Abstract
Early adverse experiences are associated with heighted vulnerability for stress-related psychopathology across the lifespan. While extensive work has investigated the effects of early adversity on neurobiology in adulthood, developmental approaches can provide further insight on the neurobiological mechanisms that link early experiences and long-term mental health outcomes. In the current review, we discuss the role of emotion regulation circuitry implicated in stress-related psychopathology from a developmental and transdiagnostic perspective. We highlight converging evidence suggesting that multiple forms of early adverse experiences impact the functional development of amygdala-prefrontal circuitry. Next, we discuss how adversity-induced alterations in amygdala-prefrontal development are associated with symptoms of emotion dysregulation and psychopathology. Additionally, we discuss potential mechanisms through which protective factors may buffer the effects of early adversity on amygdala-prefrontal development to confer more adaptive long-term outcomes. Finally, we consider limitations of the existing literature and make suggestions for future longitudinal and translational research that can better elucidate the mechanisms linking early adversity, neurobiology, and emotional phenotypes. Together, these findings may provide further insight into the neuro-developmental mechanisms underlying the emergence of adversity-related emotional disorders and facilitate the development of targeted interventions that can ameliorate risk for psychopathology in youth exposed to early life stress.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Early life stress (ELS) is associated with higher incidence of mental health problems across the lifespan, accounting for 29% of health disorders worldwide [1,2,3]. Multiple forms of postnatal adversities confer vulnerability for stress-related psychopathology, including maltreatment, neglect, parental stress or psychopathology, trauma, family conflict, poverty-related stressors, and institutionalized care [3,4,5,6]. Although these adverse exposures often occur during infancy and/or childhood, emotional difficulties often continue to persist throughout development, with three quarters of stress-related mental health diagnoses made by the age of 24 [2, 7]. Given the robust epidemiological evidence linking ELS with long-lasting emotional difficulties, it is important to identify the neurobiological mechanisms through which early experiences “get under the skin” to increase risk for psychopathology.
Developmental mechanisms of adaptation play an important role in understanding the long-term links between ELS and mental health outcomes in adulthood. According to the Dynamic Systems Theory, development is experience-driven, emerging via interactions with the environment that unfold over time [8]. In the context of ELS, several developmental theories (Barker’s hypothesis, Developmental Origins Theory, Adaptive Recalibration Model, Experiential Canalization) emphasize the role of adaptation in response to adversity, such that the organism develops in order to promote survival in the expected environment [9,10,11,12]. Similarly, the Stress-Acceleration Hypothesis posits that neurobiological changes in response to early adverse experiences are adaptive in the short-term, but may have long-term trade-offs in the functional integrity of neuro-affective circuitry and heighten vulnerability for maladaptive mental health outcomes later in life [13].
In line with this developmental perspective, the current review will discuss how early adverse experiences influence neuro-affective development to confer risk for stress-related emotion dysregulation. We will delineate how the amygdala-prefrontal circuit, implicated in threat-reactivity and emotion regulation, appears to be particularly sensitive to the effects of stress during early life. The current paper focuses on the functional development of amygdala-prefrontal circuitry, as stress-induced changes in structural development have been reviewed elsewhere [14]. Specifically, we will highlight converging evidence suggesting that multiple forms of ELS are characterized by similar functional phenotypes of neuro-affective circuitry across development: (1) heightened amygdala reactivity and (2) altered amygdala-prefrontal connectivity. Next, we will discuss how developmental changes in amygdala-prefrontal circuitry predict individual differences in symptoms of stress-related psychopathology. Finally, we will discuss potential protective factors that may buffer the effects of stress on neuro-affective development to confer more resilient long-term trajectories. Given that ELS increases risk across several, often comorbid psychiatric disorders [3, 15], this paper will focus on the neurobiology of emotion dysregulation from a transdiagnostic and dimensional perspective.
2 Target Neural Circuitry: Amygdala and Prefrontal Cortex
2.1 The Role of Amygdala-Prefrontal Circuitry in Emotion Regulation
Robust translational and clinical research has linked amygdala-prefrontal circuitry with symptoms of emotion dysregulation [16]. In adults, regulatory connections between amygdala and prefrontal cortex are critically implicated in learning and responding to emotional cues in the environment [17, 18]. The amygdala is involved in detecting salient information in the environment to initiate physiological responses to potential threat [17]. Top-down recruitment of medial prefrontal regions regulates amygdala reactivity to facilitate extinction learning [19, 20] whereas dorsolateral prefrontal regions implicated in more effortful processes, like cognitive reappraisal, modulate amygdala reactivity during emotion regulation [21]. Functional alterations of amygdala reactivity and amygdala-prefrontal connectivity have been identified in patients with internalizing and stress-related disorders, including anxiety, depression, and PTSD [22,23,24]. In the Research Domain Criteria (RDoC) recently outlined by the National Institutes of Mental Health [25], amygdala-prefrontal circuitry has been implicated in the psychological constructs of fear and sustained threat, highlighting its role in the neurobiological underpinnings of transdiagnostic dimensions of threat-reactivity and emotion regulation [26].
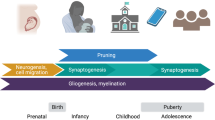
In humans, amygdala-prefrontal circuitry undergoes protracted development, with age-related changes observed across childhood, adolescence, and young adulthood. Several studies have observed heightened amygdala reactivity in response to emotionally salient cues in younger ages [27,28,29,30,31]. As amygdala reactivity declines with increasing age [27,28,29,30,31,32], the functional integrity of amygdala-mPFC circuitry continues to strengthen into young adulthood [33]. Importantly, age-related changes in amygdala reactivity and/or connectivity with the prefrontal cortex during cognitive reappraisal tasks correspond to the maturation of emotion regulation abilities across development [34,35,36]. Pediatric disorders of anxiety, depression, and PTSD are characterized by heightened amygdala reactivity and atypical amygdala-prefrontal connectivity during emotion processing tasks [37,38,39,40,41,42]. Moreover, altered patterns of age-related changes in amygdala-prefrontal connectivity have been shown in a cross-sectional sample of anxious youth and young adults [43] suggesting that deviations from the normative trajectory of amygdala-prefrontal development are associated with symptoms of emotional dysregulation in clinical samples.
2.2 Plasticity of Amygdala-PFC Circuitry in Early Life
Converging evidence across species suggests that amygdala-prefrontal circuitry is highly sensitive to environmental inputs, particularly during early life [44]. The amygdala is heavily innervated by glucocorticoid receptors [45], with the highest peak in corticotrophin releasing hormone (CRH) receptor density during the first few postnatal weeks [45]. Stress exposure during early life results in increased mRNA expression of CRH in the amygdala in rodents [46]. Importantly, the functional development of the amygdala is tightly linked to hypothalamic–pituitary–adrenal (HPA) axis function, such that increases in cortisol are associated with the developmental onset of amygdala reactivity and fear learning in rodents [47].
Several animal models of ELS (e.g., abusive maternal care, maternal separation, chronic restraint stress, and odor-shock conditioning) have shown that early adverse environments have enduring effects on amygdala structure and function [48,49,50]. Moreover, regulatory connections between amygdala and prefrontal cortex are highly susceptible to environmental influences during early life in rodent models. For example, chronic stress exposure during the juvenile stage causes dendritic atrophy in the prefrontal cortex (PFC; [48]) and alters the emergence of amygdala projections to the PFC, resulting in long-term imbalance of amygdala-prefrontal circuit function in adult rats [51]. In light of these findings, amygdala-prefrontal development may play an important role in the neurobiological etiology of emotion dysregulation in humans following ELS.
3 Effects of ELS on Amygdala-PFC Circuitry in Humans
When examining the effects of ELS on neurobiological development in humans, there are two important considerations that delineate the state of current research. First, aside from notable exceptions in which there is known timing and duration of adverse exposures (i.e., adoption from institutionalized care), many forms of ELS are chronic in nature, making it difficult to delineate the effects of stressors during specific time points across development (reviewed in [14]). Given cross-species evidence suggesting that amygdala development is most sensitive to environmental input early in life [44], the current review focuses on adverse experiences that occur during infancy and/or childhood. Second, recent theoretical frameworks have suggested that certain dimensions of adverse experiences (e.g., threat vs. deprivation) may have differential effects on neurobiological development [52]. Although early adversities are often complex exposures comprised of multiple dimensions of experience (e.g., abuse and neglect; [53]), many forms of ELS are considered threatening to children’s physical or emotional well-being [52]. In the current review, we focus on research examining threat-related alterations in neuro-affective development following exposure to ELS. Specifically, we present converging evidence suggesting that amygdala-prefrontal circuitry, implicated in threat-reactivity and emotion regulation, is a common neurobiological target impacted by multiple forms of early adverse experiences.
3.1 Effects of ELS on Amygdala Reactivity
In adults, heightened amygdala reactivity to emotional cues has been identified across several domains of ELS reported retrospectively, including maltreatment [54, 55] emotional neglect [56, 57], and lower perceived social status [58]. Recent prospective longitudinal studies have corroborated these effects, showing that cumulative childhood stressors associated with low socioeconomic status have lasting effects on amygdala function in adulthood [59, 60]. For example, childhood poverty has been associated with increased amygdala reactivity to negative relative to positive emotional cues in adulthood [60]. In the same prospective cohort, cumulative risk exposure associated with childhood poverty was directly related to higher amygdala reactivity to neutral facial expressions, suggesting that stress-related increases in amygdala reactivity may not be specific to threat-related stimuli, also extends to neutral socio-emotional cues [59].
In accordance with studies in adult ELS samples, children and adolescents with a history of early adversity also show enhanced amygdala reactivity to emotional stimuli. Previously institutionalized (PI) youth with a history of institutional care exhibit heightened amygdala reactivity to threat-related facial expressions across childhood and adolescence [61,62,63]. Similarly, increased amygdala response to negative emotional stimuli has been identified in children and adolescents with prior exposure to maltreatment [64, 65], traumatic events [66], and family violence [67]. Moreover, greater levels of stressful life events have been associated with longitudinal increases in threat-related amygdala reactivity during adolescence, suggesting that heightened amygdala reactivity may represent a neural marker of previous stress exposure [68]. Importantly, McCrory et al. [64] found that children with earlier onset of maltreatment exposure showed higher levels of amygdala reactivity to pre-attentively presented emotional stimuli, suggesting a relationship between the timing of stress exposure onset and degree of amygdala reactivity. However, further research is needed to delineate whether stress-induced increases in amygdala reactivity are primarily driven by the developmental timing (i.e., age of onset) or the duration (i.e., chronic versus acute) of adverse experiences.
3.2 Effects of ELS on Amygdala-PFC Connectivity
In addition to heightened amygdala-reactivity, ELS has also been characterized by altered functional connectivity of the amygdala with prefrontal regions. Although the valence (i.e., positive or negative) and regional specificity (i.e., dorsolateral or medial regions of PFC) of amygdala-prefrontal connectivity findings are task-dependent and often vary across studies, ELS has been consistently associated with atypical connectivity patterns relative to non-stressed control groups. In a prospective study, young adults with a history of childhood maltreatment showed atypical connectivity between the amygdala and inferior frontal gyrus when processing threat-related emotional stimuli [69]. Childhood poverty has also been associated with alterations of amygdala-prefrontal connectivity in adulthood, such that lower family income during childhood is associated with reduced amygdala-ventrolateral PFC (vlPFC) connectivity during cognitive reappraisal [70]. Importantly, cumulative stress exposure mediated the effects of family income on vlPFC recruitment during reappraisal, suggesting that associations between childhood poverty and prefrontal dysregulation are driven by effects of chronic stress [70]. Together, these findings suggest that heightened emotional reactivity following ELS may emerge from impaired top-down prefrontal regulation of amygdala reactivity in response to emotional cues.
Given that ELS is associated with atypical amygdala-prefrontal function in adulthood, recent research has examined how these adversity-induced changes emerge across development. In a cross-sectional study from early childhood to late adolescence, PI youth showed an atypical trajectory of age-related changes in threat-related amygdala-mPFC connectivity relative to comparison youth, such that PI youth exhibited more mature (i.e., adult-like) connectivity at younger ages [61]. Youth with trauma exposure also show atypical amygdala-prefrontal function in response to emotional distractors, with weaker negative connectivity between the amygdala and pregenual ACC (pgACC) relative to comparison youth [66]. Moreover, the strength of amygdala-pgACC connectivity predicted performance on the emotional conflict task, suggesting that impaired regulation of emotional distractors in trauma-exposed youth may be related to altered circuit function [66]. Similarly, PTSD youth exhibit weaker amygdala-dACC connectivity and atypical age-related changes in amygdala-mPFC connectivity in response to threat-related stimuli [42]. Importantly, the youth diagnosed with PTSD in this sample were exposed to a wide range of early adverse experiences (e.g., trauma, abuse, neglect; [42]), suggesting evidence of equifinality with regard to neuro-affective phenotypes following exposure to different forms of ELS [71].
In addition to changes in task-elicited functional connectivity, ELS has also been associated with weaker resting-state amygdala-prefrontal connectivity across developmental stages, suggesting that early adversity has long-lasting impacts on the functional integrity of emotion regulation circuitry. In adults, self-reported history of childhood trauma is associated with weaker resting-state connectivity between amygdala and pregenual ACC (pgACC; [72]). Similarly, adolescents who experienced childhood maltreatment [73] and youth with history of trauma exposure [74] show weaker amygdala-subgenual anterior cingulate cortex (sgACC) connectivity at rest. In a younger cohort of children and young adolescents, higher levels of cumulative stress during childhood predicted weaker amygdala-ACC connectivity [75]. Importantly, ELS-induced changes in amygdala connectivity may be identifiable as early as infancy. At 6 months of age, family stress, as defined by high levels of interparental conflict, is associated with altered patterns of resting-state amygdala connectivity with posterior cingulate cortex, a regional hub of the default mode network [76]. Although further research is needed to delineate how early alterations in amygdala connectivity influence longitudinal neuro-affective development, these findings highlight the potential role of amygdala connectivity as a neurobiological marker for stress vulnerability as early as the first year of life [77].
4 Amygdala-PFC Circuitry and Individual Differences in Psychopathology Following ELS
In the previous section, we presented evidence suggesting that there is some degree of equifinality in neurobiological development following ELS [71], such that different types of early adverse experiences have converging effects on the development of emotion regulation circuitry, resulting in atypical amygdala-prefrontal circuit function. However, there is also evidence of multifinality, such that there is wide heterogeneity in long-term mental health outcomes following ELS [71]. For example, similar adverse experiences (e.g., institutional care) confer risk for multiple types of psychopathology across individuals [5, 15, 71]. In the context of developmental theory (Adaptive Calibration Model, Experiential Canalization, and Stress Acceleration Hypothesis), environmentally driven changes in neurobiology represent an ontogenetic response to adversity, and may confer adaptive or maladaptive behavioral outcomes in specific domains or contexts across development [10,11,12,13]. Given the heterogeneity in mental health outcomes associated with ELS, it is important to consider how individual trajectories of neuro-affective development predict risk or resilience following exposure to early adversity. The following discussion will review recent evidence linking adversity-induced changes in amygdala-prefrontal function with individual differences in psychopathology (i.e., anxiety, depression, PTSD).
4.1 Amygdala Reactivity and Psychopathology
Individual differences in amygdala reactivity predict dimensional measures of emotional functioning in both typically developing and stress-exposed youth. In typical children and adolescents, increased amygdala reactivity to sad facial expressions predicts level of concurrent internalizing symptoms [30] and depressive symptoms [78]. Youth with trauma exposure and post-traumatic stress symptoms have shown greater amygdala reactivity to emotional facial expressions relative to non-exposed youth [38] although there are mixed findings [42, 79]. A recent study examined the interaction of early trauma exposure and psychiatric status on amygdala reactivity to emotional stimuli during childhood [80]. Amygdala response varied as a function of both early trauma and concurrent levels of psychopathology, such that children with trauma exposure and current diagnosis of major depressive disorder exhibited the greatest levels of amygdala reactivity [80]. Moreover, recent evidence suggests that heightened amygdala reactivity predicts long-term increases in negative affect in both healthy and depressed preschool children [81]. Together, these studies suggest that amygdala reactivity may represent a neural marker for current and/or future levels of stress-related psychopathology during childhood and adolescence. However, further longitudinal studies are needed to delineate the specific effects of different types of stressors on amygdala reactivity phenotypes and long-term mental health outcomes.
4.2 Longitudinal Studies of Amygdala-PFC Connectivity and Psychopathology
Recent longitudinal findings also suggest that atypical amygdala-prefrontal connectivity may represent a neurobiological risk factor for the emergence of psychopathology following ELS. In adolescents with a history of childhood maltreatment, the strength of resting-state amygdala-sgACC connectivity mediated the relationship between maltreatment exposure and internalizing symptoms, such that weaker amygdala-sgACC connectivity conferred higher levels of anxiety and depressive symptoms [73]. In a recent study of cumulative childhood stress, Pagliaccio et al. [75] examined the relationship between resting-state amygdala-ACC connectivity and longitudinal assessments of internalizing psychopathology in children. Similar to Herringa et al. [73], weaker amygdala-ACC connectivity mediated the effect of stressful and traumatic life events on current symptoms of anxiety. Moreover, amygdala-prefrontal connectivity and concurrent symptom levels were both significant predictors of anxiety symptoms one year later, providing longitudinal evidence that stress-related changes in the functional integrity of amygdala-prefrontal circuitry confer vulnerability for future stress-related psychopathology [75].
Given that amygdala functional development is tightly linked to the HPA axis [82], cortisol reactivity may play an important role in the developmental cascade linking neuro-affective changes to long-term mental health outcomes following ELS. In a long-term prospective study, Burghy et al. [83] examined the effects of cumulative maternal stress on cortisol levels during childhood and resting-state amygdala-prefrontal connectivity in late adolescence. Greater levels of maternal stress during the first year of life were associated with heightened baseline cortisol levels during childhood, suggesting a dose-dependent response in the HPA axis response to ELS [83]. Although maternal stress did not directly predict amygdala-ventromedial PFC (vmPFC) connectivity, higher childhood baseline cortisol levels were associated with altered resting-state amygdala-vmPFC connectivity in adolescent females. Moreover, the strength of amygdala-vmPFC connectivity mediated the relationship between heightened cortisol and symptoms of depression and anxiety in adolescent females, albeit in different directions. Specifically, weaker amygdala-vmPFC connectivity predicted greater symptoms of anxiety, while stronger connectivity predicted greater symptoms of depression, suggesting that divergent trajectories of amygdala-prefrontal development following ELS confer risk for different forms of internalizing psychopathology. Overall, this study provides longitudinal evidence across multiple-levels of analysis that stress-related changes in HPA-axis regulation are associated with atypical amygdala-prefrontal connectivity and heightened vulnerability for internalizing psychopathology following ELS.
4.3 Cross-Sectional Studies of Amygdala-PFC Connectivity and Psychopathology
Cross-sectional studies have examined the effects of ELS on age-related changes in the developmental trajectory of amygdala-prefrontal circuit function. PI youth with a history of orphanage care showed atypical age-related changes in task-elicited amygdala-mPFC connectivity in response to fearful faces [61]. In typically developing youth, children showed more positive amygdala-mPFC connectivity, whereas adolescents showed negative amygdala-mPFC connectivity. However, PI children showed more mature (i.e., negative) connectivity at earlier ages relative to age-matched comparisons. In line with previous literature [83], cortisol levels mediated the relationship between ELS and amygdala-mPFC connectivity, supporting the role of the HPA axis in stress-related changes in neuro-affective development [61]. Importantly, amygdala-mPFC connectivity predicted current levels of psychopathology in the PI group, such that more mature connectivity conferred lower levels of anxiety. In the context of the Stress Acceleration Hypothesis [13], these findings suggest that earlier functional maturation of this circuitry may represent an adaptive response to previous stress exposure that reduces vulnerability for emotion dysregulation. However, given the cross-sectional nature of this study, further longitudinal research is needed to delineate whether these early stress-induced adaptations predict risk or resilience in the long-term.
Atypical amygdala-prefrontal functioning has also been identified in a cross-sectional study of PTSD youth with a history of early adversity [42]. Specifically, threat-related connectivity between the amygdala and dACC/dmPFC predicted severity of avoidant symptoms in PTSD youth. Moreover, they identified altered patterns of age-related connectivity phenotypes in the PTSD group, such that amygdala-vmPFC connectivity increased with age in typically developing youth, but decreased with age in PTSD youth [42]. Similar to PI children [61], children with PTSD exhibited a more mature pattern of amygdala-vmPFC connectivity, suggesting a developmental adaptation to compensate for heightened emotional reactivity following ELS. However, adolescents with PTSD showed less mature amygdala-vmPFC connectivity relative to age-matched controls. When considering the Stress Acceleration Hypothesis, these findings suggest that early maturation of this circuitry following ELS may be adaptive during childhood, but may result in reduced functional maturity of the circuit during adolescence. Although it is possible that exposure to traumatic events at earlier vs. later stages of development (i.e., childhood vs. adolescence) may differentially alter neuro-affective development, there were no reported effects of duration-since-exposure of adversity, nor the length of PTSD diagnosis on amygdala-vmPFC connectivity in this study [42]. Although the observed age-related changes in amygdala-vmPFC connectivity were not directly associated with PTSD symptoms, these findings highlight the importance of examining developmental trajectories when considering the effects of ELS on amygdala-prefrontal function and emotional disorders.
5 Protective Factors and Neuro-Affective Development Following ELS
Although ELS is associated with a higher incidence of stress-related psychopathology, many individuals exposed to early adversity do not develop clinical disorders [84]. Moreover, individuals with history of ELS may show difficulties in specific domains of socio-emotional functioning (e.g., anxiety), but show competence in other domains (e.g., social skills; [85]). A broad literature on resilience has identified factors at both the individual level (e.g., cognitive factors) and environmental level (e.g., family, community) that contribute to individual differences in mental health and well-being following ELS [85, 86]. Given the evidence of multifinality following ELS, it is important to identify how protective factors influence neurobiological development to reduce risk for stress-related psychopathology [87, 88]. For the purposes of the current review, we will focus on protective factors of the social environment that may ameliorate the effects of ELS on neuro-affective development via social buffering.
In behavioral studies, quality caregiving and family stability have been consistently shown to promote more resilient long-term outcomes following exposure to early adversity (reviewed in [89]). For example, in the Bucharest Early Intervention Project (BEIP), youth with stable foster-care placements following institutional care showed lower levels of internalizing symptoms during early adolescence relative to those who experienced disruptions in foster care [5]. Importantly, the two groups did not differ in the amount of time spent in institutional care or psychiatric history at age 4, suggesting that the observed difference in adolescent levels of psychopathology occurred as a function of caregiver stability, as opposed to earlier levels of trauma exposure or psychopathology [5]. Similarly, longitudinal studies of childhood maltreatment have shown that family level protective factors, such as caregiving stability [90], perceived parental care [91], and parental warmth [92] are associated with reduced risk for future psychopathology. Together, these findings suggest that positive and stable caregiving is associated with lower levels of emotional problems following multiple forms of early adverse experiences.
In light of strong evidence linking caregiver support and mental health outcomes, ample research has focused on identifying the neurobiological mechanisms underlying these social buffering effects [93, 94]. Evidence across species has shown that caregivers regulate emotional and neurobiological development (reviewed in [44]). In rodent pups, maternal presence has transient effects on cortisol release and amygdala function, such that maternal presence blocks stress reactivity and fear learning during the early stage of rat pup development [82]. Similar social buffering effects have been identified in humans; parent availability reduces cortisol response to social stress [95] and enhances emotion regulation abilities in children [96]. Moreover, parental stimuli can induce transient changes in functional connectivity of amygdala-mPFC circuitry, and these neurobiological changes predict the degree of parental buffering of children’s emotion regulation abilities [96]. Together, these findings provide a plausible neurobiological mechanism through which caregivers can directly influence neuro-affective functioning during development.
Despite robust evidence of social buffering effects during typical neuro-affective development, no evidence to date has examined these effects on emotion regulation circuitry in youth with history of ELS. However, recent behavioral evidence suggests that interventions such as high-quality foster care may promote healthy emotional development in youth with a history of early institutional caregiving [97]. In the BEIP study, children with earlier placement into high-quality foster care showed greater attention bias to positive stimuli relative to children who experienced prolonged institutional rearing and typically developing children [97]. Importantly, positive attention bias in foster care youth predicted lower externalizing symptoms at age 8 and lower internalizing problems at age 12, suggesting that positivity-bias following early foster-care placement is associated with improved socio-emotional functioning in the long-term [97, 98]. However, a recent study of internationally adopted PI children and adolescents found that parental presence during a social stress task had no greater regulatory effect on cortisol reactivity relative to stranger presence, suggesting that social buffering mechanisms may exert differential effects on stress-related neurobiology depending on prior social experiences [99]. Moreover, animal models have shown that social buffering effects are diminished following atypical caregiving experiences (i.e., nursery rearing; reviewed in [94]). As such, further research is needed to investigate potential mechanisms through which protective factors such as positive parenting behaviors may be able to recalibrate the developmental trajectory of neuro-affective circuitry, and whether they exert effects over and above the effects of ELS to protect against future risk for stress-related psychopathology.
6 Limitations and Future Directions
While the current review focused on common phenotypes of neuro-affective circuitry associated with ELS, there are several directions of future research that will advance our understanding of how early adversity and protective factors influence neurobiological development and subsequent mental health outcomes. First, there is limited research examining the effects of timing and chronicity of stressors on neuro-affective functional development. Recent studies examining structural brain development have identified differential effects of adversity on amygdala volume depending on age of exposure [14, 100], and there is preliminary evidence linking the age of maltreatment exposure to degree of amygdala reactivity during childhood [64]. However, the complexity and chronicity of adverse experiences in the majority of human studies makes it challenging to differentiate whether stress-related effects on amygdala-prefrontal development occur as a function of the duration or timing of the stress exposure. Although international adoption studies can provide insight into the effects of ELS (e.g., institutional care) that occurs during a discrete developmental window, there may be limitations in its generalizability. These limitations highlight the important role of preclinical studies that use animal models of ELS. While there will always be the ethical limitations in studying stress exposure in humans, animal studies can experimentally manipulate age of onset, chronicity, and severity of ELS to allow for greater conclusions of causality. Moreover, translational research can provide more precise examination of the underlying neurobiological mechanisms associated with early adverse experiences that cannot be accessed through human neuroimaging studies.
Second, recent theoretical frameworks have emphasized importance of examining specific dimensions of early adverse experiences, such as threat and neglect, and how they influence different aspects of neurobiological development [52]. Although the current review focused specifically on threat-related alterations in amygdala-prefrontal circuitry, other dimensions of early experience may target different neural circuits (e.g., cortico-striatal circuitry) and neuro-cognitive domains (e.g., reward learning, executive functions; [52, 101]). Further longitudinal research is needed to compare how certain dimensions of adverse experiences differentially alter neurobiological circuitry to confer risk for specific domains of psychopathology.
In addition to protective factors of the social environment, genetic factors play an important role in moderating risk for emotional psychopathology following ELS [102, 103]. For example, genetic polymorphisms in neuroplasticity genes (e.g., BDNF) have been associated with ELS-related changes in neurobiological development and emotion regulation [104]. More recent work has shown that cumulative risk profiles across several HPA-related genetic alleles moderate the association between amygdala-prefrontal connectivity and anxiety symptoms in children exposed to stressful life events [75]. Importantly, genetic factors are often correlated with variability in the early environment in human studies, representing a significant challenge for researchers to differentiate the effects of genetics (e.g., parent psychopathology) from the effects of ELS (e.g., family conflict). This can include studies of adoption and foster-care cohorts, as children who display more emotional difficulties at a young age may experience greater disruptions in family placements [105]. Despite these potential confounds, not all individuals with genetic predispositions (e.g., family history of psychopathology) will develop an emotional disorder, and emerging research suggests that environmentally induced epigenetic modifications in gene expression also predict vulnerability for psychopathology [106]. For example, low socioeconomic status has been associated with longitudinal increases in promotor methylation of the serotonin transporter gene during adolescence [106]. Importantly, these epigenetic changes were associated with enhanced threat-related amygdala reactivity, which in turn predicted longitudinal increases in depressive symptoms in adolescents with a family history of depression [106]. These findings emphasize the critical role of early experiences on the developmental trajectories of neuro-affective circuitry and risk for stress-related psychopathology.
7 Conclusion
In summary, emerging research has begun to identify the developmental pathways through which early adverse experiences alter emotion regulation circuitry to increase risk for stress-related psychopathology. However, little is known regarding the differential effects of adversity on amygdala-prefrontal function during different developmental stages (i.e., infancy, childhood, adolescence) and different dimensions of exposure (i.e., maltreatment vs. neglect). Further research delineating the effects of timing and type of adversities, as well as their interplay with genetic and epigenetic factors, is needed to advance our understanding of the neuro-developmental mechanisms implicated in vulnerability for psychopathology following ELS. This research will be facilitated by the incorporation of translational studies that directly compare human studies with animal models of ELS to provide further insight into the mechanisms underlying the link between early experiences and neuro-affective development. By applying a dimensional and developmental framework to future research, we can also begin to elucidate how and when protective factors can buffer the effects of ELS on neurobiological development to mitigate long-term risk for psychopathology. Ultimately, such research will be informative for developing policies and targeted interventions to improve mental health outcomes for individuals who have experienced early adversity.
References
Green JG, Mclaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC (2010) Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry 67(2):113–123, http://doi.org/10.1001/archgenpsychiatry.2009.187
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62(6):593–602, http://doi.org/10.1001/archpsyc.62.6.593
Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM et al (2010) Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry 197(5):378–385, http://doi.org/10.1192/bjp.bp.110.080499
Essex MJ, Shirtcliff EA, Burk LR, Ruttle PL, Klein MH, Slattery MJ et al (2011) Influence of early life stress on later hypothalamic-pituitary-adrenal axis functioning and its covariation with mental health symptoms: a study of the allostatic process from childhood into adolescence. Dev Psychopathol 23(4):1039–1058, http://doi.org/10.1017/S0954579411000484
Humphreys KL, Gleason MM, Drury SS, Miron D, Nelson CA, Fox NA, Zeanah CH (2015) Effects of institutional rearing and foster care on psychopathology at age 12 years in Romania: follow-up of an open, randomised controlled trial. Lancet Psychiatry 2(7):625–634, http://doi.org/10.1016/S2215-0366(15)00095-4
Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J (2014) A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological. Arch Pediatr Adolesc Med 156:824–830
Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L et al (2010) Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49(10):980–989, http://doi.org/10.1016/j.jaac.2010.05.017
Smith LB, Thelen E (2003) Development as a dynamic system. Trends Cogn Sci 7(8):343–348, http://doi.org/10.1016/S1364-6613(03)00156-6
Barker DJP (2007) The origins of the developmental origins theory. J Intern Med 261(5):412–417, http://doi.org/10.1111/j.1365-2796.2007.01809.x
Blair C, Raver CC (2012) Child development in the context of adversity: experiential canalization of brain and behavior. Am Psychol 67(4):309–318, http://doi.org/10.1037/a0027493
Del Giudice M, Ellis BJ, Shirtcliff EA (2011) The adaptive calibration model of stress responsivity. Neurosci Biobehav Rev 35(7):1562–1592
Wadhwa P, Buss C, Entringer S, Swanson M (2010) Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med 27(5):358–368, http://doi.org/10.1055/s-0029-1237424.Developmental
Callaghan BL, Tottenham N (2016) The stress acceleration hypothesis: effects of early-life adversity on emotion circuits and behavior. Curr Opin Behav Sci 7:76–81, http://doi.org/10.1016/j.cobeha.2015.11.018
Tottenham N, Sheridan MA (2009) A review of adversity, the amygdala and the hippocampus: a consideration of developmental timing. Front Hum Neurosci 3:68, http://doi.org/10.3389/neuro.09.068.2009
De Bellis MD, Broussard ER, Herring DJ, Wexler S, Moritz G, Benitez JG (2001) Psychiatric co-morbidity in caregivers and children involved in maltreatment: a pilot research study with policy implications. Child Abuse Negl 25(7):923–944, http://doi.org/10.1016/S0145-2134(01)00247-2
Hariri AR, Holmes A (2015) Finding translation in stress research. Nat Neurosci 18(10):1347–1352, http://doi.org/10.1038/nn.4111
Davis M, Whalen PJ (2001) The amygdala: vigilance and emotion. Mol Psychiatry 6(1):13–34. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11244481
Kim JH, Hamlin AS, Richardson R (2009) Fear extinction across development: the involvement of the medial prefrontal cortex as assessed by temporary inactivation and immunohistochemistry. J Neurosci 29(35):10802–10808, http://doi.org/10.1523/JNEUROSCI.0596-09.2009
Milad MR, Rauch SL, Pitman RK, Quirk GJ (2006) Fear extinction in rats: implications for human brain imaging and anxiety disorders. Biol Psychol 73:61–71, http://doi.org/10.1016/j.biopsycho.2006.01.008
Phelps EA, LeDoux JE (2005) Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron 48(2):175–187, http://doi.org/10.1016/j.neuron.2005.09.025
Buhle JT, Silvers JA, Wager TD, Lopez R, Onyemekwu C, Kober H et al (2014) Cognitive reappraisal of emotion: a meta-analysis of human neuroimaging studies. Cereb Cortex 24:2981–2990, http://doi.org/10.1093/cercor/bht154
Etkin A, Klemenhagen KC, Dudman JT, Rogan MT, Hen R, Kandel ER, Hirsch J (2004) Individual differences in trait anxiety predict the response of the basolateral amygdala to unconsciously processed fearful faces. Neuron 44(6):1043–1055, http://doi.org/10.1016/j.neuron.2004.12.006
Koenigs M, Grafman J (2009) Posttraumatic stress disorder: the role of medial prefrontal cortex and amygdala. Neuroscientist 15(5):540–548
Murray EA, Wise SP, Drevets WC (2011) Localization of dysfunction in major depressive disorder: prefrontal cortex and amygdala. Biol Psychiatry 69(12):e43–e54, http://doi.org/10.1016/j.biopsych.2010.09.041
Morris SE, Cuthbert BN (2012) State of the art. Dialogues Clin Neurosci 14:29–37
Dillon DG, Rosso IM, Pechtel P, Killgore WDS, Rauch SL, Pizzagalli DA (2014) Peril and pleasure: an rdoc-inspired examination of threat responses and reward processing in anxiety and depression. Depress Anxiety 31(3):233–249, http://doi.org/10.1002/da.22202.Peril
Gee DG, Humphreys KL, Flannery J, Goff B, Telzer EH, Shapiro M et al (2013) A developmental shift from positive to negative connectivity in human amygdala-prefrontal circuitry. J Neurosci 33(10):4584–4593, http://doi.org/10.1523/JNEUROSCI.3446-12.2013
Guyer AE, Monk CS, McClure-Tone EB, Nelson EE, Roberson-Nay R, Adler AD et al (2008) A developmental examination of amygdala response to facial expressions. J Cogn Neurosci 20(9):1565–1582, http://doi.org/10.1162/jocn.2008.20114
Hwang S, White SF, Nolan ZT, Sinclair S, Blair RJR (2014) Neurodevelopmental changes in the responsiveness of systems involved in top down attention and emotional responding. Neuropsychologia 62:1–9, http://doi.org/10.1016/j.neuropsychologia.2014.08.003
Swartz JR, Carrasco M, Wiggins JL, Thomason ME, Monk CS (2014) Age-related changes in the structure and function of prefrontal cortex-amygdala circuitry in children and adolescents: a multi-modal imaging approach. Neuroimage 86:212–220, http://doi.org/10.1016/j.neuroimage.2013.08.018
Vink M, Derks JM, Hoogendam JM, Hillegers M, Kahn RS (2014) Functional differences in emotion processing during adolescence and early adulthood. Neuroimage 91:70–76, http://doi.org/10.1016/j.neuroimage.2014.01.035
Decety J, Michalska KJ, Kinzler KD (2012) The contribution of emotion and cognition to moral sensitivity: a neurodevelopmental study. Cereb Cortex 22(1):209–220, http://doi.org/10.1093/cercor/bhr111
Gabard-Durnam LJ, Flannery J, Goff B, Gee DG, Humphreys KL, Telzer E et al (2014) The development of human amygdala functional connectivity at rest from 4 to 23 years: a cross-sectional study. Neuroimage 95:193–207, http://doi.org/10.1016/j.neuroimage.2014.03.038
Dougherty LR, Blankenship SL, Spechler PA, Padmala S, Pessoa L (2015) An fMRI pilot study of cognitive reappraisal in children: divergent effects on brain and behavior. J Psychopathol Behav Assess 37(4):634–644, http://doi.org/10.1007/s10862-015-9492-z
McRae K, Gross JJ, Weber J, Robertson ER, Sokol-Hessner P, Ray RD et al (2012) The development of emotion regulation: an fMRI study of cognitive reappraisal in children, adolescents and young adults. Soc Cogn Affect Neurosci 7(1):11–22, http://doi.org/10.1093/scan/nsr093
Silvers JA, Shu J, Hubbard AD, Weber J, Ochsner KN (2015) Concurrent and lasting effects of emotion regulation on amygdala response in adolescence and young adulthood. Dev Sci 18(5):771–784, http://doi.org/10.1111/desc.12260
Gaffrey MS, Luby JL, Belden AC, Hirshberg JS, Volsch J, Barch DM (2011) Association between depression severity and amygdala reactivity during sad face viewing in depressed preschoolers: an fMRI study. J Affect Disord 129(1-3):364–370, http://doi.org/10.1016/j.jad.2010.08.031
Garrett AS, Carrion V, Kletter H, Karchemskiy A, Weems CF, Reiss A (2012) Brain activation to facial expressions in youth with PTSD symptoms. Depress Anxiety 29(5):449–459, http://doi.org/10.1002/da.21892
Pagliaccio D, Luby J, Gaffrey M, Belden A, Botteron K, Gotlib IH, Barch DM (2012) Anomalous functional brain activation following negative mood induction in children with pre-school onset major depression. Dev Cogn Neurosci 2(2):256–267, http://doi.org/10.1016/j.dcn.2011.11.008
Pine DS, Guyer AE, Leibenluft E (2008) Functional magnetic resonance imaging and pediatric anxiety. J Am Acad 47(11):1217–1221, http://doi.org/10.1097/CHI.0b013e318185dad0.FUNCTIONAL
Roy AK, Fudge JL, Kelly C, Perry JSA, Daniele T, Carlisi C et al (2013) Intrinsic functional connectivity of amygdala-based networks in adolescent generalized anxiety disorder. J Am Acad Child Adolesc Psychiatry 52(3):290–299.e2. http://doi.org/10.1016/j.jaac.2012.12.010
Wolf RC, Herringa RJ (2016) Prefrontal-amygdala dysregulation to threat in pediatric post-traumatic stress disorder. Neuropsychopharmacology 41(3):822–831, http://doi.org/10.1038/npp.2015.209
Kujawa A, Wu M, Klump H, Pine DS, Swain JE, Fitzgerald KD et al (2016) Altered development of amygdala-anterior cingulate cortex connectivity in anxious youth and young adults. Biol Psychiatry Cogn Neurosci Neuroimaging 1(4):345–352, http://doi.org/10.1017/CBO9781107415324.004
Callaghan BL, Sullivan RM, Howell B, Tottenham N (2014) The international society for developmental psychobiology Sackler symposium: early adversity and the maturation of emotion circuits-A cross-species analysis. Dev Psychobiol 56(8):1635–1650, http://doi.org/10.1002/dev.21260
Avishai-Eliner S, Yi SJ, Baram TZ (1996) Developmental profile of messenger RNA for the corticotropin-releasing hormone receptor in the rat limbic system. Brain Res Dev Brain Res 91(2):159–163, http://doi.org/0165380695001581
Hatalski CG, Guirguis C, Baram TZ (2012) Corticotropin releasing factor mRNA expression in the hypothalamic paraventricular nucleus and the central nucleus of the amygdala is modulated by repeated acute stress in the immature rat. J Neuroendocrinol 10(9):663–669
Moriceau S, Wilson DA, Levine S, Sullivan RM (2006) Dual circuitry for odor-shock conditioning during infancy: corticosterone switches between fear and attraction via amygdala. J Neurosci 26(25):6737–6748, http://doi.org/10.1523/JNEUROSCI.0499-06.2006
Eiland L, Ramroop J, Hill MN, Manley J, McEwen BS (2012) Chronic juvenile stress produces corticolimbic dendritic architectural remodeling and modulates emotional behavior in male and female rats. Psychoneuroendocrinology 37(1):39–47, http://doi.org/10.1016/j.psyneuen.2011.04.015
Malter Cohen M, Jing D, Yang RR, Tottenham N, Lee FS, Casey BJ (2013) Early-life stress has persistent effects on amygdala function and development in mice and humans. Proc Natl Acad Sci U S A 110(45):18274–18278, http://doi.org/10.1073/pnas.1310163110
Raineki C, Cortés MR, Belnoue L, Sullivan RM (2012) Effects of early-life abuse differ across development: infant social behavior deficits are followed by adolescent depressive-like behaviors mediated by the amygdala. J Neurosci 32(22):7758–7765, http://doi.org/10.1523/JNEUROSCI.5843-11.2012
Ishikawa J, Nishimura R, Ishikawa A (2015) Early-life stress induces anxiety-like behaviors and activity imbalances in the medial prefrontal cortex and amygdala in adult rats. Eur J Neurosci 41(4):442–453, http://doi.org/10.1111/ejn.12825
McLaughlin KA, Sheridan MA, Lambert HHK (2014) Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev 47:578–591, http://doi.org/10.1016/j.neubiorev.2014.10.012
Arata CM, Langhinrichsen-Rohling J, Bowers D, O’Brien N (2007) Differential correlates of multi-type maltreatment among urban youth. Child Abuse Negl 31(4):393–415, http://doi.org/10.1016/j.chiabu.2006.09.006
Dannlowski U, Kugel H, Huber F, Stuhrmann A, Redlich R, Grotegerd D et al (2013) Childhood maltreatment is associated with an automatic negative emotion processing bias in the amygdala. Hum Brain Mapp 34(11):2899–2909, http://doi.org/10.1002/hbm.22112
van Harmelen A-L, van Tol M-J, Demenescu LR, van der Wee NJA, Veltman DJ, Aleman A et al (2013) Enhanced amygdala reactivity to emotional faces in adults reporting childhood emotional maltreatment. Soc Cogn Affect Neurosci 8(4):362–369, http://doi.org/10.1093/scan/nss007
Bogdan R, Williamson DE, Hariri AR (2012) Mineralocorticoid receptor Iso/Val (rs5522) genotype moderates the association between previous childhood emotional neglect and amygdala reactivity. Am J Psychiatry 169:515–522, http://doi.org/10.1176/appi.ajp.2011.11060855
White MG, Bogdan R, Fisher PM, Muñoz KE, Williamson DE, Hariri AR (2012) FKBP5 and emotional neglect interact to predict individual differences in amygdala reactivity. Genes Brain Behav 11(7):869–878, http://doi.org/10.1111/j.1601-183X.2012.00837.x
Gianaros PJ, Horenstein JA, Hariri AR, Sheu LK, Manuck SB, Matthews KA, Cohen S (2008) Potential neural embedding of parental social standing. Soc Cogn Affect Neurosci 3(2):91–96, http://doi.org/10.1093/scan/nsn003
Evans GW, Swain JE, King AP, Wang X, Javanbakht A, Ho SS et al (2016) Childhood cumulative risk exposure and adult amygdala volume and function. J Neurosci Res 94(6):535–543, http://doi.org/10.1002/jnr.23681
Javanbakht A, King AP, Evans GW, Swain JE, Angstadt M, Phan KL, Liberzon I (2015) Childhood poverty predicts adult amygdala and frontal activity and connectivity in response to emotional faces. Front Behav Neurosci 9(154), http://doi.org/10.3389/fnbeh.2015.00154
Gee DG, Gabard-Durnam LJ, Flannery J, Goff B, Humphreys KL, Telzer EH et al (2013) Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proc Natl Acad Sci U S A 110(39):15638–15643, http://doi.org/10.1073/pnas.1307893110
Maheu FS, Dozier M, Guyer AE, Mandell D, Peloso E, Poeth K, Jenness J (2010) Preliminary study of medial temporal lobe function in youths with a history of caregiver deprivation and emotional neglect. Cogn Affect Behav Neurosci 10(1):34–49, http://doi.org/10.3758/CABN.10.1.34.A
Tottenham N, Hare TA, Millner A, Gilhooly T, Zevin JD, Casey BJ (2011) Elevated amygdala response to faces following early deprivation. Dev Sci 14(2):190–204, http://doi.org/10.1111/j.1467-7687.2010.00971.x
McCrory EJ, De Brito SA, Kelly PA, Bird G, Sebastian CL, Mechelli A et al (2013) Amygdala activation in maltreated children during pre-attentive emotional processing. Br J Psychiatry 202(4):269–276, http://doi.org/10.1192/bjp.bp.112.116624
McLaughlin KA, Peverill M, Gold AL, Alves S, Sheridan MA (2015) Child maltreatment and neural systems underlying emotion regulation. J Am Acad Child Adolesc Psychiatry 54(9):753–762, http://doi.org/10.1016/j.jaac.2015.06.010
Marusak HA, Martin KR, Etkin A, Thomason ME (2014) Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology 40(5):1250–1258, http://doi.org/10.1038/npp.2014.311
McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, Viding E (2011) Heightened neural reactivity to threat in child victims of family violence. Curr Biol 21(23):R947–R948, http://doi.org/10.1016/j.cub.2011.10.015
Swartz JR, Williamson DE, Hariri AR (2015) Developmental change in amygdala reactivity during adolescence: effects of family history for depression and stressful life events. Am J Psychiatry 172(3):276–283, http://doi.org/10.1176/appi.ajp.2014.14020195
Jedd K, Hunt RH, Cicchetti D, Hunt E, Cowell RA, Rogosch FA et al (2015) Long-term consequences of childhood maltreatment: altered amygdala functional connectivity. Dev Psychopathol 27:1577–1589, http://doi.org/10.1017/S0954579415000954
Kim P, Evans GW, Angstadt M, Ho SS, Sripada CS, Swain JE (2013) Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proc Natl Acad Sci U S A 110(46):18442–18447, http://doi.org/10.1073/pnas.1308240110/-/DCSupplemental.www.pnas.org/cgi/doi/10.1073/pnas.1308240110
Cicchetti D, Rogosch FA (1996) Equifinality and multifinality in developmental psychopathology. Dev Psychopathol 8:597–600. Retrieved from file://localhost/Users/lornaquandt/Documents/Papers/2007/Unknown/2007-3.pdf\npapers://4f210845-804c-495f-b761-84503ca2694d/Paper/p757
Fan Y, Herrera-Melendez AL, Pestke K, Feeser M, Aust S, Otte C et al (2014) Early life stress modulates amygdala-prefrontal functional connectivity: implications for oxytocin effects. Hum Brain Mapp 35(10):5328–5339, http://doi.org/10.1002/hbm.22553
Herringa RJ, Birn RM, Ruttle PL, Burghy CA, Stodola DE, Davidson RJ, Essex MJ (2013) Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc Natl Acad Sci U S A 110(47):19119–19124, http://doi.org/10.1073/pnas.1310766110
Thomason ME, Marusak HA, Tocco MA, Vila AM, McGarragle O, Rosenberg DR (2015) Altered amygdala connectivity in urban youth exposed to trauma. Soc Cogn Affect Neurosci 10(11):1460–1468, http://doi.org/10.1093/scan/nsv030
Pagliaccio D, Luby JL, Bogdan R, Agrawal A, Gaffrey MS, Belden AC et al (2015) Amygdala functional connectivity, HPA axis genetic variation, and life stress in children and relations to anxiety and emotion regulation. J Abnorm Psychol 124(4):817–833
Graham AM, Pfeifer JH, Fisher PA, Carpenter S, Fair DA (2015) Early life stress is associated with default system integrity and emotionality during infancy. J Child Psychol Psychiatry 56(11):1212–1222, http://doi.org/10.1111/jcpp.12409
Graham AM, Pfeifer JH, Fisher PA, Lin W, Gao W, Fair DA (2014) The potential of infant fMRI research and the study of early life stress as a promising exemplar. Dev Cogn Neurosci 12:12–39, http://doi.org/10.1016/j.dcn.2014.09.005
Pagliaccio D, Luby JL, Luking KR, Belden AC, Barch DM (2014) Brain–behavior relationships in the experience and regulation of negative emotion in healthy children: Implications for risk for childhood depression. Dev Psychopathol 26:1289–1303
Crozier JC, Wang L, Huettel SA, De Bellis MD (2014) Neural correlates of cognitive and affective processing in maltreated youth with posttraumatic stress symptoms: does gender matter? Dev Psychopathol 26(2):491–513, http://doi.org/10.1017/S095457941400008X
Suzuki H, Luby JL, Botteron KN, Dietrich R, McAvoy MP, Barch DM (2014) Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. J Am Acad Child Adolesc Psychiatry 53(7):800–813.e10. http://doi.org/10.1016/j.jaac.2014.04.013
Gaffrey MS, Barch DM, Luby JL (2016) Amygdala reactivity to sad faces in preschool children: an early neural marker of persistent negative affect. Dev Cogn Neurosci 17:94–100, http://doi.org/10.1016/j.dcn.2015.12.015
Moriceau S, Sullivan RM (2006) Maternal presence serves as a switch between learning fear and attraction in infancy. Nat Neurosci 9(8):1004–1006, http://doi.org/10.1038/nn1733
Burghy CA, Stodola DE, Ruttle PL, Molloy EK, Armstrong JM, Oler JA et al (2012) Developmental pathways to amygdala-prefrontal function and internalizing symptoms in adolescence. Nat Neurosci 15(12):1736–1741, http://doi.org/10.1038/nn.3257
McGloin JM, Widom CS (2001) Resilience among abused and neglected children grown up. Dev Psychopathol 13(4):1021–1038, http://doi.org/10.1017/S095457940100414X
Masten AS (2004) Regulatory processes, risk, and resilience in adolescent development. Ann N Y Acad Sci 1021:310–319, http://doi.org/10.1196/annals.1308.036
Jaffee SR, Caspi A, Moffitt TE, Polo-Tomás M, Taylor A (2007) Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: a cumulative stressors model. Child Abuse Negl 31(3):231–253, http://doi.org/10.1016/j.chiabu.2006.03.011
Cicchetti D, Blender JA (2006) A multiple-levels-of-analysis perspective on resilience: implications for the developing brain, neural plasticity, and preventive interventions. Ann N Y Acad Sci 1094:248–258, http://doi.org/10.1196/annals.1376.029
McLaughlin KA (2016) Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol 45(3):361–382, http://doi.org/10.1080/15374416.2015.1110823
Afifi TO, MacMillan HL (2011) Resilience following child maltreatment: a review of protective factors. Can J Psychiatry 56(5):266–272
DuMont KA, Widom CS, Czaja SJ (2007) Predictors of resilience in abused and neglected children grown-up: the role of individual and neighborhood characteristics. Child Abuse Negl 31(3):255–274, http://doi.org/10.1016/j.chiabu.2005.11.015
Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B (2007) Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl 31(3):211–229, http://doi.org/10.1016/j.chiabu.2007.02.004
Miller-Graff LE, Cater ÅK, Howell KH, Graham-Bermann SA (2016) Parent-child warmth as a potential mediator of childhood exposure to intimate partner violence and positive adulthood functioning. Anxiety Stress Coping 29(3):259–273, http://doi.org/10.1080/10615806.2015.1028030
Hennessy MB, Kaiser S, Sachser N (2009) Social buffering of the stress response: diversity, mechanisms, and functions. Front Neuroendocrinol 30(4):470–482, http://doi.org/10.1016/j.yfrne.2009.06.001
Kikusui T, Winslow JT, Mori Y (2006) Social buffering: relief from stress and anxiety. Philos Trans R Soc B Biol Sci 361(1476):2215–2228, http://doi.org/10.1098/rstb.2006.1941
Hostinar CE, Johnson AE, Gunnar MR (2014) Parent support is less effective in buffering cortisol stress reactivity for adolescents compared to children. Dev Sci 2:281–297, http://doi.org/10.1111/desc.12195
Gee DG, Gabard-Durnam L, Telzer EH, Humphreys KL, Goff B, Shapiro M et al (2014) Maternal buffering of human amygdala-prefrontal circuitry during childhood but not during adolescence. Psychol Sci 25(11):2067–2078, http://doi.org/10.1177/0956797614550878
Troller-Renfree S, Mcdermott JM, Nelson CA, Zeanah CH, Fox NA (2015) The effects of early foster care intervention on attention biases in previously institutionalized children in Romania. Dev Sci 18(5):713–722, http://doi.org/10.1111/desc.12261
Troller-renfree S, Mclaughlin KA, Sheridan MA, Nelson CA, Zeanah CH, Fox NA (2016) The benefits of a positive attention bias amongst children with a history of psychosocial deprivation. Biol Psychol. http://doi.org/10.1016/j.biopsycho.2016.04.008
Hostinar CE, Johnson AE, Gunnar MR (2015) Early social deprivation and the social buffering of cortisol stress responses in late childhood: an experimental study. Dev Psychol 51(11):1597–1608
Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH (2014) Sensitive periods of amygdala development: the role of maltreatment in preadolescence. Neuroimage 97:236–244, http://doi.org/10.1016/j.neuroimage.2014.04.025
Goff B, Tottenham N (2015) Early-life adversity and adolescent depression: mechanisms involving the ventral striatum. CNS Spectr 20(4):337–345, http://doi.org/10.1017/S1092852914000674
Heim C, Binder EB (2012) Current research trends in early life stress and depression: review of human studies on sensitive periods, gene-environment interactions, and epigenetics. Exp Neurol 233(1):102–111, http://doi.org/10.1016/j.expneurol.2011.10.032
Uher R, McGuffin P (2008) The moderation by the serotonin transporter gene of environmental adversity in the aetiology of mental illness: review and methodological analysis. Mol Psychiatry 13(2):131–146, http://doi.org/10.1038/sj.mp.4002067
Casey BJ, Glatt CE, Tottenham N, Soliman F, Bath K, Amso D et al (2009) Brain-derived neurotrophic factor as a model system for examining gene by environment interactions across development. Neuroscience 164(1):108–120, http://doi.org/10.1016/j.neuroscience.2009.03.081
Scarr S, Mccartney K (1983) How people make their own environments: a theory of genotype → environment effects author (s): Sandra Scarr and Kathleen McCartney Published by: Wiley on behalf of the Society for Research in Child Development Stable URL: http://www.jstor.org/stable/. Child Dev 54(2):424–435
Swartz JR, Hariri AR, Williamson DE (2016) An epigenetic mechanism links socioeconomic status to changes in depression-related brain function in high-risk adolescents. Mol Psychiatry. http://doi.org/10.1038/mp.2016.82
Acknowledgements
This work was supported by the NIMH under grant R01MH091864 (N. Tottenham, PI), an NSF Conference Grant conference grant BCS-1439258 (N. Tottenham, co-I), and the Dana Foundation (N. Tottenham, PI), and the NSF Graduate Research Fellowship Program under Grant No. DGE-16-44869 (M. R. VanTieghem). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institutes of Health, the National Science Foundation, or the Dana Foundation.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
VanTieghem, M.R., Tottenham, N. (2017). Neurobiological Programming of Early Life Stress: Functional Development of Amygdala-Prefrontal Circuitry and Vulnerability for Stress-Related Psychopathology. In: Vermetten, E., Baker, D.G., Risbrough, V.B. (eds) Behavioral Neurobiology of PTSD. Current Topics in Behavioral Neurosciences, vol 38. Springer, Cham. https://doi.org/10.1007/7854_2016_42
Download citation
DOI: https://doi.org/10.1007/7854_2016_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-94823-2
Online ISBN: 978-3-319-94824-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)