Abstract
Surgery of acute type A dissection must be mandatorily performed with the aid of Cardio-Pulmonary Bypass (CPB). Perfusion techniques are numerous and their use may be determined or influenced by the surgeon’s preferences, the surgical team’s culture, the procedural strategy and tactics and, by the existing physiological and anatomical damages induced by the dissection. The CPB circuit must therefore be adapted to the chosen procedural method required by the local and patient’s conditions.
In this chapter we describe the various sites and techniques of arterial cannulation and discuss their various advantages and drawbacks.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Surgery of acute type A dissection must be mandatorily performed with the aid of Cardio-Pulmonary Bypass (CPB). Perfusion techniques are numerous and their use may be determined or influenced by the surgeon’s preferences, the surgical team’s culture, the procedural strategy and tactics and, obviously, by the existing physiological and anatomical damages induced by the dissection. The CPB circuit must therefore be adapted to the chosen procedural method required by the local and patient’s conditions.
Since the first attempts of surgical repair of acute type A dissections, about five decades ago, it has appeared more and more obvious that the patient’s preoperative condition was a major determinant of the outcome of surgery. But it has also been demonstrated that, whatever the skill and the experience of the surgical team, the perfusion technique during the repair may have a major influence on the immediate outcome of the patient.
Indeed, although it might be difficult to establish a sort of hierarchy in the various causes of death or major adverse events, nobody denies presently that, together with tamponnade, pre and intraoperative malperfusion syndromes are among the main causes of the patients’ death.
Extremely dangerous malperfusions can be induced during the aortic repair. They mostly concern the central nervous system and the visceral organs. The problem is that, because of the chosen technique, or because of ignored anatomical damages or abnormalities, they may be completely ignored during the surgical procedure and recognized only at the end of the repair or in the ICU when it is too late. Most importantly, they are in general related to an inadequate arterial perfusion and can be avoided or their consequences limited by an appropriate perfusion technique.
To avoid inducing any malperfusion or worsening an existing one, it is of major importance that the false lumen be not perfused preferentially or at a higher pressure than the true lumen. This is not always possible due to the anatomical damages but, at least, the perfusion system must be aimed at perfusing both channels equally. In this regard, the type of arterial access is critical and the choice of a proper arterial cannulation site is an integral part of the surgical strategy.
Yet, although there is a general consensus within the surgical community concerning the here-above mentioned considerations, there is no agreement on the most efficacious and safest arterial cannulation method required to avoid deleterious complications during CPB [1].
In the present chapter we shall describe the various sites and techniques of arterial cannulation and discuss their various advantages and drawbacks.
The Arterial Cannulation
For several decades the question of arterial cannulation has been considered as totally resolved since cannulation of the femoral artery was almost systematic. Only less than two decades ago, it became obvious that this apparently secondary issue could be of some importance and that other modes of arterial cannulation could significantly influence the surgical results. Since then many different approaches and techniques have been described. They consist in cannulation of:
-
the femoral arteries (two sites)
-
the right axillary artery (two techniques)
-
the right brachial artery
-
the left axillary artery
-
the innominate artery
-
the common carotid arteries (two sites)
-
the ascending aorta (two techniques)
-
the apex of the left ventricle,
for a total of ten sites and five techniques of arterial access.
Cannulation of the Femoral Artery
When femoral cannulation is decided it is important to choose the side where there is a normal pulse, e.g. where the artery is supposed to be free from any dissecting process. If both arteries seem dissected, the side with the better pulse must be chosen. The artery may be approached through a vertical or horizontal incision high enough to the inguinal ligament to allow controlling and dissecting free the common femoral artery. This incision should be limited in length as large incisions are prone to induce complications such as lymphorrea and/or late local infection.
The artery is placed on snares and, after proper heparinization, cross-clamped up and downstream the chosen cannulation site. A short transverse arteriotomy is then performed and a properly sized cannula is inserted into the artery while releasing the upstream clamp. It is quite important to use a short cannula in order to avoid entering the false channel in the iliac artery. It is useless to try to insert a large diameter cannula which may damage the artery. In most cases an 18–22 French gauge cannula is large enough to allow a perfusion flow of 2.5 l/mn/m2 which is adequate for most adults.
The cannula is secured by using a tourniquet passed on the upstream snare or directly tied with the snare. It is important to carefully secure the cannula to avoid its displacement, kinking or even ejection.
The use of the femoral artery has many advantages.
One of the most important one is that it allows arterial access before the opening of the sternum. Indeed, in case of important tamponnade with severe cardiogenic shock, the opening of the sternum and pericardium may result in a sudden increase of the arterial pressure with subsequent rupture of the aorta.
Except in obese patients, the vessel is easily accessible and cannulation requires only a few minutes. In patients in severe cardiogenic shock it can be associated rapidly with femoral venous cannulation and immediate implementation of the cardiopulmonary bypass if needed.
But cannulation of the femoral artery may prove dangerous. Besides the additional incision in the groin, the retrograde aortic flow during perfusion may displace atheromatous debris or plaques, fibrinous clots, mural thrombus and lead to severe embolic lesions in patients with important atheromatous disease of the thoracic or thoraco-abdominal aorta. But because of the several intimal tears present in the aorta, the most important drawback consists in the possibility of selectively perfusing the false lumen which may dilate and induce some malperfusion syndrome or even aortic rupture.
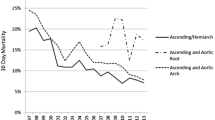
The systematic use of the femoral cannulation was probably one of the reasons why the immediate results of type A aortic dissection surgery were steady or poorly improving during the 80s and early 90s. If we, indeed, look at published reports of this period we may observe that the hospital mortality rate was generally comprised between 15 and 25 % and the strokes rate between 8 and 19 % [2, 3].
However the Yale University group recently published a large experience through which they still advocated the use of femoral cannulation. It is however to be observed that the reported hospital mortality rate was rather high as compared to many contemporary published experiences and that their experience with other mode of cannulation was extremely limited [4].
So, for the many reasons here above mentioned, the technique of femoral cannulation has lost its most prominent hegemony and many groups presently have turned to other modes of arterial access.
Cannulation of the Right Axillary Artery
Reintroduced in the mid-1990s [5], cannulation of the right axillary artery has become more and more popular. It is generally less easy and takes more time than femoral cannulation, particularly in obese patients.
The artery may be approached in the delto-pectoral sulcus or immediately under the right clavicle. At this level the artery is very seldom the site of atheromatous lesions or dissection. However, when it is chosen for cannulation, it is important to check that the innominate artery or the origin of the subclavian artery itself, are not the site of severe lesions.
The skin incision is either vertical in the delto-pectoral sulcus or horizontal following the inferior ridge of the clavicle. After partial division of the major and minor pectoralis muscles the artery is dissected free. The artery is controlled by means of snares and proximally and distally cross-clamped after proper heparinization.
Two techniques are then available.
The artery can be cannulated directly according to the same techniques as for the femoral artery. The main criticism of this method is that the artery may be too small to accept a cannula of adequate diameter to achieve proper arterial inflow during CPB even though most axillary arteries at the level of the clavicle accept an 18-French cannula through which a flow of 4 or 4.5 l/min is easily perfused.
Therefore, many groups cannulate the axillary artery by means of a small Dacron® tube (8 or 10 mm in diameter) implanted end to side on the artery. This technique has the advantage of allowing the use of a larger arterial cannula. It also permits perfusion of the whole right upper limb and control of the arterial pressure in the right radial artery.
It seems that this method, although more time-consuming gives way to improved results. Sabik et al. have published a study in which they compared direct and indirect cannulation of the right axillary artery in two groups of 140 patients each. The rate of local complications was slightly but significantly higher in the direct cannulation group. However there was no difference in terms of hospital mortality and major adverse events [6].
The technique of right axillary artery cannulation has numerous advantages.
As for the femoral artery it can be performed before the opening of the chest. By definition, cannulation of the right axillary artery allows full antegrade arterial inflow in the aorta during the whole duration of CPB. It obviates the need for cannulation changes after completion of the aortic repair. As importantly, if needed, it allows selective antegrade perfusion of the brain through the right carotid artery during the time of arch repair and distal circulatory arrest.
Conversely, it seems that the cannulation of the right axillary artery bears few drawbacks.
It is more time-consuming than the femoral artery cannulation and might be difficult to use in, patients in severe cardiogenic shock or under cardio-pulmonary resuscitation (CPR) in whom emergency is of major importance. As already stated it may be difficult in obese patients. The artery is often thinner and more fragile than the femoral artery and may be easily injured. In addition it is surrounded by important structures such as the axillary vein and its collateral network and the brachial plexus, which must be carefully managed.
Many reports have emphasized the advantages of the right axillary artery cannulation during type A dissection surgery.
Among those, four groups have recently reported their experience and compared the results obtained with femoral and right axillary artery cannulation. The hospital mortality was reduced from a mean of 23 % (19–30 %) with the femoral cannulation to a mean of 6.5 % (5–8 %) with the axillary cannulation [7–10]. Although, obviously, the studies were not randomized the difference seems convincing enough.
Presently it is without any doubt the most praised and possibly the most used technique of arterial approach in surgery of acute type A dissection.
Cannulation of the Right Brachial Artery
This technique described by a Turkish group [11] and, so far, mostly used only by this group can be associated with the technique of right axillary artery cannulation. It is indeed similar and has the same advantages and drawbacks.
In the authors’ description, the artery is approached along the internal border of the biceps just below the armpit. The 6–8 cm long vertical incision is carried down to the fascia of the biceps after identifying its medial border. After opening the aponeurotic sheath and carefully mobilizing the median nerve, the artery is dissected free, controlled on snares and cross-clamped after full heparinization of the patient. A small transverse incision is then carried out and a smooth 16–18 French gauge cannula is directly inserted into the artery.
The main drawback of the brachial artery cannulation is the limited diameter of the artery in many patients, which may prevent from using a large enough cannula. However, although the promoters of the method never suggested it, it could be easy to cannulate the artery through a side branched prosthesis as it is done with the axillary artery.
Cannulation of the Left Axillary Artery
In 1999, Neri and colleagues proposed the use of the left axillary artery [12].
The technique was employed in 20 patients over 10 years.
According to the authors, no axillary artery or brachial plexus injury, and no intraoperative malperfusion were recorded in this series. There were no new postoperative neurologic disorders and two patients (9.1 %) died in the hospital from causes not related to the perfusion technique.
Presently, this is the only published experience of the kind. It is a very limited experience which has not found any support elsewhere.
Indeed, despite the fair results obtained by the authors, it is difficult to find any advantage to this approach as compared to the use of the right axillary artery cannulation as it bears too many uncertainties and drawbacks to be adopted systematically:
-
in addition to having the same drawbacks as the right axillary artery cannulation (difficult in very obese patients, time-consuming, fragility of the vessel, surrounding structures, etc.), it provides antegrade flow to the descending and abdominal aorta but retrograde flow to the arch and ascending aorta;
-
it does not allow cerebral perfusion during the circulatory arrest (except through the left vertebral artery).
Cannulation of the Innominate Artery
Innominate artery cannulation has been used routinely by many groups for a long time but rarely published and therefore not properly advertised.
The technique of cannulation is similar to the one used for the aorta. Two purse string sutures are carried out close to the bifurcation. Tourniquets are put in place. The cannula is introduced through a short arteriotomy. A straight bevelled or angled cannula can be used. In any case the bevelled extremity is oriented downwards to the aorta. Tourniquets are tied as usual. If the innominate vein hampers the access to the artery it may be ligated and divided. This has no clinical consequence, except in a small minority of patients, a slight and transitory swelling of the left arm.
Recently it has been proposed to carry out the innominate artery cannulation through a prosthetic Dacron® tube, implanted laterally on the vessel [13]. Considering the usual size of the innominate artery, the easiness and the safety of direct cannulation, we think that this is unduly complicated and unnecessary.
The technique of innominate artery cannulation has many advantages:
-
The vessel is easily accessible in any circumstances and its approach requires no other incision than sternotomy.
-
In most adults the innominate artery has as diameter of 10–15 mm or even more. It may then easily accept a cannula similar to the ones used for aortic cannulation. The length of this artery (5–7 cm) is also sufficient to allow distal placement of the cannula and, thus, easy cross clamping or division of the vessel near its origin.
-
Alike cannulation of the right axillary artery, cannulation of the innominate artery allows full arterial inflow during CPB.
-
It allows cerebral perfusion through the right carotid artery during the time of circulatory arrest
-
It does not require that the site of arterial cannulation be changed when CPB is resumed after completion of the aortic repair.
Conversely, the innominate artery cannulation has some drawbacks, particularly when used during repair of acute type A dissection:
-
It cannot be carried out before the opening of the sternum;
-
The vessel must be free of any dissecting process or atheroma.
Cannulation of the Carotid Arteries
In 2003 Urbanski and coworkers proposed to use the common carotid arteries as the arterial access [14].
The left common carotid artery was chosen in the majority of the patients. The vessel is approached through a limited cervical vertical incision along the sterno-cleido-mastoidian muscle border. The artery is dissected free and controlled with snares. After full heparinization it is cross-clamped proximally and distally. A small vertical arteriotomy is carried out and an 8 or 10 mm Dacron® or Goretex® prosthesis is sewn end-to-side. The graft is then cannulated and the clamps removed.
In their original article the authors have reported 100 patients including 27 patients suffering from acute type A dissection. The mortality rate was 3.7 % (1 out of 27) in the dissection group and nil in the elective group for an overall mortality rate of 1 %. The stroke rate was 2 %.
This technique seems to have many advantages:
-
The vessel is easily accessible in any circumstances;
-
The vessel is generally less fragile than the right axillary or the brachial arteries;
-
Obviously, cannulation can be carried out before opening the sternum;
-
It allows direct cerebral perfusion;
-
It does not require that the site of arterial cannulation be changed during surgery.
-
Apparently it is very safe.
But the method may have also a certain number of drawbacks that may prevent most groups from adopting it.
In particular, the whole perfusion of the brain through this single approach has been questioned, especially when considering that the authors have generally used the left carotid regardless of the quality of the circle of Willis and through which the vertebral arteries cannot be perfused [14].
To obviate this criticism Urbanski and colleagues have recently published two articles in which they address this issue. In the first report they analyzed preoperatively the morphology of the Circle of Willis in 99 patients undergoing elective aortic arch surgery. Forty patients (40 %) had some abnormality of the vascular anatomy of the brain.
Nevertheless, during unilateral cerebral perfusion, the trans-cranial Doppler showed that the flow velocity in the contro-lateral middle cerebral artery varied in some cases considerably, but the flow never ceased. They concluded that the anatomical status of the circle of Willis does not correlate with functional and intra-operative tests examining the cerebral cross-perfusion [15].
In their second article they compared two groups of 100 patients each, undergoing either right or left carotid artery cannulation [16]. The neurologic disorders rate was 4 % and they could not demonstrate any difference between the two groups. However we may observe that only 42 patients (21 %) had a hemi or total arch replacement and that the mean cerebral perfusion duration was 17 + 2 min. As pointed out by Pacini in his editorial commentary: “For longer periods (of perfusion), could unilateral cerebral perfusion through one carotid be as effective as it was in the present study?” [17].
So, the excellent results obtained by the promoters of this technique need to be confirmed by larger experiences in more centres.
Cannulation of the Ascending Aorta
It may seem paradoxical to propose using the ascending aorta as a cannulation site in acute type A dissection as this segment of the vessel is, by definition, damaged by the dissecting process. Yet, two methods of ascending aortic cannulation have been described recently.
Direct “Regular” Cannulation
The group of Hannover has proposed such an approach in 2003 [18].
After median sternotomy and pericadiotomy, the cannulation site is cautiously determined on a non-dissected or less dissected aortic area by means of palpation and trans-esophageal echocardiography. The aorta is then cannulated on the chosen safe area using double-purse-string sutures as in regular non-dissected patients. The aortic cannula is inserted carefully and under control of trans-esophageal echo in order to get sure that it is placed in the true channel.
After cannulation of the right atrium, Cardiopulmonary bypass (CPB) is initiated and the patient cooled down to the target temperature. The quality of the arterial perfusion is assessed by pressure monitoring in both radial arteries and one femoral artery, as well as bilateral cerebral oxygen saturation monitoring. After reaching the anticipated HCA temperature, CPB is stopped, the aorta is opened, and the arterial cannula removed. The ascending aorta is opened, cardioplegia given through the coronary ostia. Two balloon cannulas are placed in the orifices of the innominate and left common carotid arteries and Selective Antegrade Cerebral Perfusion started. After completing the distal repair, systemic CBP is resumed through cannulation of a side branch of the prosthesis.
Following the initial publication, the technique has been adopted by several other groups, mainly in Japan. It has indeed the advantages of providing a direct and immediate antegrade flow in the aorta.
But the method has many drawbacks:
-
The cannulation cannot be carried out before the opening on the sternum;
-
In a certain number of patients the ascending aorta and proximal arch are completely and circumferentially dissected which precludes any possibility of implanting the cannula on those segments;
-
The very fragile adventitia may rupture during the completion of the purse-string sutures even though those are supposed to be placed in a safe area.
-
The tip of the cannula might be placed in the false lumen through a secondary intimal tear;
-
It requires a period of total circulatory arrest while the arch is opened and the SACP implemented;
-
It requires switching the arterial cannula after completion of the distal repair;
-
De-airing before resuming CPB might be difficult.
Recently, several reports were published by groups using the direct aortic cannulation technique. In some articles the technique was compared to a previous experience with femoral cannulation. The results were obviously improved as the mean hospital mortality rate was reduced from 17 % (8–23 %) with the femoral cannulation to 8 % (3–15 %) with the aortic cannulation [19–22]. Inoue and coworkers obtained the best results but their technique is extremely complicated, starting with femoral cannulation and then switching to the aorta and again to a side graft of the prosthesis. In addition it is a limited experience and it is to note that even though they had no clinical end-organ malperfusion the cannula was placed in the false lumen in 12.5 % of the patients [23, 24].
Direct “True Lumen” Cannulation
In 2007, Jakob and colleagues proposed to directly insert the arterial cannula into the true lumen after making a limited aortotomy on the anterior wall of the dissected ascending aorta [25].
The authors described the technique as follows:
After opening of the pericardium, a purse-string suture is placed to the right atrial appendage for venous cannulation. Immediate venous exsanguination to gravity into a standard integrated oxygenator reservoir is started with the patient oxygenated with 100 % inspired oxygen fraction over several minutes. Within 45 seconds, 3.5 to 4.5 L of blood volume is withdrawn and the ascending aorta starts collapsing, indicating low cardiac filling. Arterial systolic pressure at that time is 30 mm Hg or less. With the patient placed head down, a mid-aortic (usual adventitial) incision is made on the convex side of the ascending aorta with 1 or 2 suction devices in place. Usually, the true lumen sac is rapidly identified. In case the entry tear is located at this site, the true lumen is grasped and inspected. In case of an intact true lumen sac, a 2- to 3-cm incision is made upstream for intraluminal inspection. Then a straight cannula is inserted into the true lumen under direct vision, connected to the arterial line of the extracorporeal circuit, and open low-flow perfusion (300–400 mL/min) is immediately started. While the lungs are being inflated manually, rapid deairing of the aortic arch and ascending aorta under direct visual control is possible, followed by oblique aortic crossclamping directly adjacent and tight to the arterial cannula. This allows rapid institution of full flow and cooling of the patient to the target core temperature, usually without the necessity of an additional purse string suture fixation. This process takes less than 90 seconds [25].
In their report the authors insist on the advantages of their method:
-
It provides a rapid and safe antegrade perfusion of the whole aorta;
-
Therefore, the rate of neurologic disorders might be reduced;
-
It may be the best resort when patients are in severe cardiogenic shock and need very rapid straightforward arterial cannulation.
Nevertheless and needless to say, this technique appears quite intriguing and somewhat dangerous as it may encompass many drawbacks:
-
As all techniques implying opening the chest first, it cannot be implemented before the sternotomy;
-
The necessary massive exsanguination of the patient before the aortic cannulation may severely worsen the poor hemodynamic condition and peripheral organ perfusion in shocked patients;
-
The blood tightness around the cannula is obtained either with a lateral clamp or with a snare passed around the vessel. In many experiences, such a method has been proven to be rather uncertain due to the presence of the two channels and the intimal flap obviating a total safe occlusion. Therefore, the operating field might be flooded when the full CPB flow is resumed;
-
As for the other technique of aortic cannulation, the cannula must be switched to another site of cannulation after completion of the distal aortic repair to resume full flow CPB. Therefore the difficulty in de-airing and the danger of air embolism are increased;
-
During circulatory arrest some method of cerebral protection is necessary. This can only be provided through either profound hypothermia with or without retrograde cerebral perfusion or selective antegrade perfusion (SACP), implying the cannulation of either the innominate or the left common carotid artery or both vessels.
Conzelmann and colleagues recently published a report about their experience with 29 patients operated on for acute type A dissection using a similar technique. The only small technical difference with Jakob’s technique was the systematic use of the snare around the ascending aorta to secure the cannula and to maintain blood tightness.
There was no hospital mortality. Severe cerebral hypoxia occurred in two patients (7 %). Temporary hemiplegia occurred in four patients (14 %). No case of intraoperative malperfusion could be observed. The authors conclude that “direct true lumen cannulation is a promising surgical cannulation technique for emergency surgery in type A aortic dissection with good results. It is a simple, quick, and safe method to provide antegrade flow through the true aortic lumen”.
It is, however, noteworthy that the technique has been used in only two centres, so far, and that the experience was quite limited in time and number of patients. Larger and broader experiences are needed before accurately assessing the usefulness and quality of the method.
Cannulation of the Left Ventricular Apex
Although this technique has been known for several decades, in particular for pediatric patients, the systematic use of the left ventricle apex to insert a cannula into the ascending aorta through the aortic valve has been recently updated and proposed by Wada and co-workers [26].
After sternotomy and opening of the pericardium, a bicaval cannulation is performed for venous drainage. Then the heart is manually shifted towards the right and the apex is raised upwards. A 1-cm incision is made in the apex of the left ventricle without purse-string suture, and a 7-mm cannula is passed through the apex and across the aortic valve until positioned in the ascending aorta. The position in the true lumen is assessed by trans-esophageal echocardiographic guidance. When the tip of the cannula is properly located in the ascending aorta and in the true lumen, full flow CPB is started.
It certainly provides a good antegrade perfusion but seems to have several important drawbacks.
-
In addition to the fact that it cannot be implemented before the chest is opened, the most worrisome feature is that, in order to introduce the cannula in the apex, the heart has to be lifted and turned to the right which automatically would impair seriously the often already unstable hemodynamic condition of the patient.
-
As with ascending aortic cannulation, this technique requires removal of the arterial cannula during the aortic repair and cannulation of a new site after completion of the repair.
-
It does not allow cerebral perfusion during the aortic repair and must be associated to another mode of cerebral protection (SACP with cannulation of the supra aortic vessels or profound hypothermia).
-
In elderly patients, the repair of the left ventricle after removing the cannula might be somewhat difficult due to the fragility of the left ventricle tissues.
In their initial article that reports the largest experience published so far, the authors indicate that there were no cases in which conversion to another site of cannulation was ever necessary and that, in all cases, CPB flow was sufficient (>2.5 L/m−2/min−1). There were no malperfusion events. However the hospital mortality rate amounted to 19 % and the stroke rate to 6 %. We may observe that those results were not inferior to the average ones generally published with femoral cannulation.
Conclusion
So, after this apparently complete review of the various methods, how can we decide which is the best? This is the real core of the debate.
Cannulation of the femoral arteries has been the conventional method during decades and is, perhaps, still the most used.
However, even though it has taken three decades to the surgical community to realize it, it became obvious in the mid 90s that it could be dangerous and was the cause of, embolism, malperfusion syndromes, aortic ruptures and, therefore, responsible partly for the high mortality and morbidity rates.
So, about 15 years ago, cannulation of the right axillary artery has been proposed.
It was rapidly adopted by many centres and has proven to be efficient and safe. Together with cannulation of the innominate artery and the carotid artery cannulation, it is the only technique allowing permanent antegrade perfusion of the aorta and perfusion of the brain, without necessity for switching the cannula after completion of the repair. It is one method which has provided satisfactory and consistent results on a very large scale.
It appears presently as the method of choice, and has become more and more popular.
Many other methods have been proposed. Most of those have been used in a limited number of centres and patients. Their efficacy and safety need to be assessed through larger experiences.
However, all contemporary methods must respect one essential principle: allowing antegrade perfusion flow in the aorta. This apparently simple feature probably explains partly the dramatic improvement of the results of type A dissection surgery in recent years as it has certainly dramatically reduced the prevalence of severe intraoperative malperfusion syndromes.
So, most of the described sites and techniques have advantages and disadvantages (Table 9.1).
That’s why each one has its strong supporters and, similarly, strong opponents.
Yet, it seems presently largely demonstrated that some advantages are of paramount importance that might induce surgeons to use preferentially some techniques rather than others.
Those advantages are:
-
The perfusion of the whole aorta antegradely;
-
The possibility of getting an arterial access before opening the chest;
-
The surgical easiness and simplicity of the technique;
-
Hence, the rapidity of implementing the CBP;
-
The immediate possibility of perfusing the brain;
-
The non-necessity for removal the arterial cannula during the aortic repair or cannulating another arterial site after completion of the repair.
No technique combines all those advantages with no drawbacks. Therefore it seems important that the surgical teams be aware of the various technical methods and decides the most convenient and less harmful type of arterial access for each case according to the patient’s morphology, hemodynamic condition, anatomical and physiological lesions and impairment as well as their experience, skill, and local possibilities. No technique should be considered as the one and only.
References
Bonser RS, Ranasinghe AM, Loubani M, Evans JD, Thalji NMA, Bachet E, Carrel TP, Czerny M, Di Bartolomeo R, Grabenwöger M, Lonn L, Mestres MA, Schepens MAAM, Weigang E. Evidence, lack of evidence, controversy, and debate in the provision and performance of the surgery of acute type a aortic dissection. J Am Coll Cardiol. 2011;58:2455–74.
Bachet J, Goudot B, Dreyfus GD, Brodaty D, Dubois C, Delentdecker P, Guilmet D. Surgery for acute type A aortic dissection: the Hopital Foch experience (1977–1998). Ann Thorac Surg. 1999;67:2006–9.
Niederhäuser U, Rüdiger H, Künzli A, Seifert B, Schmidli J, Vogt P, Turina M. Surgery for acute type A aortic dissection: comparison of techniques. Eur J Cardiothorac Surg. 2000;18:307–12.
Fusco DS, Shaw RK, Tranquilli MT, Kopf GS, Elefteriades JA. Femoral cannulation is safe for type A dissection repair. Ann Thorac Surg. 2004;78:1285–9.
Sabik JF, Lytle BW, McCarthy PM, Cosgrove DM. Axillary artery: an alternative site of arterial cannulation for patients with extensive aortic and peripheral vascular disease. J Thorac Cardiovasc Surg. 1995;109:885–90.
Sabik JF, Nemeh H, Lytle BW, Blackstone EH, Gillinov AM, Rajeswaran J, Cosgrove DM. Cannulation of the axillary artery with a side-graft reduces morbidity. Ann Thorac Surg. 2004;77:1315–20.
Pasic M, Schubel J, Bauer M, Yankah C, Kuppe H, Weng Y-G, Hetzer R. Cannulation of the right axillary artery for surgery of acute type A aortic dissection. Eur J Cardiothorac Surg. 2003;24:231–6.
Moizumi Y, Motoyoshi N, Sakuma K, Yoshida S. Axillary artery cannulation improves operative results for acute type A aortic dissection. Ann Thorac Surg. 2005;80:77–83.
Reuthebuch O, Schurr U, Hellermann J, Prêtre R, Künzli A, Lachat M, Turina M. Advantages of subclavian artery perfusion for repair of acute type A dissection. Eur J Cardiothorac Surg. 2004;26:592–8.
Etz CD, Plestis KA, Kari FA, Silovitz D, Bodian CA, Spielvogel D, Griepp RB. Axillary cannulation significantly improves survival and neurologic outcome after atherosclerotic aneurysm repair of the aortic root and ascending aorta. Ann Thorac Surg. 2008;86:441–7.
Tasdemir O, Saritas A, Kucuker S, Ozatik MA, Sener E. Aortic arch repair with right brachial artery perfusion. Ann Thorac Surg. 2002;73:1837–42.
Neri E, Massetti M, Capannini G, Carone E, Tucci E, Diciolla F, Prifti E, Sass C. Axillary artery cannulation in type A aortic dissection operations. J Thorac Cardiovasc Surg. 1999;118:324–9.
Di Eusanio M, Quarti A, Pierri MD, Di Eusanio G. Cannulation of the brachiocephalic trunk during surgery of the thoracic aorta: a simplified technique for antegrade cerebral perfusion. Eur J Cardiothorac Surg. 2004;26:831–83.
Urbanski PP. Cannulation of the left common carotid artery for proximal aortic repair. J Thorac Cardiovasc Surg. 2003;126:887–8. Discussion: 889.
Urbanski PP, Lenos A, Blume JC, Ziegler V, Griewing B, Schmitt R, Diegeler A, Dinkel M. Does anatomical completeness of the circle of Willis correlate with sufficient cross-perfusion during unilateral cerebral perfusion? Eur J Cardiothorac Surg. 2008;33:402–8.
Urbanski PP, Lenos A, Zacher M, Diegeler A. Unilateral cerebral perfusion: right versus left. Eur J Cardiothorac Surg. 2010;37:1332–6.
Pacini D. How really safe is unilateral selective cerebral perfusion? Eur J Cardiothorac Surg. 2010;37(6):1336–7.
Minatoya K, Karck M, Szpakowski E, Harringer W, Haverich A. Ascending aortic cannulation for Stanford type A acute aortic dissection: another option. J Thorac Cardiovasc Surg. 2003;125:952–3.
Reece TB, Tribble CG, Smith RL, Singh RR, Stiles BM, Peeler BB, Kern JA, Kron IL. Central cannulation is safe in acute aortic dissection repair. J Thorac Cardiovasc Surg. 2007;133:428–34.
Inoue Y, Ueda T, Taguchi S, Kashima I, Koizumi K, Takahashi R, Kiso I. Ascending aorta cannulation in acute type A aortic dissection. Eur J Cardiothorac Surg. 2007;31:976–81.
Khaladj N, Shrestha M, Peterss S, Strueber M, Karck M, Pichlmaier M, Haverich A, Hagl C. Ascending aortic cannulation in acute aortic dissection type A: the Hannover experience. Eur J Cardiothorac Surg. 2008;32:792–7.
Kamiya H, Kallenbach K, Halmer D, Özsöz M, Ilg K, Lichtenberg A, Matthias KM. Comparison of ascending aorta versus femoral artery cannulation for acute aortic dissection type A. Circulation. 2009;120:S282–6.
Suzuki T, Asai T, Matsubayashi K, Kambara A, Kinoshita T, Hiramatsu N, Nishimura O. Safety and efficacy of central cannulation through ascending aorta for type A aortic dissection. Interact Cardiovasc Thorac Surg. 2010;11:34–7.
Bachet J. Editorial comment: ascending aorta cannulation in acute type A aortic dissection. Eur J Cardiothorac Surg. 2007;31:979–81.
Jakob H, Tsagakis K, Szabo A, Wiese I, Thielmann M, Herold U. Rapid and safe direct cannulation of the true lumen of the ascending aorta in acute type A aortic dissection. J Thorac Cardiovasc Surg. 2007;134:244–5.
Wada S, Yamamoto S, Honda J, Hiramoto A, Wada H, Hosoda Y. Transapical aortic cannulation for cardiopulmonary bypass in type A aortic dissection operations. J Thorac Cardiovasc Surg. 2006;132:369–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Bachet, J. (2014). Arterial Cannulation in Type A Acute Aortic Dissection: The Debate. In: Bonser, R., Pagano, D., Haverich, A., Mascaro, J. (eds) Controversies in Aortic Dissection and Aneurysmal Disease. Springer, London. https://doi.org/10.1007/978-1-4471-5622-2_9
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5622-2_9
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5621-5
Online ISBN: 978-1-4471-5622-2
eBook Packages: MedicineMedicine (R0)