Abstract
About 3% of all melanomas are of ocular origin; of these, 85% are uveal. Uveal melanomas are rare, with standardized incidence rates ranging from approximately 2 to 8 cases per 1 million people in the United States and Europe. The typical presentation of uveal melanoma depends on the site of origin: choroid, iris, or ciliary body. About 80–90% of all uveal melanomas develop in the posterior choroid. Uveal melanoma is typically a clinical rather than a pathologic diagnosis. Currently, several options are available for the management of uveal melanoma, including observation, transpupillary thermotherapy, brachytherapy, stereotactic radiotherapy, proton radiotherapy, and tumor resection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Epidemiology
About 3% of all melanomas are of ocular origin; of these, 85% are uveal, and the majority are choroidal. Uveal melanomas are rare, with standardized incidence rates ranging from approximately 2 to 8 cases per 1 million people in the United States and Europe. Mean age at diagnosis is approximately 60 years, with the incidence rate increasing to age 70. Risk factors for development of uveal melanoma include history of choroidal nevi, ipsilateral nevus of Ota, and atypical mole syndrome. Weak correlations have suggested sunlight exposure as a possible causative agent. Welders and metal workers have also been reported as having a slightly higher incidence of uveal melanoma, possibly due to ultraviolet light exposure [1].
2 Clinical Features
The typical presentation of uveal melanoma depends on the site of origin: choroid, iris, or ciliary body. About 80–90% of all uveal melanomas develop in the posterior choroid. Patients with these tumors generally present with complaints of blurred vision or floaters. Occasionally, pain, inflammation, or double vision is noted. Metamorphopsia (distortion of vision) and photopsias (flashing lights) are not uncommon symptoms and may be associated with an exudative retinal detachment [2, 3].
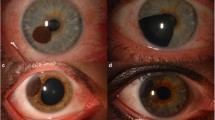
Iris melanomas are generally smaller at diagnosis than those of the choroid. Iris melanomas can grow in a circumscribed or diffuse pattern. The circumscribed type can vary in color and invade the anterior chamber, ciliary body, or posterior chamber. Diffuse iris melanomas can infiltrate the iris stroma, causing pupillary distortion.
Ciliary body melanoma can develop as a circumscribed or annular type. The circumscribed type is often brown and can invade the anterior chamber, causing elevated intraocular pressure. In contrast, the annular type grows around the ciliary body in a ring-type fashion. Ciliary body melanoma may be initially misdiagnosed as open-angle glaucoma because of the difficulty in visualizing a distinct mass [3, 4].
As the uvea has no intrinsic lymphatic drainage, metastasis occurs by hematogenous dissemination. Ciliary body melanomas can invade anteriorly toward the sclerocorneal limbus. Posteriorly located tumors can spread via the vortex veins or ciliary arteries, or they can have frank invasion past the sclera. Large peripapillary tumors can invade the optic nerve and adjacent meninges. The liver is the primary site of distant metastasis, followed by the skin and lung; brain metastasis rarely occurs [3].
3 Diagnosis
Uveal melanoma is typically a clinical rather than a pathologic diagnosis. A 20–40% misdiagnosis rate has been reported in historical series following enucleation. Yet with recent advances, this has been reduced to less than 1%. As is the case with any malignancy, a thorough systematic history should be obtained.
An external ocular examination should be performed to evaluate for dilated episcleral vessels or pigmented nodules suggestive of extraocular extension. Slit-lamp evaluation can reveal bulging of the iris, a distinct iris or ciliary body mass, cataract, or subluxation of lens. Indirect ophthalmoscopy can demonstrate details regarding tumor color, size, and configuration. Features such as drusen, subretinal fluid, retinal pigment epithelial changes, and orange pigment are important prognostic indicators that should be documented [5].
Gonioscopy should be performed for all tumors in the anterior segment. Fluorescein angiography can demonstrate pinpoint hyperfluorescence or a distinct “second” choroidal vasculature [6]. Echography should be performed in all cases and is the single most important noninvasive test. Typical ultrasonographic features of choroidal melanomas on B-scan echography include an internal acoustic quiet zone, choroidal excavation, and orbital shadowing (Fig. 15.1a). A-scan echography demonstrates low internal reflectivity with an angle kappa (Fig. 15.1b) [7, 8]. In rare cases in which these noninvasive techniques do not establish the diagnosis, tissue biopsy can be performed via an ab externo or ab interno approach.
Baseline testing should include liver function tests and chest and liver imaging (generally a computed tomography of the chest and abdomen with contrast) to rule out distant metastasis. Magnetic resonance imaging of the brain and orbit can be helpful in identifying intraocular features consistent with melanoma (Fig. 15.2).
4 Staging and Prognostic Factors
Currently, the staging process is less than ideal for uveal melanoma. Accurate use of the American Joint Committee on Cancer TNM staging system requires pathologic diagnosis, which is often not obtained in uveal melanoma cases since most are treated with brachytherapy. No widely accepted staging system is used for most iris melanomas.
In patients with uveal melanoma, prognostic factors for patient survival differ from prognostic factors for eye and vision preservation. The most important feature predicting mortality in uveal melanoma is largest basal diameter. Other factors correlating with increased morbidity include extrascleral extension, diffuse presentation, older age, male gender, rapid growth, and recurrence after treatment. Pathologic features in enucleated specimens indicative of poor prognosis include a large number of mitotic figures per high-power field or high Ki-67; a high number of tumor-infiltrating lymphocytes; and periodic acid Schiff identification of vasculogenic mimicry patterns. Fine-needle biopsy for tissue prognostication is currently undergoing scientific testing in a number of centers. Fluorescence in situ hybridization studies have suggested molecular abnormalities associated with chromosomes 1, 3, 6, and 8. Monosomy 3 strongly correlates with metastatic disease. Gene expression profiling using microarray analysis suggests that uveal melanomas can be divided into two groups. “Class 1” tumors (low grade) are thought to have a much lower risk of distant metastasis than “class 2” tumors (high grade) [9–13].
5 Background Studies
Historically, enucleation was considered the only acceptable method of managing uveal melanomas. In the late 1970s, this practice was brought into question by suggestions that enucleation might expedite metastasis by promoting intraoperative seeding of tumor cells (Zimmerman’s hypothesis) [14]. To evaluate this hypothesis, the Collaborative Ocular Melanoma Study (COMS) was organized in 1986. This was a multicenter effort with 43 participating centers in the United States and Canada. The COMS investigators conducted several studies, including two randomized trials and an observational study; in addition to reports on these studies, several technical papers have been published on the basis of the COMS results [15–17].
The observational study evaluated risk factors for growth of small melanomas (less than 3.0 mm in apical height) [18]. A total of 204 patients were enrolled and 188 were observed. On multivariate analysis, tumor characteristics associated with greater likelihood of growth included the presence of orange pigment, tumor thickness of at least 2 mm, and largest basal diameter of at least 12 mm [19].
One of the randomized clinical trials was conducted for medium-sized choroidal melanomas (2.5–10 mm in apical height and no more than 16 mm in largest basal diameter); patients were randomized to receive either enucleation or iodine-125 plaque brachytherapy [20]. Patients with tumors touching the optic disc or primarily in the ciliary body were excluded. A total of 1317 patients were randomized, and 12-year follow-up data showed no difference in melanoma-related morbidity between the two treatment arms. Visual loss secondary to brachytherapy correlated with tumor thickness, tumor proximity to the foveal avascular zone, and a history of diabetes. Visual loss was significant, with 43% of patients progressing to an acuity of 20/200 (legal blindness) within 3 years. The contralateral eye, however, was not affected by treatment. Patients with recurrence after brachytherapy were treated with enucleation for salvage; about 10% of patients who underwent enucleation had recurrence at 5 years [21]. A quality-of-life study was performed on 209 of the 1317 patients and found that visual acuity in patients who received brachytherapy was greater than that in patients who underwent enucleation until about 3–5 years after treatment [22].
In the second randomized trial, a total of 1003 patients with large tumors (greater than 10 mm in apical height or 16 mm in largest basal diameter) were randomized to enucleation with or without presurgical radiotherapy consisting of 20 Gy in five fractions [23]. This study was designed to address concerns regarding the possibility of tumor seeding during enucleation and the potential benefit of pre-enucleation radiotherapy. On 10-year follow-up, no difference was noticed in melanoma-related mortality, and neither harm nor benefit was ascribed to pre-enucleation radiotherapy [23].
In both of the randomized COMS trials—for medium and large choroidal melanoma—annual screening after treatment included liver function tests and chest radiography. The use of liver function tests to identify distant metastasis had a sensitivity of 15% and specificity of 92%; thus, the COMS authors recommended annual liver imaging. Liver echography and computed tomography are the most common methods of liver imaging, but some centers advocate the use of routine positron emission tomography scans.
6 Overview of Management
Currently, several options for the management of uveal melanoma are available, including observation, transpupillary thermotherapy, brachytherapy, stereotactic radiotherapy, charged-particle radiotherapy, and tumor resection. A choice between these modalities depends on tumor size, location, and growth pattern and the condition of the patient. The goal of vision and organ preservation should be balanced with that of tumor control. Asymptomatic tumors that are less than 10 mm in basal diameter and less than 2.5 mm in thickness may be reasonable candidates for observation. Medium-sized uveal melanomas generally receive brachytherapy but may be amenable to charged-particle radiotherapy or resection. Larger tumors are often treated by enucleation [14, 19].
7 Brachytherapy
The concept of treating uveal melanoma with brachytherapy began in the 1930s when Sir Foster Moore inserted radon 222 seeds directly into a choroidal melanoma. This technique was later changed to use of episcleral cobalt 60 and then to ruthenium 106 and iodine 125 eye plaques. Iodine 125 was used in the COMS protocol and is a practical isotope because low-energy photon radiation allows for shielding with 1 mm of lead, reducing dose to hospital personnel. Iodine 125’s half-life of 59 days allows for re-use of the seeds [24]. The plaque is shielded with gold, and the iodine 125 seeds are set in a template. These plaques can be customized to fit specific tumor locations, e.g., a notch can be placed to fit around the optic nerve. Plaques are available in various sizes ranging from 12 to 22 mm in diameter with multiple suture holes (Fig. 15.3) [24].
Ruthenium 106 is used at some institutions in Europe and has been used at our institution, but it is no longer commercially available in the United States. It is a beta emitter with a steeper dose gradient than iodine 125, allowing for lower dose delivery to surrounding structures. The half-life of ruthenium 106 is about 1 year, allowing for re-use of the plaque. This source is generally used for tumors with apical height of less than 5 mm. These plaques are thinner than the COMS iodine 125 plaques, making surgical placement easier and more comfortable for the patient.
Treatment planning begins with indirect ophthalmoscopy and ocular ultrasonography to delineate the location and exact dimensions of the tumor. The plaque size is chosen to give a 2–3 mm margin around the tumor base. As per the COMS protocol, dosing is based on the apical height measured from the scleral surface. A total dose of 85 Gy is prescribed to the apex of the tumor if the tumor apical height is greater than 5 mm; a total dose of 85 mm is prescribed to 5-mm height if the apical height is 5 mm or less. Because of the sharp dose gradient of the brachytherapy system, the apex is the prescription point and the area of minimum tumor dose. As such, much of the tumor actually receives more than the prescribed dose. Total dose rates should fall between 42.5 and 106 cGy/h. The use of a three-dimensional treatment planning system allows for decreased dose to be delivered to critical structures while ensuring dose delivery to the tumor by collimation of individual seeds [24].
Placement of the plaque is done in the operating room. The ophthalmologist transilluminates the globe and outlines the tumor shadow on the sclera. A dummy plaque is then placed over the marking, and loose sutures are placed in the suture holes. With the radiation oncologist present, the dummy plaque is removed, replaced by the radioactive plaque, and fastened in place with the sutures. A lead shield is placed over the affected eye as a safety precaution. The plaque is left in place for a number days, after which the patient is taken back to the operating room for removal of the plaque (Fig. 15.4).
This treatment is well tolerated in the short term. Late effects include dry eye, retinopathy, glaucoma, maculopathy, and scleral necrosis, depending on the proximity of the tumor and the radiation dose to adjacent structures. A significant percentage of patients develop radiation retinopathy. In a large review, poor long-term visual acuity was found to be associated with tumor location less than 5 mm from the fovea, age greater than 60 years, and use of cobalt 60 plaques [25].
8 Charged-Particle Radiotherapy
Proton radiotherapy offers the potential to deliver a homogenous and conformal dose to tumors, particularly those located close to critical structures such as the macula or optic disc. The physical properties of protons are such that stopping power is great, allowing for a high-dose deposition in the desired location with no exit dose. Restrictions related to tumor size or location are less than those with brachytherapy. The use of charged particles in treatment of uveal melanoma began in 1975, and about 20 institutions around the world have employed this approach [24].
Treatment planning is similar to the typical evaluation for uveal melanoma, with the addition of surgical tumor localization. Patients undergo intraoperative transillumination, and the base of the tumor is marked by suturing radio-opaque tantalum rings to the sclera around the tumor. Tumor and eye dimensions are entered into the treatment planning computer, and an aperture is designed for the proton beam that approximates the shape of the tumor with a 3-mm lateral margin. Doses to critical structures are calculated in the treatment plan made by the computer but assessed by the MD. During treatment, patients are immobilized, and the eye is aligned on a flashing light; the eye is monitored for movement. Lid retraction is used to reduce treatment of the eyelid. The standard dose is 60–70 cobalt Gy equivalents in four to five fractions [24].
Several extensive series of uveal melanoma patients treated with proton radiotherapy have been published. Neovascular glaucoma was the most common cause of subsequent enucleation and was more prominent in patients with larger tumor volumes [25]. Other complications included radiation maculopathy and papillopathy, which was greater among patients with tumors close to the optic disc. Vision loss was associated with dose to the macula of greater than 35 cobalt Gy equivalents, larger apical height, and a history of diabetes. Local tumor control is excellent with protons. Comparison of complication and survival rates between proton and plaque treatment is difficult since many patients are referred to proton centers because of larger tumor size or tumor location close to the optic disc or macula [26–30].
9 Surgical Techniques
9.1 Uveal Resection
Depending on the size and location of the tumor, uveal resection can be a good treatment option for globe salvage. Small iris and ciliary body tumors (less than 4 clock hours) can be safely resected by iridectomy or iridocyclectomy techniques. Some surgeons advocate hypotensive anesthesia to reduce the risk of expulsive hemorrhage. The main complications are iris coloboma and lens instability from ciliary body excision. Visually, this can lead to photophobia and polyopia. Transscleral resection of choroidal tumors was popularized in the late 1970s and 1980s; however, given the high percentage of scleral invasion in many uveal melanomas, there is concern about inadequate resection with such procedures [31]. As a result, some centers routinely treat patients with adjuvant plaque brachytherapy at the time of resection [31, 32]. This approach (uveal resection) also exposes the patient to the possibility of expulsive hemorrhage and the risk of orbital tumor seeding.
9.2 Enucleation
Primary enucleation is typically used with large uveal melanomas that involve greater than one-half of the globe. Integrated implants, such as hydroxyapatite and Medpor, are generally implanted and provide excellent cosmesis with good ocular motility. When local extraocular extension is present, a modified enucleation can be performed with excision of the overlying tissue removed en bloc with the globe. Exenteration is rarely indicated but can provide good local control in cases of diffuse orbital involvement.
9.3 Transpupillary Thermotherapy
Transpupillary thermotherapy involves a low-energy diode laser that heats the tumor and surrounding choroid to 45–60°C. The laser is generally administered in multiple sessions. As a primary treatment modality, this technique is recognized as being associated with a risk of local recurrence, especially for thicker tumors and tumors that overhang the optic nerve. Transpupillary thermotherapy is increasingly used as an adjuvant modality following plaque brachytherapy (also referred to as “sandwich” therapy, which is brachytherapy followed by thermotherapy). Significant visual field loss can occur in the area treated; other complications include extrascleral extension, hemorrhage, and vascular occlusion [33].
9.4 Pathologic Assessment
An enucleation specimen is the most common tissue specimen obtained for pathologic evaluation. The intact globe is received fresh from the operating room when tissue is harvested for research purposes and/or tissue banking. Initial pathologic assessment of the specimen includes three-dimensional measurements of the globe and the length of the attached optic nerve. Also, the iris is examined for any deformity or gross involvement by the tumor. Each external component of the eye and anterior chamber is evaluated, and any abnormalities are documented. Samples of the vortex veins, located in the posterior portion of each quadrant, should be obtained for histologic examination. The entire extraocular portion of each vein is removed, and its location is noted (Fig. 15.5). A compound microscope may be used for gross assessment of ocular specimens, as needed.
Transillumination is used to locate the intraocular mass. When a light is held directly proximal to the pupil or sclera, light is transmitted into the vitreous, which glows through the sclera when the normal ocular structures are in place. A shadow, when noted, is marked on the sclera with a colored pencil, and its location is noted relative to its distance from the limbus, optic nerve, and region involved (i.e., 11:00 to 2:00) (Fig. 15.6). The basal dimensions of the tumor are also noted. Although the shadow may correspond directly to the mass, retinal detachment can also cause a shadow that may obscure the exact size and location of the tumor.
Optimal sectioning of the tumor, following fixation in 10% buffered formalin, is generally achieved when the pupil and optic nerve are seen in cross section along with the tumor (Fig. 15.6) [34]. Horizontal, vertical, or oblique sectioning of the globe can be used to obtain this orientation.
If fresh tissue is to be harvested prior to fixation, a window or flap is opened adjacent to the tumor in the same plane from which the main tissue sections will be taken (Fig. 15.6). Normal retina and choroid are removed from the scleral flap. The tumor is then incised, using a sterile scalpel blade parallel to the window, and removed with forceps. No more than one-third of any tumor should be harvested to ensure the integrity of the specimen for histologic diagnosis. Also, tissue harvesting should be avoided when the tumor is small or flat or when it is poorly visualized.
9.5 Histologic Examination
Histologic parameters include the initial determination that the lesion is a melanoma [35]. Among the primary intraocular tumors, uveal melanoma is the most common [36]. Uveal melanomas arise most commonly in the choroidal space and less frequently in the ciliary body and iris [35]. Large choroidal melanomas may involve adjacent structures, and any such involvement is noted in the pathologic report. Both the largest tumor dimension and tumor cell types (epithelioid, spindle, or mixed), which are important predictors of outcome, are documented [37, 38]. The growth pattern of a thin, diffuse, spreading melanoma should be documented, and additional hematoxylin and eosin-stained levels of the tumor should be examined, as this growth pattern portends a higher risk of extraocular extension and high risk of metastatic potential (25% at 5 years) despite its flatness [38, 39]. Multiple hematoxylin and eosin-stained levels are examined to check for invasion of the sclera directly or around nerves and vessels and exclude extraocular tumor extension, which would warrant additional therapy. Likewise, involvement of the optic nerve, optic nerve margin, or meninges must be assessed [40].
Unlike retinoblastomas, uveal melanomas generally do not spread via the optic nerve; however, they are more likely than retinoblastomas to invade the vortex veins [38]. Thus, both the vortex veins as they course through the sclera and the extraocular portions of the vortex veins are sampled and assessed [34].
Additional intratumoral factors—including complex vascular loops (which are optimally visualized for evaluation by a periodic acid Schiff stain) and mitotic figures (number of mitoses per 10 high-power fields)—may provide additional prognostic information [40, 41]. The final pathologic report includes both the findings on gross assessment and the pathologic parameters of the uveal melanoma, which facilitates determination of mortality risk for patients with this disease.
10 Conclusion
The past two decades have seen significant advances in the ocular treatment of uveal melanomas. Large prospective randomized trials, such as the COMS, have demonstrated the efficacy and benefits of globe-salvaging approaches, such as plaque brachytherapy. Charged-particle radiotherapy has also become an accepted standard of care, particularly for tumors adjacent to critical ocular structures such as the disc and macula. Unfortunately, these advances in treatment of the primary tumor have not been accompanied by advances in treatment for distant metastatic disease, for which limited effective therapy exists. The next decade is likely to see further research in gene expression and identification of specific tumors with high metastatic potential. Those tumors should be targeted with adjuvant therapies to treat and prevent extraocular recurrence and reduce patient morbidity.
References
Singh AD, Damato B, Howard P, et al. Uveal melanoma: genetic aspects. Ophthalmol Clin North Am 2005;18(1):85–97, viii.
McLean IW, Saraiva VS, Burnier MN Jr. Pathological and prognostic features of uveal melanomas. Can J Ophthalmol 2004;39(4):343–50.
Woll E, Bedikian A, Legha SS. Uveal melanoma: natural history and treatment options for metastatic disease. Melanoma Res 1999;9(6):575–81.
McLean IW, Keefe KS, Burnier MN. Uveal melanoma. Comparison of the prognostic value of fibrovascular loops, mean of the ten largest nucleoli, cell type, and tumor size. Ophthalmology 1997;104(5):777–80.
Damato BE. An approach to the management of patients with uveal melanoma. Eye 1993;7(Pt 3):388–97.
Damato B. Detection of uveal melanoma by optometrists in the United Kingdom. Ophthalmic Physiol Opt 2001;21(4):268–71.
Liu T, Lizzi FL, Silverman RH, et al. Ultrasonic tissue characterization using 2-D spectrum analysis and its application in ocular tumor diagnosis. Med Phys 2004;31(5):1032–9.
Bakri SJ, Sculley L, Singh AD. Imaging techniques for uveal melanoma. Int Ophthalmol Clin 2006;46(1):1–13.
Onken MD, Worley LA, Person E, et al. Loss of heterozygosity of chromosome 3 detected with single nucleotide polymorphisms is superior to monosomy 3 for predicting metastasis in uveal melanoma. Clin Cancer Res 2007;13(10):2923–7.
Onken MD, Worley LA, Davila RM, et al. Prognostic testing in uveal melanoma by transcriptome profiling of fine-needle biopsy specimens. J Mol Diagn 2006;8(5):567–73.
Onken MD, Worley LA, Ehlers JP, et al. Gene expression profiling in uveal melanoma reveals two molecular classes and predicts metastatic death. Cancer Res 2004;64(20):7205–9.
Damato B, Eleuteri A, Fisher AC, et al. Artificial neural networks estimating survival probability after treatment of choroidal melanoma. Ophthalmology 2008;115(9):1598–607.
Damato B, Duke C, Coupland SE, et al. Cytogenetics of uveal melanoma: a 7-year clinical experience. Ophthalmology 2007;114(10):1925–31.
Singh AD, Damato BE, Pe’er J. Clinical Ophthalmic Oncology. Philadelphia, PA: Saunders Elsevier, 2007.
Astrahan MA, Luxton G, Jozsef G, et al. An interactive treatment planning system for ophthalmic plaque radiotherapy. Int J Radiat Oncol Biol Phys 1990;18(3):679–87.
Chiu-Tsao ST, Anderson LL, O’Brien K, et al. Dosimetry for 125I seed (model 6711) in eye plaques. Med Phys 1993;20(2 Pt 1):383–9.
de la Zerda A, Chiu-Tsao ST, Lin J, et al. 125I eye plaque dose distribution including penumbra characteristics. Med Phys 1996;23(3):407–18.
The Collaborative Ocular Melanoma Study Group. Factors predictive of growth and treatment of small choroidal melanoma. COMS report no. 5. Arch Ophthalmol 1997;115(12):1537–44.
The Collaborative Ocular Melanoma Study Group. Mortality in patients with small choroidal melanoma. COMS report no. 4. Arch Ophthalmol 1997;115(7):886–93.
Jampol LM, Moy CS, Murray TG, et al. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: IV. Local treatment failure and enucleation in the first 5 years after brachytherapy. COMS report no. 19. Ophthalmology 2002;109(12):2197–206.
Diener-West M, Earle JD, Fine SL, et al. The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma, III: initial mortality findings. COMS report no. 18. Arch Ophthalmol 2001;119(7):969–82.
Melia M, Moy CS, Reynolds SM, et al. Quality of life after iodine 125 brachytherapy vs enucleation for choroidal melanoma: 5-year results from the Collaborative Ocular Melanoma Study: COMS QOLS report no. 3. Arch Ophthalmol 2006;124(2):226–38.
Hawkins BS. The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma: IV. Ten-year mortality findings and prognostic factors. COMS report number 24. Am J Ophthalmol 2004;138(6):936–51.
Brady L. Radiotherapy of Intraocular and Orbital Tumors, second revised edition. New York, NY: Springer, 2003.
Shields CL, Shields JA, Cater J, et al. Plaque radiotherapy for uveal melanoma: long-term visual outcome in 1106 consecutive patients. Arch Ophthalmol 2000;118(9):1219–28.
Damato B, Kacperek A, Chopra M, et al. Proton beam radiotherapy of iris melanoma. Int J Radiat Oncol Biol Phys 2005;63(1):109–15.
Kodjikian L, Roy P, Rouberol F, et al. Survival after proton-beam irradiation of uveal melanomas. Am J Ophthalmol 2004;137(6):1002–10.
Dendale R, Lumbroso-Le Rouic L, Noel G, et al. Proton beam radiotherapy for uveal melanoma: results of Curie Institut-Orsay proton therapy center (ICPO). Int J Radiat Oncol Biol Phys 2006;65(3):780–7.
Gragoudas ES, Lane AM, Regan S, et al. A randomized controlled trial of varying radiation doses in the treatment of choroidal melanoma. Arch Ophthalmol 2000;118(6):773–8.
Egan KM, Gragoudas ES, Seddon JM, et al. The risk of enucleation after proton beam irradiation of uveal melanoma. Ophthalmology 1989;96(9):1377–82; discussion 1382–3.
The Collaborative Ocular Melanoma Study Group. Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study. COMS report no. 6. Am J Ophthalmol 1998;125(6):745–66.
Damato B. Treatment of primary intraocular melanoma. Expert Rev Anticancer Ther 2006;6(4):493–506.
Damato B, Jones AG. Uveal melanoma: resection techniques. Ophthalmol Clin North Am 2005;18(1):119–28, ix.
Folberg R, Verdick R, Weingeist TA, et al. The gross examination of eyes removed for choroidal and ciliary body melanomas. Ophthalmology 1986;93(12):1643–7.
The Collaborative Ocular Melanoma Study Group. Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study. COMS report no. 6. Am J Ophthalmol 1998;125(6):745–66.
Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyes with uveal metastases. Ophthalmology 1997;104(8):1265–76.
Gamel JW, Greenberg RA, McLean IW, et al. A clinically useful method for combining gross and microscopic measurements to select high-risk patients after enucleation for ciliochoroidal melanoma. Cancer 1986;57(7):1341–4.
Singh AD, Shields CL, Shields JA. Prognostic factors in uveal melanoma. Melanoma Res 2001;11(3):255–63.
Shields CL, Shields JA, De Potter P, et al. Diffuse choroidal melanoma. Clinical features predictive of metastasis. Arch Ophthalmol 1996;114(8):956–63.
Folberg R, Salomao D, Grossniklaus HE, et al. Recommendations for the reporting of tissues removed as part of the surgical treatment of common malignancies of the eye and its adnexa. The Association of Directors of Anatomic and Surgical Pathology. Hum Pathol 2003;34(2):114–8.
McLean IW, Saraiva VS, Burnier MN Jr. Pathological and prognostic features of uveal melanomas. Can J Ophthalmol 2004;39(4):343–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Ludwig, M., Garden, A.S., Williams, M.D., Gombos, D.S. (2010). Management of Uveal Melanoma. In: Esmaeli, B. (eds) Ophthalmic Oncology. M.D. Anderson Solid Tumor Oncology Series, vol 6. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-0374-7_15
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0374-7_15
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-0373-0
Online ISBN: 978-1-4419-0374-7
eBook Packages: MedicineMedicine (R0)