Abstract
Controlled cell assembly technique is a new research area in complex organ development technologies. Gelatin-based hydrogels, such as gelatin, gelatin/alginate, gelatin/chitosan, gelatin/fibrinogen, gelatin/hyaluronan, and gelatin/alginate/fibrinogen, have played an important role in the rapid fabrication of tissue or organs with well-defined structures and functions. Cryoprotectants, such as dimethylsulfoxide (DMSO) and glycerol, can be easily incorporated into the system for long-term conservation of the cell containing constructs. Hepatocytes, chondrocytes, cardiac myocytes, and adipose-derived stromal cells (ADSCs) are used to show function of the assembled cells. ADSCs can be controlled to differentiate into different targeted cell types according to their positions within the orderly predesigned three-dimensional (3D) constructs. A multicellular model for the metabolic syndrome was established along with the development of the double-syringe deposition system which lead to a hybrid cell/hydrogels construct with a vascular-like network fabricated using a digital model. The preliminary results indicate that the double-syringe assembly technique is a powerful tool for fabricating complex constructs with special intrinsic/extrinsic structures, and has the potential to be widely used in regenerative medicine and drug screening.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Although organ failure patients can be treated effectively by transplantations, these procedures are limited by donor organ availability, high costs, and the lifelong use of immunosuppressants [1]. The recent development of controlled cell assembly is a milestone in complex organ manufacturing techniques. This process requires a highly accurate three-dimensional (3D) micropositioning system with a pressure-controlled syringe to deposit cell/hydrogels structures with a lateral resolution of 10 μm (Fig. 1). Combined with the multinozzle organ manufacturing techniques novel therapeutic procedures are possible for failed organs. With the multinozzle cell assembling techniques, it is possible we were able to directly deposit different cells and hydrogels and/or other important chemical components into specific sites to form 3D living organ analogies in vitro or in vivo to mimic the respective organs at the right time, in the right position, in the right amount, and in different bioenvironments [2–10].
Hydrogels are natural or synthetic polymeric materials that typically have a dry mass between 1 and 20% that swells in water while maintaining a distinct 3D network structure by virtue of specific crosslinks [11]. Currently, several natural hydrogels, such as gelatin, chitosan, hyaluronan, alginate, fibrinogen, are being used for organ regeneration since they facilitate cell attachment and differentiation [12, 13].
Gelatin is a denatured, biodegradable polypeptide derived from the controlled partial hydrolysis of collagen, which is widely found in nature and is the major constituent of skin, bones, and connective tissue. After being chemically or physically crosslinked [14], gelatin can be used for medical purposes, including wound dressings, plasma volume expanders, and drug delivery systems [15]. Chitosan, a positively charged amino polysaccharide (poly-1, 4 d-glucoamine), derived from chitin by deacetylation, is known for its numerous and unique biological properties during wound healing. When mixed with positively charged chitosan, negatively charged gelatin ionically interacts with chitosan to form a polyionic complex. Hyaluronic acid (HA) is another major constituent of the extracellular matrix (ECM) in the human body. It can bind other large glycosaminoglycans (GAGs) and proteoglycans through specific HA–protein interactions [16]. Alginate is a collective term for a family of polysaccharides obtained from brown algae and is widely used for many medical applications [17]. Fibrin is a haemostatic wound dressing material that can be made in the form of a sponge, film, powder, and sheet [18, 19]. All of these natural polymers have been used to produce biocompatible and biodegradable hydrogels that acts as temporary replacements for medical regeneration [20, 21].
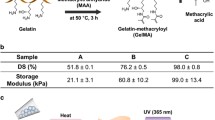
The combination of gelatin and other natural polymers made it possible to fabricate 3D constructs with rapid prototyping techniques. In the controlled cell assembly process, a series of gelatin-based hydrogels, such as gelatin, gelatin/chitosan, gelatin/hyaluronan, gelatin/alginate, gelatin/fibrinogen, and gelatin/alginate/fibrinogen, is used to obtain the necessary space and stabilizing factors for seeding various cells (Figs. 2–6) [2–10]. The cells were deposited in a sol–gel that is deposited onto a substrate surface layer by layer in a chamber at ∼10°C and the sol then is transformation into a hydrogels. The use of the natural gelatin-based hydrogels is clearly a distinct advantage for direct cell assembly technique in fabricating tissue analogs [2–10]. Besides providing cells with nutrients, the hydrogels also play an important role in supporting the whole structure. The special thermoresponsive property of gelatin allows extruded mixtures to be shaped at environmental temperatures below 20°C. However, the gels states of the gelatin-based hydrogels cannot be maintained when the structures are transferred to a 37°C environment. Consequently, after the cell-laden hydrogels are deposited the constructs have to be crosslinked or polymerized to yield a defined shape and stable 3D structure. To stabilize the structure, different crosslinkers are used. For example, glutaraldehyde solution is used to crosslink the gelatin molecules, and CaCl2 solution is used to stabilize the hydrogels structures containing alginate molecules. Due to the special properties, fibrinogen, a soluble plasma glycoprotein, is polymerized to fibrin. During this process, the polymer chains are covalently tethered to form a fibrous network that immobilizes the cells in the hydrogels system.
Some cell/hydrogels constructs with open channels made by the cell assembling machine: (a) one 3D hepatocyte/gelatin construct. Scale bar indicates 700 µm; (b) a 3D hepatocyte/gelatin/fibrinogen construct; (c) a 3D hepatocyte/gelatin/chitosan construct; (d) a 3D hepatocyte/gelatin/alginate construct.
By stabilizing the cell/hydrogels construct, a biomimetic 3D cell survival microenvironment is created. This construct can be used to address biological, mechanical, and architectural needs to promote functional tissue. The gelatin-based hydrogels networks provide a stable support for 3D constructs during the fabrication stage. During the post culture period, the gelatin-based hydrogels serves as an extracellular matrix to mimic the microenvironment in native tissue. Adipose-derived stem cells (ADSCs) can be controlled to differentiate into different targeted cell types according to their positions within the orderly predesigned 3D structure (Fig. 7). In a double-syringe deposition manufacturing system, a cell/hydrogels mixture can be placed into different regions or compartments (Figs. 8 and 9) [22, 23]. The gelatin-based hydrogels constructs provide the communication and organization support for cell assembly and set the basis for the formation of a 3D tissue or organ in vitro.
ADSCs in the gelatin/alginate/fibrinogen construct. (a) ADSCs grew and proliferated into aggregates in the hydrogels; (b) ADSCs were induced into endothelial like cells on the walls of the channel; (c) immunostaining of the 3D structure using mAbs for CD31+ cells in green and PI staining the nuclear in red.
Gelatin-Based Hydrogels for the Controlled Hepatocyte Assembly
Hepatocytes are notoriously difficult to maintain their phenotype during in vitro culture. In one of our previous studies [24], we found that a small change in the cell survival matrix constitution significantly affects hepatocyte behavior within the structure. Hepatocytes can be arranged as rods, cords, or other shapes that exhibit special polarization on an ammonia-treated collagen/chitosan (1:1) membrane.
Consequently, the choice of hydrogels plays a major role in influencing cell shapes and gene expressions that relate to cell growth and the preservation of native phenotypes. It is very difficult to attain a compatible microbioenvironment to mimic an in vivo organ, whereby the cells support one another via cell–cell interactions, supplemented by small amounts of extracellular matrices (ECMs) secreted by the cells [25]. It is well known that the success of bioartificial organs ultimately depends on the stability of the cell phenotype and its regulation by microenvironment cues [26].
Typically, as shown in Fig. 1, the first generation of a cell/hydrogels deposition system, developed in the Center of Organ Manufacturing, at Tsinghua University, consisted of a syringe with a 20 μm stainless steel capillary needle as the tip. The outer diameter of tip is 0.5 mm with an inner diameter of 0.3 mm. The tip has a flat end and is gently tapered with emery paper. The fluid of cell/matrix in the tip syringe is maintained at 0.25 mm per pulse, at 5 psi and 20 mL for volume, thus creating a driving force to deliver cell/matrix from the syringe to a poly(vinyl chloride) board. Hepatocytes embedded in the gelatin-based hydrogels are coextruded through a syringe with a needle tip onto a glass surface. These constructs are built layer by layer, by delivering the cellular containing matrices onto a stationary stage by applying pressure to a XYZ motor drive syringe. The 3D outcome of this process is a 100% interconnected porous construct, with defined architecture and can be built with a customized pattern. After deposition, more than 98% of the embedded hepatic cells remain viable.
The gelatin-based natural hydrogels, such as gelatin, gelatin/chitosan, gelatin/alginate, gelatin/hyaluronan, gelatin/fibrinogen, and gelatin/alginate/fibrinogen, are used in cell assembly as cell-loading support matrices and make the deposition processes easier. When hepatocytes are mixed with the hydrogels and deposited into special grid structures, with go-through pore-like channels under the computer control, hepatocytes are embedded in the hydrogels (Figs. 2–6) [2–10]. The hydrogels provide a highly hydrated microenvironment that allows nutrient diffusion, which supplies the necessary biochemical, cellular, and physical stimuli influencing cellular processes, such as migration, proliferation, and differentiation [27]. Otherwise, the hepatocytes die when they are 20–30 μm away from a blood supply [28].
The gelatin composite was chosen as the basic cell assembly matrix based on its special sol–gel transformation properties. The other polymers, such as chitosan, alginate, hyaluronan, and fibrinogen, are added with the expectation that they would influence different cell types to deposit into predesigned locations and to reorganize into functional 3D aggregates for in vitro culture or in vivo implantation. It is found that different polymer additives incorporated in the gelatin hydrogels resulted in different behavior by the hepatocyte [2–10]. For example, hepatocytes in the gelatin/chitosan hydrogels aggregate to form vortex like structures [3]. Due to the instability of the gelatin-based hydrogels at room temperature and normal cell culture at 37°C, chemical crosslinkers, such as glutaraldehyde, sodium tripolyphosphate (TPP), CaCl2, or thrombin, are employed to stabilize the constructs.
In general, glutaraldehyde is a toxic but an effective crosslinking agent. It is commonly used to harden gelatin by crosslinking the amino groups of proteins [29]. At certain concentrations, the crosslinking time of glutaraldehyde is directly related to structure stability. An increase in crosslinking time from 1 s to 5 min increases the stability of the 3D structures significantly. Longer crosslinking time produces rigid structures in which hepatocytes die, while less crosslinking time results in less stable structures. Hepatocytes on the outside of the extruded cell/hydrogels filaments also often die during the crosslinking process [2, 3]. Subsequently, a glutaraldehyde concentration of 2.5% and a crosslinking time of 5 s were selected [2, 3]. Under these conditions, a hydrogels that is soft and yet can be handled without losing its integrity was developed. The hydrogels state remained stable for more than 2 months. After the outside of the hydrogels was crosslinked, the hepatocytes were embedded in the gelatin macromolecules ensuring a relatively homogeneous distribution of cells in the grid. During the in vitro culture period, some of the interconnected gelatin molecules distributed in the inner parts of the structure, and the uncrosslinked material gradually dissolved at 37°C. Unlike the traditional 2D cell culture systems, the hepatocyte activity in the 3D structures is controlled by the crosslinked hydrogels networks, the soluble signals in the culture medium, as well as by cell–cell interactions. These 3D structures provide the hepatocytes with a microenvironment that more closely mimic those in the liver.
The 3D construct containing hepatocytes in a gelatin/chitosan hydrogels is formed by crosslinking with 3% TPP solution for 5 min, and then with 0.25% glutaraldehyde solution for 5 sec, respectively. If the construct is only crosslinked with TPP, a progressive loss of structure occurs after 2 weeks in culture. Apparently, the TPP in the crosslinked chitosan molecules is depleted with time and the gelatin/chitosan hydrogen is degraded by enzymes. When the concentration of TPP in the culture medium is far less than that in the crosslinked chitosan molecules, some of the TPP dissolves in the medium leading to the disassembled forms. Theoretically, the gelatin in the hydrogels should biodegrade much faster than chitosan, since hepatocytes produce enzymes that can biodegrade collagen as well as gelatin. Thus the hepatocytes are able to enzymatically digest the gelatin/chitosan hydrogels formed with TPP. Therefore, to further stabilize the structures, the cell-loaded architectures need to be treated with glutaraldehyde to provide a longer lasting hepatocyte survival environment during the in vitro culture period (Fig. 3). These structures remain intact until the cell aggregates are large enough to break the grid walls.
Similar results were obtained with the hepatocyte containing gelatin/alginate constructs [2]. After the calcium alginate hydrogels is formed, the gelatin molecules are irreversibly embedded in the calcium alginate molecules and the hepatocytes are then immobilized in the mixture. After setting, the hydrogels state remains for more than 2 weeks before the constructs appear to break down. The hydrogels structures decompose due to the loss of calcium ions in the crosslinked alginate molecules and the degradation of the gelatin/alginate hydrogen by enzymes.
In another approach, biodegradable fibrin was introduced into the gelatin-based cell system to stabilize the 3D cellular structures. Fibrin is a good haemostatic and wound dressing material that can be made in the form of sponges, films, powders, and sheets [19, 30]. During the fibrinogen gelation process, the protease thrombin cleaves the dimeric fibrinogen molecules at two symmetric sites. Once the fibrinogen is cleaved, a self assembly step takes place in which the fibrinogen monomers come together to form a noncovalently crosslinked polymer gels via the proteolytic exposure of binding sites [31]. A gelatin/fibrin hydrogels was chosen as the cell assembly matrix using a 1:1(v/v) ratio which exhibited the greatest elasticity modulus and compressive strength, and a thrombin solution (100 IU/mL) was used to polymerize the fibrinogen.
In contrast to glutaraldehyde crosslinked materials, this polymerization is reversible and can be disrupted by aprotinin, which gives the material its good processability. Furthermore, this kind of biomaterial has shown to be extremely biocompatible in vivo [32] and can be biodegraded in aqueous media by enzymolysis. To prevent polymerization of the fibrinogen within the delivery syringe, in situ preparation of the solution is recommended. After deposition, the constructs are gently bathed in cold thrombin solution and placed in a 4°C incubator for further stabilization.
There are several factors that contribute to the long survival and improved performance of hepatocytes. First, a stable 3D spatial microenvironment that mimics the liver is required. Unlike monolayer cell culture systems, the cells are enveloped by the gelatin-based hydrogels or by other cells. Second, a supply of nutrients and oxygen and expel metabolic wastes and carbon dioxide is required. Third, the hydrogels must protect the cells from harm, such as the glutaraldehyde crosslinker and culture polluted media, for example, cells die immediately when contacted directly with glutaraldehyde or after the 3D matrices break down. Fourth, the gelatin-based hydrogels can be biodegraded by the enzymes secreted by the living cells and provide space for cells to aggregate within the crosslinked membranes. Hence, the environment created must allow the cells to thrive in a 3D culture over a long time period. The crosslinked hydrogels structure provides a semi-permeable network that allows nutrient and waste infiltration, oxygen exchange, and cellular communication to occur.
In the human liver, hepatocytes are connected to each other laterally to form plate-like structures lined with three predominant types of nonparenchymal cells (NPCs) on the basal surfaces, creating sinusoids for blood flow. Organ manufacturing constructs that effectively duplicate natural organ functions must also maintain organ organization features, particularly the integration of multiple cell types that preserve distinct, integrated phenotypes. In particular, the need for angiogenesis or an established vasculature bed is evident by the success of the endothelial cells in the structures close to the culture medium.
Recently a double-syringe cell assembling technique was developed in the Center of Organ Manufacturing at Tsinghua University (Figs. 8 and 9) [22, 23]. This technique can layer two different cells simultaneously to create 3D constructs that can reproduce functions of a large population of two different cell types. The gelatin-based hydrogels are also used to provide structural stability, nutrients, and space for cell growth and aggregation. Both hepatocytes and endothelial cells were loaded in a stable structure. It is found that endothelial cells seeded on the bottom of pores are able to survive preferentially within the gelatin/chitosan channels. Regardless of the spheroids formed in the matrices, endothelial cells next to the hepatocytes undergo proliferation during the first several days (Fig. 9). The grid structures allow both the hepatocytes and endothelial cells access to nutrient and waste exchange as well as provide more surface area for endothelial cells to spread, coalesce, and elongate to form vessel-like structures throughout the channels. In addition, this technique offers many new opportunities for the design of the matrix components, the complex architectures, and for the study of the collaborations of cells, matrices as well as growth factors at different levels to meet special clinical demands.
Illustration of the digital models of the hybrid construct (the red tubelines denote the vascular network, while the yellow part was expected to form hepatic tissues): (a) a cutaway view of the full model with branched network and one-way inlet and outlet for dynamic perfusion culture; (b) the middle part of (a); (c) a CLI result of (a); (d) one CLI layer of (b).
Demonstration of an improved cell assembling controlling system and fabricating process with two syringes (the red part was made of ADSC/gelatin/alginate/fibrinogen in DMEM/F12, while the white part was made of hepatocyte/gelatin/alginate/chitosan in PBS): (a) no salivation with the improved method in the processing intervals; (b) salivation occurred with an old controlling method; (c–e) the layer-by-layer fabrication process.
It is expected that with the development of multisyringe systems, more different cells and extracellular matrices could delivered similtaneously to the connective positions or with relative accuracy into the 3D structures that mimic their respective position in organs. Thus creating a suitable environment for cell–gels and cell–cell interactions and bring about self-organization of cells or cell aggregates into metastable tissue structures with desired shapes. The multisyringe deposition system holds the promise to eventually make a human liver with whole spectrum of functions.
Establishing a Multicellular Model by 3D Cell Assembly for Metabolic Syndrome
Presently, one of the major obstacles to engineering thicker and complex tissues in vitro is the need to vascularize the tissue to maintain cell viability during tissue growth and structural organization. Currently, in vitro 3D tissue formation within a hydrogels, typically by embedding cells or cell spheroids, is limited by the slow spontaneous aggregation of cells with poorly controlled size and shape [33, 34]. The self-assembly by proliferating cells to form functional tissues below a certain density is restricted in most hydrogels because the polymer chains themselves are able to entrap cells and inhibit cell migration. Whether cells can organize within a 3D hydrogels depends on many of the characteristics of the hydrogels that influence the mass ratio of cells to hydrogels [35].
Engineered adipose tissue can be used in plastic surgery and reconstructive surgery to augment soft tissue lost due to mastectomy or lumpectomy [36, 37]. Adipose-tissue engineering with collagen scaffolds combined with human preadipocytes was recently reported [38, 39]. Patrick et al. formed adipose tissue in the rat subcutis using a porous poly(lactide-co-glycolide) scaffold preseeded with autologously isolated preadipocytes [40, 41]. ADSCs are multipotent cells found in adipose tissue and are receiving more and more attention [42].
Metabolic syndrome (MS) is a cluster of growing epidemic diseases including obesity, diabetes, hypertension, and atherosclerosis [43]. It is difficult to use the traditional techniques to develop multifunctional drugs for the metabolic syndrome (MS). Therefore, it is necessary to establish an in vitro model that addresses the more complex features of the disease.
Cell-assembly technology is a remarkable new invention developed specifically to establish multicellular models for metabolic syndrome. A software package was used to fabricate a complex structure model with orderly channels. A gelatin/alginate/fibrinogen hydrogels was used for assembling the ADSCs as a stream of drops in 3D positions that mimic the respective positions a living organ. In the 3D construct, the ADSCs control differentiation into different targeted cell types according to their positions within the orderly predesigned 3D structure. After differentiation, the ADSCs, pancreatic islets were deposited at designated locations and constituted adipoinsular axes with adipocytes. Oil red O staining confirmed that the ADSCs in the structure differentiated into adipocytes with a spherical shape while immuno-staining tests confirmed that endothelial growth factor (EGF) induced ADSCs on the walls of the channels that differentiated into mature endothelial cells and formed tubular structures throughout the engineered 3D structures. Endothelin-1 and nitric oxide release rules by the endothelial cells were coincident with that in vivo. In contrast, after preculturing with EGF, the ADSCs under the channel walls were more sensitive to differentiation into adipocytes than the cells on the walls. The reasons could be: (1) the EGF concentration under the walls of the channels was lower than that on the surface of the channels due to a diffusion gradient; (2) the mechanical properties of the surface of the channels induced the ADSCs to differentiate into endothelial cells more easily; (3) once differentiated into mature endothelial cells, the ADSCs lost all other differentiation potentials. This approach has the prospect of establishing an in vitro energy metabolic system with orderly endothelial vessel networks as well as in vascularized adipose-tissue engineering (Figs. 10 and 11) [8, 9].
Endothelin-1 and NO secretion of the endothelial cells in the 3D structures. At the 13th day, the structure was cultured with DMEM containing 25 mM glucose, (a) ET-1 secretion kinetics of the endothelial cells were measured for 24 h, ET-1 concentrations in the culture media were measured by ELISA kit. Data are mean ±SD, n = 3. (b) The media were harvested at the 15th day. NO concentrations in the culture media were detected using NO Detection kit. Data are mean ±SD, n = 6. *p < 0.01, vs. 1 μg insulin-treated group; **p < 0.01, vs. 5 μg insulin-treated group.
Cryopreservation of 3D Constructs Based on Controlled Cell Assembly
The development of tissue engineering and organ manufacturing requires effective cryopreservation technology for the cells in the 3D constructs. Cryopreservation technology plays an important role in conserving 3D constructs containing cells. Besides preserving the characteristics of the construct, it can also save resources, such as cell culture space, culture vessels, and culture medium.
The cryopreservation of 3D constructs that contain cells is different from the direct cryopreservation of single-cell suspension as there are complex connections between cells and materials in the 3D construct. Kang and coworkers analyzed the different responses between the fibroblasts exposed to low temperatures in monolayer cultures and 3D cultures [44]. They found that after recovering from the low temperatures, the cells in the 3D collagen scaffold secreted more fiber proteins and growth factors. The functional expression of the stress protein in the 3D structure was denser than those in monolayer and suspension cultures. These results indicate that the cryopreservation may bring extra benefits for the cells in 3D constructs. After the cryopreservation process, the 3D construct adapted to the pathological environment and promoted better wound healing and tissue repair [44].
With the advantages of the 3D controlled cell assembly technique, a new cryopreservation method for the 3D construct was developed. Various cryoprotectants, such as dimethylsulfoxide (DMSO), glycerol, and dextran-40, can be directly incorporated into the cell/hydrogels system and undergo a freezing/thawing process after assembly. The cells contained in the 3D construct can be preserved below −80°C for more than 1 week. After the construct undergoes a thawing process, cell viability and proliferation ability were regained. DMSO plays an important role in the cell survive processes. A cell viability of 78.7 ± 3.94% in the gelatin/alginate/fibrin hydrogels with 10% DMSO was obtained, which is much greater than that without the DMSO. This technique can potentially be used in other complex organ manufacturing areas (Figs. 12 and 13) [45].
Trypan Blue staining before and after cryopreservation: (a) ADSCs in gelatin/alginate/fibrinogen suspension without DMSO; (b) ADSCs in gelatin/alginate/fibrinogen suspension with 10% DMSO; (c) ADSCs in gelatin/alginate/fibrinogen hydrogels without DMSO before assembling; (d) ADSCs in gelatin/alginate/fibrinogen hydrogels with 10% DMSO before assembling; (e) ADSCs in gelatin/alginate/fibrinogen hydrogels without DMSO after assembling; (f) ADSCs in gelatin/alginate/fibrinogen hydrogels with 10% DMSO after assembling; (g) ADSCs in gelatin/alginate/fibrin hydrogels without DMSO after thawing; (h) ADSCs in gelatin/alginate/fibrin hydrogels with 10% DMSO after thawing.
Natural hydrogels, like gelatin, fibrin, and alginate, are commonly applied as cell-entrapping materials because of their outstanding biocompatibility and mild gelling conditions [46]. Fibrin gels is made by mixing two blood coagulation components, fibrinogen and thrombin [47]. These hydrogels also have protective effects on the cells during the freezing/thawing processes. The incorporation of the cryoprotectant, DMSO, in the gelatin/alginate/fibrinogen hydrogels has greatly improved the cell survival abilities during the assembly and freezing/thawing processes.
Summary
During the controlled cell assembly processes, cells are mixed with the gelatin-based hydrogels and placed into predesigned structures. The embedded cells remain viable and perform biological functions as long as the 3D structures are retained. The gelatin-based hydrogels protect the cells from harmful attacks, such as the glutaraldehyde crosslinker, keep the structural stable, and provide mass exchange networks. During the in vitro culture period, the hydrogels can be eventually digested by enzymes secreted by living cells or existing in the culture medium and provide more space for the cells to aggregate and communicate. With the double-syringe deposition system, two different cell types can be fabricated into a single construct. ADSCs in the 3D construct can be controlled to differentiate into specific cell types. The gelatin-based hydrogels used with cell assembly technology have the potential for high-throughput production of artificial human tissues and organs and high-throughput drug screening systems.
References
Keeffe EB (2001) Liver transplantation: current status and novel approaches to liver replacement. Gastroenterology 120(3):749–762
Yan YN, Wang XH, Xiong Z, Liu HX, Liu F, Lin F, Wu RD, Zhang RJ, Lu QP (2005) Direct construction of a three-dimensional structure with cells and hydrogel. J Bioact Compat Polym 20(3):259–269
Yan YN, Wang XH, Pan YQ, Liu HX, Cheng J, Xiong Z, Lin F, Wu RD, Zhang J, Lu QP (2005) Fabrication of viable tissue-engineered constructs with 3D cell-assembly technique. Biomaterials 26:5864–5871
Wang XH, Yan YN, Pan YQ, Xiong Z, Liu HX, Cheng J, Liu F, Lin F, Wu RD, Zhang RJ, Lu QP (2006) Generation of three-dimensional hepatocyte/gelatin structures with rapid prototyping system. Tissue Eng 12:83–90
Xu W, Wang XH, Yan YN, Zheng W, Xiong Z, Lin F, Wu RD, Zhang RJ (2007) Rapid prototyping three-dimensional cell/gelatin/fibrinogen constructs for medical regeneration. J Bioact Compat Polym 22(4):363–377
Yao R, Zhang RJ, Wang XH (2009) Design and evaluation of a cell microencapsulating device for cell assembly technology. J Bioact Compat Polym 24(S1):48–62
Yao R, Zhang RJ, Yan YN, Wang XH (2009) In vitro angiogenesis of three-dimensional tissue engineered adipose tissues. J Bioact Compat Polym 24:5–24
Xu ME, Yan YN, Liu HX, Yao R, Wang XH (2009) Control adipose-derived stromal cells differentiation into adipose and endothelial cells in a 3-D structure established by cell-assembly technique. J Bioact Compat Polym 24(S1):31–47
Xu ME, Yan YN, Liu HX, Yao R, Wang XH (2008)Establishing a multicellular model by three-dimensional cell-assembly technique for metabolic syndrome, Nature Precedings, Posted 8 Jan 2008
Wang XH, Yan YN, Zhang RJ (2007) Rapid prototyping as a tool for manufacturing bioartificial livers. Trends Biotechnol 25:505–513
Hoffman AS (2002) Hydrogels for biomedical applications. Adv Drug Deliv Rev 54:3
Heimbach D, Luterman A, Burke J, Cram A, Hunt J, Jordan M, McManus M, Solem L, Warden G, Zawacki B (1998) Artificial dermis for major burn: a multi-center clinical trial. Ann Surg 208:313–320
Chen WY, Abatangelo G (1999) Functions of hyaluronan in wound repair. Wound Repair Regen 7:79–89
Veis A (1964) The macromolecular chemistry of gelatin. Academic, New York
Schacht EH, Nobels M, Vansteenkiste S, Demeester J, Fransen J, Lemahieu A (1993) Cross-linkage of gelatin by dextran dialdehyde. Polym Gels Netw 1:213–224
Landers R, Hübner U, Schmelzeisen R, Mülhaupt R (2002) Rapid prototyping of scaffolds derived from thermoreversible hydrogels and tailored for application in tissue engineering. Biomaterials 23:4437–4447
Govan JR, Fyfe JA, Jarman TR (1981) Isolation of alginate-producing mutants of Pseudomonas fluorescens, Pseudomonas putida and Pseudomonas mendocina. J Gen Microbiol 125(1):217–220
Bergel S (1909) On the functions of fibrins. Dtsch Med Wochenschr 35:633
Ferry JD, Morrison PR (1946) Fibrin film and other products from human plasma. Ind Eng Chem 38:1217–1221
Sastry TP, Rose C, Gomathinayagam S, Ganga R (1998) Chemically modified fibrin-gelatin composites: preparation and characterization. J Appl Polym Sci 68:1109–1115
John P, Courts A (1977) The science and technology of gelatin. In: Ward AG, Courts A (eds) Academic Press, New York, p 138
Li SJ, Xiong Z, Wang XH, Yan YN, Liu HX, Zhang RJ (2009) Direct fabrication of a hybrid cell/hydrogel construct via a double-nozzle assembling technology. J Bioact Compat Polym 24:249–264
Li SJ, Yan YN, Xiong Z, Weng CY, Zhang RJ, Wang XH (2009) Gradient hydrogel construct based on an improved cell assembling system. J Bioact Compat Polym 24(S1):84–99
Wang X, Yan Y, Xiong Z, Lin F, Wu R, Zhang R, Lu Q (2005) Preparation and evaluation of ammonia treated collagen/chitosan matrices for liver tissue engineering. J Biomed Mater Res- Part B, Appl Biomater 75(1):91–98
Ong SM, Zhang C, Toh YC, Kim SH, Foo HL, Tan CH, van Noort D, Park S, Yu H (2008) A gel-free 3D microfluidic cell culture system. Biomaterials 29:3237–3244
Colette S, Ranucci AK, Surendra PB, Prabhas VM (2000) Control of hepatocyte function on collagen foams: sizing matrix pores toward selective induction of 2-D and 3-D cellular morphogenesis. Biomaterials 21:783–793
Fedorovich NE, Alblas J, de Vijn JR, Hennisnk WE, Verbout AJ, Dhert WJA (2007) Hydrogels as extracellular matrices for skeletal tissue engineering: state-of-the-art and novel application in organ printing. Tissue Eng 13:1905–1925
Kim SS, Sundback CA, Kaihara S, Benvenuto MS, Kim B, Mooney DJ, Vacanti JP (2000) Dynamic seeding and in vitro culture of hepatocytes in a flow perfusion system. Tissue Eng 6(1):39–44
Richards FM, Knowles JR (1968) Glutaraldehyde as a protein crosslinking agent. J Mol Biol 37:231–233
Bergel S (1909) On the functions of fibrins. Dtsch Med Wochenschr 35:633, Citedin-Mihaly Gerendas. Fibrin products as aids in hemostatis and wound healing. In: Koloman Laki. Fibrinogen. New York: Marcel Dekker Inc.; 1968. pp 277–316
Schense JC, Hubbell JA (1999) Crosslinking exogenous bifunctional peptides into fibrin gels with factor XIIIa. Bioconjugate Chem 10(1):75–81
Bruns H, Kneser U, Holzhüter S, Roth B, Kluth J, Kaufmann PM, Kluth D, Fiegel HC (2005) Injectable liver: a novel approach using fibrin gel as a matrix for culture and intrahepatic transplantation of hepatocytes. Tissue Eng 11:1718–1726
Bryant SJ, Anseth KS (2002) Hydrogel properties influence ECM production by chondrocytes photoencapsulated in poly(ethylene glycol) hydrogels. J Biomed Mater Res 59:63–72
Kelm JM, Timmins NE, Brown CJ, Fussenegger M, Nielsen LK (2003) Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol Bioeng 83:173–180
Tan W, Desa TA (2003) Microfluidic patterning of cells in extracellular matrix biopolymers: effects of channel size, cell type, and matrix composition on pattern integrity. Tissue Eng 9:255–267
Cho SW, Song KW, Rhie JW, Park MH, Choi CY, Kim BS (2007) Engineered adipose tissue formation enhanced by basic fibroblast growth factor and a mechanically stable environment. Cell Transplant 16(4):421–434
Griffith LG, Naughton G (2002) Tissue engineering – current challenges and expanding opportunities. Science 295:1009–1014
Patrick CW Jr (2000) Adipose tissue engineering: the future of breast and soft tissue reconstruction following tumor resection. Semin Sur Oncol 19:302–311
Patrick CW Jr, Chauvin PB, Hobley J, Reece GP (1999) Preadipocytes seeded PLGA scaffolds for adipose tissue engineering. Tissue Eng 5:139–151
von Heimburg D, Zachariah S, Heschel I, Kühling H, Schoof H, Hafemann B, Pallua N (2001) Human preadipocytes seeded on freeze-dried collagen scaffolds investigated in vitro and in vivo. Biomaterials 22:429–438
von Heimburg D, Zachariah S, Low A, Pallua N (2001) Influence of different biodegradable carriers on the in vivo behavior of human adipose precursor cells. Plast Reconstr Surg 108:411–420
Zuk PA et al (2001) Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7:211–228
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887
Liu K, Yang YJ, Mansbridge J (2000) Comparison of the stress response to cryopreservation in monolayer and three-dimensional human fibroblast cultures: stress proteins, MAP kinases, and growth factor gene expression. Tissue Eng 6(5):539–554
Sui SC, Wang XH, Liu PY, Yan YN, Zhang RJ (2009) Cryopreservation of 3D constructs based on a controlled cell assembling technology. J Bioact Compat Polym 24(5):5–19
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng: Part B 14(1):61–86
Blomback B, Bark N (2004) Fibrinopeptides and fibrin gel structure. Biophys Chem 112:147–151
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Wang, X., Yan, Y., Zhang, R. (2010). Gelatin-Based Hydrogels for Controlled Cell Assembly. In: Ottenbrite, R., Park, K., Okano, T. (eds) Biomedical Applications of Hydrogels Handbook. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-5919-5_14
Download citation
DOI: https://doi.org/10.1007/978-1-4419-5919-5_14
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-5918-8
Online ISBN: 978-1-4419-5919-5
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)