Abstract
This review tackles the unresolved issue of the existence of oxygen sensor in the body. The sensor that would respond to changes in tissue oxygen content, possibly along the hypoxia-normoxia-hyperoxia spectrum, rather than to a given level of oxygen, and would translate the response into lung ventilation changes, the major adaptive process. Studies on oxygen sensing, for decades, concentrated around the hypoxic ventilatory response generated mostly by carotid body chemoreceptor cells. Despite gaining a substantial insight into the cellular transduction pathways in carotid chemoreceptors, the exact molecular mechanisms of the chemoreflex have never been conclusively verified. The article briefly sums up the older studies and presents novel theories on oxygen, notably, hypoxia sensing. These theories have to do with the role of transient receptor potential cation TRPA1 channels and brain astrocytes in hypoxia sensing. Although both play a substantial role in shaping the ventilatory response to hypoxia, neither can yet be considered the ultimate sensor of hypoxia. The enigma of oxygen sensing in tissue still remains to be resolved.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Oxygen Sensing
Oxygen is required for life on the Earth as it is a prerequisite for cellular respiration, notably at the mitochondrial level, in all aerobic organisms. In higher concentrations than those present in the ambient air, oxygen is however harmful and toxic for organisms due to the enhancement of oxidative stress through the formation of reactive oxygen and nitrogen species, fostering aging or even death at high concentrations that damage lung structure and function, and ultimately decreasing delivery of oxygen to the arterial blood through the respiratory tract. This dichotomous action of oxygen requires that the living organisms be able to keep the physiological level of oxygen in balance and adapt to its changes. The adaptive processes suggest the possibility of forming an oxygen sensor during the evolution of life; a sensor that would pick up the level of oxygen in real time and transfer the message down to the effector systems. The presence of O2 sensor is still elusive despite decades of research on the subject.
The hitherto research has focused mostly on hypoxia, a life-threatening condition, also underlying neurodegenerative diseases, and the aging process. The attention centered on the hypoxic reflex, generating rapid lung hyperventilation, relatively easy to study and producing spectacular responses. The time sanctioned location of this reflex is the arterial chemoreceptors (Izumizaki et al. 2004). These receptors are located in the carotid body, a minute paired sensory organ whose discharge increases in proportion to reduction of oxygen and, in turn, is relayed to the brainstem respiratory network to induce an increase in lung ventilation, being proportional to the chemoreceptor discharge (Pokorski 1999). The molecular mechanisms of carotid chemoreceptor activation have been worked out relatively well (Gonzalez et al. 1994). They consist of inhibition of outwardly directed K+ channels, voltage-dependent (Buniel et al. 2008) or belonging to the TASK channel family (Buckler 2013), in the plasma membrane of chemoreceptor cells and subsequent accumulation of K+ ions leading to cell depolarization, activation of Ca2+ channels, followed by influx of Ca2+, accompanied by mobilization of Ca2+ from intracellular stores, exocytosis of putative neurotransmitters, such as dopamine, and finally excitation of the sinus nerve afferent discharge. In particular, inhibition of background TASK-like channels is considered essential for triggering the stimulus transduction cascade in chemoreceptor cells (Ortiz et al. 2012; Ortega-Sáenz et al. 2010). The inhibition of K+ channels has to do with CO formation by hemeoxygenase in chemoreceptors (Peng et al. 2010; Kumar 2007; Williams et al. 2004).
Hypoxia depletes ATP in chemoreceptor cells, which is conducive to depolarization, as K+ channels are modulated by cytosolic ATP and Ca2+ ions. However, there is a multitude of K+ channels that respond to hypoxia, with an appreciable difference depending on the species and on the kind of cell (Peers et al. 2010). There is evidence that K+ channels also are sensitive to regulation by factors originating beyond the cytosol. Jiang and Haddad (1994) have found in cell-free neuronal membrane patches that large-conductance K+ channels are inhibited by oxygen deprivation, with 50 % channel inhibition at 10 mmHg and no effect at PO2 over 20 mmHg. The level of PO2 at which the opening probability of K+ channels distinctly decreases is contentious and a source of uncertainty regarding the chemosensing mechanisms. A major criticism persists that inhibition of K+ channels is realized when the level of O2 drops to about 70–80 mmHg (Gonzalez et al. 1994; Ganfornina and López-Barneo 1991), which is much above the level producing maximal hypoxic activation of carotid sensory discharge. Therefore, closure of K+ channels outruns the hypoxic excitation of chemoreceptor cells, the two being out of phase concerning the maximum chemoreceptor discharge and ventilatory effects (Lahiri et al. 2006; Pokorski 1999). The cascade of events above outlined has a reason and support, albeit fragmentary rather than all-encompassing, of various studies. These mechanisms have never been fully verified. Further, some fragments like, for instance, the action of dopamine and a number of other neurotransmitters present in chemoreceptor cells, are controversial and shadowy.
Other hypoxia responsive systems have been unraveled along the tedious research way, such as vagally-innervated aortic bodies and airway neuroepithelial bodies (Cutz et al. 2013). There also are hypoxia-responding catecholaminergic neurons in the brain (Gonzalez et al. 1994). These additional systems seem however secondary and of less influence, as they are incapable to take over the generation of hypoxic lung hyperventilation when the carotid body action is switched off. Hyperoxia, on the other hand, decreases membrane depolarization of and neurotransmitter release from chemoreceptor cells, and consequently also chemoreceptor sensory discharge. Sensing hyperoxia seems as essential as sensing hypoxia due to oxygen toxicity mostly related to the formation of reactive oxygen species. The mechanisms of hyperoxia sensing are even more enigmatic than in case of hypoxia. The search for hypoxia/hyperoxia sensor, i.e., a sensor responding smoothly to changes in O2 content, continues. To this end, a possibility has recently arisen of the involvement of transient receptor potential cation channel, subfamily A, member 1, also known as TRPA1 channels, as the core O2 sensing element.
2 TRPA1 Channels and Chemosensing
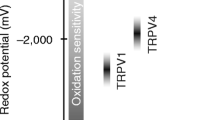
These membrane cation channels are basically engaged in airway smooth muscle contractility and inflammation and are activated by noxious stimuli and cold. Takahashi et al. (2011) have recently demonstrated that TRPA1 are capable of sensing O2, intriguingly along the hypoxia-normoxia-hyperoxia continuum rather that at either extreme. The O2 sensing would however be underlain be disparate mechanisms. In normoxia, with sufficient physiological, evolution-set level of O2, TRPA1 are rendered inactive by O2-dependent activity of prolyl hydroxylases (PHD). In hypoxia, with insufficient oxygen, and consequently less protein hydroxylation by PHD, TRPA1 would be relieved from the PHD-mediated inhibition. In hyperoxia, in turn, TRPA1 would also be relieved from the PHD-mediated inhibition, but this time due to cysteine-mediated oxidation. TRPA1’s cysteine sulfhydryl groups are highly sensitive to oxidation, the event that activates the channel.
These mechanisms have been elegantly proven in the sensory vagal system, raising a specter of a potentially uniform theory for O2 sensing across other tissues. The theory would undoubtedly reconcile a great deal of hitherto discrepant, often opposing, results and views concerning the enigma of O2 sensing. It also could shed light on the mechanism of some stimulatory effects on ventilation of extended oxygenation (Marczak and Pokorski 2004). Nonetheless, a full verification of the essential role of TRPA1 in O2 sensing would require a confirmation of the presence of TRPA1 channel receptors in the carotid body and/or their functional role in the generation of the powerful hypoxic reflex taking place in chemoreceptor cells, a time proven tenet of physiology. At this juncture, TRPA1 issue has become complicated. Investigations to identify TRPA1 in the carotid body have failed; the results are equivocal if not outright null (Gallego-Martin et al. 2015). In an effort to tackle the functional role of TRPA1 we have performed a major study in the conscious unrestrained mouse in which we pharmacologically blocked TRPA1 channels while investigating the ventilatory response to O2 changes in hypoxic, normoxic, and hyperoxic conditions as well as to hypercapnia (Pokorski et al. 2014). The main hypothesis was that if TRPA1 channels were a prerequisite for O2 responses, then O2 sensitivity would be abrogated when the channels are rendered inactive. We examined the acute two-minute-long chemosensory ventilatory responses before and after intraperitoneal injection of the specific TRPA1 antagonist HC-030031 in two doses of 50 and 200 mg/kg at approximately 1 h interval. The antagonist is a long-lived, slowly degradable agent in the body. Thus, cumulative dose of it amounted to 250 mg/kg; a dose being close to the highest ever reported antagonistic dose of HC-030031 used in a study of nocifensive behaviors (McNamara et al. 2007). Ventilation and its responses to mild 13 % and severe 7 % hypoxia, pure O2, and 5 % CO2 balanced with O2 were recorded in a whole-body plethysmograph. The results failed at several points to meet our expectation to lend support for the universality of TRPA1 channels in O2 sensing. The ventilatory augmentation in response to the severe hypoxia was diminished by about half after the TRPA1 antagonist pretreatment in the higher dose compared with the control condition without the antagonist, but it remained clearly distinct (Fig. 1). The response to hyperoxia fluctuated around the baseline both before and after the antagonist pretreatment. No real stimulation of ventilation by oxygen was noticeable, nor was there any appreciable effect of TRPA1 antagonism. The magnitude of a vigorously hyperventilatory response to hypercapnia was, likewise, unaffected by the antagonist (Fig. 2). Intriguingly, however, ventilatory response to the mild 13 % hypoxia was nearly abolished by TRPA1 antagonist pretreatment in the higher dose (Fig. 3). Taken together, the findings hardly support the concept of TRPA1 channels being a unifying sensor of O2 changes, and if so, only in the part regarding the hypoxia sensing, as posited by Takahashi et al. (2011), and only in a limited, mild range of hypoxia.
Ventilatory responses to severe hypoxia (7 % O2 in N2) in the conscious mouse before, i.e., at the background of the vehicle DMSO, and after pharmacological blockade of TRPA1 channels with the inhibitor HC-030031. (a) an example of original recordings, (b) minute ventilation at baseline, peak hypoxic response, and recovery in the three pharmacological conditions: vehicle, and two doses of the HC-030031 inhibitor 50 and 250 mg/kg; values are means (SD), brackets of the same color connecting pairs of symbols indicate significant differences at p < 0.05 (two-factor within-subject ANOVA with the Bonferroni correction). (Panel b is reproduced with permission from Pokorski et al. 2014.)
Ventilatory responses to hyperoxia (100 % O2) and hypercapnia (5 % CO2 in O2) in the conscious mouse before, i.e., at the background of the vehicle DMSO, and after pharmacological blockade of TRPA1 channels with the inhibitor HC-030031. (a) an example of original recordings, (b) minute ventilation at baseline, peak hyperoxic and hypercapnic responses, and recovery in the three pharmacological conditions: vehicle, and two doses of the HC-030031 inhibitor 50 and 250 mg/kg; values are means (SD), brackets of the same color connecting pairs of symbols indicate significant differences at p < 0.05 (two-factor within-subject ANOVA with the Bonferroni correction). (Panel b is reproduced with permission from Pokorski et al. 2014.)
Ventilatory responses to mild hypoxia (13 % O2 in N2) in the conscious mouse before, i.e., at the background of the vehicle DMSO, and after pharmacological blockade of TRPA1 channels with the inhibitor HC-030031. (a) an example of original recordings, (b) minute ventilation at baseline, peak hypoxic response, and recovery in the three pharmacological conditions: vehicle, and two doses of the HC-030031 inhibitor 50 and 250 mg/kg; values are means (SD), brackets of the same color connecting pairs of symbols a indicate significant differences at p < 0.05 (two-factor within-subject ANOVA with the Bonferroni correction). (Panel b is reproduced with permission from Pokorski et al. 2014.)
Nonetheless, the TRPA1 antagonism study has spurred novel ideas on the hypoxia sensing. The plausibility arises that hypoxia sensing consists of two components; each of different mediation depending on the level of hypoxia. Mild hypoxia would be sensed and adaptively offset by specialized chemoreceptive cells, such as airway neuroepithelial bodies, laryngeal or aortic chemoreceptors, and other vagally innervated sensors (Brouns et al. 2012; Piskuric et al. 2011). These sensors are thought of as secondary chemoreceptors, responsive to hypoxia but incapable of generating a full-fledged ventilatory response to severe hypoxia or upholding hypoxic ventilation in case the carotid bodies are rendered inactive or removed (Honda 1985). When life-threatening hypoxia is encountered, carotid chemoreceptors come to the rescue by generating a powerful defensive chemoreflex. These mechanisms would overlap throughout hypoxic exposure, with the carotid body increasing involvement along the progressively increasing lack of oxygen, which explains the suppressant effect of TRPA1 antagonism present also in severe hypoxia. The existence of such double mechanisms could also explain many a discordant, variable, or enigmatic result in investigations on the hypoxic ventilatory response, but do not set the TRPA1 channels at the core of the universal O2 sensing mechanism.
3 Astroglia and Chemosensing
Recently, attention has been diverted from the peripheral arterial chemoreceptor cells toward the brain astroglia as the potentially outstanding player in chemosensing. Astrocytes, the macroglia cells, are ubiquitous in the brainstem respiratory regions where they form extensive functionally specialized network (Kasymov et al. 2013). Aside from the interneuronal localization of astrocytes, these cells have cytoplasmic processes that terminate on blood microvessels. Astrocytes, like carotid chemoreceptor cells, express ion channels, notably K+ channels, and a spate of neurotransmitters and receptors (Bélanger and Magistretti 2009). They perform a number of active functions, known to be engaged also in the chemosensing process in the carotid body, such as influx and propagation of intracellular Ca2+ on stimulation or Ca2+-dependent neurotransmitter release. They are also vulnerable to redox changes (Angelova and Abramov 2016). These similarities between astrocytes and carotid chemoreceptor cells make astrocytes well-suited to sense and dynamically modulate the brainstem neuronal activity in response to O2 changes. Further, astrocytes residing in the central chemosensitive areas of the ventrolateral medullary surface respond to a drop in pH with intracellular Ca2+ increase and release of ATP (Kasymov et al. 2013). The astroglia excitatory response, radiating to the brainstem respiratory network, may thus also participate in shaping the central hyperventilatory response to CO2.
Hypoxia, particularly if prolonged or severe, causes brain depression which manifests, among others, in depressed lung ventilation. That is a delayed, depressant phase of the ventilatory response to hypoxia. Astrocytes, with their multifarious neuroprotective and homeostatic functions, could be engaged in the maintenance of cerebral function and ventilation in the hypoxic condition. We have investigated this hypothesis in a recent study in which the EEG activity of the forebrain and ventilation in a body box were simultaneously recorded in conscious mice (Fukushi et al. 2016). Astrocytic function was modulated pharmacologically by intraperitoneal administration of arundic acid, a specific inhibitory moderator of intensity of astrocytic activity. Two doses of arundic acid of 100 and 200 mg/kg (cumulative dose of 300 mg/kg) were employed at one hour intervals. A rather severe hypoxia of 6 % O2 balanced with N2 was induced, and ventilation and EEG responses were compared before and after pretreatment with each dose of arundic acid (Fig. 4). Arundic acid had no appreciable effects on EEG or ventilation in the normoxic condition. At the time of the development of hypoxic ventilatory depression in hypoxia, EEG got depressed as well. Arundic acid pretreatment caused further suppression of the hypoxic ventilation, accompanied by a dose-dependent suppression of the EEG gamma frequency band. These functional changes were accompanied by a strongly decreased expression of c-Fos in the dorsomedial hypothalamic nucleus, respiratory-regulating nucleus, after arundic acid pretreatment. The arundic acid-induced EEG suppression is suggestive of dimmed consciousness and hypothalamic activity, with resultant deepening of ventilatory depression in hypoxia. The corollary is that astrocytes counteract the ventilatory depression. The findings reveal that astrocytes promote cerebral function, inclusive of consciousness and ventilation, in hypoxia. This function of astrocytes leaves no doubt about their involvement in the control of ventilation. Astrocytes have been recently suggested to be directly involved in the hypoxic ventilatory response (Angelova et al. 2015).
Respiratory flow (inspiration upward) and EEG raw recordings in a conscious mouse. (a) Arrow exemplifies the onset of ventilatory fall-off during the stimulatory ventilatory response to hypoxia; (b) Respiratory flow and EEG signals during room air breathing (left column) and during the depressant phase of response to 6 % O2 in N2 (right column) at baseline (vehicle) and after pretreatment with increasing doses of arundic acid. Arundic acid caused dose-dependent suppression of both respiratory flow and EEG (Reproduced with permission from Fukushi et al. 2016.)
In synopsis, we believe we have shown that astroglia is an essential component of central nervous system sensitivity to hypoxia and is an active modulator of adaptive ventilatory responses. The issue of whether astrocytes could be the elusive hypoxia sensor remains conjectural. There is too little hard information on the innate mechanisms of astrocytic function to form an ultimate opinion on the role of astrocytes in the ventilatory chemoreflex. For the time being, connection between astrocytes and ventilation represents a holistic approach to respiratory regulation and poses an intriguing and interesting avenue of research. What science is all about is the meticulous building up on previous research, which gives rise to new questions and ideas. That undoubtedly also concerns the jigsaw puzzle of O2 sensing.
References
Angelova PR, Abramov AY (2016) Functional role of mitochondrial reactive oxygen species in physiology. Free Radic Biol Med. doi:10.1016/j.freeradbiomed.2016.06.005
Angelova PR, Kasymov V, Christie I, Sheikhbahaei S, Turovsky E, Marina N, Korsak A, Zwicker J, Teschemacher AG, Ackland GL, Funk GD, Kasparov S, Abramov AY, Gourine AV (2015) Functional oxygen sensitivity of astrocytes. J Neurosci 35:10460–10473
Bélanger M, Magistretti PJ (2009) The role of astroglia in neuroprotection. Dialogues Clin Neurosci 11(3):281–295
Brouns I, Pintelon I, Timmermans JP, Adriaensen D (2012) Novel insights in the neurochemistry and function of pulmonary sensory receptors. Adv Anat Embryol Cell Biol 211:1–115
Buckler KJ (2013) TASK-like potassium channels and oxygen sensing in the carotid body. Respir Physiol Neurobiol 157(1):55–64
Buniel M, Glazebrook PA, Ramirez-Navarro A, Kunze DL (2008) Distribution of voltage-gated potassium (Kv) and hyperpolarization-activated (HCN) channels in sensory afferent fibers in the rat carotid body. J Comp Neurol 510(4):367–377
Cutz E, Pan J, Yeger H, Domnik NJ, Fisher JT (2013) Recent advances and controversies on the role of pulmonary neuroepithelial bodies as airway sensors. Semin Cell Dev Biol 24:40–50
Fukushi I, Takeda K, Yokota S, Hasebe Y, Sato Y, Pokorski M, Horiuchi J, Okada Y (2016) Effects of arundic acid, an astrocytic modulator, on the cerebral and respiratory functions in severe hypoxia. Respir Physiol Neurobiol 226:24–29
Gallego-Martin T, Agapito T, Ramirez M, Olea E, Yuber S, Rocher A, Gomez-Nino A, Obeso A, Gonzalez C (2015) Experimental observations on the biological significance of hydrogen sulfide in carotid body chemoreception. Adv Exp Med Biol 860:9–16
Ganfornina MD, López-Barneo J (1991) Single K+ channels in membrane patches of arterial chemoreceptor cells are modulated by O2 tension. Proc Natl Acad Sci U S A 88(7):2927–2930
Gonzalez C, Almaraz L, Obeso A, Rigual R (1994) Carotid body chemoreceptors: from natural stimuli to sensory discharges. Physiol Rev 74(4):829–898
Honda Y (1985) Role of carotid chemoreceptors in control of breathing at rest and in exercise: studies on human subjects with bilateral carotid body resection. Jpn J Physiol 35(4):535–544
Izumizaki M, Pokorski M, Homma I (2004) The role of the carotid bodies in chemosensory ventilatory responses in the anesthetized mouse. J Appl Physiol 97:1401–1407
Jiang C, Haddad GG (1994) Oxygen deprivation inhibits a K+ channel independently of cytosolic factors in rat central neurons. J Physiol 481(1):15–26
Kasymov V, Larina O, Castaldo C, Marina N, Patrushev M, Kasparov S, Gourine AV (2013) Differential sensitivity of brainstem versus cortical astrocytes to changes in pH reveals functional regional specialization of astroglia. J Neurosci 33(2):435–441
Kumar P (2007) Sensing hypoxia in the carotid body: from stimulus to response. Essays Biochem 43:43–60
Lahiri S, Roy A, Baby SM, Hoshi T, Semenza GL, Prabhakar NR (2006) Oxygen sensing in the body. Prog Biophys Mol Biol 91(3):249–286
Marczak M, Pokorski M (2004) Oxygen breathing and ventilation. J Physiol Pharmacol 55(1 Pt 1):127–134
McNamara CR, Mandel-Brehm J, Bautista DM, Siemens J, Deranian KL, Zhao M, Hayward NJ, Chong JA, Julius D, Moran MM, Fanger CM (2007) TRPA1 mediates formalin-induced pain. Proc Natl Acad Sci U S A 104(33):13525–13530
Ortega-Sáenz P, Levitsky KL, Marcos-Almaraz MT, Bonilla-Henao V, Pascual A, López-Barneo J (2010) Carotid body chemosensory responses in mice deficient of TASK channels. J Gen Physiol 135(4):379–392
Ortiz FC, Del Rio R, Varas R, Iturriaga R (2012) Contribution of TASK-like potassium channels to the enhanced rat carotid body responsiveness to hypoxia. Adv Exp Med Biol 758:365–371
Peers C, Wyatt CN, Evans AM (2010) Mechanisms for acute oxygen sensing in the carotid body. Resp Physiol Neurobiol 174(3):292–298
Peng Y-J, Nanduri J, Raghuraman G, Souvannakitti D, Gadalla MM, Kumar GK, Snyder SH, Prabhakar NR (2010) H2S mediates O2 sensing in the carotid body. PNAS 107(23):10719–10724
Piskuric NA, Vollmer C, Nurse CA (2011) Confocal immunofluorescence study of rat aortic body chemoreceptors and associated neurons in situ and in vitro. J Comp Neurol 519(5):856–873
Pokorski M (1999) Control of breathing. In: Cherniack NS, Altose MD, Homma I (eds) Rehabilitation of the patient with respiratory disease. The McGraw-Hill Companies, New York, pp 69–86
Pokorski M, Takeda K, Sato Y, Okada Y (2014) The hypoxic ventilatory response and TRPA1 antagonism in conscious mice. Acta Physiol (Oxf) 210(4):928–938
Takahashi N, Kuwaki T, Kiyonaka S, Numata T, Kozai D, Mizuno Y, Yamamoto S, Naito S, Knevels E, Carmeliet P, Oga T, Kaneko S, Suga S, Nokami T, Yoshida J, Mori Y (2011) TRPA1 underlies a sensing mechanism for O2. Nat Chem Biol 7(10):701–711
Williams SE, Wootton P, Mason HS, Bould J, Iles DE, Riccardi D, Peers C, Kemp PJ (2004) Hemoxygenase-2 is an oxygen sensor for a calcium-sensitive potassium channel. Science 306(5704):2093–2097
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Pokorski, M., Takeda, K., Okada, Y. (2016). Oxygen Sensing Mechanisms: A Physiological Penumbra. In: Pokorski, M. (eds) Advancements in Clinical Research. Advances in Experimental Medicine and Biology(), vol 952. Springer, Cham. https://doi.org/10.1007/5584_2016_67
Download citation
DOI: https://doi.org/10.1007/5584_2016_67
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-48032-9
Online ISBN: 978-3-319-48033-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)