Abstract
The prevalence of hypertension increases with age making it a significant health concern for older persons. Aging involves a range of physiological changes such as increases in arterial stiffness, widening pulse pressure, changes in renin and aldosterone levels, decreases in renal salt excretion, declining in renal function, changes in the autonomic nervous system sensitivity and function and changes to endothelial function all of which may not only affect blood pressure but may also affect individual response to pharmacotherapy used to manage hypertension and prevent end organ damage and other complications associated with poor blood pressure control.
Unlike many chronic conditions where there is limited evidence for management in older populations, there is good evidence regarding the management of hypertension in the elderly. The findings from multiple large, robust trials have provided a solid evidence-base regarding the management of hypertension in older adults, showing that reduction of blood pressure in older hypertensive populations is associated with reduced mortality and morbidity. Diuretics, agents action on the renin angiotensin system, beta blockers and calcium channel blockers have all been well studied in older populations both in view of the benefits associated with blood pressure lowering and the risks associated with associated adverse events. While all antihypertensive agents will lower blood pressure, when managing hypertension in older persons the choice of agent is dependent not only on the ability to lower blood pressure but also on the potential for harm with older persons. Understanding such potential harms in older populations is essential with older persons experiencing increased sensitivity to many of the adverse effects such as dizziness associated with the use of antihypertensive agents.
Despite the wealth of evidence regarding the benefits of managing hypertension in the old and very old, a significant proportion of older individuals with hypertension have suboptimal BP control. While there is good evidence supporting blood pressure lowering in older antihypertensive agents, these have not yet been optimally translated fully into clinical guidelines and clinical practice. There appear to be considerable differences between guidelines in terms of the guidance given to clinicians. Differences in interpretation of the evidence, as well as differences in study design and populations all contribute to differences in the guideline recommendations with respect to older populations, despite the strength of the underlying scientific evidence. Differences around who is considered “old” and what BP targets and management are considered appropriate may lead to confusion among clinicians and further contribute to the evidence-practice lag.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Hypertension is the leading modifiable cause of mortality worldwide. The prevalence of hypertension increases with age making it a significant health concern for older persons. Unlike many chronic conditions, there is good evidence regarding the management of hypertension in the elderly exists and pharmacotherapy is the mainstay of treatment for most patients. Given predicted international increases in the elderly population and the wealth of evidence regarding management of hypertension in the elderly, understanding how the risks associated with hypertension increase with age as well as how physicians currently manage older patients with increased blood pressure is important. Furthermore, insight into current barriers to the provision of optimal management is essential if we are to meet the health needs of the growing older population.
1 Who Is Old?
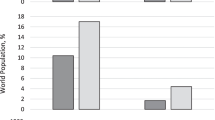
Internationally the proportion of the population that is considered older is increasing. In 1950, 8 % of the population was aged over 65 years, this increased to 10 % in 2000 and is predicted to exceed 20 % by 2050.(Department of Economic and Social Affairs United Nations 2002) It has been estimated that life expectancy for those aged 65 years has increased by 19 years for men and 17 years for women over the past century.(Rai and Mulley 2007) Projections indicate that by 2050 there will be over 2 billion older persons worldwide.(Halter 2009) However while there is international agreement that the population is aging there is less agreement regarding who should be considered “old”. (Gambert 1994) Aging encompasses a number of domains and different definitions focus on different aspects of the aging process. Chronological age is the simplest and most commonly used parameter to define age and refers simply to the number of years since birth. Yet aging is multidimensional and not just related to the duration of time in an individual’s life. Physiologically, aging refers to the general and gradual changes that human body experiences over time. Physiological aging is characterized by declining functional capacity, decreasing fertility and increased mortality all of which may vary from individual to individual. (Kirkwood and Austad 2000; Masoro and Austad 2006) Such variation among older populations and how it affects their response to pharmacotherapy is one of the challenges facing clinicians in the management of hypertension among older populations.
2 Hypertension and Aging
Population aging presents a number of healthcare challenges. There are implications in terms of resources and funding, as well as in the type of care that is delivered. Non-communicable chronic diseases such as cardiovascular disease currently account for almost two-thirds of deaths worldwide. (Mathers and Loncar 2006; Daar et al. 2007) Cardiovascular disease contributes significantly to the disease burden, disability and death in both developed and developing countries (Beaglehole et al. 2008; Murray and Lopez 1997; Yang et al. 2008) with an increasing burden among the elderly..(Daar et al. 2007; Murray and Lopez 1997) Despite predicted increases in population aging, The World Health Organization (WHO) has predicted that ischemic heart disease and stroke will remain among the leading causes of death worldwide. (Mathers and Loncar 2006) Hypertension is a major risk factor for cardiovascular disease (Menotti et al. 2004; Lim et al. 2013), affecting up to one billion individuals internationally (Chobanian et al. 2003) (Kumar 2013). It is one of the leading cause of death worldwide (The World Health Organisation 2016). The prevalence of hypertension increases with age (Fagard 2002), with approximately 30 % of the population aged under 60 years being considered hypertensive. Once we start looking at older populations, the prevalence of hypertension doubles to over 60 % for those aged over 60 years, with even higher prevalence with further aging as demonstrated by data from both the UK Framingham study (Kannel and Gordan 1978; Vasan et al. 2002; Beckett et al. 2012) and the US National Health and Nutrition Survey (NHANES) (Lloyd-Jones et al. 2005). The NHANES data demonstrates that increases in hypertension prevalence begin in adulthood, with the prevalence doubling between the ages of 20 and 40 years, and doubling again between 40 and 60 years (Kannel and Gordan 1978), while the Framingham study showed that this pattern continues with ongoing aging, with the prevalence of hypertension increasing from 27.3 % in those aged ≥ 60 years to 74.0 % in those aged over 80 years (Vasan et al. 2002).
Gender differences in the prevalence of hypertension have been noted in both younger and older populations. A number of studies have shown found that while the prevalence of hypertension is higher in younger males, this reverse after the age of 60, when the prevalence in females is greater than that in males (Halter 2009; Franklin et al. 1997; Mann 1992; Hajjar and Kotchen 2003; Primatesta and Poulter 2004; Trenkwalder et al. 1994; Gambassi et al. 1998).
Differences in the hypertension phenotype with respect to increases in systolic (SBP) compared with diastolic blood pressure (DBP) have also been reported in older hypertensive populations. Both systolic (SBP) and diastolic blood pressure (DBP) increase with age, (Franklin et al. 1997) however it has been proposed that DBP may plateau or even decrease from the age of 60 years, leaving the SBP to increase (Franklin et al. 2001). Such differences may account for the increase in isolated systolic hypertension that is noted among older populations. Increases in hypertension among older persons may be due to pathophysiological changes associated with aging such as increased peripheral vascular resistance due to arterial stiffening (Franklin et al. 1997; Mitchell et al. 2004). This increase in arterial stiffness with ageing is proposed to alter the normal hemodynamic patterns causing an increase in pulse wave velocity which is an index of arterial stiffness and a widening pulse pressure may account for age related decreases in DBP and increases in SBP (Mann 1992; Mitchell et al. 2004; Pinto 2007; Mackey et al. 2002). Other age related factors such as the changes in renin and aldosterone levels, decreases in renal salt excretion, declining in renal function, changes in the autonomic nervous system sensitivity and function and changes to endothelial function may further contribute to the increases in hypertension seen with aging (Halter 2009; Weinberger 1996; Fliser and Ritz 1998; Wallace et al. 2007). Age related life style changes such as decreased physical activity, changes in body fat composition, high sodium intake and obesity may further contribute to the development of hypertension among older persons. Moreover a synergistic effect on the risk of hypertension has been observed when multiple factors exist together (Halter 2009; Carretero and Oparil 2000; MacMahon et al. 1984; Barreto et al. 2001).
3 Pseudohypertension
Pseudohypertension is occasionally observed in older persons. In pseudohypertension, measurement of blood pressure using a sphygmomanometer results in a falsely elevated reading.(Kleman et al. 2013) This phenomenon is more common in older persons due to increased arterial stiffness, which results in falsely high reading upon blood pressure measurement due to the inability of the arteries to compress. Pseudohypertension is estimated to affect up to 7 % of patients with resistant hypertension (Kleman et al. 2013) and should be considered when older patients presenting with consistently elevated blood pressure over time but who show no signed of end organ damage or in those who treatment with antihypertensive agents result in ongoing symptoms of hypotension. In patients for whom pseudohypertension is suspected an intra-arterial blood pressure measurement is required.
3.1 Pharmacological Management of Hypertension in Older Populations
Unlike many conditions where limited evidence exists for management of those aged over 65 years due to the exclusion of older populations from clinical trials,(White 2010; Devlin 2010) the findings of multiple large, robust trials have provided a solid evidence-base regarding the management of hypertension in older adults. Adverse outcomes associated with poor blood pressure (BP) control in older persons have been well documented. A Cochrane review of 12 clinical trials showed that the management of hypertension in people aged 60 years and over was associated with a reduction in mortality (Relative Risk (RR)) = 0.9, 95 % confidence interval ((CI) 0.84–0.97).(Musini et al. 2009) The same review reported pharmacological management of hypertension in older adults was associated with significant reductions in both cardiovascular (RR = 0.77, 95 % CI 0.68–0.86) and cerebrovascular mortality (RR = 0.66, 95 % CI 0.53–0.82). (Musini et al. 2009) While life-style interventions are generally considered first-line for the management of all persons with hypertension, the majority of hypertensive patients, including older persons, will require pharmacotherapy to adequately control their blood pressure (Wallace et al. 2007). There have been a number of large well-conducted clinical trials exploring pharmacological management of hypertension in older populations and there is good evidence for the use of a variety of different antihypertensive agents in the management of hypertension in older persons (Pimenta and Oparil 2012).
3.1.1 Thiazide and Thiazide – Like Diuretics
Thiazides diuretics are one of the oldest drug classes used in the treatment of hypertension. (Huebschmann et al. 2006) Evidence of their effectiveness in lowering BP and preventing the cardiovascular and cerebrovascular adverse outcomes associated with hypertension in older people has been provided by several clinical trials, including the Hypertension in the very elderly trial (HyVET) (Beckett et al. 2012), the Swedish Trial in Old Patients with Hypertension (STOP) (Dahlöf et al. 1991; Hansson et al. 1999) and the Antihypertensive and Lipid-Lowering Treatment to prevent Heart Attack Trial; (ALLHAT) (Officers et al. 2002) studies While not all of these studies specifically recruited older participants, the mean participant age for all 3 was over 65 years, making their findings particularly pertinent to older populations.
Use of thiazide and thiazide like diuretics for the management of hypertension in older persons has declined over the past decade (Primatesta and Poulter 2004; Trenkwalder et al. 1994; Triantafyllou et al. 2010; Prencipe et al. 2000; Psaty et al. 2002). There are a number of factors that may have contributed to this decline including increased use of other non-thiazide diuretics, particularly by older persons with complicated hypertension (Van Kraaij et al. 1998) the advent of newer antihypertensives such as Calcium channel blockers (CCBs) and agents acting on the Renin Angiotensin System (RAS) and caution by prescribers due to increased risk of potential adverse drug reactions associated with the use of thiazide diuretics in frail, older persons (Onder et al. 2001; Moser 1998). Despite this general decline, the use of thiazide diuretics for the management of hypertension in the older individual remains high (Bromfield et al. 2014; Rodriguez-Roca et al. 2013; Tu et al. 2006), especially in fixed-dose combination products where they are among the most commonly used antihypertensive agents (Primatesta and Poulter 2004; Trenkwalder et al. 1994; Triantafyllou et al. 2010; Prencipe et al. 2000; Rodriguez-Roca et al. 2013; Svetkey et al. 1996).
3.1.2 Agents Acting on the Renin-Angiotensin System (RAS)
There are three main three antihypertensive classes that act on the RAS. These are the angiotensin blocking agents (ARBs), the Angiotensin converting enzyme inhibitors (ACEI) and the direct renin inhibitors (DRI). The use of both ARBs (Triantafyllou et al. 2010; Bromfield et al. 2014; Rodriguez-Roca et al. 2013) and ACEIs (Primatesta and Poulter 2004; Trenkwalder et al. 1994; Triantafyllou et al. 2010; Psaty et al. 2002; Bromfield et al. 2014; Rodriguez-Roca et al. 2013; Svetkey et al. 1996; Barker et al. 1998; Prince et al. 2012) in older populations has increased over recent years and now surpasses the use of many other antihypertensive classes. The increase in use of these agents for the management of hypertension in older populations has been supported by clinical trials such as the Second Australian National Blood Pressure (ANBP2) (Wing et al. 2003). ANBP2 demonstrated that ACEI were superior to thiazide diuretics in terms of cardiovascular outcomes in a population comprising 6083 older persons aged between 65 and 84 years. Despite benefits in cardiovascular outcomes no difference between ACEI and diuretics in terms of all cause mortality was observed. (Wing et al. 2003) In addition to increased use as monotherapy for the management of hypertension among older individuals, the use of ACEIs and ARBs in combination with other antihypertensive medications has also increased over recent years (Primatesta and Poulter 2004; Trenkwalder et al. 1994; Triantafyllou et al. 2010; Rodriguez-Roca et al. 2013; Svetkey et al. 1996). In contrast the uptake of aliskiren, a direct renin inhibitor has been slow. Aliskiren has been approved for use in older populations with hypertension since 2007 yet use of daily practice is limited in comparison to other antihypertensive agents (Bromfield et al. 2014; Rodriguez-Roca et al. 2013). The slow uptake of aliskiren for use among older persons may be in part due to concerns around limited efficacy and a poor safety profile (Parving et al. 2012; Gheorghiade et al. 2013).
3.1.3 Calcium Channel Blockers (CCBs)
Since the introduction of CCBs, the prescribing pattern of this antihypertensive medication class in older populations has increased both as monotherapy and combination therapy (Trenkwalder et al. 1994; Prencipe et al. 2000; Bromfield et al. 2014; Svetkey et al. 1996; Barker et al. 1998) and use remained steady until the mid 1990s (Psaty et al. 2002). Despite publication of the findings from the Systolic Hypertension in the Europe Trial (Syst-Eur) in 1997, which showed that treating 1000 patients for 5 years with a CCB prevented 29 strokes or 53 myocardial infarctions (MI), a decline in the use of CCB has generally been noticed in older and the very old patients since the mid-1990s.(Primatesta and Poulter 2004; Triantafyllou et al. 2010; Rodriguez-Roca et al. 2013) This decline may in part be due safety concerns with the use of CCBs older populations, including increased risk of cancer, MI and gastrointestinal haemorrhage with long-term use (Pahor et al. 1996a, b; Maclure et al. 1998).
3.1.4 Beta Blockers (BBs)
Beta blockers have been among the most commonly prescribed antihypertensive agents since their introduction into hypertension treatment (Psaty et al. 2002; Svetkey et al. 1996; Barker et al. 1998) However in recent years, use in older persons has declined following publication of a meta-analysis questioning the efficacy of the BB for hypertension and highlighting safety concerns, with an increased risk of stroke reported with use as monotherapy. (Larochelle et al. 2014) Consequently use of BBs for the management of hypertension in older populations has declined particularly as monotherapy for uncomplicated hypertension management. (Primatesta and Poulter 2004; Trenkwalder et al. 1994; Triantafyllou et al. 2010; Prencipe et al. 2000; Onder et al. 2001).
3.1.5 Alpha Blockers
While several studies have shown a slight increase in the use of alpha blockers in the management of hypertension in the old and very old (Psaty et al. 2002; Bromfield et al. 2014) in general, there has been a downward trend in the use of these agents (Trenkwalder et al. 1994; Rodriguez-Roca et al. 2013; Svetkey et al. 1996; Barker et al. 1998). This decline in use may be due to the poorer adverse effect profile of the alpha-blockers for older persons in comparison to newer agents such as the ACEI and ARBs, as well as to a lack of mortality evidence when compared with other antihypertensive agents.
3.1.6 Nitrates
While nitrates have an important role in the management of coronary artery disease, the lack of studies in older populations using nitrates for the management of hypertension have resulted in these drugs no longer having a major role in the management of hypertension. There has been some discussion around the potential benefit of nitrates for the management of hypertension in older populations, however to date they are not currently recommended in the main hypertension guidelines (Weber et al. 2014; Mancia et al. 2013a).
3.1.7 Choice of Antihypertensive Agent in Older Populations
While all antihypertensive agents will lower blood pressure, when managing hypertension in older persons the choice of agent is dependent not only on the ability to lower blood pressure but also on the potential for harm with older persons showing an increased sensitivity to many adverse effects. In general low dose thiazides, calcium channel blockers or agents acting on the renin angiotensin system appear to present the lowest risks for older populations.
3.2 Barriers to the Optimal Management of Hypertension in Older Persons
Despite the wealth of evidence regarding the benefits of managing hypertension in the old and very old, a significant proportion of older individuals with hypertension have suboptimal BP control (Falaschetti et al. 2014). A number of barriers to optimal blood pressure control in older persons have been identified. These barriers can be considered as system, prescriber or patient related (Alhawassi et al. 2015).
System–related barriers affecting blood pressure control in older populations include the variability in treatment recommendations for this population. (Schäfer et al. 2012; Psaty et al. 1995). While a number of clinical trials have been conducted in older populations, the extent to which this evidence has been incorporated into treatment guidelines and translated into practice remains unknown.
While older persons are often excluded from clinical trials for many conditions (Gross et al. 2002; Heiat et al. 2002), multiple large, well-designed trials exploring hypertension in older persons have been conducted (Dahlöf et al. 1991; Bulpitt et al. 2011). A Cochrane review published in 2009 reported 15 studies (n = 24,055 subjects) exploring the management of hypertension in those aged over 60 years (Musini et al. 2009). These findings demonstrated the considerable benefits of actively managing hypertension in older populations, as well as providing evidence regarding appropriate blood pressure (BP) targets and pharmacotherapy for this population.
Physician related barriers include differences in physician attitudes towards the risks and benefits of managing hypertension in older persons as well as differences in interpretation of the evidence. (Trenkwalder et al. 1994; Rodriguez-Roca et al. 2013).
Establishing the evidence is the first step in ensuring optimal care, yet it is well documented that there is a considerable lag in the translation of scientific evidence into current clinical practice. Moreover, incorporating the latest evidence into daily practice is something many physicians often find problematic (Spranger et al. 2004). One strategy aimed at minimizing the evidence-practice gap is the development and implementation of evidence based guidelines. Guidelines have the potential to improve care and improve patient outcomes (Grimshaw and Russell 1993) and multiple international guidelines for the management of hypertension exist.
Management of hypertension in older persons is one area where there appear to be considerable differences between guidelines in terms of the guidance given to clinicians. Differences in interpretation of the evidence, as well as differences in study design and populations all contribute to differences in the guideline recommendations with respect to older populations, despite the strength of the underlying scientific evidence. Differences around who is considered “old” and what BP targets and management are considered appropriate may lead to confusion among clinicians and further contribute to the evidence-practice lag and a recent systematic review of international hypertension guidelines found considerable variation in recommendations regarding the management of hypertension (Alhawassi et al. 2014).
4 Who Is Considered “Older” in International Guidelines?
In the 13 international guidelines for the management of hypertension included in the systematic review, three different age ranges were used to define older populations. Approximately half of the guidelines defined older populations as those aged 80 years or older, while other guidelines defined older populations as those above 65 years and one guideline included individuals aged over 60 years as older. To further add to the discussion, In the American Society of Hypertension/International Society of Hypertension (ASH/ISH) guideline (Weber et al. 2014), recommendations were given for the “middle aged to elderly population” which was defined as 55–80 years. The European Society of Cardiology (ESC) (Mancia et al. 2013a) and National Institute of Clinical excellence (NICE) (Jaques et al. 2013) guidelines referred explicitly to differing needs among older persons and provide recommendations for older populations aged below 80 years and those aged above 80.
5 BP Targets for Older Persons in the International Guidelines
In most international guidelines the same BP targets were used for younger and older populations. (Alhawassi et al. 2014) For the guidelines that did define hypertension, there was consensus that a higher BP reading was more acceptable in older persons with hypertension and that tighter blood pressure control could be considered for older populations. The majority of guidelines that provided specific BP targets for older populations defined a BP of 140/90 mmHg to be consistent with hypertension. The only guideline to provide a different BP target was the ASH/ISH guideline which specifying a slightly higher target BP of 150/90mmHG (Weber et al. 2014).
Despite the plentiful evidence supporting active management of hypertension in older persons, no guidelines specifically dedicated to the management of hypertension in the older populations were identified in the review. Specific information regarding the diagnosis and management of hypertension in older populations was included in all of the international hypertension guidelines included in the review, however there was considerable variation in the depth and scope of the recommendations. Such variation may reflect differences in the populations included in the landmark hypertension in older population studies. The HYVET (Hypertension in the very Elderly) (Bulpitt et al. 2011) recruited participants aged over 80, while the SHEP (Systolic Hypertension in the Elderly) (Perry et al. 1989) recruited those 60 years and over, and the STOP study (Swedish Trial in Old patients with Hypertension) those aged between 70 and 84 years (Dahlöf et al. 1991).
In general, there is consistency across all guidelines regarding recommendations that treatment be commenced in older individuals when systolic BP readings were above 140–150 mmHg and treatment titrated to achieve a target BP at the same level. However, despite the guideline recommendations debate continues regarding the optimal BP targets in older populations. Two Japanese studies, the JATOS (Japanese trial to assess optimal systolic BP in older hypertensive patients) (Group 2008) and VALISH (Valsartan in Elderly Isolated Systolic Hypertension) (Ogihara et al. 2010) studies failed to show an additional benefit in treating older individuals to a target of 140 mmHg systolic compared to a target of 160 mmHg, highlighting the clinical uncertainty in this area.
The major international hypertension treatment guidelines (Weber et al. 2014; Jaques et al. 2013; National Heart Foundation of Australia (National Blood Pressure and Vascular Disease Advisory Committee) 2010; James et al. 2014; Mancia et al. 2013b; Dasgupta et al. 2014; Luehr et al. 2012; Shimamoto et al. 2014) all support the use of pharmacotherapy for the management of hypertension in the elderly reflecting the findings of a 2008 meta-analysis that concluded that the benefits of pharmacotherapy for managing hypertension in older individuals is comparable to that in younger persons (Turnbull et al. 2008).
While most guidelines mentioned that tolerability of pharmacotherapy may be an issue for older persons, only two guidelines in this review discussed specific adverse effects in the elderly such as orthostatic hypotension or falls. Antihypertensive medications have been linked with adverse outcomes in a number of studies (Tinetti et al. 1995; Rejnmark 2013; Sato and Akazawa 2013)
Given global increases in life expectancy, there is a need to re-consider how we define “older” populations as well as a need to ensure they are represented in clinical trials and included in evidence based clinical treatment guidelines.
6 Adverse Reactions and Antihypertensive Medications in the Elderly
One potential age related barrier associated with antihypertensive pharmacotherapy is an increased risk of adverse reactions (Monane et al. 1997). Adverse drug reactions (ADRs) are a significant health care problem, associated with significant morbidity and mortality worldwide. The World Health Organization (WHO) define an ADR as “the response to a drug that is noxious and unintended and occurs at doses normally used in man for the prophylaxis, diagnosis or therapy of disease, or for modification of physiological function”. (National Heart Foundation of Australia (National Blood Pressure and Vascular Disease Advisory Committee) 2010) ADRs have a significant impact on heath, with between 5 and 7 % of all hospitalisations being due to an ADR and with a further 10–20 % of all hospitalized patient experiencing an ADR during their hospital admission (Davies et al. 2007, 2009; Pirmohamed et al. 2004). The burden associated with ADRs is considerable. Up to 6 % of all ADRs are fatal or have serious consequences (Moore et al. 1998; Wester et al. 2008; Lazarou et al. 1998; White et al. 1999).
Older persons have been shown to be at a high risk of ADRs. (Alhawassi et al. 2014) A systematic review estimated that at least one in ten older persons admitted to hospital will experience an ADRs, either leading to hospitalization or during hospitalization (Alhawassi et al. 2014). The very old, those aged over 80 years of age, are at an even higher risk of experiencing an ADR with up to 40 % of older adults medicine users experiencing an ADR.(Edwards and Aronson 2000; Talbot and Waller 2004) The increased risk of ADRs associated with aging is multifactorial. Physiological changes affecting pharmacokinetics and pharmacodynamics as well as increased clinical complexity, multimorbidity and polypharmacy have all been associated with an increased risk of an ADR in the elderly (Alhawassi et al. 2014).
Cardiovascular medicines, including antihypertensive medications have been associated with an increased risk of ADRs in the general adult population (Pirmohamed et al. 2004; Bond and Raehl 2006; Onder et al. 2002; Grossman and Messerli 2006; Stas et al. 2006; Bates et al. 1999; Field et al. 2004; Gribbin et al. 2010; Tinetti et al. 2014; Rende et al. 2013). One study found that over two thirds of adults using antihypertensive therapy has experienced an adverse reaction to their medication (National Heart Foundation of Australia (National Blood Pressure and Vascular Disease Advisory Committee) 2010; Olsen et al. 1999). Side effects associated with antihypertensive agents are well documented in the product information for each medication and it is well known that older persons are more sensitive to a number of antihypertensive side effects, such as hypotension. The Hypertension Detection and Follow-up Program study, although not mainly designed to study ADR, found that about 33 % patients had experienced at least one drug side effect and required antihypertensive medications discontinuation (Curb et al. 1985).
There have been a number of concerns regarding both the role of poorly controlled blood pressure and the use of antihypertensive agents with a number of common conditions in the elderly such as dementia and falls (Dharmarajan and Dharmarajan 2015). The use of centrally acting ACEI has been associated with reduced rates of cognitive decline (Gao et al. 2013). A systematic review of 18 observation studies comprising 1.3 million older individuals reported similar findings, suggesting that the benefits in terms of cognitive function appeared associated with both CCBs and those medicines affecting the renin angiotensin system (Rouch et al. 2015). Given that these findings are based upon observational data it remains uncertain if the observed benefit in terms of cognitive decline is directly due to the use of the individual antihypertensive agents or if it is a benefit of optimising blood pressure control in older individuals.
Falls are a common adverse occurrence that increases in prevalence with age. While multiple factors such as cognitive function, comorbid conditions, functional status and environment may play a role in falls (Dharmarajan and Dharmarajan 2015), antihypertensive medications have long been recognised as contributing factors (Butt et al. 2013; Callisaya et al. 2014; Gribbin et al. 2011; Lee and Goeres 2015). However the evidence around the role of antihypertensive medications in falls is conflicting. A large meta-analysis exploring if any of the commonly used antihypertensive agents (thiazide diuretics, ACEI, ARBs, CCBs and BB) were associated with an increased risk of falls failed to confirm the association. Despite these findings there has been multiple studies demonstrating a dose dependent significant increase in the risk of falls with the use of antihypertensive medications across multiple antihypertensive agents (Butt et al. 2013; Callisaya et al. 2014; Gribbin et al. 2011; Lee and Goeres 2015). Given that all antihypertensive medications may cause hypotension, and that older persons appear to have an increased sensitivity to such effects, balancing the benefits of optimal blood pressure control with minimization and avoidance of adverse effects remains a challenge in clinical practice.
7 Conclusions
Antihypertensive medications are widely used by older persons and have critical role in decreasing hypertension related mortality and morbidity for older persons. However, achieving optimal blood pressure control may be challenging among older populations. Despite considerable high quality evidence regarding the benefits of blood pressure management in older persons, translation of this evidence into treatment recommendations in clinical guidelines remains problematic internationally. Furthermore increased medication related harm and adverse reactions associated with the aging further add to complexity to the optimal management of hypertension in older populations.
References
Alhawassi TM, Krass I, Bajorek BV, Pont LG (2014) A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clin Interv Aging 9:2079–2086
Alhawassi TM, Krass I, Pont LG (2015) Prevalence, prescribing and barriers to effective management of hypertension in older populations: a narrative review. J Pharm Policy Pract 8:24
Barker WH, Mullooly JP, Linton KL (1998) Trends in hypertension prevalence, treatment, and control in a well-defined older population. Hypertension 31(1):552–559
Barreto SM, Passos VMA, Firmo JOA, Guerra HL, Vidigal PG, Lima-Costa MFF (2001) Hypertension and clustering of cardiovascular risk factors in a community in Southeast Brazil: the Bambuí Health and Ageing Study. Arq Bras Cardiol 77(6):576–581
Bates DW, Miller EB, Cullen DJ, Burdick L, Williams L, Laird N et al (1999) Patient risk factors for adverse drug events in hospitalized patients. Arch Intern Med 159(21):2553–2560
Beaglehole R, Ebrahim S, Reddy S, Voûte J, Leeder S (2008) Prevention of chronic diseases: a call to action. Lancet 370(9605):2152–2157
Beckett N, Peters R, Tuomilehto J, Swift C, Sever P, Potter J et al (2012) Immediate and late benefits of treating very elderly people with hypertension: results from active treatment extension to Hypertension in the Very Elderly randomised controlled trial. BMJ 344
Bond C, Raehl CL (2006) Adverse drug reactions in United States hospitals. Pharmacotherapy 26(5):601–608
Bromfield SG, Bowling CB, Tanner RM, Peralta CA, Odden MC, Oparil S et al (2014) Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and Older, 1988–2010. J Clin Hypertens 16(4):270–276
Bulpitt C, Beckett N, Peters R, Leonetti G, Gergova V, Fagard R et al (2011) Blood pressure control in the Hypertension in the Very Elderly Trial (HYVET). J Hum Hypertens 26(3):157–163
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH (2013) The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int 24(10):2649–2657
Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK (2014) Greater daily defined dose of antihypertensive medication increases the risk of falls in older people--a population-based study. J Am Geriatr Soc 62(8):1527–1533
Carretero OA, Oparil S (2000) Essential hypertension part I: definition and etiology. Circulation 101(3):329–335
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al (2003) The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289(19):2560–2571
Curb JD, Borhani NO, Blaszkowski TP, Zimbaldi N, Fotiu S, Williams W (1985) Long-term surveillance for adverse effects of antihypertensive drugs. JAMA 253(22):3263–3268
Daar AS, Singer PA, Persad DL, Pramming SK, Matthews DR, Beaglehole R et al (2007) Grand challenges in chronic non-communicable diseases. Nature 450(7169):494–496
Dahlöf BHL, Lindholm L, Schersten B, Ekbom T, Wester P (1991) Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP-Hypertension). Lancet 338(8778):1281–1285
Dasgupta K, Quinn RR, Zarnke KB, Rabi DM, Ravani P, Daskalopoulou SS et al (2014) The 2014 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Canadian J Cardiol 30(5):485–501
Davies EC, Green CF, Mottram DR, Pirmohamed M (2007) Adverse drug reactions in hospitals: a narrative review. Curr Drug Saf 2(1):79–87
Davies EC, Green CF, Taylor S, Williamson PR, Mottram DR, Pirmohamed M (2009) Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS One 4(2):e4439
Department of Economic and Social Affairs United Nations (2002) World population ageing: 1950–2050. UN
Devlin G (2010) Women and elderly: subgroups under-represented in clinical trials. Curr Opin Cardiol 25(4):335–339
Dharmarajan TS, Dharmarajan L (2015) Tolerability of antihypertensive medications in older adults. Drugs Aging 32(10):773–796
Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356(9237):1255–1259
Fagard RH (2002) Epidemiology of hypertension in the elderly. Am J Geriatr Cardiol 11(1):23–28
Falaschetti E, Mindell J, Knott C, Poulter N (2014) Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet 383(9932):1912–1919
Field TS, Gurwitz JH, Harrold LR, Rothschild J, DeBellis KR, Seger AC et al (2004) Risk factors for adverse drug events among older adults in the ambulatory setting. J Am Geriatr Soc 52(8):1349–1354
Fliser D, Ritz E (1998) Relationship between hypertension and renal function and its therapeutic implications in the elderly. Gerontology 44(3):123–131
Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB et al (1997) Hemodynamic patterns of age-related changes in blood pressure The Framingham Heart Study. Circulation 96(1):308–315
Franklin SS, Jacobs MJ, Wong ND, Gilbert J, Lapuerta P (2001) Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension 37(3):869–874
Gambassi G, Lapane K, Sgadari A, Landi F, Carbonin P, Hume A et al (1998) Prevalence, clinical correlates, and treatment of hypertension in elderly nursing home residents. Arch Intern Med 158(21):2377–2385
Gambert SR (1994) Who are the “elderly”? Geriatr Nephrol Urol 4(1):3–4
Gao Y, O’Caoimh R, Healy L, Kerins DM, Eustace J, Guyatt G et al (2013) Effects of centrally acting ACE inhibitors on the rate of cognitive decline in dementia. BMJ Open 3(7)
Gheorghiade M, Böhm M, Greene SJ, Fonarow GC, Lewis EF, Zannad F et al (2013) Effect of aliskiren on postdischarge mortality and heart failure readmissions among patients hospitalized for heart failure: the ASTRONAUT randomized trial. JAMA 309(11):1125–1135
Gribbin J, Hubbard R, Gladman JR, Smith C, Lewis S (2010) Risk of falls associated with antihypertensive medication: population-based case–control study. Age Ageing:afq092
Gribbin J, Hubbard R, Gladman J, Smith C, Lewis S (2011) Risk of falls associated with antihypertensive medication: self-controlled case series. Pharmacoepidemiol Drug Saf 20(8):879–884
Grimshaw JM, Russell IT (1993) Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 342(8883):1317–1322
Gross CP, Mallory R, Heiat A, Krumholz HM (2002) Reporting the recruitment process in clinical trials: who are these patients and how did they get there? Ann Intern Med 137(1):10–16
Grossman E, Messerli FH (2006) Long-term safety of antihypertensive therapy. Prog Cardiovasc Dis 49(1):16–25
Group JS (2008) Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res 31(12):2115–2127
Hajjar I, Kotchen TA (2003) Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 290(2):199–206
Halter JB (2009) Hazzard’s geriatric medicine and gerontology. McGraw-Hill Companies
Hansson LLL, Ekbom T, Dahlöf B, Lanke J, Scherstén B et al (1999) Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet 354(9192):1751–1756
Heiat A, Gross CP, Krumholz HM (2002) Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med 162(15):1682–1688
Huebschmann AD, Bublitz C, Anderson RJ (2006) Are hypertensive elderly patients treated differently? Clin Interven Aging 1(3):289
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J et al (2014) 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311(5):507–520
Jaques H, National Institute for H, Clinical E (2013) NICE guideline on hypertension. Eur Heart J 34(6):406–408
Kannel WB, Gordan T (1978) Evaluation of cardiovascular risk in the elderly: the Framingham study. Bull N Y Acad Med 54(6):573–591
Kirkwood TB, Austad SN (2000) Why do we age? Nature 408(6809):233–238
Kleman M, Dhanyamraju S, DiFilippo W (2013) Prevalence and characteristics of pseudohypertension in patients with “resistant hypertension”. J Am Soc Hypertens 7(6):467–470
Kumar J (2013) Epidemiology of hypertension. Clinical Queries. Nephrology 2(2):56–61
Larochelle P, Tobe SW, Lacourcière Y (2014) β-blockers in hypertension: studies and meta-analyses over the years. Can J Cardiol 30(5):S16–S22
Lazarou J, Pomeranz BH, Corey PN (1998) Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 279(15):1200–1205
Lee DS, Goeres LM (2015) Higher antihypertensive dose increases risk of falls in older people. Evid Based Nurs 18(3):96
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al (2013) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2224–2260
Lloyd-Jones DM, Evans JC, Levy D (2005) Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA 294(4):466–472
Luehr DWT, Burke R, Dohmen F, Hayes R, Johnson M, Kerandi H, Margolis K, Marshall M, O’Connor P, Pereira C, Reddy G, Schlichte A, Schoenleber M (2012) Hypertension diagnosis and treatment. Institute for Clinical Systems Improvement [Internet]. Updated November 2012. Available from: http://bit.ly/Hypertension1112
Mackey RH, Sutton-Tyrrell K, Vaitkevicius PV, Sakkinen PA, Lyles MF, Spurgeon HA et al (2002) Correlates of aortic stiffness in elderly individuals: a subgroup of the Cardiovascular Health Study. Am J Hypertens 15(1):16–23
Maclure M, Dormuth C, Naumann T, McCormack J, Rangno R, Whiteside C et al (1998) Influences of educational interventions and adverse news about calcium-channel blockers on first-line prescribing of antihypertensive drugs to elderly people in British Columbia. Lancet 352(9132):943–948
MacMahon SW, Blacket RB, Macdonald GJ, Hall W (1984) Obesity, alcohol consumption and blood pressure in Australian men and women the National Heart Foundation of Australia Risk Factor Prevalence Study. J Hypertens 2(1):85–91
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M et al (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219
Mann SJ (1992) Systolic hypertension in the elderly: pathophysiology and management. Arch Intern Med 152(10):1977–1984
Masoro EJ, Austad SN (2006) Handbook of the biology of aging. Academic press
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(11):e442
Menotti A, Lanti M, Kafatos A, Nissinen A, Dontas A, Nedeljkovic S et al (2004) The role of a baseline casual blood pressure measurement and of blood pressure changes in middle age in prediction of cardiovascular and all-cause mortality occurring late in life: a cross-cultural comparison among the European cohorts of the Seven Countries Study. J Hypertens 22(9):1683–1690
Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA et al (2004) Changes in arterial stiffness and wave reflection with advancing age in healthy men and women the Framingham Heart Study. Hypertension 43(6):1239–1245
Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J (1997) The effects of initial drug choice and comorbidity on antihypertensive therapy compliance* results from a population-based study in the elderly. Am J Hypertens 10(7):697–704
Moore N, Lecointre D, Noblet C, Mabille M (1998) Frequency and cost of serious adverse drug reactions in a department of general medicine. Br J Clin Pharmacol 45(3):301–308
Moser M (1998) Why are physicians not prescribing diuretics more frequently in the management of hypertension? JAMA 279(22):1813–1816
Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 349(9064):1498–1504
Musini VM, Tejani AM, Bassett K, Wright JM (2009) Pharmacotherapy for hypertension in the elderly. Cochrane Database Syst Rev 2009(4):CD000028
National Heart Foundation of Australia (National Blood Pressure and Vascular Disease Advisory Committee) (2010) Guide to management of hypertension 2008. Updated December 2010. Accessed via https://heartfoundation.org.au/images/uploads/publications/HypertensionGuidelines2008to2010Update.pdf on April 15, 2016
Officers A, Coordinators for the ACRGTA, Lipid-Lowering Treatment to Prevent Heart Attack T (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288(23):2981–2997
Ogihara T, Saruta T, Rakugi H, Matsuoka H, Shimamoto K, Shimada K et al (2010) Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension 56(2):196–202
Olsen H, Klemetsrud T, Stokke HP, Tretli S, Westheim A (1999) Adverse drug reactions in current antihypertensive therapy: a general practice survey of 2586 patients in Norway. Blood Press 8(2):94–101
Onder G, Gambassi G, Landi F, Pedone C, Cesari M, Carbonin P et al (2001) Trends in antihypertensive drugs in the elderly: the decline of thiazides. J Hum Hypertens 15(5):291–297
Onder G, Pedone C, Landi F, Cesari M, Della Vedova C, Bernabei R et al (2002) Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc 50(12):1962–1968
Pahor M, Carbonin P, Guralnik J, Havlik R, Furberg C (1996a) Risk of gastrointestinal haemorrhage with calcium antagonists in hypertensive persons over 67 years old. Lancet 347(9008):1061–1065
Pahor M, Guralnik JM, Ferrucci L, Corti M-C, Salive ME, Cerhan JR et al (1996b) Calcium-channel blockade and incidence of cancer in aged populations. Lancet 348(9026):493–497
Parving H-H, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD et al (2012) Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med 367(23):2204–2213
Perry HM Jr, Smith WM, McDonald RH, Black D, Cutler JA, Furberg CD et al (1989) Morbidity and mortality in the Systolic Hypertension in the Elderly Program (SHEP) pilot study. Stroke 20(1):4–13
Pimenta E, Oparil S (2012) Management of hypertension in the elderly. Nat Rev Cardiol 9(5):286–296
Pinto E (2007) Blood pressure and ageing. Postgrad Med J 83(976):109–114
Pirmohamed M, James S, Meakin S, Green C, Scott AK, Walley TJ et al (2004) Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ 329(7456):15–19
Prencipe M, Casini A, Santini M, Ferretti C, Scaldaferri N, Culasso F (2000) Prevalence, awareness, treatment and control of hypertension in the elderly: results from a population survey. J Hum Hypertens 14(12):825–830
Primatesta P, Poulter NR (2004) Hypertension management and control among English adults aged 65 years and older in 2000 and 2001. J Hypertens 22(6):1093–1098
Prince MJ, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y et al (2012) Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens 30(1):177–187
Psaty BM, Koepsell TD, Yanez ND, Smith NL, Manolio TA, Heckbert SR et al (1995) Temporal patterns of antihypertensive medication use among older adults, 1989 through 1992: an effect of the major clinical trials on clinical practice? JAMA 273(18):1436–1438
Psaty BM, Manolio TA, Smith NL, Heckbert SR, Gottdiener JS, Burke GL et al (2002) Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med 162(20):2325–2332
Rai GS, Mulley GP (2007) Elderly medicine: a training guide. Elsevier Health Sciences
Rejnmark L (2013) The ageing endocrine system: fracture risk after initiation of antihypertensive therapy. Nat Rev Endocrinol 9(4):189–190
Rende P, Paletta L, Gallelli G, Raffaele G, Natale V, Brissa N et al (2013) Retrospective evaluation of adverse drug reactions induced by antihypertensive treatment. J Pharmacol Pharmacotherap 4(Suppl1):S47
Rodriguez-Roca GC, Llisterri JL, Prieto-Diaz MA, Alonso-Moreno FJ, Escobar-Cervantes C, Pallares-Carratala V et al (2013) Blood pressure control and management of very elderly patients with hypertension in primary care settings in Spain. Hypertens Res 37(2):166–171
Rouch L, Cestac P, Hanon O, Cool C, Helmer C, Bouhanick B et al (2015) Antihypertensive drugs, prevention of cognitive decline and dementia: a systematic review of observational studies, randomized controlled trials and meta-analyses, with discussion of potential mechanisms. CNS Drugs 29(2):113–130
Sato I, Akazawa M (2013) Polypharmacy and adverse drug reactions in Japanese elderly taking antihypertensives: a retrospective database study. Drug Healthcare Patient Saf 5:143–150
Schäfer H-H, De Villiers JN, Sudano I, Dischinger S, Theus G-R, Zilla P et al (2012) Recommendations for the treatment of hypertension in the elderly and very elderly–a scotoma within international guidelines. Swiss Med Wkly Epub
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M et al (2014) The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 37(4):253–387
Spranger CB, Ries AJ, Berge CA, Radford NB, Victor RG (2004) Identifying gaps between guidelines and clinical practice in the evaluation and treatment of patients with hypertension. Am J Med 117(1):14–18
Stas S, Appesh L, Sowers J (2006) Metabolic safety of antihypertensive drugs: myth versus reality. Current Hypertens Rep 8(5):403–408
Svetkey LP, George LK, Tyroler HA, Timmons PZ, Burchett BM, Blazer DG (1996) Effects of gender and ethnic group on blood pressure control in the elderly. Am J Hypertens 9(6):529–535
Talbot J, Waller P (2004) Stephens’ detection of new adverse drug reactions. Wiley, New York
The World Health Organisation (2016) Projections of mortality and causes of death, 2015 and 2030. Accessed via http://www.who.int/healthinfo/global_burden_disease/projections/en/on 15 April 2016
Tinetti ME, Inouye SK, Gill TM, Doucette JT (1995) Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA 273(17):1348–1353
Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP et al (2014) Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med 174(4):588–595
Trenkwalder P, Ruland D, Stender M, Gebhard J, Trenkwalder C, Lydtin H et al (1994) Prevalence, awareness, treatment and control of hypertension in a population over the age of 65 years: results from the Starnberg Study on Epidemiology of Parkinsonism and Hypertension in the Elderly (STEPHY). J Hypertens 12(6):709
Triantafyllou A, Douma S, Petidis K, Doumas M, Panagopoulou E, Pyrpasopoulou A et al (2010) Prevalence, awareness, treatment and control of hypertension in an elderly population in Greece. Rural Remote Health 10(2):1225
Tu K, Campbell NR, Chen Z, McAlister FA (2006) Thiazide diuretics for hypertension: prescribing practices and predictors of use in 194,761 elderly patients with hypertension. Am J Geriatr Pharmacother 4(2):161–167
Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F et al (2008) Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ 336(7653):1121–1123
Van Kraaij D, Jansen R, Gribnau F, Hoefnagels W (1998) Loop diuretics in patients aged 75 years or older: general practitioners’ assessment of indications and possibilities for withdrawal. Eur J Clin Pharmacol 54(4):323–327
Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D’Agostino RB et al (2002) Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA 287(8):1003–1010
Wallace SM, McEniery CM, Mäki-Petäjä KM, Booth AD, Cockcroft JR, Wilkinson IB (2007) Isolated systolic hypertension is characterized by increased aortic stiffness and endothelial dysfunction. Hypertension 50(1):228–233
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG et al (2014) Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens 32(1):3–15
Weinberger MH (1996) Salt sensitivity of blood pressure in humans. Hypertension 27(3):481–490
Wester K, Jonsson AK, Spigset O, Druid H, Hagg S (2008) Incidence of fatal adverse drug reactions: a population based study. Br J Clin Pharmacol 65(4):573–579
White SM (2010) Including the very elderly in clinical trials. Anaesthesia 65(8):778–780
White TJ, Arakelian A, Rho JP (1999) Counting the costs of drug-related adverse events. Pharmacoeconomics 15(5):445–458
Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL et al (2003) A comparison of outcomes with angiotensin-converting--enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 348(7):583–592
Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC et al (2008) Emergence of chronic non-communicable diseases in China. Lancet 372(9650):1697–1705
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing AG
About this chapter
Cite this chapter
Pont, L., Alhawassi, T. (2016). Challenges in the Management of Hypertension in Older Populations. In: Islam, M.S. (eds) Hypertension: from basic research to clinical practice. Advances in Experimental Medicine and Biology(), vol 956. Springer, Cham. https://doi.org/10.1007/5584_2016_149
Download citation
DOI: https://doi.org/10.1007/5584_2016_149
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-44250-1
Online ISBN: 978-3-319-44251-8
eBook Packages: MedicineMedicine (R0)