Abstract
Conservatively, ten million people in the USA alone may suffer from RH and may be similarly prevalent elsewhere. Given the strong linear correlation between hypertension and cardiovascular outcomes, better control is paramount. We favor a multi-pronged approach. It may not suffice to address this by pharmacologic means only. Careful attention to modifiable risk factors, particularly sodium intake, adhering to a proper diet (i.e. DASH), and avoiding agents, i.e. non-steroidals, that can elevate the blood pressure, is key. Frequent follow up to establish the right treatment regimen and home blood pressuring monitoring can have a strong impact on control. Finally, consideration of device therapy may be a more viable option in the future.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Resistant hypertension
- Hyperaldosteronism
- Renovascular hypertension
- Obstructive sleep apnea
- Cushing syndrome
- Chronic kidney disease
- Liddle syndrome
- Coarctation of aorta
- Pheochromocytoma
- Sympathectomy
- Carotid sinus baroreceptor electrical stimulation
1 Introduction
Hypertension is the most common chronic disease in the developed world. Between 2005 and 2008, the National Health and Nutrition Examination Survey (NHANES) estimated that nearly one quarter of U.S. adults were hypertensive, and of those only one half were considered controlled. Therefore, adequate control is of utmost public health importance given the linear relationship between blood pressure and cardiovascular risk.
While essential hypertension (EH) usually results from a complex interaction between genetic traits and lifestyle factors such as weight, stress, and sodium intake, several other defined forms of hypertension exist. Among these are white coat hypertension, masked hypertension, resistant hypertension (RH), refractory hypertension and pseudohypertension. This chapter will focus on RH which is defined as a blood pressure of >140/90 despite appropriate adherence to a regimen of three antihypertensive agents including a diuretic. Its actual prevalence unknown, estimates in several recent studies show it to be an increasingly common finding.
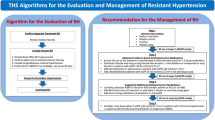
Therapy in RH, as in EH, requires not only pharmacologic intervention, but also lifestyle modification, careful scrutiny of pharmacologic and herbal remedies, supplements, and over the counter agents. Device therapy may offer promise in the future. Certain epidemiologic factors appear more prevalent in the RH population than in other hypertensive cohorts. Recognition of these patients is a challenge to clinicians but several clues may identify patients for targeted therapies.
In this chapter, we will describe the epidemiology, prognosis, disease states, diagnostic evaluation, non-pharmacologic and pharmacologic treatment of RH.
2 Establishing the Diagnosis
Distinguishing RH from other forms of hypertension is critical. The sine qua non of RH is a blood pressure > 140/90 on three maximally dosed/tolerated drugs including a well-dosed diuretic, preferably a thiazide or mineralocorticoid antagonist rather than a loop diuretic which tends to be less effective in blood pressure control (Sarafidis 2011). Correct blood pressure measuring is also critical and is described elsewhere (Kaplan and et al. 2010). Table 1 lists the forms of hypertension and associated diagnostic criteria.
3 Epidemiology
The actual prevalence of RH is unknown but estimates range from 8 to 15 % of all hypertensive subjects. An ethnically diverse cross-sectional study done in the Kaiser-Permanente system in Southern California between 2006 and 2007 revealed 12.8 % of all hypertensive individuals met criteria for RH. This was particularly common among males, those of black race, obese, and older subjects. Diabetes mellitus, ischemic heart disease, congestive heart failure, and chronic kidney disease (CKD) also associated with RH (Pimenta et al. 2012).
In the most recent National Health and Nutrition Examination Survey (NHANES) between 2005 and 2008, among 6000 adults with hypertension, 11.8 % had RH. Between 1988–1994 and 1999–2004 the prevalence was estimated to 5.5 and 8.5 % respectively. In today’s terms, based on the latest NHANES data some 76 million Americans are hypertensive, of which 12 % or nine million individuals may be resistant (Pimenta et al. 2012; Persell 2011).
In the Antihypertensive and Lipid-Lowering Treatment To Prevent Heart Attack trial (ALLHAT), International Verapamil-Trandolapril Study (INVEST), and Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trials RH was estimated at 8–15 % of these hypertensive cohorts (The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group 2002; Pepine et al. 1998; Jamerson et al. 2008).
4 Prognosis
Patients with RH are at greater risk for end organ damage such as left ventricular hypertrophy (LVH), CKD, and albuminuria than those patients who have controlled blood pressure (Sarafidis 2011).
Retrospectively, Daugherty et al. found that RH was significantly associated with a 47 % increased risk of adverse cardiovascular outcomes (Daugherty 2012). Armario studied 513 patients in a Spanish cohort with RH finding LVH by echocardiography in 57 %; 46 % had albuminuria (Armario 2011).
Successfully lowering blood pressure in RH may reduce cardiovascular events. Pisoni et al showed a 96 % reduction in cardiovascular events over 18 months with the use of 3 antihypertensive agents versus placebo in patients with severe diastolic hypertension (Pisoni 2009).
Sales et al demonstrated the additional clinical benefits of ambulatory blood pressure monitoring (ABPM) in RH and found that elevated systolic and diastolic blood pressures predicted cardiovascular and overall mortality (Salles et al. 2008).
5 RH: Associated Medical Conditions: Secondary Causes of Hypertension and Workup
Table 2 lists the most common causes of RH.
5.1 Primary Hyperaldosteronism
Among patients with RH, primary hyperaldosteronism (PHA) is likely the most common identifiable cause. In an analysis of 88 patients with RH, 20 % had PHA (Calhoun et al. 2002). Acelajado et al. found a 17 % prevalence of RH due to PHA (Acelajado 2011).
Screening should occur in hypertensive subjects with unexplained or unprovoked hypokalemia, or if induced by diuretics, resisting correction. Those with a strong family history of hypertension, especially early-onset (<40 years), drug resistant hypertension, hypertensive with an adrenal “incidentaloma,” should also be screened. Morning samples for plasma aldosterone concentration (PAC), plasma renin activity (PRA) and an aldosterone to renin ratio (ARR) are obtained. We suggest holding MRAs and continuing all other drugs to avoid accelerating hypertension.
An ARR above 20 is consistent with PHA. Additionally, a PAC of greater than 15 ng/dl yields a positive screening result. Twenty-four urinary aldosterone measurements confirm the diagnosis. Salt sensitivity is diagnosed when the Aldosterone levels are relatively high but fail to reach threshold values for PHA. These patients are highly responsive to MRAs but also to simple sodium restriction.
Computed tomography (CT) represents the best test for this for confirming an adrenal tumor. Incidental adrenal adenomas are found in 4 % of the general population on CT, and are particularly common after the age of 40. Proceeding to adrenal vein sampling is reasonable in the hypertensive patient over 40 with an adenoma. This can help lateralize the hormonal excess and direct surgical excision. In bilateral adrenal hyperplasia medical therapy with MRAs is best. (Mantero 2000).
5.2 Renovascular Hypertension
Renovascular hypertension is common among hypertensive patients with multiple risk factors for atherosclerotic disease, particularly those with RH.
An abdominal bruit and known history of athereosclerosis and tobacco use are commonly seen. Patients challenged with ACE inhibitors (ACE I) or Angiotensin Receptor Blockers (ARB may get ischemic nephropathy due to the effects on Angiotensin II and the efferent renal arteriole. Bloodwork usually shows an elevated PRA and PAC. Once suspected, imaging modalities, particularly duplex ultrasonography, magnetic resonance angiography (MRA) and computed tomography angiography (CTA) are performed.
In duplex ultrasonography, reliable detection of RAS is operator dependent and sensitivity and specificity do not compare favorably with MRA or CTA. MRA confers the risk of gadolinium induced nephrogenic systemic fibrosis, a syndrome linked to individuals with a GFR <30 ml/min. CTA requires a significant volume of contrast and may be contraindicated in those with advancing CKD. Conventional intraarterial angiography can confirm diagnosis. Unfortunately, three separate trials have shown no benefit to interventional approaches relative to medical management and this often leads to a diagnostic quandary as to whether to pursue this diagnosis at all (Cooper et al. 2014; The Astral Trial Investigators 2009; Bax et al. 2009).
Therapy usually includes dual anti-platelet therapy, antihyperlipidemic drugs, and blood pressure control. Use of ACE I or ARB is generally discouraged due to the risk of ischemic nephropathy (Cooper et al. 2014).
5.3 Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) occurs when there is a partial or complete collapse of the airway during sleep. Affecting nearly 2.4 % of adults, it is associated with mortality and cardiovascular risks (Drager 2010). The Ohasama study showed each 5 % deficiency in the normal decline in nocturnal blood pressure was associated with an approximate 20 % increase in risk of cardiovascular mortality (Ohkubo et al. 2000). The prevalence of OSA in hypertensive patients may be as high as 56 % and in resistant hypertensive patients, nearly 80 %.
Polysomnography confirms the diagnosis when the apnea hypopnea index (AHI) is greater than 5. Alajmi et al. identified ten randomized controlled trials that found that the effects of CPAP on reduction of blood pressure were modest and not significant. Reductions in BP tended to be larger in patients with severe OSA (AHI > 30), and a trend for systolic BP reduction was associated with higher CPAP adherence (Alajmi 2007; Hyun 2015).
5.4 Chronic Kidney Disease
Broadly this diagnosis captures glomerular and vascular disorders, hypertension, diabetic kidney disease and other forms. The Chronic Renal Insufficiency Cohort (CRIC) investigators looked at nondialysis CKD patients. Fully 40 % of the cohort had RH and among these there was a higher risk of congestive heart failure and CKD progression versus those without RH (Thomas 2015).
Increased fluid and sodium retention and subsequent intravascular expansion leads to treatment resistance. Khosla et al found that MRAs are effective and safe to reach goal blood pressure amongst patients with diabetic nepheropathy when added to a triple antihypertensive regimen of diuretic, ACE I and Calcium Channel Blocker (CCB). Aside from the reduction of blood pressure, they are modestly antiproteinuric (Khosla 2009; Williams et al. 2015). Treating the underlying renal disorder may also be of some benefit.
5.5 Cushing Syndrome
Hypertension is present in 70–90 % of patients with Cushing’s syndrome (Moneva 2002).
Screening consists of an early morning Cortisol reading which can be verified either by a low dose dexamethasone suppression test (DST) or measurement of a 24-h urinary free cortisol level. Following DST a morning plasma cortisol level is drawn. Levels greater than 5 mg/dL are consistent with Cushing’s Syndrome. Alternatively, a 24 h urine cortisol level over 55 mcg confirms the diagnosis. Further testing/imaging should follow to determine if there is an ectopic, pituitary or adrenal source. CT or MRI of the pituitary and adrenals should secure the diagnosis.
The therapy used in Cushing Syndrome to treat patients with hypertension is the same treatment of EH. The use of MRA may be particularly effective in patients with very high cortisol levels. In a study by Ulick et al, cortisol was the major mineralocorticoid in ectopic ACTH syndrome (Moneva 2002; Ulick et al. 1992).
5.6 Coarctation of the Aorta
Coarctation of the aorta accounts for approximately 6–8 % of congenital heart disease in infants and children. Although rare compared with other causes of secondary hypertension, accounting for only 0.2 % of the adult population, clinicians should be aware of the elements of physical exam abnormalities that can point to the diagnosis (Prisant 2004). Aortic imaging confirms the diagnosis. Early correction is advised (Prisant 2004; Yetman 1997).
5.7 Liddle Syndrome
Liddle Syndrome is a rare form of autosomal dominant hypertension. Clinically, hypertension usually begins in childhood. Genetic testing is available but costly. Diagnosis is often clinical. Despite a clinical presentation typical of primary aldosteronism, PRA and PAC are low. Potassium-sparing diuretics are the therapy of choice in Liddle syndrome (Rose 2001).
5.8 Pheochromocytoma
Pheochromocytomas account for fewer than 0.2 % cases of hypertension. Almost one half of these patients have RH whereas most of the rest have apparent EH (Stein 1981).
Once suspected, interfering medications, such as tricyclics and other psychoactive agents, in the screening and confirmation of the diagnosis should be discontinued 2 weeks prior to the assessment. Screening includes 24 h urinary and plasma catecholamine levels and may include MIBG scintigraphy. Although 10 % of pheochromocytomas are extra-adrenal, 95 % are intra-abdominal. CT or MRI of the abdomen are highly sensitive (98–100 %) but only 70 % specific due to the high prevalence of adrenal “incidentalomas.” (Guerrero 2009)
Surgical resection is the definitive treatment. Preoperatively, therapy is aimed at controlling blood pressure and prevent intraoperative HTN. Phenoxybenzamine is the preferred drug of choice as well as propanolol which is initiated thereafter. This order of treatment is important to avoid stimulating unopposed alpha adrenergic receptors (Tauzin-Fin 2004).
6 RH: Lifestyle Factors/Modifications
While establishing a secondary cause can allow the practitioner to address a specific issue, i.e. treating PHA with an MRA, often a secondary cause is elusive. In the a section below drug options will be discussed. As medical costs continue to climb, efforts to find inexpensive solutions to expensive problems is paramount. If the prevalence estimates of RH are correct at 8–15 % of the hypertensive population, the economic implications are astounding. This assumes that lowering blood pressure will lead to fewer cardiovascular, cerebrovascular and renal outcomes. Correcting modifiable risk factors may offer a very cost-sensitive way to approach this problem. The upcoming Triumph trial will look at an RH population and assess the value of exercise training, low sodium diet, DASH diet, and weight management (Blumenthal et al. 2015). Our current practice is to address these factors as we would in other hypertensive populations in the hopes the results will be similar. Table 3 lists many of the modifiable risk factors and the magnitude of their effects.
6.1 Sodium Consumption
The majority of patients with RH may consume more than 10 g of sodium per day. In a resistant population on a mean off 3–4 antihypertensive agents, Calhoun et al demonstrated that lower sodium intake (50 mmol/day vs 250 mmol) decreased blood pressures by 23/10 mmHg (office readings and ABPM) (Calhoun 2009). In current guidelines for hypertensive individuals, dietary sodium should be less than 100 mmol/ day or 2.4 g of sodium chloride (Calhoun 2009). For salt sensitive patients, even lower amounts of sodium may be necessary. Two pivotal trials highlight the effect of sodium restriction and how it is magnified by Thiazide diuretic usage. Fothersby et al studied 17 untreated subjects with a mean systolic BP of 176 +/− 11 mmHg and simply applied an 80–100 mmol/day sodium restriction without any antihypertensive agents. The BP fell a disappointing 5/2 mmHg. Gavras et al however showed that by adding a thiazide diuretic to an austere sodium diet (10 mmol/day) BP fell 21/7 mmHg (Gavras 1981; Fothersby 1993).
6.2 Weight Loss
The Dietary Approaches to Stopping Hypertension (DASH) trial utilized a Mediterranean diet with low fat, high fiber, rich in calcium and potassium, and lowered systolic BP by 11 mmHg in just 2 weeks’ time. When sodium restriction was added the BP fell a bit further but was less well-tolerated (Sacks et al. 2001). We target a BMI goal of < 25 kg/m2. The German Hydra Trial demonstrated that for a BMI > 40 kg/m(2) vs < 25 kg/m(2), there was 5.3 fold increased risk of RH and a 3.2 fold risk of refractory hypertension (Sharma et al. 2004). The additive effect of exercise and alcohol moderation can be a useful adjunct.
6.3 Over the Counter Agents, Supplements, and Medications That Can Raise Blood Pressure
A growing trend toward alternative therapies exists and patients often seek “non-traditional” therapies to treat various maladies. Additionally, certain over the counter agents can raise the blood pressure and should be avoided, particularly in those with RH. Other agents are medically necessary, e.g. immunosuppressants in a transplant recipient and little can be done. Table 4 lists these and recommendations/comments.
6.4 Pharmacologic Therapy
While certain forms of RH mandate specific therapy, i.e. CPAP for OSA or adrenalectomy for an aldosterone secreting tumor, when there is no such directed therapy, there is little available data to guide treatment options. To satisfy the definition of RH, diuretic therapy is mandatory, and we prefer thiazides and mineralocorticoid antagonists to loop diuretics. Further, lacking much guidance in the literature we advocate using the first line agents from the Joint National Committee VIII recommendations which would include treating with an ACE I or ARB and a dihydropyridine CCB such as Amlodipine (James et al. 2014). The Pathways II trial showed that among those with RH, Aldactone was superior to Bisoprolol or Doxazosin for blood pressure control. The Resistant Hypertension Optimal Treatment Trial is a Brazilian study will compare spironolactone to clonidine as the best fourth agent to a standard regimen that includes diuretics, ace inhibitors/angiotensin receptor blockers and a calcium channel blocker (Williams et al. 2015; Krieger et al. 2014).
We further recommend those with RH purchase a blood pressure cuff, be instructed on proper use, and keep a diary of readings. Calibrating the cuff with an office cuff can be helpful. Ambulatory blood pressure monitoring intuitively makes sense but is not reimbursed, is expensive and not widely available. Patients are counseled that controlling blood pressure may take weeks to months or longer and requires frequent follow up.
6.5 Device Therapy
In light of the prevalence of RH and hypertension in general, the inherent difficulties in effectively treating the disease(s), and potential impact of a successful non-pharmacological therapy, several different devices have been trialed. Unfortunately, the results have thus far been disappointing.
Surgical sympathectomy in the 1920s “cured” hypertension but at the expense of causing syncope and a host of other neurologic findings (Grimson et al. 1949). Catheter-based renal denervation resulted whereby an electrical pulse within the renal arterial lumen severs sympathetic fibers from the brain to the kidney. Initial results from the european Symplicity II investigators were promising (office blood pressure fell systolically by 32 mmHg versus placebo) but failed in a larger trial (Esler et al. 2010; Bhatt et al. 2014).
Carotid Sinus Baroreceptor Electrical Stimulators send an impulse to the brain that BP is actually higher reflexively causing reduction in sympathetic output, and lower BP. Of the 265 subjects with RH in the trial nearly 80 % of those treated experienced a 44 mmHg decline in systolic blood pressure. As the trial failed to meet 2 of its 5 pre-specified endpoints (short-term efficacy and procedure-related adverse events) it remains unapproved in the U.S. by the Food and Drug Administration (Bisognano 2011).
Central Arteriovenous Anastomosis creates a conduit anastomosis between large vessels, shunting substantial blood volume into high-capacity, low-resistance venous system, thereby decreasing total systemic vascular resistance and therefore BP. Lobo et al studied 88 patients with RH and found mean office systolic blood pressure and mean ambulatory blood pressure fell by 26.9 and 13.5 mmHg among those treated versus 3.7 and 0.5 mmHg not treated (Lobo 2015). Median and vagus nerve stimulators may offer promise as well but remain poorly studied.
Works Cited
Acelajado MC, Calhoun DA (2011) Aldosteronism and resistant hypertension. Int J Hypertens 2011:837817. doi:10.4061/2011/837817
Alajmi M (2007) Impact of continuous positive airway pressure therapy on blood pressure in patients with obstructive sleep apnea hypopnea: a meta analysis of randomized control trials. LUNG 185(2):67–72
Armario P (2011) Prevalence of target organ damage and metabolic abnormalities in resistant hypertension. Med Clin (Barc) 137(10):435–439
Bax L et al (2009) Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 150:840–848
Bhatt D et al (2014) A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370:1393–1401
Bisognano JD (2011) Baroflex activation lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol 58(7):765–73
Blumenthal JA et al (2015) Lifestyle modification for resistant hypertension: the TRIUMPH randomized clinical trial. Am Heart J 170(5):986–994
Calhoun D (2009) Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 54:475–481
Calhoun D (2010) Sleep and hypertension. CHEST 138(2):434–443
Calhoun DA et al (2002) Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension 40:892–896
Cooper C et al (2014) Stenting and medical therapy for atherosclerotic renal- artery stenosis. N Engl J Med 370:13–22
Daugherty SL (2012) Incidence and prognosis of resistant hypertension in hypertensive patients. Hypertension 125(13):1635–1642
Drager L (2010) Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol 105(8):1135–1139
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M (2010) Renal sympathetic denervation in patients with treatment-resistant hypertension (the SYMPLICITY HTN-2 Trial): a randomised controlled trial. Lancet 376:1903–1909
Fothersby M (1993) Effects of moderate sodium restriction on clinic and twenty-four-hour ambulatory blood pressure in elderly hypertensive subjects. J Hypertens 11
Gavras H (1981) Role of reactive hyperreninemia in blood pressure changes induced by sodium depletion in patients with refractory hypertension. Hypertension 3(4): 441–447, Jul–Aug
Grimson KS, Orgain ES, Anderson B, Broome RA, Longino FH (1949) Results of treatment of patients with hypertension by total thoracic and partial to total lumbar sympathectomy, splanchnicectomy and celiac ganglionectomy. Ann Surg 129:850–871
Guerrero M (2009) Clinical spectrum of pheochromocytoma. J Am Coll Surg 209(6):727–732
Hyun JM (2015) Clinical features of obstructive sleep apnea that determine its high prevalence in resistant hypertension. Yonsei Med K 56(5):1258–1265
Jamerson K et al (2008) Benazepril plus Amlodipine or Hydrochorothiazide for hypertension in high risk patients. N Engl J Med 359:2417–2428
James P et al (2014) Evidence-based guidelines for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC8). JAMA 311:284–427
Kaplan N et al (2010) Clinical hypertension. Lippincott, Philadelphia, Print
Khosla N (2009) Predictors of hyperkalemia risk following hypertension control with aldosterone blockade. Am J Nephrol 30(5):418–424
Krieger EM et al (2014) Resistant hypertension optimal treatment trial: a randomized controlled trial. Clin Cardiol 37(6):388
Lobo M (2015) Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension.(the ROX CONTROL HTN study): a randomised controlled trial. Lancet 385: 1634–1641
Mantero F (2000) A survey on adrenal incidentaloma in Italy. Study Group on adrenal tumors of the Italian Society of Endocrinology. J Clin Endocrinol Metab 637
Moneva M (2002) Pathophysiology of adrenal hypertension. Semin Nephrol 22:44–53
Ohkubo T et al (2000) Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens 18(7):847–854
Pepine CJ, Handberg-Thurmond E, Marks RG et al (1998) Rationale and design of the International Verapamil SR/Trandolapril Study (INVEST): an Internet-based randomized trial in coronary artery disease patients with hypertension. J Am Coll Cardiol 32(5):1228–1237
Persell SD (2011) Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 57:1076–1080
Pimenta E et al (2012) Resistant hypertension: incidence, prevalence, and prognosis. Circulation 125(13):1594–1596
Pisoni R (2009) Characterization and treatment of resistant hypertension. Curr Cardiol Rep 11:407–413
Prisant L (2004) Coarctation of the aorta: a secondary cause of hypertension. J Clin Hypertens 6:347–350
Rose BD (2001) Clinical physiology of acid–base and electrolyte disorders. McGraw Hill, New York, Print
Sacks F et al (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. New Engl J Med 344(1):3–10
Salles GF et al (2008) Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med 168(21):2340–2346
Sarafidis P (2011) Epidemiology of resistant hypertension. J Clin Hypertens 13:523–528
Sharma A et al (2004) High prevalence and poor control of hypertension in primary care: a cross-sectional study. J Hypertens 22:479–486
Stein P (1981) A simplified diagnostic approach to pheochomocytoma. A review of the literature and report of one institution's experience. Medicine (Baltimore) 46–66
Tauzin-Fin P (2004) Effects of perioperative alpha block on haemodynamic control during laparoscopic surgery for phaeochromocytoma. Br J Anaestholy 92:512–517
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs. diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA 288:2981–2997
The Astral Trial Investigators (2009) Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 361:1953–1962
Thomas G (2015) Prevalance and prognostic significance of apparent treatment resistant hypertension in chronic kidney disease: Report from the Chronic Renal Insufficiency Cohort Study. Hypertension 67(2):387–396
Ulick S et al (1992) Cortisol inactivation overload: a mechanism of mineralocorticoid hypertension in the ectopic adrenocorticotropin syndrome. J Clin Endocrinol Metab 74:963–967
Williams B et al (2015) Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet 386:2059–2068
Yetman AT (1997) Balloon angioplasty of recurrent coarctation: a 12 year review. J Am Coll Cardiol 30(3):811–816
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing AG
About this chapter
Cite this chapter
Valsan, D., Burhan, U., Teehan, G. (2016). Resistant Hypertension. In: Islam, M.S. (eds) Hypertension: from basic research to clinical practice. Advances in Experimental Medicine and Biology(), vol 956. Springer, Cham. https://doi.org/10.1007/5584_2016_38
Download citation
DOI: https://doi.org/10.1007/5584_2016_38
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44250-1
Online ISBN: 978-3-319-44251-8
eBook Packages: MedicineMedicine (R0)