Abstract
The interplay between tumors and their immunologic microenvironment is complex and difficult to decipher, but its understanding is of seminal importance for the development of novel prognostic markers and therapeutic strategies. This chapter discusses tumor−immune interactions in several human cancers that illustrate various aspects of this complexity and proposes an integrated scheme of the impact of local immune reactions on clinical outcome. Thus, the fact that a strong infiltration of memory T cells with a Th1 and cytotoxic pattern is the strongest predictor for recurrence and metastasis is exemplified in colorectal cancer in which intratumoral chemokines shape an efficient immune reaction. Based on these data, we propose an immune score that predicts recurrence in early stage (UICC-TNM stage I-II) cancers. Studies on non-small lung cancers have confirmed findings of colorectal cancers and have addressed the question of the sites where antitumor immune reactions may take place. Tertiary lymphoid structures (TLS) adjacent to the tumor nest are sites of intense activity with mature dendritic cells in contact with T cells and germinal-like centers with proliferating B cells. The large number of these TLS being correlated with disease specific and overall survival tempts to postulate that they are privileged sites to mount an efficient antitumor reaction. Inflammation is a major component of human tumors and chronic inflammation is generally of bad prognosis. Head and neck cancers are highly inflammatory and two ways to modulate inflammation in these diseases are presented here: soluble IL-15 receptor α (IL-15 Rα) increases the pro-inflammatory effect of IL-15 and aggravates inflammation resulting in poor prognosis when found at high levels in the plasma of patients. By contrast, infiltration of regulatory T cells is paradoxically beneficial for local control of head and neck tumors, probably by “cooling down” the inflammatory process. The modulation of other aspects of innate immunity may also result in paradoxical effects such as the signaling through Toll like receptors 7 and 8 expressed on lung tumor cells which induce an aggressive tumoral phenotype. Finally, the analysis of primary intraocular lymphoma, which develops in the eye, exemplifies the induction of an antitumor immune reaction in an “immune sanctuary,” presenting all the complexities of the tumor–immune interplay in “open” tissues such as the colon or the lung.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The fact that the immune system may prevent the occurrence of tumors has been largely documented in immunodeficient mice (Shankaran et al. 2001) and individuals in whom cancer incidence is much higher than in immunocompetent hosts (Van der Meer et al. 1993; Birkeland et al. 1995). Although demonstrative of the concept that nascent cancer cells can be viewed as “foreign” or “danger” by a competent immune system, these observations are of little clinical interest for treating clinically established cancer. They indeed support the concept of immunosurveillance (Burnet 1970) and prompt to treat immunodeficiency to restore the best immunocompetence to prevent infections and potential cancers rather than providing clues for immunotherapy of cancers that have already reached a clinical stage.
However, in the recent years, it appeared that the immune system may also influence the clinical outcome of patients with established tumors. The demonstration in mice that the dormancy stage of a cancer, i.e., a period of months or years during which cancer cells are present in the body usually after reductive surgical and/or radio-chemo therapy, is controlled in great part by interferon-responsive immune cells, creating an equilibrium between immunity and cancer (Koebel et al. 2007), provided the scientific bases for adjuvant immunotherapies. In humans, it is well known that tumors with a similar histopathologic stage, referred as TNM (Greene and Sobin 2009) (T (extension of the primary tumor), N (lymph node invasion), M (distant metastasis)) may behave differently in terms of recurrence and survival. Thus, although the TNM classification utilized worldwide is a good prognostic staging system since cancers with no lymph node invasion or distant metastasis (T1-4, N0, M0) have a better clinical outcome than advanced cancers (T1-4, N+, M+), there are frequent discrepancies. Indeed, some patients with small tumor burden experience rapid recurrence even after curative treatment, while others with advanced cancers show surprisingly good prognosis. Thus, in colorectal cancer, patients with lymph node invasion (UICC-TNM stage III) have a likelihood of recurrence of 50–60% within 5 years, but a significant proportion of patients (about 30%) with no detectable lymph node or distant metastasis (UICC-TNM stages I/II) present with recurrent disease within few years (O'Connell et al. 2004; Pagès et al. 2005).
Whether an immune control is responsible for keeping potentially metastatic or invading cancer cells in hold (“equilibrium”) in humans is also an intensive field of investigation as it would provide novel prognostic markers as well as new therapeutic avenues. When quantitative and functional analyses of intratumoral immune reactions became available, data accumulated to show that a high lymphocytic infiltration in the primary tumor usually correlates with a better clinical outcome in patients with cancer (reviewed in Pagès et al. 2010). Moreover, the functional orientation of the infiltrating lymphocytes seems to be instrumental for the control of recurrence. For instance, quantification of cytokine gene expression in uterine cervical tumors, resected from early-stage patients, revealed that low levels of interferon (IFNγ) transcripts at the tumor site were associated with recurrence within 2 years after surgery (Tartour et al. 1998). Similar data were reported in colorectal (Pagès et al. 1999) and prostatic cancers (Lebel-Binay et al. 2000). These observations are reminiscent of the findings of Schreiber and Smyth (Koebel et al. 2007; Dunn et al. 2006; Smyth et al. 2006) demonstrating in mice that the equilibrium phase was largely dependent on IFNγ. Altogether these data suggest that the presence of a strong Th1 compartment in a primary tumor is associated with, and putatively controls, metastatic cells release, circulation and / or nidation. However, the immune reaction in tumors is complex with the recruitment of many cells playing opposite effects, Th1 versus Th2, T reg versus cytotoxic T cells, NK, and NK-T cells, etc… Moreover, tumors are sites of intense inflammation, which is often detrimental for the host when macrophages support tumor growth and neovascularization (Balkwill and Mantovani 2001; Coussens and Werb 2002), but is sometimes beneficial when acute inflammation, such as in bladder cancer following acute infections or therapy by BCG (Lamm 1992), results in cancer cell destruction. In the recent years, comprehensive analyses of the intratumoral immune cells and molecules gave new insights into the understanding of the role of the immune system in controlling tumor growth and spreading to other organs (Galon et al. 2007; Pagès et al. 2008; Bindea et al. 2009). They permitted the identification of immunological prognostic markers (Pagès et al. 2009, 2010) and should eventually provide new ways to refine cancer therapy. In this chapter, we mainly discuss our own data on the analysis of the intratumoral immune infiltrates in human cancers, their functional orientation, the respective importance of Th1, T reg, cytotoxic, and memory T cells, as well as the formation of tertiary lymphoid structures (TLS), composed of mature dendritic cells (DC) and T and B lymphocytes, adjacent to the tumor, in view of their prognostic value and their dynamic interactions. To illustrate the general character of the host−immune interactions, four examples of human tumors will be addressed: colorectal cancer, a visceral disease open to diet and bacterial antigens ; lung carcinoma, a tumor open to airways ; head and neck inflammatory cancer; and primary intra-ocular lymphoma, an hematological cancer developing in an immunopriviledged site. Finally, we will propose some new insights on how some cancer cells may divert innate immune reactions to protect themselves from acute inflammation and chemotherapy.
2 “In Situ” Immune Contexture, the Strongest Prognostic Factor for Recurrence and Overall Survival: The Case of Colorectal Cancer
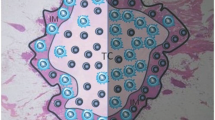
Histopathological analysis of colorectal cancers shows that these tumors are infiltrated by inflammatory and lymphocytic cells, in variable quantities (Dalerba et al. 2003). A closer look reveals that the latter is not distributed randomly, but seem to be organized in more or less dense infiltrations in the tumoral zone, referred to as center of the tumor (CT), in boarding edges at the invasive margin (IM) of tumoral nests (Fig. 1a), and in lymphoid islets adjacent to the tumor. This organization is seen in many other solid tumors and the potential role of the lymphoid islets will be discussed later when presenting the example of lung carcinoma.
We have extensively analyzed the impact of the quantity, the functional orientation, and the location of the immune cells of the tumor microenvironment – that we propose to call the “immune contexture” – on cancer recurrence, metastasis, and patient survival. In a retrospective study of 959 colorectal tumors, followed for over 15 years in the digestive surgery ward of European Hospital Georges Pompidou, we first searched for early signs of metastasis in the primary tumor. We observed venous emboli (VE), lymphatic invasion (LI), and perineural infiltration (PI) in 27% of the tumors. Applying univariate and multivariate Cox analysis, we found that the presence of one early sign of metastasis (VE or LI or PI) was associated with bad prognosis both in terms of disease free survival (DFS) and overall survival (OS). The presence of the three signs was of even worse prognosis. We, then, asked the question of whether the “in situ” immune infiltrates were different in VELIPI (−) and VELIPI (+) tumors. For this purpose, we undertook a comprehensive quantification of immune gene expression by Q-PCR, immune cell identification by flow cytometry of extracted living cells, and tissue micro-array of tumors using antibodies recognizing immune cell subsets. The conclusion of this analysis was that high numbers of memory T cells, particularly effector/memory T cells correlated with lack of early signs of metastasis (VELIPI (−)) and that tumors with low numbers of memory T cells had local (VELIPI(+)) or distant (N+ or M+) metastasis (Pagès et al. 2005). Not only is there a particular immune pattern associated with metastasis at the time of surgery but, more importantly, the “in situ” immune reaction is associated with DFS and OS. Thus, we found that expression of genes associated with adaptive immunity (T-bet, IRF1, IFNγ, CD8α, granzyme B, granulysin) and not genes associated with inflammation (IL-8, VEGF, CEACAM-1, MMP-7) or immuno-suppression (TGFβ, IL-10, B7-H3, CD32b) were associated with lack of metastasis and recurrence (Pagès et al. 2005). Enumeration of cells of adaptive immunity within the tumors revealed an interesting aspect: even if all the T cells or CD8 cells or granulysin-expressing cells or memory (CD45RO) cells were associated with good prognosis, taking into account their location and combining two markers greatly improved their prognostic impact. By combining the analysis of several zones in the CT and in the IM, we found that high infiltrates of memory T cells (CD3/CD45RO) or potential cytotoxic T cells (CD8/CD45RO/granulysin +) (Fig. 1b) both in the center and the IM were highly significantly (p < 10−11) associated with very good prognosis, both in terms of DFS and OS. Tumors with low memory T or cytotoxic T cells in both zones (Fig. 1c) were associated with very bad clinical outcome. Heterogenous (Hi-Lo or Lo-Hi) tumors were intermediate but rather on the bad prognosis side. These differences hold true for all T (tumor extension), N (lymph node involvement), and M (distant metastasis) stages and remained the only significant factor – with bowel perforation – for disease free and OS in multivariate Cox analysis when classically used histo-prognostic factors (tumor extension, lymph node metastasis and differentiation) were no longer significant (Galon et al. 2006).
These observations, confirmed on two independent cohorts, change the paradigm of cancer prognosis at least for colorectal cancer (Galon et al. 2007), and propose novel prognostic tools (Pagès et al. 2010) that may guide cancer therapy.
The fact that it is not only the overall quantity or even the functional orientation but also the location of the immune cells that influence tumor recurrence supports the concept that distinct cells with selective functions may, at different tumor locations, play a crucial role in controlling metastasis escape. Analysis are in progress to determine if each region has a different influence on cancer-related progression i.e., tumor size, lymph node, or distant metastasis.
A second indication that clinical outcome is associated with selective immune contexture was provided by the analysis of the coordination of immune gene expression. We studied a cohort of early stage colorectal cancers in which we confirmed the association of high memory T cell infiltration in CT and IM and good prognosis. We, then, performed a gene expression screening (108 genes) looking for immune, inflammation, and angiogenesis-associated genes whose expression correlated, or not, with high CD3/CD45RO infiltration in CT and IM. The results were straightforward: not surprisingly, genes associated with T cell memory were found overexpressed in CD3/CD45RO high tumors and under-expressed in the others ; strikingly, two other clusters of genes were coordinatively coexpressed in tumors with high CD3/CD45RO infiltration: genes involved in Th1 and cytotoxic T cell functions. Genes associated with Th2 functions, suppression, inflammation, and vascularization were not associated with memory T cell infiltration (Pagès et al. 2009).
These data show that a coordinated immune reaction is associated with the immune pattern which predicts clinical outcome. It is therefore likely that Th1 and cytotoxic T cells contribute to keep in hold potential metastatic cells at early stages of the metastatic process. This hypothesis is supported by the fact that, although of no statistic influence by itself, high expression of VEGF gene counteracts the beneficial effect of IRF1 (Th1-associated) or granulysin (cytotoxic granules) high gene expression (Camus et al. 2009). We therefore postulate that the presence of high numbers of memory Th1 and cytotoxic T cells in the center and the IM of primary tumors controls the attempts of metastatic cells to leave through vascular or lymphatic vessels. When the tumor grows, with zones of hypoxia, VEGF is produced that increases the tumor neovascularization offering more emigration possibilities to metastatic cells overcoming even a strong coordinated immune reaction. VEGF also inhibits DC maturation that may result in an increase of Treg in the tumor microenvironment (reviewed in Johnson et al. 2009). Finally, when the immune contexture is disrupted, no effective control of metastasis and therefore recurrence and survival can anymore be carried out by the immune infiltrate, even it is still present in the tumor (Fig. 2) (Camus et al. 2009). This hypothesis is supported by the analysis of patients who were metastatic at the time of diagnosis and surgery, despite high tumor infiltration by memory T cells. Strikingly, even if the total numbers of memory T cells in these tumors were similar to those of tumors of patients with no metastasis, they lacked the effector/memory T cell subset (Camus et al. 2009). This observation provides a third indication of the need of a finely tuned immune pattern to control tumor spread and invasion.
Immune control of metastasis: Coordinated high T cell density in the CT and at its invasive margin controls metastatic cell dissemination. Four major immune profiles within primary tumors of colorectal cancers are found: (1) strong and coordinated immune response with memory Th1 and cytotoxic T cells control cancer metastasis (“Im4,” 10% relapse) (2) same conditions with additional angiogenesis which favors tumor cell dissemination (“Im3,” 50% relapse) (3) low coordination of the immune response (“Im2,” 50% relapse) (4) weak or low immune response and coordination (“Im0, Im1,” 80% relapse). Potential antitumor circulating memory T cells generated in the primary tumor may control metastatic cells and prevent recurrence after surgery
The identification of factors involved in shaping an efficient immune pattern was approached by using informatic tools and biomolecular networks (Bindea et al. 2009). Databases were explored looking for genes with the following characteristics: conserved genomic neighborhood, phylogenetic profiling, coexpression analysis, literature co-occurrence, and encoded proteins interactions with the subset of genes that had been experimentally shown to be associated with recurrence and DFS. The genes most highly predicted were those of specific chemokines (CX3CL1, CXCL10, CXCL9) and adhesion molecules. When tested on our series, their expression correlated with high densities of T cell infiltration and DFS (Mlecnik et al. 2010) (Fig. 2). In addition, the expression of relevant chemokine genes was associated with that of particular T cell receptor families which correlated with patient’s survival (Mlecnik et al. 2010) suggesting that specific T cells could be involved in disease control.
In addition, to enlighten some aspects of host–tumor interactions, the analysis of the immune contexture may also provide novel useful prognostic markers. As in all solid tumors, prognosis of colorectal cancer is currently defined by the TNM staging which describes tumor spread into the intestinal wall, the regional lymph nodes, and distant organs metastatic invasion (Greene and Sobin 2009). This staging system is crucial, particularly for patients with no detectable lymph node invasion (stage I and II) who are usually treated by surgery alone. However, 15–25% of these patients will relapse and may have benefited from adjuvant chemotherapy. We, thus, performed a study to determine if the immune pattern may help to discriminate between relapsing and nonrelapsing early stage patients. Based on our analyses of coordination of an efficient immune infiltrate, we defined an immune score (Im) on the basis of densities of CD8/CD45RO T cells in CT and IM zones. Thus, tumors with low CD8 T cells and low CD45RO T cells in CT and IM were classified Im0, tumors with high infiltrates of cells positive with one marker in one zone were classified Im1, and then Im2 and Im3 up to Im4 for tumors with high infiltrates of CD8 and CD45RO cells in both CT and IM. The analysis of 353 early-stage (stages I and II) colorectal cancers using the immune score revealed a highly significant correlation between DFS and OS and the immune scoring. Thus, patients with a low immune score (Im0) were of very bad prognosis (75% recurrence at 5-year), whereas patients with a high immune score (Im4) experienced a very low level of recurrence (5% at 5-year) and 86% remained alive. The immune scoring, that was significant over TNM staging, therefore provides a precise prognostic staging to predict recurrence and may therefore encourage to treat patients with low immune score with adjuvant therapies (Fig. 2) (Pagès et al. 2009).
3 Induction of Functionally Active Tertiary Lymphoid Structures in the Vicinity of Tumoral Beds as Potential Sites of “In Situ” Immune Reactions: The Example of Lung Carcinoma
Lung carcinoma is the first cause of death by cancer worldwide with an incidence of over 1.2 million cases/year and a death rate of c.a. 1.1 million cases/year. Curative treatment is surgical for early-stage cancers, followed or not by adjuvant radiotherapy and/or chemotherapy. Lung carcinoma develops in a context of chronic inflammation, in most cases induced by tobacco smoking, but also by asbestos, chronic pulmonary infections, or bronchial obstructive diseases. Lung is at the interface of airways, filtering polluants, bacteria, or viruses that create acute inflammation which may influence clinical outcome of established lung cancers. Lung carcinoma therefore represents a very suitable model to study immune-cancer cell interactions taking place in an adaptive and innate inflammatory microenvironment. A first cohort of 74 early-stage (T1 or T2, N0 or N1, M0) lung cancer patients, without any neo-adjuvant therapy, was analyzed for their immune contexture and the prognostic impact of various immune compartments. Lymphocytic infiltration was found to be a heterogeneously distributed variable between tumors and distributed, as in colorectal cancers, in the center, the IM, and in lymphoid islets adjacent to the tumor nests (Fig. 3a). In addition to T and B cells, we particularly analyzed the quantity and the distribution of DC subsets. The different populations of DC were found diversely located within the tumor. The CD1a+ Langerhans cells were scattered inside the tumor beds showing tight functions with cancer cells, whereas the CD14+/− CD68low Factor XIIIa+ interstitial DC slipped into the interstices of tumor cells and CD123+ plasmacytoid DC concentrated at the IM of tumor nodules. Intratumoral DC were in an immature stage since they lacked the expression of the maturation markers DC-Lamp and CD83. Mature DC-Lamp+ cells were found only in the lymphoid islets adjacent to the tumor nests. The extremely low number of DC in nontumoral lung suggests that factors produced by the tumor microenvironment allow the recruitment of DC precursors into the tumor bed without inhibiting their differentiation or maturation. A careful analysis of these lymphoid islets revealed that they resemble canonical secondary lymphoid structures with a T cell zone containing the mature DC in close contact with T cells (Fig. 3b), and a B-cell follicle characterized by the presence of proliferating Ki67+ B cells and the presence of CD21+ follicular DC network (Dieu-Nosjean et al. 2008; Kawamata et al. 2009). These lymphoid islets have therefore the characteristics of functionally active TLS where an ongoing immune reaction takes place. Similar structures have been described in the lungs of human fetuses and infants (Gould and Isaacson 1993) and disappear in normal adult lungs (Tschernig and Pabst 2000). They have been called Bronchus-Associated Lymphoid Tissues (BALT) and, in adults, they reappear in inflammatory lung diseases, such as fibrosis, pneumonia, pneumonitis, or smoking. In patients with tumors, we searched for the presence of TLS at a distance from the tumor and rarely found any. We therefore propose that they are induced by the tumor or the tumor-associated inflammation and call them tumor-induced BALT (Ti-BALT). It is tempting to postulate that Ti-BALT are a location where an efficient immune reaction is shaped before, or in addition to, a response in the draining lymph nodes, where it could be subverted by metastatic cell establishment. Indeed, immune subversion or suppression must be postulated to explain why lymph nodes are the first metastatic sites and why invasion of the sentinel lymph node is a strong deleterious prognostic factor despite the fact that it should be the site of an intense immune reaction. There are indeed examples of immune responses that are not dependent on secondary lymphoid organs. For example, splenectomized alymphoblastic mice can reject xenografts (Tesar et al. 2004), clear viral infections (Moyron-Quiroz et al. 2004), or develop an allergic response (Gajewska et al. 2001; Halle et al. 2009). If Ti-BALT are sites where an efficient tumor-associated immune response is generated, they should be associated with relevant immune cell infiltration and impact cancer prognosis. Indeed the density of Ti-BALT is heterogeneous between tumors, some presenting with high densities, others with low. We took advantage of the fact that Ti-BALT were the only sites where mature DC-Lamp + DC were present to precisely assess the density of DC-Lamp+ cells as a surrogate marker for Ti-BALT. We established that there was a strong correlation between the number of Ti-BALT and that of DC-Lamp+ DC in the same fields. We, then, correlated the density of mature DC to other immunological and clinical parameters. The density of mature DC, T, and B lymphocytes correlated with each other. A precise analysis of correlations between high and low DC-Lamp densities and intra-tumoral lymphocyte populations revealed a significant positive correlation with T cell infiltration in CT and IM of the tumors, as well as with T cells with Th1 orientation (T-bet positive). Interestingly, a strong correlation was also found with B cell infiltration in CT and IM and the potential significance of this observation is currently under investigation. In contrast, there was no correlation between high and low DC-Lamp density and clinical parameters such as gender, age, smoking history, histological type (adenocarcinoma or squamous cell carcinoma), histopathological staging (T1, T2, N0, N1), or tumor differentiation. When the patients’ cohort was followed for DFS and OS over a period of 4 years, the DC-Lamp+ DC density strongly correlated with a favorable clinical outcome. Thus, DFS was 88% in patients with high DC-Lamp+ DC infiltration versus 51% in patients with low DC-Lamp+ DC density (Dieu-Nosjean et al. 2008). It was even more striking when DSS with 95% of patients not dying from their cancer in DC-Lamp high tumors compared to 45% in DC-Lamp low tumors (Fig. 3c).
Characterization of Ti-BALT in NSCLC: Presence of Ti-BALT (arrow) in lung tumor section counterstained with hematoxylin and eosin (a). DC-Lamp+ mature DC (red) home exclusively into CD3+ T –cell (blue) rich area of Ti-BALT (b). Kaplan-Meier curves of disease-specific survival (Log-rank test) for 74 patients with early-stage NSCLC according to the density of tumor-infiltrating mature DC-Lamp + DC (c). Original magnification: A, ×100; B, ×200. T, tumor nest
These data confirm the observations in colorectal cancer and extend them by showing that TLS adjacent to, and potentially induced by, the tumor could be the first sites of shaping an efficient antitumor reaction. The interaction of mature DC with T cells may result in the generation of memory T cells some with cytotoxic efficiency, that prevent potentially metastatic cells to leave the primary tumor. There may also be sites where circulating memory T cells are generated that are long lived and may control cancer cells disseminating in the periphery (blood, bone narrow) or when they search nidation in distant organs. Finally, the density of mature DC may identify patients with early-stage lung cancer with high risk of relapse.
4 Subversion of Innate Immunity Receptors: Stimulation of Toll Like Receptors on Lung Carcinoma Cells Modulates Cell Survival and Response to Chemotherapy
Lung being a site of frequent inflammation and lung cancers often developing in a context of chronic inflammation, we investigated the presence and the role of Toll Like Receptors (TLR) on lung cancer specimens from Non Small Cell Lung Cancer (NSCLC) patients. TLR are pattern recognition receptors for pathogen-associated molecular patterns (PAMP) and endogeneous molecules released from injured and necrotic cells (DAMP) (Kumar et al. 2009). Lungs are frequently exposed to viruses such as influenza or respiratory syncitia virus, that are mainly recognized by endogenous TLR3, 7 and 8 (Kumar et al. 2009). Among the 11 different TLR described to date, we thus focused our study on TLR7 and TLR8, receptors for ssRNA (Diebold et al. 2004; Heil et al. 2004) and to a minor extent on TLR3, receptor for dsRNA (Liu et al. 2008). The stimulation of TLR7, TLR8, and TLR3 that are commonly expressed by cells of the immune system leads to the activation of NFΚΒ and the production of proinflammatory cytokines (Napolitani et al. 2005; Hart et al. 2005; Larangé et al. 2009). It induces a rapid antiviral response via the induction of type I and type II IFN which in turn enhance the adaptive immune response. Imiquimod, a TLR7 agonist is currently used topically to treat basal cell carcinoma (Tillman and Carroll 2008) or systemically in clinical trials in melanoma as immuno-stimulants and vaccine adjuvants (Dudek et al. 2007). We observed by immunohistochemistry that immune cells infiltrating NSCLC express TLR7 and TLR8 in situ, particularly within the TiBALT (Cherfils-Vicini et al. 2010).
An increasing body of evidence suggest that TLR are also expressed by nonimmune cells such as epithelial cells (Droemann et al. 2003; Tissari et al. 2005; Gribar et al. 2008) and therefore can maintain local inflammation during chronic infections. In agreement with these observations, we have detected that bronchial epithelial cells but not alveolar cells express TLR7 and TLR8 on nontumoral lung tissue sections (Cherfils-Vicini et al. 2010). Therefore, TLR7 and TLR8 may be one of the first line of defense against viruses in bronchial epithelium.
However, a close immuno-histochemical examination of tumor cells in NSCLC sections revealed that they expressed TLR7 and TLR8, at variable levels, regardless of their histological type, adenocarcinoma or squamous cell carcinoma. A first analysis of 13 tumors (8 adenocarcinoma and 5 squamous cell carcinoma) showed that all expressed TLR8 but in variable quantities; two-thirds of them were TLR7 positive, half being highly labeled. This heterogeneous expression of TLR7 and TLR8, receptors for single stranded RNA, suggested that high expressing and low expressing tumors may behave differently in the case of viral infections, or in the presence of endogenous ligands for these TLR, which could be released in the tumor microenvironment. To determine which effect could be induced by TLR7 and TLR8 triggering, we used two model cell-lines, A549 as a prototype of adenocarcinoma and SK-MES as prototypic of squamous cell carcinoma, that express TLR7 and 8. Triggering of both cell lines by Loxoribine (a TLR7 agonist), poly U (a TLR8 agonist), or gardiquimod (an agonist of both) resulted in better cell survival due to resistance to apoptosis, as assessed by a strong induction of expression of the antiapoptotic gene and protein, Bcl-2. Triggering of A549 or SK-MES by TLR7 and TLR8 agonists also induced the modulation of other genes (up regulation of CCR4 and down regulation of CD80, CD86, HLA-DR, and Fibronectin 1) which are often associated with an aggressive tumoral phenotype. The analysis of genes expressed in tumoral cells isolated from fresh tumor specimen showed that tumor cells had a transcription pattern similar to that of cell lines triggered through TLR7 and 8, suggesting that they were in an activated state in situ (Cherfils-Vicini et al. 2010).
Some patients with lung cancer are treated by neo-adjuvant polychemotherapy, consisting in platinum salts and often gemcitabine or navelbine. Both A549 and SK-MES cells stimulated by Loxoribin or Poly U were found to be resistant to chemotherapy-induced cell death. It is therefore tempting to postulate that tumoral cells which express TLR7 or TLR8 at high levels could be stimulated upon viral induced inflammation and become resistant to chemotherapy (Cherfils-Vicini et al. 2010). We are currently analyzing a cohort of lung cancer patients having received neo-adjuvant chemotherapy before surgical resection in order to assess whether high TLR7 or TLR8 expressors are less susceptible to chemotherapy than low expressors. If it were so, it would provide a novel mechanism by which tumor cells gain growth and spreading advantages, i.e., resistance to apoptosis, to chemotherapy, expression of chemokine receptors, loss of Fibronectin 1, etc. It also calls some warning on the use of TLR7 agonists as adjuvants in cancer treatment, prompting to characterize the expression of TLR7 on the tumor cells before treatment by TLR agonists. Several reports describe the expression of TLR 4 and TLR9 in lung carcinoma (Droemann et al. 2005; He et al. 2007; Ren et al. 2009). TLR expression by tumor cells of nonhematopoietic origin appears to be quite a general phenomenon as TLR2, TLR3, TLR4, TLR5, and/or TLR9 expressions have been documented in many cancer types (reviewed in Sato et al. 2009). In most cases TLR activation of cancer cells promotes survival, activates production of proinflammatory cytokines and chemokines, promotes angiogenesis, and therefore contributes to cancer progression. However, the response to TLR3 seems more complex and can induce opposite effects depending on the cell type. TLR3 ligation by Poly IC or Poly AU on breast cancer cells induces apoptosis in an IFNα dependent manner (Salaun et al. 2006; André 2005). In melanoma a proapoptotic response has been described in the presence of Poly IC as well as the induction of NFκΚB and production of proinflammatory cytokines (Salaun et al. 2007). We observed that the triggering of TLR3 induced apoptosis of A459 cells whereas it promoted survival of SK-MES cells. Moreover, in some cases the addition of Poly IC to chemotherapy increased sensitivity to chemotherapy-induced cell death. (Cherfils-Vicini et al. 2010).
The fact that TLR stimulation regulates cell survival and modulates their sensitivity to chemotherapy reinforces the importance of TLR expression status on tumor cells in patient’s response to treatments.
5 “Paradoxical” Control of Inflammation Influences Clinical Outcome in Head and Neck Cancer
Head and neck cancers are a group of diseases affecting all sites of the upper respiratory tract, from the oral cavity to the larynx, through the oropharynx, the hypopharynx, and the epilarynx. Tobacco, synergized by alcohol, being the main causal factor, head and neck cancers have a higher incidence in males. Human papilloma viruses (HPV) have also been implicated in the genesis of these tumors. In any case, they develop in a context of chronic inflammation which usually persists during the clinical stage of the cancer. Classical treatment consists of surgical resection accompanied by radio/chemotherapy. However, despite new treatment modalities and their success in terms of organ preservation, survival rates have not improved over recent years.
Head and neck squamous cell carcinoma have quite intensively been investigated and the strong inflammatory component of these tumors is well established. In addition to macrophages, there exist, in some tumors, strong T lymphocyte infiltrates with all components of an adaptive immune reaction, i.e., CD3, CD4, and CD8 ; they are likely to control some aspects of tumor spreading, leading to recurrence and ultimately to death. In a first part of our studies, we tackled the question of cytokines that maintain and activate T cell functions. Two cytokines are major players in this prospect: IL-2 and IL-15 (Waldmann 2006). The latter appeared to be of particular interest in the context of head and neck tumors as it is not only critical for “in vivo” T cell survival and function but is also a strong inducer of inflammatory cytokines such as IL-6, TNFα, IL-17, etc. (Ohteki et al. 2006). We became interested by what appeared to be an IL-15 paradox: in mice models, IL-15 behaves as an antitumoral factor as it activates antitumoral CD8 and NK cells (Yajima et al. 2002; Kobayashi et al. 2005), rescues CD8 T cells from tolerance to leukemic cells (Teague et al. 2006), or improves the antitumoral activity of passively transferred CD8 T cells (Klebanoff et al. 2004). However, in humans, high intratumoral expression of IL-15 is associated with poor clinical outcome in lung (Seike et al. 2007) and head and neck (Nguyen et al. 2007) carcinomas.
IL-15 binds with high affinity to the IL-15 receptor (IL-15R)α chain, which associates with the IL-2 receptor (IL-2R)β and IL-2Rγ chains to tranduce IL-15 signaling. The trimeric receptor is therefore similar to the complex involved in IL-2 signaling where CD25 (IL-2Rα) would be the IL-2 specific counterpart of IL-15Rα. We had previously reported in a large cohort of 234 head and neck cancers that high serum levels of soluble IL-2R (sCD25) correlated with poor prognosis, both at the local regional level (control of recurrence) and for OS (Tartour et al. 2001). We measured levels of sIL-15R in the sera from 53 head and neck patients and compared them to that found in sera from 40 healthy individuals. We found significant quantities of circulating IL-15Rα in 66% of patients sera compared to very low levels, except one case, in sera from normal individuals. Interestingly, serum levels of sIL-15R had a clinical impact: patients with no circulating sIL-15Rα had a significantly longer recurrence free survival and OS than patients with circulating sIL-15R. What could be the underlying mechanisms by which sIL-15R exert its deleterious impact? To address this question, we analyzed IL-15Rα in head and neck tumors. Seventeen out of 48 tumors expressed IL-15Rα whereas normal epithelial cells did not. They also expressed ADAM-17 a protease that cleaves membrane associated IL-15Rα to produce soluble receptor. There was indeed a correlation between the expression of ADAM-17 by tumor cells and serum levels of IL-15Rα. It is therefore likely that sIL-15Rα is produced by the tumor cells. Is it only a marker of tumor mass or does it perform biological functions that could explain its prognostic impact? We produced recombinant sIL-15Rα that we added to IL-15 to measure its effects on IL-15 mediated activities. To our surprise, sIL-15Rα did not act as a decoy receptor, but greatly synergized IL-15 induced production of IL-6, TNFα, and IL-17 by human peripheral blood mononuclear cells. It also increased IL-15, but not IL-2, induced CD8 proliferation. We propose that, with other pro-inflammatory components, the pro-inflammatory effect of the IL-15/sIL-15Rα complex dominates over that of the CD8 activation at the tumor site and entertains the bed for local tumor recurrence (Badoual et al. 2008).
Due to the high inflammatory content of head and neck tumors, it is possible that the lymphocytic infiltrates have no clinical impact, either because they are anergic or apoptotic or because they are overcome. We revisited various aspects of T cell infiltration in a cohort of 84 head and neck patients with squamous cell carcinoma in which the tumor had been resected. In contrast to colorectal cancer for example, we found no prognostic impact of the number of CD8 T cells. When infiltrating CD4 T cells were enumerated, we found large numbers in 60% of the tumors. In view of their heterogeneity, we counted CD4+CD25+, CD4+CD69+, and CD4+Foxp3+ cells. Multivariate Cox analysis of histopathological (T stage) and immune (CD4+CD69+ and CD4+Foxp3+) markers revealed that CD4+Foxp3+ was associated with lack of local recurrence but not OS whereas CD4+CD69+ correlated with good survival but not local control (Badoual et al. 2006). This contrasts with a deleterious reported impact of the number of Foxp3+ cells (Curiel et al. 2004; Hiraoka et al. 2006; Fu et al. 2007).
Such a “paradoxical” beneficial effect of Treg (or at least Foxp3 positive T cells) has also been reported in colorectal cancer in man (Salama et al. 2009) and on the induction of colon cancer (Erdman et al. 2003, 2006) or spontaneous intestinal adenoma (Erdman et al. 2005) in mice. It is striking that the tumors in which Foxp3 positive T cells have been reported to be of favorable prognosis are highly inflammatory. We think that the overall interpretation of these data is that in inflammatory tumors, high numbers of infiltrating Treg are beneficial in terms of local control by their anti-inflammatory activities whereas activation of a tumor specific memory CD8 T cell response is necessary to control metastatic spread and OS (Badoual et al. 2009) (Fig. 4).
Paradoxical effects of Treg: Treg are of good prognosis (on the left) in inflammatory tumors when they inhibit the protumoral effect of inflammation mediated by protumoral cytokines such as IL-6, IL-17, TNF, and IL-15/sIL-15R. Treg are of bad prognosis (on the right) when they inhibit the tumor specific memory CD8 T cells necessary to control metastatic spread and overall survival
In fact, inflammation and immunosuppression are often associated in the tumor microenvironment. For example the proinflammatory cytokine IL-6 in conjunction with TGFβ permits the differentiation of Th17 cells (Wilson et al. 2007) which amplifies local recruitment of inflammatory cells (Ciree et al. 2004) and the production of other inflammatory mediators. However, IL-6 will also activate STAT3, a transcription factor overexpressed in 58.9% of head and neck tumors (Nagpal et al. 2002). Other factors, upregulated in head and neck cancer (IL-10, VEGF…), could also increase the expression of STAT3. Activation of STAT3 will be responsible for various immunosuppressive activities such as the blockade of DC maturation and the release of IL-10, which inhibits T cell and macrophage activation and downregulates HLA expression (Kortylewski and Yu 2008).
Other inflammatory cytokines (TNFα, IL-1…) will induce cyclooxygenase 2 (COX-2) that converts arachidonic acids to PGE2, a prostaglandin responsible for various immunosuppressive activities. Indeed, PGE2 has been reported to enhance IL-10 production, down-regulate DC function and inhibit IL-12 production in DC (Harizi et al. 2002). PGE2 facilitates the expansion of FoxP3+CD4+CD25+ naturally occurring regulatory T (nTreg) cells (Baratelli et al. 2005) and the induction of IL-10 producing CD4+ type 1 regulatory T (Tr1) cells in a COX-2–positive microenvironment (Akasaki et al. 2004; Bergmann et al. 2007). It is therefore tempting to postulate that the beneficial effects of anti-inflammatory compounds such as aspirin or Cox2 inhibitors in the prevention of human cancers, particularly colorectal cancer, may be not only the consequence of blockade of the well-known pro-tumoral effects of inflammation but also in part by “cooling” the tumor microenvironment, allowing a diluted or inhibited local immune reaction to control the tumor.
6 The Immune Reaction in a Tumor Developing in an Immuno-Priviledged Site: The Case of Primary Intraocular Lymphoma
The eye is considered to be an immunological sanctuary lacking any inflammatory and lymphocytic infiltration in its physiological state. In contrast, the vitreous cavity naturally contains immunosuppressive molecules such as TGFβ or VIP which are believed to suppress any attempt of potential immunological aggression. In pathology, the eye may be the site of an intense inflammation such as in uveitis, origin of which can be infectious or autoimmune (Bodaghi 2005; Mochizuki 2009).
Some tumors can develop in the eye, among which are retinoblastoma, choroïd ocular melanoma, and primary intraocular lymphoma (PIOL). PIOL is a rare disease from the group of Diffuse Large B-cell Lymphoma (DLCBL) and is usually called “uveitis masquerade syndrome” as it frequently displays misleading symptoms with forms of infectious uveitis. PIOL is genetically very similar to central nervous system lymphoma of other locations such as intra-cerebral, spinal cord, and lepto-meningeal lymphomas. Like other tumors developing in immune-privileged sites or in immune-compromised individuals, PIOLs are very aggressive with a 5-year survival rate of less than 5%. In addition, PIOLs have very peculiar invading characteristics with 85% developing cerebral lymphoma and 80% metastasing to the controlateral eye (Nussenblatt et al. 2006). The question therefore arose to the existence of immune surveillance toward PIOL in the eye. The presence of T cells in tumoral eyes has been reported and we confirmed this point. On measuring the cytokine levels in the vitreous humor from 17 PIOL patients, high levels of IL-10 were detected mainly produced by the B cell lymphomatous cells as previously reported since IL-10 levels are considered as a diagnostic marker for PIOL (Cassoux et al. 2007). We found low levels of IFNγ but no evidence for a local IL-2 and IL-4 production (Fig. 5). The presence of IFNγ and the lack of IL-2 support the hypothesis of an ongoing impaired Th1 reaction in the tumoral eye. In view of the prognostic impact of a strong “in situ” Th1 infiltration in many tumors, as discussed above, we investigated more thoroughly the immune reaction in the eyes with PIOL. Owing to the scarce quantities obtained after surgical vitreous biopsy of human PIOL, we established a murine model of PIOL in which one eye of BALB/c mice was intravitreally injected with murine B lymphoma IIA1.6 cells (Touitou et al. 2007). As a control, PBS was injected in the eyes of naïve mice. The tumor cells progressively invaded and filled the whole posterior chamber. The tumoral and control eyes were surgically removed at day 19 and dissected for functional studies. Firstly, we observed a progressive increase of T cells, both CD4 and CD8 in the tumoral eyes. No T lymphocytes were found in the control eyes. Secondly, when living cells were incubated in medium for 36 h, IL-10 (produced by the lymphomatous cells; data not shown) and small amounts of IFNγ were detected, but no IL-2 or IL-4, mimicking the human situation (Fig. 5). Polyclonal T-cell stimulation using anti-CD3/CD28 antibodies resulted in the induction of IL-2 secretion, a high increase of IFNγ but did not allow IL-4 detection in the supernatants. Conversely, LPS had little effect on lymphocyte-produced cytokines, but highly increased the production of inflammatory (IL-6 and TNFα) cytokines (data not shown). Our mouse model confirmed the human situation showing that an impaired Th1 response is present in PIOL tumoral eyes, and can be rescued by proper T cell stimulation (anti-CD3/CD28). We question the possible reason for this impaired reaction by searching for regulatory T cells. We indeed found CD4+CD25+FoxP3+ cells in tumoral eyes of PIOL mice and not in the PBS control eyes. Interestingly, there was a strong correlation between the number of intratumoral Treg and the number of tumoral B cells in the eye. Although, the total number of CD4 and CD8 T cells also increased with time, there was no correlation with the number of tumoral B cells (unpublished data). This observation suggests that in an immunopriviledged site, physiologically prone to suppression, there may be a major role for Treg in promoting tumor growth by impairing potentially efficient immune reactions.
Cytokine profile in eyes with intraocular lymphoma and influence of T-cell stimulation on cytokine secretion: (a) 25 µL of vitreous humor from patients with nonhaemorrhagic retinal detachment (RD) or primary intraocular lymphoma (PIOL) was subjected to IL-2, IFNγ and IL-4 measurement using a human (hu) Cytometric Bead Array Flex (BD Biosciences), according to the manufacturer’s instructions. (b) 100,000 murine ocular cells obtained from PBS (filled dots) or IIA1.6-GFP (open dots) injected eyes were cultured in medium alone, or stimulated in vitro with anti-CD3ε and anti-CD28 mAbs (BD Biosciences). After 36 h, culture supernatants were assayed for IL-2, IFNγ, and IL-4 using a mouse (mu) Cytometric Bead Array Flex (BD Biosciences), according to the manufacturer’s instructions. Each dot corresponds to the result of an individual eye and the horizontal black bars symbolize the mean of the respective results. The dashed lines represent the baseline of detection for each cytokine
7 Conclusions
Through different examples drawn from our analyses of human tumors, we propose a few rules emerging to understand host−tumor interactions. We first believe that the microenvironmental immune reaction is essential in the natural history of a cancer. A strong Th1/cytotoxic memory T cell infiltrate, correctly located in tumoral territories is needed to control evading potential metastatic cells. The reaction needs to be coordinated and is influenced by other microenvironmental factors such as VEGF which induces a strong neovascularization but also acts as an immunosuppressive factor by blocking DC maturation thus favoring Treg production. A relevant adaptive immune reaction may be shaped in the draining lymph nodes but even more accurately in TLS adjacent to the tumor beds which behave as tertiary lymphoid organs. In these structures where mature DC interact with T cells and follicular DC with proliferating B cells, efficient memory T cells, both CD4 and CD8, are educated and may infiltrate the tumor to keep metastasis on hold. It is also possible that some educated memory T cells leave into the periphery where they control metastatic cells that have escaped the primary tumor, which explains the strong prognostic value of T memory cells and TLS on OS. In particular situations, such as highly inflammatory tumors or tumors developing in immunopriviledged sites, Treg may have a strong impact by diminishing inflammation or impairing immune responses. In case of inflammation decreased by Treg, one would expect a strong positive effect of Treg locally, rather than on distant metastasis, as is the case in head and neck cancer. Finally, a good knowledge of the complex tumor-immune cell interactions “in situ” provides excellent prognostic markers and therapeutic avenues. In this respect, it is of interest that efficient antiangiogenic therapy correlates with a decrease of Treg in responding patients (Adotevi et al., submitted). Tools now exist and time has come for a routinely adapted analysis of the intratumoral immune reaction, in addition to the classical tumor-associated markers, in clinical human cancers.
References
Akasaki Y, Liu G, Chung NH, Ehtesham M, Black KL, Yu JS (2004) Induction of a CD4+ T regulatory type 1 response by cyclooxygenase-2-overexpressing glioma. J Immunol 173:4352–4359
Badoual C, Hans S, Rodriguez J, Peyrard S, Klein C, Agueznay Nel H, Mosseri V, Laccourreye O, Bruneval P, Fridman WH, Brasnu DF, Tartour E (2006) Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin Cancer Res 12:465–472
Badoual C, Bouchaud G, Agueznay Nel H, Mortier E, Hans S, Gey A, Fernani F, Peyrard S, -Puig PL, Bruneval P, Sastre X, Plet A, Garrigue-Antar L, Quintin-Colonna F, Fridman WH, Brasnu D, Jacques Y, Tartour E (2008) The soluble alpha chain of interleukin-15 receptor: a proinflammatory molecule associated with tumor progression in head and neck cancer. Cancer Res 68:3907–3914
Badoual C, Hans S, Fridman WH, Brasnu D, Erdman S, Tartour E (2009) Revisiting the prognostic value of regulatory T cells in patients with cancer. J Clin Oncol 27:e5–e6, author reply e7
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545, Review
Baratelli F, Lin Y, Zhu L, Yang SC, Heuze-Vourc'h N, Zeng G, Reckamp K, Dohadwala M, Sharma S, Dubinett SM (2005) Prostaglandin E2 induces FOXP3 gene expression and T regulatory cell function in human CD4+ T cells. J Immunol 175:1483–1490
Bergmann C, Strauss L, Zeidler R, Lang S, Whiteside TL (2007) Expansion of human T regulatory type 1 cells in the microenvironment of cyclooxygenase 2 overexpressing head and neck squamous cell carcinoma. Cancer Res 67:8865–8873
Bindea G, Mlecnik B, Hackl H, Charoentong P, Tosolini M, Kirilovsky A, Fridman WH, Pagès F, Trajanoski Z, Galon J (2009) ClueGO: a Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics 25:1091–1093
Birkeland Sa, Hamilton-Dutoit S, Sandvej K, Andersen Hm, Bendtzen K, Møller B, Jørgensen Ka (1995) EBV-induced post-transplant lymphoproliferative disorder (PTLD). Transplant Proc 27:3467–3472
Bodaghi B (2005) New etiological concepts in uveitis. J Fr Ophtalmol 28:547–555
Burnet FM (1970) The concept of immunological surveillance. Prog Exp Tumor Res 13:1–27
Camus M, Tosolini M, Mlecnik B, Pages F, Kirilovsky A, Berger A, Costes A, Bindea G, Charoentong P, Bruneval P, Trajanoski Z, Fridman W-H, Galon J (2009) Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res 69:2685–2693
Cassoux N, Giron A, Bodaghi B, Tran TH, Baudet S, Davy F, Chan CC, Lehoang P, Merle-Béral H (2007) IL-10 measurement in aqueous humor for screening patients with suspicion of primary intraocular lymphoma. Invest Ophthalmol Vis Sci 48:3253–3259
Cherfils-Vicini J, Platonova S, Gillard M, Laurans L, Validire P, Caliandro R, Magdeleinat P, Mami-Chouaib F, Dieu-Nosjean MC, Fridman WH, Damotte D, Sautès-Fridman C, Cremer I (2010) Triggering of TLR7 and TLR8 expressed by human lung cancer cells induces cell survival and chemoresistance. J Clin Invest 120(4):1285–1297
Ciree A, Michel L, Camilleri-Broet S, Jean Louis F, Oster M, Flageul B, Senet P, Fossiez F, Fridman WH, Bachelez H, Tartour E (2004) Expression and activity of IL-17 in cutaneous T-cell lymphomas (mycosis fungoides and Sezary syndrome). Int J Cancer 112:113–120
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, Evdemon-Hogan M, Conejo-Garcia JR, Zhang L, Burow M, Zhu Y, Wei S, Kryczek I, Daniel B, Gordon A, Myers L, Lackner A, Disis ML, Knutson KL, Chen L, Zou W (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10:942–949
Dalerba P, Maccalli C, Casati C, Castelli C, Parmiani G (2003) Immunology and immunotherapy of colorectal cancer. Crit Rev Oncol Hematol 46:33–57
Diebold SS, Kaisho T, Hemmi H, Akira S, Reis e Sousa C (2004) Innate antiviral responses by means of TLR7-mediated recognition of single-stranded RNA. Science 303:1529–1531
Dieu-Nosjean MC, Antoine M, Danel C, Heudes D, Wislez M, Poulot V, Rabbe N, Laurans L, Tartour E, De Chaisemartin L, Lebecque S, Fridman Wh, Cadranel J (2008) Long-term survival for patients with non-small-cell lung cancer with intratumoral lymphoid structures. J Clin Oncol 26:4410–4417
Droemann D, Goldmann T, Branscheid D, Clark R, Dalhoff K, Zabel P, Vollmer E (2003) Toll-like receptor 2 is expressed by alveolar epithelial cells type II and macrophages in the human lung. Histochem Cell Biol 119:103–108
Droemann D, Albrecht D, Gerdes J, Ulmer AJ, Branscheid D, Vollmer E, Dalhoff K, Zabel P, Goldmann T (2005) Human lung cancer cells express functionally active Toll-like receptor 9. Respir Res 6:1
Dudek AZ, Yunis C, Harrison LI, Kumar S, Hawkinson R, Cooley S, Vasilakos JP, Gorski KS, Miller JS (2007) First in human phase I trial of 852A, a novel systemic toll-like receptor 7 agonist, to activate innate immune responses in patients with advanced cancer. Clin Cancer Res 13:7119–7125
Dunn GP, Koebel CM, Schreiber RD (2006) Interferons, immunity and cancer immunoediting. Nat Rev Immunol 6:836–848
Erdman SE, Poutahidis T, Tomczak M, Rogers AB, Cormier K, Plank B, Horwitz BH, Fox JG (2003) CD4+ CD25+ regulatory T lymphocytes inhibit microbially induced colon cancer in Rag2-deficient mice. Am J Pathol 162:691–702
Erdman SE, Sohn JJ, Rao VP, Nambiar PR, Ge Z, Fox JG, Schauer DB (2005) CD4+CD25+ regulatory lymphocytes induce regression of intestinal tumors in ApcMin/+ mice. Cancer Res 65:3998–4004
Erdman SE, Rao VP, Poutahidis T, Ihrig MM, Ge Z, Feng Y, Tomczak M, Rogers AB, Horwitz BH, Fox JG (2006) CD4(+)CD25(+) regulatory lymphocytes require interleukin 10 to interrupt colon carcinogenesis in mice. Cancer Res 63:6042–6050
Fu J, Xu D, Liu Z, Shi M, Zhao P, Fu B, Zhang Z, Yang H, Zhang H, Zhou C, Yao J, Jin L, Wang H, Yang Y, Fu YX, Wang FS (2007) Increased regulatory T cells correlate with CD8 T-cell impairment and poor survival in hepatocellular carcinoma patients. Gastroenterology 132:2328–2339
Gajewska BU, Alvarez D, Vidric M, Goncharova S, Stämpfli MR, Coyle AJ, Gutierrez-Ramos JC, Jordana M (2001) Generation of experimental allergic airways inflammation in the absence of draining lymph nodes. J Clin Invest 108:577–583
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Berger A, Camus M, Mlecnik B, Bruneval P, Molidor R, Cugnenc P-H, Trajanoski Z, Fridman WH, Pagès F (2006) Type, density, and location of immune cells within human colorectal tumors predicts clinical outcome. Science 313:1960–1964
Galon J, Fridman WH, Pages F (2007) The adaptive immunologic microenvironment in colorectal cancer: a novel perspective. Cancer Res 67:1883–1886
Gould SJ, Isaacson PG (1993) Bronchus-associated lymphoid tissue (BALT) in human fetal and infant lung. J Pathol 169:229–234
Greene FL, Sobin LH (2009) A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC. J Surg Oncol 99:269–272
Gribar SC, Anand RJ, Sodhi CP, Hackam DJ (2008) The role of epithelial Toll-like receptor signaling in the pathogenesis of intestinal inflammation. J Leukoc Biol 83:493–498
Halle S, Dujardin HC, Bakocevic N, Fleige H, Danzer H, Willenzon S, Suezer Y, Hämmerling G, Garbi N, Sutter G, Worbs T, Förster R (2009) Induced bronchus-associated lymphoid tissue serves as a general priming site for T cells and is maintained by dendritic cells. J Exp Med 206:2593–2601
Harizi H, Juzan M, Pitard V, Moreau JF, Gualde N (2002) Cyclooxygenase-2-issued prostaglandin e(2) enhances the production of endogenous IL-10, which down-regulates dendritic cell functions. J Immunol 168:2255–2263
Hart OM, Athie-Morales V, O'Connor GM, Gardiner CM (2005) TLR7/8-mediated activation of human NK cells results in accessory cell-dependent IFN-gamma production. J Immunol 175:1636–1642
He W, Liu Q, Wang L, Chen W, Li N, Cao X (2007) TLR4 signaling promotes immune escape of human lung cancer cells by inducing immunosuppressive cytokines and apoptosis resistance. Mol Immunol 44:2850–2859
Heil F, Hemmi H, Hochrein H, Ampenberger F, Kirschning C, Akira S, Lipford G, Wagner H, Bauer S (2004) Species-specific recognition of single-stranded RNA via toll-like receptor 7 and 8. Science 303:1526–1529
Hiraoka N, Onozato K, Kosuge T, Hirohashi S (2006) Prevalence of FOXP3+ regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clin Cancer Res 12:5423–5434
Johnson B, Osada T, Clay T, Lyerly H, Aorse M (2009) Physiology and therepeutics of vascular endothelial growth factor in tumor immuno-suppression. Curr nol ned 9:702–707
Kawamata N, Xu B, Nishijima H, Aoyama K, Kusumoto M, Takeuchi T, Tei C, Michie SA, Matsuyama T (2009) Expression of endothelia and lymphocyte adhesion molecules in bronchus-associated lymphoid tissue (BALT) in adult human lung. Respir Res 10:97
Klebanoff CA, Finkelstein SE, Surman DR, Lichtman MK, Gattinoni L, Theoret MR, Grewal N, Spiess PJ, Antony PA, Palmer DC, Tagaya Y, Rosenberg SA, Waldmann TA, Restifo NP (2004) IL-15 enhances the in vivo antitumor activity of tumor-reactive CD8+ T cells. Proc Natl Acad Sci USA 101:1969–1974
Kobayashi H, Dubois S, Sato N, Sabzevari H, Sakai Y, Waldmann TA, Tagaya Y (2005) Role of trans-cellular IL-15 presentation in the activation of NK cell-mediated killing, which leads to enhanced tumor immunosurveillance. Blood 105:721–727
Koebel CM, Vermi W, Swann JB, Zerafa N, Rodig SJ, Old LJ, Smyth MJ, Schreiber RD (2007) Adaptive immunity maintains occult cancer in an equilibrium state. Nature 450:903–907
Kortylewski M, Yu H (2008) Role of Stat3 in suppressing anti-tumor immunity. Curr Opin Immunol 20:228–233
Kumar H, Kawai T, Akira S (2009) Toll-like receptors and innate immunity. Biochem Biophys Res Commun 388:621–625
Lamm DL (1992) Long-term results of intravesical therapy for superficial bladder cancer. Urol Clin North Am 19:573–580
Larangé A, Antonios D, Pallardy M, Kerdine-Römer S (2009) TLR7 and TLR8 agonists trigger different signaling pathways for human dendritic cell maturation. J Leukoc Biol 85:673–683
Lebel-Binay S, Berger A, Zinzindohoué F, Cugnenc P, Thiounn N, Fridman WH, Pagès F (2000) Interleukin-18: biological properties and clinical implications. Eur Cytokine Netw 11:15–26
Liu L, Botos I, Wang Y, Leonard JN, Shiloach J, Segal DM, Davies DR (2008) Structural basis of toll-like receptor 3 signaling with double-stranded RNA. Science 320:379–381
Mlecnik B, Tosolini M, Charoentong P, Kirilovsky A, Bindea G, Berger A, Camus M, Gillard M, Bruneval P, Fridman Wh, Pagès F, Trajanoski Z, Galon J (2010) Biomolecular network reconstruction reveals mechanisms of immune reaction associated with improved prognosis in colorectal cancer. Gastroenterology 138:1429–1440
Mochizuki M (2009) Regional Immunity of the Eye. Acta Ophthalmol, Nov 7, Epub ahead of print
Moyron-Quiroz JE, Rangel-Moreno J, Kusser K, Hartson L, Sprague F, Goodrich S, Woodland DL, Lund FE, Randall TD (2004) Role of inducible bronchus associated lymphoid tissue (iBALT) in respiratory immunity. Nat Med 10:927–934
Nagpal JK, Mishra R, Das BR (2002) Activation of Stat-3 as one of the early events in tobacco chewing-mediated oral carcinogenesis. Cancer 94:2393–2400
Napolitani G, Rinaldi A, Bertoni F, Sallusto F, Lanzavecchia A (2005) Selected Toll-like receptor agonist combinations synergistically trigger a T helper type 1-polarizing program in dendritic cells. Nat Immunol 6:769–776
Nguyen ST, Hasegawa S, Tsuda H, Tomioka H, Ushijima M, Noda M, Omura K, Miki Y (2007) Identification of a predictive gene expression signature of cervical lymph node metastasis in oral squamous cell carcinoma. Cancer Sci 98:740–746
Nussenblatt RB, Chan CC, Wilson WH, Hochman J, Gottesman M and the CNS and Ocular Lymphoma Workshop Group (2006) International Central Nervous System and Ocular Lymphoma Workshop: recommendations for the future. Ocul Immunol Inflamm 14:139–144.
O'Connell JB, Maggard MA, Ko CY (2004) Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst 96:1420–1425
Ohteki T, Tada H, Ishida K, Sato T, Maki C, Yamada T, Hamuro J, Koyasu S (2006) Essential roles of DC-derived IL-15 as a mediator of inflammatory responses in vivo. J Exp Med 203:2329–2338
Pagès F, Berger A, Henglein B, Piqueras B, Danel C, Zinzindohoue F, Thiounn N, Cugnenc PH, Fridman WH (1999) Modulation of interleukin-18 expression in human colon carcinoma: consequences for tumor immune surveillance. Int J Cancer 84:326–330
Pagès F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R et al (2005) Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med 353:2654–2666
Pagès F, Galon J, Fridman WH (2008) The essential role of the in situ immune reaction in human colorectal cancer. J Leukoc Biol 84:981–987
Pagès F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C, Fridman WH (2010) Immune infiltration in human tumors, a prognostic factor that should not be ignored. Oncogene 29:1093–1102
Pagès F, Kirilovsky A, Mlecnik B, Asslaber M, Tosolini M, Bindea G, Lagorce C, Wind P, Bruneval P, Zatloukal K, Trajanoski Z, Berger A, Fridman Wh, Galon J (2009) In situ Cytotoxic and Memory T Cells Predict Outcome in Early-Stage Colorectal Cancer Patients. J Clin Oncol 35:5944–5951
Ren T, Xu L, Jiao S, Wang Y, Cai Y, Liang Y, Zhou Y, Zhou H, Wen Z (2009) TLR9 signaling promotes tumor progression of human lung cancer cell in vivo. Pathol Oncol Res 15:623–630
Salama P, Phillips M, Grieu F, Morris M, Zeps N, Joseph D, Platell C, Iacopetta B (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 27:186–192
Salaun B, Coste I, Rissoan MC, Lebecque SJ, Renno T (2006) TLR3 can directly trigger apoptosis in human cancer cells. J Immunol 176:4894–4901
Salaun B, Lebecque S, Matikainen S, Rimoldi D, Romero P (2007) Toll-like receptor 3 expressed by melanoma cells as a target for therapy? Clin Cancer Res 13:4565–4574
Sato Y, Goto Y, Narita N, Hoon DS (2009) Cancer Cells Expressing Toll-like Receptors and the Tumor Microenvironment. Cancer Microenviron 2(Suppl 1):205–214
Seike M, Yanaihara N, Bowman ED, Zanetti KA, Budhu A, Kumamoto K, Mechanic LE, Matsumoto S, Yokota J, Shibata T, Sugimura H, Gemma A, Kudoh S, Wang XW, Harris CC (2007) Use of a cytokine gene expression signature in lung adenocarcinoma and the surrounding tissue as a prognostic classifier. J Natl Cancer Inst 99:1257–1269
Shankaran V, Ikeda H, Bruce AT, White JM, Swanson PE, Old LJ, Schreiber RD (2001) IFNgamma and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature 410:1107–1111
Smyth MJ, Dunn GP, Schreiber RD (2006) Cancer immunosurveillance and immunoediting: the roles of immunity in suppressing tumor development and shaping tumor immunogenicity. Adv Immunol 90:1–50
Tartour E, Gey A, Sastre-Garau X, Lombard Surin I, Mosseri V, Fridman WH (1998) Prognostic value of intratumoral interferon gamma messenger RNA expression in invasive cervical carcinomas. J Natl Cancer Inst 90:287–294
Tartour E, Mosseri V, Jouffroy T, Deneux L, Jaulerry C, Brunin F, Fridman WH, Rodriguez J (2001) Serum soluble interleukin-2 receptor concentrations as an independent prognostic marker in head and neck cancer. Lancet 357:1263–1264
Teague RM, Sather BD, Sacks JA, Huang MZ, Dossett ML, Morimoto J, Tan X, Sutton SE, Cooke MP, Ohlén C, Greenberg PD (2006) Interleukin-15 rescues tolerant CD8+ T cells for use in adoptive immunotherapy of established tumors. Nat Med 12:335–341
Tesar BM, Chalasani G, Smith-Diggs L, Baddoura FK, Lakkis FG, Goldstein DR (2004) Direct antigen presentation by a xenograft induces immunity independently of secondary lymphoid organs. J Immunol 173:4377–4386
Thaunat O, Hanf W, Dubois V, McGregor B, Perrat G, Chauvet C, Touraine JL, Morelon E (2009) Chronic humoral rejection mediated by anti-HLA-DP alloantibodies: insights into the role of epitope sharing in donor-specific and non-donor specific alloantibodies generation. Transpl Immunol 20:209–211
Tillman DK Jr, Carroll MT (2008) A 36-month clinical experience of the effectiveness of curettage and imiquimod 5% cream in the treatment of basal cell carcinoma. J Drugs Dermatol 7:s7–s14
Tissari J, Sirén J, Meri S, Julkunen I, Matikainen S (2005) IFN-alpha enhances TLR3-mediated antiviral cytokine expression in human endothelial and epithelial cells by up-regulating TLR3 expression. J Immunol 174:4289–4294
Touitou V, Daussy C, Bodaghi B, Camelo S, de Kozak Y, Lehoang P, Naud MC, Varin A, Thillaye-Goldenberg B, Merle-Béral H, Fridman WH, Sautès-Fridman C, Fisson S (2007) Impaired th1/tc1 cytokine production of tumor-infiltrating lymphocytes in a model of primary intraocular B-cell lymphoma. Invest Ophthalmol Vis Sci 48:3223–3229
Tschernig T, Pabst R (2000) Bronchus-associated lymphoid tissue (BALT) is not present in the normal adult lung but in different diseases. Pathobiology 68:1–8, Review
Van der Meer JW, Weening RS, Schellekens PT, van Munster IP, Nagengast FM (1993) Colorectal cancer in patients with X-linked agammaglobulinaemia. Lancet 341:1439–1440
Waldmann TA (2006) The biology of interleukin-2 and interleukin-15: implications for cancer therapy and vaccine design. Nat Rev Immunol 6:595–601, Review
Wilson NJ, Boniface K, Chan JR, McKenzie BS, Blumenschein WM, Mattson JD, Basham B, Smith K, Chen T, Morel F, Lecron JC, Kastelein RA, Cua DJ, McClanahan TK, Bowman EP, de Waal Malefyt R (2007) Development, cytokine profile and function of human interleukin 17-producing helper T cells. Nat Immunol 8:950–957
Yajima T, Nishimura H, Wajjwalku W, Harada M, Kuwano H, Yoshikai Y (2002) Overexpression of interleukin-15 in vivo enhances antitumor activity against MHC class I-negative and -positive malignant melanoma through augmented NK activity and cytotoxic T-cell response. Int J Cancer 99:573–578
Acknowledgments
This work was supported by grants from Association pour la Recherche sur le Cancer (ARC), National Cancer Institute (INCa), Canceropole Ile de France, Ville de Paris, Inserm, European Union (7FP, Geninca Consortium grant number 202230), Laboratoire Français de fractionnement et des Biotechnologies (LFB), and Pôle de Compétitivité Ile de France (Immucan). The authors wholeheartedly thank the doctoral and postdoctoral fellows, as well as the engineers and colleagues who performed the biological and statistical experiments: C. Badoual, G. Bindea, M. Camus, J. Cherfils, C. Daussy, L. de Chaisemartin, N. El Houda Afneznay, A. Gey, A. Kirilovski, C. Lagorce, L. Laurans, F. Marliot, B. Mlecnik, R. Molidor, F. Sandoval, M. Tosolini, V. Touitou, and Z. Trajanovski. They acknowledge the trustfull and enthusiastic collaboration with devoted and interactive clinicians and pathologists:M. Antoine, A. Berger, B. Bodaghi, D. Brasnu, P. Bruneval, J. Cadranel, N. Cassou, C. Danel, S. Hans, P. Le Hoang, H. Merle Béral, S. Oudart, P. Validire, P. Wind, and F. Zinzindouhé.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Fridman, W.H. et al. (2010). Immune Infiltration in Human Cancer: Prognostic Significance and Disease Control. In: Dranoff, G. (eds) Cancer Immunology and Immunotherapy. Current Topics in Microbiology and Immunology, vol 344. Springer, Berlin, Heidelberg. https://doi.org/10.1007/82_2010_46
Download citation
DOI: https://doi.org/10.1007/82_2010_46
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-14135-5
Online ISBN: 978-3-642-14136-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)