Abstract
The present study aimed to characterize microcirculatory responses to anesthesia in brain tissue. With multi-photon excitation fluorescence microscopy, intra-cortical capillary dimension and red blood cell (RBC) flow were successfully visualized up to a depth of ∼0.6 mm from the cortical surface in rats anesthetized with either isoflurane or α-chloralose. We observed that the diameter of the major cerebral artery was ∼100 µm under isoflurane, but ∼75 µm under α-chloralose. The capillary diameter was observed to be larger under α-chloralose than isoflurane: 5.1 ± 1.2 µm vs. 4.8 ± 1.1 µm, respectively. A significant difference in the mean RBC speed measured in single capillaries was observed: 0.4 ± 0.4 mm/s under α-chloralose vs. 1.5 ± 0.4 mm/s under isoflurane. In agreement with these observations, arterio-venous transit-time and laser-Doppler flowmetry consistently showed a significant reduction of the RBC and plasma blood speed under α-chloralose relative to isoflurane. These findings may indicate that local blood flow regulatory mechanisms exist at the capillary level for the balance of oxygen supply and demand induced by anesthesia in the brain tissue.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
A variety of brain tissue oxygen levels have been observed in animals under general anesthesia [1]. The direct and indirect effects of anesthesia involve the degree of anesthetic action on cerebral metabolic rate of oxygen (CMRO2) and cerebral blood flow (CBF).
In a previous study, we found that rodents treated with inhalation anesthetics (e.g., isoflurane) or intravenous anesthetics (e.g., α-chloralose) that are widely used for brain activation studies, showed quite different behaviors for the activation-induced cortical hemodynamics [2]. Since hemodynamic-based brain imaging techniques rely on the microcirculatory responses to local neural activity, the effects of anesthesia on the brain microcirculation are critically important for interpretation of the imaging signals. However, the effects of anesthesia on the brain microcirculation, such as vessel dimension and red blood cell (RBC) flow remain unaddressed.
In the present study, we directly measured intracortical capillary dimension and RBC flow in the cerebral cortex of rats anesthetized with either volatile isoflurane or injectable α-chloralose. A biocompatible fluorescent dye was intravenously injected for visualization of blood plasma and cortical microvasculature was three-dimensionally visualized with in vivo multi-photon excitation fluorescent microscopy up to a depth of 0.6 mm from the cortical surface. Intraluminal vascular dimension and fluorescently labeled RBC speed were then measured.
2 Materials and Methods
All animal protocols were approved by the NIRS Animal Experiment Committee. The animals (250–350 g Sprague-Dawley rats, N = 9) were initially anesthetized with 4–5% isoflurane and maintained with 2% during surgical procedures. The animal was mechanically ventilated and physiologic parameters (e.g., end-tidal CO2, anesthetic gas concentration, respiratory rate, heart rate, and mean arterial blood pressure) were monitored throughout all experiments. Arterial blood gas was periodically measured, and respiratory rate and minute ventilation volume were adjusted as needed. Rectal temperature was maintained at 37.0 ± 0.2°C.
A portion of the left skull (3 mm by 3 mm) over the somatosensory area was removed. The opened area was filled with physiologic saline solution. For experiments, the anesthesia level was first maintained with isoflurane (∼1.4%) and then switched to α-chloralose (45 mg/kg/h, i.v.), as previously reported [2]. For visualization of the cortical vasculature, a bolus of Qdot® 605 (1 µM in buffered solution, Invitrogen) was intravenously injected (0.2–0.4 ml). The cortical vasculature was then visualized with multi-photon excitation fluorescent microscope (TCS SP5, Leica Microsystems) with an excitation wavelength of 900 nm (MaiTai, Ti:Sapphire laser, Spectra-Physics). The objective lens was a 20× water-immersion lens (0.5 NA, Leica Microsystems). The 512 pixel by 512 pixel images covered a cortical area of 456 µm by 456 µm with a pixel resolution of 0.89 µm. To obtain the three-dimensional structure, contiguous images were captured up to a depth of 0.6 mm from the cortical surface with a step size of 0.01 mm in the z-direction. The region of interest was selected with care to avoid areas having vessels of a relatively large size at the cortical surface. A final image was taken to cover an area of 912 µm by 912 µm in the x-y plane by scanning four adjacent regions. For display purposes, a maximum-intensity projection was constructed from contiguous images obtained in the z-direction.
Based on their pulsation and branching geometry, arterial and venous networks were distinguished at the cortical surface, and then tracked into the parenchyma tissue. To measure capillary diameter, a maximum intensity projection was created from every 0.1-mm thickness in the z-direction and then the width in the image was calculated. A single capillary was defined as the single vessel having cross-sectional thickness less than 8 µm and for which both edges continued to two new vessels as a branching.
The RBC speed was measured by tracking a FITC-labeled RBC through a single capillary. Time-lapse images were obtained at a rate of 14–167 frames per second, depending on the number of lines to be scanned in each single frame. The scanning area was set to cover the whole structure of the single-capillary shape (i.e., 64–256 lines). Similarly, the speed of blood plasma was evaluated by tracking 0.1-µm diameter fluorescent beads that were intravenously injected. For the measurement of mean arterio-venous transit time, a bolus injection (0.1 ml) of fluorescently labeled RBCs or fluorescent beads was performed via the femoral vein. The time-lapse image was obtained with a 5× objective lens at a rate of seven frames per second. Statistical significance was determined with a t-test (P < 0.05).
3 Results
There was no detectable difference in the measured physiologic parameters (arterial blood gas and blood pressure) between isoflurane and α-chloralose conditions (Table 1). We observed that the diameter of the principal artery at the cortical surface was ∼100 µm under isoflurane, but ∼75 µm under α-chloralose. The results showed that the principal artery shrank significantly after induction with α-chloralose. However, the intracortical capillary diameter was slightly larger under α-chloralose (5.1 ± 1.2 µm, n = 1682 vessels) compared to the isoflurane condition (4.8 ± 1.1 µm, n = 1746 vessels). A statistically significant difference was observed between two conditions. These results indicate that the upstream and downstream vessels react differently depending on the anesthetics.
The mean RBC speed in a single capillary was significantly lower under α-chloralose relative to the isoflurane condition: 0.4 ± 0.4 mm/s under α-chloralose vs. 1.5 ± 0.4 mm/s under isoflurane. Under α-chloralose, some RBCs were found to be very slow (<0.01 mm/s), whereas most RBCs measured under isoflurane had a relatively high speed (0.4–3.0 mm/s).
As expected, the arterio-venous transit-time of the labeled RBCs was significantly longer under α-chloralose (2.8 ± 1.7 s at peak-to-peak) as compared to the isoflurane condition (1.0 ± 0.9 s). Similar results were observed for the transit time of blood plasma: 1.8 ± 1.3 s under α-chloralose and 1.2 ± 0.7 s under isoflurane. These results indicated that the both RBC and plasma blood speed were significantly lower under α-chloralose relative to isoflurane conditions.
4 Discussion
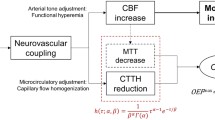
It has been previously shown by other groups that the baseline CBF under α-chloralose was 30–50% lower than under isoflurane in rat somatosensory cortex, i.e. 70–90 mL/100 g/min under α-chloralose [3, 4] vs. 130–150 mL/100 g/min under isoflurane [5, 6]. In a previous study, we found the baseline CBF measured with laser-Doppler flowmetry was 31% lower under α-chloralose compared with isoflurane [2]. Our measurements of the arterial dimension are in good agreement with these literature data, indicating that the tone in the upstream resistance vessels has a significant role in the regulatory mechanism of the baseline CBF induced by anesthesia. However, we also found that the effect of the anesthesia on the intracortical capillary diameter was opposite to the arterial response. Namely, a larger capillary diameter was observed under α-chloralose as compared to the isoflurane condition. This might indicate that the upstream arteries and intracortical microvessels have separate or independent mechanisms for the regulation of local CBF.
Our results for the mean RBC speed consistently showed that the speed was significantly lower under α-chloralose relative to the isoflurane condition. The results are consistent with previous CBF data. However, the measured RBC speed under isoflurane was relatively high. Kleinfeld et al. (1998) reported that the intra-cortical RBC speed was 0.77 mm/s in rats anesthetized with urethane [7]. The ranges of RBC speed in capillaries were reported as 0.3–3.2 mm/s [8]. In the present study, we showed that the variable speed of RBCs could be due to a local regulatory mechanism rather than upstream arterial regulation. Since the capillary volume and speed of RBCs critically affect oxygen transfer processes from nearby blood vessels to the energy consuming tissue site, it is worthwhile to compare the tissue oxygen level between both anesthesia conditions. Our group has reported that the mean tissue oxygen level in rat somatosensory cortex was 29 mmHg under α-chloralose and 33 mmHg under isoflurane [9, 10]. Another study with electron paramagnetic resonance oximetry showed that the mean tissue oxygen level at normoxic conditions was 13 mmHg under a cocktail of α-chloralose and urethane and 38 mmHg under isoflurane [11]. The data from those studies were in good agreement with the CBF data; higher CBF produces higher tissue oxygen and vice versa. The anesthesia may also affect the tissue oxygen metabolic rate in a different manner, and thus a possible scenario where the effect of anesthesia on the energy metabolism becomes a dominant factor leading to the observed difference in tissue oxygen level cannot be ruled out. However, it should be noted that endothelial cells have the ability to control their dimension by sensing the nearby blood oxygenation level [12], which may play a role in adjusting local oxygen demand and supply via regulation of capillary volume and RBC speed. Further studies are needed to elucidate the full regulatory mechanism for the local regulation of the microvascular dimensions and RBC traffic.
References
Ndubuizu, O., LaManna, J. C., 2007, Brain tissue oxygen concentration measurements, Antioxid Redox Signal. 9:1207–1219.
Masamoto, K., Kim, T., Fukuda, M., Wang, P., Kim, S. G., 2007, Relationship between neural, vascular, and BOLD signals in isoflurane-anesthetized rat somatosensory cortex, Cereb Cortex. 17:942–950.
Ueki, M., Linn, F., Hossmann, K. A., 1988, Functional activation of cerebral blood flow and metabolism before and after global ischemia of rat brain, J Cereb Blood Flow Metab. 8:486–494.
Lee, S. P., Duong, T. Q., Yang, G., Iadecola, C., Kim, S. G., 2001, Relative changes of cerebral arterial and venous blood volumes during increased cerebral blood flow: implications for BOLD fMRI, Magn Reson Med. 45:791–800.
Maekawa, T., Tommasino, C., Shapiro, H. M., Keifer-Goodman, J., Kohlenberger, R. W., 1986, Local cerebral blood flow and glucose utilization during isoflurane anesthesia in the rat, Anesthesiology. 65:144–151.
Lenz, C., Frietsch, T., Futterer, C., Rebel, A., van Ackern, K., Kuschinsky, W., Waschke, K. F., 1999, Local coupling of cerebral blood flow to cerebral glucose metabolism during inhalational anesthesia in rats: desflurane versus isoflurane, Anesthesiology. 91:1720–1723.
Kleinfeld, D., Mitra, P. P., Helmchen, F., Denk, W., 1998, Fluctuations and stimulus-induced changes in blood flow observed in individual capillaries in layers 2 through 4 of rat neocortex, Proc Natl Acad Sci U S A. 95:15741–15746.
Hudetz, A. G., 1997, Blood flow in the cerebral capillary network: a review emphasizing observations with intravital microscopy, Microcirculation. 4:233–252.
Masamoto, K., Kershaw, J., Ureshi, M., Takizawa, N., Kobayashi, H., Tanishita, K., Kanno, I., 2007, Apparent diffusion time of oxygen from blood to tissue in rat cerebral cortex: implication for tissue oxygen dynamics during brain functions, J Appl Physiol. 103:1352–1358.
Masamoto, K., Vazquez, A., Wang, P., Kim, S. G., 2008, Trial-by-trial relationship between neural activity, oxygen consumption, and blood flow responses, Neuroimage. 40:442–450.
Hou, H., Grinberg, O. Y., Taie, S., Leichtweis, S., Miyake, M., Grinberg, S., Xie, H., Csete, M., Swartz, H. M., 2003, Electron paramagnetic resonance assessment of brain tissue oxygen tension in anesthetized rats, Anesth Analg. 96:1467–1472.
Inoue, K., Tomita, M., Fukuuchi, Y., Tanahashi, N., Kobari, M., Takao, M., Takeda, H., Yokoyama, M., 2003, Dynamic observation of oxygenation-induced contraction of and transient fiber-network formation-disassembly in cultured human brain microvascular endothelial cells, J Cereb Blood Flow Metab. 23:821–828.
Acknowledgments
This work was partially supported by KAKENHI (#19800065).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this paper
Cite this paper
Masamoto, K., Obata, T., Kanno, I. (2010). Intracortical Microcirculatory Change Induced by Anesthesia in Rat Somatosensory Cortex. In: Takahashi, E., Bruley, D. (eds) Oxygen Transport to Tissue XXXI. Advances in Experimental Medicine and Biology, vol 662. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-1241-1_7
Download citation
DOI: https://doi.org/10.1007/978-1-4419-1241-1_7
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-1239-8
Online ISBN: 978-1-4419-1241-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)