Abstract
Proximal acute aortic dissection [type A] remains a disease with a poor prognosis. High peri-operative open surgical mortality and a significant turn-down rate contribute towards the poor prognosis. Thoracic endovascular stent grafting has revolutionized the treatment of distal [type B] acute aortic dissection. Endovascular therapy may now offer a potential treatment for some patients with type A dissection. Less invasive endovascular therapy, obviates the need for sternotomy and cardiopulmonary bypass, may reduce perioperative morbidity and offers a solution for those patients declined conventional intervention due to co-morbidity or severe complications of the disease. Thoracic stent grafting in the ascending aorta presents specific challenges due to proximity to the aortic valve, navigation over the steep aortic arch and pulsatile aortic movement. The experience of treating Type A dissection with endovascular techniques has evolved slowly but there are now a number of successful case reports in this field.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Type A acute aortic dissection [TAAD] is a catastrophic arterial insult with significant mortality and morbidity associated with open surgical therapy. Although surgical results have improved with modern techniques, enhanced cardiopulmonary bypass, cerebral protection, biologic glue and tailored postoperative surveillance, overall in-hospital mortality remains as high as 30 % [1]. One of the most important, although rarely addressed issues with acute Type A dissection, is the number of patients who are considered unfit for open surgical repair. This figure may reach 30–40 %, and this is probably an underestimate as it does not include patients turned down for surgery at the point of referral [2]. The in-hospital mortality for patients managed medically is dismal (59 % die without leaving hospital) [3].
Endovascular solutions have become the preferred management of many complex aortic diseases, and TEVAR is now considered my many to be the primary treatment modality for patients with aneurysms of the descending thoracic aorta, acute complicated Type B aortic dissection and traumatic aortic injury. The ascending aorta represents the new endovascular frontier [4] and clearly there is a requirement for improved outcomes in TAAD. In this chapter the possible role of endovascular solutions to TAAD is explored.
Epidemiology
The reported estimates of thoracic aortic dissection [TAD] are 2.9–4.3 cases per 100,000 persons per year. Approximately two-thirds of TADs involve the ascending aorta [Stanford type A]. The incidence appears to be rising, although this may simply be a function of improved diagnostic imaging. TAAD is more common in men, with an average age at onset of 61 years. The principle risk factors are hypertension, aortic dilatation, congenital cardiovascular defects and hereditary connective tissue disorders [e.g. Marfan’s]. A feature of acute aortic syndrome, it is likely that the incidence of TAAD will increase as emergency departments utilise more cross sectional imaging and patients are more rigorously investigated.
Current Gold Standard
Open surgical repair remains the gold standard treatment TAAD, and is likely to remain so for the majority of patients. Independent preoperative predictors of mortality include advancing age, prior cardiac surgery, hypotension on presentation, and myocardial ischaemia [5]. A significant proportion of patients are considered inappropriate candidates for surgical repair as their pre-operative state predicts a poor outcome from surgery.
The Place for an Endovascular Solution
Thoracic endovascular repair [TEVR] of complicated type B aortic dissections [TBAD] has revolutionised the management of this disease [6–9]. The reduced physiological insult associated with this minimally invasive technique has transformed the perioperative outcomes for TBAD. Experience gained from TEVR for TBAD and the ever increasing complexity of aortic disease treated endovascularly has led a natural progression around the aortic arch, with hybrid and totally endovascular solutions being described [10]. The early results of endovascular repair of complex aortic arch pathology have been reasonable and appear to demonstrate proof of concept. Long term results however remain largely undefined.
With the success of TEVR, new applications have been sought for this technology. One area of potential interest is the ascending aorta. Several pathologies may be candidates for endovascular treatment including isolated ascending aortic aneurysms, cannulation site false aneurysms and some Type A dissections. The anatomical and physiological challenges to endovascular therapy of the ascending aorta remain formidable and include:
-
Proximal fixation close to the aortic valve and coronary ostia
-
Distal fixation which may impinge on the innominate artery
-
Curvature of the distal ascending aorta
-
Sizing discrepancies in pathological conditions
-
Haemodynamic forces in this arterial segment
-
Potential for fatal retrograde dissection
-
Potential for disruption of the aortic valve
-
Potential damage to the left ventricle with ventricular perforation
-
Difficulties in access through a tortuous iliac and thoracic aortic segment
Many of the technical challenges are the same as encountered in percutaneous aortic valve therapy, which have been overcome with dedicated endovascular equipment and knowledge of anatomical constraints to valve delivery [11].
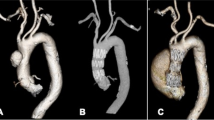
Morphological Suitability
Endovascular suitability is dependent on adequate access vessels, appropriately sized proximal and distal landing zones, and luminal diameter compatible with available stent-grafts. In acute dissection additional exclusions to endovascular repair include disturbed aortic valve function and prior coronary revascularisation. The principle determinant of suitability is the location of the primary proximal entry tear. This must lie a minimum of 20 mm distal to the sino-tubular junction to allow stent coverage of the flap whilst maintaining coronary blood flow. The mean distance, representing the safe landing zone, from sinotubular junction to innominate artery ostia is reported to be 63.4 ± 10.2 mm [12].
Two studies have explored the feasibility of endovascular repair of TAAD based purely on cross-sectional imaging. They report that, based on current device designs 32–50 % of patients currently undergoing open repair for TAAD could potentially be candidates for endovascular repair, from a purely technical perspective [13, 14].
Clearly, in the future, specific endografts will be designed and used for the ascending aorta. In our practice a dedicated ascending aortic endografts has been developed with Cook Medical. The nitinol based stent graft has features specifically designed for use in this challenging anatomy:
-
A delivery system capable of delivering the stent to the ascending aorta from a femoral route
-
A tip capable of atraumatic entry to the left ventricle
-
Stable delivery with accurate placement
-
Length and diameter compatible with the ascending aorta
Specific Challenges and Solutions
The anatomical and physiological challenges to endovascular therapy of the ascending aorta remain formidable. They include proximal graft fixation close to the aortic valve and coronary ostia and a distal landing zone that may impinge on the innominate artery. The steep curvature of the distal ascending aorta and the sizing discrepancies found in acute pathology highlight the requirement for pathology-specific grafts. The haemodynamic forces in the ascending aorta resist accurate graft deployment, whilst the distal cone of current grafts prohibits deployment close to the aortic valve. Accurate device control and deployment is hindered by loss of torque control through tortuous iliac vessels into the 270° aortic arch.
Technique
Meticulous planning is essential. ECG-gated contrast enhanced CT images, to minimise motion artefact, should be examined on dedicated vascular workstations. All measurements should be based on centreline-of-flow reconstructions. Preoperative echocardiography is essential to detect aortic valve insufficiency or regurgitation. It also allows accurate measurement of distance between dissection entry tear and coronary ostia. Grafts are over-sized 5–10 % relative to the native true lumen to minimise aortic trauma.
Planning of the access route is essential. The transfemoral route is preferred but if there are difficulties in the iliac access vessels the subclavian or carotid route may be utilised. There have been suggestions that in the future, a transapical or transeptal route may be used. In our early experience, surgery has been performed under general anaesthesia. At deployment of the endograft the cardiac output must be managed to reduce the haemodynamic displacement forces. In our practice overdrive pacing is used for this purpose. Serial angiography is performed to ensure accurate deployment and patency of the coronary arteries and supra-aortic trunks. Ballooning of the endograft is not recommended.
Particular Risks
There are additive risks when operating further round the aortic arch, particularly with the increased instrumentation, requirement for reduced systemic blood pressure at deployment and proximity to the aortic valve [15]. Stroke is perhaps the most catastrophic complication; the risks increase with more proximal procedures [16]. This may occur as a consequence of instrumentation around the diseased aortic arch or extension of the dissection into the supra-aortic branches.
The fragility of the aortic wall exposes patients to potentially fatal retrograde dissection [RTAD] into the coronary vessels or rupturing into the pericardium. RTAD may also be related to proximal bare springs of the endografts and overall stiffness of the endoprosthesis relative to the mobile pulsating ascending aorta [17]. These factors are relevant when designing future ascending aortic devices; making them compliant and flexible to interact with the aortic wall with an atraumatic proximal fixation. There is a clear requirement for a novel stent configuration to meet the diverse biomechanical forces and match the morphology.
Operating so close to the heart exposes the patient to wire and/or device trauma to the aortic valve or left ventricle. Cardiac trauma can be minimised by delivery systems with enhanced trackability and conformation, and accurate wire control throughout the procedure. This issue further highlights the requirement for custom ascending aortic devices without the long nosecones of traditional thoracic endoprostheses. Extra stiff short atraumatic wires with floppy tips, capable of sitting in the left ventricle, will enhance safety at deployment.
Current Series/Case Reports
The first case report of complete endovascular treatment of TAAD was published in 2004. Infra-aortic endovascular cuffs have generally been used as they are short enough not to cover the innominate artery, although they are limited by relatively short delivery systems. This represents an off-licence use, and therefore should only be used when all alternative options have been exhausted. The first report utilising a made-for-purpose Zenith ascending dissection device was published in 2011 [11]. These devices, specific to the ascending aorta, are undergoing proof of concept studies and offer the first glimpse of a robust endovascular solution with broad applicability. All the case reports of endovascular management of TAAD describe successful outcome beyond 30-days; none report any significant perioperative morbidity. A more realistic description of the likely risks of this procedure is described in the Chinese series of Ye et al. In their series of mixed acute and chronic ascending dissections they experienced a 20 % stroke rate and 10 % 30-day mortality [18].
Future Developments
It is becoming apparent that different aortic pathologies require diverse stent-graft solutions. Off-licence techniques such as using aortic cuffs for TAAD are likely to compromise outcomes and are unlikely to offer a robust solution. Experience with specific ascending aortic devices will clarify understanding of the behaviour of these devices in the ascending aorta, and through entering cases into registries, document their durability and applicability. Equally registries should gather data on all cases turned-down for surgical treatment. This would further clarify the demand for an endovascular solution.
A new generation of lower profile thoracic devices [16Fr] are set to be launched. This would permit a left axillary artery approach to be taken, reducing the distance between access and disease and facilitating more precise deployment.
Conclusions
Endovascular development may offer a therapeutic modality for cases of surgically untreatable type A dissection. Proof of concept studies are in progress using stent-grafts designed specifically for the ascending aorta. Vascular surgeons, cardiologists and cardiothoracic surgeons should be encouraged to recruit patients that are ineligible for open surgery to these studies. It is inevitable that in the future thoracic endovascular surgeons will become integral to the multidisciplinary team caring for patients with TAAD as they have for type B dissection.
References
Tsai TT, Evangelista A, Nienaber CA, Trimarchi S, Sechtem U, Fattori R, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114(1 Suppl):I350–6.
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903.
Trimarchi S, Eagle KA, Nienaber CA, Rampoldi V, Jonker FH, De Vincentiis C, et al. Role of age in acute type A aortic dissection outcome: report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140(4):784–9.
Chuter TA. Endovascular repair in the ascending aorta: stretching the limits of current technology. J Endovasc Ther. 2007;14(6):799–800.
Rampoldi V, Trimarchi S, Eagle KA, Nienaber CA, Oh JK, Bossone E, et al. Simple risk models to predict surgical mortality in acute type A aortic dissection: the International Registry of Acute Aortic Dissection score. Ann Thorac Surg. 2007;83(1):55–61.
Dake MD, Kato N, Mitchell RS, Semba CP, Razavi MK, Shimono T, et al. Endovascular stent-graft placement for the treatment of acute aortic dissection. N Engl J Med. 1999;340(20):1546–52.
Nienaber CA, Fattori R, Lund G, Dieckmann C, Wolf W, von Kodolitsch Y, et al. Nonsurgical reconstruction of thoracic aortic dissection by stent-graft placement. N Engl J Med. 1999;340(20):1539–45.
Cambria RP, Crawford RS, Cho JS, Bavaria J, Farber M, Lee WA, et al. A multicenter clinical trial of endovascular stent graft repair of acute catastrophes of the descending thoracic aorta. J Vasc Surg. 2009;50(6):1255–64. e1–4.
Eggebrecht H, Nienaber CA, Neuhauser M, Baumgart D, Kische S, Schmermund A, et al. Endovascular stent-graft placement in aortic dissection: a meta-analysis. Eur Heart J. 2006;27(4):489–98.
Holt PJ, Johnson C, Hinchliffe RJ, Morgan R, Jahingiri M, Loftus IM, et al. Outcomes of the endovascular management of aortic arch aneurysm: implications for management of the left subclavian artery. J Vasc Surg. 2010;51(6):1329–38.
Metcalfe MJ, Karthikesalingam A, Black SA, Loftus IM, Morgan R, Thompson MM. The first endovascular repair of an acute type A dissection using an endograft designed for the ascending aorta. J Vasc Surg. 2012;55:220–2.
Malkawi AH, Hinchliffe RJ, Yates M, Holt PJ, Loftus IM, Thompson MM. Morphology of aortic arch pathology: implications for endovascular repair. J Endovasc Ther. 2010;17(4):474–9.
Moon MC, Greenberg RK, Morales JP, Martin Z, Lu Q, Dowdall JF, et al. Computed tomography-based anatomic characterization of proximal aortic dissection with consideration for endovascular candidacy. J Vasc Surg. 2011;53(4):942–9.
Sobocinski J, O’Brien N, Maurel B, Bartoli M, Goueffic Y, Sassard T, et al. Endovascular approaches to acute aortic type A dissection: a CT-cased feasibility study. Eur J Vasc Endovasc Surg. 2011;42(4):442–7.
Chiesa R, Melissano G, Tshomba Y, Civilini E, Marone EM, Bertoglio L, et al. Ten years of endovascular aortic arch repair. J Endovasc Ther. 2010;17(1):1–11.
Melissano G, Tshomba Y, Bertoglio L, Rinaldi E, Chiesa R. Analysis of stroke after TEVAR involving the aortic arch. Eur J Vasc Endovasc Surg. 2012;43:269–75.
Dong ZH, Fu WG, Wang YQ, da Guo Q, Xu X, Ji Y, et al. Retrograde type A aortic dissection after endovascular stent graft placement for treatment of type B dissection. Circulation. 2009;119(5):735–41.
Ye C, Chang G, Li S, Hu Z, Yao C, Chen W, et al. Endovascular stent-graft treatment for Stanford type A aortic dissection. Eur J Vasc Endovasc Surg. 2011;42(6):787–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Nordon, I.M., Thompson, M.M. (2014). The Prospects for Total Endovascular Repair of Acute Type A Aortic Dissection. In: Bonser, R., Pagano, D., Haverich, A., Mascaro, J. (eds) Controversies in Aortic Dissection and Aneurysmal Disease. Springer, London. https://doi.org/10.1007/978-1-4471-5622-2_16
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5622-2_16
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5621-5
Online ISBN: 978-1-4471-5622-2
eBook Packages: MedicineMedicine (R0)