Abstract
Hyaline articular cartilage is an avascular and insensate tissue with a distinct structural organization, which provides a low-friction and wear-resistant interface for weight-bearing surface articulation in diarthrodial joints. Ideally, articular cartilage is maintained in homeostasis over the lifetime of an individual, with its biomechanical properties inherently suited to transmit a wide variety of physiologic loads through a functional range of motion. Although its viscoelastic characteristics make it ideally suited to transmit a wide variety of physiologic loads through a functional range of motion while maintaining homeostasis, it also displays an intrinsic inability to heal when injured in the skeletally mature individual. Thus, articular cartilage lesions commonly lead to significant disability, joint dysfunction and ultimately osteoarthritis. Current treatment options are limited and often ineffective at restoring healthy articular cartilage, especially in complex cartilage defects involving large areas of damage and associated subchondral bone loss. While several options for repair of articular cartilage defects do exist, fresh osteochondralallografting currently remains the only technique that restores anatomically appropriate, mature hyaline cartilage in large articular defects. Osteochondralallografting is a valuable and uniquely versatile cartilage restoration technique that can address even complex or multiple lesions in topographically challenging environments by restoring the anatomy of the native joint both macroscopically and microscopically with a solid orthotopic replacement. As a result, osteochondralallografts have emerged to play an increasingly vital role in the clinical algorithm of cartilage restoration.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Assess and optimize the biological and mechanical environment of the joint.
-
Minimize the osseous portion of the allograft to 3–6 mm except on tibial grafts, and where predicated by lesion topography.
-
Remove all residual soft tissue and perform pressurized lavage of osseous graft portion to remove marrow elements prior to insertion.
-
Avoid excessively impacting the graft during insertion.
-
Ensure adequate stability; utilize adjunctive fixation where necessary.
1 Indications
Due to their compound osteoarticular nature, fresh osteochondral allografts are uniquely suited to address a wide spectrum of articular cartilage pathology, especially in disease entities that present with an osseous deficiency. Primary treatment can be considered for purely chondral defects whose size poses a relative contraindication for other treatments, and especially those that present with a loss of containment or bone involvement exceeding a depth of 6–10 mm. Allografts have also proven valuable in the salvage of knees that have failed other cartilage resurfacing procedures such as microfracture, autologous chondrocyte implantation, and osteochondral autologous plug transfer [1].
Specific conditions most amenable to allografting include osteochondritis dissecans (OCD) [2], osteonecrosis [3], and posttraumatic defects [4]. Other indications for allografting of the knee include select cases of multifocal or bipolar lesions as encountered in isolated, unicompartmental patellofemoral or tibiofemoral osteoarthritis in patients of an age and activity level that is not optimally suited for partial or total knee arthroplasty. In case of an absent meniscus, this can be implanted as part of a compound graft attached to its correlating tibial plateau, avoiding many of the size match and fixation pitfalls associated with isolated meniscal allograft transplantation. The advantage of an allogenous graft source is that even large and complex lesions can be resurfaced by reintroducing orthotopically appropriate, mature hyaline cartilage without inducing donor site morbidity and, with the fixation issue predictably relegated to bone-to-bone healing.
2 Contraindications
Although bipolar and multi-compartmental allografting have been moderately successful in the younger individual, allografting should not be considered an alternative to prosthetic arthroplasty in patients with advanced multi-compartment arthrosis and of an age and activity level suitable for prosthetic replacement. Likewise, the presence of open physes in the skeletally immature individual is a relative contraindication. Other relative contraindications to the allografting procedure include uncorrected ligamentous instability, meniscal insufficiency or contributory axial malalignment of the limb, which should be addressed prior or concomitantly to optimize the biomechanical environment. The presence of inflammatory disease, crystal-induced arthropathy or unexplained global synovitis generally represents a contraindication to cartilage repair procedures.
3 Alternative Treatments
Focal small to medium sized osteochondral lesions may be amenable to autologous grafting techniques or autologous chondrocyte implantation (ACI, see Chaps. 10 and 11), which has shown good outcomes in well-contained, unipolar lesions. Although a “sandwich” modification to the ACI procedure has been postulated to address significant bony deficiencies, results of this technique have not been individually reported. Overall, lesions that meet inclusion criteria for osteochondral allografting are often poorly suited for other cartilage restoration procedures, especially in the revision situation. None of these restorative procedures should be considered an alternative to prosthetic arthroplasty in an individual with symptoms, age and activity level that is appropriate for prosthetic replacement.
When considering realigning osteotomy in addition to an osteochondral allograft to address axial malalignment, staging the procedure is advised when the osteotomy site is juxtaposed to the allograft site as not to jeopardize the microvascularity of the recipient bone bed. Patients gaining satisfactory symptomatic relief from an isolated osteotomy alone may not require further surgical intervention but should be followed closely for signs of disease progression.
4 Results
The use of osteochondral transplants in biologic reconstruction of the knee joint has a long-standing clinical history internationally, and has evolved into a mainstay of clinical practice in the United States over the last quarter century. Traditionally, the allograft outcomes literature has been compounded by a high contingent of salvage cases owing to the lack of suitable treatment alternatives. However, the results of osteochondral allografting compare favorably to those of other cartilage restoration procedures in matched indications, with consistent reports of good to excellent outcomes in excess of 80 % of cases at a mean follow up of up to 10 years (Table 9.1). Retrieval studies have demonstrated that viable chondrocytes are present and mechanical properties of the collagen matrix are maintained many years after transplantation [14, 15].
5 Surgical Technique
5.1 Femoral Condyle [16]
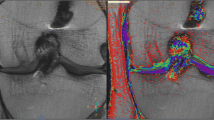
The patient is positioned supine with a proximal thigh tourniquet. A leg or foot holder is helpful in accessing the lesion by positioning and maintaining the leg in between 70° and 100° of flexion. A standard midline incision is made from the center of the patella to the tip of the tibial tubercle. For most femoral condyle lesions, a minimal anterior approach is sufficient, and eversion of the patella is not necessary. This skin incision is elevated subcutaneously, either medially or laterally to the patellar tendon, ipsilateral to the location of the lesion. A retinacular incision is then made from the superior aspect of the patella inferiorly, incising the fat pad without disrupting the anterior horn of the meniscus or damaging the articular surface. Once the joint capsule and synovium have been incised and the joint has been entered, retractors are placed medially and laterally, taking care to protect the cruciate ligaments and articular cartilage in the notch. The knee is then flexed or extended to the proper degree of flexion that presents the lesion to be treated into the arthrotomy site (Fig. 9.1). Excessive degrees of flexion limit the ability to mobilize the patella. The lesion then is inspected and palpated with a probe, to determine the extent, margins, and maximum size. In some cases where the lesion is posterior or very large, the meniscus may have to be detached and reflected, leaving a small cuff of tissue adjacent to the anterior attachment of the meniscus for reattachment at closure.
The two commonly used techniques for the preparation and implantation of osteochondral allografts are the dowel technique and the shell graft technique. Each technique has advantages and disadvantages. The dowel technique is a similar technique in principle to autologous osteochondral transfer systems [refer to chapter]. This technique is optimal for contained condylar lesions between 15 and 35 mm in diameter. Fixation is generally not required in circumferentially contained lesions due to the stability achieved with the press fit of the dowel. Disadvantages include the fact that many lesions are not conducive to the use of a circular coring system, such as very posterior femoral, tibial, patellar, and trochlear lesions. Additionally, more ovoid a lesion in shape require more normal cartilage to be sacrificed at the recipient site in order to accommodate the circular donor plug. Shell grafts are technically more difficult to perform and typically require fixation. However, depending on the technique employed, less normal cartilage may need to be sacrificed. Also, certain lesions are more amenable to shell allografts due to their location.
5.2 Dowel Allograft
There are several similar proprietary instrumentation systems that are currently available for the preparation and implantation of dowel allografts up to 35 mm in diameter. After a size determination is made using a sizing guide dowel (Fig. 9.2), a guide wire is driven into the center of the lesion, perpendicular to the curvature of the articular surface. The size of the proposed graft then is determined, utilizing sizing dowels, remembering that overlapping dowels (in a “snowman” configuration) can possibly deliver the best area coverage. The remaining articular cartilage is scored circumferentially, and a core reamer is used to remove the remaining articular cartilage and at least 3–4 mm of subchondral bone (Fig. 9.3). In deeper lesions, fibrous and sclerotic bone is removed to a healthy, bleeding osseous base. More extensive lesions should be manually curetted and packed with morselized autologous bone graft to fill these more extensive osseous defects. The guide pin then is removed, and circumferential depth measurements of the prepared recipient site are made and recorded.
The same lesion as shown in Fig. 9.1, being sized with a sizing dowel
The corresponding orthotopic location of the recipient site then is identified on the graft. The graft is placed into a graft holder (Fig. 9.4) (or alternately, held securely with bone-holding forceps). A saw guide then is placed in the appropriate position and alignment, again perpendicular to the articular surface; and an appropriate sized tube saw is used to core out the graft under continuous irrigation. Prior to removing the graft dowel from the condyle, an identifying mark is made to ensure proper orientation upon implantation. Once the graft cylinder is amputated using an oscillating saw and removed, depth measurements, which were taken from the recipient, are transferred to the bony portion of the graft (Fig. 9.5). This graft then is cut with an oscillating saw, trimmed with a rasp to the appropriate thickness in all four quadrants, and the deep edges of the bone plug can be chamfered with a rongeur and bone rasp. Often this must be done multiple times to ensure precise thickness, preferably refashioning the graft rather than the recipient site and optimally keeping the allograft and host cartilage moist throughout the procedure. Usually, a dowel plug will only comprise several millimeters of subchondral bone (Fig. 9.6). The aim is to transplant as much bone as is necessary to reconstruct an osseous defect, and as little as possible to minimize the bioburden to the host, as well as to optimize the rate limiting step of creeping substitution by minimizing the amount of allogeneic bone to be reconstituted. Prior to final implantation, the graft is irrigated copiously with pulsatile lavage to remove marrow elements and debris, and the recipient site can be dilated using a slightly oversized tamp in order to ease the insertion of the graft to prevent excessive impact loading of the articular surface when the graft is inserted. At this point, any remaining osseous defects are bone grafted. The allograft is then inserted by hand in the appropriate rotation. In case of a line to line fit it is often possible to seat the graft with gentle manual pressure or by using the appositional joint surface as a fulcrum while gently cycling the knee through a range of motion. Alternatively, a cupped mallet can be used to gently tamp the graft into place until it is flush, again minimizing mechanical insult to the articular surface of both the native and graft tissue.
Once the graft is seated, a determination is made whether additional fixation is required. Circumferentially contained dowels often provide an inherentlystable press fit that requires no additional fixation (Fig. 9.7). If necessary, bioabsorbable pins are utilized, particularly if the graft is large or borders the intercondylar notch. Sometimes the graft needs to be trimmed in the notch region, to prevent impingement. The knee is then brought through a complete range of motion, in order to confirm that the graft is stable and there is no catching or soft-tissue obstruction noted. At this point, the wound is irrigated copiously, and, if no further adjunct procedures are planned, routine closure is performed.
5.3 Shell Allograft
Shell allografts are employed for lesions that cannot be addressed by single or multiple plugs, either due to size, shape, or location, and depend on a free hand technique. The defect is accessed, identified, and assessed through the previously described arthrotomy. The circumference of the lesion is marked with a surgical pen. An attempt is made to create a geometric shape that is amenable to hand crafting a shell graft while minimizing the sacrifice of normal cartilage. A #15 scalpel blade is used to demarcate the lesion, and all tissue inside this mark is removed with ring curettes or other suitable instrumentation. Using motorized burrs and sharp curettes, the defect is then debrided down to a subchondral depth of 4–5 mm. Deeper cystic defects, again, are curetted by hand and later bone grafted. The allograft is fashioned in a freehand fashion, initially slightly over sizing the graft and carefully removing excess bone and cartilage as necessary through multiple trial fittings. If there is deeper bone loss in the defect, more bone can be left on the graft and the defect can be grafted with cancellous bone prior to graft insertion. The graft is placed flush with the articular surface. The need for fixation is based on the degree of inherent stability. Bioabsorbable pins are typically used when fixation is required but compression screws may be used as an alternative. Wound irrigation and routine closure are performed as previously described.
6 Postoperative Regimen
Patients are allowed full range of motion post-operatively, unless there are other additional reconstructive procedures that would dictate alternative rehabilitation. While range of motion exercises and quadriceps strengthening generally are introduced early, patients are usually maintained in a toe-touch-only weight-bearing status for a period of at least 8 weeks, ultimately depending on radiographic evidence of incorporation. At 4 weeks, patients are allowed closed-chain exercises such as cycling. Progressive weight bearing as tolerated usually is allowed at 3 months, and the patient is allowed to return to recreation and sports when functional rehabilitation is complete, usually at 6 months. Typically, braces are not utilized, unless the grafting involves the patellofemoral joint, where flexion is limited to <45° for the first 4–6 weeks, or in cases where bipolar tibial femoral grafts are used, an unloader or range of motion brace can be employed to prevent excessive stress on the grafted surfaces.
7 Avoiding Pitfalls and Complications
7.1 Graft Selection
In current practice, small-fragment fresh osteochondral allografts are not HLA type or blood group matched between donor and recipient, and no immunosuppression is used. Rather, the allografts are matched to recipients on size alone. Preoperatively, the patient’s knee is sized using an anterioposterior radiograph with a standardized magnification marker. A measurement of the medial-lateral dimension of the tibia is then made, just below and parallel to the joint surface. The measurement is accurately adjusted for magnification, and the tissue bank compares this to direct measurements on the donor tibial plateau. A match is considered acceptable within a tolerance of ±2 mm; however, it should be noted that there is a significant variability in anatomy. In particular, in treating osteochondritis dissecans, the pathologic condyle typically is larger, wider, and flatter; therefore, a larger donor should generally be used. In general, it is technically less challenging to fit a larger donor to a smaller recipient condyle than vice versa, due to radius of curvature. The surgeon is ultimately responsible to inspect the tissue intended for transplantation, optimally before beginning the actual procedure. This should include affirming site, size, and integrity of the tissue including packaging, and adequacy of storage and refrigeration.
7.2 Allograft Failure [15]
Failure of the allograft procedure can occur due to nonunion or late fragmentation and graft collapse. While healing of the graft-host interface reliably occurs, particularly with smaller grafts, the degree of revascularization appears to be variable. Fragmentation and collapse typically occurs in areas of unvascularized allograft bone. Since it merely serves as an osteoconductive scaffold for healing to the host by creeping substitution, which is a rate limited process, the portion of transplanted bone should be minimized wherever possible, without compromising stability of the graft as warranted by the clinical situation. This will also minimize the potential antigenic burden of marrow elements possibly remaining in the transplanted cancellous bone. Patients with graft collapse typically present with new onset pain or mechanical symptoms. Radiographs may show joint space narrowing, cysts, or sclerotic regions. Magnetic resonance imaging can help rule out contributory concomitant joint pathology in the differential diagnosis of post-operative symptoms. Depending on the status of the knee joint and patient factors, the treatment options include observation, removal of the fragmented portion of the graft, repeat allografting, or conversion to arthroplasty.
8 Conclusion
Fresh osteochondral allografts have a role in the treatment of a wide spectrum of osteoarticular pathology, particularly in combined lesions presenting with an osseous and a chondral component. The operative procedure for the treatment of femoral condylar lesions is straightforward but demands precision to achieve reproducible results and to minimize early graft failures related to surgical technique. While many clinical and basic scientific studies support the theoretical foundation and efficacy of the use of small fragment allografts, more scientific validation of empirical clinical practice is still needed. The indications for the use of fresh osteochondral allografts continue to evolve, including use in other diathrodial joints.
References
Görtz S, Bugbee WD. Fresh osteochondral allografts: graft processing and clinical applications. J Knee Surg. 2006;19(3):231–40.
Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907–14.
Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allografting for steroid-associated osteonecrosis of the femoral condyles. Clin Orthop Relat Res. 2010;468(5):1269–78.
Gross AE, Shasha N, Aubin P. Long-term followup of the use of fresh osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res. 2005;435:79–87.
Chu CR, Convery FR, Akeson WH, Meyers M, Amiel D. Articular cartilage transplantation. Clinical results in the knee. Clin Orthop Relat Res. 1999;360:159–68.
Krych AJ, Robertson CM, Williams 3rd RJ. Return to athletic activity after osteochondral allograft transplantation in the knee. Am J Sports Med. 2012;40(5):1053–9.
McDermott AG, Langer F, Pritzker KP, Gross AE. Fresh small-fragment osteochondral allografts. Long-term follow-up study on first 100 cases. Clin Orthop Relat Res. 1985;197:96–102.
Ghazavi MT, Pritzker KP, Davis AM, Gross AE. Fresh osteochondral allografts for post-traumatic osteochondral defects of the knee. J Bone Joint Surg Br. 1997;79(6):1008–13.
Beaver RJ, Mahomed M, Backstein D, Davis A, Zukor DJ, Gross AE. Fresh osteochondral allografts for post-traumatic defects in the knee. A survivorship analysis. J Bone Joint Surg Br. 1992;74(1):105–10.
McCulloch PC, Kang RW, Sobhy MH, Hayden JK, Cole BJ. Prospective evaluation of prolonged fresh osteochondral allograft transplantation of the femoral condyle: minimum 2-year follow-up. Am J Sports Med. 2007;35(3):411–20.
Williams 3rd RJ, Ranawat AS, Potter HG, Carter T, Warren RF. Fresh stored allografts for the treatment of osteochondral defects of the knee. J Bone Joint Surg Am. 2007;89(4):718–26.
LaPrade RF, Botker J, Herzog M, Agel J. Refrigerated osteoarticular allografts to treat articular cartilage defects of the femoral condyles. A prospective outcomes study. J Bone Joint Surg Am. 2009;91(4):805–11.
Garrett JC. Osteochondral allografts for reconstruction of articular defects of the knee. Instr Course Lect. 1998;47:517–22.
Jamali AA, Hatcher SL, You Z. Donor cell survival in a fresh osteochondral allograft at twenty-nine years. A case report. J Bone Joint Surg Am. 2007;89(1):166–9.
Williams SK, Amiel D, Ball ST, et al. Analysis of cartilage tissue on a cellular level in fresh osteochondral allograft retrievals. Am J Sports Med. 2007;35(12):2022–32.
Gortz S, Bugbee WD. Allografts in articular cartilage repair. J Bone Joint Surg Am. 2006;88(6):1374–84.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Görtz, S., McCulloch, P.C. (2014). Osteochondral Allograft Transplantation: Surgical Technique and Results. In: Emans, P., Peterson, L. (eds) Developing Insights in Cartilage Repair. Springer, London. https://doi.org/10.1007/978-1-4471-5385-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5385-6_9
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5384-9
Online ISBN: 978-1-4471-5385-6
eBook Packages: MedicineMedicine (R0)