Abstract
In this study we hypothesized that the alleviation of neurological symptoms long after internal carotid artery (ICA) stenting may be related to sustained improvement of cerebral perfusion. Thirty-four subjects (F/M; 15/19) with >70% stenosis of a single internal carotid artery and neurological symptoms, who underwent a carotid artery stenting procedure, were studied. Brain computed tomography perfusion (CTP) imaging was performed before and 3 years after ICA stenting. The following relative variables were compared: cerebral blood flow (rCBF), cerebral blood volume (rCBV), mean transit time (rMTT), time to peak (rTTP), and permeability surface area product (rPS). A survey also was conducted to compare the patients’ clinical symptoms. Overall, we found that a trend toward rMTT decline was the only persisting change after ICA stenting. We then stratified the patients into the subgroups of <2%, 2–5%, and > 5% rMTT decline and found that those with a rMTT decline >2% reported a prominent reduction in subjective clinical symptoms such as headache, dizziness, tinnitus, blurred vision, transient blindness, a sense of gravity of the head, and pain in the eyeballs. We conclude that a shortened mean rMTT, likely reflecting improved cerebral microcirculation, underlies the improvement of neurological symptoms in patients with ICA stenosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Blood transit time
- Cerebral blood flow
- Computed tomography perfusion
- Internal carotid artery
- Neurological symptoms
1 Introduction
Internal carotid artery (ICA) stenosis-related brain hypoperfusion is associated with neurological, psychiatric, and psychological deficits, manifesting as headache, dizziness, tinnitus, blurred vision, transient blindness, a sense of gravity in the head, and pain in the eyeballs. These symptoms associate with cognitive and mood decline. Neuropsychological deficits may not be as apparent as the neurological ones, but they add to the downgrading of quality of life. Numerous studies have demonstrated that ICA stenosis, without transient ischemic episodes or strokes, is a detriment to executive functions and memory (Wang et al. 2016; Romero et al. 2009; Sztriha et al. 2009; Popovic et al. 2011; Mathiesen et al. 2004). It has been demonstrated that cognitive function may improve in symptomatic patients after ICA recanalization, with both endarterectomy and carotid stenting (Yamashita et al. 2012; Chida et al. 2010). Interestingly, Grunwald et al. (2006) have shown cognitive improvements in word fluency and delayed recall in neuropsychological tests conducted 24 h after carotid artery stenting also in asymptomatic patients. Results, akin to those outlined above, have been reported by Wang et al. (2017) and Picchetto et al. (2013) in asymptomatic patients.
ICA stenosis is considered an independent risk factor for stroke (Goessens et al. 2007). It also contributes to the pathophysiology of depression (Rao et al. 2001; Mathiesen et al. 2004; Bakker et al. 2000), and it is a risk factor for suicides in stroke patients (Lovett and Rothwell 2002). According to Huang et al. (2012), ICA stenting relieves post-stroke depression in high-grade ICA stenosis patients over the time of 1 month. A therapeutic effect of stenting is superior to that exerted by selective serotonin reuptake inhibitors in these patients. In contrast, however, Picchetto et al. (2013) have observed no difference between pre- and post-scoring in the neuropsychological evaluation of depression and anxiety carried out in asymptomatic ICA stenosis patients subjected to stenting.
Cerebral blood flow (CBF), which may be assessed during computed tomography perfusion (CTP) examination, improves after ICA stenting (Szarmach et al. 2017; Frydrychowski et al. 2013; Trojanowska et al. 2006; Niesen et al. 2004). However, two other CTP-derived variables, namely, blood-brain barrier (BBB) permeability and mean transit time (MTT), are less recognized in the research and diagnosis of ICA stenosis. The BBB functioning is impaired, and the diffusion of fluid, blood, or contrast molecules into the extravascular space is augmented in the pathologic states such as neoplastic or inflammatory diseases, ischemia, and neurodegenerative disorders (Topakian et al. 2010; Jain et al. 2008). We have demonstrated that elevated BBB permeability can be reversed in subjects with ICA stenosis after stenting (Szarmach et al. 2017). A disease-enhanced BBB permeability can be considered a radiological marker of neuroinflammation. A decline in BBB permeability with improvement of cerebral blood circulation, and thus increased delivery of oxygen to the brain tissue, suggests that the overall brain ischemic and inflammatory status improves.
Prolongation of MTT is increasingly linked to a cerebral small vessel disease (Arba et al. 2017; Cao et al. 2016). Such diseases, in turn, are associated with the accumulation of immune cells and erythrocytes in the brain microvessel lumina (Kaiser et al. 2014; Mencl et al. 2013; Schreiber et al. 2013; Rouhl et al. 2012; Schreiber et al. 2012). The MTT is prolonged in subjects with ICA stenosis (Szarmach et al. 2017). Importantly, acute MTT decline, 4–6 weeks after ICA stenting, sends a positive signal for the long-term MTT downward response (Winklewski et al. 2019). Thus, MTT decline after stenting strongly suggests the possibility of functional improvement in brain microcirculation.
Several authors have suggested that relative MTT (rMTT), which is the symptomatic hemisphere-to-asymptomatic hemisphere MTT ratio, may represent an early and sensitive parameter for the detection of perfusion changes (Duan et al. 2012; Merckel et al. 2012; Wilkinson et al. 2003). Consequently, we hypothesized that the long-term decline in rMTT after ICA stenting may be interrelated with the alleviation of neurological symptoms reported by patients.
2 Methods
2.1 Patient Population
There were 34 patients (F/M; 15/19) of the mean age of 69.7 ± 7.6 years, suffering from ICA stenosis, investigated during 2010–2014 (Table 1). The patients were qualified for a carotid artery stenting procedure in the Department of Cardiac and Vascular Surgery of the Medical University of Gdansk in Poland.
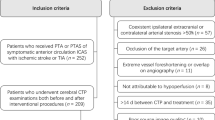
A general neurological and internal examination of all the patients was performed before the stenting procedure. Patients with stenosis of more than 70% within a single internal carotid artery and with concomitant neurological symptoms (i.e., headache, dizziness, tinnitus, blurred vision, transient blindness, a sense of gravity of the head, and pain in the eyeballs) were included in the study. In all patients, duration of carotid artery stenosis was longer than 5 years. The degree of artery stenosis, according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET 1991), was evaluated using Doppler ultrasonography and confirmed immediately prior to stent implantation by digital subtraction angiography (DSA). Only were patients with a complete circle of Willis and normal vertebral arteries included in the evaluation.
Patients with bilateral hemodynamically significant (i.e., >70%) stenosis of cranial arteries, patients with complete occlusion of one vessel, or those who had experienced extensive ischemic brain stroke were excluded from the study. Consequently, in the patients included in the study, stenosis on the contralateral side was hemodynamically insignificant (i.e., <50%). Patients with abnormal blood pressure, heart rate values, uncontrolled hyperthyroidism, renal insufficiency, hypersensitivity to iodine, or a history of adverse effects following the administration of contrast agents were also excluded from the study.
2.2 Imaging Protocol
The imaging protocol of the study included a Doppler examination, non-contrast axial computed tomography, CTP, and DSA. All images are taken before and after the injection of an iodinate contrast medium. The DSA, as a gold standard in neuroradiology, is performed in patients with various types of vascular pathology, such as aneurysm, arteriovenous malformation, fistula, and vessel occlusion or stenosis. This radiographic technique visualizes cerebral vessels with the minimum view of a background tissues.
The CTP imaging was performed before and 3 years after ICA stenting. The imaging was done using a 64-MDct Light Speed VCT XT scanner (GE Healthcare Technologies, Waukesha, WI). Non-contrast axial computed tomography scans allowed for the identification of signs of active bleeding, acute ischemic stroke, or features of increased intracranial pressure. The axial images acquired for CT perfusion at 40 mm in cine mode (CTP 4 cm) were initiated 5 s after the start of 40 mL of the nonionic iodine-based intravascular contrast agent, OPTIRAY 350 (Mallinckrodt, St. Louis, MO), administered into an antecubital vain at an injection rate of 4 mL/s. After contrast injection, an additional bolus of 40 mL of physiological saline was administered. The acquisition parameters for the CT examinations were the following: tube voltage 80 kV, 150 mAs, slice thickness 5 mm, rotation time 1/s, field of view (FOV) 25 cm, time interval between reconstructed images 0.5–1 s, total exposure time 45 s, interval 0.5 mm, gantry angle parallel to and above the orbital roof to avoid radiation exposure to the lens, image matrix 512 x 512, and eight slices. A total of 272 slices from 34 patients were obtained, with a scan time of 45 s.
The arterial input function was chosen within the anterior cerebral artery (segment A2) on the basal ganglia level. The venous output region was selected from the superior sagittal sinus. All of the listed acquisition parameters were applied as provided by the manufacturer for the brain perfusion study.
2.3 Image Post-processing
The raw data were transferred to a dedicated diagnostic workstation (AW 4, GE Healthcare Technologies, Waukesha, WI) and analyzed using a research version of the CTP post-processing software package (CT Perfusion v4.3.1) (GE Healthcare Technologies, Waukesha, WI) to create color maps of dynamic cerebral enhancement, represented as CBF, cerebral blood volume (CBV), mean transit time (MTT), time to peak (TTP), and permeability surface area product (PS).
This diagnostic application offers two different evaluation modes. The first mode, the “neuro-brain stroke” mode, calculates the perfusion metrics of MTT, CBF, CBV, and TTP for brain stroke assessment using the maximum slope method (Lin et al. 2007; Fiorella et al. 2004). The MTT characterizes the average time of contrast agent residence within the tissue. In mathematical terms, the mean transit time is computed as the time between the initial impulse and the time of arrival. The MTT is computed and displayed in seconds. The CBF is derived from the initial value of the impulse residue function and is computed and displayed in mL per 100 g of wet tissue per minute. The CBV is computed and displayed in mL per 100 g of wet tissue. The blood volume is the product of blood flow and mean transit time: CBV = CBF × MTT. The TTP is the time between the onset of enhancement transient (last pre-enhancement image) and the peak value of time curve (image with the maximum value before the first post-enhancement image). The time to peak is computed and displayed in seconds, using the raw time curve data directly.
The second mode, known as the “neuro-brain tumor” mode, calculates microvascular permeability (PS) and fractional blood volume based on the Johnson and Wilson model (St Lawrence and Lee 1998a, b). The PS is computed and displayed in mL per 100 g of wet tissue per minute. It is computed from the impulse residue function. Contrast agent diffusion appears in the impulse residue function as a residual enhancement that occurs after the initial impulse response and decreases exponentially with time.
Two experienced neuroradiologists blinded to clinical information (medical history, side, and time of operation) independently manually drew two standardized elliptical mirrored regions of interest (ROI). The ROI (approximately 10 cm2 each) was determined on all analyzed levels, over the cortical gray matter centered 20 mm from the brain edge. The large vessels were automatically excluded via brain perfusion software. The absolute values of CTP parameters (MTT, TTP, CBF, CBV, and PS) of one hemisphere in the region of middle cerebral artery distribution and contralateral mirroring areas in functional maps were measured. Then, the relative parameters were calculated as the symptomatic hemisphere-to-asymptomatic hemisphere ratios.
2.4 Patient Surveys
A survey was given to patients who qualified for the stenting procedure. The first survey was carried out on the day of admission. The second survey was performed after the follow-up perfusion scan (approximately 3 years after the procedure). The flowing questions were asked:
-
Headache: Yes/No
-
Dizziness: Yes/No
-
Tinnitus: Yes/No
-
Blurred vision: Yes/No
-
Transient blindness: Yes/No
-
A sense of gravity of the head: Yes/No
-
Pain in the eyeballs: Yes/No
3 Results
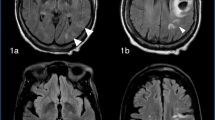
Relative CBF, CBV, MTT, TTP, and PS values did not change 3 years after stenting, compared to the baseline values measured before stenting (Table 2). Nevertheless, a clear trend toward rMTT decline was observed. When a subgroup analysis was performed, it appeared that three separate groups of patients could be distinguished: (1) patients with rMTT decline greater than 5%, (2) patients with rMTT decline between 2% and 5%, and (3) patients with rMTT decline less than 2%. Improvement in clinical symptoms, reported by patients, was related to a decline in rMTT. A prominent improvement was reported with a rMTT decline greater than 2% (Figs. 1, 2, and 3).
In the group with the greatest rMTT decline, the number of reported headaches was reduced from 7 to 2, dizziness from 9 to 4, tinnitus from 5 to 3, blurred vision from 4 to 2, transient blindness from 2 to 1, a sense of gravity of the head from 2 to 0, and pain in the eyeballs from 3 to 1. In the group with rMTT decline between 5% and 2%, the number of reported headaches was reduced from 9 to 3, dizziness from 7 to 3, tinnitus from 11 to 4, and blurred vision and a sense of gravity of the head from 2 to 0.
In contradistinction, in patients without an appreciable decline in rMTT (<2%), clinical symptoms either did not change or actually worsened (Fig. 3). In this group, the number of reported headaches remained unchanged (3 cases before and after ICA stenting), dizziness decreased from 4 to 3, tinnitus from 3 to 2, blurred vision increased from 2 to 4, transient blindness increased from 3 to 4, a sense of gravity of the head increased from 2 to 4, and pain in the eyeballs remained unchanged (3 cases before and after ICA stenting).
4 Discussion
The main finding of the study is that relative decreases in MTT were associated with improvements in the clinical symptoms reported by patients with ICA stenosis, 3 years after the stenting procedure, providing that the decreases were greater than 2% of the baseline level noted before stenting. Taking into account both objective measurements and self-assessed symptoms allows for a more complete evaluation of the influence of the stenting procedure. In the literature, CBF is the most often used variable for the evaluation of treatment effects in patients with ICA stenosis. There is a need to focus on the influence of treatment on the perception of quality of life, especially for the extended periods of time, longer than a year (Shan et al. 2015). The assessment of quality of life can be helpful in the estimation of the effectiveness of treatment in terms of stroke prevention and in comparison of different types of treatments, and as such it is an important therapeutic goal (Fadrná et al. 2018). Assessing quality of life in this group of patients is also vital, since the very presence of severe carotid stenosis may predispose patients to lower general well-being and lower satisfaction with life, let alone depressive and cognitive impairment (Pucite et al. 2017).
There is an ongoing discussion regarding the pathomechanisms involved in cerebral small vessel disease and the subsequent development of neurological symptoms and cognitive decline. According to some authors, vascular stiffening, increased pulse pressure, and carotid pulsatility are the major factors leading to the development of white matter hyperintensities and neurological and cognitive deterioration (Wardlaw et al. 2017; van Sloten et al. 2015; Aribisala et al. 2014; Singer et al. 2014). There is a contradicting theory, indicating that a prolonged brain hypoperfusion results in hypoxia, inflammation, and oxidative stress, followed by a blood-brain barrier collapse (Ding et al. 2017; Duncombe et al. 2017; Szarmach et al. 2017; Kim et al. 2012).
In this study we demonstrated that subjective symptoms reported by patients might be related to changes in cerebral microcirculation. Consequently, our study refocuses clinical attention on the interventional and non-interventional medical procedures aiming to maintain blood flow in cerebral small vessels, such as carotid artery recanalization, proper pharmacological therapy, and lifestyle modifications. The predominant notion of numerous reports is that MTT is the most sensitive marker of cerebral perfusion changes. However, calculation of accurate absolute values of this parameter is impractical, while using absolute threshold values in making therapeutic decisions is dubious due to the parameter’s strong correlation with numerous external factors, e.g., cardiac output, age, or a degree of stenosis (Zhang et al. 2013; Esteban and Cervera 2004; Koenig et al. 2001). Consequently, we assessed relative MTT in this study, i.e., the ratio of symptomatic hemisphere-to-asymptomatic hemisphere MTT.
ICA stenosis was diagnosed in all patients by a Doppler examination more than 5 years before surgery. Due to stringent inclusion criteria, consisting of <70% stenosis within a single ICA, the population of this study was homogeneous in terms of cerebral hemodynamic parameters and was characterized by low CBF and low CBV. As a result, ICA stenosis on the contralateral side must have been hemodynamically insignificant (<50%), as evidenced by other studies (Ricotta et al. 2011; Nicolaides et al. 2005; Samson et al. 1999). Patients with bilateral hemodynamically significant, i.e., >70%, stenosis of the cranial arteries were excluded from the study. Although a relatively narrow population can be seen a limitation of this study, its homogeneity could enhance the reliability of results. The present findings justify further research with the use of magnetic resonance imaging (MRI). In particular, a combination of dynamic susceptibility contrast MRI (DSC-MRI), dynamic contrast-enhanced MRI (DCE-MRI), and blood oxygen level-dependent imaging MRI (BOLD-MRI) could provide comprehensive information on the effect on the functional brain status of cerebral microcirculation and blood-brain barrier permeability fluctuations. Such studies with the concomitant neuropsychological assessment are currently under way.
Quantitative CTP data are highly dependent on the post-processing software. Software differences are frequently considered the main cause of variability in perfusion results relative to inter-operator and intra-operator differences (Kudo et al. 2010; Kamalian et al. 2011; Zussman et al. 2011). In this study we used the equipment manufactured by one producer and the same post-processing procedure for all subjects. Further, there were two experienced neuroradiologists who independently drew standardized elliptical mirrored ROIs, with the area of approximately 10 cm2 each, on the section level of the reference CT image over the cortical gray matter of the middle cerebral artery territory. Finally, in all subjects, we used a coverage size of 40 mm, which is well-suited for detecting perfusion parameters owing to the high density of scans (Szarmach et al. 2016).
In conclusion, we believe we have conclusively demonstrated in this study that subjective symptoms reported by patients suffering from ICA stenosis might be related to changes in cerebral microcirculation. Further studies with the extensive use of various MRI techniques are warranted to assess how changes in the brain microcirculation and blood-brain barrier functional status are related to patients’ self-reported quality of life and to overall patients’ functional status.
References
Arba F, Mair G, Carpenter T, Sakka E, Sandercock PAG, Lindley RI, Inzitari D, Wardlaw JM, IST–3 Trial Collaborators (2017) Cerebral white matter hypoperfusion increases with small–vessel disease burden. Data from the Third International Stroke Trial. J Stroke Cerebrovasc Dis 26:1506–1513
Aribisala BS, Morris Z, Eadie E, Thomas A, Gow A, Valdés Hernández MC, Royle NA, Bastin ME, Starr J, Deary IJ, Wardlaw JM (2014) Blood pressure, internal carotid artery flow parameters, and age–related white matter hyperintensities. Hypertension 63:1011–1018
Bakker FC, Klijn CJ, Jennekens–Schinkel A, Kappelle LJ (2000) Cognitive disorders in patients with occlusive disease of the carotid artery: a systematic review of the literature. J Neurol 247:669–676
Cao W, Yassi N, Sharma G, Yan B, Desmond PM, Davis SM, Campbell BC (2016) Diagnosing acute lacunar infarction using CT perfusion. J Clin Neurosci 29:70–72
Chida K, Ogasawara K, Aso K, Suga Y, Kobayashi M, Yoshida K, Terasaki K, Tsushina E, Ogawa A (2010) Postcarotid endarterectomy improvement in cognition is associated with resolution of crossed cerebellar hypoperfusion and increase in 123I–iomazenil uptake in the cerebral cortex: a SPECT study. Cerebrovasc Dis 29(4):343–351
Ding L, Hong Y, Peng B (2017) Association between large artery atherosclerosis and cerebral microbleeds: a systematic review and meta–analysis. Stroke Vasc Neurol 2:7–14
Duan Y, Li G, Yang Y, Li J, Huang H, Wang H, Xu F, Chen W (2012) Changes in cerebral hemodynamics after carotid stenting of symptomatic carotid artery. Eur J Radiol 81:744–748
Duncombe J, Kitamura A, Hase Y, Ihara M, Kalaria RN, Horsburgh K (2017) Chronic cerebral hypoperfusion: a key mechanism leading to vascular cognitive impairment and dementia. Closing the translational gap between rodent models and human vascular cognitive impairment and dementia. Clin Sci 131:2451–2468
Esteban JM, Cervera V (2004) Perfusion CT and angio CT in the assessment of acute stroke. Neuroradiology 46:705–715
Fadrná T, Mikšová Z, Herzig R, Langová K, Ličman L, Školoudík D (2018) Factors influencing quality of life in patients followed in the neurosonology laboratory for carotid stenosis. Health Qual Life Outcomes 16(1):79
Fiorella D, Heiserman J, Prenger E, Partovi S (2004) Assessment of the reproducibility of postprocessing dynamic CT perfusion data. AJNR Am J Neuroradiol 25:97–107
Frydrychowski AF, Winklewski PJ, Szarmach A, Halena G, Bandurski T (2013) Near–infrared transillumination back scattering sounding––new method to assess brain microcirculation in patients with chronic carotid artery stenosis. PLoS One 8:e61936
Goessens BM, Visseren FL, Kappelle LJ, Algra A, van der Graaf Y (2007) Asymptomatic carotid artery stenosis and the risk of new vascular events in patients with manifest arterial disease: the SMART Study. Stroke 38:1470–1475
Grunwald IQ, Supprian T, Politi M, Struffert T, Falkai P, Krick C, Backens M, Reith W (2006) Cognitive changes after carotid artery stenting. Neuroradiology 48:319–323
Huang H, Chen K, Guo T, Zhang Y, Qu W, Zhou Z, Liu G, Chen L (2012) Treatment with carotid angioplasty stent placement for post-stroke depression compared to antidepressants. Neurosciences (Riyadh) 17(1):53–56
Jain R, Ellika SK, Scarpace L, Schultz LR, Rock JP, Gutierrez J, Patel SC, Ewing J, Mikkelsen T (2008) Quantitative estimation of permeability surface–area product in astroglial brain tumors using perfusion CT and correlation with histopathologic grade. Am J Neuroradiol 29:694–700
Kaiser D, Weise G, Möller K, Scheibe J, Pösel C, Baasch S, Gawlitza M, Lobsien D, Diederich K, Minnerup J, Kranz A, Boltze J, Wagner DC (2014) Spontaneous white matter damage, cognitive decline and neuroinflammation in middle–aged hypertensive rats: an animal model of early–stage cerebral small vessel disease. Acta Neuropathol Commun 2:169
Kamalian S, Kamalian S, Maas MB, Goldmacher GV, Payabvash S, Akbar A, Schaefer PW, Furie KL, Gonzalez RG, Lev MH (2011) CT cerebral blood flow maps optimally correlate with admission diffusion–weighted imaging in acute stroke but thresholds vary by postprocessing platform. Stroke 42:1923–1928
Kim HA, Miller AA, Drummond GR, Thrift AG, Arumugam TV, Phan TG, Srikanth VK, Sobey CG (2012) Vascular cognitive impairment and Alzheimer’s disease: role of cerebral hypoperfusion and oxidative stress. Naunyn Schmiedeberg’s Arch Pharmacol 385:953–959
Koenig M, Kraus M, Theek C, Klotz E, Gehlen W, Heuser L (2001) Quantitative assessment of the ischemic brain by means of perfusion–related parameters derived from perfusion CT. Stroke 32:431–437
Kudo K, Sasaki M, Yamada K, Momoshima S, Utsunomiya H, Shirato H, Ogasawara K (2010) Differences in CT perfusion maps generated by different commercial software: quantitative analysis by using identical source data of acute stroke patients. Radiology 254:200–209
Lin K, Kazmi KS, Law M, Babb J, Peccerelli N, Pramanik BK (2007) Measuring elevated microvascular permeability and predicting hemorrhagic transformation in acute ischemic stroke using first–pass dynamic perfusion CT imaging. AJNR Am J Neuroradiol 28:1292–1298
Lovett JK, Rothwell PM (2002) Suicide in a patient with symptomatic carotid occlusion. J R Soc Med 95:93–94
Mathiesen EB, Waterloo K, Joakimsen O, Bakke SJ, Jacobsen EA, Bønaa KH (2004) Reduced neuropsychological test performance in asymptomatic carotid stenosis: The Tromso Study. Neurology 62:695–701
Mencl S, Garz C, Niklass S, Braun H, Göb E, Homola G, Heinze HJ, Reymann KG, Kleinschnitz C, Schreiber S (2013) Early microvascular dysfunction in cerebral small vessel disease is not detectable on 3.0 Tesla magnetic resonance imaging: a longitudinal study in spontaneously hypertensive stroke–prone rats. Exp Transl Stroke Med 5:8
Merckel LG, Van der Heijden J, Jongen LM, van Es HW, Prokop M, Waaijer A (2012) Effect of stenting on cerebral CT perfusion in symptomatic and asymptomatic patients with carotid artery stenosis. AJNR Am J Neuroradiol 33:280–285
NASCET – North American Symptomatic Carotid Endarterectomy Trial Collaborators (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high–grade carotid stenosis. N Engl J Med 325:445–453
Nicolaides AN, Kakkos SK, Griffin M (2005) Severity of asymptomatic carotid stenosis and risk of ipsilateral hemispheric ischaemic events: results from the ACSRS study. Eur J Vasc Endovasc Surg 30:275–284
Niesen WD, Rosenkranz M, Eckert B, Meissner M, Weiller C, Sliwka U (2004) Hemodynamic changes of the cerebral circulation after stent–protected carotid angioplasty. Am J Neuroradiol 25:1162–1167
Picchetto L, Spalletta G, Casolla B, Cacciari C, Cavallari M, Fantozzi C, Ciuffoli A, Rasura M, Imperiale F, Sette G, Caltagirone C, Taurino M, Orzi F (2013) Cognitive performance following carotid endarterectomy or stenting in asymptomatic patients with severe ICA stenosis. Cardiovasc Psychiatry Neurol 2013:342571
Popovic IM, Lovrencic–Huzjan A, Simundic AM, Popovic A, Seric V, Demarin V (2011) Cognitive performance in asymptomatic patients with advanced carotid disease. Cogn Behav Neurol 24:145–151
Pucite E, Krievina I, Miglane E, Erts R, Krievins D (2017) Influence of severe carotid stenosis on cognition, depressive symptoms and quality of life. Clin Pract Epidemiol Ment Health 13:168–180
Rao R, Jackson S, Howard R (2001) Depression in older people with mild stroke, carotid stenosis and peripheral vascular disease: a comparison with healthy controls. Int J Geriatr Psychiatry 16:175–183
Ricotta JJ, Aburahma A, Ascher E (2011) Updated society for vascular surgery guidelines for management of extracranial carotid disease. J Vasc Surg 54:e1–e31
Romero JR, Beiser A, Seshadri S, Benjamin EJ, Polak JF, Vasan RS, Au R, DeCarli C, Wolf PA (2009) Carotid artery atherosclerosis, MRI indices of brain ischemia, aging, and cognitive impairment: the Framingham study. Stroke 40:1590–1596
Rouhl RP, Damoiseaux JG, Lodder J, Theunissen RO, Knottnerus IL, Staals J, Henskens LH, Kroon AA, de Leeuw PW, Tervaert JW, van Oostenbrugge RJ (2012) Vascular inflammation in cerebral small vessel disease. Neurobiol Aging 33:1800–1806
Samson RH, Showalter DP, Yunis JP, Dorsay DA, Kulman HI, Silverman SR (1999) Hemodynamically significant early recurrent carotid stenosis: an often self–limiting and self–reversing condition. J Vasc Surg 30:446–452
Schreiber S, Bueche CZ, Garz C, Kropf S, Angenstein F, Goldschmidt J, Neumann J, Heinze HJ, Goertler M, Reymann KG, Braun H (2012) The pathologic cascade of cerebrovascular lesions in SHRSP: is erythrocyte accumulation an early phase? J Cereb Blood Flow Metab 32:278–290
Schreiber S, Bueche CZ, Garz C, Braun H (2013) Blood brain barrier breakdown as the starting point of cerebral small vessel disease? New insights from a rat model. Exp Transl Stroke Med 5:4
Shan L, Shan J, Saxena A, Robinson D (2015) Quality of life and functional status after carotid revascularisation: a systematic review and meta–analysis. Eur J Vasc Endovasc Surg 49:634–645
Singer J, Trollor JN, Baune BT, Sachdev PS, Smith E (2014) Arterial stiffness, the brain and cognition: a systematic review. Ageing Res Rev 15:16–27
St Lawrence KS, Lee TY (1998a) An adiabatic approximation to the tissue homogeneity model for water exchange in the brain: I. Theoretical derivation. J Cereb Blood Flow Metab 18:1365–1377
St Lawrence KS, Lee TY (1998b) An adiabatic approximation to the tissue homogeneity model for water exchange in the brain: II. Experimental validation. J Cereb Blood Flow Metab 18:1378–1385
Szarmach A, Halena G, Kaszubowski M, Piskunowicz M, Szurowska E, Frydrychowski AF, Winklewski PJ (2016) Perfusion computed tomography: 4 cm versus 8 cm coverage size in subjects with chronic carotid artery stenosis. Br J Radiol 89:20150949
Szarmach A, Halena G, Kaszubowski M, Piskunowicz M, Studniarek M, Lass P, Szurowska E, Winklewski PJ (2017) Carotid artery stenting and blood–brain barrier permeability in subjects with chronic carotid artery stenosis. Int J Mol Sci 18:E1008
Sztriha LK, Nemeth D, Sefcsik T, Vecsei L (2009) Carotid stenosis and the cognitive function. J Neurol Sci 283:36–40
Topakian R, Barrick T, Howe F, Markus H (2010) Blood–brain barrier permeability is increased in normal–appearing white matter in patients with lacunar stroke and leucoaraiosis. J Neurol Neurosurg Psychiatry 81:192–197
Trojanowska A, Drop A, Jargiello T, Wojczal J, Szczerbo–Trojanowska M (2006) Changes in cerebral hemodynamics after carotid stenting: evaluation with CT perfusion studies. J Neuroradiol 33:169–174
van Sloten TT, Protogerou AD, Henry RM, Schram MT, Launer LJ, Stehouwer CD (2015) Association between arterial stiffness, cerebral small vessel disease and cognitive impairment: a systematic review and meta–analysis. Neurosci Biobehav Rev 53:121–130
Wang T, Mei B, Zhang J (2016) Atherosclerotic carotid stenosis and cognitive function. Clin Neurol Neurosurg 146:64–70
Wang T, Sun D, Liu Y, Mei B, Li H, Zhang S, Zhang J (2017) The impact of carotid artery stenting on cerebral perfusion, functional connectivity, and cognition in severe asymptomatic carotid stenosis patients. Front Neurol 8:403
Wardlaw JM, Allerhand M, Eadie E, Thomas A, Corley J, Pattie A, Taylor A, Shenkin SD, Cox S, Gow A, Starr JM, Deary IJ (2017) Carotid disease at age 73 and cognitive change from age 70 to 76 years: a longitudinal cohort study. J Cereb Blood Flow Metab 37:3042–3052
Wilkinson ID, Griffiths PD, Hoggard N, Cleveland TJ, Gaines PA, Macdonald S, McKevitt F, Venables GS (2003) Short–term changes in cerebral microhemodynamics after carotid stenting. AJNR Am J Neuroradiol 24:1501–1507
Winklewski PJ, Kaszubowski M, Halena G, Sabisz A, Chwojnicki K, Piskunowicz M, Kurhaluk N, Szurowska E, Szarmach A (2019) Computed tomography indicators of cerebral microperfusion improve long term after carotid stenting in symptomatic patients. Acta Biochim Pol https://doi.org/10.18388/abp.2017
Yamashita T, Ogasawara K, Kuroda H, Suzuki T, Chida K, Kobayashi M, Yoshida K, Kubo Y, Ogawa A (2012) Combination of preoperative cerebral blood flow and 123I–iomazenil SPECT imaging predicts postoperative cognitive improvement in patients undergoing uncomplicated endarterectomy for unilateral carotid stenosis. Clin Nucl Med 37(2):128–133
Zhang J, Wang J, Geng D, Li Y, Song D, Gu Y (2013) Whole–brain CT perfusion and CT angiography assessment of Moyamoya disease before and after surgical revascularization: preliminary study with 256–slice CT. PLoS One 8:e57595
Zussman BM, Boghosian G, Gorniak RJ, Olszewski ME, Read KM, Siddiqui KM, Flanders AE (2011) The relative effect of vendor variability in CT perfusion results: a method comparison study. AJR Am J Roentgenol 197:468–473
Acknowledgments
The study was funded by the statutory budgets of the medical universities of Gdansk and Warsaw. Dr. Pawel J. Winklewski was supported by the Polish National Science Center grant 2017/01/X/NZ5/00909.
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The experimental protocol of the study was approved by the Ethics Committee of the Medical University in Gdansk, Poland.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Szarmach, A. et al. (2019). Relative Cerebral Blood Transit Time Decline and Neurological Improvement in Patients After Internal Carotid Artery Stenting. In: Pokorski, M. (eds) Advances in Biomedicine. Advances in Experimental Medicine and Biology(), vol 1176. Springer, Cham. https://doi.org/10.1007/5584_2019_378
Download citation
DOI: https://doi.org/10.1007/5584_2019_378
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-25372-1
Online ISBN: 978-3-030-25373-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)