Abstract
With a depleting ozone layer and increasing ultraviolet radiation exposure, the incidence of eyelid cancers is on the rise, and we can expect a growing need for eyelid reconstruction. Several reconstructive techniques may be appropriate for a particular eyelid defect. The choice of procedure by the surgeon depends on the patient’s age, the degree of eyelid laxity and quality of eyelid skin, the location and size of the defect, and the surgeon’s preference. Regardless of the surgical procedure chosen, the goals of the procedure should be restoration of both the anatomy and the dynamic function of the eyelid, creation of a stable eyelid margin, acceptable vertical eyelid height, adequate eyelid closure, smooth posterior epithelial surface, and maximum cosmesis and symmetry.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
With a depleting ozone layer and increasing ultraviolet radiation exposure, the incidence of eyelid cancers is on the rise, and we can expect a growing need for eyelid reconstruction. The following chapter details eyelid reconstruction following tumor resection.
2 General Principles
Regardless of the surgical procedure chosen, the goals of the procedure should be restoration of both the anatomy and the dynamic function of the eyelid, creation of a stable eyelid margin, acceptable vertical eyelid height, adequate eyelid closure, smooth posterior epithelial surface, and maximum cosmesis and symmetry. The reconstructive technique chosen for eyelid defects largely depends on the extent of full-thickness horizontal lid resection. The surgeon may be surprised at the final size of a lid defect following tumor excision if frozen-section histopathologic examination proves the tumor to be more extensive than clinically estimated. Therefore, the patient should be counseled about the potential extent of the eyelid defect based on the anatomic location and type of cancer.
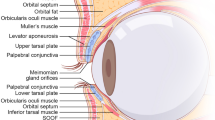
For the purposes of repair, the eyelids can be thought of as being made of an anterior and a posterior lamella. The anterior lamella consists of the skin and orbicularis muscle, while the posterior lamella is made up of the tarsus and conjunctiva. It is important to reconstruct both the anterior and posterior lamellae. Reconstruction of either the anterior or the posterior lamella may be accomplished with a graft, but grafts should not be used to reconstruct both lamellae since one of the layers must act as a pedicle flap and provide the blood supply. A graft placed upon another graft has a high probability of failure. Horizontal tension should be maximized at the expense of vertical tension to avoid postoperative eyelid malposition. In so doing, the surgeon must evaluate for horizontal lid laxity.
Medial and lateral canthal fixation should always be optimized, and an attempt should be made to match like tissue to like tissue in each lamella. Before any graft is sized, the anatomical defect should be narrowed as much as possible. The surgeon should avoid, whenever feasible, creating a defect that cannot be closed. When presented with alternatives, choosing the simplest technique is often wise. Finally, for complex and large defects encompassing more than the immediate periorbital soft tissues, it may be necessary to engage specialists from other disciplines, such as facial plastic surgery, to collaborate with the oculoplastic surgeon in surgical planning and reconstruction.
3 Eyelid Defects Not Involving the Eyelid Margin
Partial-thickness eyelid defects not involving the eyelid margin frequently result from Mohs surgery for skin cancers. Defects that do not involve the eyelid margin can be repaired by direct closure as long as the procedure does not distort the eyelid margin. Undermining of superficial tissues may sometimes be necessary to avoid undue wound tension. Tension of wound closure should be directed horizontally to avoid lower eyelid ectropion, eyelid retraction, and lagophthalmos. Avoiding vertical tension requires the placement of vertically oriented incision lines.
When undermining does not allow direct approximation, advancement or transposition procedures utilizing local skin flaps may be undertaken. The most commonly used flaps are advancement flaps, including sliding and rotation flaps, and transposition flaps, including z-plasty and rhomboid flaps [1]. The simplest skin-and-muscle flap is a sliding flap. It requires wide undermining to allow it to “slide” into the defect. The second simplest flap is the advancement flap, which requires wide undermining followed by relaxing incisions to allow the flap to “advance” into the defect. The resultant excess tissue adjacent to the flap can be trimmed by removing Burrow’s triangles of skin on either side of the flap [2]. Semicircular and rotation flaps are types of advancement flaps that are rotated into the defect. Z-plasty and rhomboid flaps are transposition flaps, entailing transfer of the flap from a nonadjacent area into the defect by lifting the flap over normal tissue [3]. Transposition flaps are often helpful in the repair of larger defects. These different flaps are often used in combination to work around facial contours. Flaps typically provide the best tissue match and cosmetic result but necessitate planning to limit secondary deformities. Although skin graft procedures are usually less challenging to perform, a skin graft may not be an appropriate choice for a deep defect or if postoperative adjuvant radiation therapy is planned.
Upper eyelid defects involving the anterior lamella are best repaired with full-thickness skin grafts from the contralateral upper lid. Preauricular or retroauricular grafts may also be utilized, but their greater thickness may hinder upper lid mobility and cosmesis. Lower eyelid defects not involving the margin and without significant soft tissue depth can be repaired using a skin graft from the upper eyelid or the preauricular or retroauricular skin. When tissue is not available from the upper lid or periauricular locations, full-thickness grafts may be harvested from the supraclavicular fossa or the inner upper arm. It should be remembered that skin grafts will shrink, somewhat, and produce some traction on the eyelid in the direction of the graft [2]. Surgeons must be vigilant not to place hair-bearing skin grafts near the eyelid margin as this may lead to future corneal irritation.
Split-thickness grafts should be avoided in periocular reconstructions as the cosmetic result is inferior to full-thickness grafts. They are only recommended in the surgical care of severe facial burns when adequate full-thickness skin is unavailable.
4 Small Defects Involving the Lower Eyelid Margin
Small defects that involve the lower eyelid margin can be repaired by direct closure assuming that the surrounding tissue is sufficiently lax so that undue tension is not placed on the wound. Primary closure is typically carried out when less than 33% of the lid margin is involved (Fig. 18.1). If a larger defect is present, adjacent tissue advancement or grafting of distant tissue may be needed. During primary closure, an additional 3–5 mm of medial mobilization may be obtained from the remaining lateral lid margin by severing the inferior limb of the lateral canthal tendon via a canthotomy and a cantholysis. During closure, the lid margin should be repaired with interrupted 6-0 silk sutures, which are left long and incorporated into subsequent skin sutures to ensure that they do not rub against the cornea. Three margin sutures should be placed—through the tarsus, the lash line, and the gray line. The tarsus should be repaired with 5-0 absorbable polyglactin suture.
Possible complications resulting from direct closure include a notch at the eyelid margin and wound dehiscence. A notch at the eyelid margin can be prevented by ensuring precise approximation of the tarsal margin and placing additional silk sutures at the eyelid margin [2]. Occasionally, wound dehiscence may occur. This tends to happen when there is excess tension on the wound or when the tissues are chronically inflamed. If the wound is too tight, thought should be given to performing a cantholysis to relieve the tension. Additionally, well-placed tarsal sutures at the lid margin and tarsal base help prevent dehiscence.
5 Moderate Defects Involving the Lower Eyelid Margin
Moderate defects are defined as those involving 33–50% of the margin. They are repaired by advancement of the lateral portion of the eyelid using semicircular advancement or rotation flaps. The most common repair technique utilizes a modified superior Tenzel semicircular rotation flap in conjunction with an inferior cantholysis. The flap should not extend as far as the brow superiorly, nor should it extend beyond the lateral orbital rim laterally [2]. Complications resulting from the use of the semicircular flap are usually caused by poor placement of the flap at the lateral canthus. The deep tissue of the flap must be securely fixed to the periorbita on the inner aspect of the lateral orbital rim [2], since ectropion is likely to result from poor fixation. Also, the semicircular rotation flap may result in a rounded lateral canthus, making secondary revisions necessary.
Tarsoconjunctival flaps are very useful for larger lower eyelid defects. These flaps are taken from the undersurface of the upper eyelid and may be transplanted into the lower lid defect to reconstruct the posterior lamella. Please see the next section for more details.
6 Large Defects Involving the Lower Eyelid Margin
Lower eyelid defects that involve greater than 50% of the lid margin—require adjacent tissue advancement for repair (Fig. 18.2a). One such approach involves the use of a modified tarsoconjunctival flap (Hughes flap) taken from the undersurface of the upper eyelid. The flap is advanced from the upper lid into the posterior lamellar defect of the lower lid (Fig. 18.2b) [4]. Care should be taken when tarsal grafts are harvested to preserve the marginal 3–4 mm tarsal height in the upper eyelid to prevent donor-lid margin distortion. The tarsoconjunctival flap can be covered with various types of skin flaps or a full-thickness skin graft; the latter is our preferred choice for anterior lamella reconstruction over the tarsoconjunctival flap [5, 6]. The skin graft can be harvested from the upper eyelid using a blepharoplasty-type incision, usually from the same side, or it can be harvested from the retroauricular area (Fig. 18.2c). The modified Hughes procedure thus results in a bridge of conjunctiva from the upper lid across the visual axis for approximately 6 weeks. The vascularized pedicle of conjunctiva is subsequently released in a staged, second procedure once vascularization of the lower lid flap is achieved (Fig. 18.2d). The timing of the second stage of the modified Hughes procedure (when the pedicle of the flap is severed) depends on many factors. From the standpoint of vascular supply, studies have shown that a Hughes flap with good blood supply can be separated as early as 2 weeks after the first stage. However, there is a higher likelihood of lower eyelid ectropion after early separation of the flap. When postoperative adjuvant radiation therapy is planned for cutaneous cancers of the lower eyelid, it is necessary to separate the Hughes flap within 4–6 weeks after the first stage to allow for shielding of the globe and to allow radiation therapy to begin in a timely fashion (within 4–6 weeks after ablative surgery).
Large left lower eyelid defect closed with a Hughes flap. (a) Defect. (b) Intraoperative appearance after tarsoconjunctival flap harvested from upper eyelid has been sutured to lower eyelid. (c) Intraoperative appearance after full-thickness skin graft harvested from upper eyelid has been sutured over tarsoconjunctival flap of lower eyelid. (d) Postoperative appearance 6 months after repair and administration of postoperative adjuvant radiation therapy
Because it is an eyelid-sharing technique and may result in complications, the modified Hughes procedure should be avoided in certain patient groups whenever possible. Children under age 7 should not undergo this procedure as it may precipitate occlusion amblyopia. This procedure should also be avoided in the seeing eye of a monocular patient. Several complications may result following a modified Hughes procedure. For instance, the patient may develop an eyelid malposition. If the lower eyelid margin skin rotates inward, the patient is likely to develop keratitis, either from the keratinized skin surface or from the fine lanugo hairs arising from the skin [2]. The risk of this complication can be reduced during the second stage of the procedure when the surgeon transects the advancement flap. Specifically, care should be taken to angle the incision to create a longer posterior lamella with more conjunctiva than skin [2]. The conjunctiva can then be advanced over the lid margin, leaving it nonkeratinized. Another complication that may occur following the modified Hughes procedure is upper lid retraction. To reduce this risk, the Müller muscle should be dissected away from conjunctiva and not be advanced with the tarsoconjunctival flap during the first stage of the procedure [2]. During the second stage of the procedure, the conjunctiva of the upper lid is left unsutured; it may even be recessed if retraction is a concern [2]. Sloughing of the skin graft may also occur following the Hughes procedure, but this is an uncommon occurrence. If blood or fluid collect beneath the donor graft, poor donor–host apposition will occur, resulting in graft failure. Drainage holes in the skin graft will prevent any fluid accumulation under the graft [2]. A bolster suture that is placed over the graft will keep it firmly apposed to the underlying vascular bed [2]. Necrosis of the tarsoconjunctival flap is another rare complication and results from a poorly vascularized flap.
Alternative procedures include full-thickness pedicled flaps [7, 8] and a free tarsoconjunctival graft from the contralateral upper lid with an overlying vascularized bipedicled skin-and-muscle flap [9]. Another useful technique is the tarsal transposition flap, as described by Hewes et al. [10]. The advantage of these procedures is that only one surgical stage is needed and visual axis occlusion is avoided, but in our experience the outcomes are not as predictable as those of a modified Hughes procedure for large defects of the lower eyelid.
A large rotating cheek flap (Mustardé flap) works well for repair of a large anterior lamellar defect, but for posterior lamellar replacement, it must be coupled with a tarsal substitute, such as a free tarsoconjunctival autograft, hard palate mucosa, nasal septum cartilage and mucosa, full-thickness buccal mucous membrane, Hughes flap, free periosteal graft, or homologous tarsus [11–17]. The Mustardé cheek rotation flap often results in a rounded lateral canthus and is associated with a high risk of lower eyelid ectropion; thus, secondary revisions are often needed.
7 Small Defects Involving the Upper Eyelid Margin
Upper eyelid defects involving less than 33% of the lid margin can be repaired by primary closure. Mirroring what is possible with the lower lid, the superior crus of the lateral canthal tendon can be lysed to obtain an additional 3–5 mm of medial mobilization of the remaining lateral lid margin.
8 Moderate Defects Involving the Upper Eyelid Margin
Upper eyelid defects involving 33–50% of the lid margin are repaired by advancement of the lateral portion of the lid. A lateral canthotomy and superior cantholysis are performed, and a reverse Tenzel semicircular skin flap is created inferior to the lateral brow and canthus to allow additional mobilization of the lid [18–20].
Tarsal sharing procedures, which consist of an adjacent sliding tarsoconjunctival flap from the remaining part of the upper lid covered by either a skin–orbicularis advancement flap or a full-thickness skin graft, have also been described for repair of the upper lid.
9 Large Defects Involving the Upper Eyelid Margin
Upper eyelid defects involving greater than 50% of the lid margin are most commonly repaired utilizing a Cutler–Beard procedure (Fig. 18.3a). This technique involves advancing a composite full-thickness lower eyelid flap into the upper eyelid defect by passing it posterior to the remaining lower lid margin (Fig. 18.3b) [21]. Lysis of the flap is the second stage of the procedure and typically is performed 6–8 weeks after the first stage (Fig. 18.3c) [2].
Large right upper eyelid defect closed with a Cutler–Beard flap. (a) Defect. (b) Postoperative appearance following first stage of procedure showing the full-thickness lower eyelid flap sutured into the upper eyelid defect, coursing posterior to the intact lower eyelid margin. (c) Postoperative appearance of reconstructed right upper eyelid 6 months after repair
This procedure, however, results in a relatively thick and immobile upper eyelid. Upper eyelid stability is enhanced by placing a spacer graft, such as donor sclera or AlloDerm, in the upper eyelid [2]. To decrease postoperative keratitis, it is also helpful to lyse the flap in such a way that the conjunctival surface is longer than the skin surface. The conjunctiva can then be draped forward over the lid margin and sutured to the skin anteriorly [2]. Other potential complications of a Cutler–Beard procedure include blepharoptosis, lagophthalmos, and even lid retraction [2]. Upper eyelid retraction can be avoided by waiting a minimum of 6 weeks before performing the second-stage procedure and by transecting the flap approximately 2 mm below the level of the upper lid [2]. Necrosis of the bridge in the lower lid may result if the vascular supply is compromised. In creating the bridge during the first-stage procedure, the marginal arterial arcade should be avoided by making the incision 4 mm below the lid margin [2].
A potential alternative to a Cutler–Beard procedure for large upper lid defects is placement of a free tarsoconjunctival graft from the contralateral upper lid and coverage of this graft with a skin–muscle flap if the amount of redundant upper lid skin is adequate. However, for deep defects of the upper eyelid with loss of tissue extending into the conjunctival fornix and anterior orbit, a free tarsoconjunctival graft is not adequate, and a Cutler–Beard flap would be more appropriate.
A lower eyelid switch flap or median forehead flap has also been described for use in repairing large upper lid defects. If the upper lid defect is wide but shallow, involving only the lid margin, a tarsoconjunctival flap from the area just superior to the defect can be advanced inferiorly to replace the posterior lamella [2]. This flap must be well dissected toward the fornix. The levator aponeurosis is dissected away from the anterior face of the tarsus to prevent upper lid retraction during the postoperative period [2]. It may then be covered by either a full-thickness skin graft or a skin–orbicularis flap.
10 Lateral Canthal Defects
A key element of reconstruction in the lateral canthus is maintenance of the lower eyelid position and avoidance of lower eyelid ectropion. This is usually achieved by a lower eyelid tightening procedure that involves attaching the lower eyelid to the lateral orbital rim [2]. If the periorbita is of poor quality or absent, drill holes can be placed in the lateral orbital rim near Whitnall’s tubercle (the lateral orbital tubercle) [2]. In most individuals, the vertical position of the lateral canthus is approximately 2 mm higher than the vertical position of the medial canthus. Following extensive lower lid surgery, the lateral canthus tends to retract inferiorly. Thus, the lateral canthus should be positioned superiorly enough that the lower lid and canthus maintain good anatomic orientation.
Laterally based transposition flaps or upper lid tarsus and conjunctiva can be utilized for large lower lid defects that extend to the lateral canthus [22]. Free skin grafts can be used to cover these flaps. Semicircular advancement skin flaps may also be used for defects extending to the lateral canthus. Occasionally, strips of periosteum and temporalis fascia still attached at the lateral orbital rim can be used to attach the remaining lateral lid margins to the lateral orbital rim [22, 23].
11 Medial Canthal Defects
Large medial canthal defects require good fixation of the residual upper and lower eyelid to the medial canthal tendon insertion area (Fig. 18.4a). The fixation suture should be posterior enough and with solid attachment to the bone to achieve good apposition of the eyelid against the globe. Fixation may be carried out with heavy permanent suture, wire, or titanium miniplates [24]. In the majority of cases, the lid can be fixated by suturing its medial aspect to the deep tissues in the region of the posterior lacrimal crest, where the posterior limb of the medial canthal tendon normally inserts [2]. Various local flaps and grafts can be used to cover soft tissue defects in the medial canthal area. Full-thickness skin grafts are ideal for shallow defects of the medial canthus. For deeper defects, various forms of transposition flaps are more appropriate. A very useful flap for this location is a glabellar flap (Fig. 18.4b) [25–27]. Flaps can withstand postoperative adjuvant radiation therapy, if it is needed [27].
Loss of the lacrimal drainage apparatus, including the canaliculi, is common after removal of medial canthal cancers. We typically do primary repair of canaliculi with silicone stenting only for defects that involve up to 5 mm of canalicular loss; otherwise, we prefer to perform lacrimal bypass surgery, including placement of a Pyrex glass tube (“Jones tube”), after the soft tissue reconstruction in the medial canthal angle has stabilized and only if the patient has symptomatic epiphora.
Spontaneous granulation (“laissez faire” granulation) of anterior lamellar defects has been used with varying success because of cicatrix formation [28]. This is best used when the defect straddles the medial canthal tendon with approximately equal areas above and below the tendon [2]. In such cases, tissue shrinkage that occurs postoperatively should be symmetrical, minimizing the risk of displacement of the canthus or of lower lid ectropion. Of note, healing with a laissez faire strategy takes much longer than healing with grafts and flaps and requires daily care to avoid infection and prominent scars.
References
Patrinely JR, Marines HM, Anderson RL. Skin flaps in periorbital reconstruction. Surv Ophthalmol 1987;31:249–61.
Arthurs BP. Tumor excision and eyelid reconstruction. In: Della Rocca RC, Bedrosian EH, Arthurs BP, editors. Ophthalmic Plastic Surgery Decision Making and Techniques. New York, NY: McGraw-Hill, 2002:117–35.
Harvey J. Modified “double Z-plasty” in the closure of medial canthal defects. Ophthalmic Surg 1987;18:120–2.
Hughes WL, editor. Reconstructive Surgery of the Eyelids, second edition. St. Louis, MO: Mosby, 1954.
Smith B, Lisman R. Preparation of split thickness auricular cartilage for use in ophthalmic plastic surgery. Ophthalmic Surg 1982;13:1018–21.
Baylis HI, Rosen N, Neuhaus RW. Obtaining auricular cartilage for reconstructive surgery. Am J Ophthalmol 1982;93:709–12.
Anderson RL, Weinstein GS. Full thickness bipedicle flap for total lower eyelid reconstruction. Arch Ophthalmol 1987;105:570–6.
Anderson RL, Jordan DR, Beard C. Full-thickness unipedicle flap for lower eyelid reconstruction. Arch Ophthalmol 1988;106:122–5.
Leone CR, Van Gemert JV. Lower lid reconstruction using tarsoconjunctival grafts and bipedicle skin–muscle flap. Arch Ophthalmol 1989;107:758–60.
Hewes EH, Sullivan JH, Beard C. Lower eyelid reconstruction by tarsal transposition. Am J Ophthalmol 1976;81:512–4.
Kanski JJ, editor. Clinical Ophthalmology: A Systematic Approach, fifth edition. London: Butterworth Heinemann, 2003:25–6.
Putterman AM. Viable composite grafting in eyelid reconstruction. Am J Ophthalmol 1978;85:237–41.
Cohen MS, Shorr N. Eyelid reconstruction with hard palate mucosa grafts. Ophthal Plast Reconstr Surg 1992;8:183–95.
Siegel RJ. Palatal grafts for eyelid reconstruction. Plast Reconstr Surg 1985;76:411–4.
Brown BZ. The use of homologous tarsus as a donor graft in lid surgery. Ophthal Plast Reconstr Surg 1985;1:91–5.
Hurwitz JJ, Corin SM, Tucker SM. The use of free periosteal grafts in extensive lower lid reconstruction. Ophthalmic Surg 1989;20:415–9.
Jordan DR, Tse DT, Anderson RL, et al. Irradiated homologous tarsal plate banking: a new alternative in eyelid reconstruction: part II. Human data. Ophthal Plast Reconstr Surg 1990;6:168–76.
Tenzel RR. Reconstruction of the central one-half of an eyelid. Arch Ophthalmol 1975;93:125–6.
Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology 1978;85:1164–9.
Levine MR, Buckman G. Semicircular flap revisited. Arch Ophthalmol 1986;104:915.
Cutler NL, Beard C. A method for partial and total upper eyelid reconstruction. Am J Ophthalmol 1955;39:1.
Leone CR. Lateral canthal reconstruction. Ophthalmology 1987;94:238–41.
Holt JE, Holt GR, Van Kirk M. Use of temporalis fascia in eyelid reconstruction. Ophthalmology 1984;91:89–93.
Howard GR, Nerad JA, Kersten RC. Medial canthoplasty with microplate fixation. Arch Ophthalmol 1992;110:1793–7.
Dortzbach RK, Hawes MJ. Midline forehead flap in reconstructive procedures of the eyelids and exenterated socket. Ophthalmic Surg 1981;12:257–68.
Teske SA, Kersten RC, Devoto MH, et al. The modified rhomboid transposition flap in periocular reconstruction. Ophthal Plast Reconstr Surg 1998;14:360–6.
Spinelli HM, Jelks GW. Periocular reconstruction: a systematic approach. Plast Reconstr Surg 1993;91:1017–24.
Lowry JC, Bartley GB, Garrity JA. The role of second-intention healing in periocular reconstruction. Ophthal Plast Reconstr Surg 1997;13:174–88.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Shinder, R., Esmaeli, B. (2010). Reconstructive Surgery for Eyelid Defects. In: Esmaeli, B. (eds) Ophthalmic Oncology. M.D. Anderson Solid Tumor Oncology Series, vol 6. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-0374-7_18
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0374-7_18
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-0373-0
Online ISBN: 978-1-4419-0374-7
eBook Packages: MedicineMedicine (R0)