Abstract
Traumatic brain injury has ripple effect on the physical, cognitive, behavioral, and emotional domains of quality of life and portends a long-term neurological disability in survivors. In this study we evaluated the prognostic role of demographic and clinico-radiological variables on the hospitalization length and mortality in 71 of patients with frontal brain contusions. The receiver operating characteristic (ROC) plots were performed, with area under the curve (AUC) values, for graphical comparison of variables that would predict mortality and hospitalization length. We found that the best prognostics of mortality were the Glasgow Coma Scale score, the motor function score, and the Rotterdam CT score, with AUC values of 0.873, 0.836, and 0.711, respectively. Concerning the prediction of hospitalization length, the AUC showed inappreciable differences, with the highest values for the Glasgow Coma Scale score, Rotterdam CT score, and the serum cortisol level in a 0.550–0.600 range. Curve estimation, based on multivariate analysis, showed that the scores of motor function, Glasgow Coma Scale, and Rotterdam CT correlated best with the prediction of both mortality and hospitalization length, along with the upward dynamic changes of serum cortisol for the latter. We conclude that basically simple and non-invasive assessment in survivors of acute traumatic brain contusion is helpful in predicting mortality and the length of hospital stay, which would be of essential value in better allocation of healthcare resources for inpatient treatment and rehabilitation and for post-hospital patient’s functioning.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Acute brain injury is the most common sequelae of all traumatic incidents. Frontal contusions comprise 43.4% of the intracranial pathologies resulting from trauma (Papo et al. 1982). Moreover, such contusions have a ripple effect on the physical, cognitive, behavioral, and emotional domains of quality of life, and they also harbinger variable long-term neurological disabilities among the survivors (Kurland et al. 2012). Although most of the patients are initially neurologically preserved, there is a high tendency for rapid progression of brain lesions, leading to sudden brain herniation and eventual death (Chen et al. 2018; Rehman et al. 2008). Brain injury also embarks a significant negative effect on daily lives of patients and caretakers, and it connotes a substantial enduring socioeconomic burden for families and society (Chen et al. 2006).
There is a paucity of neurosurgical studies pertaining to the prognostic value of various clinical factors in predicting the length of hospitalization and mortality among patients with traumatic brain injury. Thus, this study seeks to predict outcome in patients with traumatic frontal contusions based on demographic and clinico-radiological variables referring to the total length of hospitalization and mortality.
2 Methods
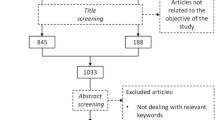
2.1 Patients and Study Design
There were 71 patients enrolled in the study with the diagnosis of traumatic frontal contusions who were hospitalized in the Department of Neurosurgery at the Nobel Medical College and Teaching Hospital in Biratnagar, Nepal, during January 2017 and June 2019. Exclusion criteria consisted of significant associated polytrauma with hemodynamic instability, patient’s refusal to participate in the study, or leaving the hospital in the course of treatment against medical advice.
We evaluated demographic and clinico-radiological variables that could have a bearing in predicting the length of hospitalization and mortality (outcomes) among patients with traumatic frontal contusions, such as patient age, gender, initial Glasgow Coma Scale, Rotterdam computed tomography (CT) score, assessment of motor function, bilateralism on opposing body sides, changes in the serum cortisol and thyroid hormones from the first to the third day of admission, accompanying polytrauma, management mode, and the presence of other concurrent brain lesions. Study outcomes were the length of hospitalization and the mortality rate in patients with traumatic frontal contusions.
2.2 Sample Size and Data Elaboration
The minimum sample size, required to achieve the study goal, was calculated as 32 patients using the following formula:
where z is 1.96 at 95% confidence interval; p, 20% prevalence of traumatic frontal contusions; q, 1-p; and d, 10% margin of error.
The receiver operating characteristic (ROC) plots were performed, with area under curve (AUC) values, for graphical presentation and comparing variables that would be useful for predicting the length of hospitalization and morbidity among patients with traumatic frontal contusions. The analysis of variance (ANOVA) and multivariate logistic regression, along with the logistic coefficient curve, were used to evaluate the effects of different variables, which could affect the two outcome variables: mortality rate and hospitalization length. The analysis was performed using a commercial statistical package of SPSS v16 (IBM Corp., Armonk, NY).
3 Results
In the ROC analysis, the best predictors of mortality in patients with traumatic frontal contusion were the score of the Glasgow Coma Scale, motor function score, and Rotterdam CT score, with the AUC values of 0.873, 0.836, and 0.711, respectively (Fig. 1). One-way ANOVA for predicting mortality yielded a significant p-value only for the three variables aforementioned; 0.001, 0.003, and 0.005, respectively. Concerning the prediction of hospitalization length, the AUC showed inappreciable differences, with the highest values also for the Glasgow Coma Scale score (0.592), Rotterdam CT score (0.589), and the serum cortisol level (0.564) (Fig. 2).
In multivariate analysis, curve estimation of the size and direction of the relationship between a predictor, i.e., clinical and radiological variables investigated, and the response outcomes, i.e., mortality and hospitalization length, are depicted in Figs. 3 and 4, respectively, For mortality, the best prediction yielded the motor score (p = 0.001), Glasgow Coma scale score (p = 0.001), and Rotterdam CT score (p = 0.047). For the hospitalization length, prediction was significantly associated with the Glasgow Coma Scale score (p = 0.001), Rotterdam CT score (p = 0.001), mode of management (p = 0.001), serum cortisol content (p = 0.006), and the presence of concurrent brain lesions (p = 0.005).
4 Discussion
In this study we assessed the efficacy of clinico-radiological and biochemical variables in predicting mortality and hospitalization length of patients with traumatic frontal brain contusions. There is a paucity of studies addressing the issue that is of substantial practical interest in the face of frequency of such injuries and uncertain outcome and complicating management. In the assessment, we used a spectrum of different factors and variables, such as the Glasgow Coma Scale score, the Rotterdam CT score, and the motor function score at presentation, the presence of concurrent brain pathologies, the associated polytrauma, and the dynamics of changes in the content of serum cortisol and thyroid hormones. We also took into account patients’ demographics such as age and gender and the management algorithm performed in these patients. The findings, in general, were that the factors above outlined positively correlated with both mortality and hospitalization length in patients with acute frontal brain injury as depicted in curve estimation, based on multivariate regression analysis (Figs. 3 and 4). There were, however, differences in the prognostic power among these factors.
The Glasgow Coma Scale was the most significant item in predicting both mortality and hospitalization length in patients with traumatic frontal contusions. For mortality, the AUC value corresponding to this scale in the ROC plot amounted to 0.873. The finding pointing to the essential importance of the scale in the patient assessment is in line with other previous studies on the subject (Arango-Lasprilla et al. 2010; Hung et al. 2004). However, the score of motor function at presentation and the Rotterdam CT score ran closely behind the Glasgow Coma scale score in predicting mortality, in terms of the AUC values. Moreover, the assessment of motor function seems superior and more reliable in some patients, as the eye and verbal components of the Glasgow Coma Scale might be adversely influenced by drugs, alcohol intoxication, or patient intubation. In addition, motor function assessment is the only one clearly and objectively achievable when a full Glasgow Coma Scale cannot be performed. The Rotterdam CT score, which helps evaluate the course of acute traumatic brain injuries (Munakomi 2016), also appeared useful in predicting both mortality and hospitalization length in our patients. The score was a particularly strong determinant regarding mortality, with the AUC of 0.711.
In addition, we found in this study that an upward change in the serum cortisol during the first few days of hospitalization due to frontal brain injury was a significant prognostic of mortality. The role of the assessment of serum cortisol in such patients is a contentious issue. In contradistinction to the present finding, Hannon et al. (2011) have found that patients with a low level of cortisol would rather have increased mortality. That finding has not been supported by a study of Olivecrona et al. (2013) who have failed to substantiate the presence of a relationship between dynamic changes in cortisol and mortality after brain injury. The discrepancy among the studies concerning the relation of serum cortisol to mortality is not readily explicable and requires further exploration using alternative study designs.
Referring to the hospitalization length, in general, the variables investigated showed narrow differences in the ROC plot, within a 0.550–0.600 range of AUC values. The Glasgow Coma Scale score and the Rotterdam CT score appeared the most significant determinants with the AUC of 0.592 and 0.589, respectively. However, the serum cortisol level and polytrauma, including concurrent brain lesions, also ranked high in the ability to determine the hospitalization course. In this study, fractures of long bones accounted for the majority of associated polytrauma. Fractures of the pelvis and lower limbs immobilize patients and delay physical rehabilitation, which increases the risk of pulmonary embolism, prolongs the hospital stay, and increases the risk of mortality. These results are in line with those reported by Tardif et al. (2017) and Stewart et al. (2013), except that the latter study has reported chest injuries, rather than bone fractures, as being prevalent among patients with acute traumatic brain injury. Likewise, patient age was another factor that was found of significance in predicting the length of hospital stay in the present study, with increasing age prolonging the stay. Older age carries the inherent risk of comorbidities, such as pre-existing hypertension, diabetes, or cognitive impairments, which all hinders the management of a treatment course in acute brain trauma, in turn leading to a prolongation of hospital stay (Lazaridis et al. 2015; Vitaz et al. 2003).
A limitation in interpreting the findings of the study is that it was performed in a rather small sample of 71 patients with traumatic frontal brain injury hospitalized in a single tertiary medical center. The results obtained should be validated in larger multi-center prospective randomized trials. Nonetheless, we believe we have shown that basically simple and non-invasive assessment in survivors of acute traumatic brain contusion may be helpful in gaining predictive knowledge on the length of hospital stay and plausible mortality. This knowledge is of essential value for better allocation of healthcare resources concerning the management of inpatient treatment and rehabilitation, which would eventually lead to better outcome and post-hospital quality of life.
References
Arango-Lasprilla JC, Ketchum JM, Cifu D, Hammond F, Castillo C, Nicholls E, Watanabe T, Lequerica A, Deng X (2010) Predictors of extended rehabilitation length of stay after traumatic brain injury. Arch Phys Med Rehabil 91(10):1495–1504
Chen H, Meng H, Lu ZX (2006) Prospective study on family burden following traumatic brain injury in children. Chin J Epidemiol 27:307–310
Chen JH, Li PP, Yang LK, Chen L, Zhu J, Hu X, Wang YH (2018) Value of ventricular intracranial pressure monitoring for traumatic bifrontal contusions. World Neurosurg 113:e690–e701
Hannon MJ, Sherlock M, Thompson CJ (2011) Pituitary dysfunction following traumatic brain injury or subarachnoid haemorrhage – in “Endocrine Management in the Intensive Care Unit”. Best Pract Res Clin Endocrinol Metab 25(5):783–798
Hung KS, Liang CL, Wang CH, Chang HW, Park N, Hank Juo SH (2004) Outcome after traumatic frontal intracerebral haemorrhage: a comparison of unilateral and bilateral haematomas. J Clin Neurosci 11(8):849–853
Kurland D, Hong C, Aarabi B, Gerzanich V, Simard JM (2012) Hemorrhagic progression of a contusion after traumatic brain in- jury: a review. J Neurotrauma 29:19–31
Lazaridis C, Yang M, DeSantis SM, Luo ST, Robertson CS (2015) Predictors of intensive care unit length of stay and intracranial pressure in severe traumatic brain injury. J Crit Care 30(6):1258–1262
Munakomi S (2016) A comparative study between Marshall and Rotterdam CT scores in predicting early deaths in patients with traumatic brain injury in a major tertiary care hospital in Nepal. Chin J Traumatol 19(1):25–27
Olivecrona Z, Dahlqvist P, Koskinen LO (2013) Acute neuro-endocrine profile and prediction of outcome after severe brain injury. Scand J Trauma Resusc Emerg Med 21:33
Papo I, Caruselli G, Scarpelli M, Luongo A (1982) Mass lesions of the frontal lobes in acute head injuries. A comparison with temporal lesions. Acta Neurochir 62(1–2):47–72
Rehman T, Ali R, Tawil I, Yonas H (2008) Rapid progression of traumatic bifrontal contusions to transtentorial herniation: a case report. Cases J 1(1):203
Stewart TC, Alharfi IM, Fraser DD (2013) The role of serious concomitant injuries in the treatment and outcome of paediatric severe traumatic brain injury. J Trauma Acute Care Surg 75(5):836–842
Tardif PA, Moore L, Boutin A, Dufresne P, Omar M, Bourgeois G, Bonaventure PL, Kuimi BL, Turgeon AF (2017) Hospital length of stay following admission for traumatic brain injury in a Canadian integrated trauma system: a retrospective multicenter cohort study. Injury 48(1):94–100
Vitaz TW, Jenks J, Raque GH, Shields CB (2003) Outcome following moderate traumatic brain injury. Surg Neurol 60(4):285–291
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Nobel Medical College and Teaching Hospital in Biratnagar, Nepal (approval no. 134/2018).
Informed Consent
Written informed consent was obtained from the patients, their relatives, or next of kin, depending on the patient’s clinical status, of all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Munakomi, S., Thingujam, J., Bajracharya, A., Gurung, S., Shrestha, S. (2020). Prognostics of Hospitalization Length and Mortality in Patients with Traumatic Frontal Brain Contusions. In: Pokorski, M. (eds) Health and Medicine. Advances in Experimental Medicine and Biology(), vol 1279. Springer, Cham. https://doi.org/10.1007/5584_2020_529
Download citation
DOI: https://doi.org/10.1007/5584_2020_529
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-51120-3
Online ISBN: 978-3-030-51121-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)