Abstract
Surgical treatment strategies for acute type A aortic dissection continue to evolve. Proximal reconstruction typically involves aortic valve resuspension with preservation of the aortic root, unless the tear site extends into the aortic root. Although there is strong consensus on proximal aortic reconstruction strategy, open distal aortic reconstruction as a transverse hemiarch replacement under circulatory arrest is still not adopted by many groups, even though evidence supports for this distal reconstructive strategy. In addition to proximal and distal aortic stabilization, one of the essential aspects of repair remains reapposition of the dissection flap in the aortic root and the ascending aorta. To this effect, there is literature supporting for many techniques, including placement of adhesives into the dissection flap and/or placement of felt material in the dissection flap to reappose the intima, media and the adventia of the dissected aorta. But overall, there is no clear consensus on the ideal technique for apposition of the dissection flap.
In this chapter, we review various distal reconstructive strategies for type A aortic dissection, with a focus on the role for transverse hemiarch open distal aortic reconstruction. We also review the current literature on the use of adhesives such as glue products for aortic reconstruction. Finally, we discuss our institutional bias for proximal and distal aortic reconstruction of type A aortic dissection, and our typical practice in the use of felt material/adhesives for treating the proximal aortic root and distal aortic arch dissection flap.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Acute type A dissection remains one of the most lethal and challenging operative emergencies facing cardiothoracic surgeons. Over the past 20 years, significant improvements with regards to cardiopulmonary bypass, myocardial protection and cerebral perfusion strategies have improved overall and longterm survival in patients presenting with acute type A aortic dissection. Regardless, there are still some fundamental, contentious issues with regards to the operative strategy for this disease. Due to the lack of randomized, controlled trials in dealing with this acute condition, several issues in the operative management of this disease are yet to be truly defined.
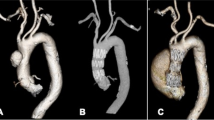
Various strategies have shown variable results in the hands of surgeons at different institutions. Additionally, the disease process can present with a wide range of acute symptoms extending from subclinical presentation, to mild chest pain, to cardiac tamponade, to cerebral malperfusion and visceral malperfusion syndromes. Also, the anatomical presentation of this disease can be quite variable, and this often predicts the severity of the disease process and post operative and long-term outcome. Anatomic presentation can vary from straightforward DeBakey II dissection involving the ascending aorta only, to complex DeBakey I presentation, with great vessel dissection/involvement and multiple dissection flaps in the arch, descending thoracic aorta, or the aortic root. Given this complexity of clinical and anatomical presentation, one can understand why outcomes with this disease can be variable.
Given these issues, evidence based analysis is difficult with regards to this disease process as the patient population differs significantly, as do the surgical methods and the surgical experience. To our knowledge there is no meta-analysis available dividing the patients into subgroups of aortic dissection and analyzing outcomes. Therefore, even though there is general consensus among the surgical community regarding the proximal reconstruction needed for aortic dissection, the distal reconstruction strategy remains undefined with different outcomes reported by different institutions.
For proximal reconstruction of a DeBakey I or II aortic dissection, not involving a right or left coronary sinus, the coronary vessels or the aortic annulus, operative strategy typically involves an aggressive resection with over-sewing of the dissected flap at the sinotubular junction with a tube graft anastomoses at the proximal end. If the sinus is not dilated and the aortic valve is competent, the aortic root is left alone. In situations where the aortic root is aneurismal or dissected, an aortic root replacement or valve sparing aortic root reimplantation is recommended. This decision between a root replacement or a valve sparing root reimplantation should be made based on several factors including patient age, co morbid status, acuity of dissection, preoperative cardiac function, the feasibility of valve reimplantation, and the overall patient clinical and hemodynamic status [1].
Distal reconstructions for DeBakey I and II dissections have ranged from ascending aorta replacement with the cross clamp in place to an extensive total arch replacement with a frozen elephant trunk operation. There are no randomized trials or meta-analysis to strongly advocate one type of distal reconstructive procedure over another. There is a general consensus and mounting evidence to suggest the extent of the aggressiveness of the approach should be based on the anatomy of the dissection I tear site.
In this chapter we will review the reconstructive strategies for proximal and distal aortic reconstruction in DeBakey I and II dissection repair with a specific focus on the extent of the distal reconstruction to be pursued and its related outcomes. Given the variability of the reported outcomes in the literature, we will also include our own institutional biases in the management of this complex disease process.
Another topic that has been periodically debated in the past 20 years in the management of aortic dissection has been the use of adhesives/glue products for proximal and distal reconstruction suture lines. Typically this strategy has been employed for two primary reasons: [1] Poor tissue noted during the operation leads to attempts to have proper sealing anastomoses with low postoperative bleeding and reoperation rates [2]. Glue products have been utilized in order to promote false lumen thrombosis and may improve long term and immediate outcomes in this difficult patient population.
As the literature with regards to the distal reconstruction in aortic dissection repair is somewhat undefined, the literature with the regards to the utility of glue products in aortic dissection repair is even more contentious [2]. Several institutions, primarily in Europe and Japan, have shown variable outcomes with regards to use of glue in aortic dissection repair. Results have varied from demonstrating decreased postoperative bleeding rates, decreased transfusion rates, and improved long term mortality and morbidity to results at the other end of the extreme- tissue necrosis at the site of glue placement, pseudo-aneurysm formation and worse long term outcomes [3–5]. Given this confusing evidence, this report will include some of the findings noted within the literature with a few notes regarding our institutional practice.
Operative Strategy in Aortic Dissection Repair
At our institution we assessed all type A aortic dissection cases using the DeBakey classification. For dissection confined to the ascending aorta (DeBakey II dissections) the management strategy is more straightforward than DeBakey I dissections, where the extent of the dissection includes the ascending aorta and the descending thoracic aorta. Of note, DeBakey I dissections are almost three times more frequent than DeBakey II dissections [6]. Typically the primary intimal tear is located in the ascending aorta in 75–80 % of the cases, followed by the transverse aorta in 10–15 % of the cases. The descending thoracic aorta is the least common site of the primary intimal tear (2 %) [7, 8].
In almost all patients presenting with acute type A aortic dissection the treatment of choice still remains an operation unless significant co-morbidity prevents surgical intervention. Of note, patient’s age and re-operative cardiac surgery should not be factors preventing needed surgical intervention. Even though the operative mortality of aortic dissection repair ranges from 12 to 30 %, surgical intervention still has superior outcomes to non-operative management (up to 60 % in-hospital mortality). Patients with evidence of hemodynamic collapse, aortic rupture, cardiac tamponade, cardiac ischemia, coronary or cerebral malperfusion, visceral malperfusion and limb ischemia, have increased risk of mortality during this operation due to these risk factors. Nonetheless, even in this patient population, operative intervention is still recommended given the high associated mortality of medical management [1]. Of note, the above listed factors should play an important role in the decision-making process of the extent and the type of repair pursued in acute aortic dissection, in addition to the anatomic factors.
There is significant variation in surgical strategy at the intra-institutional and inter-institutional level in many aspects of operative repair for aortic dissection. These include differences in circulation management, including cardiopulmonary bypass, the decision to utilize or not to utilize circulatory arrest, and, if performing circulatory arrest, to use antegrade or retrograde perfusion, and level of hypothermia to be achieved before arresting the patient’s circulation.
Cannulation strategy for cardiopulmonary bypass can vary from using the femoral artery, to the right axillary artery or the ascending aorta itself, directly. Perfusion strategies can vary from using hypothermic circulatory arrest with retrograde cerebral perfusion via the superior vena cava or direct antegrade cerebral perfusion using the right axillary artery or through the great vessel cannulation. Although these factors may have variable effects on outcome, discussing the results obtained with these strategies is beyond the scope of this review. But it is important for the reader to understand the added layer of confusion and complexity to the results obtained when comparing which reconstructive strategy has better outcomes.
Reconstruction Strategy: Proximal Reconstruction
For standard DeBakey I or II dissections, typically the proximal aspect of the dissection flap ends at or slightly below the sinotubular junction. Often the non-coronary sinus and a portion of the right coronary sinus are involved, but this does not mean that a root replacement needs to be performed. Unlike distal reconstruction strategies, in proximal reconstruction there is a general consensus in the cardiac surgery community regarding the extent of the operation [9–11]. In the typical case, the proximal operation consists of a proximal ascending aortic anastomoses performed just above the sinotubular junction with a straight tube graft. This may necessitate some repair work of the sinotubular junction, including felt placement and, at times, glue placed into the dissection flap that extends into the sinus segment.
As long as the coronary vessels are not extensively involved, or the dissection flap does not go into the aortic annulus, or there is no tear site or rupture at the root, typically the intimal flap in the sinus segment can be repaired with this technique. Upon repair of the intimal flap and closure of the false lumen, a valve resuspension is performed, assuming the aortic valve is competent. Then a tube graft is sewn proximally above the sinotubular junction. If the coronary vessels are involved or there is extensive valve incompetence, then the surgeon needs to make a decision with regards to an aortic root replacement or a root reimplantation procedure.
In the setting of aortic dissection repair, a root reimplantation is not a trivial undertaking by any manner. The surgeon has to be aware of the acuity of the situation, the co-morbid status and the clinical presentation of the patient, and the patient’s age before making the decision to perform a root reimplantation procedure versus a root replacement. Typically, at our institution, for young patients in whom no extensive valve repair work is required, and the cardiac function of the patient is adequate, we perform a reimplantation procedure. In rare cases one may find a damaged valve with a root that can be repaired, and in these situations the patient requires an aortic valve replacement with a concomitant ascending aorta replacement. Therefore, overall, there is a general consensus in the management of the proximal reconstruction in DeBakey I or II aortic dissections.
Reconstruction Strategy: Distal Reconstruction
Unlike the general consensus noted with the proximal reconstruction strategy during aortic dissection repair, the distal reconstruction algorithm is less clearly defined [12–16]. Distal reconstruction options include, from conservative distal ascending aortic anastomosis with the cross clamp in place, to a total arch replacement with a frozen elephant trunk placed under circulatory arrest.
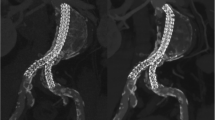
Although, at our institution we still see patients referred from outside centers for evaluation of distal ascending/aortic arch dilatation after type A dissection repair without circulatory arrest, in general the consensus is that the distal reconstruction should be performed under circulatory arrest so that any cross clamped aorta dissected aorta resected. At our institution both DeBakey type I and type II dissections are treated with at least an extended transverse hemiarch distal reconstruction performed under circulatory arrest. In DeBakey I dissection cases, there are a few surgeons who will perform concomitant antegrade stenting of the descending thoracic aorta under circulatory arrest in order to decrease the future, potential morbidity of dilatation of the distal, aneurismal dissected aorta [6, 10, 11].
Although there are reports supporting hemiarch reconstruction and those advocating for an aggressive total arch plus/minus elephant trunk repair [15–17], to our knowledge there is no strong evidence in the literature to argue for an aggressive strategy, such as a total arch replacement with elephant trunk for DeBakey type I dissections.
A hemiarch reconstruction with an antegrade stent deployed into the descending thoracic aorta is advocated by a few groups, including a few surgeons at our institution [6, 10, 11, 17, 18]. The outcomes of this additional stenting procedure are still unclear, though there is evidence mounting that although it may not improve overall survival, it may significantly decrease the associated morbidity of a future open thoracoabdominal operation [11]. In our opinion, empiric total arch replacement ± elephant trunk for standard Type A dissections is an overly aggressive approach, without substantial evidence to show survival or co morbidity benefit over performing an aggressive transverse hemiarch.
There is very good data supporting the importance of performing a hemiarch operation for type A dissection [18]. In a retrospective review performed by the group at Washington University, of a 119 patients undergoing acute type A dissection repair, 34 % of the patients underwent hemiarch operations versus 66 % undergoing an ascending aortic operation alone [6]. In this study, hemiarch replacement did not increase the operative risk as compared to ascending aorta replacement alone. At 10 year follow-up, freedom from reoperation was 81 % overall with a long-term survival of 60 %. Between the two groups, there was no difference at 5 years in survival but at 10 years there was an increasing trend towards higher survival in the hemiarch group as compared to the ascending group, though this was not statistically significant. In addition, the ascending aortic replacement group had an 8 % reoperation rate requiring an ascending aortic reconstruction whereas none in the hemiarch group required an anterior reconstruction.
In another study by Ohtsubo et al. in the Annals of Thoracic Surgery, 5 year actuarial survival rates suggested that a hemiarch replacement had better outcomes than an ascending aortic replacement alone or a total arch replacement for type A dissection [19]. The paper suggested that an aggressive total arch had poorer long-term outcomes than a hemiarch procedure. In support of this finding, in a risk model predicting surgical mortality in acute type A dissection presented by the IRAD group, they found that performing a hemiarch replacement during acute type a dissection repair was an independent predictor of favorable surgical outcomes [1]. The study looked at 682 patients and found that cases involving more extensive proximal reconstruction, including aortic valve replacement or root replacement, were associated with higher surgical mortality, whereas, the contrary was true for the distal reconstruction strategy. In comparison to an ascending aortic replacement alone, the circulatory arrest management with a hemiarch reconstruction at the distal aorta was associated with lower surgical mortality. Therefore, the paper suggested that all type A dissection repairs should be done with a distal reconstruction being performed under circulatory arrest with a hemiarch approach.
Kim et al.. looked at their institutional experience with total arch repair versus transverse hemiarch in the management of acute DeBakey 1 dissection [14]. In a retrospective review of 188 consecutive patients undergoing hemiarch (n = 144) versus total arch (n = 44 patients) replacements, 5 year unadjusted survival and permanent neurologic injury rates were significantly higher in the total arch group than the hemiarch group (survival: 66 % vs. 83 % and neurologic injury free: 43 % vs. 75 %). After adjustment for baseline characteristics they noted that the total arch group patients were at greater risks of death (hazard ratio of 2.38) and permanent neurologic injury (hazard ratio of 3.25) compared to the hemiarch group. The study suggested that operative intervention more extensive than hemiarch distal aortic reconstruction did not improve long term survival or risk of neurologic injury. Rates of aortic reoperation or aortic dilatation greater than 55 mm also did not significantly defer between these two groups. In a large analysis of the German registry for acute dissection, database a total of 658 patients with DeBakey 1 dissection were studied [15]. Patients undergoing ascending aorta plus hemiarch replacement (n = 518) were compared to those undergoing total arch replacement or an elephant trunk repair (n = 140). The study found that the total arch group had higher mortality (25.7 % vs. 18.5 %) although not statistically significant (p = 0.867). New onset of neurological deficit or new malperfusion deficit rate was similar in both groups. The study concluded that more aggressive approaches of aortic arch treatment can be performed without higher perioperative risk. Although the study assessed perioperative morbidity to be similar, it did show a trend towards increasing mortality in the total arch/elephant trunk group. Long term outcome data was not reported. Therefore even though the study suggested that total arch replacement in DeBakey 1 dissection, can be performed relatively safely, it did not show that there was any survival or morbidity improvement with this procedure compared to a hemiarch replacement. In certain situations with aortic arch tear cerebral malperfusion, a total arch replacement may be a requirement. But this need for total arch replacement in DeBakey 1 dissection repair is not an imperative treatment but more a decision to be made based on the anatomy of the dissection involving the aortic arch.
Given these mixed results noted with the extent of distal resection reconstruction for DeBakey 1 dissection our institutional practice over the past 15 years has remained the same. Unless there is extensive aortic arch tear or involvement of cerebral malperfusion, all DeBakey 1 dissection cases undergo a transverse hemiarch reconstruction distally under circulatory arrest. Over the past 5 years a few surgeons have performed concomitant antegrade stenting of the proximal descending thoracic aorta under circulatory arrest for DeBakey 1 dissection [6, 11]. Although it is important to note that this is not our standard practice. Early midterm analysis in these patients undergoing concomitant antegrade stent grafting suggests that the postoperative and follow up survival in these patients is equal to the transverse hemiarch replacement group only. Of importance, similar to other groups, we have noted an increasing rate of false lumen obliteration and elimination of the need for open thoracoabdominal aortic intervention in the stented group. Clearly further follow up will be required to assess if concomitant antegrade stent grafting of the descending thoracic aorta for DeBakey 1 dissection provides any improvement in survival, although there is evidence suggesting that it eliminates the morbidity of an open thoracoabdominal operation [11]. Therefore, we advocate that all patients with DeBakey 1 dissection undergo at least transverse hemiarch replacement under circulatory arrest for distal reconstruction. The evidence for empiric total arch replacement without the involvement of great vessel dissection, arch tear, or cerebral malperfusion is not strong [20]. Given that there is no strong evidence to support immediate or long term survival with total arch replacement, we advocate that this approach not be empirically undertaken for all DeBakey I dissection confers any long term benefit without affecting postoperative outcomes.
In summary, we believe that for the following main reasons the standard operation for DeBakey 1 dissection should be an ascending aorta plus transverse hemiarch graft replacement. The aortic root and aortic valve proximally should be preserved unless there is a good indication for replacement or reimplantation. Similarly for distal reconstruction beyond a transverse hemiarch graft, empiric total arch replacement ± elephant trunk is not advocated for these reasons. One, there is no strong evidence to support that there is a survival benefit for more extensive distal reconstruction than a transverse hemiarch. In fact several series report higher postoperative and longterm mortality in patients undergoing total arch replacement [1, 8, 17, 19, 21]. Although there is some evidence that suggesting that the distal reoperation rate is decreased with total arch replacement, this is not offset by the overall evidence suggesting a higher associated mortality with this more extensive reconstruction [20, 22]. Two, though there are suggestions that reoperation rates may be lower with total arch replacement, there is no strong evidence to support this statement. Several reports suggest that the distal reoperation rate is not influenced by the extent of resection beyond a hemiarch replacement. In this context it is also important to recognize that increasing the false lumen obliteration rate does not necessarily translate to decreasing distal reoperation rate. Three, it is important to recognize that DeBakey I dissection is a high mortality, high risk operation. The inherit nature of this disease carries with it a high level of morbidity and mortality. Therefore it is prudent to surgically intervene to the level that is only necessary so that the immediate postoperative outcomes are not worsened. It is also important to recognize that the long term survival in dissection patients still remains poor probably reflecting the overall lethality of this disease and the associated co morbid status of these patients [15]. Until a multicenter randomized clinical trial can be organized to thoroughly study this question, we believe that further extensive resections beyond a hemiarch reconstruction cautiously adopted if they show equivocal postoperative outcomes with improved long term benefit as compared to transverse hemiarch reconstruction.
The Use of Glue Products in Debakey 1 Dissection Repair
The use of gelatin resorcinol formalin (GRF) glue in the treatment of acute aortic dissection repair was first reported in 1979 by Guilmet and Bachet [23]. Since then, glue products have been extensively used and reported in the aortic dissection literature. To this day, the results of these small, retrospective series studies have been mixed with certain groups strongly advocating the use of glue products for aortic dissection repair with others opposing their use [24, 25]. The controversy of the use of glue products picked up steam in a review in 1999 by Fukunaga et al. [26]. In this study in a cohort of patients undergoing acute aortic dissection repair in which glue products were used reoperation rate of 16 % was noted. Following this study several reports have appeared over the past 10–15 years suggesting a harmful role for the use of glue products in acute aortic dissection repair [12, 13, 27, 28].
There have also been reports advocating the use of glue products in providing aortic root and distal aortic stability in aortic dissection [3]. It is important to note that all of these studies were observational, retrospective analyses. Therefore, to this day there has been no definitive study advocating or negating a role for glue products in type A dissection repair. We will briefly review a few studies that suggest harmful role of glue in acute aortic dissection followed by some that report greater long term aortic root and distal aortic stabilization with the use of glue products. We will conclude by providing our institutional bias with the use of glue in the operative management of type A dissection.
Fukunaga et al.. 1999, reported a review of 164 patients who were operated on for acute aortic dissection [26]. One hundred forty eight of these patients had GRF glue used for reinforcement of the dissected proximal and distal aortic segments. Early postoperative mortality was 26 % and 16 patients died late postoperatively. There were 22 reoperations in 20 patients of which 9 had developed complications in the aortic segment that underwent GRF glue application. The study went on to conclude that though GRF glue use may improve resuspension of the aortic layers in dissection repair, it may increase the risk of late postoperative complications, especially proximally near the aortic root. In another large study performed by Suzuki et al.. 269 pts underwent acute type A aortic dissection repair. In GRF patients a 16 % rate of false aneurysm was noted [28]. Twenty four patients required reoperation. During the reoperations, it was noted that the GRF glue site showed significant degeneration of the aorta with tissue necrosis, severe local inflammation along with organized old thrombi. Similar studies by Hata and Suzuki also suggested that the GRF glue used during dissection repair was associated with a late reoperation rate [4, 28]. Histological analyses of resected specimen at reoperation showed medial smooth muscle cell loss of nuclei, inflammation and tissue necrosis [29]. These studies suggested that though use of glue products may help improve early morbidity in aortic dissection repair, it appears to be associated with an increasing late reoperation rate.
Several studies from literature also report for increased durability of aortic anastomoses in aortic dissection repair due to the use of fibrin glue products [3, 25, 30]. In a Japanese study retrospectively reviewing 100 patients undergoing acute aortic dissection repair, the use of a fabric with fibrin glue was associated with excellent long term survival with a low reoperation rate [25]. In this cohort, 5 and 10 year survival was 75 and 59 % with freedom from aortic reoperation at 98 % at 5 and 10 year follows up. The study concluded that the use of fibrin glue resulted in low, early, and late mortality, as well as low reoperation rate. In a study by Yamanaka et al., 140 acute aortic dissection patients were followed over a mean period of 44 months [30]. All these patients had techniques of aortic reconstruction in which felt patches and glue product were used. In this cohort, overall operative mortality was 9.3 % with freedom from aortic reoperation rate of 100 %. A study by Hata et al. showed similar results suggesting for a role of glue products in acute aortic dissection repair [3]. In this study with reoperation free rate at 89 % at 3 year follow up, histological analysis at the reoperation site showed that there was no adverse tissue reaction at the site of glue use. Bachet et al. reported a series of 171 patients with acute type A dissection repair followed over a mean period of 79 months [5]. All these patients had aortic stumps reinforced with GRF glue. 22 patients (16 %) underwent reoperations for a total of 28 total reoperations. Reoperative mortality was 27 %. Actuarial late survival rates were 56 and 36 % at 10 and 15 year follow-up period. The study concluded the GRG glue was an extremely useful tool in acute aortic dissection repair [5]. The use of this product appears to have a beneficial effect on long term results. Survival in this cohort however, seems to be more dependent on the patient presentation and overall condition. Similarly Bavaria et al. [31], reported a prospective randomized multicenter study looking at bioglue use in aortic dissection. This study suggested that bioglue patients had shorter operative time less blood loss and shorter hypothermic circulatory arrest times. Based on this, the study advocated for the use of bioglue as surgical adhesive in acute aortic dissection repair. A small study by Chao et al. [24] from Massachusetts General Hospital also supported the role of bioglue in aortic dissection repair. In this experience the use of bioglue was associated with shorter circulatory arrest times, lower operative blood loss, shorter post-operative intubation times, lower transfusion requirements, and fewer take-backs for bleeding. These studies reinforced the beneficial effects of the use of glue adhesives/adjuncts in the immediate post-operative period for acute aortic dissection repair. At the University of Pennsylvania, we utilize the bioglue product selectively for aortic dissection repair [32]. Typically bioglue is used in conjunction with Teflon glue felt to reconstruct the aortic wall for both proximal and distal reconstruction. This involves placement of Teflon felt into the dissection flap at the proximal or distal suture line, reinforcing this with a small amount of bioglue and then re-approximating the flap with a running 5–0 prolene stitch. In our experience this form of a neomedia utilizing the Teflon plus bioglue is associated with decreased post-operative bleeding. Therefore we advocate for the meticulous and judicial use of bioglue products in acute aortic dissection repair. Its beneficial effects seem to be primarily in the immediate postoperative recovery of the patient, and its use has not been definitely shown to increase the reoperation rate over long term follow up.
References
Rampoldi V, Trimarchi S, Eagle KA, Nienaber CA, Oh JK, International Registry of Acute Aortic Dissection (IRAD) Investigators, et al. Simple risk models to predict surgical mortality in acute type A aortic dissection: the International Registry of Acute Aortic Dissection score. Ann Thorac Surg. 2007;83(1):55–61.
Karck M. The glue crisis in surgery of acute aortic dissection type A is ongoing. Eur J Cardiothorac Surg. 2012;41(4):e36–7. Epub 2012 Feb 6.
Hata M, Shiono M, Sezai A, Iida M, Negishi N, et al. Type A acute aortic dissection: immediate and mid-term results of emergency aortic replacement with the aid of gelatin resorcin formalin glue. Ann Thorac Surg. 2004;78(3):853–7; discussion 857.
Hata H, Takano H, Matsumiya G, Fukushima N, Kawaguchi N, Sawa Y. Late complications of gelatin-resorcin-formalin glue in the repair of acute type A aortic dissection. Ann Thorac Surg. 2007;83(5):1621–6.
Bachet J, Goudot B, Dreyfus G, Banfi C, Ayle NA, et al. The proper use of glue: a 20-year experience with the GRF glue in acute aortic dissection. J Card Surg. 1997;12(2 Suppl):243–53; discussion 253–5.
Geirsson A, Bavaria JE, Swarr D, Keane MG, Woo YJ, et al. Fate of the residual distal and proximal aorta after acute type A dissection repair using a contemporary surgical reconstruction algorithm. Ann Thorac Surg. 2007;84:1955–64.
Halstead JC, Meier M, Etz C, Spielvogel D, Bodian C, et al. The fate of the distal aorta after repair of acute type A aortic dissection. J Thorac Cardiovasc Surg. 2007;133:127–35.
Kirsch M, Soustelle C, Houël R, Hillion ML, Loisance D. Risk factor analysis for proximal and distal reoperations after surgery for acute type A aortic dissection. J Thorac Cardiovasc Surg. 2002;123:318–25.
Easo J, Weigang E, Hölzl PP, Horst M, Hoffmann I, et al. Influence of operative strategy for the aortic arch in DeBakey type I aortic dissection: analysis of the German Registry for Acute Aortic Dissection Type A. J Thorac Cardiovasc Surg. 2011;144:617–23.
Jakob H, Tsagakis K, Tossios P, Massoudy P, Thielmann M, et al. Combining classic surgery with descending stent grafting for acute DeBakey type I dissection. Ann Thorac Surg. 2008;86:95–102.
Pochettino A, Brinkman WT, Moeller P, Szeto WY, Moser W, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg. 2009;88:482–90.
Geirsson A. Extended arch resection in acute type A aortic dissection: CON. Cardiol Clin. 2010;28(2):343–7.
Urbanski PP, Lenos A, Schmitt R, Diegeler A. Extended arch resection in acute type A aortic dissection: PRO. Cardiol Clin. 2010;28(2):335–42.
Kim JB, Chung CH, Moon DH, Ha GJ, Lee TY, Jung SH, et al. Total arch repair versus hemiarch repair in the management of acute DeBakey type I aortic dissection. Eur J Cardiothorac Surg. 2011;40(4):881–7. Epub 2011 Feb 18.
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903.
Kazui T, Yamashita K, Washiyama N, Terada H, Bashar AH, Suzuki T, Ohkura K. Impact of an aggressive surgical approach on surgical outcome in type A aortic dissection. Ann Thorac Surg. 2002;74(5):S1844–7; discussion S1857–63.
Uchida N, Shibamura H, Katayama A, Shimada N, Sutoh M, et al. Operative strategy for acute type A aortic dissection: ascending aortic or hemiarch versus total arch replacement with frozen elephant trunk. Ann Thorac Surg. 2007;84(6):1955–64; discussion 1955–64.
Moon MR, Sundt 3rd TM, Pasque MK, Barner HB, Huddleston CB, et al. Does the extent of proximal or distal resection influence outcome for type A dissections? Ann Thorac Surg. 2001;71(4):1244–9; discussion 1249–50.
Ohtsubo S, Itoh T, Takarabe K, Rikitake K, Furukawa K, et al. Surgical results of hemiarch replacement for acute type A dissection. Ann Thorac Surg. 2002;74(5):S1853–6; discussion S1857–63.
Hirotani T, Kameda T, Kumamoto T, Shirota S. Results of a total aortic arch replacement for an acute aortic arch dissection. J Thorac Cardiovasc Surg. 2000;120:686–91.
Sabik JF, Lytle BW, Blackstone EH, McCarthy PM, Loop FD, et al. Long-term effectiveness of operations for ascending aortic dissections. J Thorac Cardiovasc Surg. 2000;119:946–62.
Zierer A, Voeller RK, Hill KE, Kouchoukos NT, Damiano Jr RJ, et al. Aortic enlargement and late reoperation after repair of acute type A aortic dissection. Ann Thorac Surg. 2007;84:479–87.
Guilmet D, Bachet J, Goudot B, Laurian C, Gigou F, et al. J Thorac Cardiovasc Surg. 1979;77(4):516–21.
Chao HH, Torchiana DF. BioGlue: albumin/glutaraldehyde sealant in cardiac surgery. J Card Surg. 2003;18(6):500–3.
Nakajima T, Kawazoe K, Kataoka T, Kin H, Kazui T, et al. Midterm results of aortic repair using a fabric neomedia and fibrin glue for type A acute aortic dissection. Ann Thorac Surg. 2007;83(5):1615–20.
Fukunaga S, Karck M, Harringer W, Cremer K, Rhein C, et al. The use of felatin-resource-formalin glue in acute aortic dissection type A. Eur J Cardiothorac Surg. 1999;15:564–70.
Bingley JA, Gardner MA, Stafford EG, Mau TK, Pohlner PG, et al. Late complications of tissue glues in aortic surgery. Ann Thorac Surg. 2000;69(6):1764–8.
Suzuki S, Imoto K, Uchida K, Takanashi Y. Aortic root necrosis after surgical treatment using gelatin-resorcin-formaldehyde (GRF) glue in patients with acute type A aortic dissection. Ann Thorac Cardiovasc Surg. 2006;12:333–40.
Kazui T, Washiyama N, Bashar AH, Terada H, Suzuki K, et al. Role of biologic glue repair of proximal aortic dissection in the development of early and midterm redissection of the aortic root. Ann Thorac Surg. 2001;72(2):509–14.
Yamanaka K, Hori Y, Ikarashi J, Nakatsuka D, Hirose K. Durability of aortic valve preservation with aortic root reconstruction for a acute type A aortic dissection. Eur J Cardiothorac Surg. 2012. doi:10.1093/ejcts/EZR292.
Coselli JS, Bavaria JE, Fehrenbacher J, Stowe CL, Macheers SK, et al. Prospective randomized study of BioGlue surgical adhesive used as a hemostatic and structural adjunct. J Am Coll Surg. 2003;197(2):243–52; discussion 252–3.
Bavaria JE, Brinster DR, Gorman RC, Woo YJ, Gleason T, et al. Advances in the treatment of acute type A dissection: an integrated approach. Ann Thorac Surg. 2002;74:S1848–52.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Vallabhajosyula, P., Komlo, C., Wallen, T., Szeto, W.Y., Bavaria, J.E. (2014). Have Hemiarch Replacements and Adhesives Improved Outcomes in Acute Type A Dissection?. In: Bonser, R., Pagano, D., Haverich, A., Mascaro, J. (eds) Controversies in Aortic Dissection and Aneurysmal Disease. Springer, London. https://doi.org/10.1007/978-1-4471-5622-2_12
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5622-2_12
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5621-5
Online ISBN: 978-1-4471-5622-2
eBook Packages: MedicineMedicine (R0)