment, increasing immunological tolerance, and decreasing cell death. To date, studies have investigated umbilical cord blood cells, neural cells, mesenchymal cells from diverse tissues, and adult hematopoietic stem cells as sources for the treatment of stroke, all reporting success to some extent. However, most investigations are restricted to animal studies, as clinical translation is sometimes difficult. Less invasive forms of cell administration, use of cells that are better tolerated by the host immune system, and availability in easily accessible tissues are priorities to most recent research. Moreover, the use of adult stem cells as primary donor source for cell therapy has become a topic of contention in both the scientific field and the public community because of safety and ethical concerns that hinder clinical applications of cells from embryonic and fetal origins.
Knowledge about the mechanisms of action of the cells on the injured site has changed over the years, contributing to advances in their application. Firstly, cell differentiation may not be necessary to promote repair. This observation implies that cells derived from adult tissues, which do not usually differentiate as easily as the pluripotential cells from more immature tissues, may be used. Second, regeneration may occur without cell migration to the site of injury. This finding implies the utility of intravenous applications of the cells, instead of the more invasive local injections. As an extension to this idea is the notion that cell therapy for central nervous system disorders may proceed without the need for mechanically disrupting the brain (i.e., neurosurgical manipulations), since cells no further need to cross the blood-brain barrier to reach their therapeutic target.
Today, it is established that stem cells may be derived from numerous tissues, with some variability in their therapeutic potentials. In this context, menstrual cells may be a precious finding, because they derive from a disposable tissue, are readily available, and share common properties with less mature cell types, such as high differentiation potentiality and little immunogenicity. A major advantage of menstrual cells is their application for autologous transplantation which should circumvent many immunological complications and adverse side effects associated with mismatched donor cells and transplant recipients. Recently, these cells have been applied in experimental and clinical studies, and the effect of menstrual blood cells on basal ganglia disorders is the main subject of this chapter.
Investigation of Stem Cells
Today’s challenge is to find the perfect cell, which should be immature enough to hold multipotential differentiation properties and yet safe to not induce malignancy. It should also modulate the immune system, decreasing destructive aggression but preserving its ability to fight pathogens. Finally, it should be able to induce changes in the targeted tissue, either restoring its function or promoting repair. Several cell types match the above criteria and have been applied in experimental and clinical research; however, in most cases ethical and practical issues are a concern. Stem cells from bone marrow, for instance, work well on most studies, but cell harvesting through bone marrow aspiration or leukapheresis is needed and the number of cells obtained may be not enough. Other sources, like the liver, skin, heart, or even induced pluripotent stem (iPS) cells, are also available but the isolation and culture of those cells is currently costly and technically complicated [32, 42, 65]. There is interest, therefore, in acquiring stem cells from disposable and easily accessible tissues, such as the amnion and amniotic fluid, placenta, umbilical cord tissue, adipose tissue, and, more recently, menstrual blood.
Because of ethical and safety reasons associated with embryonic stem cells, the last decade has witnessed the wide use of adult stem cells as graft source for cell therapy. In the United States, the previous government moratorium on the use of embryonic stem cells also arguably influenced the shift of cell based-therapies toward the use of adult stem cells. A majority of the studies have explored adult stem cells harvested from the bone marrow. Nonetheless, although numerous applications of hematopoietic stem cell transplantation for malignant and nonmalignant diseases have been reported, there is still a paucity of this treatment in neurological disorders. Moreover, compatibility issues restrict the use of adult hematopoietic stem cells, requiring fully or close to fully HLA-matched donors. In the last years, new adult stem cell donor tissues have been investigated, as alternatives to bone marrow, comprising a rich research field to be explored. Umbilical cord blood, amnion, and placenta provide stem cells that are thought to possess a higher immunosuppressive potential, are better tolerated by the host immune system, and preserve multipotential differentiation capacity. Of note, the mesenchymal cells, or stromal cells, harvested from those tissues share interesting phenotypic and functional features with embryonic stem cells and also to mesenchymal cells derived from bone marrow, like the ability to modulate the immune system and to stimulate tissue repair, which have already been applied for the treatment of autoimmune and degenerative diseases.
Stroke
Stroke is the third leading cause of death [86] and the primary cause of long-term disability in the United States [18]. Despite successful efforts to decrease incidence and mortality of cerebrovascular diseases, they still remain as a major concern in clinical setting. There is a negative impact on economic productivity, as approximately 15–30 % of first-time stroke patients become permanently disabled and 20 % still require institutional care 3 months after stroke [7]. For the year of 2010, the American Heart Association estimated direct and indirect costs of stroke of $73.7 billion [54]. Therefore, every effort to decrease the incidence of strokes and their consequential sequelae is urgently warranted.
Tissue plasminogen activator (tPA) is the only therapeutic agent approved by the US Food and Drug Administration indicated for ischemic stroke. The drug catalyzes the transformation of plasminogen into plasmin, which acts as a potent thrombolytic agent and is used to restore the blood flow, thus minimizing immediate tissue death. In 1995, an American clinical trial demonstrated that patients treated with tPA within 3 hours of beginning of symptoms presented less disability 3 months later [81]. The results were also supported by a similar concomitant European trial [36]. Since then, the FDA and, later, the European Medicines Agency have approved the drug, and it has been applied as standard therapy in emergency rooms all over the world. Numerous other studies also supported the early use of tPA, demonstrating a direct correlation between time elapsed to begin treatment and long-term neurological impairment [1, 59, 71].
The application of tPA, however, is greatly limited by the therapeutic window of 3 h. Most patients are not able to reach an Emergency Room and complete the neurologic triage within that timeframe and, therefore, are excluded from the beneficial effects of the drug. In fact, in 2008 only 1.8–2.1 % of all patients affected by ischemic strokes in the United States received the therapy [46]. Further studies have tried to evaluate the possibility of extending the limit beyond 3 h, but the results were nonconclusive, with an increase in mortality due to hemorrhagic complications [17, 22, 37]. Some controversy was created by subsequent studies, which showed that the results of tPA treatment were not as favorable as once suggested and, most importantly, that its beneficial effects were restricted to a small population of the stroke patients. In 2006, analysis of the European data indicated that higher age; male gender; history of previous strokes; comorbidities, such as hypertension and diabetes; and higher severity of the stroke were associated with poor outcomes after tPA therapy [44]. Moreover, new research has shown that while tPA renders clot clearance within the intravascular space, it can be deleterious to the brain through worsening of the already altered blood-brain-barrier permeability, in addition to direct neurotoxic effects [87]. It is clear that tPA for ischemic stroke benefits a very selective group of patients. Those who are not able to avail of the 3-h tPA efficacy period and would have to deal with the long-term consequences of the disease, most often, are relegated to rehabilitation therapy. This significant unmet clinical need for stroke thus warrants investigations into novel treatments with wide therapeutic windows such as restorative interventions, including cell-based therapy.
Inflammation After Stroke
The acute blood supply interruption that takes place in ischemic stroke promotes almost instant cell death of the infarct core. The surrounding ischemic penumbra area comprises the tissue that retains structural integrity, but lacks function. It has a less defined outcome and may either evolve to death or to recovery, depending on the reestablishment of blood flow within the first hours after stroke [34]. Once the hypoxic insult is settled, a complex cascade of events takes place, in which inflammation seems to have a major role [26]. Following the sudden drop in oxygen and glucose supply that begins immediately after the interruption of blood flow, intracellular Ca++ concentrations increase, as a consequence of the Na+/K+-ATPase and Ca++/H+-ATPase pumps malfunctioning, associated to the reversed function of the Na+/Ca++ transporters [25]. The high concentrations of the ions activate Ca++-dependent enzymes, leading to cytotoxicity, formation of free radicals, and cell death. In parallel, ischemia triggers neuronal depolarization, leading to glutamate excitotoxicity, considered a major pathophysiological event of stroke [69], also contributing to neuronal death. Soon other inflammatory responses arise, with generation of free oxygen radicals and nitric oxide, activation of neighboring glia, and migration of other inflammatory cells from the systemic circulation, which once more promote further neuronal death.
Local and migrated cells participate of the inflammatory response. Activated astrocytes contribute to the formation of glial scar, therefore limiting the extension of injury. In long term, however, the scar restrains the migration of cells and hampers repair of the injured tissue. Interestingly, Faulkner et al. [29] demonstrated that the inhibition of astrocyte activation following spinal cord injury increased neuron death, possibly because astrocytes also secrete neurotrophic factors (NGF and BDGF), which are important for tissue repair and modulation of synaptic plasticity [47]. The microglia also take part in recovery by removing debris and harmful substances from the parenchyma. Likewise, neurons themselves contribute to increase the inflammatory response, through the release of free radicals and inflammatory cytokines. Finally, endothelial cells are also affected, with opening of the blood-brain barrier and subsequent passage of cells and proinflammatory agents into the central nervous system (CNS).
In the last years, research has targeted inflammatory components of stroke, aiming to reduce the extension of injury in the CNS. Anti-inflammatory interventions may attenuate the secondary cell death associated with ischemic stroke and, likely, lessen neurological impairments among other progressive disabilities. Specific inflammatory agents have been blocked, such as ICAM-1, IL-1 receptor, nitric oxide, TNF-α, and, more recently, Toll-like receptors [27]. Others have focused on more general interventions, also trying to abrogate inflammation, such as induced hypothermia, corticosteroids, and minocycline [28, 50, 60]. To this end, finding a novel anti-inflammatory strategy, such as the use of cell therapy, to at least minimize the injuries and at most reverse the outcome of stroke is a logical therapeutic approach toward improving the quality of life for many stroke patients.
In the cell-based therapy context, inflammation is necessary. The presence of cytokines is essential for cell migration to the site of injury and for production of neurotrophic agents, but their excess may decrease graft survival and directly contribute to neuronal death. On the opposite way, the stem cells themselves may modulate the inflammatory setting, inhibiting the reactive immune cells, increasing tolerance, and promoting a cytokine shift toward a less inflammatory Th2 profile [45, 53, 75].
Injury following stroke can be divided in three consecutive stages, important for the different therapeutic opportunities implied in each [40]. In the 24 h that immediately follow stroke, attempts to restore the blood flow would be neuroprotective, therefore preventing further early neuronal death and restricting the extent of the penumbra area. Thereafter, once the injury is established, the interventions would be mainly restorative and cell-based therapies would have their best indications. It is known that during the first month after stroke the brain produces inflammatory signals, which can be used to opportunely attract cells injected in the systemic circulation to the site of injury. It is also during this period that the interventions may restore the viability of the tissue in the penumbra area. Terminated the first month, the inflammation decreases and scars and structural damage persist. Stem cells still have a possible therapeutic role in this last phase, but they should be delivered directly into the nervous tissue, through the aid of scaffolds and surgical procedures.
Inflammation plays a double-edged sword role in stroke, as in other CNS inflammatory and neurodegenerative diseases [3, 23, 56]. Contrary to previous beliefs, it is unquestionable today that inflammation and immune activation are present in the CNS and, even further, that the CNS influences and is influenced by systemic inflammatory processes. Following stroke, inflammatory markers, such as IL-6, C-reactive protein, matrix metalloproteinase, and monocyte chemoattractant factor-1 (MCP-1), are detected in increased levels in the peripheral blood [85]. In the brain tissue, cytokine production is induced immediately after the ischemic injury, followed by the release of chemokines and adhesion molecules, recruitment of immune cells to the parenchyma, and, finally, activation of immigrated and endogenous cells [72, 90]. Some of the inflammatory agents, such as IL-6, nitric oxide (NO), and TNF-α, have antagonistic effects on the tissue, acting as protective in early phases and detrimental in late stages of injury [57, 62, 78]. For instance, in multiple sclerosis, which is an inflammatory autoimmune disease, TNF-α is known to mediate injury, but blocking this cytokine in a clinical trial resulted in worsening of the disease [80]. Shohami et al. [76], on the other hand, demonstrated that the inhibition of TNF-α improved the outcome of closed head injury rats, decreasing inflammation and protecting neurons from death. Based on such observations, it is discussed that the timing of intervention, either stimulating or inhibiting inflammatory responses, is of main importance for the success of treatment [77].
In summary, at early stages, inflammation is desired and necessary. However, at chronic period, if inflammation persists and no therapeutic intervention is employed to correct this aberrant response, then such host tissue response to injury will exacerbate the disease progression. Along this line, the initiation of anti-inflammatory regimen after stroke is critical to the resulting outcome, and it represents an opportune niche for the application of cell-based therapies. Additional critical analyses of inflammation as a friend and foe of stroke are needed to fully decipher the mechanisms of action of inflammation in stroke onset and progression.
The Role of Stem Cells in Stroke
In stroke, inflammation must be restrained and tissue destruction must be minimized or even repaired. Reinforced by the previous knowledge acquired from treatment of basal ganglia disorders, stem cells seem the ideal therapeutic tool. To date, several studies using stem cells for experimental stroke have been published [15, 30, 48], and their beneficial effects are becoming well established, although still questioned by some researchers [88].
The use of stem cells in stroke is criticized because their exact targets and mechanisms of action are still unknown and need investigation. However, evidence shows that they can be effective through multiple pathways, all leading to improvement of the injury. Taguchi et al. suggested an angiogenic effect of CD34-positive (CD34+) cells from umbilical cord blood on the ischemic area of stroke [79]. They observed that the cells injected systemically into a mouse model of stroke secreted growth factors (VEGF, FGF2, and IGF-1), induced formation of vascular channels, and, secondarily, promoted migration of neuronal precursors into the injured areas, which differentiated and improved nervous function. The addition of anti-angiogenic agents abolished the beneficial effect of the cells, demonstrating the importance of vessels in nervous repair. The issue was later discussed by Saghatelyan [74], which supported the hypothesis that vasculature-guided neuronal migration can be observed not only following stroke but also as part of the normal brain development. More recently, endothelial progenitor cells injected into the systemic circulation of mice migrated to the stroke area, promoted repair, and improved behavior, in comparison to controls, reinforcing the importance of angiogenesis [91]. Finally, Nakagomi et al. [66] demonstrated that the addition of endothelial precursors to neural stem cells, engrafted in mouse models of brain ischemia, enhanced cell survival, proliferation, and differentiation, when compared to injections of neural stem cells alone.
In the same study published by Taguchi et al., the authors reported that CD34-negative (CD34-) cells were not able to promote tissue repair after stroke. Boltze et al. refuted this last idea through a study in which CD34+ and CD34- cell populations from umbilical cord blood were injected intravenously and had equivalent effects on rat models of stroke [12]. In particular, both cell subtypes promoted functional improvement and migrated to the area of injury, although differentiation into neural markers expressing cells was not detected. The authors hypothesize that CD133+ CD34- cells might have a role in tissue repair equally as CD34+ cells. This type of discrepant results, although may be construed as hindering the progress of cell therapy, actually exemplifies that the field is maturing and that there is a healthy atmosphere among stem cell researchers to confirm, refute, and validate efficacy and safety data. In the end, such rigorous preclinical studies will benefit the transplant recipient.
Until recently, it was believed that cell effectiveness would be conditional on their migration to the site of injury. In fact, several authors observed a direct relationship between cell migration to the site of injury and behavioral improvement [8, 43]. However, Borlongan et al. [15] observed, in rat models of stroke, that umbilical cord blood cells were able to promote repair even when not detected in the tissue, probably through the production of growth factors, cytokines, and other therapeutic molecules that were able to reach the target. Adding importance to that idea, in the last years, considerable research has studied the effect of neurotrophic agents on stroke, as it happened in basal ganglia disorders. Neurotrophic agents influence cell survival, proliferation, differentiation, function, and plasticity [39, 55]. They also have a role in physiological endogenous repair, and increased levels can be detected in injured neuronal sites [21]. They protect neurons from the cytotoxic insults generated during inflammation, with anti-excitotoxic and antioxidant functions, besides improving mitochondrial function.
Administration of agents with specific angiogenic functions, such as VEGF, angiopoietins, factors that influence Notch signaling, among others, have generated interesting results in neural support [2, 4, 5]. Additionally, some studies have addressed the use of genetically modified cells to release neurotrophic factors at the site of injury. The cells would be used as vehicles, attracted to the inflammatory area of stroke, and the growth factors would promote angiogenesis and provide support to neuronal progenitors in the brain [61]. Neurotrophic agents are considered promising for stroke therapy, but their stable and long-term effectiveness still warrants additional investigations, owing in part technical problems related to the manufacturing production of these molecules at clinically therapeutic doses. The combination of neurotrophic factor treatment with cell therapy seems interesting and perhaps will provide exciting results in the future.
Parkinson’s and Huntington’s Disease
Experimental stroke studies share overlapping research themes with other animal models of basal ganglia disorders, mainly Parkinson’s disease and Huntington’s disease, in which numerous therapeutic strategies have been described, aiming to improve survival of remaining neurons, abrogate the ongoing neurotoxic processes, or functionally replace the destroyed tissue [2]. Cell-based therapy is considered promising and different cell types have been used. Fetal neural tissue, neuronal stem and progenitor cells, tissue engineered to secrete neurotransmitters or neurotrophic factors, para-neuronal cells which support neurons, and grafts that may assist the reconstruction of injured axonal pathways have been documented in the literature, with variable results. A major long-standing conundrum in cell therapy is finding the most optimal donor cells. While the more differentiated cells have been thought to offer tissue-specific transplant regimen tailored to treat the specific diseases, their mature phenotype (albeit also mature immune system) renders them to be immunologically rejected by the host and, therefore, rapidly eliminated. On the other hand, less differentiated cells such as the embryonic stem cells are also attractive, since they are better tolerated by the host immune system and have more plasticity, but the risk of uncontrolled proliferation and tumor formation strongly limits their applications.
Parkinson’s disease is a common neurodegenerative disease that affects about 2 % of the population over 65 years of age. Progressive loss of the dopamine-producing neurons from the midbrain substantia nigra, that project into the striatum, cause tremor, rigidity, and hypokinesia. Experimental studies have been conducted for approximately 30 years, with interesting data from cell-based therapies, despite some major hurdles [10, 11, 33]. The best results were achieved with transplantation of fetal mesencephalic tissue into the striatum, which is the target for dopamine action. In humans, transplantation for Parkinson’s disease has been reported since 1982, with initially successful and later disappointing results [9, 51, 58]. The major barrier observed was poor survival of adult grafts in the host brain, which was to some extent solved with the use of tissue from fetal origin. Still, only about 10 % of the transplanted cells survive in the host tissue [38]. Fetal mesencephalic tissue has been used to replace the lost neurons and restore dopamine production and comprises an important progress in the field. To date, between 300 and 400 patients have already been grafted with the fetal mesencephalic tissue, but while some report outstanding outcomes, with some patients leaving medication, others fail to observe major effects [6]. The inconsistency of results, ascribed to ethical concerns, limited tissue availability, emergence of unexpected dyskinesias, and high rates of graft rejection, still hamper the application of this therapy and stimulate the search for alternatives.
Huntington’s disease is genetically determined, with progressive neurodegeneration primarily of the striatum, inducing motor and psychiatric dysfunctions. As in Parkinson’s disease, several attempts to delay the progression of the disease have been studied. Treatment of Huntington’s disease, though, is complex and requires more than simple neurotransmitter replacement, in that reestablishment of the striatal network is needed. Transplantation of fetal striatal tissue proved to be effective in experimental models of the disease, with symptomatic improvement and evidence of graft incorporation; however controversial establishment of connections with the host striatum remains to be resolved [13, 14, 35]. Clinical trials have been conducted with modest results; while some patients present motor and cognitive improvements after transplantation, others fail to benefit from the procedure [52].
In evaluating the progress of cell therapy for Parkinson’s and Huntington’s diseases, it is evident that there are technical disparities among the centers that might influence the results and some guidelines are to be determined. Age of the patient, disease stage, number of cells, surgical technique to implant the cells, and tissue conservation, among others, are reported as parameters to be defined. Moreover, neurotrophic factors promote neuroprotection, which is essential in both diseases, and some authors propose to combine their use with the transplanted cells [2]. Other strategies, using antioxidant, anti-excitotoxic, bioenergetic, immunosuppressants, and antiapoptotic agents are also suggested either as stand-alone monotherapy or as adjunct to cell transplantation.
At present, besides the satisfactory results obtained with the transplanted fetal tissue, there is a continued search for other cell sources aiming to treat Parkinson’s and Huntington’s diseases. Little availability of the embryonic tissue is the main reason. Recently, a clinical trial conducted in India tested mesenchymal cells for Parkinson’s disease, but while safety was established, efficacy could not be evaluated due to the study design [82]. Similarly, rat models of Huntington’s disease were treated with mesenchymal cells genetically modified to express growth factors, evolving with delay of disease progression [24]. Other researchers focus on neural tissue differentiated from human embryonic stem cells, but the studies are still in the experimental level, mainly because of safety reasons. These cells, even after differentiation, retain the capacity to form tumors, and attempts to reverse it have decreased their survival [31, 73]. Finally, there is recent effort in treating Parkinson’s disease with autologous induced pluripotent stem (iPS) cells, which are interesting for their adult cell origin, avoiding ethical issues. Their safety, however, remains questionable, since formation of neural overgrowths was observed in rats transplanted with these cells, similarly to what was seen with embryonic stem cells [83], likely owing to the lack of regulatory mechanisms in controlling the “stemness” technology employed to revert these mature cells into their undifferentiated plastic state.
Several cell-based studies are being investigated for basal ganglia disorders, mainly using cells already differentiated into neural tissue. While it is still early to apply them in large-scale clinical trials, much of the knowledge acquired from experimental studies can be transposed to the treatment of other diseases. Stroke, for instance, is also considered a basal ganglia disease, and cell therapy has been extensively applied to it as discussed above.
Applications of Stem Cells Derived from the Endometrium
The presence of stem cells in the endometrium was described about 30 years ago, from the observation that the upper layers of this tissue shed and were renovated each month, but that the cells that were shed represented nonviable cells. In particular, the cells in the basalis were viable but not the shed cells from the functionalis [67, 70]. Only in the last few years, however, have endometrial cells been better characterized [19, 63, 68]. In vitro investigations have determined clonogenicity, multipotentiality, and expression of markers of pluripotency, such as Oct-4, SSEA-4, and c-kit, which are frequently found in more immature cell types, including the embryonic stem cells. Finally, an experimental study demonstrated that menstrual blood-derived stromal cells promoted functional improvement of damaged heart tissue, with evidence of cell engraftment and transdifferentiation into cardiac tissue [41].
In the nervous system context, Borlongan et al. [16], published the results of menstrual blood cell transplantation in experimental stroke. Stromal-like menstrual blood stem cells were isolated, expanded, and, at last, selected for CD117 or C-kit receptor, a marker associated with high proliferation, migration, and survival [20]. In vitro studies showed that the expanded cells maintained expression of embryonic-like stem cell phenotypic markers, such as Oct4, SSEA, and Nanog, even when cultured up to 9 passages, as an evidence of the safety and reliability of these cells, and some were induced to express neural markers (MAP2 and Nestin) [16, 68]. Moreover, when added to cultured rat neurons exposed to a hypoxic insult, the menstrual blood cells provided neuroprotection and when applied to rat stroke models, less neurologic deficit was observed on behavioral tests, irrespective of the injection site, i.e., systemic or local administration into the striatum. However, analysis of the tissue, after animal sacrifice, revealed that although human cells were detected in the rat brain, some migrating to areas other than the injected, they did not show signs of differentiation, expressing their original markers. Once more, there is evidence that cell differentiation is not the main pathway of neuroprotection or neuroregeneration.
Wolff et al. [84] reported the use of endometrial-derived neural cells in a Parkinson’s disease immunocompetent mouse model. Endometrial-derived stromal cells were differentiated in vitro into dopamine-producing cells, which expressed the neural markers nestin and tyrosine hydroxylase, and were then engrafted into the brains of the animals. Migration, differentiation, and production of dopamine were detected in vivo, demonstrating the therapeutic potential of these cells to functionally restore the damaged tissue, either through cell replacement or endogenous repair.
The only clinical study yet published evaluated the safety aspects of endometrial-derived stromal cells administration [89]. Four patients with multiple sclerosis were treated with intrathecal injections of 16–30 million cells and one of the patients also received an additional intravenous injection of the same cells. No adverse events were registered, as expected, and the authors reported functional stabilization. However, the longest follow-up reached 12 months, and any conclusions about effectiveness of the treatment seem premature in this long-term and slowly progressive illness.
Future Expectations
Research on cell therapy for stroke has reached great proportions, especially because of the possibility of translational studies, which have already started. Most studies use the knowledge of neuroregenerative areas of the brain, more specifically the hippocampus and, still with some controversy, the subventricular zone to guide their studies, although some have shown cell migration and repair of areas other than those considered as highly neurogenic [49, 64]. Furthermore, it seems clear that the rescue of the penumbra area after stroke is decisive for functional outcome and a great opportunity for cell therapy. Stem cells promote neuroprotection, via modulation of the activated immune system as one major pathway. Tissue repair is also described and, although cell differentiation is observed in the experimental setting, its importance to the final outcome of the treatment is still undefined.
Menstrual cells are a novel therapeutic option in this field and have great potential. Ease of access, availability, and safety are considered their main key to future clinical studies. Most important for effectiveness purposes, however, is the immature behavior of these cells, in which pluripotency and proliferation circumvent the main challenges of tissue repair. The menstrual cells represent, therefore, an important therapeutic tool that may improve the outcome of stroke and decrease the disability of future patients. Further experimental studies are still required, especially to determine the exact mechanisms of action and, perhaps, establish new therapeutic applications for these cells.
References
Alexandrov AV, Burgin WS, Demchuk AM, El-Mitwalli A, Grotta JC. Speed of intracranial clot lysis with intravenous tissue plasminogen activator therapy, sonographic classification and short-term improvement. Circulation. 2001;103:2897–902.
Alexi T, Borlongan CV, Faull RL, et al. Neuroprotective strategies for basal ganglia degeneration: Parkinson’s and Huntington's diseases. Prog Neurobiol. 2000;60:409–70.
Amor S, Puentes F, Baker D, van der Valk P. Inflammation in neurodegenerative diseases. Immunology. 2010;129:154–69.
Androutsellis-Theotokis A, Rueger MA, Park DM. Angiogenic factors stimulate growth of adult neural stem cells. PLoS One. 2010;5:e9414.
Arboleda-Velasquez JF, Zhou Z, Shin HK, et al. Linking Notch signaling to ischemic stroke. Proc Natl Acad Sci U S A. 2008;105:4856–61.
Arenas E. Towards stem cell replacement therapies for Parkinson’s disease. Biochem Biophys Res Commun. 2010;396:152–6.
Asplund K, Stegmayr B, Peltonen M. From the twentieth to the twenty-first century: a public health perspective on stroke. In: Ginsberg MD, Bogousslavsky J, editors. Cerebrovascular disease pathophysiology, diagnosis, and management. Malden: Blackwell Science; 1998. p. 901–18.
Barzilay R, Levy YS, Melamed E, Offen D. Adult stem cells for neuronal repair. Isr Med Assoc J. 2006;8:61–6.
Björklund A, Stenevi U, Dunnett SB, Iversen SD. Functional reactivation of the deafferented neostriatum by nigral transplants. Nature. 1981;289:497–9.
Björklund A, Lindvall O. Cell replacement therapies for central nervous system disorders. Nat Neurosci. 2000;3:537–44.
Björklund A, Cenci MA. Recent advances in Parkinson’s disease: basic research. Prog Brain Res. 2010;183:ix–x.
Boltze J, Kowalski I, Geiger K, et al. Experimental treatment of stroke in spontaneously hypertensive rats by CD34+ and CD34- cord blood cells. Ger Med Sci. 2005;3:Doc09.
Borlongan CV, Koutouzis TK, Poulos SG, Saporta S, Sanberg PR. Bilateral fetal striatal grafts in the 3-nitropropionic acid-induced hypoactive model of Huntington’s disease. Cell Transplant. 1998;7:131–7.
Borlongan CV, Stahl CE, Freeman TB, Hauser RA, Sanberg PR. Neural transplantation and Huntington’s disease, what can we learn from the 3-nitropionic acid model. In: Sanberg PR, Nishino H, Borlongan CV, editors. Mitochondrial inhibitors and neurodegenerative disorders. Totowa: Humana Press; 1999.
Borlongan CV, Hadman M, Sanberg CD, Sanberg PR. Central nervous system entry of peripherally injected umbilical cord blood cells is not required for neuroprotection in stroke. Stroke. 2004;35:2385–9.
Borlongan CV, Kaneko Y, Maki M, et al. Menstrual blood cells display stem cell-like phenotypic markers and exert neuroprotection following transplantation in experimental stroke. Stem Cells Dev. 2010;19:439–51.
Carpenter CR, Keim SM, Milne WK, Meurer WJ, Barsan WG, The Best Evidence in Emergency Medicine Investigator Group. Thrombolytic therapy for acute ischemic stroke beyond 3 hours. J Emerg Med. 2011;40:82–92.
Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults, United States. MMWR Morb Mortal Wkly Rep. 1999;50:120–5.
Chan RW, Schwab KE, Gargett CE. Clonogenicity of human endometrial epithelial and stromal cells. Biol Reprod. 2004;70:1738–50.
Cho NH, Park YK, Kim YT, Yang H, Kim SK. Lifetime expression of stem cell markers in the uterine endometrium. Fertil Steril. 2004;81:403–7.
Connor B, Dragunow M. The role of neuronal growth factors in neurodegenerative disorders of the human brain. Brain Res Rev. 1998;27:1–39.
Cronin CA. Intravenous tissue plasminogen activator for stroke, a review of the ECASS III results in relation to prior clinical trials. J Emerg Med. 2010;38:99–105.
Del Zoppo G, Ginis I, Hallenbeck JM, et al. Inflammation and stroke, putative role for cytokines, adhesion molecules and iNOS in brain response to ischemia. Brain Pathol. 2000;10:95–112.
Dey ND, Bombard MC, Roland BP, et al. Genetically engineered mesenchymal stem cells reduce behavioral deficits in the YAC128 mouse model of Huntington’s disease. Behav Brain Res. 2010;214:193–200.
Durukan A, Tatlisumak T. Acute ischemic stroke: overview of major experimental rodent models, pathophysiology, and therapy of focal cerebral ischemia. Pharmacol Biochem Behav. 2007;87:179–97.
Emsley CA, Smith CJ, Tyrrell PJ, Hopkins SJ. Inflammation in acute ischemic stroke and its relevance to stroke critical care. Neurocrit Care. 2008;9:125–38.
Fan H, Li L, Zhang X, Liu Y, Yang C, Yang Y, Yin J. Oxymatrine downregulates TLR4, TLR2, MyD88, and NF-kappaB and protects rat brains against focal ischemia. Mediators Inflamm. 2009;2009:704–6.
Faraji J, Lehmann H, Metz GA, Sutherland RJ. Stress and corticosterone enhance cognitive recovery from hippocampal stroke in rats. Neurosci Lett. 2009;462:248–52.
Faulkner JR, Herrmann JE, Woo MJ, et al. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J Neurosci. 2004;24:2143–55.
Felfly H, Muotri A, Yao H, Haddad GG. Hematopoietic stem cell transplantation protects mice from lethal stroke. Exp Neurol. 2010;225:284–93.
Friling S, Andersson E, Thompson LH, et al. Efficient production of mesencephalic dopamine neurons by Lmx1a expression in embryonic stem cells. Proc Natl Acad Sci U S A. 2009;106:7613–8.
Gerbal-Chaloin S, Duret C, Raulet E, et al. Isolation and culture of adult human liver progenitor cells, in vitro differentiation to hepatocyte-like cells. Methods Mol Biol. 2010;640:247–60.
Glavaski-Joksimovic A, Virag T, Chang QA, et al. Reversal of dopaminergic degeneration in a parkinsonian rat following micrografting of human bone marrow-derived neural progenitors. Cell Transplant. 2009;18:801–14.
Green RA, Odergren T, Ashwood T. Animal models of stroke: do they have value for discovering neuroprotective agents? Trends Pharmacol Sci. 2003;24:402–8.
Guzman R, Meyer M, Lovblad KO, et al. Striatal grafts in a rat model of Huntington’s disease, time course comparison of MRI and histology. Exp Neurol. 1999;156:180–90.
Hacke W, Kaste M, Fieschi C, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA. 1995;274:1017–25.
Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29.
Hagell P, Brundin P. Cell survival and clinical outcome following intrastriatal transplantation in Parkinson’s disease. J Neuropathol Exp Neurol. 2001;60:741–52.
Hefti F. Pharmacology of neurotrophic factors. Annu Rev Pharmacol Toxicol. 1997;37:239–67.
Hess DC, Borlongan CV. Cell-based therapy in ischemic stroke. Expert Rev Neurother. 2008;8:1193–201.
Hida N, Nishiyama N, Miyoshi S, et al. Novel cardiac precursor-like cells from human menstrual blood-derived mesenchymal cells. Stem Cells. 2008;26:1695–704.
Huang HI, Chen SK, Ling QD, et al. Multilineage differentiation potential of fibroblast-like stromal cells derived from human skin. Tissue Eng Part A. 2010;16:1491–501.
Jin K, Sun Y, Xie L, et al. Comparison of ischemia-directed migration of neural precursor cells after intrastriatal, intraventricular, or intravenous transplantation in the rat. Neurobiol Dis. 2005;18:366–74.
Kent DM, Selker HP, Ruthazer R, Bluhmki E, Hacke W. Can multivariable risk-benefit profiling be used to select treatment-favorable patients for thrombolysis in stroke in the 3- to 6-hour time window? Stroke. 2006;37:2963–9.
Kim SY, Cho HS, Yang SH, et al. Soluble mediators from human neural stem cells play a critical role in suppression of T-cell activation and proliferation. J Neurosci Res. 2009;87:2264–72.
Kleindorfer D, Lindsell CJ, Brass L, Koroshetz W, Broderick JP. National US estimates of recombinant tissue plasminogen activator use, ICD-9 codes substantially underestimate. Stroke. 2008;39:924–8.
Kriz J. Inflammation in ischemic brain injury, timing is important. Crit Rev Neurobiol. 2006;18:145–57.
Leu S, Lin YC, Yuen CM, et al. Adipose-derived mesenchymal stem cells markedly attenuate brain infarct size and improve neurological function in rats. J Transl Med. 2010;8:63.
Li JM, Zhu H, Lu S, et al. Migration and differentiation of human mesenchymal stem cells in the normal rat brain. Neurol Res. 2011;33:84–92.
Linares G, Mayer SA. Hypothermia for the treatment of ischemic and hemorrhagic stroke. Crit Care Med. 2009;37(7 Suppl):S243–9.
Lindvall O, Rehnerona S, Brundin P, et al. Human fetal dopamine neurons grafted into the striatum in two patients with severe Parkinson’s disease. a detailed account of methodology and a 6-month follow-up. Arch Neurol. 1989;46:615–31.
Lindvall O, Björklund A. First step towards cell therapy for Huntington’s disease. Lancet. 2000;356:1945–6.
Lindvall O, Kokaia Z. Stem cells in human neurodegenerative disorders–time for clinical translation? J Clin Invest. 2010;120:29–40.
Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary, heart disease and stroke statistics-2010 update, a report from the American Heart Association. Circulation. 2010;121:948–54.
Loughlin AJ, Woodroofe MN, Cuzner ML. Modulation of interferon-gamma-induced major histocompatibility complex class II and Fc receptor expression on isolated microglia by transforming growth factor-beta 1, interleukin-4, noradrenaline and glucocorticoids. Immunology. 1993;79:125–30.
Lucas SM, Rothwell NJ, Gibson RM. The role of inflammation in CNS injury and disease. Br J Pharmacol. 2006;147 Suppl 1:S232–40.
Luheshi NM, Rothwell NJ, Brough D. Dual functionality of interleukin-1 family cytokines: implications for anti-interleukin-1 therapy. Br J Pharmacol. 2009;157:1318–29.
Madrazo I, Francobourland R, Ostrosky-Solis F, et al. Fetal homotransplant to the striatum of parkinsonian subjects. Arch Neurol. 1990;47:1281–5.
Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome, the NINDS rt-PA stroke study. Neurology. 2000;55:1649–55.
Matsukawa N, Yasuhara T, Hara K, et al. Therapeutic targets and limits of minocycline neuroprotection in experimental ischemic stroke. BMC Neurosci. 2009;10:126.
Maurer MH, Thomas C, Bürgers HF, Kuschinsky W. Transplantation of adult neural progenitor cells transfected with vascular endothelial growth factor rescues grafted cells in the rat brain. Int J Biol Sci. 2007;4:1–7.
McCoy MK, Tansey MG. TNF signaling inhibition in the CNS: implications for normal brain function and neurodegenerative disease. J Neuroinflammation. 2008;5:45.
Meng X, Ichim TE, Zhong J, et al. Endometrial regenerative cells: a novel stem cell population. J Transl Med. 2007;5:57.
Mezey E, Chandross KJ, Harta G, Maki RA, McKercher SR. Turning blood into brain: cells bearing neuronal antigens generated in vivo from bone marrow. Science. 2000;290:1779–82.
Mosna F, Annunziato F, Pizzolo G, Krampera M. Cell therapy for cardiac regeneration after myocardial infarct, which cell is the best? Cardiovasc Hematol Agents Med Chem. 2010;8:227–43.
Nakagomi N, Nakagomi T, Kubo S, et al. Endothelial cells support survival, proliferation, and neuronal differentiation of transplanted adult ischemia-induced neural stem/progenitor cells after cerebral infarction. Stem Cells. 2009;9:2185–95.
Padykula HA. Regeneration in the primate uterus, the role of stem cells. Ann N Y Acad Sci. 1991;622:47–52.
Patel AN, Park E, Kuzman M, et al. Multipotent menstrual blood stromal stem cells, isolation, characterization and differentiation. Cell Transplant. 2008;17:303–11.
Park DH, Borlongan CV, Willing AE, et al. Human umbilical cord blood cell grafts for brain ischemia. Cell Transplant. 2009;18:985–98.
Prianishnikov VA. On the concept of stem cell and a model of functional-morphological structure of the endometrium. Contraception. 1978;18:213–23.
Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome? A meta-analysis. Stroke. 2007;38:967–73.
Rothwell NJ, Luheshi GN. Interleukin 1 in the brain: biology, pathology and therapeutic target. Trends Neurosci. 2000;23:618–25.
Roy NS, Cleren C, Singh SK, et al. Functional engraftment of human ES cells-derived dopaminergic neurons enriched by coculture with telomerase-immortalized midbrain astrocytes. Nat Med. 2006;12:1259–68.
Saghatelyan A. Role of blood vessels in the neuronal migration. Semin Cell Dev Biol. 2009;20:744–50.
Saino O, Taguchi A, Nakagomi T, et al. Immunodeficiency reduces neural stem/progenitor cell apoptosis and enhances neurogenesis in the cerebral cortex after stroke. J Neurosci Res. 2010;88:2385–97.
Shohami E, Bass R, Wallach D, Yamin A, Gallily R. Inhibition of tumor necrosis factor alpha (TNFalpha) activity in rat brain is associated with cerebroprotection after closed head injury. J Cereb Blood Flow Metab. 1996;16:378–84.
Shohami E, Ginis I, Hallenbeck JM. Dual role of tumor necrosis factor alpha in brain injury. Cytokine Growth Factor Rev. 1999;10:119–30.
Suzuki S, Tanaka K, Suzuki N. Ambivalent aspects of interleukin-6 in cerebral ischemia: inflammatory versus neurotrophic aspects. J Cereb Blood Flow Metab. 2009;29:464–79.
Taguchi A, Soma T, Tanaka H, et al. Administration of CD34+ cells after stroke enhances neurogenesis via angiogenesis in a mouse model. J Clin Invest. 2004;114:330–8.
The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. TNF neutralization in MS: results of a randomized, placebo-controlled multicenter study. Neurology. 1999;53:457–65.
The National Institute of Neurological Disorders and Stroke (NINDS) rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7.
Venkataramana NK, Kumar SK, Balaraju S, et al. Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson’s disease. Transl Res. 2010;155:62–70.
Wernig M, Zhao J, Pruszak J, et al. Neurons derived from reprogrammed fibroblasts functionally integrate into the fetal brain and improve symptoms of rats with Parkinson’s disease. Proc Natl Acad Sci U S A. 2008;105:5856–61.
Wolff EF, Gao XB, Yao KV, et al. Endometrial stem cell transplantation restores dopamine production in a Parkinson’s disease model. J Cell Mol Med. 2011;15:747–55.
Worthmann H, Tryc AB, Deb M, et al. Linking infection and inflammation in acute ischemic stroke. Ann N Y Acad Sci. 2010;1207:116–22.
Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths, final data for 2007. Natl Vital Stat Rep. 2010;57:131–4.
Yepes M, Roussel BD, Ali C, Vivien D. Tissue-type plasminogen activator in the ischemic brain, more than a thrombolytic. Trends Neurosci. 2009;32:48–55.
Zawadzka M, Lukasiuk K, Machaj EK, Pojda Z, Kaminska B. Lack of migration and neurological benefits after infusion of umbilical cord blood cells in ischemic brain injury. Acta Neurobiol Exp. 2009;69:46–51.
Zhong Z, Patel AN, Ichim TE, et al. Feasibility investigation of allogeneic endometrial regenerative cells. J Transl Med. 2009;7:15.
Jin R, Yang G, Li G. Inflammatory mechanisms in ischemic stroke: role of inflammatory cells. J Leukoc Biol. 2010;87:779–89.
Fan Y, Shen F, Frenzel T, et al. Endothelial progenitor cell transplantation improves long-term stroke outcome in mice. Ann Neurol. 2010;67:488–97.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag London
About this chapter
Cite this chapter
Rodrigues, M.C.O. et al. (2015). Menstrual Blood Transplantation Therapy for Stroke and Other Neurological Disorders. In: Bhattacharya, N., Stubblefield, P. (eds) Regenerative Medicine. Springer, London. https://doi.org/10.1007/978-1-4471-6542-2_6
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6542-2_6
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6541-5
Online ISBN: 978-1-4471-6542-2
eBook Packages: MedicineMedicine (R0)