Visual assessment of brain FDG PET data represents a fundamental skill, independent of the particular clinical indication toward which it is being applied. In our imaging facility, we routinely employ a systematic approach for evaluating regional metabolism throughout the brain. In addition, beginning in 2004, software tools approved by the Food and Drug Administration for quantifying relative regional activity became available to assist with that evaluation. This chapter first describes key aspects of a skilled visual assessment, and then examines methods of regional quantification that are practical in typical clinical environments, and, finally, illustrates an approach toward scan interpretation that integrates the visual and quantifying information present in clinical PET scans.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Posterior Cingulate Cortex
- Interhemispheric Fissure
- Average Cortex
- Generalize Atrophy
- Cortical Hypometabolism
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Visual assessment of brain FDG PET data represents a fundamental skill, independent of the particular clinical indication toward which it is being applied. In our imaging facility, we routinely employ a systematic approach for evaluating regional metabolism throughout the brain. In addition, beginning in 2004, software tools approved by the Food and Drug Administration for quantifying relative regional activity became available to assist with that evaluation. This chapter first describes key aspects of a skilled visual assessment, and then examines methods of regional quantification that are practical in typical clinical environments, and, finally, illustrates an approach toward scan interpretation that integrates the visual and quantifying information present in clinical PET scans.
Visual Assessment
Systematic visual examination of a clinical brain PET scan involves a number of key elements that are important to include in every assessment, at least implicitly, and if abnormalities are identified, then certainly explicitly mentioned in the interpretive report. These elements can generally be considered in five sequential steps, as outlined here.
Step 1: Optimizing Technical Quality
An important initial step in examining any imaging study is to assess its technical quality. This is done implicitly and, assuming that technical quality is adequate, this part of the assessment will not usually enter into the language of the clinical report. Considerations with respect to technical quality include filtering at a level that is not so rough (small full width at half maximum) as to leave the images too noisy, nor so smooth (large full width at half maximum) as to degrade the resolution to the point of not being able to make out small areas of variation in metabolism; displaying the images at sufficient zoom to allow them to be adequately seen, but still all included side by side in presenting a splash view of slices on the screen from one end of the brain to the other (e.g., superior to inferior planes, in the transaxial orientation), so that relative levels of metabolism throughout the brain can be readily compared; assessing the blood glucose level of the patient at the time of tracer administration (levels that are too high compete for FDG transport across the blood–brain barrier, as well as across the membrane of cells in the brain, reducing the statistical count quality of the image); and placing the patient’s brain symmetrically with respect to the plane of the ring of detectors, so that the ability to assess symmetry in the brain will not be compromised or complicated by tilt. Parameters for filtering smoothness and zoom usually need only be established at the outset for each type of instrument at each imaging facility, and as these are in part a matter of subjective taste of the interpreters, should be initially determined empirically. Images of a representative brain or phantom can be reconstructed by the technologists with a variety of zoom sizes and using filters over a range of full width at half maximum. In contrast, blood glucose levels and symmetry of placement will need to be considered for each acquired study.
For neuropsychiatric indications, patients should fast for at least 4 h before a FDG PET study, as with whole body studies done for oncologic indications; regimens for managing antidiabetic medications and food intake in diabetic patients can also be carried out in the same way as for whole body oncology studies. We do a finger-stick assessment of each patient before administration of FDG. A blood glucose level below 150 mg/dL (8.3 mmol/L) is desirable. It is recommended to have a policy in place such that if the level is much in excess of this (e.g., 180 or 200 mg/dL) that the interpreting physician be notified. Depending on the situation of the patient (e.g., distance of residence, schedule flexibility) and of the imaging facility (e.g., whether a physician is on site, and tightness of camera schedule), several options are possible. It may be decided to send the patient home and reschedule the study for a different day and different time of day; or, it may be decided to wait 1–2 h and re-check the blood glucose level to see if it has decreased to an acceptable level; or regular insulin may be administered intravenously according to a sliding scale, blood glucose re-checked in 20–30 min, and FDG administered at that time if its level has fallen appreciably (if not, another dose of insulin followed by another 20–30 min wait can be tried). If this latter approach is used, it is important to wait for at least 20 min after each insulin administration before giving FDG, in order to avoid driving the radiotracer into peripheral tissues and thus defeat the purpose of diminishing competition with blood glucose for uptake into the brain. 1
On the other hand, for neuro-oncologic indications, the instruction to the patient to fast before the PET scan may be omitted entirely; in fact, the patient should be advised to come to a morning study after having had a good breakfast, or to an afternoon study following a good lunch. This is apparently due to uptake of glucose into normal brain tissue becoming saturated at lower concentrations than is the case for the uptake of glucose into the higher-grade brain tumors for which FDG PET is obtained, and so the target-to-background contrast of tumor relative to normal brain tissue is actually enhanced by the presence of an elevated blood glucose level.
The PET scan (Fig. 2.1) should be inspected to ensure symmetric presentation. This can be done readily on transaxial views with respect to in-plane rotation by simply looking for tilt of the long axis of the brain away from the vertical, and with respect to out-of-plane rotation by examining structures below where most of the brain tissue lies, such as the photopenia representing the petrous ridges of the skull (Fig. 2.1, arrows), ensuring that they are symmetric in appearance (thus avoiding problems relating to asymmetry of the brain tissue itself). If visual inspection reveals asymmetric placement, the technologist responsible for processing the image can be asked to re-orient the brain image symmetrically, making the job of interpretation much more straightforward. This is particularly worthwhile since most facilities now obtain brain images by three-dimensional (3D) acquisition, providing resolution that is more nearly isotropic for all dimensions of the brain data. We would also recommend that the processing technologists be trained to automatically inspect the reconstructed images for asymmetry in the manner described previously, and as a matter of routine re-slice the brain volume to produce the most symmetric presentation, in advance of providing the images to the workstations where they will be interpreted.
Steps 2 and 3: Global Assessments
If it has not already been done, this is the time to set the color scale and its intensity thresholds to optimize the pixel display and to do so in a way that is reproducible from scan to scan. For this purpose, we recommend always beginning with a linear scale, such as the inverse linear grayscale; one knows that if a brain region has twice as much radioactivity associated with it, then it will be twice as dark in this black-on-white image. In the brain, FDG reflects the energy-expensive process of synaptic activity, and synapses are concentrated in the gray matter structures of the brain. Once the color scale has been selected, it is thus important to take maximal diagnostic advantage of the scale by spreading out most of its gradations over the gray matter intensities of the brain image. To do this, the lower intensity threshold can be raised until just before cortex appears affected, usually when approximately 90% of the scalp activity has been pushed into the background range of the scale (i.e., white, in the case of the inverse grayscale); the upper intensity threshold can then be adjusted until approximately 10% of the brain appears in the upper range of the scale (i.e., black, in the case of the inverse grayscale). In this way, the entire gray range of the color scale will be spread over 90% of the range of gray matter level metabolism of the brain. A problem in using color scales such as rainbow scales and other nonlinear display scales for the initial diagnostic assessment is that the way that the image appears to the interpreter becomes highly susceptible to precisely where the upper and lower intensity thresholds have been set. Therefore, it is recommended that those other scales be used, if at all, only after the interpreter has examined the brain scan using the more reproducible display offered by the linear scale as detailed previously.
Once technical quality has been taken care of, the next step in examining a brain PET scan is to assess the gross structure of the patient’s brain. We emphasize gross structure, because fine structural details should of course be assessed using structural imaging modalities (CT or MR) that provide the highest spatial resolution. It is nevertheless worth taking note at this stage of structural features of the scan such as areas of missing or deformed tissue that may represent moderate-sized cerebrovascular insults; asymmetry secondary to mass effects; relative expansion of the white matter/ventricular space suggestive of hydrocephalus; posttraumatic, postsurgical, or other disease-related changes; or extra tissue that may represent tumor. Most routinely, however, what will be assessed at this stage is the degree of any atrophy that is present, which can then be qualitatively rated as slight, mild, moderate, or severe. Generalized atrophy can be assessed at the level of the lateral ventricles by examining the interhemispheric fissure (Fig. 2.2, arrows in leftmost image of second row) and at the level of the third ventricle by examining the separation between the left and right sides of the thalamus (Fig. 2.2, arrow in middle image, third row). In young healthy subjects, before the onset of atrophy, left and right cerebral hemispheres, as well as left and right thalami, will be in close apposition to each other. To the extent that widening is seen at both levels, those findings are consistent with generalized atrophy. Evident sulcal widening within each hemisphere should also be mentioned. In describing the atrophy apparent on functional images secondary to age-related change, we use the qualitative terms slight, mild, and moderate to indicate the degree of atrophy typically seen in scans of patients in their forties to sixties, sixties to seventies, and seventies to eighties respectively, and use severe to indicate a degree of atrophy generally seen only under pathologic circumstances, whereas the descriptor itself is used independently of the age of the particular patient being evaluated. For example, it might be stated in describing the scan of a 50-year-old subject that there is moderate widening of the interhemispheric fissure and interthalamic distance, consistent with a degree of generalized atrophy that is greater than typical for a patient of this age; precisely the same description would be given if the scan belonged to an 80 year old, except for omission of the words greater than.
One reason that the description of global structural changes is necessary relates to the third step in our systematic approach, an assessment of the level of global metabolism of the cerebral cortex (Fig. 2.3). This is because we can have altered metabolism in two different ways. For example, hypometabolism can be present in an absolute sense, meaning that there would be (if one were to measure it semi-invasively) fewer milligrams of glucose being used per minute per 100 g of gray matter, or hypometabolism can be present in which there is less glucose being used because there is less gray matter remaining. Thus, it is important to have an idea of how much brain tissue is present in order to know how much metabolism it is fair to expect.
In assessing global cortical metabolism, it is critically important to use internal reference structures, so as not to be misled by anomalies of the way in which the brain is displayed. A couple rules of thumb can be especially useful in assessing the global level of cortical metabolism. First, in a healthy person in the absence of significant atrophy, the putamen and caudate nuclei of the basal ganglia (Fig. 2.3, arrows in rightmost image, first row) should have a level of metabolism approximately 9%–15% higher than frontal and parietal cortex, whereas the cerebellar cortex (Fig. 2.3, arrows in leftmost image, second row) should have a level of metabolism at least 10% lower than frontal and parietal cortex. This means that average cortex should have a level of metabolism (or darkness, on the inverse linear grayscale, shown in Fig. 2.3) falling approximately midway between that of the cerebellum and basal ganglia. Second, in a healthy person in the absence of significant atrophy, the thalamus (Fig. 2.3, arrows in leftmost image, first row) should have a level of metabolism approximately isometabolic with the frontal and parietal cortex. To the extent that the average cortical metabolic level is seen to fall closer to the cerebellar level than the basal ganglia level of metabolism, and correspondingly below the level of thalamic metabolism, that would be consistent with global cortical hypometabolism. When this pattern is seen, the first thing to check is whether it can be accounted for by a similar level of global cortical atrophy, as often occurs in older patients. (Also see comments below on effects of normal aging on cerebellar metabolism, which can further contribute to this pattern.) If so, combining this with the global structural assessment of the prior step, it is appropriate to state something such as, “a moderate degree of generalized atrophy typical for age, with atrophy-associated global cortical hypometabolism, is seen.” Other common causes of global cortical hypometabolism include central nervous system depressants such as those used as muscle relaxants, anxiolytics, hypnotics, and for sedation, as well as falling asleep during the FDG uptake period.
If, conversely, basal ganglia and thalamic levels of metabolism appear to fall below the level of general cortical metabolism, one should strongly suspect that image reconstruction was performed without adequate attenuation correction. Inadequate attenuation correction causes the deeper structures of the brain to appear washed out because of the greater degree of attenuation occurring as the photons emitted from the more central structures pass through more surrounding tissue, before they are able to reach the scanner detectors. In this case, the scan should be reconstructed with proper attenuation correction before interpretation is rendered. If the problem has stemmed from a failed transmission scan, the study often can still be salvaged by applying a calculated attenuation correction algorithm, taking advantage of the relatively regular ellipsoid shape of the brain.
Steps 4 and 5: Focal Assessments
The final steps of our systematic examination of brain PET are to evaluate for focal cortical and focal noncortical abnormalities. These steps tend to be, understandably, the most difficult to master, as the brain is composed of dozens of distinct structural and functional regions, each comprising its own characteristic levels of metabolism.2–5 Thus, it is necessary to develop through experience a strong sense of what the normal range of appearance should be for each region, to recognize when an individual region falls outside of that range, and finally, to arrive at a differential diagnosis that accounts for the constellation of any abnormalities noted.
In carrying out the fourth step, identifying focal cortical abnormalities, it is important to distinguish areas of true hypometabolism from areas of apparent hypometabolism caused by tissue loss and partial volume effects. This is done by concomitantly being attuned to the structural details of the brain (e.g., where the gyri are thicker and where they are thinning, where the sulci are widened by atrophic changes) and also where metabolism in adjacent tissue has been diminished by other processes. Visual assessments of cortical metabolism should be made only while mentally accounting for such changes. As an example of a common interpretive error, the superior aspects of parietal cortex may appear to be diminished in intensity in older patients, leading to the description of biparietal hypometabolism, and possibly the misinterpretation of the scan as revealing early Alzheimer’s disease. Isolated superior biparietal hypometabolism should in fact never be interpreted as representing Alzheimer’s disease, which characteristically affects inferior parietal cortex before more superior cortex is affected. What this pattern most often reflects is the atrophy of normal aging, in which sulcal widening affecting the external face of the cortical ribbon leads to a partial volume effect apparent in the most superior transaxial planes, which can be readily confirmed by examining the corresponding sagittal views.
Once structural considerations are taken into account, the next issue facing the interpreter is to know the relative levels of metabolism to expect among different regions of the cortex. The most important characteristic features of cortical metabolism as reflected in the FDG PET images are summarized here. First, metabolism in the temporal cortex is visibly lower than cortical metabolism in the frontal, parietal, and occipital lobes in the brains of healthy adults of all ages. Moreover, it is normal for anterior temporal metabolism to be lower than posterior temporal metabolism. Because of partial volume effects with surrounding white matter levels of metabolism, it is also normal for medial temporal cortical metabolism to appear lower than lateral temporal metabolism.
Second, it is normal for the cingulate cortex (the medially lying cortex seen immediately above the white matter of the corpus callosum on sagittal planes viewed near midline, as well as in the most inferior transaxial planes sliced along the canthomeatal line to demonstrate a continuous strip of cortex stretching anteriorly to posteriorly; Fig. 2.4) to demonstrate visibly higher metabolism in the posterior cingulate than in the anterior cingulate cortex and than average cortex of the frontal, parietal, and of course temporal lobes. The posterior cingulate cortex has, in fact, the highest level of metabolism of any non-sensory/motor-activated part of the cerebral cortex and can be 20%–40% more metabolic than average cortex found in the other regions of young healthy brains. The cingulate cortex is a part of the brain that tends to atrophy faster than average cortex, however, so that the gradient of posterior cingulate to frontoparietotemporal cortex becomes less apparent with age. Nevertheless, it should maintain an appearance of intensity more similar to basal ganglia than to average cortex in healthy subjects. Assessment of this cortical region takes on special importance in the context of a dementia evaluation, because the posterior cingulate cortex happens to also be the region of the brain in which metabolism declines most significantly in the earliest stages of Alzheimer’s disease.6
Third, heterogeneity resulting from variable sensory activation can be expected. Thus, in a PET scan acquired after FDG uptake has proceeded with eyes open (as we recommend), it is normal for metabolism in the occipital lobe to appear greater than metabolism in other lobes of the brain. Likewise, if the patient’s attention was attracted asymmetrically to either the left or right visual field during the uptake period, asymmetric occipital metabolism may be seen. For similar reasons, metabolism in sensorimotor cortex, and in the superior temporal lobe corresponding to auditory cortex, is often seen to be mildly elevated above the level of metabolism found in surrounding cortex.
Fourth, apart from the sensorimotor region, metabolism along the lateral aspect of the frontal and parietal lobes, after accounting for gyral thickness and sulcal width, should be fairly homogeneous in the brains of adults in the middle-age range.
As for focal noncortical abnormalities, we have already reviewed what relative levels of metabolism to expect for cerebellum, thalamus, and basal ganglia structures. At this point, any asymmetries in metabolism of those structures from left to right, or nonuniformities in metabolism of those regions from anterior to posterior, should be noted. In looking for those abnormalities, it is important to examine the parts of each structure in the planes in which they are most robust, to avoid partial volume effects caused by activity in these relatively thin structures being averaged with the relatively low level activity above and below them. One should bear in mind, for example, that the plane in which the right caudate nucleus head of the basal ganglia appears most robust may differ from the plane in which the right lentiform nucleus of the basal ganglia is best appreciated, or that the plane in which a structure is best seen on one side of the brain may be slightly offset from the plane in which its contralateral counterpart is best seen.
Lastly, with respect to effects of healthy aging on cortical metabolism (Fig. 2.5), because the metabolism of the prefrontal region, particularly the most medial and anterior portions of the frontal lobe (Fig. 2.5, arrows in left image of bottom row), typically declines faster than metabolism of average cortex, it is normal for prefrontal metabolism to be slightly greater than parietal metabolism in young people, and slightly lower than parietal metabolism in older adults. Otherwise, the pattern of metabolism seen throughout the cortex in healthy brains remains relatively stable throughout adulthood. Finally, it should be noted that the metabolism of the cerebellum tends to increase during normal aging. This is seen visually not only as a relative effect caused by global hypometabolism of the cortex, but also reflects an actual increased rate of glucose utilization by the cerebellum in absolute terms in elderly subjects.3
Quantification
Several issues need to be considered with respect to quantifying brain PET studies in the context of rendering clinical interpretations. For example, is it necessary to quantify the scans or is visual interpretation adequate? When is it most helpful to perform quantification? What strategies may be employed to obtain quantifying data, and what software packages are available for implementing those strategies?
With respect to whether quantification of brain PET is necessary, the answer is clearly no, in the sense that it has been seen that substantial diagnostic and prognostic accuracies with regard to dementing disorders are achievable through visual interpretation alone7 when performed by experienced readers of brain PET scans. Nevertheless it may be helpful in several ways to have quantitative information available. For example, for readers without a lot of experience in reading brain PET who are faced with the task of rendering an occasional interpretation (a common occurrence, given the traditionally relatively low volume of neurologic PET scans relative to oncologic PET scans in many clinical environments), it may be useful for increasing their interpretive confidence and accuracy. We recently assessed this type of utility in a systematic examination of the readings of brain PET scans by five physicians in our nuclear medicine residency program; with use of an FDA-approved commercially available software tool dedicated to brain PET quantification, the physicians interpreted scans correctly 8%–13% more often (based on the criterion standard of long-term clinical follow-up), relative to relying on their visual analyses alone. The information can also be used to provide even expert readers with quantitative context (e.g., “Lateral temporal metabolism appears asymmetric, with left-sided activity measuring 15% lower than on the right.”) or statistical support (e.g., “Activity in posterior cingulate cortex falls 3.5 standard deviations below the normal mean for this region.”), to supplement their interpretations with findings they visually have noted, as well as to perhaps draw their attention to imaging findings that may have been overlooked initially.
Of course, quantification is essential for the purpose of addressing questions that are intrinsically quantitative, not only questions about groups of subjects (e.g., “In healthy human brain tissue, how much more metabolically active is the posterior cingulate than the anterior cingulate cortex?” or “Which patients have more severe hypometabolism in posterior cingulate cortex—Alzheimer or frontotemporal dementia patients?”), but also quantitative questions in an individual patient relative to a normal group (“How hypometabolic is the posterior cingulate cortex in this patient, who clinically appears to have mild AD?”) or statistical questions (“Is the observed degree of hypometabolism in the inferior parietal cortex statistically significant for that brain region?”).
Another useful role for quantification of brain PET images is in defining the degree of change over time between two or more scans obtained for the same patient. For example, neurodegenerative dementing processes are associated with inexorable decline of the metabolism of involved brain regions. The metabolic decline precedes and parallels symptomatic decline. Thus, if a patient’s memory measurably worsens over 1 or 2 years and that deterioration is a result of incipient Alzheimer’s disease, it can then be expected that metabolism of posterior cortical regions will have declined during that interval. In the absence of a pathologic process, on the other hand, regional cerebral metabolism tends to be more quantitatively stable than neuropsychological performance (the latter being more prone to day-to-day, and even hour-to-hour, variability related to factors such as motivation, alertness, practice effects, and so forth). Thus, a significant decline in regional metabolism can be expected to provide a more sensitive (better signal-to-noise ratio because of smaller test variance) and more specific (based on characteristic patterns of regional cerebral involvement, coupled with being less prone to influence from nondisease processes) indicator of the presence of Alzheimer’s and other neurodegenerative disease processes, than changes in neuropsychological test scores of individual patients. In patients with initially borderline abnormal scans who have regional hypometabolism suggesting the presence of an incipient disease process, quantifiable interval decline in the quantitatively borderline regions adds assurance to the diagnosis that the initial scan suggests, even if those changes remain very mild.
Once the decision to quantify brain PET data has been made, the next issues to be addressed involve choosing an appropriate strategy for obtaining quantifying data and selecting a software package among several now available with which to implement that strategy. The quantifying approaches that are in clinical use generally fall into either of two categories: (1) those based on measuring activity in a neuroanatomically or functionally defined region of interest (ROI) of the brain, and (2) those based on measurements of activity in individual image pixels or their 3D counterpart, voxels.
ROIs that are manually defined by an operator with appropriate neuroanatomic training on images containing pertinent anatomic landmarks provide a gold standard of regional activity. As might be expected, however, such an approach requires a level of neuroanatomic expertise and is sufficiently time- and labor-intensive that it is not considered to be practical to implement for routine clinical interpretations of brain PET images. An exception is when there is a well-defined focus (or small number of foci) to be measured (e.g., an area of suspected tumor growth), around which ROIs can be easily defined. In the evaluation of dementia, in contrast, numerous regions in need of quantification exist, but they are not easy to define (dorsolateral prefrontal cortex, inferior parietal lobule, posterior cingulate cortex, angular and marginal gyri, sensorimotor cortex, and so forth).
During the last decade, a number of innovative investigators developed voxel- or pixel-based approaches designed to reduce the time and labor involved in the manual ROI method, such as the statistical parametric mapping approach initially developed by Friston and colleagues in the United Kingdom, as implemented in several versions of SPM software, and the three-dimensional stereotactic surface projection (3D SSP) method developed by Minoshima and his colleagues in the United States as implemented in NeuroStat and, more recently, other versions of 3D SSP-based software. These methods, which can sample thousands of pixel/voxel units denoted by their location in an image derived from warping the patient’s individual scan into some form of template space, lend themselves to relatively automated output of quantitative or statistical units and then referred to locations in the original patient’s brain image, which they are meant to represent. This allows for a rapid sampling of the brain volume, without neuroanatomic expertise needed for the quantification process itself. Of course, to analyze the output, the reader must possess an appropriate level of neuroanatomic expertise and must generally also assume that the individual pixel/voxel units have been assigned locations that correspond closely with the neuroanatomic sites in the patient’s brain, before the image-warping process, from which the measured activity was derived.
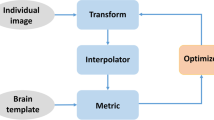
The standardized region of interest (SROI) approach combines elements of both the manual ROI and pixel/voxel-based approaches. Anatomically and functionally defined regions are defined on a brain template, thereby essentially encoding the neurologic expertise of the developers into the program. Hundreds of these SROIs can be predefined and then applied to an individual patient’s brain, which has undergone elastic transformation to the template space (or, alternatively, the template-defined SROIs may be warped to the patient’s brain scan), so that the end-user can obtain an automated determination of the levels of activity measured in all brain regions in a matter of seconds, rather than the many hours it would require to obtain comparable information by the manual ROI method.
In the United States, the FDA approves medical imaging software to be marketed for clinical applications under its purview to regulate medical devices. The first software product dedicated to the quantification of brain PET scans to receive approval from the FDA was released in 2004, and it employs the SROI approach described previously. The essential features and algorithms underlying that software were originally developed by the author and his colleagues at the University of California, Los Angeles (UCLA) to facilitate research focused on measuring the utility of brain PET applied to diagnostic and prognostic assessments of patients undergoing clinical evaluation for cognitive impairment. The University of California subsequently licensed marketing and development rights to Syntermed, Inc. (Atlanta, GA), which distributes the software package under the name NeuroQ. Other FDA-approved products that have been commercially released at the time of this writing include Scenium (Siemens AG, New York, NY) and MIMneuro (MIMvista Corp., Cleveland, OH). These products differ from each other, not only with respect to the visual appearance of their displays and the display features offered, but in more substantive ways as well, including the underlying algorithms used for quantification, the tradeoffs made in versatility versus dedicated application to clinical brain PET interpretation, the degree to which straightforward quality control by the user versus presentation of the output following an opaque black box quantification process is enabled, the options provided for normalizing the PET data, and the readiness with which the findings evident in the visual display can be related to the numeric results of analysis, as might be given in a clinical report. Although we use a wide variety of software applications for analysis of brain PET scans applied to a diverse range of our research activities at UCLA (including packages not approved by the FDA, such as SPM), the product we use for automated quantification of brain PET to assist with rendering our clinical interpretations continues to be NeuroQ. For this reason, it has been employed, and its output illustrated, in many of the cases described in this book; this is a direct reflection of the actual working practices of the authors and should not be interpreted as implying its superiority over other products that are available for quantifying brain PET scans.
Clinical Reports
Once a patient’s scan has been analyzed qualitatively and quantitatively, the remaining task faced by the examiner is to prepare a clinical report that describes the pertinent findings and integrates them to logically support a prognostic or diagnostic conclusion, addressing the clinical question for the which patient is being evaluated. If the approach for systematic examination of the brain PET scans described in this chapter is followed, it lends itself readily to direct translation of that process into a written report. Findings can be sequentially listed as technical comments (when necessary, to qualify an interpretation), global structural and metabolic assessments, focal cortical observations, focal noncortical observations, and (when performed) quantitative and statistical measures, all in a standard three- or four-item format. We discourage listing quantifying measures that are not pertinent to the visual observations; this minimizes the risk of being distracted from the interpretation by numeric artifacts and avoids losing the reader of the report in a sea of numbers. By the time patients are symptomatic for whatever it is that has led to their referral, any neuropathologic processes underlying their symptoms that have metabolic consequences generally will have had an impact on brain function that is visually observable (or, as Bob Dylan put it, “You don’t need a weatherman to know which way the wind blows”—although it may be of interest to supplement that qualitative determination with a statement about how fast it is blowing.)
To make all this more concrete, consider the case of a 73-year-old woman who underwent brain FDG PET for evaluation of mild cognitive changes, whose scan demonstrates mild hypometabolism that covers areas that are highly characteristic of incipient Alzheimer’s disease (Fig. 2.6, left). As we follow along the lateral contour from the frontal cortex (top half of image) to parietotemporal cortex (bottom half of image) seen in that plane, metabolism is seen to mildly decline bilaterally and is slightly lower on the right side of the brain (left side of image). The right parietotemporal cluster of regions was found to fall more than three standard deviations below normal. Also in that leftmost image, the posterior cingulate cortex is seen to display a similar level of metabolism, even though this region normally should be considerably more metabolically active than average cortex. A systematic examination of the remainder of the patient’s scan led to the following report of findings and overall conclusion.
Results of quantification of a brain PET scan, using a standardized region of interest (SROI) approach. Among the three larger images on the left side of the window, the leftmost image shows an axial plane from the patients’ original PET scan, the center image shows the corresponding plane from the normal template on which are outlined SROI contours sampling posterior cortical regions in white, and the rightmost image demonstrates that plane from the patient’s scan after being transformed into template space, with those areas sampled by the SROIs that are hypometabolic (as defined by falling in the lowest 5% of a normal distribution) displayed in color. On the right side of the window, 12 axial planes from the template are shown extending from superior to inferior levels for anatomic reference, with the superimposed color scale corresponding to the results of quantification of the patient’s brain data. In that two-dimensional scale, areas that are bright blue are normal, areas that are bright red are the most abnormal in both magnitude and in terms of statistical significance of the abnormality relative to a normal database, and intermediate shades represent areas of abnormality that may be statistically significant, but by a lesser magnitude. (Courtesy of NeuroQ, Syntermed, Inc., Atlanta, GA.)
Findings
-
1.
The gross structure of the brain demonstrates mild widening of the interhemispheric fissure and interthalamic space, consistent with mild generalized cerebral atrophy.
-
2.
The pattern of FDG metabolism in this scan shows mild but extensive bilateral parietal (somewhat worse on right) and posterior cingulate cortical hypometabolism and mild bilateral temporal cortical hypometabolism. The occipital metabolism is less prominent than is typically seen in an eyes-open study.
-
3.
Basal ganglia metabolism is robust, and the activity of the thalamus and brainstem is unremarkable. The cerebellar cortex shows mild crossed cerebellar diaschisis with the left-sided metabolism slightly lower than right.
-
4.
SROI analysis quantifies the posterior cingulate and parietotemporal cortical metabolism as falling approximately 2–3 standard deviations below normal mean, and temporal regions as ranging from approximately 1–5 standard deviations below normal mean, all as normalized to pons.
Conclusion
The conclusion is posterior-predominant mild cortical hypometabolism, particularly affecting parietal, temporal, and posterior cingulate cortex, as described previously. This pattern is most commonly seen in the context of Alzheimer’s-like changes occurring in the patient’s brain.
The first three items in the Findings section are based on visual analysis of the patient’s scan, examined in the order detailed in the first section of this chapter. The fourth item in the Findings section described results of scan quantification that are pertinent to that visual analysis and the diagnostic assessment that is about to be presented. As articulated in the Conclusion, note that in the absence of clinical dementia, regardless of how characteristic the scan findings are, a diagnosis of Alzheimer’s disease per se cannot be reached, given that a key criterion for having that disease is the presence of dementia. Nevertheless, the presence of the biochemical processes that will eventually lead to that diagnosis is indicated by the pattern of metabolism, as conveyed in the final sentence of the report. Similarly, although not a part of this patient’s current clinical picture, if it can be confirmed that the patient had eyes open during the FDG uptake period, the decrease in occipital metabolism could reflect early changes associated with cortical deposition of Lewy bodies.
Summary
Regardless of what other tools are brought to bear on the process, the clinical interpretation of brain PET scans must be built on the foundation of a skilled visual assessment of the pattern of radiotracer uptake. That assessment involves examining at least five aspects of the study, as detailed in this chapter: (1) technical quality, (2) structural integrity of the brain, (3) global metabolism, particularly of the cortex, (4) focal cortical metabolism, and (5) focal noncortical metabolism (most often including basal ganglia, thalamus, cerebellum, and brainstem). In the past few years, software tools have become available to assist with this analysis, which can be used to lend quantitative and statistical support to interpretations suggested by the observed uptake patterns. Applying the acquired skills and tools in this way to FDG PET scans obtained of patients undergoing scanning for dementia-related conditions, qualitative and quantitative findings may be fluidly integrated into final written reports that contribute to the diagnostic evaluation as described in the next chapter.
References
1. Buchert R, Santer R, Brenner W, et al. Computer simulations suggest that acute correction of hyperglycemia with an insulin bolus protocol might be useful in brain FDG PET. Nuklearmedizin 2009:(in press).
2. Minoshima S, Frey KA, Burdette JH, Interpretation of metabolic abnormalities in Alzheimer’s disease using three-dimensional stereotactic surface projections (3D-SSP) and normal database. J Nucl Med 1995;36:237P.
3. Moeller JR, Ishikawa T, Dhawan V. The metabolic topography of normal aging. J Cereb Blood Flow Metab 1996;16:385–398.
4. Ishii K, Sakamoto S, Sasaki M. Cerebral glucose metabolism in patients with frontotemporal dementia. J Nucl Med 1998;39:1875–1878.
5. Silverman DHS, Alavi A. PET imaging in the assessment of normal and impaired cognitive function. Radiol Clin North Am 2005;43:67–77.
6. Minoshima S, Giordani B, Berent S. Metabolic reduction in the posterior cingulate cortex in very early AD. Ann Neurol 1997;42:85–94.
7. Silverman DHS. Brain F-18-FDG PET in the diagnosis of neurodegenerative dementias: comparison with perfusion SPECT and with clinical evaluations lacking nuclear imaging. J Nucl Med 2004;45:594–607.
Silverman DHS, Small GW, Chang CY et al. Positron emission tomography in evaluation of dementia: regional brain metabolism and longterm outcome. JAMA 2001;286:2120–2127.
Silverman DH, Truong CT, Kim SK, et al. Prognostic value of regional cerebral metabolism in patients undergoing dementia evaluation: comparison to a quantifying parameter of subsequent cognitive performance and to prognostic assessment without PET. Mol Genet Metab 2003;80:350–355.
Silverman DH, Mosconi L, Ercoli L, et al. Positron emission tomography scans obtained for the evaluation of cognitive dysfunction. Semin Nucl Med 2008;38:251–61.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Science + Business Media, LLC
About this chapter
Cite this chapter
Silverman, D.H. (2009). Clinical Interpretation of Brain PET Scans: Performing Visual Assessments, Providing Quantifying Data, and Generating Integrated Reports. In: Silverman, D. (eds) PET in the Evaluation of Alzheimer's Disease and Related Disorders. Springer, New York, NY. https://doi.org/10.1007/978-0-387-76420-7_2
Download citation
DOI: https://doi.org/10.1007/978-0-387-76420-7_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-0-387-76419-1
Online ISBN: 978-0-387-76420-7
eBook Packages: MedicineMedicine (R0)