Abstract
The developmental origin of health and disease hypothesis states that adverse fetal and early childhood exposures can predispose to obesity, cardiovascular, and neurodegenerative diseases (NDDs) in adult life. Early exposure to environmental chemicals interferes with developmental programming and induces subclinical alterations that may hesitate in pathophysiology and behavioral deficits at a later life stage. The mechanisms by which perinatal insults lead to altered programming and to disease later in life are still undefined. The long latency between exposure and onset of disease, the difficulty of reconstructing early exposures, and the wealth of factors which the individual is exposed to during the life course make extremely difficult to prove the developmental origin of NDDs in clinical and epidemiological studies. An overview of animal studies assessing the long-term effects of perinatal exposure to different chemicals (heavy metals and pesticides) supports the link between exposure and hallmarks of neurodegeneration at the adult stage. Furthermore, models of maternal immune activation show that brain inflammation in early life may enhance adult vulnerability to environmental toxins, thus supporting the multiple hit hypothesis for NDDs’ etiology. The study of prospective animal cohorts may help to unraveling the complex pathophysiology of sporadic NDDs. In vivo models could be a powerful tool to clarify the mechanisms through which different kinds of insults predispose to cell loss in the adult age, to establish a cause–effect relationship between “omic” signatures and disease/dysfunction later in life, and to identify peripheral biomarkers of exposure, effects, and susceptibility, for translation to prospective epidemiological studies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Neurodevelopment
- Heavy metals
- Pesticides
- Maternal immune activation
- Alzheimer’s disease
- Parkinson’s disease
- Exposome
1 General Introduction
Since the publication in 1993 in The Lancet of the paper by Barker et al. (1993) indicating that fetal undernutrition was a major risk factor for cardiovascular diseases, a great body of experimental and epidemiological evidence has been accumulating, indicating that exposure to an unfavorable environment in early life is associated with a significantly increased risk of later disease, a phenomenon termed “early life programming.” The Barker’s hypothesis formed the basis for the developmental origins of health and disease (DOHaD) hypothesis that, further to fetal nutrition, considered a wider spectrum of adverse fetal and childhood exposures that can predispose to chronic diseases later in life. In such expanded view of the original Barker’s hypothesis, not only malnutrition, but also the quality of the maternal diet, the intake of micronutrients, maternal smoking, and prenatal maternal stress may account for the relationship of the prenatal environment to adult disorders including cancer, metabolic, neuroendocrine, and neurodegenerative and cognitive diseases in adult life (Gillman 2005; Hanson 2013; Tarantal and Berglund 2014).
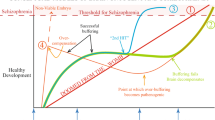
Knowledge about the mechanism(s) by which fetal insults lead to altered programming and to disease later in life is still scarce, and as discussed in the following paragraphs, it is mainly derived from experimental studies. The long latency between exposure and disease and the lack of a clear pathological phenotype before disease onset make extremely difficult to assess the underlying mechanisms in clinical studies. Lahiri et al. (2009) suggested that environmental factors play a role in chronic disease etiology by inducing latent epigenetic changes. These authors described the association of early environment with disease onset especially with respect to Alzheimer’s disease (AD), proposing a “Latent Early-life Associated Regulation” (LEARn) model that considers environmental exposures as “hits”. According to this model, all neurodegenerative disorders come under the category of a “n” hit latent model, where early-life exposure leads to epigenetic perturbations in the genes, which remain silent until a second hit triggers the development of disease. The multiple hit hypothesis appears as particularly suited to explain the etiology of complex neuropsychiatric and neurologic diseases that share a highly sporadic nature characterized by genetic and environmental risk factors. It also explains the relatively long latency between exposure and disease, as subclinical deficits occurring during specific windows of developmental plasticity do not become manifest without a second hit occurring later in life (Heindel et al. 2015).
The DOHaD models, to date, have focused mainly on skewed nutritional states and/or low birthweight (Morley 2006), while the role played by exposures to environmental agents, such as water and air pollution and chemicals in food, either alone or in combination, has only recently come to attention. This is somewhat surprising since there is vast literature on the developmental neurotoxicity that indicates an inverse association between chemical exposure and child neurodevelopment (Bellinger 2014 for an updated review). Extensive evidence also shows that some environmental agents alter developmental programming via changes in gene expression or imprinting that do not result in malformations but in functional deficits that become apparent later in life. However, much less attention has been posed to the role that early exposure to environmental toxins may play in predisposing to neuropsychiatric and neurodegenerative in adult or even old age. This can be explained by several factors: the methodological constraints related to the difficulty of establishing cause–effect relationships between early exposure and disease manifestation (discussed in Sect. 2.4) and the lack of reliable biomarkers that can predict increased risk in early life stages, together with the still diffused idea that neurodegenerative diseases (NDDs) are linked to pathological brain aging.
In the present review, we will describe the general frame of the developmental origin of NDDs and the challenges posed to experimental and epidemiological research investigating the role of environmental pollutants as risk factors. We will then present an overview of animal studies that have assessed the delayed effects of either single or multiple perinatal toxic insults, evidencing neurobehavioral alterations resembling the major hallmarks of human NDDs.
2 Developmental Neurotoxicity and Neurodegenerative Diseases: A Common Playground?
2.1 Introduction
The human nervous system develops over a very long period extending from the embryonic period through puberty. About two weeks after conception, the neural plate folds to form the neural tube, and cells formed during this period of rapid proliferation migrate to a different position where they differentiate into neurons and neuroglia. In the human fetus, cell migration is nearly complete in the neocortex and in most of the brain by the sixth month of gestation (Gupta et al. 2005). During the remainder of intrauterine development, neurons differentiate and connect with each other. The period of rapid synaptogenesis or the so-called brain growth spurt (in humans occurring between the last three months of pregnancy and the 2nd postnatal year) is considered one of the most important processes that take place during brain development (Garner et al. 2002). This process is crucial not only in neurodevelopment but also plays a vital role in synaptic plasticity, learning, memory, and adaptation throughout life. Without this process, no complex brain network can be established, as synapse is the fundamental unit of connectivity and communication between neurons (Tau and Peterson 2010). During the brain growth spurt, substantially more connections are formed than those that will be eventually retained as many of them will be gradually discarded by apoptotic mechanisms. The process of synapse elimination is a normal part of development (Tau and Peterson 2010; Shonkoff 2000), and both endogenous (neurotrophic factors, synthesis, and release of neurotransmitters, hormones) and environmental factors (i.e., sensorial inputs) concur to influence the fine matchup between pre- and postsynaptic neurons. Altogether, brain development is made up of several interactive and temporally overlapping stages. A plethora of mechanisms regulates each of these sequential steps, and some of the major signaling cascades and trophic factors in the developing brain play a role in the aging or neurodegenerating brain. In a recent review, Kovacs et al. (2014) highlighted the commonalities between neuronal loss and neuronal development. These authors performed an overview of NDDs according to major proteins deposited (i.e., β-amyloid and tau protein); they observed that genes that are mutated in NNDs code for protein, which are highly expressed throughout neural development. Characterization of the mechanisms underlying hippocampal neurogenesis in the fetal and adult brain points to the involvement of the same gene products, namely of proteins that seem to drive either synaptogenesis or synaptic dysfunction depending on the age factor. This is the case of reelin, presenilins (PS), Notch-1, and brain-derived neurotrophic factor (BDNF). Furthermore, proteins representing hallmarks of NDDs might also play a crucial physiological role during brain development and adult neurogenesis. Specifically, the amyloid precursor protein (APP) significantly contributes to neurite outgrowth and hippocampal development (Billnitzer et al. 2013), α-synuclein has a key role in synaptic vesicle recycling and is expressed in normal fetal brain, and phosphorylation of the tau protein takes place during fetal development (Goedert et al. 1993). Altogether, though the majority of data originate from animal model research and still await confirmation in humans, there is substantial support to the view that pathological changes observed in NDDs could be in part the result of aberrant neuroplasticity mechanisms settled during the fetal life (Bugiani 2011). In this light, the study of the toxicants’ effects on brain development is possibly crucial for unraveling the complex NDDs’ etiology.
2.2 Brain Plasticity and Vulnerability
The remarkable plasticity of the brain during the fetal and neonatal periods is a double-edged sword as it renders this organ extremely responsive to environmental factors. On the one hand, early environmental inputs can interact with genetic factors to promote the development of neuronal circuits and functions (Sale et al. 2014); on the other hand, early negative conditions (i.e., stress, toxic insults) can act in the opposite direction, increasing the chances to develop neurodevelopmental disorders or diseases in adulthood. Diverse environmental stressors—chemical pollutants, drugs, nutritional factors, maternal infection, stress, and deprivation—may interfere with typical brain developmental trajectories. In order to cope with insults perturbing prenatal environment, the fetus develops compensatory strategies that could be adaptive or disruptive, resulting in interindividual variability in the total neuronal and glial burden and functional reserve.
Exposure to toxicants at any point during brain development may result in aberrant neural structure or function. The end points affected may vary depending on the timing and duration of exposure. Toxic disruption of early maturational events are more likely to result in neural tube defects or major malformation (i.e., anencephaly, spina bifida), while toxic interference with later developmental events results more commonly in cytoarchitectural and molecular alterations that might be expressed as behavioral dysfunction. Specifically, damage or destruction of neurons by chemical compounds when they are in the process of synapses formation, integration, and formation of neural networks will derange the organization and function of these networks, thereby setting the stage for subsequent impairment of learning and memory (Kovacs et al. 2014).
It was not until the early 1990s that significant evidence emerged showing that low-dose exposures to metals such as methylmercury and lead, though not producing teratogenic effects evident at birth, could result in later behavioral dysfunctions in children (Gilbert and Grant-Webster 1995; Banks et al. 1997). Similar results were later identified for the perinatal exposure to other environmental contaminants such as pesticides (Eskenazi et al. 2007; Perera et al. 2009), polychlorobiphenyls (Winneke 2011), polybrominated diphenyl ethers (Herbstman et al. 2010), and phthalates (Whyatt et al. 2012). These observations were consistent with the emergent DOHaD concept and shifted the emphasis of developmental toxicology from the study of teratogenic effects to functional changes occurring during development and becoming manifest only after a latent period (Bellinger 2009; Miller 1986). Mechanistic studies carried out in animals and in in vitro models point to multiple pathways and targets of toxicity for several established neurotoxicants, depending on the dosage or time window of exposure (Neal et al. 2011; Roy et al. 2004; Slotkin and Seidler 2009). A reconsideration of the targets of toxicity of the major environmental pollutants in the developing brain could possibly reveal significant commonalities between pathophysiology of neurodevelopmental disorders and the cognitive decline associated to NDDs (see the case of developmental lead exposure, Sect. 3.2.1).
2.3 The Multiple Hit Hypothesis for Neurodegenerative Diseases
Because the most of cases of NDDs onset late in life, they have been traditionally considered as linked to aging, but recent evidence suggests that the aging process is less important than was thought in the past. According to the LEARn model, all sporadic NDDs are characterized by ‘n’ hit latent model. Their onset in adulthood may be the consequence of alteration in gene regulation induced by early-life exposures that, after a silent period, lead to disease. Under this perspective, the old age may be the point in time where any change in developmental programming produced by multiple hits interacts sufficiently to cause overt disease (Logroscino 2005). Under LEARn, early-life stressors modify potential expression levels of disorder-associated genes in a latent manner. Latent changes in these genes are maintained by epigenetic mechanisms such as DNA methylation, DNA oxidation, and chromatin reorganization. Alterations in gene expression lead to altered protein synthesis and eventually to altered numbers and/or location of cells.
The multiple hit hypothesis firstly advanced to explain the etiology of PD (Calne and Langston 1983) might be applied to other major NNDs. In this light, the environmental insult could act via a one hit or even two/three hit scenarios, where the fetal insult may be the first event. Fetal exposure to a toxicant would lead by itself to disease later in life, as the neurotoxicant may induce subclinical injury to neural or glial cells, which leads to progressive loss of function. The developing organism initially compensates for the mild deficit, but the functional reserve and plasticity of the brain would be overcome with time, and loss of function (including behavioral deficits) would appear (Reuhl 1991). A mechanistic hypothesis proposed that early exposures to neurotoxic chemicals reduce the number of neurons in critical areas of the brain, setting in motion a self-perpetuating process of neurodegeneration (Langston et al. 1999). In some cases, the fetal exposure needs to be combined with a neonatal exposure either to the same or different compound or to an adult exposure to cause the pathophysiology. Thus, the initial deficit would only be unmasked by subsequent exogenous influences (stress, disease, additional chemical exposure) or by the natural aging process (Costa et al. 2004).
2.4 Environmental Chemicals and Neurodegenerative Diseases: Limits and Constraints of Epidemiological Studies and the Need of Experimental Models
A role for environmental toxicants in increasing risk of NNDs, such as PD and AD, has been advanced based on case–control retrospective studies (Santibáñez et al. 2007; Van Maele-Fabry et al. 2012). Specifically, AD and PD have been associated to metals and pesticide occupational exposure, but data are far from being conclusive (Hertzman et al. 1990; Liou et al. 1997).
Testing the hypothesis of the neurodevelopmental basis of NDDs in human population presents significant methodological problems. One of the most significant challenges is the issue of silent toxicity, as the developing nervous system is endowed with marked ability to compensate for insults. At variance from neurodevelopmental disorders, exposures may have occurred many decades before the diagnosis of AD or PD; thus, the assessment of chemical exposures is almost impossible to reconstruct in retrospective studies. In addition, the lack of reliable biomarkers makes difficult to obtain information on the fetal environment of an adult individual. Prospective studies linking fetal exposure to adult diseases require decades of follow-up and may be confounded by multiple factors (i.e., coexposure, lifestyle, genetic vulnerability) modulating the risk of the original environmental insult. The methodological constraints widely recognized in neurodevelopmental toxicity studies, namely dose–response estimation, individual dimension of the exposure history, and robustness of the clinical outcome (De Felice et al. 2015), are amplified by the “time” factor in studies on the developmental origin of NDDs. Of the 112 existing EU human cohorts established for studying NDDs, only five of them have followed people continuously from birth into adulthood; though many factors are currently under study (i.e., gene background, nutrition, lifestyle), the issue of early exposure history is scarcely considered (JPND Action Group 2013).
Overall, the epidemiological and clinical data collected so far, while supporting the hypothesis of a contribution of environmental factors to NDDs, highlight the enormous difficulty of establishing causative links between each of these factors and the health outcome. The simultaneous exposure of an individual to multiple risk factors, which may interact in an additive, synergistic, or even antagonistic way along the life course, remains to be explained and defined. Recently, the exposomic approach, considering all the endogenous and environmental factors to which an individual is exposed during the life span, has suggested a procedural framework to understand the fetal origin of adult diseases. In the exposome framework, the complex origin of human chronic diseases can be unfolded by means of several omic signatures possibly describing exposure, effects, individual vulnerability, and their dynamic interplay (Wild 2012). However, peripheral biomarkers of exposure so far available for many environmental chemicals are indeed poor predictors of effects on the brain (Stangle et al. 2004); to complicate the picture further, in the case of late-onset neurologic diseases, biomarkers of effect should be able to capture early biological changes and predict later health effects.
In this framework, studies with laboratory rodents allow evaluation of important parameters, such as dose–response relationships, critical periods of susceptibility, and the relative contribution of genetic, epigenetic, and environmental factors. So far, the use of animal models has been of paramount importance to investigate the mechanisms by which chemicals influence brain development in humans (Vorhees 1986). In particular, animal models are a powerful tool to test what combination of adverse environmental factors produces significant disruption of neurobehavioral development that leads to clinically relevant outcome in later stages. Notably, this kind of information can only be achieved by testing the living organism, as the face validity of an animal model of NDD consists primarily in a robust behavioral phenotype that can be associated to the appearance of neurodegenerative features (Crawley 2012).
3 Assessing the Role of Environmental Exposures in Neurodegenerative Diseases’ Etiology: An Overview of the in Vivo Models
3.1 Introduction
The role of environmental chemicals and their mechanisms of action in the etiology of sporadic AD and PD have been extensively discussed in the recent review by Chin-Chan et al. (2015). Based on epidemiological and experimental evidence, the authors identified neurotoxic metals, such as lead (Pb), mercury (Hg), aluminum (Al), cadmium (Cd), manganese (Mn), and arsenic (As), as well as some classes of pesticides as significant environmental risk factors. As mentioned above, most of studies suggesting association between these chemical agents and idiopathic AD or PD refer to occupational exposure (Santibáñez et al. 2007; Firestone et al. 2010). Many are case–control studies (Parrón et al. 2011) and very few population studies considered internal exposure to a specific compound in relation to disease occurrence (Richardson et al. 2014; Kim et al. 2015). The mechanisms by which chemicals with very different modes of action might promote neurodegeneration are still undetermined. For example, the pesticide class includes more than 1000 active ingredients including insecticides, herbicides, and fungicides. Among those possibly implicated in AD or PD etiology, the organophosphorus compounds such as carbamates and organophosphate (OP) are potent inhibitors of acetylcholinesterase (AChE) and could affect APP processing (Giacobini et al. 1996); organochlorines (OC) can impair the functioning of the mitochondrial system and produce free radicals increasing oxidative stress and promoting cell death; bipyridyls such as paraquat (PQ) can generate free radicals that are able to cross the blood–brain barrier and damage neurons (Kumar et al. 2015).
In their extensive review, Chin-Chan et al. (2015) described several experimental studies (in vitro and in vivo) that have focused on metabolic pathways relevant for AD and PD pathogenesis. It is worth noting that in the large majority of the in vivo studies reviewed, rodents or non-human primates were exposed to chemicals at the adult stage. The metabolism of APP, phosphorylation of tau protein, aggregation of α-synuclein, production of proinflammatory cytokines, and reactive oxygen species generation appear as common targets of metals and pesticides’ neurotoxicity following adult exposure. Furthermore, transgenic (Tg) models carrying mutation in candidate genes support the hypothesis that both genetic vulnerability and environmental neurotoxicants converge on neuroinflammation as an outcome linked or leading to neurodegeneration. It is worth noting that the very earliest neuronal and pathological changes characteristic of AD suggest oxidative stress as a very early contributor to the disease (Nunomura et al. 2001) and that oxidative stress appears to play a major role in degeneration of DA neurons in PD (Dias et al. 2013).
In the following sections, we will present the more robust experimental studies including fetal and/or neonatal exposure to known environmental neurotoxicants, which support the link between chemical exposure and hallmarks of neurodegeneration at the adult stage. In many of the studies, the significant alteration in one or more of these hallmarks was also paralleled by motor and/or cognitive disturbances, reproducing in the rodent model the clinical behavioral traits of AD and PD affected individuals in the initial stages of the disease. We chose to include in this overview also rodent studies exploring the delayed neurobehavioral effects of maternal infection. The paradigm of maternal infection models a condition of early immune activation and consequent exposure of the fetal brain to proinflammatory cytokines: This can affect the development of brain circuitries leading to neurobehavioral dysfunctions in the progeny (Knuesel et al. 2014). As shown below, studies combining maternal infection with a subsequent toxic insults support the validity of the multiple hit hypothesis, as an unfavorable fetal environment increases later vulnerability to neurotoxicants. Tables 1, 2 and 3 illustrate synthetically the experimental studies discussed in this chapter.
3.2 Alzheimer’s Disease (AD)
AD is the most common neurodegenerative disease worldwide. The main pathological hallmarks of AD are beta-amyloid plaques (Aβ) and neurofibrillary tangles (NTFs) composed of hyperphosphorylated tau protein (p-tau), which spread through the cortex in a predictable pattern as Alzheimer’s disease progresses causing nerve cell degeneration and cognitive impairment (Selkoe and Schenk 2003). Early onset familial AD is rare and is characterized by autosomal dominant heritability, due to mutations in the genes for APP, presenilin-1 (PSEN1), and presenilin-2 (PSEN2). The prevalent form of AD typically develops after 60 years of age; the etiology of late-onset sporadic AD (LOAD) has not yet been resolved, but it has been suggested that it could result from a multifactorial process involving both genetic and environmental factors (Reitz et al. 2011). Diseases presenting increased inflammatory processes such as hypercholesterolemia, hypertension, atherosclerosis, coronary heart disease, obesity, and diabetes are indeed risk factors for AD (Blennow et al. 2006), and thus, inflammation is suggested to have a causal role also in LOAD pathogenesis. Several candidate risk genes have been identified for LOAD: They mainly involve proteins implicated in critical pathogenic pathways, namely Aβ synthesis and processing, oxidative stress, and inflammation/apoptosis (Ballard et al. 2011).
Adverse environmental factors might further increase the risk impose by genetic makeup, by acting on cell pathways implicated in AD. Neurotoxic metals such as Pb, Hg, Al, Cd, and As, as well as some pesticides and metal-based nanoparticles, have been involved in AD due to their ability to increase Aβ peptide and the phosphorylation of tau protein, causing senile/amyloid plaques and NFTs characteristic of AD, and to enhance oxidative stress and inflammatory responses (Casado et al. 2008). In spite of this consistent evidence, studies considering environmental exposure have been underrepresented in the AD literature, possibly due to the challenges of retrospective exposure assessment in older adults (Bakulski et al. 2012).
3.2.1 Heavy Metals and AD
-
Lead
Among heavy metals, a large body of clinical data supports an association between occupational Pb exposure and cognitive decline with aging as higher levels of Pb in blood and/or bone were accompanied by poor cognitive performance in different cognitive tests (Nordberg et al. 2000; Wright et al. 2003; Weisskopf et al. 2004). Pb is a well-known neurotoxicant in children. Even at relatively low and subclinical levels, epidemiologic studies demonstrate prenatal and childhood Pb exposure affects IQ and behavior up to young adulthood (Lanphear et al. 2005; McFarlane et al. 2013). Recent studies using both in vivo models and primary neuronal cultures indicate that Pb exposure during pregnancy may negatively modify important neuronal pathways implicated in synaptic plasticity, learning, and memory (Neal and Guilarte 2010). In this framework, the potential link between developmental exposure to Pb and increased risk of developing AD later in life has been thoroughly investigated in experimental studies with rodents and primates. Li et al. (2010) found tau hyperphosphorylation and Aβ increase in hippocampus associated with deficits in learning and memory in mice offspring exposed to Pb from conception to weaning.
A line of research investigated the link between perinatal Pb exposure, alteration of APP metabolism, and cognitive impairment at later life stages. Basha et al. (2005) exposed rats to Pb from birth through postnatal day (PND) 20 by systemic administration and monitored the lifetime expression of the APP gene, finding overexpression of APP levels and Aβ aggregation 20 months after exposure to Pb had ceased. These results have been replicated on monkeys, exposed to Pb from birth until the end of the first year of age (Wu et al. 2008). The expression of AD-related genes (APP, β-site APP cleaving enzyme 1 (BACE1)), as well as their transcriptional regulator (Sp1), was elevated in aged (23-year-old) monkeys following early exposure to Pb. Furthermore, levels of amyloid plaques increased in the frontal cortex. These latent effects were paralleled by a decrease in DNA methyltransferase activity and higher levels of oxidative damage to DNA, indicating that epigenetic mechanisms elicited by Pb in early life influenced the expression of AD-related genes and promoted DNA damage and pathogenesis.
Bihaqi et al. (2014) evaluated the impact of Pb exposure at different lifetimes (during either development or adulthood) on cognitive functions and biochemical pathways associated with AD in mice. This study showed that only mice early exposed to Pb (0.2 % Pb acetate), namely during the first 20 days of postnatal life through the mother’s milk, showed cognitive impairment at 18 months of age, which further progressed by 24 months. In Pb-exposed rats, cognitive impairment was accompanied by up-regulation of AD biomarkers (APP, Αβ, and BACE1) and overabundance of p-tau. Long-term effects of developmental exposure to Pb has been evaluated also in relation to tau pathology in non-human primates (Bihaqi and Zawia 2013). In this study, female monkeys were exposed to Pb (1.5 mg/kg/day) from birth until the end of the first year of life, and then, they were examined at 23 years of age. Results showed that Pb exposure elevated the mRNA and protein levels of tau as well as its transcriptional regulators and favoured abundant tau phosphorylation in the frontal cortex of aged primates. This study suggests some evidence that Pb during development triggers neurodegenerative processes that have much in common with those implicated in human AD.
Due to the role of developmental exposure of Pb in increase of Aβ, which is known to generate reactive oxygen species in the aging brain, Bolin et al. (2006) investigated the hypothesis that early exposure to Pb, in specific developmental windows, determines the outcome of oxidative damage late in life. Rat pups were exposed to Pb (0.2 % Pb acetate) at different ages (from PND 1 to 20 or from 18 to 20 months), showing that the level of 8-hydroxy-2′-deoxyguanosine (8-oxo-dG), one of the major products of DNA oxidation and a reliable marker of oxidative stress, was elevated 20 months after exposure to Pb had ceased. The effect of Pb on 8-oxo-dG levels did not occur if animals were exposed to Pb only in old age. These increases in DNA damage occurred in the absence of any Pb-induced changes in general antioxidant capacity in the cerebral cortex.
The existence of a critical phase of sensitivity to Pb effects was also supported by other studies. Dosunmu et al. (2012) assessed global gene expression patterns in mice, developmentally exposed to Pb (0.2 % Pb acetate) from gestational day (GD) 13 until PND 20. The selected time points of PND 20 and 700 represented early and late time points of the animal for microarray analysis, where genes that were down- and up-regulated were identified, clustered, and analyzed for their relationship to DNA methylation. Prior exposure to Pb revealed a repression of genes related to the immune response, metal-binding, metabolism, and transcription/transduction coupling. More in detail, the authors identified 150 genes for a transcriptional profile of normal aging and environmentally perturbed aging. In normal aging, those genes are up-regulated, but prior developmental Pb exposure caused a strong repression of these genes. DNA methylation appears to play an important role in the down-regulation of these genes suggesting that early-life exposure to Pb interferes with the methylation pattern of genes and has an impact on the organism’s capacity to respond in old age. These findings would support the LEARn model of NDDs, as the toxic effects of Pb are maintained through the life span in the form of latent epigenetic changes.
Recently, Ashok et al. (2015) treated rats with a mixture of As + Cd + Pb at environmentally relevant concentration, from GD 5 to 6 months of age. They identified dose-dependent increase of Αβ in frontal cortex and hippocampus as early as the post-weaning age. The metal mixture activated the proamyloidogenic pathway, mediated by increase in APP, and subsequent BACE1 and PS-mediated APP processing. Investigating the mechanism of Aβ induction revealed an augmentation in oxidative stress-dependent neuroinflammation that stimulated APP expression. When the authors examined the effects of individual metals and binary mixtures in comparison with the tertiary mixtures, they found that Pb triggered maximum induction of Aβ, whereas individual As or Cd had a relatively non significant effect on Aβ despite enhanced APP. Together, these data demonstrate that exposure to As + Cd + Pb induces earlier manifestation of AD-like pathology that is synergistic, and oxidative stress, and inflammation dependent. These data open the way to further experimental research modeling real exposure scenarios to mixtures of chemicals.
Developmental origin of Pb-induced neurodegenerative disease has been investigated also in zebrafish (Dania rerio), an aquatic vertebrate model system, which presents a high sequence homology (i.e., 70 %) with the human genome (Howe et al. 2013). Zebrafish are increasingly used to understand the mechanisms of developmental Pb neurotoxicity through evaluation of changes in gene expression and neurobehavioral alterations (Lee and Freeman 2014). Data collected in this model generally supported the hypothesis that developmental exposure to Pb exhibits latent effects on the expression of genes that are involved in neurodegenerative processes during old age.
3.2.2 Pesticides and AD
Several epidemiological studies have suggested the association between pesticides and impairment of cognitive functions and AD-like dementia, but the underlying mechanisms have been poorly explored in experimental models (Baldi et al. 2011; Hayden et al. 2010). Among the class of pesticides with neurotoxic activity, OPs are the subject of increasing concern. OPs make up approximately 50 % of all insecticides used in the world (Colborn 2006) and are intensively investigated for their suspected developmental neurotoxicity (Rosas and Eskenazi 2008). These compounds, largely used in agriculture, as well as in the home and garden, for pest control, exert their acute neurotoxic effects through AChE inhibition and consequent cholinergic stimulation. However, increasing evidence indicates that, as other environmental chemicals, OPs exert developmental toxicity at low doses with mechanisms different from those observed at higher doses, including modulation of several family of genes involved in brain development (Moreira et al. 2010). In vitro studies show that OP compounds impair mitochondrial bioenergetics and induce ROS generation (Wani et al. 2014). In particular, as concern chlorpyrifos (CPF), the most widely applied compound in the OP class in the USA, it interferes with brain and behavior development through a variety of cellular and molecular mechanisms that appear as independent from inhibition of AChE (Androutsopolous et al. 2013; Eaton et al. 2008; Venerosi et al. 2012).
Notwithstanding the recognized effect of this OP insecticide on oxidative stress end points (Cole et al. 2011), developmental exposure to these compounds has never been considered under the perspective of neurodegenerative disease etiology. However, three recent studies using a genetic model of vulnerability to AD, the APP Tg mice (Tg2576 mice) evidenced a potential increased susceptibility to both OP insecticides and bipyridyl herbicide PQ. Specifically, CPF caused a significant increase in Aβ levels in the cortex and hippocampus, as well as increased memory loss and reduced motor activity in Tg2576 mice 6 months after a single administration (Salazar et al. 2011), an effect that has not been confirmed by Peris-Sampedro et al. (2014). Another study showed that treatment of wild type and Tg2576 mice with PQ (10 mg/kg/twice a week/3 weeks) produced a significant increase in Aβ levels in Tg mice, associated with mitochondrial oxidative damage in cerebral cortex and impairment of learning and memory. Interestingly, the overexpression of peroxiredoxin 3, a mitochondrial antioxidant defense enzyme, produced an improvement in cognitive functions and a significant reduction in Aβ levels in Tg2576 exposed to PQ (Chen et al. 2012), suggesting that pro-oxidant xenobiotics like PQ can contribute to AD.
3.2.3 Maternal Infection and AD
As illustrated previously, experimental and clinical data support the inflammation hypothesis of AD etiology. It suggests that neuroinflammatory response triggers and follows the Aβ increase in the AD brain and significantly interferes with memory processes (Heneka et al. 2015; Heppner et al. 2015). The administration of the bacterial endotoxin lipopolysaccharide (LPS) or polyinosinic:polycytidylic acid (PolyI:C) to pregnant rodents was among the first animal models examining the long-term consequences of prenatal immune challenge on adult brain functioning (Meyer 2014). In experimental studies, LPS is used to increase proinflammatory cytokines in the pregnant female’s organism, mimicking an infective state that can induce abnormalities in the fetus neurodevelopment (Knuesel et al. 2014).
Chen et al. (2011) injected female mice with LPS (50 mg/kg) daily during late pregnancy (from GD 15 to GD 17). The offspring exposed prenatally to LPS, although showing normal development of sensorimotor and cognitive functions, had an accelerated age-related impairment of both spatial and non-spatial learning and memory in middle age. In a subsequent study by Krstic et al. (2012), female mice received a single injection of PolyI:C (5 mg/kg) at GD 17. Adult and aged offspring showed cognitive decline and AD-like neuropathology such as increase of APP protein and its proteolytic fragments and altered tau phosphorylation, in parallel with impairments in working memory. A second immune challenge in adulthood exacerbated this pathological phenotype, with appearance of Aβ-like plaque deposition. In this same study, Tg AD mice (3xTg-AD), overexpressing the human variants of AD-relevant genes, were challenged with PolyI:C at the preplaque stage of 4 months and showed accumulation of APP and increase of Aβ deposits resembling the morphology of Aβ plaques in human patients with AD. Taken together, these results indicated that systemic immune challenges are able to promote AD-like neuropathology in both wild-type (PolyI:C exposure at GD17) and genetically (3xTg-AD) predisposed animals, in agreement with both causative and exacerbating role of systemic immune challenges on AD development.
3.3 Parkinson’s Disease (PD)
Parkinson’s disease (PD) is the second most common neurodegenerative disease after AD, characterized by depletion of dopaminergic cell bodies in the substantia nigra pars compacta (SNpc) with subsequent loss of dopamine (DA) in the nigrostriatal system, and intracytoplasmic inclusions termed as Lewy bodies, containing aggregates of the protein α-synuclein as well as other substances (Barlow et al. 2007). Studies on familial PD show an autosomal pattern, either dominant or recessive, identifying some genetic mutations and chromosal loci responsible for this form. Several loci (PARK1-15) and genes have been linked to familial forms of the disease. The majority of PD cases are, however, sporadic “idiopathic” forms, and the recent application of genome-wide screening revealed almost 20 genes implicated in mitochondrial function, in detoxification, and/or protection against oxidative stress that might contribute to disease risk. It is striking that none of the genes implicated to date is specifically expressed in DA neurons. Instead, many of the implicated genes have rather general neuronal or cellular functions in and outside of the brain, suggesting that DA neurons are more susceptible to stress than other neurons (Lees et al. 2009; Westerlund et al. 2010).
The cause of sporadic PD is unknown, with uncertainty about the role of environmental toxins and genetic factors. The environmental hypothesis posits that PD-related neurodegeneration results from exposure to a dopaminergic neurotoxin. The finding that people intoxicated with the chemical 1-methyl-4pheny l-1, 2, 3, 6-tetrahydropyridine (MPTP) developed a syndrome nearly identical to PD (Langston et al. 1983) prompted the interest in environmental causes of PD (Tanner et al. 2014). The herbicide PQ is structurally similar to 1-methyl-4-phenylpyridinium (MPP+), the active metabolite of MPTP. Similar to MPP+, the insecticide rotenone is also a mitochondrial poison present in the environment. Yet, there are no convincing data to implicate any specific toxin as a cause of sporadic PD, and chronic environmental exposure to MPP+ or rotenone is unlikely to cause PD per se. Another possibility is that an endogenous toxin may be responsible for PD neurodegeneration. Distortions of normal DA metabolism might create toxic substances (i.e., reactive oxygen species) because of environmental exposures or inherited differences in metabolic pathways (Dauer and Przedborski 2003; Sandy et al. 1996).
Several environmental contaminants, known to cause nigrostriatal damage at toxic concentrations, could contribute to PD by interference with mitochondrial respiratory functions and ROS generation (Di Monte 2003; Jenner 2003). The insecticides PQ, rotenone, and the fungicide MB are agricultural chemicals that have each been linked to nigrostriatal damage and the emergence of parkinsonian symptoms, via epidemiological surveys, clinical case reports, and/or animal models. Exposure to various metals has long been suggested to increase risk of PD, based on experimental studies, but human evidence remains inconclusive (Lai et al. 2002; Tanner et al. 2014).
3.3.1 Heavy Metals and PD
-
Iron
Iron (Fe2+), the most abundant metal present in the human brain, has been proposed to play a role in the pathogenesis of PD for its pro-oxidants characteristics that may lead to ROS generation (Sian-Hülsmann et al. 2011). Several studies have focused on the ability of Fe2+, as well as other metals to facilitate the aggregation of the PD-related protein α-synuclein, but very few studies investigated the impact of early exposure to Fe2+ on development of PD hallmarks in adult life. In the study by Fredriksson et al. (1999) at the age of 3 months, offspring exposed in utero to Fe2+ (3.7 or 37.0 mg/kg) on GD 10–12 showed marked hypokinesia and lack of habituation in spontaneous activity. These effects were more pronounced in mice treated with the higher dose that showed also a dose-dependent impaired performance in the radial arm maze. Brain Fe2+ content was significantly increased in the basal ganglia, but not in the frontal cortex at the higher dose group. In a second study from the same group (Fredriksson et al. 2000), mice were treated in the neonatal stage with Fe2+ (7.5 mg/kg) on either PND 3–5, 10–12, or 19–21. Adult mice treated with Fe2+ on PND 3–5 and 10–12 showed effects similar to those found after gestational exposure on spontaneous motor behavior and learning performance, more marked in animals treated at PND 10–12.
The role of Fe2+ in oxidative stress and superoxide dismutase (SOD) activity may be implicated in the adverse delayed effects of this metal (Dal-Pizzol et al. 2001). Male rats were treated with Fe2+ (7.5 or 15 mg/kg) from PND 10 to 12, measuring at 3 months different indexes of oxidative stress. Notably and according to previous clinical and experimental studies, this study demonstrated that Fe2+ exposure during a critical neonatal period induced oxidative stress and modulated SOD activity restricted to SN in adult rats. Finally, Kaur et al. (2007) investigated the role of early exposure of Fe2+ at a dose (120 µg/g of carbonyl iron) equivalent to that found in iron-fortified human infant formula as a risk factor for PD-like neurodegeneration. Neonatally exposed mice were challenged at adulthood with the toxin MPTP that induces depletion of neostriatal dopamine. Neonatal Fe2+ feeding alone did not induce decrease in striatum (ST) dopamine levels in 2-month-old mice, also when they were challenged with MPTP. However, at 12, 16, and 24 months of age, mice treated with Fe2+ showed more marked DA depletion following acute administration of MPTP than vehicle-treated mice. It is worth noting that Fe2+ is important for many biological reactions such as the synthesis and release of neurotransmitters. In particular, the neonatal period is critical for the establishment of normal Fe2+ content in the adult brain and its regional distribution; deficiency such as excess of this metal can perturb the typical neurological development. These results highlight the need of epidemiological research in humans, especially on the potential long-term effects of Fe2+ supplementation during infancy (i.e., milk) on neurological functions in adulthood.
-
Manganese
Manganese (Mn) was related to PD since 1837, when it was noted that high Mn exposures caused an extrapyramidal syndrome that resembles the dystonic movements associated with parkinsonian symptoms (Couper 1837; Jankovic 2005). Several evidence on the influence of Mn on neurodegenerative processes has been collected in in vitro models. A single study comparing in vitro and in vivo experiments showed that oxidative stress, mitochondrial dysfunction, and neuroinflammation are implicated in Mn-induced neurodegeneration (Milatovic et al. 2009).
Two experimental studies suggest that early Mn exposure might have profound effects on later-life susceptibility to neurotoxins and subsequent degeneration (Cordova et al. 2012, 2013). Cordova et al. (2012) show for the first time in vivo the link between early Mn exposure (from PND 8 to 12) and the modulation of intracellular signaling pathways. Oxidative stress, DA cell death, and later-life impairment in motor function were also observed. In a subsequent study, the same authors investigated the effects of longer exposure to Mn in developing rats. They demonstrated that exposure to Mn (5, 10, and 20 mg/kg) from PND 8 to 27 caused significant deficits in motor coordination and increased signs of oxidative stress in the ST in rats at 3, 4, or 5 weeks of age (Cordova et al. 2013).
3.3.2 Pesticides and PD
One-hit studies
Experimental models assessing the causative link between exposure to pesticides and PD-like neurodegeneration have focused on the effects of environmental toxins on the DA nigrostriatal system. This system develops both pre- and postnatally, with receptor development occurring predominantly in the postnatal period (Giorgi et al. 1987; Voorn et al. 1988). As described above, the chemical structure of the insecticide PQ resembles that of MPP+, the toxic metabolite that mediates the effects of the parkinsonism-inducing agent MPTP. Similarly, administration of PQ to mice produces several neurotoxic effects, including damage of the DA nigrostriatal system (McCormack et al. 2002). Dithiocarbamate fungicides also possess DA activity: Maneb (MB) administered acutely exacerbates the behavioral symptoms induced by MPTP in mice (hypokinesia and catalepsy). Similar effects have been described with the OC herbicide dieldrin, an inhibitor of mitochondrial respiration.
Richardson et al. (2006) showed that perinatal exposure to low doses of dieldrin (0.3, 1, or 3 mg/kg every 3 days) during gestation and lactation altered the levels of the dopamine transporter (DAT) and vesicular monoamine transporter 2 (VMAT2) at 12 weeks of age. The alterations of both the DA markers were exacerbated by MPTP injections at 12 weeks. Wilson et al. (2014) investigated the effects of in utero exposure to endosulfan, an OC insecticide, in male offspring at 3 months of age. Female mice received endosulfan (1 mg/kg) every 2 days from 2 weeks before breeding until end of lactation. The authors found a reduced expression of DAT and tyrosine hydroxylase (TH) in the ST of treated mice, exacerbated by exposure to additional insults such as MPTP. Endosulfan failed to cause the same effects when administered at the same dose and for the same period to adult mice. These findings indicate that gestation and lactation are critical windows of sensitivity to endosulfan exposure and development of nigrostriatal DA system.
Two studies evaluated the effects of developmental exposure to the herbicide atrazine (ATR) during gestation and lactation on DA system development (Li et al. 2014; Sun et al. 2014). The in utero exposure to ATR (25 or 50 mg/kg) from GD 0 to PND 1 reduced the level of DA and expression of orphan nuclear hormone (Nurr1), VMAT2, DAT, and TH genes in ST and SN, respectively, at 6 months of age (Li et al. 2014). In a second study, the authors assessed the effects of a more prolonged exposure to ATR given to pregnant mice from GD 5 to PND 22 at the same doses of the previous study: DA concentrations and mRNA levels of Nurr1 were decreased in the offspring at 12 months of age. Decreased Nurr1 levels paralleled changes in the mRNA levels of VMAT2, which controls the transport and reuptake of DA (Sun et al. 2014).
-
Two-hit studies
In line with the double hit hypothesis, it has been suggested that developmental exposure to either PQ or MB alone, or in combination, would result in permanent nigrostriatal DA system neurotoxicity, and secondly, it would render this system more susceptible to a second chemical challenge later in life. In the study of Thiruchelvam et al. (2002), mice were exposed to PQ, MB, and PQ + MB from PND 5 to 19 and then rechallenged with the single agents or with the combination at 6.5 months of age. Developmental and adult exposure to PQ + MB combination produced the greatest damage of the nigrostriatal DA system and a significant reduction in motor activity. Furthermore, increased sensitivity to the rechallenge with PQ and MB either alone or in combination was observed in only those animals treated neonatally with the combination. Vice versa, exposure to PQ or MB alone produced minimal changes, but after adult rechallenge, a significant decrease in DA levels and nigral cell count was found, confirming that adult re-exposure might unmask a condition of silent toxicity. Thus, developmental exposures of mice to PQ + MB combination led not only to a permanent and selective loss of DA neurons in the SNpc but also enhanced the impact of these pesticides administered during adulthood relative to developmental only or adult only treatment. Exposure to MB alone during gestation resulted in enhanced response to PQ in adulthood, including notable reductions in levels of DA and its metabolites and loss of nigral DA neurons, despite the structural dissimilarity and the different mode of action of PQ and MB (Cory-Slechta et al. 2005).
Another line of research considered the role of in utero exposure to MB, combined with subsequent exposure to PQ, in disrupting the nigrostriatal system (Barlow et al. 2004). Pregnant mice were exposed to MB or PQ on GD 10–17, at doses ten times lower than those used in young adult studies; 2-month-old offspring received either PQ or MB at the doses used for adult mice for 8 days. One week after the termination of the second treatment, mice were assessed in a motor activity task and then sacrificed to measure brain DA markers. The authors observed only in males exposed prenatally to MB and then in the adulthood to PQ, a 95 % decrease of locomotor activity, associated to decreased levels of striatal DA, increased striatal DA turnover, and selective reduction in DA neurons of the SNpc. The authors concluded that the sequence of exposures is critical, since prenatal exposure to PQ followed by adult challenges with MB failed to produce marked alteration of locomotor activity or any DA neuron loss (Barlow et al. 2004).
3.3.3 Maternal Infection and PD
Inflammation and reduced antioxidant defenses (i.e., reduced glutathione activity) have been implicated in PD pathogenesis (McGeer et al. 2001). Intrauterine infection might lead to nigral cell loss in the fetal brain and subsequent permanent decrease in DA neurons, secondary to inflammation. In such framework, Zhu et al. (2007) assessed the effects of prenatal LPS exposure on glutathione (GSH) metabolism in rat brain. They observed a disturbance of GSH homeostasis in offspring of dams administered with LPS at GD 10.5, which possibly makes DA neurons more susceptible to the secondary chemical insult. Wang et al. (2009) have observed significant reduction of DA and serotonin (5-HT) levels accompanied by loss of DA and 5-HT neurons in SN and in the dorsal raphe nucleus (DRN) in adult rats offspring of pregnant dams exposed to a single injection of LPS (33 μg/kg) at GD 10.5. Fan et al. (2011) assessed the effects of intracerebral injection of LPS (1 mg/kg) in male rat pups at PND 5. Although on PND 70 rats spontaneously recovered the neurobehavioral dysfunction induced by LPS, the authors observed persistent injury to DA system and strong inflammatory response including increased activation of microglia and inflammatory cytokines in the brain. When challenged with METH (0.5 mg/kg), LPS-exposed rats showed increased METH-induced locomotion and stereotyped behaviors as compared to control rats (Tien et al. 2011).
3.3.4 Multiple Hits in PD: Maternal Infection and Chemical Insult Combination
Other their life span, human beings are exposed to mixtures of chemicals as well as to several non-chemical risk factors. One of the main questions in the assessment of the environmental hypothesis of PD etiology is whether sequential exposures to different kinds of risk factors across the lifetime would result in cumulative neurotoxicity to the nigrostriatal DA system. Various models based on “multiple hits” have been developed, assuming that prenatal inflammation makes the brain more susceptible to subsequent exposure to DA neurotoxins.
The first studies combining maternal infection with exposure to an environmental neurotoxicant at a later life stage were carried out by Ling et al. (2004a, b). Rats were exposed to LPS prenatally and then administered with a subtoxic dose of the DA neurotoxin rotenone (1.25 mg/kg per day for 14 days) when 16 months old. The combined effects of prenatal LPS and postnatal rotenone exposure produced higher DA cell loss compared with the effects of single exposure to either LPS or rotenone. Prenatal LPS exposure also led to increased levels of oxidized proteins and the formation of α-synuclein and eosin-positive inclusions resembling Lewy bodies. In the second study, the same authors (Ling et al. 2004a, b) injected on PND 99 the neurotoxin 6-hydroxydopamine (6-OHDA) or saline into animals exposed to either LPS or saline prenatally. The results showed that animals exposed to prenatal LPS or postnatal 6-OHDA alone had fewer DA neurons than controls, while the two toxins combined produced a greater loss. They conclude that prenatal exposure to LPS produces permanent cell loss accompanied by an inflammatory state that leads to further DA neuron loss once in the presence of subsequent neurotoxin exposure.
Fan et al. (2011a) found that neonatal intracerebral injection of LPS following administration of rotenone at low dose (1.25 mg/kg) for 14 days from PND 70 resulted in PD-like neurobehavioral deficits later in life. In agreement with this hypothesis, Tien et al. (2013) demonstrated that neonatal LPS exposure enhanced the rotenone-induced accumulation of α-synuclein aggregation and DAT protein expression in the SN. Overall, these studies show that brain inflammation in early life may enhance adult susceptibility to develop neurodegenerative hallmarks triggered by environmental toxins.
To compare the effects of gestational LPS exposure with neonatal systemic LPS exposure on adult DA neuron susceptibility to rotenone neurotoxicity, rats were administered with LPS at PND 5 (Cai et al. 2013) and, at adulthood, were challenged with rotenone at a dose of 1.25 mg/kg per day for 14 days. Briefly, rotenone induced loss of DA neurons and PD-like motor impairment in 3-month-old rats that had experienced neonatal LPS exposure, but not in those without the LPS exposure. These results support the view that although neonatal systemic LPS exposure may not necessarily lead to loss of DA neurons in the SN, it could cause persistent functional alterations that predispose the nigrostriatal system to be damaged by environmental toxins.
Another recent line of evidence concerns air pollution, which has been associated with adverse neurological and behavioral effects in children and adults. Increases in neuroinflammation, oxidative stress, and glial activation have been identified as putative mechanisms by which air pollution exposures may impair central nervous system function in adults. Particulate matter, one of many components of ambient outdoor air pollution, causes elevation in cytokines and oxidative stress in the brain (Campbell et al. 2005). Given the evidence suggesting susceptibility of both the SN and ST to components of air pollution, two studies assessed whether exposure of mice to concentrated ambient ultrafine particles (CAPS; <100 nm diameter) during the first two weeks of life would alter susceptibility to induction of the PD phenotype by the combined administration of PQ + MB, utilizing 10 mg/kg PQ and 30 mg/kg MB 2 × per week for 6 weeks (Thiruchelvam et al. 2000, 2003). Animals treated with CAPS in the early postnatal period show enhanced response to PQ + MB combination. Both CAPS and PQ + MB elevated glutamate levels in ST, consistent with potential excitotoxicity. These findings demonstrate the ability of postnatal CAPS to produce locomotor dysfunction and dopaminergic and glutamatergic changes, independent of PQ + MB, in brain regions involved in PD (Allen et al. 2014).
4 Concluding Remarks
Increasing evidence indicates that events occurring in the earliest stages of human development may influence both resilience and vulnerability to several adult diseases, including neuropsychiatric and neurologic disorders. As stated by Olden et al. (2011), the timing of environmental exposure is a crucial factor that influences the size of the gene–environment interaction: Whereas genes may contain the potential for adverse health outcomes, subsequent exposure to environmental triggers is required to initiate physiological or pathological pathways responsible for health and disease.
Experimental models confirm this general view. Research in animals has clearly shown that diverse environmental stressors may interfere with typical brain developmental trajectories in critical time windows, inducing silent subclinical alterations that may hesitate in pathophysiology and overt functional (e.g., behavioral) deficits at a later life stage. The bulk of data produced by developmental neurotoxicologists since the 1980s has started a series of epidemiological studies to assess the possible link between subtoxic exposure to chemical pollutants and neurobehavioral effects in children. Thanks to such combined effort, recent advances in research offer important clues into the complex etiology of autism and other neurodevelopmental disorders, indicating that developmental exposure to chemicals cannot be ruled out (Rossignol et al. 2014). Specifically, variations in candidate genes may confer higher individual vulnerability to environmental toxicants. Of note, the convergence of risk factors on the same cell/molecular pathways in critical developmental windows, combined with a vulnerable gene makeup, would trigger the development of the disorders or predispose to adverse health outcome later on. As an example, children at risk for autism may present constitutionally reduced antioxidant defenses: This may render the individual more vulnerable to oxidative stress and inflammatory processes produced by both xenobiotic exposure and maternal infection during pregnancy (Rose et al. 2012).
A similar research effort has not been taking place as concerns the developmental origin of NDDs and the role of environmental factors in increasing risk. As discussed in Chap. 1, the long latency between exposure and disease occurrence, the difficulty of reconstructing exposures that occurred several decades before disease manifestation, and the wealth of factors which the individual is exposed to during the life course make the developmental origin of NDD a promising but difficulty provable hypothesis. Nonetheless, given the huge public health impact of NDDs, identification of early risk factors would be crucial to design prevention and/or intervention strategies: In this perspective, the comprehension of the environmental etiology of major NDDs requires innovative study paradigms with multifaceted and multidisciplinary approaches.
The experimental findings presented in Chap. 2 prove the utility of in vivo models and support a role of environmental chemicals in increasing risk of NDDs. These experiments showed not only that an environmental insult in early life has long-term irreversible consequences, but also that the insult must occur during a critical period in development to have its maximal effect. Gestational and neonatal exposure to metals and pesticides as well as experimentally induced maternal infection both lead to alterations in developmental programming that are expressed as an irreversibly altered function. The functional effects often include significant motor and/or cognitive impairments resembling the pathological phenotypes of major human NDDs. Most of these models present strong construct validity, as the more robust hallmarks of AD and PD are associated with the functional impairment. Furthermore, epigenetic processes seem to play a key role in the mechanisms underlying these phenomena, as shown by the finding that perinatal exposure to Pb modulates the expression of AD-related genes, influencing the course of amyloidogenesis and oxidative DNA damage via DNA methylation (Dosunmu et al. 2012). Among environmental pollutants, Pb is a paradigmatic example of a developmental neurotoxicant able to interfere with developmental programming through different and possibly interrelated mechanisms. These include the antagonism of NMDA receptors in the early developmental phases, which is the key event at the basis of Pb interference with synaptogenesis, neural network formation, and behavioral plasticity (Toscano and Guilarte 2005), but Pb also induces latent changes in antioxidant defenses and mitochondrial redox dysfunction that may trigger neurodegeneration-related pathways at later life stages (Caito and Aschner 2015).
The experiments assessing the double or multiple hit hypothesis, either by rechallenging the animal with the same or a different chemical compounds at different life stages or by presenting a chemical insult in the adulthood following fetal exposure to maternal inflammation, support the LEARn hypothesis advanced by Lahiri et al. (2007). The end result of the fetal insult in fact is an animal that is sensitized such that it will be more susceptible to diseases later in life, provided the occurrence of a second hit. In such framework, the exposure of the fetal brain to proinflammatory cytokines secondary to maternal infection appears as a major causative factor of altered developmental programming and enhanced vulnerability. This supports the view that neurodevelopmental and neurodegenerative disorders do share pathogenic pathways: Abnormal immune activation in the early stage of brain development may constitute the common event predisposing to disease at some point in the life span of the individual.
The question arising at this point is as to whether experimental findings may help to fill the huge gaps in knowledge that lay beneath the developmental hypothesis for NDDs. Whereas some of the studies here reviewed offer interesting clues for the mechanistic underpinnings of chemical-related effects, experimental models on this topic are still at their beginning. The very nature of the problem requires the establishment of prospective animal cohorts: This implies the use of developmental exposures with multilevel analysis of the embryos, fetus, and pups, as well as of later life stages to trace dysfunction/disease. Research must use environmentally relevant doses, dose–response curves, and the examination of the relationship between the molecular mechanism proposed and the disease/dysfunction studied. This would also require the use of the new technologies of gene expression profiling and epigenetics: A critical component is the development of a direct correlation and eventually a cause–effect relationship between the alterations in gene expression during the development (either increased, decreased, or inappropriate timing) to alterations in “omic” signatures that may predict a specific disease or dysfunction later in life. To date, no available biomarker is a clear and validated indicator of typical brain development. Recent studies suggest that placental miRNA expression profiles and DNA methylation of specific genes are associated with measures of neurobehavioral outcome in the infants as well as with increased risks of neurological and NDDs (Sheinerman and Umansky 2013); altered Aβ protein in plasma is related with neurodegenerative risk after prenatal Pb exposure (Mazumdar et al. 2012). In vivo models could be instrumental to identify robust peripheral biomarkers of exposure, effects, and susceptibility, to be subsequently verified in large prospective human cohort studies to establish biologically plausible links between early chemical exposure and later health effects.
References
Allen JL, Liu X, Weston D et al (2014) Consequences of developmental exposure to concentrated ambient ultrafine particle air pollution combined with the adult paraquat and maneb model of the Parkinson’s disease phenotype in male mice. Neurotoxicology 41:80–88
Androutsopoulos VP, Hernandez AF, Liesivuori J et al (2013) A mechanistic overview of health associated effects of low levels of organochlorine and organophosphorous pesticides. Toxicology 307:89–94
Ashok A, Rai NK, Tripathi S et al (2015) Exposure to As-, Cd-, and Pb-mixture induces Aβ, amyloidogenic APP processing and cognitive impairments via oxidative stress-dependent neuroinflammation in young rats. Toxicol Sci 143(1):64–80
Bakulski KM, Rozek LS, Dolinoy DC et al (2012) Alzheimer’s disease and environmental exposure to lead: the epidemiologic evidence and potential role of epigenetics. Curr Alzheimer Res 9(5):563–573
Baldi I, Gruber A, Rondeau V et al (2011) Neurobehavioral effects of long-term exposure to pesticides: results from the 4-year follow-up of the PHYTONER study. Occup Environ Med 68(2):108–115
Ballard C, Gauthier S, Corbett A et al (2011) Alzheimer’s disease. Lancet 377(9770):1019–1031
Banks EC, Ferretti LE, Shucard DW (1997) Effects of low level lead exposure on cognitive function in children: a review of behavioral, neuropsychological and biological evidence. Neurotoxicology 18(1):237–281
Barker DJ, Gluckman PD, Godfrey KM et al (1993) Fetal nutrition and cardiovascular disease in adult life. Lancet 341(8850):938–941
Barlow BK, Richfield EK, Cory-Slechta DA et al (2004) A fetal risk factor for Parkinson’s disease. Dev Neurosci 26(1):11–23
Barlow BK, Cory-Slechta DA, Richfield EK et al (2007) The gestational environment and Parkinson’s disease: evidence for neurodevelopmental origins of a neurodegenerative disorder. Reprod Toxicol 23(3):457–470
Basha MR, Wei W, Bakheet SA et al (2005) The fetal basis of amyloidogenesis: exposure to lead and latent overexpression of amyloid precursor protein and beta-amyloid in the aging brain. J Neurosci 25(4):823–829
Bellinger DC (2009) Interpreting epidemiologic studies of developmental neurotoxicity: conceptual and analytic issues. Neurotoxicol Teratol 31:267–274
Bellinger DC (2014) Mercury and pregnancy. Birth Defects Res A Clin Mol Teratol 100:1–3
Bihaqi SW, Zawia NH (2013) Enhanced taupathy and AD-like pathology in aged primate brains decades after infantile exposure to lead (Pb). Neurotoxicology 39:95–101
Bihaqi SW, Bahmani A, Subaiea GM et al (2014) Infantile exposure to lead and late-age cognitive decline: relevance to AD. Alzheimers Dement 10(2):187–195
Billnitzer AJ, Barskaya I, Yin C et al (2013) APP independent and dependent effects on neurite outgrowth are modulated by the receptor associated protein (RAP). J Neurochem 124(1):123–132
Blennow K, de Leon MJ, Zetterberg H (2006) Alzheimer’s disease. Lancet 368(9533):387–403
Bolin CM, Basha R, Cox D et al (2006) Exposure to lead and the developmental origin of oxidative DNA damage in the aging brain. FASEB J 20(6):788–790
Bugiani O (2011) Alzheimer’s disease: ageing-related or age-related? New hypotheses from an old debate. Neurol Sci 32:1241–1247
Cai Z, Fan LW, Kaizaki A et al (2013) Neonatal systemic exposure to lipopolysaccharide enhances susceptibility of nigrostriatal dopaminergic neurons to rotenone neurotoxicity in later life. Dev Neurosci 35(2–3):155–171
Caito SW, Aschner M (2015) Mitochondrial redox dysfunction and environmental exposures. Antioxid Redox Signal 23(6):578–595
Calne DB, Langston JW (1983) Aetiology of Parkinson’s disease. Lancet 2(8365–66):1457–1459
Campbell A, Oldham M, Becaria A et al (2005) Particulate matter in polluted air may increase biomarkers of inflammation in mouse brain. Neurotoxicology 26:133–140
Casado A, Encarnación López-Fernández M, Concepción Casado M et al (2008) Lipid peroxidation and antioxidant enzyme activities in vascular and Alzheimer dementias. Neurochem Res 33(3):450–458
Chen GH, Wang H, Yang QG et al (2011) Acceleration of age-related learning and memory decline in middle-aged CD-1 mice due to maternal exposure to lipopolysaccharide during late pregnancy. Behav Brain Res 218(2):267–279
Chen L, Yoo SE, Na R et al (2012) Cognitive impairment and increased Aβ levels induced by paraquat exposure are attenuated by enhanced removal of mitochondrial H(2)O(2). Neurobiol Aging 33(2):432.e15–26)
Chin-Chan M, Navarro-Yepes J, Quintanilla-Vega B (2015) Environmental pollutants as risk factors for neurodegenerative disorders: Alzheimer and Parkinson diseases. Front Cell Neurosci 9:124
Colborn T (2006) A case for revisiting the safety of pesticides: a closer look at neurodevelopment. Environ Health Perspect 114(1):10–17
Cole TB, Beyer RP, Bammler TK et al (2011) Repeated developmental exposure of mice to chlorpyrifos oxon is associated with paraoxonase 1 (PON1)-modulated effects on cerebellar gene expression. Toxicol Sci 123(1):155–169
Cordova FM, Aguiar AS Jr, Peres TV et al (2012) In vivo manganese exposure modulates Erk, Akt and Darpp-32 in the striatum of developing rats, and impairs their motor function. PLoS ONE 7(3):e33057
Cordova FM, Aguiar AS Jr, Peres TV et al (2013) Manganese-exposed developing rats display motor deficits and striatal oxidative stress that are reversed by Trolox. Arch Toxicol 87(7):1231–1244
Cory-Slechta DA, Thiruchelvam M, Barlow BK et al (2005) Developmental pesticide models of the Parkinson disease phenotype. Environ Health Perspect 113(9):1263–1270
Costa LG, Aschner M, Vitalone A et al (2004) Developmental neuropathology of environmental agents. Annu Rev Pharmacol Toxicol 44:87–110
Couper J (1837) On the effects of black oxide of manganese when inhaled into the lungs. Br Ann Med Pharm Vital Stat Gen Sci 1:41–42
Crawley JN (2012) Translational animal models of autism and neurodevelopmental disorders. Dialogues Clin Neurosci 14:293–305
Dal-Pizzol F, Klamt F, Frota ML Jr et al (2001) Neonatal iron exposure induces oxidative stress in adult Wistar rat. Brain Res Dev Brain Res 130(1):109–114
Dauer W, Przedborski S (2003) Parkinson’s disease: mechanisms and models. Neuron 39(6):889–909
De Felice A, Ricceri L, Venerosi A, Chiarotti F, Calamandrei G (2015) Multifactorial origin of neurodevelopmental disorders: approaches to understanding complex etiologies. Toxics 3(1):89–129
Di Monte DA (2003) The environment and Parkinson’s disease: is the nigrostriatal system preferentially targeted by neurotoxins. 2(9):531–538
Dias V, Junn E, Mouradian MM (2013) The role of oxidative stress in Parkinson’s disease. J Parkinsons Dis 3(4):461–491
Dosunmu R, Alashwal H, Zawia NH (2012) Genome-wide expression and methylation profiling in the aged rodent brain due to early-life Pb exposure and its relevance to aging. Mech Ageing Dev 133(6):435–443
Eaton DL, Daroff RB, Autrup H et al (2008) Review of the toxicology of chlorpyrifos with an emphasis on human exposure and neurodevelopment. Crit Rev Toxicol 38(Suppl 2):1–125
Eskenazi B, Marks AR, Bradman A et al (2007) Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ Health Perspect 115:792–798
Fan LW, Tien LT, Lin RC et al (2011a) Neonatal exposure to lipopolysaccharide enhances vulnerability of nigrostriatal dopaminergic neurons to rotenone neurotoxicity in later life. Neurobiol Dis 44(3):304–316
Fan LW, Tien LT, Zheng B et al (2011b) Dopaminergic neuronal injury in the adult rat brain following neonatal exposure to lipopolysaccharide and the silent neurotoxicity. Brain Behav Immun 25(2):286–297
Firestone JA, Lundin JI, Powers KM et al (2010) Occupational factors and risk of Parkinson’s disease: a population-based case-control study. Am J Ind Med 53(3):217–223
Fredriksson A, Schröder N, Eriksson P et al (1999) Neonatal iron exposure induces neurobehavioural dysfunctions in adult mice. Toxicol Appl Pharmacol 159(1):25–30
Fredriksson A, Schröder N, Eriksson P et al (2000) Maze learning and motor activity deficits in adult mice induced by iron exposure during a critical postnatal period. Brain Res Dev Brain Res 119(1):65–74
Garner CC, Zhai RG, Gundelfinger ED et al (2002) Molecular mechanisms of CNS synaptogenesis. Trends Neurosci 25(5):243–251
Giacobini E, Mori F, Lai CC (1996) The effect of cholinesterase inhibitors on the secretion of APPS from rat brain cortex. Ann N Y Acad Sci 777:393–398
Gilbert SG, Grant-Webster KS (1995) Neurobehavioral effects of developmental methylmercury exposure. Environ Health Perspect 103(Suppl 6):135–142
Gillman MW (2005) Developmental origins of health and disease. N Engl J Med 353(17):1848–1850
Giorgi O, De Montis G, Porceddu ML et al (1987) Developmental and age-related changes in D1-dopamine receptors and dopamine content in the rat striatum. Brain Res 432(2):283–290
Goedert M, Jakes R, Crowther RA et al (1993) The abnormal phosphorylation of tau protein at Ser-202 in Alzheimer disease recapitulates phosphorylation during development. Proc Natl Acad Sci USA 90(11):5066–5070
JPND Action Group (2013) Report of the JPND action group. www.jpnd.eu
Gupta RK, Hasan KM, Trivedi R et al (2005) Diffusion tensor imaging of the developing human cerebrum. J Neurosci Res 81:172–178
Hanson MA (2013) Developmental origins of obesity and non-communicable disease. Endocrinol Nutr 60(Suppl 1):10–11
Hayden KM, Norton MC, Darcey D et al (2010) Occupational exposure to pesticides increases the risk of incident AD: the cache county study. Neurology 74(19):1524–1530
Heindel JJ, Balbus J, Birnbaum L et al (2015) developmental origins of health and disease: integrating environmental influences. Endocrinology 156(10):3416–3421
Heneka MT, Carson MJ, El Khoury J et al (2015) Neuroinflammation in Alzheimer’s disease. Lancet Neurol 14(4):388–405
Heppner FL, Ransohoff RM, Becher B (2015) Immune attack: the role of inflammation in Alzheimer disease. Nat Rev Neurosci 16(6):358–372
Herbstman JB, Sjodin A, Kurzon M et al (2010) Prenatal exposure to PBDEs and neurodevelopment. Environ Health Perspect 118:712–719
Hertzman C, Wiens M, Bowering D et al (1990) Parkinson’s disease: a case-control study of occupational and environmental risk factors. Am J Ind Med 17(3):349–355
Howe K, Clark MD, Torroja CF et al (2013) The zebrafish reference genome sequence and its relationship to the human genome. Nature 496(7446):498–503
Jankovic J (2005) Searching for a relationship between manganese and welding and Parkinson’s disease. Neurology 64(12):2021–2028
Jenner P (2003) Oxidative stress in Parkinson’s disease. Ann Neurol 53(Suppl 3):S26–S36
Kaur D, Peng J, Chinta SJ et al (2007) Increased murine neonatal iron intake results in Parkinson-like neurodegeneration with age. Neurobiol Aging 28(6):907–913
Kim JT, Son MH, Lee DH et al (2015) Partitioning behavior of heavy metals and persistent organic pollutants among feto-maternal bloods and tissues. Environ Sci Technol 49(12):7411–7422
Knuesel I, Chicha L, Britschgi M et al (2014) Maternal immune activation and abnormal brain development across CNS disorders. Nat Rev Neurol 10(11):643–660
Kovacs GG, Adle-Biassette H, Milenkovic I et al (2014) Linking pathways in the developing and aging brain with neurodegeneration. Neuroscience 269:152–172
Krstic D, Madhusudan A, Doehner J et al (2012) Systemic immune challenges trigger and drive Alzheimer-like neuropathology in mice. J Neuroinflammation 9:151
Kumar A, Leinisch F, Kadiiska MB et al (2015) Formation and implications of alpha-synuclein radical in Maneb- and Paraquat-induced models of Parkinson’s disease. Mol Neurobiol (Epub ahead of print)
Lahiri DK, Maloney B, Basha MR et al (2007) How and when environmental agents and dietary factors affect the course of Alzheimer’s disease: the “LEARn” model (latent early-life associated regulation) may explain the triggering of AD. Curr Alzheimer Res 4(2):219–228
Lahiri DK, Maloney B, Zawia NH (2009) The LEARn model: an epigenetic explanation for idiopathic neurobiological diseases. Mol Psychiatry 14(11):992–1003
Lai BC, Marion SA, Teschke K et al (2002) Occupational and environmental risk factors for Parkinson’s disease. Parkinsonism Relat Disord 8(5):297–309
Langston J, Ballard P, Tetrud J et al (1983) Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 219:979–980
Langston JW, Forno LS, Tetrud J et al (1999) Evidence of active nerve cell degeneration in the substantia nigra of humans years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine exposure. Ann Neurol 46(4):598–605
Lanphear BP, Hornung R, Khoury J et al (2005) Low level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect 113:894–899
Lee J, Freeman JL (2014) Zebrafish as a model for investigating developmental lead (Pb) neurotoxicity as a risk factor in adult neurodegenerative disease: a mini-review. Neurotoxicology 43:57–64
Lees AJ, Hardy J, Revesz T (2009) Parkinson’s disease. Lancet 373:2055–2066
Li N, Yu ZL, Wang L et al (2010) Increased tau phosphorylation and betaamyloid in the hippocampus of mouse pups by early life lead exposure. Acta Biologica Hungarica 61(2): 123–134
Li Y, Sun Y, Yang J et al (2014) Age-dependent dopaminergic dysfunction following fetal exposure to atrazine in SD rats. Environ Toxicol Pharmacol 37(3):1275–1282
Ling ZD, Chang Q, Lipton JW et al (2004a) Combined toxicity of prenatal bacterial endotoxin exposure and postnatal 6-hydroxydopamine in the adult rat midbrain. Neuroscience 124(3):619–628
Ling Z, Chang QA, Tong CW et al (2004b) Rotenone potentiates dopamine neuron loss in animals exposed to lipopolysaccharide prenatally. Exp Neurol 190(2):373–383
Liou HH, Tsai MC, Chen CJ et al (1997) Environmental risk factors and Parkinson’s disease: a case-control study in Taiwan. Neurology 48(6):1583–1588
Logroscino G (2005) The role of early life environmental risk factors in Parkinson disease: what is the evidence? Environ Health Perspect 113(9):1234–1238
Mazumdar M, Xia W, Hofmann O et al (2012) Prenatal lead levels, plasma amyloid beta levels, and gene expression in young adulthood. Environ Health Perspect 120:702–707
McCormack AL, Thiruchelvam M, Manning-Bog AB et al (2002) Environmental risk factors and Parkinson’s disease: selective degeneration of nigral dopaminergic neurons caused by the herbicide paraquat. Neurobiol Dis 10(2):119–127
McFarlane AC, Searle AK, Van Hooff M et al (2013) Prospective associations between childhood low-level lead exposure and adult mental health problems: the Port Pirie cohort study. Neurotoxicology 39:11–17
McGeer PL, Yasojima K, McGeer EG (2001) Inflammation in Parkinson’s disease. Adv Neurol 86:83–89
Meyer U (2014) Prenatal poly(i:C) exposure and other developmental immune activation models in rodent systems. Biol Psychiatry 75(4):307–315
Milatovic D, Zaja-Milatovic S, Gupta RC et al (2009) Oxidative damage and neurodegeneration in manganese-induced neurotoxicity. Toxicol Appl Pharmacol 240(2):219–225
Miller MW (1986) Effects of alcohol on the generation and migration of cerebral cortical neurons. Science 233:1308–1311
Moreira EG, Yu X, Robinson JF et al (2010) Toxicogenomic profiling in maternal and fetal rodent brains following gestational exposure to chlorpyrifos. Toxicol Appl Pharmacol 245(3):310–325
Morley R (2006) Fetal origins of adult disease. Semin Fetal Neonatal Med 11(2):73–78
Neal AP, Guilarte TR (2010) Molecular neurobiology of lead (Pb(2+)): effects on synaptic function. Mol Neurobiol 42(3):151–160
Neal AP, Worley PF, Guilarte TR (2011) Lead exposure during synaptogenesis alters NMDA receptor targeting via NMDA receptor inhibition. Neurotoxicology 32:281–289
Nordberg M, Winblad B, Fratiglioni L et al (2000) Lead concentrations in elderly urban people related to blood pressure and mental performance: results from a population-based study. Am J Ind Med 38(3):290–294
Nunomura A, Perry G, Aliev G et al (2001) Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol 60(8):759–767
Olden K, Isaac L, Roberts L (2011) Neighborhood-specific epigenome analysis: the pathway forward to understanding gene-environment interactions. N C Med J 72(2):125–127
Parrón T, Requena M, Hernández AF et al (2011) Association between environmental exposure to pesticides and neurodegenerative diseases. Toxicol Appl Pharmacol 256(3):379–385
Perera FP, Li Z, Whyatt R et al (2009) Prenatal airborne polycyclic aromatic hydrocarbon exposure and child IQ at age 5 years. Pediatrics 124:e195–e202
Peris-Sampedro F, Salazar JG, Cabré M et al (2014) Impaired retention in AβPP Swedish mice six months after oral exposure to chlorpyrifos. Food Chem Toxicol 72:289–294
Reitz C, Brayne C, Mayeux R (2011) Epidemiology of Alzheimer disease. Nat Rev Neurol 7(3):137–152
Reuhl KR (1991) Delayed expression of neurotoxicity: the problem of silent damage. Neurotoxicology 12(3):341–346
Richardson JR, Caudle WM, Wang M et al (2006) Developmental exposure to the pesticide dieldrin alters the dopamine system and increases neurotoxicity in an animal model of Parkinson’s disease. FASEB J 20(10):1695–1697
Richardson JR, German D, Levey A (2014) Alzheimer disease risk factors. JAMA Neurol 71(8):1051
Rosas LG, Eskenazi B (2008) Pesticides and child neurodevelopment. Curr Opin Pediatr 20(2):191–197
Rose S, Melnyk S, Pavliv O et al (2012) Evidence of oxidative damage and inflammation associated with low glutathione redox status in the autism brain Transl. Psychiatry 2(7):e134
Rossignol DA, Genuis SJ, Frye RE (2014) Environmental toxicants and autism spectrum disorders: a systematic review. Trans Psychiatry 4:e360
Roy TS, Seidler FJ, Slotkin TA (2004) Morphologic effects of subtoxic neonatal chlorpyrifos exposure in developing rat brain: regionally selective alterations in neurons and glia. Brain Res Dev Brain Res 148:197–206
Salazar JG, Ribes D, Cabré M et al (2011) Amyloid β peptide levels increase in brain of AβPP Swedish mice after exposure to chlorpyrifos. Curr Alzheimer Res 8(7):732–740
Sale A, Berardi N, Maffei L (2014) Environment and brain plasticity: towards an endogenous pharmacotherapy. Physiol Rev 94(1):189–234
Sandy MS, Armstrong M, Tanner CM et al (1996) CYP2D6 allelic frequencies in young-onset Parkinson’s disease. Neurology 47(1):225–230
Santibáñez M, Bolumar F, García AM (2007) Occupational risk factors in Alzheimer’s disease: a review assessing the quality of published epidemiological studies. Occup Environ Med 64(11):723–732
Selkoe DJ, Schenk D (2003) Alzheimer’s disease: molecular understanding predicts amyloid-based therapeutics. Annu Rev Pharmacol Toxicol 43:545–584
Sheinerman KS, Umansky SR (2013) Circulating cell-free microRNA as biomarkers for screening, diagnosis and monitoring of neurodegenerative diseases and other neurologic pathologies. Front Cell Neurosci 7:150
Shonkoff JP (2000) From neurons to neighborhoods: the science of early childhood development. National Academy Press, Washington
Sian-Hülsmann J, Mandel S, Youdim MB et al (2011) The relevance of iron in the pathogenesis of Parkinson’s disease. J Neurochem 118(6):939–957
Slotkin TA, Seidler FJ (2009) Oxidative and excitatory mechanisms of developmental neurotoxicity: transcriptional profiles for chlorpyrifos, diazinon, dieldrin, and divalent nickel in PC12 cells. Environ Health Perspect 117:587–596
Stangle DE, Strawderman MS, Smith D et al (2004) Reductions in blood lead overestimate reductions in brain lead following repeated succimer regimens in a rodent model of childhood lead exposure. Environ Health Perspect 112:302–308
Sun Y, Li YS, Yang JW et al (2014) Exposure to atrazine during gestation and lactation periods: toxicity effects on dopaminergic neurons in offspring by downregulation of Nurr1 and VMAT2. Int J Mol Sci 15(2):2811–2825
Tanner CM, Goldman SM, Ross GW et al (2014) The disease intersection of susceptibility and exposure: chemical exposures and neurodegenerative disease risk. Alzheimers Dement 10(3 Suppl):S213–S225
Tarantal AF, Berglund L (2014) Obesity and lifespan health–importance of the fetal environment. Nutrients 6(4):1725–1736
Tau GZ, Peterson BS (2010) Normal development of brain circuits. Neuropsychopharmacology 35(1):147–168
Thiruchelvam M, Brockel BJ, Richfield EK et al (2000) Potentiated and preferential effects of combined paraquat and maneb on nigrostriatal dopamine systems: environmental risk factors for Parkinson’s disease? Brain Res 873(2):225–234
Thiruchelvam M, Richfield EK, Goodman BM et al (2002) Developmental exposure to the pesticides paraquat and maneb and the Parkinson’s disease phenotype. Neurotoxicology 23(4–5):621–633
Thiruchelvam M, McCormack A, Richfield EK et al (2003) Age-related irreversible progressive nigrostriatal dopaminergic neurotoxicity in the paraquat and maneb model of the Parkinson’s disease phenotype. Eur J Neurosci 18(3):589–600
Tien LT, Cai Z, Rhodes PG et al (2011) Neonatal exposure to lipopolysaccharide enhances methamphetamine-induced reinstated behavioral sensitization in adult rats. Behav Brain Res 224(1):166–173
Tien LT, Kaizaki A, Pang Y et al (2013) Neonatal exposure to lipopolysaccharide enhances accumulation of α-synuclein aggregation and dopamine transporter protein expression in the substantia nigra in responses to rotenone challenge in later life. Toxicology 308:96–103
Toscano CD, Guilarte TR (2005) Lead neurotoxicity: from exposure to molecular effects. Brain Res Brain Res Rev 49(3):529–554
Van Maele-Fabry G, Hoet P, Vilain F et al (2012) Occupational exposure to pesticides and Parkinson’s disease: a systematic review and meta-analysis of cohort studies. Environ Int 1(46):30–43
Venerosi A, Ricceri L, Tait S et al (2012) Sex dimorphic behaviors as markers of neuroendocrine disruption by environmental chemicals: the case of chlorpyrifos. Neurotoxicology 33(6):1420–1426
Voorn P, Kalsbeek A, Jorritsma-Byham B et al (1988) The pre- and postnatal development of the dopaminergic cell groups in the ventral mesencephalon and the dopaminergic innervation of the striatum of the rat. Neuroscience 25(3):857–887
Vorhees RA (1986) Handbook of behavioral teratology. Plenum Press, New York
Wang S, Yan JY, Lo YK et al (2009) Dopaminergic and serotoninergic deficiencies in young adult rats prenatally exposed to the bacterial lipopolysaccharide. Brain Res 1265:196–204
Wani WY, Sunkaria A, Sharma DR et al (2014) Caspase inhibition augments Dichlorvos-induced dopaminergic neuronal cell death by increasing ROS production and PARP1 activation. Neuroscience 258:1–15
Weisskopf MG, Wright RO, Schwartz J et al (2004) Cumulative lead exposure and prospective change in cognition among elderly men: the VA normative aging study. Am J Epidemiol 160(12):1184–1193
Westerlund M, Hoffer B, Olson L (2010) Parkinson’s disease: exit toxins, enter genetics. Prog Neurobiol 90:146–156
Whyatt RM, Liu X, Rauh VA et al (2012) Maternal prenatal urinary phthalate metabolite concentrations and child mental, psychomotor, and behavioral development at 3 years of age. Environ Health Perspect 120:290–295
Wild CP (2012) The exposome: from concept to utility. Int J Epidemiol 41:24–32
Wilson WW, Shapiro LP, Bradner JM et al (2014) Developmental exposure to the organochlorine insecticide endosulfan damages the nigrostriatal dopamine system in male offspring. Neurotoxicology 44:279–287
Winneke G (2011) Developmental aspects of environmental neurotoxicology: Lessons from lead and polychlorinated biphenyls. J Neurol Sci 308:9–15
Wright RO, Tsaih SW, Schwartz J et al (2003) Lead exposure biomarkers and mini-mental status exam scores in older men. Epidemiology 14(6):713–718
Wu J, Basha MR, Brock B et al (2008) Alzheimer’s disease (AD)-like pathology in aged monkeys after infantile exposure to environmental metal lead (Pb): evidence for a developmental origin and environmental link for AD. J Neurosci 28(1):3–9
Zhu Y, Carvey PM, Ling Z (2007) Altered glutathione homeostasis in animals prenatally exposed to lipopolysaccharide. Neurochem Int 50(4):671–680
Acknowledgments
Supported by FP7 HEALS Grant No. 603946 “Health and Environment-wide Associations based on Large Population Surveys,” by CROME Grant No. LIFE12 ENV/GR/001040 “Cross-Mediterranean Environment and Health Network,” and by Ministry of Health-ISS Project 13CAL “Identification of early markers of pathology in rodent models of autism: role of endogenous endoretroviruses.”
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Tartaglione, A.M., Venerosi, A., Calamandrei, G. (2015). Early-Life Toxic Insults and Onset of Sporadic Neurodegenerative Diseases—an Overview of Experimental Studies. In: Kostrzewa, R.M., Archer, T. (eds) Neurotoxin Modeling of Brain Disorders—Life-long Outcomes in Behavioral Teratology. Current Topics in Behavioral Neurosciences, vol 29. Springer, Cham. https://doi.org/10.1007/7854_2015_416
Download citation
DOI: https://doi.org/10.1007/7854_2015_416
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34134-7
Online ISBN: 978-3-319-34136-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)