Abstract
The workplace is, apart from smoking, a clearly identified cause for the development of chronic obstructive lung diseases, including asthma (Trupin et al. 2003). Many asthmatic subjects complain that their symptoms are worse at work as related to exposure to their workplace physical and psychological environmental stimuli. Epidemiological studies in the general population show that from 5% to one-third of all asthmatic subjects answer “yes” to the question: “Are your asthmatic symptoms worse at work?” (Blanc and Toren 1999; Johnson et al. 2000). Asthma in the workplace (AWP) encompasses several entities (Fig. 18.1) (Vandenplas and Malo 2003; Bernstein et al. 2006). First, some workplaces can cause asthma, mostly in subjects who, before starting to work, reported no respiratory symptoms. This condition is labelled “occupational asthma” (OA). Two causal mechanisms are implicated. Workers may develop an “allergy” to a product present at work or develop asthmatic symptoms after accidental inhalation of a product generated at abnormally high concentrations. Second, asthmatic subjects may report that their symptoms are aggravated or exacerbated at work although the workplace is not the cause of asthma. Third, several variants of asthma related to the workplace have been described. For instance, some workers in aluminium potrooms develop symptoms that share features of symptoms experienced by asthmatic subjects. Also, a condition that is called occupational eosinophilic bronchitis reproduces the pathologic but not the lung function features of OA.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Occupational Asthma
- Asthmatic Subject
- Safety Data Sheet
- Specific Inhalation Challenge
- Eosinophilic Bronchitis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
General Considerations
Definitions
The workplace is, apart from smoking, a clearly identified cause for the development of chronic obstructive lung diseases, including asthma (Trupin et al. 2003). Many asthmatic subjects complain that their symptoms are worse at work as related to exposure to their workplace physical and psychological environmental stimuli. Epidemiological studies in the general population show that from 5% to one-third of all asthmatic subjects answer “yes” to the question: “Are your asthmatic symptoms worse at work?” (Blanc and Toren 1999; Johnson et al. 2000). Asthma in the workplace (AWP) encompasses several entities (Fig. 18.1) (Vandenplas and Malo 2003; Bernstein et al. 2006). First, some workplaces can cause asthma, mostly in subjects who, before starting to work, reported no respiratory symptoms. This condition is labelled “occupational asthma” (OA). Two causal mechanisms are implicated. Workers may develop an “allergy” to a product present at work or develop asthmatic symptoms after accidental inhalation of a product generated at abnormally high concentrations. Second, asthmatic subjects may report that their symptoms are aggravated or exacerbated at work although the workplace is not the cause of asthma. Third, several variants of asthma related to the workplace have been described. For instance, some workers in aluminium potrooms develop symptoms that share features of symptoms experienced by asthmatic subjects. Also, a condition that is called occupational eosinophilic bronchitis reproduces the pathologic but not the lung function features of OA.
OA is a type of asthma caused by an agent present in the workplace. It is defined as “a disease characterized by variable airflow limitation and/or airway hyper-responsiveness and/or inflammation due to causes and conditions attributable to a particular occupational environment and not to stimuli encountered outside the workplace” (Bernstein et al. 2006). As regards the allergic type of OA, two categories of causal agents present at work can be identified. Those derived from proteins exert their allergic effect through an IgE-mediated mechanism, a situation similar to the allergic type of common asthma. The other category of agents is chemicals. In this case, the mechanism is rarely IgE-mediated and is still generally unknown. The other type of OA is rarer. It is caused by an irritant accidental exposure at work. This condition is referred to as “irritant-induced asthma” or Reactive Airways Dysfunction Syndrome (RADS) if the accident is unique and not recurrent.
Occupational Asthma
Occupational Asthma with a Latency Period
This condition represents 80–90% of all cases of OA. A worker exposed at work to a potential sensitizer may develop an “allergy” to this product with rhinoconjunctival and respiratory symptoms. The natural history of this condition is illustrated in Fig. 18.2 with a list of factors that may play a role at each step. After acquiring sensitization, some subjects may first develop rhinoconjunctival symptoms. We may also hypothesize that some subjects will first develop airway inflammation, followed by airway hyper-responsiveness and changes in airway calibre. Some subjects will develop OA. After removal from exposure, subjects generally improve, but the majority is still left with asthmatic symptoms and abnormalities of airway function and hyper-responsiveness. We know that the shorter the period with symptoms while at work, has been, the more likely subjects are to be cured from asthma, as summarized elsewhere (Becklake et al. 2006). Administration of anti-inflammatory preparations in addition to cessation of exposure may maximize the chance of recovery (Malo et al. 1996).
The list of agents causing OA includes more than 250 high- (proteinaceous) and low- (chemicals) molecular-weight agents. Table 18.1 gives the most frequent causes and occupations. Lists are available on the Web (http://www.asthme.csst.qc.ca and http://www.asmanet.com, both French- and English-language sites). The mechanism of sensitization to high-molecular-weight agents is similar to what is described for ubiquitous allergens, i.e. IgE-mediated (Lemière et al. 2006a). For most low-molecular-weight agents, the mechanism remains unknown.
The diagnosis of OA is based on a decision tree that is shown in Fig. 18.3 (Chan-Yeung and Malo 1995). The clinical history is sensitive but not specific. Symptoms generally considered to be classic, such as improvement of symptoms during weekends and vacations combined with worsening of asthma while at work are not satisfactory predictors of the presence of OA (Vandenplas et al. 2005). For high-molecular-weight agents, nasal and ocular symptoms are most important to document as they often accompany and even precede asthma symptoms and are significant predictors of the presence of OA (Vandenplas et al. 2005). For low-molecular-weight agents, no symptoms have been identified as good predictors of OA. What is important for a physician who sees an asthmatic subject is to always inquire about the subject’s type of work and, as importantly, about the nature of products present at work and not only those handled by the patient. Exhaustive lists of agents reported as causing OA have been published on the Web (see http://www.asthme.csst.qc.ca and http://www.asmanet.com, both French-language sites). Safety data sheets (SDS) can help but are not entirely reliable. Many sensitizers present at concentrations lower than 1% are not identified (Bernstein 2002). Every adult-onset asthmatic subject should be questioned about his/her current and past workplaces and, if agents known to cause OA are present, objectively investigated. In OA, the severity of the asthmatic condition is generally worse than for asthma not caused by the workplace (LeMoual et al. 2005). Not only current but also past workplaces should be investigated, as the resulting asthma condition may have been caused by a product to which the worker is no longer exposed. The majority of subjects with OA are indeed left with permanent asthma even after stopping exposure to the agent that caused OA (see below). For high-molecular-weight agents, even if standardized allergens exist, their quality is highly variable. This being said, it would be highly unlikely for a baker with OA not to have positive skin tests to flour or enzymes. The same applies for a laboratory worker exposed to rodents. Therefore, a simple prick test can be used to identify the presence of sensitization, at least for some high-molecular-weight allergens. The absence of immunological sensitization in these circumstances makes the diagnosis of OA highly unlikely, unless some other sensitizers are present in the workplace. As shown in Fig. 18.3, the status of immunological sensitization can be assessed for high-molecular-weight agents only.
After examining immunological sensitization, the next step is to verify whether the target organ, in this case the bronchi, is involved. This can be done by assessing airway calibre and responsiveness to methacholine, as well by assessing inflammation. This evaluation enables the clinician to find out whether the subject has asthma. Once this is done, the crucial thing to find out is whether asthma is caused by the workplace. This can be done either by exposing the worker in a hospital laboratory to the possible etiological agent by specific inhalation challenges or by returning the worker to his/her workplace and comparing changes in airway function and inflammation for a period at work and off work. For this, serial assessment of peak expiratory flows (PEF) can be used. Also, a technician can go to the workplace and assess airway calibre during a workshift. At the end of the workshift, airway responsiveness and inflammation are reassessed.
As cited by Murphy, “the investigation of allergic problems requires the inquisitiveness of a Sherlock Holmes, the genius of Thomas Edison, the patience of Diogenes and the optimism of an idiot” (Murphy 1976).
Occupational Asthma Without a Latency Period: Irritant-Induced Asthma and Reactive Airways Dysfunction Syndrome
The consequences of accidental inhalation injuries were recognized in the early twentieth century, during World War I. Exposures to war gases such as mustargen caused acute lung injury and edema, which were more frequent causes of death than bronchial damage. However, not until mid-century was bronchial damage documented, especially in civil populations living close to railways who were accidentally exposed to spills producing irritant vapours such as chlorine (Das and Blanc 1993) and ammonia. Assessment of bronchial responsiveness to pharmacological agents was more routinely carried out in the investigation of cases. The Bhopal accident, which exposed the civilian population to monoisocyantes (Nemery 1996), and, more recently, the World Trade Center disaster (Scanlon 2002), during which firefighters inhaled a vast amount of a mixture of dry particles, aerosols and vapours, represented major occurrences of the so-called Reactive Airways Dysfunction Syndrome (acronym = RADS), a label proposed by Brooks and colleagues (Brooks et al. 1985) in 1985.
The more general term of irritant-induced asthma, which was more recently proposed for this syndrome, may encompass not only RADS, which is related to a single accident, but also instances of recurrent episodes, sometimes in workers exposed to lower but still irritant concentrations of a gas, vapour or dust (Gautrin et al. 2006a).
The diagnosis is based on the clinical history of a subject free of respiratory diseases who is acutely exposed to an agent (most often a vapour) generated at high concentrations and who presents an intense nasal burn (Meggs 1994) with important coughing and, less consistently or at a later stage, shortness of breath and wheezing. Reversible airway obstruction or hyper-responsiveness is documented in the hours or days following the accident. Examination of bronchial biopsies obtained from sufferers and animals close to the inhalational accident shows important desquamation of the epithelium followed by more important thickening of the submucosal space than what is found in asthma and in OA with a latency period (Gautrin et al. 1994; Demnati et al. 1998a; Martin et al. 2003), which explains lesser reversibility of airway obstruction to an inhaled bronchodilator. As for OA with a latency period, this syndrome leaves permanent asthmatic sequelae (Malo et al. 1994). Approximately one-quarter of affected subjects are cured around 2 years after the inhalational accidents (Malo et al. 1994), a proportion similar to that found in OA with a latency period. In an animal model, early administration of steroids soon after the inhalational accident has been shown to be beneficial (Demnati et al. 1998b). Administration of parenteral and inhaled steroids is also recommended in humans (Lemière et al. 1997).
Work-Aggravated Asthma
Work-aggravated asthma (WAA) is defined as pre-existing or concurrent asthma that is exacerbated by workplace exposure (Wagner and Wegman 1998; Vandenplas and Malo 2003; Bernstein et al. 2006), implying that the workplace triggers but does not induce asthma.
According to epidemiologic studies that used various definitions of WAA based on self-reports, 18–34% of the respondents reported worsening of asthma in association with work (Saarinen et al. 2003; Axon et al. 1995; Tarlo 2000; Blanc and Toren 1999; Goe et al. 2004; Johnson et al. 2000). Henneberger not only defined WAA based on a self-reported symptom-work association, but also required that the participant was likely to be exposed to agents liable to cause asthma at work, as determined by researchers who reviewed self-reported details about the participant’s job (Henneberger et al. 2006). In this study, 24% of the employed adults with asthma met the symptom and exposure criteria for WAA.
Differentiating OA from WAA is often difficult in clinical practice. Workers with WAA tend to show functional characteristics similar to those shown by subjects with OA (Girard et al. 2004). However, subjects with OA show eosinophilic airway inflammation when exposed to a specific agent at their workplace, whereas subjects with WAA show neutrophilic airway inflammation (Girard et al. 2004). Although subjects with OA tend to improve after removal from exposure, subjects with WAA do not show significant improvement in their respiratory function (Lemière et al. 2006b).
Few data are available regarding the socio-economic consequences of WAA. However, WAA seems to be associated with substantial socio-economic consequences. Labarnois et al. evaluated the socio-economic outcome of subjects experiencing work- related asthma symptoms (Larbanois et al. 2002). Although the rate of job change or work loss was seen to be higher in OA subjects, they found that the rates of work disruption and income loss were similar among both OA and WAA subjects, indicating that WAA and OA may have a similar socio-economic impact.
Variants
Eosinophilic Bronchitis
Eosinophilic bronchitis is a condition identified in 1989 in subjects complaining of chronic cough (Gibson et al. 1989). Eosinophilic bronchitis has been shown to be the cause of 12% of cases of chronic cough (Brightling et al. 1999). This condition was also reported in the occupational setting in a subject who developed respiratory symptoms on exposure to cyanoacrylates (Lemière and Hargreave 1999). This condition has been reported with several other occupational agents. Diagnostic criteria have been proposed (Quirce 2004): isolated chronic cough (lasting more than 3 weeks) that worsens at work, sputum eosinophilia greater than 2.5% in either spontaneous or induced sputum, increases in sputum eosinophilia related to exposure to the offending agent (either at work or after a specific inhalation challenge in the laboratory), spirometry parameters within normal limits and not significantly affected by exposure to the offending agent, absence of airway hyper-responsiveness to methacholine both at work and away from work, and other causes of chronic cough ruled out. This condition is likely to be underestimated since induced sputum is not routinely performed in many centers. Although it is not known whether subjects with occupational eosinophilic bronchitis will develop OA if they stay exposed to the offending agent, it would seem medically prudent to remove symptomatic subjects from the workplace.
Aluminium Potroom Asthma
Workers in aluminium potrooms often suffer from respiratory symptoms with some wheezing. Although reversible airway obstruction and hyper-responsiveness can be demonstrated in these symptomatic workers, changes in airway calibre during a workshift do not generally, except in rare cases (Desjardins et al. 1994), reach levels that are considered significant to diagnose OA, which is a 20% fall in FEV1 (Bernstein and Merget 2006).
Grain-Dust Induced Asthma
Exposure to grain dust can cause a variety of respiratory symptoms, including OA as such and asthma-like syndromes and non-allergen-induced airflow obstruction (Chan-Yeung et al. 2006). In addition, exposure to grain dust is often accompanied by the development of fixed chronic airway obstruction.
As a Burden to Health
Medico-Legal Considerations
OA is an accepted medico-legal condition in most countries (Dewitte et al. 1994; Bersntein et al. 2006). Workers can therefore apply to their respective national agencies for compensation, provided that they have access to such insurance. Many workers fail to apply because the social and financial benefits they may derive are minimal, as in the U.K. or France. Application may even make the situation worse since workers may suffer employment prejudice. Too often, the diagnosis is not based on objective evidence (Moscato et al. 2002; Ameille et al. 2003; Nicholson et al. 2005). A compatible history is considered sufficient in most instances, which should not be the case since clinical history is sensitive but not specific (see above). Making a wrong diagnosis has major social and financial consequences for workers, employers and medico-legal agencies. On the one hand, advising a worker (in most instances, these are young workers) to leave his/her job often results in retraining and unemployment. On the other hand, telling a worker not to leave his/her job if he/she suffers from OA will result in more severe asthma (deaths have been reported in subjects who remain at their workplace (Ortega et al. 2002)) and less likelihood of being free of asthmatic sequelae, since the longer the symptoms last, the more likely asthma will persist (Becklake et al. 2006).
Ideally, workers should not remain exposed to the agent that caused OA. The main focus should be placed on rehabilitation programs with financial compensation and not on financial compensation alone, because affected workers are generally young and can be retrained in a new job. If this is not achievable, at least reducing exposure should be the aim. Although long-term assessment of workers who are less exposed has not been carried out, there are documented short-term advantages (Slovak et al. 1985; Vandenplas et al. 1995). Workers should be encouraged to take inhaled anti-inflammatory preparations to hasten improvement (Malo et al. 1996). The cost of medications used to control asthma should be covered by the medico-legal agencies.
Medico-legal considerations should also include the possibility of allocating impairment/disability since permanent sequelae are the rule more often than not. Studies of the natural history of OA show that the rate of improvement is greater in the two first years or so after leaving work with some improvement thereafter, though at a slower rate (Malo and Ghezzo 2004). For practical reasons, it has been suggested that workers be re-assessed for permanent impairment/disability approximately 2 years after stopping exposure.
Impairment represents a loss in function, whereas disability is the impact of this loss on the worker’s life (Bersntein et al. 2006). To assess the former, a scaling system has been advocated (American Medical 2001) based on recommendations made by the American Thoracic Society (American Thoracic Society 1993) that include key elements, i.e. airway calibre and hyper-responsiveness, as well as the need for medication to control asthma as proposed in Quebec in 1984 (Dewitte et al. 1994). One of several tools used to assess disability is to evaluate answers to a disease-specific questionnaire on quality of life with asthma (Juniper et al. 1999). This questionnaire was administered to nearly 100 workers who were accepted by the Quebec medico-legal agency and seen 2 years after cessation of exposure. Most were employed. Quality of life was minimally affected (Malo et al. 1993). The same conclusion was reached more recently in a small group of workers from Ontario, Canada, with OA due to latex, who found alternative jobs (Al-Otaibi et al. 2005).
Prevention Issues
Since reducing or even eliminating possible harmful exposures is a key issue in the prevention of OA, all prevention programs should first be focused on industrial hygiene measures. It has been demonstrated in many epidemiological studies that exposure is the single most important determinant of OA (Becklake et al. 2006). There is general agreement that atopic workers (i.e. those with documented allergies to general ubiquitous inhaled allergens such as house dust, mites, pollens, pets, and moulds) should not be excluded from at-risk workforces. Although they are at greater risk of developing sensitization to high-molecular-weight agents, the risk is not high enough (ORs in the order of 2–4 depending on the study) to justify such interventions. Moreover, since 50% of young individuals are atopic (Gautrin et al. 1997), it would be impractical to exclude 50% of possible workers from specific workplaces.
We do not know for sure whether medical primary (before symptoms start) or secondary (pre-clinical status, in this instance once sensitization has occurred) prevention programs in high-risk workplaces are efficient and cost-effective (Tarlo and Liss 2005). How useful is performance in allergy skin tests to flour and enzymes in bakers and to rodent proteins in workers exposed to laboratory animals? How useful is the assessment of bronchial responsiveness and repeating this test serially? What is sure is that once the disease is present (tertiary prevention), early removal from exposure is crucial as discussed above.
Epidemiology
General Considerations
Epidemiology is a discipline that studies the distribution and determinants of health-related states and disease in populations (Last 1995). The determinants include environmental and personal host factors. In the context of an occupational disease, environmental factors are those encountered in the workplace and include exposure to various types of contaminants, physical stress and factors related to workplace organization (Becklake et al. 2006). A determinant has been defined as “any physical, biological, social, cultural or behavioural factor that can influence the study outcome” (e.g. work-related asthma) (Last 1995).
Occupational exposures to airborne particulates, gases and vapours are measured to assess exposure–response relationships. Such relationships are useful to (1) determine a link of causality between suspected exposure and the disease, in this context, work-related asthma, and (2) provide objective evidence to control exposure levels in the workplace.
Epidemiological studies of OA may be conducted with different objectives in mind, using different designs and in different populations, and the definition of OA may differ accordingly (Becklake et al. 2006). Because the definition does not conform to the clinical definition, terms such as “asthma-like” and “probable OA” have been used (Manfreda et al. 1993; Gautrin et al. 2001a).
Study approaches and design in the context of investigations of OA have been described and discussed in terms of strengths and weaknesses by Becklake et al. (2006). These designs include randomized control trials, longitudinal (cohort) studies, case-control (case-referent) studies, cross-sectional (prevalence) studies and clinical case reports. The selection of the most appropriate design should be based on the purpose of answering a study question as discussed by McDonald (1995). Other considerations in choosing a study design include more practical issues, such as the availability of a suitable population, appropriate instruments to measure the study outcome and exposure, and resources. Randomized clinical trials are usually not feasible in the context of the study of OA, except when the effect of a treatment on recovery from OA is examined (Malo et al. 1996). Cross-sectional studies have been widely used to determine the prevalence of OA (Gautrin et al. 2003; Mapp et al. 2005). This type of design is likely to provide underestimates of the rates of the disease due to survivor bias (caused by attrition from the workforce for health reasons) (Newman-Taylor and Venables 1984; Becklake et al. 2006). Prospective cohort studies are used to estimate the incidence and determinants of work-related asthma; this approach has been used, for example, in cohorts of apprentices entering a program in which they are exposed to known sensitizers (De Zotti and Bovenzi 2000; Gautrin et al. 2000, 2001a; Archambault et al. 2001; Rodier et al. 2003; El-Zein et al. 2003; Walusiak et al. 2004), in specific workforces (Brisman et al. 2004) and among members of a health maintenance organization (Vollmer et al. 2005). Case-control (retrospective) studies are designed to examine the role of environmental (exposure) and host risk factors; nested case-control analysis within a cohort offers the advantage that cases can be compared with controls with similar exposure when host determinants, including genetic polymorphisms, are studied, or alternatively with controls with similar socio-cultural, economic and education backgrounds to study the effect of occupational exposure (Cullinan et al. 2001; Brisman et al. 2003).
Methodological issues of importance in epidemiological studies include measurement of outcomes and risk factors. As pointed out by Becklake et al. (2006), the tools used to measure health outcomes are similar to those used in the clinical setting; in a chapter of Asthma in the Workplace, the authors discuss the importance of using a standardized approach with all measuring instruments, including those used to assess symptoms, immunological status, lung function and bronchial responsiveness to “minimize differential across comparison groups” (Becklake et al. 2006). Similar precautions need to be taken for measurements of exposure.
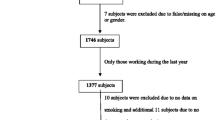
Depending on the objective of the epidemiological study, the size of the study population and the resources available, the methods used for case identification may be more or less exhaustive. Questionnaires have been used as the only method of assessment for a number of workforce-based or community-based studies to assess the prevalence of work-related asthma; however, questionnaires are very sensitive and poorly specific. For example, in a workforce-based study of workers exposed to guar gum in the carpet industry, 23/162 had symptoms suggestive of OA, but only two had a confirmed diagnosis of OA using specific challenge tests (Malo et al. 1990), considered the gold standard for the diagnosis of OA (Vandenplas et al. 2006). An algorithm has been proposed for the investigation of OA in epidemiological studies including the following measures (1) questionnaire, (2) skin prick tests and/or immunological testing with the suspected specific etiologic agent, when feasible, (3) assessment of non-specific bronchial responsiveness, (4) serial peak flow monitoring and/or specific inhalation tests (Chan-Yeung and Malo 1995). When participants in an epidemiological study take part in an investigation beyond a questionnaire, one or more of the above mentioned measures are added. Toelle et al. suggested that in epidemiological studies, ascertainment of asthma and of OA should be based on a questionnaire and confirmed bronchial hyper-responsiveness using challenge tests to non-specific pharmacological agents (Toelle et al. 1992) that have been used safely for field studies (Troyanov et al. 2000). In prospective studies conducted in apprentices exposed to high-molecular-weight allergens, the diagnosis of “probable OA” was based on immunological evidence and objective testing for bronchial responsiveness (Gautrin et al. 2001a; Archambault et al. 2001) on the assumption that 80% of subjects with skin reactivity to a specific allergen and confirmed bronchial hyper-responsiveness would react to a specific challenge test with the appropriate inhalant (Cockcroft et al. 1987).
Frequency and Determinants
The frequency of asthma in the workplace can be assessed by several means. Surveys in the general population propose figures that are higher (5% up to one-third of all asthmatic subjects) than those obtained from sentinel projects where potential cases are reported by physicians and medicolegal statistics, especially for countries that accept cases based on diagnostic confirmation through objective evidence (10–15 cases/million workers in Quebec).
Prevalence
The prevalence of work-related respiratory symptoms suggestive of OA and of OA has been investigated in several different workplace surveys and among workers in the same occupational groups, e.g. laboratory-animal facilities, large bakeries, snow-crab and other seafood processing plants, food processing plants, farms, silk works, latex-glove manufacturing plants, carpet manufacturing plants, the pharmaceutical industry, plastic and varnish production plants and/or utilization, spray-painting, hairdressing, production of resins, sawmill, welding, textile (dyes), hospitals, greenhouses, etc. (Becklake et al. 2006). These results are helpful in providing information about the scope of the problem in high-risk workplaces, although they are potentially prone to survivor bias. The well-known survivor effect (selection “out”) is probably the most important bias affecting prevalence estimates from cross-sectional surveys in individual workplaces. Observed differences in the prevalence of OA due to the same agent may be accounted for, at least in part, by particular conditions at a given site, such as exposure to other asthmagenic agents or respiratory irritants. Large discrepancies in the prevalence of work-related symptoms and OA between workforces exposed to different agents of low molecular weight (e.g. isocyanates) or high molecular weight (e.g. flour, laboratory animals) have been reported. One might question whether these are entirely attributable to the agents themselves or to other circumstances, for instance, ascertainment of cases of OA, country, differential effect of other factors such as work practice, and potential identified/non-identified biases. An additional source of controversy in the ascertainment of OA is that it can be defined as either new-onset asthma or WAA (Toren et al. 2000).
Prevalence studies in workforce-based studies remain useful for the evaluation of interventions to control exposure to a specific contaminant, as was the case for enzyme detergents. Prevalence rates of respiratory symptoms and skin reactivity have successively decreased from 50% in the 1960s (Mitchell and Gandevia 1971) but rose again in the late 1990s (Cullinan et al. 2000; Vanhanen et al. 2000); these variations have led researchers to identify various causes that were followed by changes in formulation processes.
Incidence
A few prospective cohort studies have been designed in selected high-risk professions to assess the incidence and determinants of probable OA among apprentices newly exposed to high-molecular-weight agents (De Zotti and Bovenzi 2000; Gautrin et al. 2001a, b, 2002; Archambault et al. 2001; Brisman et al. 2003; Walusiak et al. 2004), and low-molecular-weight sensitizers (El-Zein et al. 2003; 2005). A summary of key features of the prospective studies carried out in apprentices by Gautrin and coworkers is presented in Table 18.2. The cumulative incidence of probable OA (work-related new chest symptoms and increase in bronchial hyper-responsiveness) over an average period of 15 months of intermittent exposure to welding fumes while training to become a welder was 13.8% (32/232) (El-Zein et al. 2003). In comparison, the incidence of the outcome (new work-related chest symptoms) in bakers’ studies varied between 12% (Brisman et al. 2004) and 4.2% (Cullinan et al. 2001), which appeared to be somewhat lower.
Estimates of the incidence of OA have mainly been made using National and Regional Disease Registers, Surveillance Systems and medico-legal statistics, although these systems were not primarily intended for that purpose. The Sentinel Event Notification System for Occupational Risk (SENSOR) was introduced in several states in the United States in the 1980s, based on mandatory or voluntary reporting of work-related diseases (Matte et al. 1990). This system was mainly developed to identify and investigate workplaces at risk and implement interventions. In the United Kingdom, two voluntary reporting schemes have been set up since 1989. The Surveillance of Work-related and Occupational Respiratory Diseases (SWORD) is based on voluntary reporting from selected specialists in occupational or respiratory medicine in the country (McDonald et al. 2005). The other system, a Surveillance Scheme of OA in the West Midlands Region, was designed to study the incidence of OA in this specific area (Gannon and Burge 1993). Recent figures from SWORD show stabilization and even a reduction in the number of new cases of OA (McDonald et al. 2005). Similar surveillance systems have been initiated in the Canadian provinces of Quebec (Provencher et al. 1997) and British Columbia (Contreras et al. 1994), in France (Ameille et al. 2003) and in South Africa (Hnizdo et al. 2001). Other sources used to derive estimates of the incidence of OA include Medico-legal Statistics in the province of Quebec (Lagier et al. 1990) and in Finland (FROD) (Reijula et al. 1996), as well as self-reporting systems as in Sweden (Toren 1996). There are large differences between countries in the estimates of incidence of OA derived from these sources, ranging from 20 per million per year in the United Kingdom to 187 per million per year in Finland, as illustrated and discussed by Becklake et al. (Becklake et al. 2006). These differences may be attributed to methodological differences (in case ascertainment and classification of job), the type of industries, as well as differences in reporting. Within a country, differences in time are useful to indicate trends in incidence rates overall and for specific causal agents (such as isocyanates or latex). Despite some weaknesses of these schemes for obtaining valid estimates of the incidence of OA, they have been successfully used to derive information on the distribution of the disease by occupational categories and the frequency of afflicted workers by agent.
Adult-Onset Asthma Attributable to Work Exposures: Population Attributable Risk (PAR%)
Since the 1990s, there has been increased interest in the proportion of adult-onset asthma that could be attributable to work exposure. Blanc and Toren (1999), in a review of studies that used different epidemiological designs, arrived at a median estimate of 9% of attributable risk of asthma to work exposure, and 15% when only high-quality studies were considered. Estimates of PAR% have been derived from community-based surveys and population-based incidence studies. In community-based studies in large populations (more than 1,000 and up to several thousand) of male and female adults in countries around the world (Europe, Canada, the United States, New Zealand and Singapore), consistent associations were found between wheezing complaints or asthma diagnosed by a physician, and those being exposed at work to non-specific agents or to dust alone or to dust with fumes and/or gases (irritants). Becklake et al. (2006) reviewed selected studies in which the PAR% ranged from 3% in studies from Spain (Kogevinas et al. 1996) and New Zealand (Fishwick et al. 1997), to 23% in Canada (Becklake et al. 1996) and 33% in Singapore (Ng et al. 1994). Becklake et al. (2006) also discussed the strength of these studies, which involve not only the population of workers currently exposed, but also all those who have ever been exposed in workplaces at risk, thus reducing survivor effects.
A population-based incidence study included the entire employed Finnish population. The cohort was followed for 10 years, using two registers, one of clinically established persistent asthma, the other of census data (for information on employment) (Karjalainen et al. 2001). A total of 49,575 incident cases of asthma were recorded, and the fraction attributable to work was 29% for males and 17% for females. The proportion attributable to work according to the Finnish Register of Occupational Diseases was ∼5% (Reijula et al. 1996). As discussed earlier (Gautrin et al. 2003), this discrepancy in the PAR% figures between the two sources of data may be due to failure to recognize association with work exposure, or physicians’ failure to submit workers for evaluation. The Finnish study also found excess risk of asthma in workplaces associated with exposure to irritants such as dust, welding and soldering fumes, disinfectants, traffic, exhaust combustion and cold air (Karjalainen et al. 2002). Other community-based studies have found increased risks of asthma in jobs associated with irritant exposures but not habitually with OA, for example among construction and textile workers (Ng et al. 1994), cleaners (Kogevinas et al. 1999; Karjalainen et al. 2000), shoemakers, metal-plating workers and electrical machinery workers (Arif et al. 2002).
Exposure–Response Relationships
In cohort studies investigating the incidence and determinants of OA, time spent in contact with the responsible agent has been used as a surrogate of exposure when objective measurements were not available. In a cohort of apprentices exposed to laboratory animals, a dose–response relationship was shown between the number of hours of contact with rodents in the laboratory and the incidence of specific skin reactivity to rodent urinary proteins independently of host factors (atopy, pre-exposure respiratory symptoms during the pollen season); the risk was 2.5 times greater in subjects exposed to the longest compared to the shortest of three duration categories (Gautrin et al. 2000). Prospective studies of laboratory-animal workers (Cullinan et al. 1999), flour mill and bakery workers (Cullinan et al. 2001) and acid anhydride workers (Barker et al. 1998) performed in the United Kingdom were reviewed by Newman-Taylor (Newman Taylor 2002). They all showed evidence of exposure–response relationships between direct measures of exposure and the risk of developing work-related chest symptoms. Another study using a case-control design found an exposure–response relationship between measurements of isocyanate and OA (McDonald et al. 2000). As noted earlier, such studies provide strong evidence for developing preventive strategies (Gautrin et al. 2003) for agents that are responsible for a substantial number of cases of OA.
Sociopsychological Impacts
Not only is OA a multifactorial lung disease that is associated with significant health impacts, but it also has important personal, financial and sociopsychological impacts.
Quality of Life Impacts
Once a diagnosis of OA has been confirmed and patients’ are removed from the workplace, this does not guarantee a swift recovery. In fact, respiratory symptoms may persist for years, even following cessation of exposure (Becklake et al. 2006). It has been estimated that as many as 70% of patients experience persistent symptoms and nonspecific airway hyper-responsiveness, and the majority of patients who develop OA with or without a latency period do not recover. It is therefore not surprising that patients with OA may suffer a significantly reduced quality of life following diagnosis. A study by Malo and coworkers found that patients with OA with a latency period report having significantly reduced quality of life in at least four life domains (activity limitations, asthma symptoms, management of environmental triggers, and emotional distress) 2 years after cessation of exposure (Malo et al. 1993). The impact was, however, mild, and this can be explained by the fact that only 8% of them were still unemployed at the time of the study. Moreover, this study found that patients with OA suffered from worse asthma-related quality of life than non-OA patients matched for disease severity. This suggests that the quality of life impacts of OA may exceed those of ‘traditional’ asthma, and highlights the magnitude of this diagnosis’ impact on functional status (Al-Otaibi et al. 2005).
Psychological Impacts
The idea that asthma may be related to psychological factors is not new. Negative emotions have long been considered important asthma triggers, with references to asthma as being “passion-induced” and related to mood dating back as far as 200 BC (Gregerson 2003). By the late nineteenth and early twentieth centuries, Sir William Osler viewed asthma as a “neurotic affection” in which imbalances of the nervous system and emotional factors played a fundamental role (Osler 1892). Since then, a growing number of studies have provided evidence of a link between various psychosocial factors and asthma (Gregerson 2003). Data from both clinical and community settings suggest that psychiatric disorders, and mood and anxiety disorders in particular, are disproportionately more prevalent among asthmatics relative to the general population. Point prevalence rates of anxiety disorders (e.g., panic disorder, generalized anxiety disorder, and social phobia) and mood disorders (e.g., major and minor depressive disorder) are especially high among asthmatics, ranging from 16–52% for anxiety disorders(Goodwin et al. 2003; Naciemento et al. 2002; Perna et al. 1997) and 14–41% for mood disorders (Goodwin et al. 2003; Naciemento et al. 2002; Perna et al. 1997; Goldney et al. 2003; Netjeck et al. 2001). A recent study by Lavoie and coworkers including over 500 asthma outpatients indicated that 31% of asthmatics meet criteria for one or more current mood (20%) or anxiety (23%) disorders (Lavoie et al. 2006). Rates of certain disorders (i.e., panic disorder and major depressive disorder) are as much as six times more prevalent among asthmatics relative to the general population. However, the extent to which patients with OA suffer as much (if not more) psychiatric comorbidity at the time they are still exposed at work and are affected with asthmatic symptoms is not yet known, and future studies are needed to assess this.
Not only is psychological stress common in asthmatic subjects, but there is a vast literature linking symptoms of psychological stress to increased asthma morbidity. For example, symptoms of anxiety and depression have been associated with increased asthma severity, increased use of emergency services, increased symptom reporting, poorer pulmonary function, lengthier hospital stays, and increased use of reliever medication (Rimington et al. 2001; Janson et al. 1994; Kaptein 1982; Kolbe et al. 1996).To date, relatively few studies have evaluated associations between actual psychiatric disorders (which imply experiencing psychological stress at a level that is clinically significant and impairs daily functioning) and asthma morbidity. However, the few studies conducted have yielded similar results. For example, one study found associations between major depressive disorder (assessed using the Primary Care Evaluation for Mental Disorders, PRIME-MD) and worse nocturnal asthma symptoms, worse waking asthma symptoms, and worse asthma-related quality of life (Goldney et al. 2003). A related study found that asthmatics identified as having a psychiatric disorder (according to the Structured Clinical Interview for DSM-III-R) were more likely to have poorly controlled asthma, demonstrate worse medication adherence, and have greater drop-out rates from asthma management programs relative to patients without a psychiatric disorder (Kolbe et al. 1996). A study by Lavoie and coworkers also found evidence of an association between psychiatric disorders and greater asthma morbidity (Lavoie et al. 2005). Collectively, these studies indicate a strong association between both psychological stress and psychiatric disorders and increased asthma morbidity.
Despite strong associations between psychiatric disorders, high levels of psychological stress, and asthma morbidity, these associations remain unexplored in patients with OA. When one also considers the scope of the burden associated with non-OA and applies those potential impacts to patients who were for years disease-free, an additional psychological burden associated with OA that surpasses that of non-OA can be hypothesized. High job-specific stress is common and associated with worse health outcomes in patients with several chronic illnesses (e.g., hypertension and cardiovascular disease). For example, perceived job stress (defined as severity and frequency of stressful job tasks), job strain (defined as high job demands and low decision latitude), job insecurity, and threat of unemployment have been associated with increased risk of cardiovascular disease (Kang et al. 2005), incident hypertension (Markovitz et al. 2004; Levenstein et al. 2001), and non-fatal myocardial infarction (Lee et al. 2004).
We are aware of only one study to date to specifically assess levels of psychological stress in patients with OA after removal from exposure (Yacoub et al. submitted). In this study, psychological distress levels were assessed using two self-report instruments: the Psychiatric Symptom Index (PSI) (Illfeld 1976) and Millon Clinical Multiaxial Inventory (MCMI) (Millon 1994) in 40 workers with OA 2 years after cessation of exposure. This study found that levels of anxiety, depression, and cognitive dysfunction were all in the clinical range according to the PSI, suggesting that not only are the psychological consequences of OA significant but they may affect a range of psychological factors. It is noteworthy that psychological distress levels were measured at least 2 years after workers received their diagnosis and after they had been removed from the workplace, suggesting that psychological distress in these patients may persist beyond receiving the diagnosis and beyond withdrawal from the workplace. Certain psychiatric disorders were also found to be common in this sample, with anxiety disorders and dysthymia (a chronic form of depression) affecting approximately 35% and 22.5% of patients, respectively. Though preliminary and in need of replication, these results suggest that patients with OA are anxious and many are chronically depressed, a finding that is consistent with previous studies in subjects with non-OA (Goodwin et al. 2003; Lavoie et al. 2005). However, it is noteworthy that rates of anxiety disorders and dysthymia in Yacoub et al.’s study were much higher than those observed in previous studies with non-occupational asthmatics (e.g., 35% vs. 23%)(Yacoub et al. submitted), which suggests that the psychological consequences (like quality of life impacts) of OA, may exceed those of non-OA.
Social and Financial Costs
General Considerations
Asthma is a common medical condition and a frequent cause of work disability. Unlike many chronic medical conditions that primarily affect older persons, asthma disproportionately affects those of working age. Because it is prevalent during ages of peak participation in the workforce and because its impact can be severe, asthma is one of the leading medical conditions associated with work limitations and work loss. A study done between 1983 and 1985 showed that 326,000 adults in the United States between the ages of 18 and 44 were limited in their ability to work by asthma (Laplante 1988). This represents approximately 10% of all persons with asthma in this age group (Ries 1986). Indeed, 21% of asthmatic subjects complain of worsening of their asthma when they are at work (Saarinen et al. 2003). The estimated asthma-related cost of lost work days for persons 18 years and older in the workforce is $284.7 million per annum alone (Weiss et al. 1992). Costs can be estimated using PAR estimates (Leigh et al. 2002). Leigh et al. used a PAR of 15% for both asthma and COPD to calculate costs, with the human capital method that breaks down costs into direct categories, such as medical expenses, as well as indirect categories, such as lost earnings and lost home production. The 15% PARs result in costs of $1.6 billion for asthma, 74% direct and 26% indirect. These estimates are conservative, since costs associated with pain and suffering as well as the value of care rendered by family members were not included.
Concerning risk factors for work disability among adults with asthma, in a cross-sectional survey of 698 registered patients of pulmonary and allergy internal medicine subspecialists, Blanc et al. (1996) showed that the severity of asthma score predicted both complete disability (odds ratio –OR-, 7.9; 95% CI, 4.2–15 per 10-point increment) and partial disability (OR 2.6; 95% CI, 1.6–4.2), and taking illness severity into account, job conditions, occupation, and work exertion carried a combined disability OR of 3.9 (95% CI, 1.7–8.6). Blanc et al. (1996) concluded that work disability is common among adults with asthma receiving specialist care. Severity of disease is a powerful predictor, but not the sole predictor of disability in this group. Working conditions, including job-related exposures, are associated with added disability risk even after taking illness severity into account.
Social Impact
Occupational Asthma with a Latency Period
From an international perspective, although OA is a condition that is under the jurisdiction of medico-legal authorities, in most countries, examination of cases is often unsatisfactory and takes time. The protection offered to workers is generally inadequate. Affected workers frequently continue to be exposed or encounter serious socio-economic losses (Gannon et al. 1993; Ameille and Descatha 2005; Larbanois et al. 2002). Although a study published on the outcome of workers who stayed at the same job with pharmacologic treatment after a diagnosis of OA found no significant differences in any of the morbidity outcomes (FEV1, PD20, PEF variability, use of rescue salbutamol, respiratory symptom score) as compared to baseline or run-in values after 3 years of follow up in 20 workers (Marabini et al. 2003), this study has many limitations: small number of subjects and lack of power of the analysis, uncontrolled study, and selection of workers who had mild-to-moderate and not moderate to severe persistent asthma. Although none of the subjects deteriorated, none recovered from asthma even if they wore respiratory protection at work. Therefore, there is a consensus that workers with OA should not remain in the same job after diagnosis.
OA with a latency period generally affects young workers. This is different from standard pneumoconiosis such as silicosis and asbestosis, in which a very long latency period is generally the rule and compensation agencies deal with older workers. For OA, workers generally get sensitized in the first few years after starting exposure, even more generally so in the case of high-molecular-weight proteinaceous agents (Malo et al. 1992). It is therefore mandatory to offer rehabilitation programs adapted to these young workers. Rather than offering a lump sum, emphasis should be put on retraining these workers in a new job in which they will no longer be exposed to the agent causing OA. Although most workers with OA will still have asthma even after stopping exposure, asthma is generally mild and most workers are able to carry on almost any type of work. If the emphasis is put on adequate 1–2-year rehabilitation programs (this is generally long enough to retrain young workers into a new job) with financial compensation, very few workers are unable to find another job. In a study of 134 workers carried out in Quebec 2 years after cessation of exposure, only 8% were still unemployed (Dewitte et al. 1994). Moreover, workers generally report a satisfactory quality of life (see above).
Irritant-Induced Asthma
There is little published information about the socio-economic consequences of RADS, time lost from work, and the outcome. Some authors have reported a worse prognosis in workers exposed to spills without prior history of disease (Gautrin et al. 2006b). It is also relevant to distinguish work-exacerbated asthma (with a history of previous asthma) from irritant-induced asthma. Workers with the latter condition have more prolonged symptoms after exposure and seem less likely to have returned to the same work environment in comparison with workers with work-exacerbated asthma (Chatkin et al. 1999; Tarlo et al. 1995). In a descriptive epidemiological study of work-related cases of RADS, Henneberger et al. found more information on the outcome of these workers (Henneberger et al. 1993). In that study, cases of work-related asthma were identified in four states in the United States during 1993–1995 as part of the Sentinel Event Notification Systems for Occupational Risks (SENSOR) program. Information gathered by follow-back interview was used to describe 123 work-related RADS cases and compare them to 301 other work-related asthma cases in which the onset of disease was associated with a known asthma inducer. RADS represented 14% of all new-onset work-related cases identified by the state SENSOR surveillance systems. RADS cases had significant adverse medical and occupational outcomes identified by follow-back interview. In particular, 89% still had breathing problems, 78% had sought emergency care and 39% had been hospitalized for work-related breathing problems; 54% had applied for worker compensation benefits; and 41% had left the company where they experienced onset of asthma. These values were equal to or higher than the comparable figures for those work-related OA cases in which onset was attributed to a known inducer. The authors concluded that RADS cases represent a minority of all work-related asthma cases, but the adverse health impact of this condition appears to equal that of cases of OA with a latency period, a conclusion also reached in a study carried out by Malo and coworkers (Malo et al. 1994).
Work-Aggravated Asthma
Despite its immense medical and societal importance, very little is known about the importance of asthma-related work disability and the prognosis of these workers compared to workers with true OA. Two recent studies explored this topic. Larbanois et al. investigated the socio-economic outcomes of subjects who experienced WAA symptoms in the absence of demonstrable OA and compared these outcomes with those of subjects with documented OA (Larbanois et al. 2002). Subjects (n = 157) who were being investigated for work-related asthma were surveyed. Of these, 86 had OA, ascertained by a positive specific inhalation challenge (SIC), and 71 had a negative SIC response. After a median interval of 43 months (range 12–85 months), the subjects were interviewed to collect information on employment status, income changes, and asthma-related work disability. Rates of work disruption and income loss at follow-up were similar in subjects with negative SIC (46% and 59% respectively) and in those with OA (38% and 62%). The median loss as a percentage of initial income was 23% in subjects with negative SIC and 22% in subjects with OA. Asthma-related work disability, defined as any job change or work loss due to asthma, was slightly more common in subjects with OA (72%) than in those with negative SIC (54%). More recently, Lemière et al. (2006b) conducted a cross-sectional study in subjects previously investigated for work-related asthma within 1–4 years of their original diagnosis of OA or WAA. Subjects were considered to have OA if they showed a positive specific inhalation challenge to an occupational agent, whereas subjects were considered as having WAA if they reported a worsening of their asthma symptoms when at work but showed a negative specific inhalation challenge to occupational agents. Clinical, functional, inflammatory and occupational characteristics were reassessed in both classes of subjects. Eighteen subjects with OA and 10 with WAA were assessed. All subjects with OA had to change their work environment, except one worker who had developed OA due to exposure to an occupational sensitizer used by a colleague working next to him. No subjects with WAA remained in the same workplace post-diagnosis. These two studies therefore show that, even in the absence of demonstrable OA, work-related asthma symptoms are associated with considerable socio-economic consequences.
Costs
Compensation
In the context of OA, provisions for temporary and permanent disability should be applied (see above) (Bersntein et al. 2006). These result in significant costs. Once the diagnosis is confirmed, the subject should be considered 100% impaired on a permanent basis in terms of the job that caused the illness, as well as other jobs entailing exposure to the same causative agent. It is important for subjects with OA with a latency period to no longer be exposed to the causal agent, as further exposure will increase the risk of deterioration of asthma (Côté et al. 1990; Moscato et al. 1999). In subjects with OA with a latency period, the threshold level of exposure for developing symptoms, airway obstruction and/or hyper-responsiveness is very much lower than that required for “sensitization.” Subjects may react to a minute amount of the causative agent, which precludes any further exposure to the product. Financial compensation should be offered in every instance where there is a loss of earning power. Workers should be re-assessed 2 years after leaving exposure for permanent disability/impairment (see above). Compensation is not the same in all countries; most compensation systems are administered by national agencies (Dewitte et al. 1994; Bersntein et al. 2006). However, in the United States, disputes are usually settled through litigation in an adversarial setting. Evidence from witnesses is presented. Once a claim is accepted, complete medical care is provided and medical expenses are paid either by the privately insured employer or by the state compensation fund for workers who qualify under various programs (Bersntein et al. 2006). In most U.S. states, workers’ compensation wage replacement equals two-thirds of workers’ pre-disability wages, up to a maximum determined from the statewide average weekly wage for the duration of disability.
In Quebec, it has been estimated that a case of OA with a latency period accepted by the provincial medico-legal agency costs an average of $50,000 CAN in the late 1980s (Dewitte et al. 1994). There was an increase to $75,000 CAN since, with a plateau thereafter (Table 18.3). Approximately 80% of that sum is allocated as temporary indemnities insuring a full salary for the period of 1–2 years required for finding a new job with or without retraining. The rest is allocated for permanent disability indemnities.
Surveillance Program in High-Risk Workplaces
A consensus statement in 1995 suggested that “routine surveillance be performed in all workers with exposure to agents known to cause asthma and especially if cases of work-related asthma have occurred at a particular worksite” (Chan-Yeung 1995). Surveillance decisions in occupational settings must often be made without evidence of relative benefits and costs. A surveillance program with workers exposed to diisocyanates in Ontario coupled an industrial hygiene approach, by which levels of exposure were reduced, and a medical surveillance. Although this has resulted in a reduction of cases after a few years, it is not known if these gains were principally due to the industrial hygiene program or the medical surveillance, or both (Tarlo et al. 1997a), (b) in a period during which cases of OA due to diisocyanates diminished worldwide, even in countries where no surveillance programs were applied.
Using the example of diisocyanate-induced OA, the most common type of OA with a latency period, Wild et al. recently published a model-based approach to evaluate the costs and benefits of surveillance from the perspectives of both employers and society (Wild et al. 2005). The authors used a mathematical simulation model of diisocyanate-induced OA to compare annual surveillance to passive case finding. Outcome measures included symptom-free days, quality adjusted life years (QALY), direct costs, productivity losses, and incremental cost effectiveness ratio (CER), measured from both perspectives. For 100,000 exposed workers, surveillance resulted in 683 fewer cases of disability over 10 years. Surveillance conferred benefits at an incremental cost of $24,000/QALY (employer perspective; $13.33/SFD) and was a cost saving from the societal perspective. Baseline results placed the CER for surveillance for diisocyanate-induced OA within the acceptable range. Costs from the societal and employer perspectives differed substantially, with a more attractive CER from the societal perspective, suggesting opportunities for employer/societal cost-sharing.
Conclusion
Asthma in the workplace can have important health and socio-economic consequences (Vandenplas et al. 2003). As regards health issues, workers should be investigated by objective means, not by questionnaires alone. If the workplace is shown to be the cause of the asthma (referred to as “occupational asthma with a latency period,” see above), workers should ideally be removed from exposure, as this always has a beneficial effect, including complete cure from asthma, whereas continuing exposure leads to worsened asthma. As regards socio-economic impact, workers with asthma caused by the workplace should be offered satisfactory rehabilitation programs so as to minimize impairment/disability. If there is no cure for the asthma as a result of cessation of exposure, compensation should be offered.
References
Al-Otaibi S, Tarlo SM, House R (2005) Quality of life in patients with latex allergy. Occup Med 55:88–92
Ameille J, Descatha A (2005) Outcome of occupational asthma. Curr Opin Allergy Clin Immunol 5:125–128
Ameille J, Pauli G, Calastreng-Crinquand A, Vervloët D, Iwatsubo Y, Popin E, Bayeux-Dunglas MC, Kofperschmitt-Kubler MC (2003) ONAP and the corresponding members of the. Reported incidence of occupational asthma in France, 1996–99. Occup Environ Med 60:136–142
American Medical Association (2001) In: Cocchiarella L, Andersson GBJ (eds) Guides to the evaluation of permanent impairment, 5th edn. American Medical Association, Chicago, IL
American Thoracic Society (1993) Guidelines for the evaluation of impairment/disability in patients with asthma. Am Rev Respir Dis 147:1056–1061
Archambault S, Malo JL, Infante-Rivard C, Ghezzo H, Gautrin D (2001) Incidence of sensitization, symptoms and probable occupational rhinoconjunctivitis and asthma in apprentices starting exposure to latex. J Allergy Clin Immunol 107:921–923
Arif AA, Whitehead LW, Delclos GL, Tortolero SR, Lee ES (2002) Prevalence and risk factors of work related asthma by industry among United States workers: data from the third national health and nutrition examination survey (1988–94). Occup Environ Med 59:505–11
Axon EJ, Beach JR, Burge PS (1995) A comparison of some of the characteristics of patients with occupational and non-occupational asthma. Occup Med 45:109–111
Barker RD, van Tongeren MJ, Harris JM, Gardiner K, Venables KM, Newman Taylor AJ (1998) Risk factors for sensitisation and respiratory symptoms among workers exposed to acid anhydrides: a cohort study. Occup Environ Med 55:684–691
Becklake M, Ernst P, Chan-Yeung M, Manfreda J, Dimich-Ward H, Sears M, Siersted H (1996) The burden of asthma attributable to work exposures in Canada. Am J Respir Crit Care Med 153:A433
Becklake MR, Chan-Yeung M, Malo JL (2006) Epidemiological approaches in occupational asthma. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the workplace, 3rd edn. Taylor & Francis, New York, 37–85
Bernstein JA (2002) Material safety data sheets: are they reliable in identifying human hazards? J Allergy Clin Immunol 110:35–8
Bernstein IL, Chan-Yeuno M, Malo JL, Merget R, Bernstein OI eds (2006) Metals. In: Asthma in the workplace, 3rd edn. Taylor & Francis, New York, pp 525–554
Bernstein IL, Chan-Yeung M, Malo JL, Berstein DI (2006) Asthma in the workplace, 3rd edn. Taylor & Francis, New York
Bersntein IL, Keskinen H, Blanc PD, Chan-Yeung M, Malo JL (2006) Medicolegal aspects, compensation aspects, and evaluation of impairment/disability. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the Workplace, 3rd edn. Taylor & Francis, New York, pp 319–351
Blanc PD, Toren K (1999) How much asthma can be attributed to occupational factors? Am J Med 107:580–587
Blanc PD, Cisternas M, Smith S, Yelin EH (1996) Asthma, employment status, and disability among adults treated by pulmonary and allergy specialists. Chest 109:688–696
Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID (1999) Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med 160:406–410
Brisman J, Lillienberg L, Belin L, Ahman M, Jarvholm B (2003) Sensitization to occupational allergens in bakers’ asthma and rhinitis: a case-referent study. Int Arch Occup Environ Health 76:167–170
Brisman J, Nieuwenhuijsen MJ, Venables KM (2004) Exposure–response relations for work related respiratory symptoms and sensitisation in a cohort exposed to alpha-amylase. Occup Environ Med 61:551–553
Brooks SM, Weiss MA, Bernstein IL (1985) Reactive airways dysfunction syndrome (RADS); persistent asthma syndrome after high level irritant exposures. Chest 88:376–84
Chan-Yeung M (1995) Assessment of asthma in the workplace. Chest 108:1084–1117
Chan-Yeung M, Malo JL (1995) Occupational asthma. N Engl J Med 333:107–112
Chan-Yeung M, Bernstein IL, Essen Von S, Singh J, Schwartz DA (2006) Acute airway diseases due to organic dust exposure. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the workplace, 3rd edn. Taylor & Francis, New York, pp 641–682
Chatkin CJM, Tarlo SM, Liss G, Banks D, Broder I (1999) The outcome of asthma related to workplace exposures. Chest 116:1780–1785
Cockcroft DW, Murdock KY, Kirby J, Hargreave F (1987) Prediction of airway responsiveness to allergen from skin sensitivity to allergen and airway responsiveness to histamine. Am Rev Respir Dis 135:264–7
Contreras GR, Rousseau R, Chan-Yeung M (1994) Occupational respiratory diseases in British Columbia, Canada in 1991. Occup Env Med 51:710–712
Côté J, Kennedy S, Chan-Yeung M (1990) Outcome of patients with cedar asthma with continuous exposure. Am Rev Respir Dis 141:373–6
Cullinan P, Cook A, Gordon S, Nieuwenhuijsen MJ, Tee RD, Venables KM, McDonald JC, Newman Taylor AJ (1999) Allergen exposure, atopy and smoking as determinants of allergy to rats in a cohort of laboratory employees. Eur Respir J 13:1139–1143
Cullinan P, Taylor AJ, Taylor Newman AJ, Hole AM, Jones M, Barnes F, Jolliffe G (2000) An outbreak of asthma in a modern detergent factory. Lancet 356:1899–1900
Cullinan P, Cook A, Nieuwenhuijsen MJ, Sandiford C, Tee RD, Venables KM, McDonald JC, Taylor Newman AJ (2001) Allergen and dust exposure as determinants of work-related symptoms and sensitization in a cohort of flour-exposed workers; a case-control analysis. Ann occup hyg 45:97–103
Das R, Blanc PD (1993) Chlorine gas exposure and the lung: a review. Toxicol Ind Health 9:439–455
De Zotti R, Bovenzi M (2000) Prospective study of work related respiratory symptoms in trainee bakers. Occup Environ Med 57:58–61
Demnati R, Fraser R, Ghezzo H, Martin JG, Plaa G, Malo JL (1998a) Time-course of functional and pathological changes after a single high acute inhalation of chlorine in rats. Eur Respir J 11:922–928
Demnati R, Fraser R, Martin JG, Plaa G, Malo JL (1998b) Effects of dexamethasone on functional and pathological changes in rat bronchi caused by high acute exposure to chlorine. Toxicol Sci 45:242–246
Desjardins A, Bergeron JP, Ghezzo H, Cartier A, Malo JL (1994) Aluminium potroom asthma confirmed by monitoring of forced expiratory volume in one second. Am J Respir Crit Care Med 150:1714–1717
Dewitte JD, Chan-Yeung M, Malo JL (1994) Medicolegal and compensation aspects of occupational asthma. Eur Respir J 7:969–980
El-Zein M, Malo JL, Infante-Rivard C, Gautrin D (2003) Incidence of probable occupational asthma and of changes in airway calibre and responsiveness in apprentice welders. Eur Respir J 22:513–518
El-Zein M, Infante-Rivard C, Malo JL, Gautrin D (2005) Is metal fume fever a determinant of welding related respiratory symptoms and/or increased bronchial responsiveness? A longitudinal study. Occup Environ Med 62:688–694
Fishwick D, Pearce N, D’Souza W, Lewis S, Town I, Armstrong R, Kogevinas M, Crane J (1997) Occupational asthma in New Zealanders: a population based study. Occup Environ Med 54:301–306
Gannon PF, Burge PS (1993) The SHIELD scheme in the West Midlands Region, United Kingdom. Midland Thoracic Society Research Group. Br J Ind Med 50(9):791–796
Gannon PFG, Weir DC, Robertson AS, Burge PS (1993) Health, employment, and financial outcomes in workers with occupational asthma. Br J Ind Med 50:491–496
Gautrin D, Boulet LP, Boutet M, Dugas M, Bhérer L, L’Archevêque J, Laviolette M, Côté J, Malo JL (1994) Is reactive airways dysfunction syndrome a variant of occupational asthma? J Allergy Clin Immunol 93:12–22
Gautrin D, Infante-Rivard C, Dao TV, Magnan-Larose M, Desjardins D, Malo JL (1997) Specific IgE-dependent sensitization, atopy and bronchial hyperresponsiveness in apprentices starting exposure to protein-derived agents. Am J Respir Crit Care Med 155:1841–1847
Gautrin D, Ghezzo H, Infante-Rivard C, Malo J-L (2000) Incidence and determinants of IgE-mediated sensitization in apprentices: a prospective study. Am J Respir Crit Care Med 162:1222–1228
Gautrin D, Infante-Rivard C, Ghezzo H, Malo JL (2001a) Incidence and host determinants of probable occupational asthma in apprentices exposed to laboratory animals. Am J Respir Crit Care Med 163:899–904
Gautrin D, Ghezzo H, Infante-Rivard C, Malo JL (2001b) Natural history of sensitization, symptoms and diseases in apprentices exposed to laboratory animals. Eur Respir J 17:904–908
Gautrin D, Ghezzo H, Infante-Rivard C, Malo JL (2002) Incidence and host determinants of work-related rhinoconjunctivitis in apprentice pastry-makers. Allergy 57:913–918
Gautrin D, Newman-Taylor AJ, Nordman H, Malo JL (2003) Controversies in epidemiology of occupational asthma. Eur Respir J 22:551–559
Gautrin D, Bernstein IL, Brooks SM, Henneberger PK (2006) Reactive airways dysfunction syndrome and irritant-induced asthma. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the Workplace, Taylor & Francis, New York, 581–629
Gautrin D, Bernstein IL, Brooks SM, Henneberger PK (2006) Reactive airways dysfunction syndrome and irritant-induced asthma. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the workplace, 3rd edn. Taylor & Francis, New York, pp 579–627
Gibson PG, Dolovich J, Denburg J, Ramsdale EH (1989) Chronic cough: Eosinophilic bronchitis without asthma. Lancet 1:1346–1348
Girard F, Chaboillez S, Cartier A, Côté J, Hargreave FE, Labrecque M, Malo JL, Tarlo S, Lemière C (2004) An effective strategy for diagnosing occupational asthma. Induced sputum. Am J Respir Crit Care Med 170:845–850
Goe SK, Henneberger PK, Reilly MJ, Rosenman KD, Schill DP, Valiante D, Flattery J, Harrison R, Reinisch F, Tompowsky C, Filios MS (2004) A descriptive study of work aggravated asthma. Occup Environ Med 61:512–517
Goldney RD, Ruffin R, Fisher LJ, Wilson DH (2003) Asthma symptoms associated with depression and lower quality of life: a population survey. Med J Aust 178:437–441
Goodwin RD, Jacobi F, Thefeld W (2003) Mental disorders and asthma in the community. Arch Gen Psychiatry 60:1125–1130
Gregerson MB (2003) The historical catalyst to cure asthma. In: Brown ES (ed) Asthma: social and psychological factors and psychosomatic syndromes. Basel, Karger, pp 16–41
Henneberger PK, Ferris Jr, BG, Sheehe PR (1993) Accidental gassing incidents and the pulmonary function of pulp mill workers. Am Rev Respir Dis 148:63–67
Henneberger PK, Derk SJ, Sama SR, Boylstein RJ, Hoffman CD, Preusse PA, Rosiello RA, Milton DK (2006) The frequency of workplace exacerbation among health maintenance organisation members with asthma. Occup Environ Med 63:551–557
Hnizdo E, Esterhuizen TM, Rees D, Lalloo UG (2001) Occupational asthma as identified by the Surveillance of Work-related and Occupational Respiratory Diseases programme in South Africa. Clin Exp Allergy 31:32–39
Illfeld FW (1976) Further validation of a psychiatric symptom index in a normal population. Psychol Rep 39:1215–1228
Janson C, Bjornsson E, Hetta J, Boman G (1994) Anxiety and depression in relation to respiratory symptoms and asthma. Am J Respir Crit Care Med 149:930–934
Johnson AR, Dimich-Ward HD, Manfreda J, Becklake MR, Ernst P, Sears MR, Bowie DM, Sweet L, Chan-Yeung M (2000) Occupational asthma in adults in six Canadian communities. Am J Respir Crit Care Med 162:2058–2062
Juniper EF, Buist AS, Cox FM, Ferrie PJ, King DR (1999) Validation of a standardized version of the asthma quality of life questionnaire. Chest 115:1265–1270
Kang MG, Koh SB, Cha BS, Park JK, Baik SK, Chang SJ (2005) Job stress and cardiovascular risk factors in male workers. Prev Med 40:583–588
Kaptein AA (1982) Psychological correlates of length of hospitalization and rehospitalization in patients with acute, severe asthma. Soc Sci Med 16:725–729
Karjalainen A, Kurppa K, Virtanen S, Keskinen H, Nordman H (2000) Incidence of occupational asthma by occupation and industry in Finland. Am J Ind Med 37:451–458
Karjalainen A, Kurppa K, Martikainen R, Klaukka T, Karjalainen J (2001) Work is related to a substantial portion of adult-onset asthma incidence in the Finnish population. Am J Resp Crit Care Med 164:565–568
Karjalainen A, Kurppa K, Martikainen R, Karjalainen J, Klaukka T (2002) Exploration of asthma risk by occupation-extended analysis of an incidence study of the Finnish population. Scand J Work Environ Health 28:49–57
Kogevinas M, Anto JM, Soriano JB, Tobias A, Burney P (1996) The risk of asthma attibutable to occupational exposures: A population-based study in Spain. Spanish Group of the European Asthma Study. Am J Respir Crit Care Med 154:137–143
Kogevinas M, Anto JM, Sunyer J, Tobias A, Kromhout H, Burney P (1999) Group and the European Community Respiratory Health Survey Study. Occupational asthma in Europe and other industrialised areas: a population-based study. Lancet 353:1750–1754
Kolbe J, Vamos M, Fergusson W, Elkind G, Garrette J (1996) Differential influences on asthma self-management knowledge and self-management behavior in acute severe asthma. Chest 110:1463–1468
Lagier F, Cartier A, Malo JL (1990) Statistiques médico-légales sur l’asthme professionnel au Québec de 1986 à 1988. Medico-legal statistics on occupational asthma in Quebec between 1986 and 1988. Rev Mal Respir 7:337–341
Laplante M (1988) Data on disability from the National Health Interview Survey 1883–1985. InfoUsed Report. US National Institute on Disability and Rehabilitation Research, Washington, DC
Larbanois A, Jamart J, Delwiche JP, Vandenplas O (2002) Socioeconomic outcome of subjects experiencing asthma symptoms at work. Eur Respir J 19:1107–1113
Last JM (1995) A dictionary of epidemiology, 3rd edn. Oxford University Press, Oxford, pp 1–180
Lavoie KL, Cartier A, Labrecque M, Bacon SL, Lemière C, Malo JL, Lacoste G, Barone S, Verrier P, Ditto B (2005) Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respir Med 99:1249–1257
Lavoie KL, Bacon SL, Cartier A, Barone S, Ditto B, Labrecque M (2006) What’s worse for asthma control and quality of life: depressive disorders, anxiety disorders, or both? Chest 130:1039–1047
Lee S, Colditz GA, Berkman LF, Kawashi I (2004) Prospective study of job insecurity and coronary heart disease in US women. Ann Epidemiol 14:24–30
Leigh JP, Romano PS, Schenker MB, Kreiss K (2002) Costs of occupational COPD and asthma. Chest 121:264–72
Lemière C, Hargreave FE (1999) Occupational eosinophilic bronchitis without asthma. Can J Allergy Clin Immunol 4:332–335
Lemière C, Malo JL, Boutet M (1997) Reactive airways dysfunction syndrome due to chlorine: sequential bronchial biopsies and functional assessment. Eur Respir J 10:241–244
Lemière C, Biagini RE, Zeiss CR (2006) Immunological and inflammatory assessments. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the workplace, 3rd edn. Taylor & Francis, New York, 179–197
Lemière C, Pelissier S, Chaboillez S, Teolis L (2006b) Outcome of subjects diagnosed with occupational asthma and work-aggravated asthma after removal from exposure. J Occup Environ Med 48:656–659
LeMoual N, Siroux V, Pin I, Kauffmann F, Kennedy SM (2005) (EGEA) on behalf of the epidemiological study on the genetics and environment of asthma. Asthma severity and exposure to occupational asthmogens. Am J Respir Crit Care Med 172:440–445
Levenstein S, Smith MW, Kaplan GA (2001) Psychosocial predictors of hypetension in men and women. Arch Inter Med 161:1341–1346
Malo JL, Ghezzo H (2004) Recovery of methacholine responsiveness after end of exposure in occupational asthma. Am J Respir Crit Care Med 169:1304–1307
Malo JL, Cartier A, L’Archevêque J, Ghezzo H, Soucy F, Somers J, Dolovich J (1990) Prevalence of occupational asthma and immunological sensitization to guar gum among employees at a carpet-manufacturing plant. J Allergy Clin Immunol 86:562–9
Malo JL, Ghezzo H, D’Aquino C, L’Archevêque J, Cartier A, Chan-Yeung M (1992) Natural history of occupational asthma: relevance of type of agent and other factors in the rate of development of symptoms in affected subjects. J Allergy Clin Immunol 90:937–944
Malo JL, Dewitte JD, Cartier A, Ghezzo H, L’Archevêque J, Boulet LP, Côté J, Bédard G, Boucher S, Champagne F, Tessier G, Contandriopoulos AP (1993) Quality of life of subjects with occupational asthma. J Allergy Clin Immunol 91:1121–1127
Malo JL, Cartier A, Boulet LP, L’Archevêque J, Saint-Denis F, Bhérer L, Courteau JP (1994) Bronchial hyperresponsiveness can improve while spirometry plateaus two to three years after repeated exposure to chlorine causing respiratory symptoms. Am J Respir Crit Care Med 150:1142–1145
Malo JL, Cartier A, Côté J, Milot J, Leblanc C, Paquette L, Ghezzo H, Boulet LP (1996) Influence of inhaled steroids on the recovery of occupational asthma after cessation of exposure: an 18-month double-blind cross-over study. Am J Crit Care Respir Med 153:953–960
Manfreda J, Becker AB, Wang PZ, Roos LL, Anthonisen NR (1993) Trends in physician-diagnosed asthma prevalence in Manitoba between 1980 and 1990. Chest 103:151–157
Mapp CE, Boschetto P, Maestrelli P, Fabbri LM (2005) Occupational asthma. Am J Respir Crit Care Med 172:280–305
Marabini A, Siracusa A, Stopponi R, Tacconi C, Abbritti G (2003) Outcome of occupational asthma in patients with continuous exposure: a 3-year longitudinal study during pharmacologic treatment. Chest 124:2372–6
Markovitz JH, Matthews KA, Whooley M, Lewis CE, Greenlund KJ (2004) Increases in job strain are associated with incident hypertension in the CARDIA study. Ann Behav Med 28:4–9
Martin JG, Campbell HR, Iijima H, Gautrin D, Malo JL, Eidelman DH, Hamid Q, Maghni K (2003) Chlorine-induced injury to the airways in the mouse. Am J Respir Crit Care Med 168:568–574
Matte TD, Hoffman RE, Rosenman KD, Stanbury M (1990) Surveillance of occupational asthma under the SENSOR model. Chest 98:173S–178S
McDonald JC (1995) Methodology. Study design. In: McDonald JC (ed) Epidemiology of work related diseases. BMJ:325–351
McDonald JC, Keynes HL, Meredith SK (2000) Reported incidence of occupational asthma in the United Kingdom, 1989–97. Occup Environ Med 57:823–829
McDonald JC, Chen Y, Zekveld C, Cherry NM (2005) Incidence by occupation and industry of acute work related respiratory diseases in the UK, 1992–2001. Occup Environ Med 62:836–842
Meggs WJ (1994) RADS and RUDS-The toxic induction of asthma and rhinitis. J Toxicol Clin Toxicol 32:487–501
Millon T (1994) Millon multiaxial inventory, 3rd edn. National Computer Systems, Minneapolis, MN
Mitchell CA, Gandevia B (1971) Respiratory symptoms and skin reactivity in workers exposed to proteolytic enzymes in the detergent industry. Am Rev Respir Dis 104:1–12
Moscato G, Dellabianca A, Perfetti L, Brame B, Galdi E, Niniano R, Paggiaro P (1999) Occupational asthma. A longitudinal study on the clinical and socioeconomic outcome after diagnosis. Chest 115:249–256
Moscato G, Dellabianca A, Maestrelli P, Paggiaro P, Romano C, de Zotti R, Marabini A, Voltolini S, Crippa M, Previdi M, Bramé B, Benzon R, Siracusa A (2002) Features and severity of occupational asthma upon diagnosis: an Italian multicentric case review. Allergy 57:236–242
Murphy RLH (1976) Industrial diseases with asthma. In: Weiss EB, Segal MS (eds) Bronchial asthma, Little, Brown and Cie, Boston, pp 517–536
Naciemento I, Nardi AE, Valenca AM, Lopes FL, Mezzasalma MA, Nascentes R, Zin WA (2002) Psychiatric disorders in asthmatic outpatients. Psychiatry Res 110:73–80
Nemery B (1996) Late consequences of accidental exposure to inhaled irritants: RADS and the Bhopal disaster. Eur Respir J 9:1973–1976
Netjeck V, Brown E, Khan D, Moore J, Wagner J, Perantie D (2001) Prevalence of mood disorders and relationship to asthma severity in patients at an inner-city asthma clinic. Ann Allergy Asthma Immunol 87:129–133
Newman Taylor A (2002) Asthma and work. Ann Occup Hyg 46:563–574
Newman-Taylor AJ, Venables KM (1984) Clinical and epidemiological methods in investigating occupational asthma. Clin Immunol Allergy 4:3–17
Ng TP, Hong CY, Goh LG, Wong ML, Koh KTC, Ling SL (1994) Risks of asthma associated with occupations in a community-based case-control study. Am J Ind Med 25:709–718
Nicholson PJ, Cullinan P, Newman TAJ, Burge PS, Boyle C (2005) Evidence based guidelines for the prevention, identification, and management of occupational asthma. Occup Environ Med 62:290–299
Ortega HG, Kreiss K, Schill DP, Weissman DN (2002) Fatal asthma from powdering shark cartilage and review of fatal occupational asthma literature. Am J Ind Med 42:50–54
Osler W (1892) The principles and practice of medicine. D. Appleton & Cie, New York, Special Edition Copyright 1978, The Classics of Medicine Library, Birmingham, AL
Perna G, Bertani A, Politi E, Colombo G, Bellodi L (1997) Asthma and panic attacks. Biol Psychiatry 42:625–630
Provencher S, Labrèche FP, De GL (1997) Physician based surveillance system for occupational respiratory diseases: the experience of PROPULSE, Québec, Canada. Occup Env Med 54:272–276
Quirce S (2004) Eosinophilic bronchitis in the workplace. Curr Opin Allergy Clin Immunol 4:87–91
Reijula K, Haahtela T, Klaukka T, Rantanen J (1996) Incidence of occupational asthma and persistent asthma in young adults has increased in Finland. Chest 110:58–61
Ries P (1986) Current estimates from the National health Interview Survey: United States, 1984. National Health Survey, Series 10, no 156. DHHS Publication (PHS), Washington, DC
Rimington LD, Davies DH, Lowe D, Pearson MG (2001) Relationship between anxiety, depression, and morbidity in adult asthma patients. Thorax 56:266–271
Rodier F, Gautrin D, Ghezzo H, Malo JL (2003) Incidence of occupational rhinoconjunctivitis and risk factors in animal-health apprentices. J Allergy Clin Immunol 112:1105–1111
Saarinen K, Karjalainen A, Martikainen R, Uitti J, Tammilehto L, Klaukka T, Kuppa K (2003) Prevalence of work-aggravated symptoms in clinically established asthma. Eur Respir J 22:305–309
Scanlon PD (2002) World Trade Center cough – A lingering legacy and a cautionary tale. N Engl J Med 347:840–842
Slovak AJM, Orr RG, Teasdale EL (1985) Efficacy of the helmet respirator in occupational asthma due to laboratory animal allergy (LAA). Am Ind Hyg Assoc J 46:411–5
Tarlo SM (2000) Workplace respiratory irritants and asthma. Occup Med: State Art Rev 15:471–483
Tarlo SM, Liss GM (2005) Prevention of occupational asthma–practical implications for occupational physicians. Occup Med (Lond) 55:588–594
Tarlo SM, Liss G, Corey P, Broder I (1995) A workers’ compensation claim population for occupational asthma. Chest 107:634–641
Tarlo SM, Liss GM, Banks DE (1997a) Assessment of the relationship between isocyanate exposure levels and occupational asthma. Am J Ind Med 32:517–521
Tarlo SM, Banks D, Liss G, Broder I (1997b) Outcome determinants for isocyanate induced occupational asthma among compensation claimants. Occup Environ Med 54:756–761
Toelle BG, Peat JK, Salome CM, Mellis CM, Woolcock AJ (1992) Toward a definition of asthma for epidemiology. Am rev Respir Dis 146:633–637
Toren L (1996) Self reported rate of occupational asthma in Sweden 1990–2. Occup Environ Med 53:757–761
Toren K, Brisman J, Olin AC, Blanc PD (2000) Asthma on the job: work-related factors in new-onset asthma and in exacerbations of pre-existing asthma. Respir Med 94:529–535
Troyanov S, Malo JL, Cartier A, Gautrin D (2000) Frequency and determinants of exaggerated bronchoconstriction during shortened methacholine challenge tests in epidemiological and clinical set-ups. Eur Respir J 16:9–14
Trupin L, Earnest G, SanPedro M, Balmes JR, Eisner MD, Yelin E, Katz PP, Blanc PD (2003) The occupational burden of chronic obstructive pulmonary disease. Eur Respir J 22:462–469
Vandenplas O, Malo JL (2003) Definitions and types of work-related asthma: a nosological approach. Eur Respir J 21:706–712
Vandenplas O, Delwiche JP, Depelchin S, Sibille Y, Vande Weyer R, Delaunois L (1995) Latex gloves with a lower protein content reduce bronchial reactions in subjects with occupational asthma caused by latex. Am J Respir Crit Care Med 151:887–891
Vandenplas O, Toren K, Blanc P (2003) Health and socioeconomic impact of work-related asthma. Eur Respir J 22:689–697
Vandenplas O, Ghezzo H, Munoz X, Moscato G, Perfetti L, Lemière C, Labrecque M, L’Archevêque J, Malo JL (2005) What are the questionnaire items most useful in identifying subjects with occupational asthma? Eur Respir J 26:1056–1063
Vandenplas O, Cartier A, Malo JL (2006) Occupational challenge tests. In: Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI (eds) Asthma in the workplace, 3rd edn. Taylor & Francis, New York, 227–252
Vanhanen M, Tuomi T, Tiikkainen U, Tupasela O, Voutilainen R, Nordman H (2000) Risk of enzyme allergy in the detergent industry. Occup Environ Med 57:121–125
Vollmer WM, Heumann MA, Breen VR, Henneberger PK, O’connor EA, Villnave JM, Frazier EA, Buist AS (2005) Incidence of work-related asthma in members of a health maintenance organization. J Occup Environ Med 47:1292–1297
Wagner GR, Wegman DH (1998) Occupational asthma: Prevention by definition. Am J Ind Med 33:427–429
Walusiak J, Hanke W, Gorski P, Palczynski C (2004) Respiratory allergy in apprentice bakers: do occupational allergies follow the allergic march? Allergy 59:442–450
Weiss KB, Gergen PJ, Hodgson TA (1992) An economic evaluation of asthma in the United States. N Engl J Med 327:571–572
Wild DM, Redlich CA, Paltiel AD (2005) Surveillance for isocyanate asthma: a model based cost effectiveness analysis. Occup Environ Med 62:743–749
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Malo, JL., Lemière, C., Gautrin, D., Labrecque, M., Lavoie, K. (2010). Asthma and the Workplace. In: Harver, A., Kotses, H. (eds) Asthma, Health and Society. Springer, Boston, MA. https://doi.org/10.1007/978-0-387-78285-0_18
Download citation
DOI: https://doi.org/10.1007/978-0-387-78285-0_18
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-0-387-78284-3
Online ISBN: 978-0-387-78285-0
eBook Packages: MedicineMedicine (R0)