Abstract
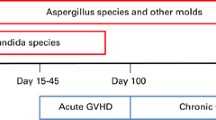
Since the first hematopoietic stem cell transplant (HSCT) was performed more than 50 years ago, significant progress has been attained in the field, with changes in conditioning regimens, stem cell sources, and outcomes. The preparative regimen for HSCT may be fully myeloablative or less aggressive (nonmyeloablative). Different sources of stem cells have been used, including bone marrow (BM), peripheral blood stem cells (PBSCs), and cord blood. Stem cells may originate from an identical twin (syngeneic), one’s own self (autologous), and another donor (allogeneic). Allogeneic donors may be related (family members) or unrelated to the recipients, with match or mismatch in human leukocyte antigens (HLA). Finally, manipulation of grafts (e.g., T cell depletion, CD34+ selection) may be used to modulate outcomes such as graft-versus-host disease (GVHD) and relapsed malignancy. All these variables impact the risks, timing, and outcomes of opportunistic infections, including invasive fungal infections (IFIs). Historically, infections due to Candida species have been predominately encountered soon after HSCT (prior to engraftment), while invasive mould infections, mainly invasive aspergillosis (IA), occur both early and later (after engraftment). Damage of the gastrointestinal tract mucosa and neutropenia due to conditioning regimens – particularly those designed to be myeloablative – represent the main risks for IFIs prior to engraftment. Neutrophil and T cell impairment associated with delayed engraftment or GVHD and associated therapies are the main risks for IFIs later after a HSCT.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hematopoietic Stem Cell Transplant
- Candida Species
- Antifungal Therapy
- Invasive Aspergillosis
- Fusarium Species
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Since the first hematopoietic stem cell transplant (HSCT) was performed more than 50 years ago, significant progress has been attained in the field, with changes in conditioning regimens, stem cell sources, and outcomes. The preparative regimen for HSCT may be fully myeloablative or less aggressive (nonmyeloablative). Different sources of stem cells have been used, including bone marrow (BM), peripheral blood stem cells (PBSCs), and cord blood. Stem cells may originate from an identical twin (syngeneic), one’s own self (autologous), and another donor (allogeneic). Allogeneic donors may be related (family members) or unrelated to the recipients, with match or mismatch in human leukocyte antigens (HLA). Finally, manipulation of grafts (e.g., T cell depletion, CD34+ selection) may be used to modulate outcomes such as graft-versus-host disease (GVHD) and relapsed malignancy. All these variables impact the risks, timing, and outcomes of opportunistic infections, including invasive fungal infections (IFIs). Historically, infections due to Candida species have been predominately encountered soon after HSCT (prior to engraftment), while invasive mould infections, mainly invasive aspergillosis (IA), occur both early and later (after engraftment). Damage of the gastrointestinal tract mucosa and neutropenia due to conditioning regimens – particularly those designed to be myeloablative – represent the main risks for IFIs prior to engraftment. Neutrophil and T cell impairment associated with delayed engraftment or GVHD and associated therapies are the main risks for IFIs later after a HSCT.
The incidence, epidemiology, and clinical outcomes of IFIs among HSCT recipients have changed over the last several decades as a result of changes in the host, preventive strategies, and antifungal therapies. While the frequency of invasive candidiasis has decreased since the early 1990s, increasing frequency of IA among HSCT recipients was noted during the 1990s [1–3]. In addition, IFIs due to moulds other than Aspergillus, namely the Zygomycetes and Fusarium species, have also been appreciated as a significant problem [4, 5]. The clinical presentation, dynamically changing epidemiology, and outcomes of the most frequently observed IFIs, namely candidiasis, aspergillosis, zygomycosis (also known as mucormycosis), and other moulds, will be discussed.
Invasive Candidiasis
Clinical Presentation
The main risks for Candida infections post HSCT include skin and mucosal membrane damage due to the presence of central intravenous catheters and conditioning-related gastrointestinal mucositis, respectively. Neutropenia before engraftment is another significant factor impacting risks for invasive candidiasis, and this is affected by the preparative regimens, stem cell source, HSCT manipulation, which is longer with ablative conditioning, and use of cord blood. HSCT recipients with Candida infections most commonly present with candidemia, which can be accompanied by sepsis. Candidemia may be sustained despite administration of appropriate therapy and rapidly disseminate to involve other organs. A diffuse maculopapular skin rash may be observed. As skin lesions in HSCT recipients may represent a number of different entities, it is pertinent to rapidly identify these findings and proceed with the appropriate diagnostic procedure to obtain a diagnosis in a timely fashion.
Hepatosplenic candidiasis is the result of Candida species invasion into the portal vasculature and subsequent dissemination to the liver and spleen. Clinical presentation frequently occurs when neutropenia resolves and inflammation develops. Blood cultures are negative in the vast majority of cases, and the diagnosis is usually made based on clinical suspicion. Patients present with right upper quadrant pain and tenderness on physical examination and have abnormal liver enzymes. Computed tomography (CT) or magnetic resonance imaging (MRI) of the abdomen may reveal liver, spleen, and/or kidney micronodular lesions. For a definitive diagnosis, biopsy of hepatic lesions is required, if feasible, which may reveal fungal forms consistent with Candida species. In clinical practice, diagnosis is frequently based on the presence of fever, abdominal pain, elevated alkaline phosphatase, and liver lesions on imaging. Notably, multiple other organisms (e.g., bacteria, filamentous fungi) may present similarly and should be appropriately ruled out. Finally, resolution of signs and symptoms may be late despite appropriate antifungal therapy.
Epidemiology
In the 1980s Candida species were appreciated to be the major fungal pathogen affecting HSCT recipients, with reported incidence rates between 11% and 18% [6–8]. This observation was followed by two large randomized, placebo-controlled trials testing primary antifungal prophylaxis with fluconazole after autologous and allogeneic HSCT [7, 9]. A significant decrease in IFIs, mainly due to Candida species, was observed in both studies. In one study, fluconazole administration was significantly associated with decreased overall mortality among allogeneic HSCT recipients [9, 10]. The above studies resulted in the widespread administration of fluconazole for antifungal prophylaxis in the early posttransplant period in the early 1990s and lower rates (4.7–7%) of invasive candidiasis among HSCT recipients [7–9, 11, 12]. Epidemiologic studies performed in European centers suggest that the incidence of candidiasis among allogeneic HSCT recipients has remained low (1–3%) since the 1980s [13–16] (Fig. 1). Differences in conditioning, transplant practices, and prophylactic strategies among different centers and countries may, in part, account for differences in epidemiology and outcomes.
In early studies, C. albicans counted for >50% of episodes, followed by C. tropicalis; C. glabrata and C. krusei were less frequently identified [6]. However, the epidemiology of Candida species among HSCT recipients has changed; the proportion of invasive infection caused by potentially azole-resistant Candida species, such as C. glabrata and C. krusei, has increased since the early 1990s, perhaps as a result of the selective pressure from extensive use of fluconazole [11, 12, 15–19] (Fig. 2). Wingard et al. reported a sevenfold increase between 1989 and 1990 in the frequency of invasive candidiasis due to C. krusei in patients with leukemia and HSCT recipients that received fluconazole for prophylaxis compared with those who did not receive prophylaxis (p = 0.0002) [17]. The same group reported higher rates of infection due to C. glabrata among leukemic patients and HSCT recipients receiving fluconazole [20]. Recent prospectively collected data from a multicenter registry on HSCT recipients who had IFIs between 2004 and 2007 suggest that species other than C. albicans are the most common cause of invasive candidiasis, with C. glabrata most frequently isolated (43.5%) [19]. Finally, resistance developing among traditionally azole-susceptible Candida species can occur. In one study, 5.3% of C. albicans isolated were found to be resistant to fluconazole, which is consistent with other concurrent reports [11, 21, 22].
Invasive Mould Infections
Clinical Presentation
HSCT recipients are at risk for invasive mould infections by virtue of their underlying disease, complications, and administered therapies. The most frequently encountered moulds affecting HSCT recipients include Aspergillus species, Fusarium species, Scedosporium species, and the agents of mucormycosis. HSCT recipients are exposed to moulds through direct skin inoculation and gastrointestinal tract invasion, but the predominant exposure is via inhalation. Normally, macrophages identify and kill conidia in the alveoli before they germinate and form hyphae. Therapies for GVHD, including high-dose corticosteroids and other immunosuppressive agents, significantly affect neutrophil and T cell function, both pertinent for containing mould infections, preventing tissue invasion, and clearing pulmonary inflammation [23–26]. Risk factors for IA appear to differ based on the timing after transplant, with neutropenia and GVHD being the major driving forces before and after engraftment, respectively (Table 1). Recent data suggest that polymorphisms in different pattern recognition receptors (e.g., Toll-like receptors) and other genes, such as those regulating plasminogen, in HSCT donors and recipients may also affect the risks for IA following HSCT [27–29].
Invasive mould infections among HSCT recipients may present with local invasion of lung and sinuses or with dissemination to multiple sites. Aspergillus species are the most frequent cause, identified in more than 90% of pulmonary invasive mould disease, followed by other filamentous fungi, including Fusarium species, Scedosporium species, and the agents of mucormycosis [4, 5, 30]. Clinical and radiologic presentations of pulmonary syndromes due to different moulds are often similar. Patients present with fever, cough, dyspnea, hemoptysis, and pleuritic chest pain [5, 31]. A “halo sign” (nodular lesion surrounded by a halo representing alveolar hemorrhage) may be identified in up to 93% of patients with acute pulmonary IA [32–37]. Notably, the halo sign is not specific for IA, as other infections can present similarly, including those caused by other moulds and bacteria, such as Pseudomonas species [38–40]. Radiographic patterns may be variable, especially in non-neutropenic hosts [35, 36, 41]. Abnormalities may include small or large nodules, patchy, segmental, or wedge-shaped consolidations, peribronchial infiltrates, tree-in-bud distribution, and cavities [35, 36] (Fig. 3). Recent studies suggest that allogeneic HSCT recipients with IA in the setting of GVHD may present with variable radiographic findings, such as bronchopneumonia or focal infiltrates rather than isolated nodules [41]. Retrospective data suggest that presence of concomitant sinusitis, multiple (>10) pulmonary nodules, and pleural effusion may be predictive of pulmonary mucormycosis [42]. Because therapies differ, aggressive diagnostic workup, including bronchoscopy and testing for galactomannan, should be promptly initiated to allow the accurate diagnosis of invasive mould infections and initiation of appropriate therapies.
Radiographic presentations of aspergillosis in allogeneic HSCT recipients. Appearance can vary from (a) isolated pulmonary lesions, to (b) cavitary lesions, to (c and d) infiltrates. Infiltrates are frequently pleural based (c and d), and ground glass changes can appear surrounding nodular lesions (a) or as an isolated finding (d)
Sinusitis is a common manifestation of invasive mould infections among HSCT recipients, with Aspergillus species and the Zygomycetes representing the major pathogens. Sinus disease can be very subtle and is occasionally found on routine sinus CT, but most patients present with facial tenderness, congestion, and fever. A CT scan showing sinus disease is not specific, as multiple different moulds and bacterial pathogens can cause sinusitis. Definitive diagnosis relies on biopsy and culture of the affected tissue, if feasible. These organisms may invade and spread into the orbits or brain causing significant necrosis of the palate, often presenting as a necrotic, black eschar. The absence of distinct lesions upon direct visualization of the sinuses should not exclude tissue biopsy.
Invasive mould infections among HSCT recipients can spread to other contiguous sites or rapidly disseminate to skin, leading to multiple papular to nodular necrotic lesions, and to other organs, including the lungs and brain [4, 43–48]. Fusarium species can sporulate in vivo and produce adventitious forms that disseminate and are able to grow in blood cultures [4, 49]. A classic presentation of fusariosis is that of disseminated papular-to-ulcerated skin lesions and blood cultures positive for a filamentous organism [48, 50]. Other filamentous organisms, predominately S. prolificans, can also be detected in blood cultures [45, 51].
Epidemiology
In the 1990s data from the Fred Hutchinson Cancer Research Center in Seattle, Washington, suggested that the incidence of IA among allogeneic HSCT recipients increased compared to the 1980s (11.2% vs 5.7%, respectively; p = 0.02) [1]. Multiple centers have since reported that the rates of IA among allogeneic HSCT recipients remained as high as 10% during the 1990s and early 2000s [2–4, 13, 14, 52–54]. All HSCT recipients are not equally affected by Aspergillus species. The incidence of IA differs based on factors predicting severity and duration of neutropenia and GVHD: (1) type of transplant (lower among autologous [0–5.3%] compared to allogeneic HSCT [10%]), (2) HLA match (higher in HLA mismatched and unrelated donors [10.5% vs matched related 7.3%]), and (3) graft manipulation (higher in T-cell-depleted [4–16%] vs unmanipulated grafts [2.2–7%]) [2, 4, 15, 53–58]. In contrast, differences in the conditioning regimen do not seem to significantly affect the incidence of IA postallogeneic HSCT, with recipients of nonablative conditioning regimens exhibiting high risks during GVHD [57, 59–62].
Although less frequently encountered, the incidence of mucormycosis among HSCT recipients significantly increased from 0.25% (10 cases among 4,020 HSCT recipients) between 1989 and 1998 to 1.5% (13 of 834) from 2002 to 2004 in one center [30]. Similarly, other groups have reported a relative increase in the frequency of infections due to moulds other than IA among HSCT recipients since the 1990s (Fig. 3) [4, 15, 19, 30].
Despite the routine administration of prophylactic therapy and aggressive monitoring of HSCT recipients, almost one-third of IA cases are observed prior to engraftment, particularly among autologous HSCT recipients [3, 15, 19]. However, the majority of cases of other mould infections occur post engraftment, during periods of acute or chronic GVHD [3, 4, 19, 30, 48, 63, 64]. In one series, all cases of zygomycosis and fusariosis occurred after engraftment, with >50% diagnosed after day 100 [3].
A. fumigatus has been the most commonly isolated Aspergillus species in HSCT recipients with IA, ranging from 22.1 to 80.5% in different series (Fig. 4) [1, 4, 13–15, 19, 52]. The frequency of infections with A. flavus, A. terreus, and A. niger has varied in different studies, but these species are noted much less commonly than A. fumigatus [1, 4, 13–15, 19, 52, 57]. Clusters of cases of IA due to A. ustus or A. calidoustus, both potentially multi-drug-resistant pathogens, have been reported among HSCT recipients [65–67]. Recently infections caused by previously unrecognized species within the section Fumigati, specifically A. lentulus, Neosartorya udagawae, and N. pseudofischeri, have been reported in HSCT recipients from multiple centers [68–72]. These species include several that exhibit high resistance profiles to multiple antifungal agents, including voriconazole and amphotericin B, which raises questions regarding the potential clinical significance of antifungal resistance in cases with poor outcomes. In addition, A. terreus has been reported to be resistant to amphotericin B [73–75].
The above observations underscore the importance of establishing a microbiologic diagnosis for IA when feasible. Unfortunately, recent reports suggest that Aspergillus species remain either unknown or not identified in as many as 49–62% of cases (Fig. 4) [15, 19]. This may, in part, be related to the availability of noninvasive diagnostic tests such as CT scans and galactomannan assays that provide a possible or probable diagnosis without requiring an invasive procedure such as bronchoscopy and lung tissue biopsy. Although this may facilitate and, at times, expedite the diagnosis of IA, the emergence of new Aspergillus species with different susceptibility profiles and azole resistance among Aspergillus species should be taken into consideration when treating HSCT recipients with IA, particularly those that fail to respond to the administered therapies.
Prevention
Therapy of IFIs entails both preventive strategies as well as treatment of established infection. In HSCT recipients, prevention of infection is critical. It can be argued that the most important therapeutic advances in the supportive care of HSCT recipients within the last decade have occurred due to the effective measures to prevent gram-negative bacterial infections, CMV disease, and candidiasis. One multivariable analysis of outcomes among unrelated donor HSCT recipients with chronic myelogenous leukemia found that two important predictors of overall survival were receipt of ganciclovir for preventing CMV infection and fluconazole for preventing candidiasis [76].
Strategies to prevent fungal infections may rely on administration of antifungals “prophylactically” in high-risk patients, “empirically” in patients with fever during neutropenia, and “preemptively” in patients in whom a more specific indicator of fungal infection is detected. There are advantages and disadvantages to each of these strategies.
Prophylaxis
Prophylactic administration of azole antifungal drugs has become common practice in HSCT recipients. Several randomized trials performed in the early 1990s showed efficacy in preventing candidiasis [7, 9]. The first large randomized trial that compared fluconazole with placebo until neutrophil engraftment in both autologous and allogeneic HSCT recipients showed that fluconazole was associated with decreased fungal infections and fungal infection-related deaths, but there was no difference in overall survival [7]. A second trial compared fluconazole with placebo, both administered for a longer period of time during GVHD in allograft recipients [9]. The results of this trial, and a subsequent long-term follow-up study of the same randomized cohort, verified that fluconazole decreased infections, infection-related deaths, and the overall mortality rate of allograft recipients [9, 10]. Another study documented that the prophylactic use of fluconazole decreased the incidence of hepatosplenic candidiasis in HSCT recipients [77]. Optimal doses and duration of fluconazole administration continue to be a matter of debate.
Unfortunately, the successful prevention of fungal infections has been dampened due to the emergence of azole-resistant Candida species and moulds. Most reports suggest that liberal azole use is associated with selection of resistant Candida species, namely C. glabrata and C. krusei [11, 78, 79]. Perhaps more importantly, the incidence of IA has increased in many centers, with this organism surpassing yeasts as the cause of infection-related mortality. The estimated incidence of IA approximates 10–15% in most HSCT centers, with the majority of infections diagnosed late after engraftment – during GVHD [1, 53, 80]. Due to this shift in epidemiology, efforts turned toward establishing a preventive strategy that would encompass moulds as well as yeasts.
Several studies were performed to determine if itraconazole was better than placebo, amphotericin B, or fluconazole for preventing infection in neutropenic patients [81–83]. Although the results of these studies suggested promise regarding prevention of IA, the studies were not performed in high-risk HSCT recipients. Two trials that compared outcomes of HSCT patients who received either itraconazole or fluconazole for at least 100 days after transplant demonstrated the potential utility of itraconazole in preventing invasive mould infections; however, the rate of toxicities was high [84]. Two large studies have demonstrated utility of posaconazole in preventing IFI, especially those caused by moulds, in HSCT patients with GVHD and in patients who are neutropenic following therapy for acute myelocytic leukemia or myelodysplastic syndrome [85, 86]. Another large trial that compared outcomes of voriconazole to fluconazole in “standard risk” HSCT recipients has been completed, with numbers of IFI suggesting potential utility of the mould-active drug [87]. Finally, other methods of administering mould-active antifungals, such as inhaled lipid amphotericin B formulations, may provide utility in preventing IA, but this practice is not yet the standard of care [88].
Empirical and Preemptive Therapy
Another approach to prevention of IFIs is to administer antifungal agents to neutropenic patients with fever that persists despite antibiotics. This practice was established in the 1980s, with the performance of two randomized trials that compared outcomes of febrile neutropenic patients who received either no antifungal therapy or amphotericin B deoxycholate [89, 90]. Both trials showed that amphotericin B was associated with fewer fungal infections. Which antifungal is best for treating fever during neutropenia has been the subject of multiple studies performed subsequently. Most of these studies did not enroll enough HSCT patients to compare efficacy of preventing infection, especially in people already receiving some type of systemically absorbed antifungal drug as prophylaxis [91]. Evaluation of toxicity end points and composite variables showed efficacy, but fewer toxicities with empirical therapy with fluconazole, itraconazole, and lipid formulations of amphotericin B compared to amphotericin B deoxycholate [91, 92]. Whether the toxicity concerns are great enough to warrant the use of the more expensive formulations is a matter of continued debate. Expense has limited their widespread adoption in many large cancer centers. Mould-active triazole antifungal drugs, such as voriconazole and lipid amphotericin B formulations, may be appropriate for treatment of fever during neutropenia in HSCT recipients who have received fluconazole prophylactically [93, 94]. However, fever during neutropenia is not frequently caused by fungal infections in patients who are receiving prophylaxis. Recent studies have found that <5% of high-risk HSCT recipients who are febrile while receiving systemically absorbed antifungal prophylaxis actually had fungal infections as a cause of their fevers [94].
Preemptive is a term used to describe therapy administered early during the course of infection in some settings in an attempt to prevent the development of disease. For CMV, strategies using pp65 antigenemia and PCR to identify infection in HSCT recipients have been very successful at preventing CMV disease and attributable mortality [95]. The development of new diagnostic assays for fungal infections may allow for the similar development of preventive strategies. Early studies focused on the use of serial CT-scanning to initiate early antifungal therapy. Although one small study noted that screening with sensitive radiographic tests may lead to decreased Aspergillus-associated mortality compared to historic controls, the costs and inability to routinely screen for long durations after HSCT have limited the applicability of this approach [96]. Other studies have reported that screening with PCR or antigenemia assays may permit establishment of an earlier diagnosis of aspergillosis [97].
Recently, two large studies have evaluated, in a comparative fashion, the potential utility of preemptive therapy. In one, patients were randomized to “standard care” versus care augmented with PCR-based screening. Results did not demonstrate clear benefits in the PCR-based approach; more antifungals were used and there was no large difference in clinical outcomes [98]. Another study randomized neutropenic patients to receive either “standard care” with empirical therapy or an approach that utilized composite clinical and laboratory criteria, including galactomannan screening tests, to trigger the initiation of antifungal therapy [99]. In that study, there were trends to fewer IFIs, particularly those caused by Candida species, in the standard “empirical” therapy arm, suggesting that a preemptive approach driven by these clinical criteria may not be sufficient for early therapy in patients who are not receiving fluconazole as prophylactic therapy. While these studies have tremendous importance in providing first efforts for comparative evaluation of preemptive approaches, neither can be considered to provide definitive results, and more efforts are needed to optimize preventative strategies.
Other Methods
Aside from prophylactic or preemptive antifungal administration, other methods to prevent IFIs in HSCT recipients include avoiding exposure and minimizing the severity or duration of risk. Aspergillus and other moulds are most frequently acquired from the hospital or external environment, although a certain number of HSCT patients who develop disease early after transplant appear to have reactivation from a previously acquired infection. Efforts to minimize exposure to Aspergillus species during the periods of risk have focused on air filtration, either through laminar airflow or high-efficiency particulate air (HEPA) filtration. No randomized trials have been performed to measure the utility of these measures; however, several multivariable models to define risk factors for IA have shown that both may be useful to prevent infection early after transplant [1, 100, 101]. The important limitation to using containment practices is that they are only useful during the period of time during which they are employed. Many experienced clinicians have recently questioned the utility of laminar air flow at a time when disease is most frequently acquired outside of the hospital, late after transplant.
The environmental source of Aspergillus species has also been called into question with the results of several recent studies suggesting that moulds may be a common contaminant in hospital water supplies [102–106]. The findings of Aspergillus (including A. fumigatus) and Fusarium species in hospital water supplies, with high amounts of spores recovered in and around patient bathrooms, have led some clinicians to suggest that it may be prudent to avoid aerosolization of water through showering during the period of high risk. Other studies have reported outbreaks of hospital-acquired A. terreus infections from apparent association with vegetation (plants) within the hospital [107].
Although the exact environmental source of moulds is rarely determined, even during periods of outbreaks, most centers have instituted infection control practices that focus on air monitoring, patient avoidance of vegetation and food known to have high mould content, such as pepper, and patient avoidance of activities that are associated with aerosolization of conidia, including mowing the lawn, gardening, vacuuming, etc. More studies are necessary to determine whether other infection control practices can minimize infection late after HSCT.
It may also be possible to prevent infection by minimizing the severity and the duration of risks. Efforts to prevent fungal infections have focused on the roles of immune modulators to decrease neutropenia. Few placebo-controlled randomized studies employing hematopoietic growth factors or granulocyte infusions to prevent infection have been performed; however, the results of small randomized trials and risk factor analyses suggest that minimizing the period of neutropenia is associated with fewer Candida and Aspergillus infections [108]. Optimizing risk reduction during the GVHD period is important, and recent risk factor analyses have shown that factors other than neutropenia, namely corticosteroid exposure, viral (CMV) infections, and lymphopenia may be the strongest predictors of post-engraftment aspergillosis [2, 53]. Minimizing the use of corticosteroids for GVHD is prudent, when possible.
Treatment
For a long time, clinicians have balanced the need for establishing a microbial diagnosis of fungal infections with the desire to minimize complications associated with invasive procedures. Mould infections are especially difficult to diagnose with certainty without performance of some type of invasive procedure, such as bronchoalveolar lavage or lung biopsy. Although complications are rare subsequent to lavage, lung biopsy may elicit hemorrhage and infection in neutropenic, thrombocytopenic patients [109]. One may treat patients with suggestive radiographic lesions presumptively with antifungal agents; however, without a definitive diagnosis, there is a substantial risk of administering misdirected therapy. Establishing a microbial diagnosis has become especially important now that multiple effective antifungal drugs other than amphotericin B deoxycholate are available for use.
Treatment of Candidiasis
Therapy of infections caused by Candida depends on the causative species. While fluconazole has been shown to be equivalent to amphotericin B for treatment of candidemia in nonneutropenic patients, candidiasis in neutropenic patients and HSCT recipients is frequently caused by azole-resistant organisms, such as C. glabrata or C. krusei [1, 110, 111]. In these patients, even C. albicans may become resistant to fluconazole through continued exposure during prophylactic therapy [11, 78, 112]. For this reason, and because azole drugs, especially fluconazole and itraconazole, have not been evaluated extensively for therapy of invasive infection in severely immunosuppressed patients, standard therapy of bloodstream infection should include an amphotericin B formulation or an echinocandin. Therapy with lipid formulations of amphotericin B or one of the echinocandins is supported by the results of randomized trials, in which these agents – caspofungin, micafungin, and anidulafungin – were compared with amphotericin B, lipid formulations of amphotericin B, or fluconazole. Results of these studies suggest comparable efficacy, with potentially fewer toxicities associated with echinocandin therapy [113–116]. Duration of therapy for candidemia should continue for at least 2 weeks after the first negative blood culture in order to minimize the likelihood of metastatic sequelae, such as chorioretinitis and endocarditis [117].
Multiple antifungal drugs, including fluconazole, have been shown to be effective for the treatment of hepatosplenic candidiasis, as most infections are caused by susceptible C. albicans. Although no randomized studies have been performed to identify the best antifungal agent for treatment, most clinicians favor the use of an amphotericin B formulation as initial therapy, followed by maintenance therapy with an azole antifungal until resolution of lesions occurs [118]. Anecdotal success has been reported using echinocandin antifungals for therapy of hepatosplenic candidiasis as well, which is consistent with the distribution of these drugs to the liver [119]. The reader is referred to a detailed discussion of treatment of Candida infections in Chap. 11.
Treatment of Mould Infections
Historically, the only effective therapy for mould infections was amphotericin B. The introduction of new triazoles and echinocandins has now challenged this “gold standard,” with evidence that alternative therapy may be indicated for non-Aspergillus mould infections and for treatment of infection that does not initially respond to amphotericin B formulations. No randomized studies have compared therapy with amphotericin B deoxycholate to lipid formulations of amphotericin B, although the latter formulations have fewer nephrotoxicities and infusion-related toxicities, both of which may occur at high frequency in HSCT recipients [94, 120]. Differentiating infections with Aspergillus species and other mould pathogens has become critical, as optimal therapy for each may differ. While amphotericin B remains the current therapy of choice for zygomycosis, several retrospective open-label studies suggest that the best outcomes result from therapy with high doses of lipid amphotericin B formulations in conjunction with aggressive surgical debridement of involved tissue and granulocyte stimulation or replacement [5, 121]. Emerging data indicate that optimal therapy for Fusarium species and Scedosporium species may be a mould-active triazole antifungal drug. Reports of outcomes using voriconazole and posaconazole have been encouraging, leading some experienced clinicians to suggest that these drugs should now be considered first-line therapy for these opportunistic filamentous mould infections.
The historic algorithm for treating IA has been to administer amphotericin B deoxycholate as initial (primary) therapy and then to switch to either a mould-active triazole, an echinocandin, or a lipid formulation of amphotericin B if the patient develops serious toxicities or fails to respond to initial therapy. Only one randomized, double-blind study has been performed to evaluate the use of a lipid formulation of amphotericin B as primary therapy for IA. In this study, amphotericin B colloidal dispersion (ABCD) at a dose of 6 mg/kg/day was equivalent in efficacy to amphotericin B deoxycholate, 1.0–1.5 mg/kg/day, but was associated with significantly less nephrotoxicity [122]. Despite the lack of data to support superior efficacy, the lipid formulations are favored by many clinicians because of their potential to deliver high doses of amphotericin B to target tissues without an increase in toxicities. A recent study that compared two doses of liposomal amphotericin B (3 mg/kg vs 10 mg/kg) did not demonstrate better outcomes with the higher dose, in which there were also more toxicities [123]. Salvage studies have shown that voriconazole, posaconazole, and caspofungin are associated with successful therapy when used as a second-line agent in approximately 40% of patients.
The algorithm for standard therapy for IA changed with trials that compared amphotericin B with voriconazole. Although the response rates of aspergillosis in allogeneic HSCT recipients using amphotericin B formulations only approximated 10–15%, responses were noted in 26% of allogeneic HSCT patients who received voriconazole either as primary or secondary therapy [33, 124–126]. More convincing evidence that voriconazole may be an effective therapy comes from the randomized trial that compared voriconazole as primary therapy with the standard algorithm of amphotericin B followed by the investigator’s choice of other licensed antifungal therapy. The results of this trial indicate that clinical outcomes and overall survival rates improve with voriconazole used as primary therapy [127].
In vitro and in vivo studies suggest that combination antifungal therapy, employing an echinocandin with either a mould-active triazole or an amphotericin B formulation for IA, may be more efficacious [128–131]. Retrospective data from the Fred Hutchinson Cancer Center showed that voriconazole combined with caspofungin as salvage treatment of IA in HSCT recipients, most of whom had received an allogeneic transplant, was associated with improved 3-month survival compared to voriconazole alone [132]. In multivariate model analyses, salvage therapy with the combination of voriconazole and caspofungin was associated with reduced mortality rates, compared with therapy with voriconazole (HR, 0.28; 95% CI, 0.28–0.92; p = 0.01), independent of other prognostic variables [132]. A prospective double-blind, randomized, multicenter, international study to address the efficacy of combination therapy of voriconazole with an echinocandin in HSCT recipients and high-risk hematologic malignancy patients is currently underway (Clinical Trials Gov: NCT00531479).
Recently, attention has turned toward the potential need for therapeutic drug monitoring to assure “good” levels of voriconazole. Studies have shown that approximately 20% of patients do not have measurable levels of the drug despite standard dosing, and if levels are too high, there may be a higher incidence of neurotoxicity and/or hepatotoxicity [133–135]. While the optimal algorithm for dosing and following up on voriconazole has yet to be defined, levels have to at least be considered, especially in patients who are not responding or who have demonstrated toxicities. Clinical studies evaluating the safety and efficacy of the various combinations, especially combining voriconazole with an echinocandin, are underway. Common practice is to continue antifungal therapy for the duration of time that the patient is receiving immunosuppressive drugs. Allogeneic HSCT recipients with pulmonary mould infections should receive prolonged antifungal therapy, at least as long as they are receiving high doses of corticosteroid therapy for GVHD. The cumulative dose and duration of corticosteroid exposure are closely associated with negative outcomes of antifungal therapy; consequently, every effort should be made to minimize exposure to corticosteroids [33].
Adjunctive Therapy
The utility of adjunctive therapy using immune modulating agents, such as hematopoietic growth factors or granulocyte transfusions, continues to be a matter of debate. No definitive randomized studies have been performed. Up to now, studies have only justified the safety of immunomodulating therapy, with anecdotes suggesting efficacy. Granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) are used frequently in patients who are neutropenic and have invasive fungal infections. Adjunctive immunotherapy may be especially important for treatment of mould infections characterized by a large circulating fungal burden and relative resistance to antifungal drugs, as with disseminated fusariosis. In addition, other reports emphasize that outcomes of therapy for zygomycosis improve with rapid resolution of neutropenia [5]. The potential utility of neutrophil transfusions as adjunctive therapy has been rejuvenated with the development of G-CSF-primed community donor transfusions [136]. Studies evaluating the safety and efficacy of such transfusions, and the use of interferon-gamma for adjunctive therapy of aspergillosis in neutropenic patients, are either ongoing or in development.
The role of surgical debridement of pulmonary fungal lesions is also a matter of debate, as no randomized studies have been performed, and noncontrolled studies are impacted by selection bias. Anecdotal reports and case series suggest that there is a definite role for surgical resection in patients who present with severe hemoptysis and fungal lesions abutting large vessels, and in patients in whom further myelosuppressive therapy is intended [137]. In many centers, patients who present pretransplant with isolated pulmonary fungal lesions undergo resection when possible. This practice is justified by the results of case series that suggest that recurrent fungal infection occurs less frequently in patients who have undergone surgical resection before myeloablative therapy. As mentioned above, surgical resection of infection caused by Zygomycetes appears to be strongly associated with successful therapy.
Clinical Outcomes
Clinical outcomes among HSCT recipients with invasive candidiasis remain poor, in part due to the underlying compromised immune status and organ function of these patients. Mortality rates ranged between 22% and 40% during the 1980–1990s [6, 8, 11]. In a US multicenter study performed between 2004 and 2007, the crude 12-week mortality rate among HSCT recipients with invasive candidiasis was found to be 48.9% [19]. Although less frequently encountered due to routine prophylaxis with fluconazole, invasive candidiasis appears to be a significant factor affecting outcomes among HSCT recipients. More aggressive HSCT practices, such as performing high-risk transplants, might have resulted in sicker patients with worse prognoses due to their comorbidities and prolonged immunosuppressed state. Estimating the actual attributable mortality of invasive candidiasis in this population is difficult.
The reported 4–12-month mortality rates among HSCT recipients with IA have historically been as high as 90% [1, 2, 4, 33]. Recent data suggest that outcomes may be improving, with 12-week overall survival ranging from 44 to 64.5% [19, 138, 139]. Improved contemporary clinical outcomes may in part reflect improved diagnostic modalities leading to earlier recognition of IA and prompt initiation of antifungal treatment at an earlier stage. In fact, early diagnosis of pulmonary IA based on chest CT scan was associated with improved 12-week survival rate (71% vs 53%, p < 0.01) and treatment response (52% vs 29%, p < 0.001) [37]. The availability of potent and well-tolerated antifungal agents might have also allowed for earlier treatment initiation and improved outcomes. Different centers have reported an association between improved survival rates and voriconazole administration [138, 139]. In addition, transplant-related variables, such as nonmyeloablative conditioning and use of peripheral blood cells as a stem cell source, have been associated with improved survival rates [138, 139]. In contrast, predictors of mortality among HSCT recipients with IA have included younger age, HLA-mismatched donors, neutropenia, monocytopenia, abnormal renal and liver function, disseminated disease, presence of a pleural effusion, administration of corticosteroids, and uncontrolled GVHD [19, 139, 140].
While the clinical outcomes of IA appear to be improving, survival among HSCT recipients with mucormycosis and other mould infections remains poor, with reported mortality rates ranging between 64% and 100% [4, 19, 121]. Historically, HSCT recipients with an invasive infection due to Fusarium species have had poor outcomes, with survival rates ranging between 13% and 21% [4, 48, 141]. Similarly, infections with Scedosporium species have been associated with 30-day mortality rates reaching 100% [4]. The prolonged duration of profound immunosuppression of HSCT recipients, cumbersome and frequent late diagnosis of these infections, and limited treatment options likely contribute to the poor outcomes associated with mould infections.
References
Wald A, Leisenring W, van Burik JA, Bowden RA. Epidemiology of Aspergillus infections in a large cohort of patients undergoing bone marrow transplantation. J Infect Dis. 1997;175(6):1459–66.
Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood. 2002;100(13):4358–66.
Garcia-Vidal C, Upton A, Kirby KA, Marr KA. Epidemiology of invasive mould infections in allogeneic stem cell transplant recipients: biological risk factors for infection according to time after transplantation. Clin Infect Dis. 2008;47(8):1041–50.
Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34(7):909–17.
Kontoyiannis DP, Wessel VC, Bodey GP, Rolston KV. Zygomycosis in the 1990s in a tertiary-care cancer center. Clin Infect Dis. 2000;30(6):851–6.
Goodrich JM, Reed EC, Mori M, et al. Clinical features and analysis of risk factors for invasive candidal infection after marrow transplantation. J Infect Dis. 1991;164(4):731–40.
Goodman JL, Winston DJ, Greenfield RA, et al. A controlled trial of fluconazole to prevent fungal infections in patients undergoing bone marrow transplantation. N Engl J Med. 1992;326(13):845–51.
Meyers JD. Fungal infections in bone marrow transplant patients. Semin Oncol. 1990;17(3 Suppl):10–3.
Slavin MA, Osborne B, Adams R, et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation-a prospective, randomized, double-blind study. J Infect Dis. 1995;171(6):1545–52.
Marr KA, Seidel K, Slavin MA, et al. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Blood. 2000;96(6):2055–61.
Marr KA, Seidel K, White TC, Bowden RA. Candidemia in allogeneic blood and marrow transplant recipients: evolution of risk factors after the adoption of prophylactic fluconazole. J Infect Dis. 2000;181(1):309–16.
Safdar A, van Rhee F, Henslee-Downey JP, Singhal S, Mehta J. Candida glabrata and Candida krusei fungemia after high-risk allogeneic marrow transplantation: no adverse effect of low-dose fluconazole prophylaxis on incidence and outcome. Bone Marrow Transplant. 2001;28(9):873–8.
Jantunen E, Ruutu P, Niskanen L, et al. Incidence and risk factors for invasive fungal infections in allogeneic BMT recipients. Bone Marrow Transplant. 1997;19(8):801–8.
Martino R, Subira M, Rovira M, et al. Invasive fungal infections after allogeneic peripheral blood stem cell transplantation: incidence and risk factors in 395 patients. Br J Haematol. 2002;116(2):475–82.
Pagano L, Caira M, Nosari A, et al. Fungal infections in recipients of hematopoietic stem cell transplants: results of the SEIFEM B-2004 study-Sorveglianza Epidemiologica Infezioni Fungine Nelle Emopatie Maligne. Clin Infect Dis. 2007;45(9):1161–70.
Jantunen E, Nihtinen A, Volin L, et al. Candidaemia in allogeneic stem cell transplant recipients: low risk without fluconazole prophylaxis. Bone Marrow Transplant. 2004;34(10):891–5.
Wingard JR, Merz WG, Rinaldi MG, Johnson TR, Karp JE, Saral R. Increase in Candida krusei infection among patients with bone marrow transplantation and neutropenia treated prophylactically with fluconazole. N Engl J Med. 1991;325(18):1274–7.
Persons DA, Laughlin M, Tanner D, Perfect J, Gockerman JP, Hathorn JW. Fluconazole and Candida krusei fungemia. N Engl J Med. 1991;325(18):1315.
Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infection in adult hematopoietic stem cell transplant recipients: analysis of multicenter prospective antifungal therapy (PATH) alliance registry. Clin Infect Dis. 2009;48(3):265–73.
Wingard JR, Merz WG, Rinaldi MG, Miller CB, Karp JE, Saral R. Association of Torulopsis glabrata infections with fluconazole prophylaxis in neutropenic bone marrow transplant patients. Antimicrob Agents Chemother. 1993;37(9):1847–9.
Nolte FS, Parkinson T, Falconer DJ, et al. Isolation and characterization of fluconazole- and amphotericin B-resistant Candida albicans from blood of two patients with leukemia. Antimicrob Agents Chemother. 1997;41(1):196–9.
Mori T, Matsumura M, Kanamaru Y, et al. Myelofibrosis complicated by infection due to Candida albicans: emergence of resistance to antifungal agents during therapy. Clin Infect Dis. 1997;25(6):1470–1.
Brummer E, Kamberi M, Stevens DA. Regulation by granulocyte-macrophage colony-stimulating factor and/or steroids given in vivo of proinflammatory cytokine and chemokine production by bronchoalveolar macrophages in response to Aspergillus conidia. J Infect Dis. 2003;187(4):705–9.
Grazziutti ML, Rex JH, Cowart RE, Anaissie EJ, Ford A, Savary CA. Aspergillus fumigatus conidia induce a Th1-type cytokine response. J Infect Dis. 1997;176(6):1579–83.
Hebart H, Bollinger C, Fisch P, et al. Analysis of T-cell responses to Aspergillus fumigatus antigens in healthy individuals and patients with hematologic malignancies. Blood. 2002;100(13):4521–8.
Philippe B, Ibrahim-Granet O, Prevost MC, et al. Killing of Aspergillus fumigatus by alveolar macrophages is mediated by reactive oxidant intermediates. Infect Immun. 2003;71(6):3034–42.
Bochud PY, Chien JW, Marr KA, et al. Toll-like receptor 4 polymorphisms and aspergillosis in stem-cell transplantation. N Engl J Med. 2008;359(17):1766–77.
Zaas AK, Liao G, Chien JW, et al. Plasminogen alleles influence susceptibility to invasive aspergillosis. PLoS Genet. 2008;4(6):e1000101.
Kesh S, Mensah NY, Peterlongo P, et al. TLR1 and TLR6 polymorphisms are associated with susceptibility to invasive aspergillosis after allogeneic stem cell transplantation. Ann NY Acad Sci. 2005;1062:95–103.
Kontoyiannis DP, Lionakis MS, Lewis RE, et al. Zygomycosis in a tertiary-care cancer center in the era of aspergillus-active antifungal therapy: a case-control observational study of 27 recent cases. J Infect Dis. 2005;191(8):1350–60.
Hachem R, Sumoza D, Hanna H, Girgawy E, Munsell M, Raad I. Clinical and radiologic predictors of invasive pulmonary aspergillosis in cancer patients: should the European Organization for Research and Treatment of Cancer/Mycosis Study Group (EORTC/MSG) criteria be revised? Cancer. 2006;106(7):1581–6.
Kuhlman JE, Fishman EK, Siegelman SS. Invasive pulmonary aspergillosis in acute leukemia: characteristic findings on CT, the CT halo sign, and the role of CT in early diagnosis. Radiology. 1985;157(3):611–4.
Ribaud P, Chastang C, Latge JP, et al. Survival and prognostic factors of invasive aspergillosis after allogeneic bone marrow transplantation. Clin Infect Dis. 1999;28(2):322–30.
Caillot D, Couaillier JF, Bernard A, et al. Increasing volume and changing characteristics of invasive pulmonary aspergillosis on sequential thoracic computed tomography scans in patients with neutropenia. J Clin Oncol. 2001;19(1):253–9.
Kami M, Kishi Y, Hamaki T, et al. The value of the chest computed tomography halo sign in the diagnosis of invasive pulmonary aspergillosis. An autopsy-based retrospective study of 48 patients. Mycoses. 2002;45(8):287–94.
Horger M, Hebart H, Einsele H, et al. Initial CT manifestations of invasive pulmonary aspergillosis in 45 non-HIV immunocompromised patients: association with patient outcome? Eur J Radiol. 2005;55(3):437–44.
Greene RE, Schlamm HT, Oestmann JW, et al. Imaging findings in acute invasive pulmonary aspergillosis: clinical significance of the halo sign. Clin Infect Dis. 2007;44(3):373–9.
Greene R. The radiological spectrum of pulmonary aspergillosis. Med Mycol. 2005;43 Suppl 1:S147–54.
Primack SL, Hartman TE, Lee KS, Muller NL. Pulmonary nodules and the CT halo sign. Radiology. 1994;190(2):513–5.
Lee YR, Choi YW, Lee KJ, Jeon SC, Park CK, Heo JN. CT halo sign: the spectrum of pulmonary diseases. Br J Radiol. 2005;78(933):862–5.
Kojima R, Tateishi U, Kami M, et al. Chest computed tomography of late invasive aspergillosis after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005;11(7):506–11.
Chamilos G, Marom EM, Lewis RE, Lionakis MS, Kontoyiannis DP. Predictors of pulmonary zygomycosis versus invasive pulmonary aspergillosis in patients with cancer. Clin Infect Dis. 2005;41(1):60–6.
Martino P, Gastaldi R, Raccah R, Girmenia C. Clinical patterns of Fusarium infections in immunocompromised patients. J Infect. 1994;28 Suppl 1:7–15.
Jahagirdar BN, Morrison VA. Emerging fungal pathogens in patients with hematologic malignancies and marrow/stem-cell transplant recipients. Semin Respir Infect. 2002;17(2):113–20.
Husain S, Munoz P, Forrest G, et al. Infections due to Scedosporium apiospermum and Scedosporium prolificans in transplant recipients: clinical characteristics and impact of antifungal agent therapy on outcome. Clin Infect Dis. 2005;40(1):89–99.
Garcia-Arata MI, Otero MJ, Zomeno M, de la Figuera MA, de las Cuevas MC, Lopez-Brea M. Scedosporium apiospermum pneumonia after autologous bone marrow transplantation. Eur J Clin Microbiol Infect Dis. 1996;15(7):600–3.
Safdar A, Papadopoulos EB, Young JW. Breakthrough Scedosporium apiospermum (Pseudallescheria boydii) brain abscess during therapy for invasive pulmonary aspergillosis following high-risk allogeneic hematopoietic stem cell transplantation. Scedosporiasis and recent advances in antifungal therapy. Transpl Infect Dis. 2002;4(4):212–7.
Nucci M, Marr KA, Queiroz-Telles F, et al. Fusarium infection in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2004;38(9):1237–42.
Liu K, Howell DN, Perfect JR, Schell WA. Morphologic criteria for the preliminary identification of Fusarium, Paecilomyces, and Acremonium species by histopathology. Am J Clin Pathol. 1998;109(1):45–54.
Dignani MC, Anaissie E. Human fusariosis. Clin Microbiol Infect. 2004;10 Suppl 1:67–75.
Idigoras P, Perez-Trallero E, Pineiro L, et al. Disseminated infection and colonization by Scedosporium prolificans: a review of 18 cases, 1990–1999. Clin Infect Dis. 2001;32(11):E158–65.
Baddley JW, Stroud TP, Salzman D, Pappas PG. Invasive mould infections in allogeneic bone marrow transplant recipients. Clin Infect Dis. 2001;32(9):1319–24.
Grow WB, Moreb JS, Roque D, et al. Late onset of invasive Aspergillus infection in bone marrow transplant patients at a university hospital. Bone Marrow Transplant. 2002;29(1):15–9.
Cornet M, Fleury L, Maslo C, Bernard JF, Brucker G. Invasive aspergillosis surveillance network of the assistance Publique-Hopitaux de Paris. Epidemiology of invasive aspergillosis in France: a six-year multicentric survey in the greater Paris area. J Hosp Infect. 2002;51(4):288–96.
Jantunen E, Salonen J, Juvonen E, et al. Invasive fungal infections in autologous stem cell transplant recipients: a nation-wide study of 1188 transplanted patients. Eur J Haematol. 2004;73(3):174–8.
Mihu CN, King E, Yossepovitch O, et al. Risk factors and attributable mortality of late aspergillosis after T-cell depleted hematopoietic stem cell transplantation. Transpl Infect Dis. 2008;10(3):162–7.
Morgan J, Wannemuehler KA, Marr KA, et al. Incidence of invasive aspergillosis following hematopoietic stem cell and solid organ transplantation: interim results of a prospective multicenter surveillance program. Med Mycol. 2005;43 Suppl 1:S49–58.
van Burik JA, Carter SL, Freifeld AG, et al. Higher risk of cytomegalovirus and Aspergillus infections in recipients of T cell-depleted unrelated bone marrow: analysis of infectious complications in patients treated with T cell depletion versus immunosuppressive therapy to prevent graft-versus-host disease. Biol Blood Marrow Transplant. 2007;13(12):1487–98.
Labbe AC, Su SH, Laverdiere M, et al. High incidence of invasive aspergillosis associated with intestinal graft-versus-host disease following nonmyeloablative transplantation. Biol Blood Marrow Transplant. 2007;13(10):1192–200.
Junghanss C, Marr KA, Carter RA, et al. Incidence and outcome of bacterial and fungal infections following nonmyeloablative compared with myeloablative allogeneic hematopoietic stem cell transplantation: a matched control study. Biol Blood Marrow Transplant. 2002;8(9):512–20.
Fukuda T, Boeckh M, Carter RA, et al. Risks and outcomes of invasive fungal infections in recipients of allogeneic hematopoietic stem cell transplants after nonmyeloablative conditioning. Blood. 2003;102(3):827–33.
Martino R, Caballero MD, Canals C, et al. Reduced-intensity conditioning reduces the risk of severe infections after allogeneic peripheral blood stem cell transplantation. Bone Marrow Transplant. 2001;28(4):341–7.
Imhof A, Balajee SA, Fredricks DN, Englund JA, Marr KA. Breakthrough fungal infections in stem cell transplant recipients receiving voriconazole. Clin Infect Dis. 2004;39(5):743–6.
Trifilio SM, Bennett CL, Yarnold PR, et al. Breakthrough zygomycosis after voriconazole administration among patients with hematologic malignancies who receive hematopoietic stem-cell transplants or intensive chemotherapy. Bone Marrow Transplant. 2007;39(7):425–9.
Pavie J, Lacroix C, Hermoso DG, et al. Breakthrough disseminated Aspergillus ustus infection in allogeneic hematopoietic stem cell transplant recipients receiving voriconazole or caspofungin prophylaxis. J Clin Microbiol. 2005;43(9):4902–4.
Panackal AA, Imhof A, Hanley EW, Marr KA. Aspergillus ustus infections among transplant recipients. Emerg Infect Dis. 2006;12(3):403–8.
Alastruey-Izquierdo A, Cuesta I, Houbraken J, Cuenca-Estrella M, Monzon A, Rodriguez-Tudela JL. In vitro activity of nine antifungal agents against clinical isolates of Aspergillus calidoustus. Med Mycol. 2010;48:97–102.
Balajee SA, Gribskov JL, Hanley E, Nickle D, Marr KA. Aspergillus lentulus sp. nov., a new sibling species of A. fumigatus. Eukaryot Cell. 2005;4(3):625–32.
Balajee SA, Nickle D, Varga J, Marr KA. Molecular studies reveal frequent misidentification of Aspergillus fumigatus by morphotyping. Eukaryot Cell. 2006;5(10):1705–12.
Chim CS, Ho PL, Yuen KY. Simultaneous Aspergillus fischeri and Herpes simplex pneumonia in a patient with multiple myeloma. Scand J Infect Dis. 1998;30(2):190–1.
Jarv H, Lehtmaa J, Summerbell RC, Hoekstra ES, Samson RA, Naaber P. Isolation of Neosartorya pseudofischeri from blood: first hint of pulmonary aspergillosis. J Clin Microbiol. 2004;42(2):925–8.
Vinh DC, Shea YR, Sugui JA, et al. Invasive aspergillosis due to Neosartorya udagawae. Clin Infect Dis. 2009;49(1):102–11.
Lass-Florl C, Kofler G, Kropshofer G, et al. In-vitro testing of susceptibility to amphotericin B is a reliable predictor of clinical outcome in invasive aspergillosis. J Antimicrob Chemother. 1998;42(4):497–502.
Steinbach WJ, Stevens DA, Denning DW. Combination and sequential antifungal therapy for invasive aspergillosis: review of published in vitro and in vivo interactions and 6281 clinical cases from 1966 to 2001. Clin Infect Dis. 2003;37 Suppl 3:S188–224.
Rex JH, Pfaller MA, Walsh TJ, et al. Antifungal susceptibility testing: practical aspects and current challenges. Clin Microbiol Rev. 2001;14(4):643–58.
Hansen JA, Gooley TA, Martin PJ, Appelbaum F, Chancey TR, Clift RA, et al. Bone marrow transplants from unrelated donors for patients with chronic myeloid leukemia. N Engl J Med. 1998;338:962–8.
van Burik JH, Leisenring W, Myerson D, et al. The effect of prophylactic fluconazole on the clinical spectrum of fungal diseases in bone marrow transplant recipients with special attention to hepatic candidiasis. An autopsy study of 355 patients. Medicine (Baltimore). 1998;77(4):246–54.
Marr KA, White TC, van Burik JA, Bowden RA. Development of fluconazole resistance in Candida albicans causing disseminated infection in a patient undergoing marrow transplantation. Clin Infect Dis. 1997;25(4):908–10.
Bodey GP, Mardani M, Hanna HA, et al. The epidemiology of Candida glabrata and Candida albicans fungemia in immunocompromised patients with cancer. Am J Med. 2002;112(5):380–5.
Williamson EC, Millar MR, Steward CG, et al. Infections in adults undergoing unrelated donor bone marrow transplantation. Br J Haematol. 1999;104(3):560–8.
Menichetti F, Del Favero A, Martino P, et al. Itraconazole oral solution as prophylaxis for fungal infections in neutropenic patients with hematologic malignancies: a randomized, placebo-controlled, double-blind, multicenter trial. GIMEMA infection program. Gruppo Italiano Malattie Ematologiche dell’ Adulto. Clin Infect Dis. 1999;28(2):250–5.
Harousseau JL, Dekker AW, Stamatoullas-Bastard A, et al. Itraconazole oral solution for primary prophylaxis of fungal infections in patients with hematological malignancy and profound neutropenia: a randomized, double-blind, double-placebo, multicenter trial comparing itraconazole and amphotericin B. Antimicrob Agents Chemother. 2000;44(7):1887–93.
Morgenstern GR, Prentice AG, Prentice HG, Ropner JE, Schey SA, Warnock DW. A randomized controlled trial of itraconazole versus fluconazole for the prevention of fungal infections in patients with haematological malignancies. U.K. multicentre antifungal prophylaxis study group. Br J Haematol. 1999;105(4):901–11.
Marr KA, Crippa F, Leisenring W, et al. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood. 2004;103(4):1527–33.
Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356(4):348–59.
Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356(4):335–47.
Wingard JR, Carter SL, Walsh TJ, et al. Randomized, double-blind trial of fluconazole vs. voriconazole for the prevention of invasive fungal infection (IFI) after allogeneic hemotopoietic cell transplantation. Blood 2010; doi: 10.1182/blood-2010–02-268151.
Rijnders BJ, Cornelissen JJ, Slobbe L, et al. Aerosolized liposomal amphotericin B for the prevention of invasive pulmonary aspergillosis during prolonged neutropenia: a randomized, placebo-controlled trial. Clin Infect Dis. 2008;46(9):1401–8.
Pizzo PA, Robichaud KJ, Gill FA, Witebsky FG. Empiric antibiotic and antifungal therapy for cancer patients with prolonged fever and granulocytopenia. Am J Med. 1982;72(1):101–11.
EORTC International Antimicrobial Therapy Cooperative Group. Empiric antifungal therapy in febrile granulocytopenic patients. Am J Med. 1989;86(6 Pt 1):668–72.
Marr KA. Empirical antifungal therapy-new options, new tradeoffs. N Engl J Med. 2002;346(4):278–80.
Walsh TJ, Hiemenz JW, Seibel NL, et al. Amphotericin B lipid complex for invasive fungal infections: analysis of safety and efficacy in 556 cases. Clin Infect Dis. 1998;26(6):1383–96.
Walsh TJ, Finberg RW, Arndt C, et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med. 1999;340(10):764–71.
Walsh TJ, Pappas P, Winston DJ, et al. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med. 2002;346(4):225–34.
Boeckh M. Current antiviral strategies for controlling cytomegalovirus in hematopoietic stem cell transplant recipients: prevention and therapy. Transpl Infect Dis. 1999;1(3):165–78.
Caillot D, Casasnovas O, Bernard A, et al. Improved management of invasive pulmonary aspergillosis in neutropenic patients using early thoracic computed tomographic scan and surgery. J Clin Oncol. 1997;15(1):139–47.
Walsh TJ, Chanock SJ. Diagnosis of invasive fungal infections: advances in nonculture systems. Curr Clin Top Infect Dis. 1998;18:101–53.
Hebart H, Loffler J, Reitze H, et al. Prospective screening by a panfungal polymerase chain reaction assay in patients at risk for fungal infections: implications for the management of febrile neutropenia. Br J Haematol. 2000;111(2):635–40.
Cordonnier C, Pautas C, Maury S, et al. Empirical versus preemptive antifungal therapy for high-risk, febrile, neutropenic patients: a randomized, controlled trial. Clin Infect Dis. 2009;48(8):1042–51.
Sherertz RJ, Belani A, Kramer BS, et al. Impact of air filtration on nosocomial Aspergillus infections. Unique risk of bone marrow transplant recipients. Am J Med. 1987;83(4):709–18.
Cornet M, Levy V, Fleury L, et al. Efficacy of prevention by high-efficiency particulate air filtration or laminar airflow against Aspergillus airborne contamination during hospital renovation. Infect Control Hosp Epidemiol. 1999;20(7):508–13.
Anaissie EJ, Costa SF. Nosocomial aspergillosis is waterborne. Clin Infect Dis. 2001;33(9):1546–8.
Anaissie EJ, Stratton SL, Dignani MC, et al. Pathogenic Aspergillus species recovered from a hospital water system: a 3-year prospective study. Clin Infect Dis. 2002;34(6):780–9.
Anaissie EJ, Kuchar RT, Rex JH, et al. Fusariosis associated with pathogenic Fusarium species colonization of a hospital water system: a new paradigm for the epidemiology of opportunistic mould infections. Clin Infect Dis. 2001;33(11):1871–8.
Warris A, Gaustad P, Meis JF, Voss A, Verweij PE, Abrahamsen TG. Recovery of filamentous fungi from water in a paediatric bone marrow transplantation unit. J Hosp Infect. 2001;47(2):143–8.
Warris A, Voss A, Abrahamsen TG, Verweij PE. Contamination of hospital water with Aspergillus fumigatus and other moulds. Clin Infect Dis. 2002;34(8):1159–60.
Lass-Florl C, Rath P, Niederwieser D, et al. Aspergillus terreus infections in haematological malignancies: molecular epidemiology suggests association with in-hospital plants. J Hosp Infect. 2000;46(1):31–5.
Wingard J. Growth factors and other immunomodulators. In: Bowden R, Ljungman P, Paya C, editors. Transplant Infections. Philadelphia: Lippincott-Raven; 1998. p. 367–78.
Hoffer FA, Gow K, Flynn PM, Davidoff A. Accuracy of percutaneous lung biopsy for invasive pulmonary aspergillosis. Pediatr Radiol. 2001;31(3):144–52.
Rex JH, Bennett JE, Sugar AM, et al. A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia. Candidemia Study Group and the National Institute. N Engl J Med. 1994;331(20):1325–30.
Viscoli C, Castagnola E, Machetti M. Antifungal treatment in patients with cancer. J Intern Med Suppl. 1997;740:89–94.
Marr KA, Lyons CN, Ha K, Rustad TR, White TC. Inducible azole resistance associated with a heterogeneous phenotype in Candida albicans. Antimicrob Agents Chemother. 2001;45(1):52–9.
Mora-Duarte J, Betts R, Rotstein C, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med. 2002;347(25):2020–9.
Kuse ER, Chetchotisakd P, da Cunha CA, et al. Micafungin versus liposomal amphotericin B for candidaemia and invasive candidosis: a phase III randomised double-blind trial. Lancet. 2007;369(9572):1519–27.
Pappas PG, Rotstein CM, Betts RF, et al. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin Infect Dis. 2007;45(7):883–93.
Reboli AC, Rotstein C, Pappas PG, et al. Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med. 2007;356(24):2472–82.
Pappas PG, Kauffman CA, Anies D, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35.
Kontoyiannis DP, Luna MA, Samuels BI, Bodey GP. Hepatosplenic candidiasis. A manifestation of chronic disseminated candidiasis. Infect Dis Clin North Am. 2000;14(3):721–39.
Groll AH, Walsh TJ. Caspofungin: pharmacology, safety and therapeutic potential in superficial and invasive fungal infections. Expert Opin Investig Drugs. 2001;10(8):1545–58.
Wingard JR, White MH, Anaissie E, et al. A randomized, double-blind comparative trial evaluating the safety of liposomal amphotericin B versus amphotericin B lipid complex in the empirical treatment of febrile neutropenia. L Amph/ABLC Collaborative Study Group. Clin Infect Dis. 2000;31(5):1155–63.
Herbrecht R, Letscher-Bru V, Bowden RA, et al. Treatment of 21 cases of invasive mucormycosis with amphotericin B colloidal dispersion. Eur J Clin Microbiol Infect Dis. 2001;20(7):460–6.
Bowden R, Chandrasekar P, White MH, et al. A double-blind, randomized, controlled trial of amphotericin B colloidal dispersion versus amphotericin B for treatment of invasive aspergillosis in immunocompromised patients. Clin Infect Dis. 2002;35(4):359–66.
Cornely OA, Maertens J, Bresnik M, et al. Liposomal amphotericin B as initial therapy for invasive mould infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial). Clin Infect Dis. 2007;44(10):1289–97.
Denning DW, Ribaud P, Milpied N, et al. Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis. 2002;34(5):563–71.
Patterson TF, Kirkpatrick WR, White M, et al. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. Aspergillus study group. Medicine (Baltimore). 2000;79(4):250–60.
Lin SJ, Schranz J, Teutsch SM. Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis. 2001;32(3):358–66.
Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347(6):408–15.
Arikan S, Lozano-Chiu M, Paetznick V, Rex J. In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother. 2002;46:245–7.
Perea S, Gonzalez G, Fothergill AW, Kirkpatrick WR, Rinaldi MG, Patterson TF. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of Aspergillus spp. Antimicrob Agents Chemother. 2002;46:3039–41.
Kirkpatrick WR, Perea S, Coco BJ, Patterson TF. Efficacy of caspofungin alone and in combination with voriconazole in a Guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother. 2002;46:2564–8.
Kontoyiannis DP, Hachem R, Lewis RE, et al. Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer. 2003;98:292–9.
Marr KA, Boeckh M, Carter RA, et al. Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis. 2004;39:797–802.
Trifilio S, Pennick G, Pi J, et al. Monitoring plasma voriconazole levels may be necessary to avoid subtherapeutic levels in hematopoietic stem cell transplant recipients. Cancer. 2007;109(8):1532–5.
Trifilio S, Singhal S, Williams S, et al. Breakthrough fungal infections after allogeneic hematopoietic stem cell transplantation in patients on prophylactic voriconazole. Bone Marrow Transplant. 2007;40(5):451–6.
Pascual A, Calandra T, Bolay S, Buclin T, Bille J, Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46(2):201–11.
Hubel K, Dale DC, Liles WC. Granulocyte transfusion therapy: update on potential clinical applications. Curr Opin Hematol. 2001;8(3):161–4.
Offner F, Cordonnier C, Ljungman P, et al. Impact of previous aspergillosis on the outcome of bone marrow transplantation. Clin Infect Dis. 1998;26(5):1098–103.
Nivoix Y, Velten M, Letscher-Bru V, et al. Factors associated with overall and attributable mortality in invasive aspergillosis. Clin Infect Dis. 2008;47(9):1176–84.
Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA. Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis. 2007;44(4):531–40.
Cordonnier C, Ribaud P, Herbrecht R, et al. Prognostic factors for death due to invasive aspergillosis after hematopoietic stem cell transplantation: a 1-year retrospective study of consecutive patients at French transplantation centers. Clin Infect Dis. 2006;42(7):955–63.
Nucci M, Anaissie EJ, Queiroz-Telles F, et al. Outcome predictors of 84 patients with hematologic malignancies and Fusarium infection. Cancer. 2003;98(2):315–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Neofytos, D., Marr, K.A. (2011). Fungal Infections in Stem Cell Transplant Recipients. In: Kauffman, C., Pappas, P., Sobel, J., Dismukes, W. (eds) Essentials of Clinical Mycology. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-6640-7_29
Download citation
DOI: https://doi.org/10.1007/978-1-4419-6640-7_29
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-6639-1
Online ISBN: 978-1-4419-6640-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)