Abstract
Besides having a direct cytotoxic effect on tumor cells, electrochemotherapy also has a vascular-disrupting effect. Application of electric pulses to the tumor induces transitory, but profound, reduction in tumor perfusion and oxygenation of tumors. When bleomycin or cisplatin are present at the time of tissue electroporation, endothelial cells in tumor blood vessels are also affected, leading to their apoptotic death. As a consequence, blood flow in the treated tumor is reduced, leading to extensive tumor cell necrosis and regression. Therefore, electrochemotherapy can be beneficially used in the treatment of bleeding metastases, as demonstrated in several reported cases. A model of vascular changes after application of electric pulses to the tumor and a model of vascular changes after electrochemotherapy are proposed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
A functioning vascular supply is essential for solid tumor growth and metastasis. It is known that in the absence of angiogenesis, tumors are not able to develop beyond a few millimeters and therefore remain dormant. The angiogenic switch enables neovascularization of tumors and consequently rapid tumor growth, metastasis, and tumor progression [1]. The newly developed vessels have specific physiological and biological features that distinguish them from normal vessels. These differences include a relative lack of vascular smooth muscle cells, abnormal and chaotic branching patterns, and the absence of innervation. Endothelial cells in neovascularized tumors differ from those in normal tissue; they have distinct molecular markers, and their proliferation is much faster. Therefore, tumor vasculature, due to its physiological and molecular specificity, is a specific target for tumor treatment [2].
There are two concepts of vascular-targeted agents as cancer therapeutics that act on tumor blood vessels; those inhibiting the formation of new blood vessels (antiangiogenic agents), and those that act on the established blood vessels (vascular-disrupting agents). Antiangiogenic agents are considered cytostatic in nature, in contrast to vascular-disrupting agents, which are thought to be cytotoxic. The antiangiogenic agents exert their effect within days and require chronic dosing, oral or intravenous, whereas vascular-disrupting agents are effective within minutes and require acute dosing, mostly intravenously [3].
Both categories of vascular-targeted therapies are clinically available, the prominent antiangiogenic agent being bevacizumab (avastin), whilst combretastatin A4-P is the major vascular-disrupting agent. Although they are distinguished by their mode of action, there is some overlap between the two groups, with agents classified according to their primary site of action [4–6].
Electrochemotherapy
Electrochemotherapy consists of chemotherapy followed by local application of electric pulses to the tumor to increase drug delivery into cells. Drug uptake can be increased by electroporation only for those drugs whose transport through the plasma membrane is normally impeded [7]. Among many drugs which have been tested so far, only bleomycin and cisplatin have transitioned from preclinical testing to clinical trials. In vitro studies demonstrated a several-fold increase in their cytotoxicity after electroporation of cells. In vivo, electroporation of tumors after local or systemic administration of either of the drugs, that is, electrochemotherapy, proved to be an effective antitumor treatment. In preclinical studies on several tumor models, electrochemotherapy with either bleomycin or cisplatin was assessed in detail, and parameters for effective local tumor control were determined [8, 9]. Several clinical studies were performed demonstrating that electrochemotherapy is effective in local tumor control of cutaneous and subcutaneous tumor nodules of different histology. So far, predominantly melanoma skin metastases have been treated, with ∼70% long-lasting complete responses of the treated nodules [10–12].
Besides membrane electroporation, which facilitates drug transport and its accumulation in the cell, other mechanisms that are involved in antitumor effectiveness of electrochemotherapy have been described [8, 9].
Modifying Effect of Electric Pulses on Tumor Blood Flow
The application of electric pulses to tissues induces a transient but reversible reduction in blood flow. Several studies have investigated changes in blood volume, perfusion, and oxygenation in tumors and normal tissue after application of electric pulses. The first study, using albumin-(Gd-DTPA) contrast-enhanced magnetic resonance imaging (MRI), has demonstrated that 30 min after application of electric pulses to SA-1 tumors, tumor blood volume is reduced from 20% in untreated tumors to 0% in electroporated tumors [13]. A pharmacological study with 86RbCl extraction technique in the same tumor model was also done, exploring time dependence of the perfusion changes. A significant reduction of tumor perfusion (∼30% of control) was observed within 1 h following the application of electric pulses to the tumors. Thereafter, tumor blood flow slowly recovered, almost reaching the pretreatment level within 24 h. No change in perfusion was induced in untreated contralateral normal leg muscle. A similar pattern of blood flow reduction was induced when a second set of electric pulses was applied to the tumor following a 24-h interval. The degree of tumor blood flow reduction was dependent upon the number of electric pulses applied; a smaller effect was observed if less than eight pulses were applied. Furthermore, the degree of blood flow reduction was also dependent on the amplitude of electric pulses applied; electric pulses with an amplitude higher than 600 V induced reduction in tumor blood flow [14]. In subsequent studies, it was demonstrated that the results obtained with the 86RbCl extraction technique correlated with the Patent Blue staining technique, which is a much more simple method for measuring tissue perfusion [15].
The changes in tumor perfusion were shown to correlate with changes in tumor oxygenation, as measured by the electron paramagnetic resonance (EPR) technique. The maximal reduction in partial oxygen pressure (pO2) level was observed 2 h after application of electric pulses to the tumor (∼40% of control), with recovery to the pretreatment level within 10 h after application [16]. This study also demonstrated that changes in the tumor blood flow are instantaneous, occurring during the application of electric pulses, as demonstrated by laser Doppler flowmetry [17].
In vitro studies have shown that application of electric pulses to a monolayer of endothelial cells results in a profound disruption of microfilament and microtubule cytoskeletal networks, loss of contractility, and loss of cadherin-formed cell-to-cell junctions in the vascular endothelial lining immediately after electroporation, which recovered within 60 min after electroporation, without any significant loss of cell viability. The cytoskeletal effects of electroporation were paralleled by a rapid increase in endothelial monolayer permeability, giving an indication of putative mechanisms responsible for the observed increase in permeability and cessation of blood flow in vivo [18].
A tumor is a heterogeneous tissue consisting of tumor stromal cells and a capillary network. When a tumor mass is exposed to an electric field that is used for electrochemotherapy, all cells in the tissue are exposed [19, 20]. In a mathematical model, it was validated that endothelial cells in the lining of small tumor blood vessels are exposed to an electric field that can increase their permeability. The model predicted that endothelial cells lining the tumor blood vessels are exposed to a ∼40% higher electric field than the surrounding tumor cells. This indicates that tumor endothelial cells are a valid target for electroporation [17].
A histological study of tumors exposed to electric pulse application examined blood vessel changes. Changes in endothelial cell shape were observed 1 h after application of electric pulses. Endothelial cells turned spherical in shape and became swollen, and the lumen of blood vessels was narrowed (Fig. 7.1) [17].
Morphological changes in tumor blood vessels after electroporation. Swollen endothelial cells (a, b) and narrowed lumens (c, d). Tumor tissue specimens were formalin-fixed and paraffin-embedded. Two consecutive 5 μm thick sections were cut from each paraffin block and stained with hematoxylin eosin or immunohistochemically using anti-CD31 antibody to visualize blood vessels
The observed effects of tumor blood flow modification after application of electric pulses were also observed in normal muscle tissue in mice. Similar effects on leg perfusion, measured by Patent Blue, were observed in mice, with a wide variety of electric pulse amplitudes and pulse durations (10–20,000 μs and 0.1–1.6 kV/cm) [21].
Based on all the gathered information on vascular effects of electric pulses in the tumor, a model of the sequence of changes is proposed (Fig. 7.2):
-
1.
Disruption of cytoskeletal networks causing endothelial cells to turn spherical in shape.
-
2.
Increased leakage of plasma into the interstitial space.
-
3.
Increased interstitial fluid pressure and vascular resistance leading to a narrowed vascular lumen and reduced blood flow.
-
4.
Restoration of tumor blood flow within 24–48 h due to the effect on endothelial cells and vascular permeability being reversible.
The studies indicate that vascular reactions induced by application of electric pulses to the tissue are important for the kinetics of drug delivery used in electrochemotherapy or plasmid delivery in gene electrotransfer. The vascular lock causes drug entrapment by temporary cessation of tissue perfusion induced by electric pulses, leading to a prolonged exposure of the tissue to the previously injected drug, plasmid DNA, or other nucleic acid molecules, as demonstrated in the case of electrochemotherapy with cisplatin [8, 21, 22].
Modifying Effect of Electrochemotherapy on Tumor Blood Flow
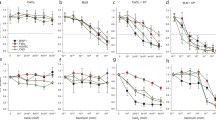
Modifying effects of electrochemotherapy on tumor blood flow, measured by tumor perfusion and oxygenation as well as histological changes, were studied and compared to vascular changes observed after application of electric pulses without the accompanying injection of a drug [17]. Studies on electrochemotherapy with bleomycin as well as with cisplatin have demonstrated that changes, within 2 h in tumor perfusion and oxygenation, are identical to those observed after the application of electric pulses alone. Immediately after treatment, tumor perfusion was maximally reduced. Approximately 30 min later, the tumors started to reperfuse in both groups; in the tumors treated by electrochemotherapy, the reperfusion leveled after ∼1 h and stayed at 20% up to 48 h after the treatment, whereas the tumors treated with application of electric pulses alone continued to reperfuse. The changes in tumor perfusion were demonstrated to be similar when using electrochemotherapy with either bleomycin or cisplatin. The degree of changes was demonstrated to be dependent on the drug dosage used in electrochemotherapy. For example, a lower bleomycin dose (1 mg/kg) resulted in less reduction of tumor perfusion than a higher dose (4 mg/kg). The low dose also resulted in gradual reperfusion of the tumors, which was in all cases significantly delayed compared to perfusion changes after application of electric pulses alone, whereas the higher dose of bleomycin resulted in complete shutdown of tumor perfusion and a high percentage of tumor cures (70%) [15–17].
The changes in perfusion following electrochemotherapy correlated with tumor oxygenation. EPR oxymetry demonstrated that electrochemotherapy induced an instantaneous reduction in pO2 levels to ∼25% of the pretreatment level, which is a more profound effect than the one caused by application of electric pulses alone. Tumor oxygenation subsequently correlated with changes observed after application of electric pulses for up to 2 h post-treatment; however, the recovery of tumor oxygenation was much slower, returning to the pretreatment level with a delay as long as 2 days [16, 17]. Short- and long-term perfusion changes were confirmed by power Doppler ultrasonography of tumors, as well as by determination of the hypoxic area in the tumors by staining of cells with pimonidazole, a marker of tumor hypoxia [17, 23]. Furthermore, it was demonstrated that electroporation of human endothelial HMEC-1 cells, even after short-term drug exposure, significantly enhanced the cytotoxicity of bleomycin and cisplatin [24].
All these data indicate that in vivo electrochemotherapy, especially with bleomycin, may directly damage the vascular endothelium, accounting for its vascular-disrupting effect. Detailed histological analyses of tumors after electrochemotherapy demonstrated that the same morphological changes in endothelial cells occurred as after application of electric pulses to the tumors; endothelial cells turned spherical in shape and became swollen, and the lumen of blood vessels was narrowed. However, apoptotic morphological characteristics were found in some vessels 8 h after electrochemotherapy. Furthermore, blood vessels were stacked with erythrocytes and extravasation of erythrocytes was also observed. Apoptotic endothelial cells were not observed in the control group or in tumors treated with either electric pulses or bleomycin alone (Fig. 7.3) [17].
Morphological changes in tumor blood vessels after electrochemotherapy with bleomycin. Swollen endothelial cells turned spherical in shape (a), increased vascular resistance to tumor blood flow (b), and apoptotic endothelial cells (c, d). Tumor tissue specimens were formalin-fixed and paraffin-embedded. Two consecutive 5 μm thick sections were cut from each paraffin block and stained with hematoxylin eosin or immunohistochemically using ant-caspase 3 antibody to visualize apoptotic cells
Based on all the gathered information on vascular effects of electrochemotherapy with bleomycin or cisplatin, a model of the sequence of changes is proposed (Fig. 7.4), which shares details with the model proposed for the application of electric pulses and includes further changes due to the presence of the chemotherapeutic drug:
-
1.
Disruption of cytoskeletal networks causing endothelial cells to turn spherical in shape.
-
2.
Increased leakage of plasma into the interstitial space.
-
3.
Increased interstitial fluid pressure and vascular resistance leading to a narrowed vascular lumen and reduced blood flow.
-
4.
Apoptosis of endothelial cells due to the presence of an increased amount of the chemotherapeutic drug.
-
5.
No or significantly delayed vascular reperfusion, depending on the degree of vascular disruption.
Clinical Application
As hemorrhaging cutaneous metastases are a common clinical problem, some reports on successful treatment with electrochemotherapy have already been described. Gehl et al. described two cases of successful management of bleeding melanoma skin metastases [25, 26]. The first case established the effectiveness of electrochemotherapy in the treatment of nine bleeding, ulcerated nodules on the chest wall, with immediate cessation of bleeding after administration of electric pulses and complete regression of all nodules [25]. The second case demonstrated a palliative effect of electrochemotherapy in dealing with eight metastases on the head and scalp, with complete regression of all but one of the metastases (87%) [26]. An even bigger skin metastasis (3.5 × 3 cm in diameter) was treated by electrochemotherapy at our Institute of Oncology Ljubljana [27]. The bleeding metastasis was located on the leg and amputation of the leg was initially considered as a definitive cure. However, electrochemotherapy with bleomycin given intravenously was performed, and immediately after delivery of the electric pulses, the bleeding stopped and did not recur. The lesion developed a crust and decreased in size in a matter of weeks. At the end of the 3-week observation period, the lesion was in partial response (Fig. 7.5).
These reports show that electrochemotherapy represents a novel approach in the palliation of bleeding metastases. Surgery can be suitable for management of small bleeding lesions, but with larger or multiple lesions, amputation is the only possible surgical approach [28]. Furthermore, no studies have been performed so far to establish the palliative effect of radiotherapy on bleeding melanoma nodules. On the other hand, in a study by Fraker et al., an isolated limb perfusion with melphalan and tumor necrosis factor-alpha proved to be an effective palliative treatment of advanced bleeding melanoma. Symptomatic improvement was achieved in 5 of 6 patients with bleeding or ulcerated nodules [29]. In addition, several other studies report on the limb-sparing effect of isolated limb perfusion. Noorda et al. reported on a series of 21 patients with recurrent or persistent melanoma who underwent repeated isolated limb perfusion with tumor necrosis factor alpha and melphalan, with a median follow-up of 18 months and 95% limb salvage rate [30]. In a study by Grunhagen et al., limb salvage was achieved in 36 out of 37 patients, one patient undergoing amputation due to treatment toxicity [31]. However, according to Sasso et al., intra-arterial embolization is a treatment of choice in the management of bleeding melanoma [32].
Conclusion
A comparison between isolated limb perfusion for bleeding metastases and electrochemotherapy points to the many advantages of the latter. Patients are often in overall poor physical condition and electrochemotherapy offers an excellent alternative due to its once-only treatment strategy, high probability of immediate relief, as well as the modest degree of patient discomfort experienced. Currently, its main clinical application remains restricted to palliative treatment of cutaneous and subcutaneous tumor nodules refractory to conventional treatment. However, electrochemotherapy should also be considered as a treatment modality in patients with refractory bleeding tumor nodules.
References
Folkman J. Anti-angiogenesis: new concept for therapy of solid tumors. Ann Surg. 1972;175:409–16.
Folkman J. Angiogenesis: an organizing principle for drug discovery. Nat Rev. 2007;6:273–86.
Siemann DW, Bibby MC, Dark GG, Dicker AP, Eskens F, Horsman MR, et al. Differentiation and definition of vascular-targeted therapies. Clin Cancer Res. 2005;11:416–20.
Tozer GM, Kanthou C, Baguley BC. Disrupting tumour blood vessels. Nat Rev. 2005;5:423–35.
Neri D, Bicknell R. Tumor vascular targeting. Nat Rev. 2005;5:436–46.
Hinnen P, Eskens F. Vascular disrupting agents in clinical development. Br J Cancer. 2007;96:1159–65.
Mir LM. Bases and rationale of the electrochemotherapy. EJC Suppl. 2006;4:38–44.
Mir LM, Orlowski S. Mechanisms of electrochemotherapy. Adv Drug Del Rev. 1999;35:107–18.
Sersa G, Cemazar M, Miklavcic D, Rudolf Z. Electrochemotherapy of tumours. Radiol Oncol. 2006;40:163–74.
Marty M, Sersa G, Garbay JR, Gehl J, Collins CG, Snoj M, et al. Electrochemotherapy – an easy, highly effective and safe treatment of cutaneous and subcutaneous metastases: Results of ESOPE (European Standard Operating Procedures of Electrochemotherapy) study. EJC Suppl. 2006;4:3–13.
Quaglino P, Montera C, Osella-Abate S, Barberis M, Illengo M, Rissone M, et al. Electrochemotherapy with intravenous bleomycin in the local treatment of skin melanoma mestastases. Ann Surg Oncol. 2008;15:2215–22.
Sersa G, Miklavcic D, Cemazar M, Rudolf Z, Pucihar G, Snoj M. Electrochemotherapy in treatment of tumors. EJSO. 2008;34:232–40.
Sersa G, Beravs K, Cemazar M, Miklavcic D, Demsar F. Contrast enhanced MRI assessment of tumor blood volume after application of electric pulses. Electro Magnetobiol. 1998;17:299–306.
Sersa G, Cemazar M, Parkins CS, Chaplin DJ. Tumour blood flow changes induced by application of electric pulses. Eur J Cancer. 1999;35:672–7.
Sersa G, Cemazar M, Miklavcic D, Chaplin DJ. Tumor blood modifying effect of electrochemotherapy with bleomycin. Anticancer Res. 1999;19:4017–22.
Sersa G, Krzic M, Sentjurc M, Ivanusa T, Beravs K, Kotnik V, et al. Reduced blood flow and oxygenation in SA-1 tumours after electrochemotherapy with cisplatin. Br J Cancer. 2002;87:1047–54.
Sersa G, Jarm T, Kotnik T, Coer A, Podkrajsek M, Sentjurc M, et al. Vascular disrupting action of electroporation and electrochemotherapy with bleomycin in murine sarcoma. Br J Cancer. 2008;98:388–98.
Kanthou C, Kranjc S, Sersa G, Tozer G, Zupanic A, Cemazar M. The endothelial cytoskeleton as a target of electroporation based therapies. Mol Cancer Ther. 2006;5:3145–52.
Miklavcic D, Corovic S, Pucihar G, Pavselj N. Importance of tumour coverage by sufficiently high local electric field for effective electrochemotherapy. EJC Suppl. 2006;4:45–51.
Pavselj N, Miklavcic D. Numerical modeling in electroporation-based biomedical applications. Radiol Oncol. 2008;42:159–68.
Gehl J, Skovsgaard T, Mir LM. Vascular reactions to in vivo electroporation: characterization and concequences for drug and gene delivery. Biochim Biophys Acta. 2002;1569:51–8.
Cemazar M, Miklavcic D, Scancar J, Dolzan V, Golouh R, Sersa G. Increased platinum accumulation in SA-1 tumor cells after in vivo electrochemotherapy with cisplatin. Br J Cancer. 1999;79:1386–91.
Coer A, Cemazar M, Plazar N, Sersa G. Comparison between hypoxic markers pimonidazole and glucose transporter 1 (Glut-1) in murine fibrosarcoma tumours alter electrochemotherapy. Radiol Oncol. 2009;43:195–202.
Cemazar M, Parkins CS, Chaplin DJ, Tozer GM, Sersa G. Electroporation of human microvascular endothelial cells: evidence of an anti-vascular mechanism of electrochemotherapy. Br J Cancer. 2001;84:565–70.
Gehl J, Geertsen PF. Efficient palliation of haemorrhaging malignant melanoma skin metastases by electrochemotherapy. Melanoma Res. 2000;10:585–9.
Gehl J, Geertsen PF. Palliation of haemorrhaging and ulcerated malignant cutaneous tumors using electrochemotherapy. EJC Suppl. 2006;4:35–7.
Snoj M, Cemazar M, Srnovrsnik T, Paulin Kosir S, Sersa G. Limb sparing treatment of blooding melanoma recurrence by electrochemotherapy. Tumori. 2009;95:398–402.
Fletcher WS, Pommier RF, Lum S, Wilmarth TJ. Surgical treatment of metastatic melanoma. Am J Surg. 1998;175:413–7.
Fraker DL, Alexander HR, Andrich M, Rosenberg SA. Palliation of regional symptoms of advanced extremity melanoma by isolated limb perfusion with melphalan and high-dose tumor necrosis factor. Cancer J Sci Am. 1995;1:104–5.
Noorda EM, Vrouenraets BC, Nieweg OE, van Geel AN, Eggermont AM, Kroon BB. Repeat isolated limb perfusion with TNFalpha and melphalan for recurrent limb melanoma after failure of previous perfusion. Eur J Surg Oncol. 2006;32:318–24.
Grunhagen DJ, de Wilt JH, Graveland WJ, van Geel AN, Eggermont AM. The palliative value of tumor necrosis factor alpha-based isolated limb perfusion in patients with metastatic sarcoma and melanoma. Cancer. 2006;106:156–62.
Sasso CM, Hubner C, Wall S. Intraarterial embolization of bleeding melanoma. J Vasc Nurs. 1995;13:27–8.
Acknowledgments
The authors acknowledge the financial support from the state budget of the Slovenian Research Agency (P3-0003). The authors acknowledge the help of Prof. Marko Snoj, Prof. Andrej Coer, Dr. Simona Kranjc, and Dr. Mireille Treeby in preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Sersa, G., Cemazar, M. (2011). Vascular-Disrupting Action of Electrochemotherapy: Mode of Action and Therapeutic Implications. In: Kee, S., Gehl, J., Lee, E. (eds) Clinical Aspects of Electroporation. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-8363-3_7
Download citation
DOI: https://doi.org/10.1007/978-1-4419-8363-3_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-8362-6
Online ISBN: 978-1-4419-8363-3
eBook Packages: MedicineMedicine (R0)