Abstract
Diagnosis of intestinal disease related to vascular disorders could represent a critical diagnostic challenge for the emergency radiologist. Terms such as “ischemia” and “infarction” of the intestine are often used erroneously as synonyms: however, whereas the ischemia could be a totally reversible event, the infarction corresponds to a tissue death with no chance for the tissue to heal. Both terms indicate as different degrees or stages of disease an injury caused by interruption of the blood supply to the intestinal tissue. It is possible to distinguish three main different conditions underlying an intestinal ischemic event: arterial blood supply deficiency mainly related to embolism or thrombosis; impaired venous drainage; decreased mesenteric blood flow or low-flow state. Acute mesenteric ischemia can be considered a real, true emergency because of the associated significant mortality rate, which can be extremely high. A prompt diagnosis of any intestinal ischemic disorder of the intestine is imperative. However, because most patients affected by bowel ischemia can present with nonspecific signs and symptoms, it could be difficult to diagnose intestinal ischemia or infarction. Diagnostic imaging and especially multidetector computed tomography (MDCT) could be of great help in the management of patients with acute abdomen related to suspected acute mesenteric ischemia. Knowledge of the pathophysiology of the intestine is essential in order to recognize findings related to pathologic changes of the intestine affected by vascular disorders in different stages of disease from different causes. In this chapter, MDCT findings of disorders from impaired venous drainage and from arterial blood flow insufficiency involving the small and the large intestine will be considered, considering also criteria for differential diagnosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Epidemiology
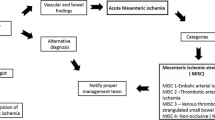
In patients with acute abdominal syndrome, diagnosis of intestinal disease related to vascular disorders could represent a critical diagnostic challenge for the emergency radiologist. Terms such as “ischemia” and “infarction” of the intestine are often used erroneously as synonyms; however, whereas the ischemia could be a totally reversible event, the infarction corresponds to a tissue death with no chance for the tissue to heal. Both terms indicate as different degrees or stages of disease an injury caused by interruption of the blood supply to the intestinal tissue (Fenoglio-Preiser et al. 2008). It is possible to distinguish three main different conditions underlying an intestinal ischemic event (Paterno and Longo 2008; Klatte et al. 1982): arterial blood supply deficiency mainly related to embolism or thrombosis (splanchnic); impaired venous drainage (postsplanchnic); decreased mesenteric blood flow or low-flow state (i.e., cardiac failure, myocardial infarction, bleeding, and hypovolemia) (presplanchnic). Acute mesenteric ischemia can be considered a real, true emergency because of the associated significant mortality rate, which can range between 30 and 90% (Paterno and Longo 2008; Herbert and Steele 2007; Martinez and Hogan 2004). The incidence of this pathologic entity was estimated in a large study based on either autopsies or operations as 12.9 per 100,000 persons per year, increasing with age and equally distributed among males and females (Acosta 2010). The same study reported the incidence of superior mesenteric artery occlusion, nonocclusive mesenteric ischemia, and mesenteric vein thrombosis as 68, 16, and 16%, respectively. It is obvious that a prompt diagnosis of any intestinal ischemic disorder of the intestine is imperative. However, because most patients affected by bowel ischemia can present with nonspecific signs and symptoms, especially those who have other pressing clinical issues, it could be difficult to recognize ischemia or infarction of the bowel (Gore et al. 2008). Clinical questions in patients with acute abdomen from intestinal ischemia are different in most cases. Often other diseases (appendicitis, diverticulitis, bowel obstruction, peptic ulcer disease, gastroenteritis, infectious ileocolitis, inflammatory bowel disease, pancreatitis, cholecystitis, and rupture of an aortic aneurysm) enter the clinician’s mind as the most likely diagnosis, with ischemia placed at the bottom of the differential diagnosis (Gore et al. 2008). Diagnostic imaging and especially multidetector computed tomography (CT) could be of great help in the management of patients with acute abdomen related to suspected acute mesenteric ischemia; however, in order to acquire important information for an efficient radiologic diagnosis, knowledge of the pathophysiology of the intestine is essential.
2 Physiopathology
In the acute ischemic disease of the intestine, multiple factors and processes contribute to develop bowel wall damage: cellular dysfunction, edema, and death caused by the interruption of a normal blood supply to the intestinal tissue; subsequent anoxia leads to lactic acidosis and anaerobic metabolism (Fenoglio-Preiser et al. 2008). It has been reported that to cause a tissue injury, the overall hematic supply to the small intestine has to be reduced by more than 50% (Fenoglio-Preiser et al. 2008; Bulkley et al.1985). The first sign of damage from ischemia is represented by increased capillary permeability, followed by epithelial cell injury if the ischemic event continues and persists (Fenoglio-Preiser et al. 2008). Mucosal damage then proceeds with coagulative necrosis development (Fenoglio-Preiser et al. 2008). If after an ischemic event reperfusion occurs, a reverse process could allow regeneration of the cells and washout of the toxic metabolites (Fenoglio-Preiser et al. 2008). The correlated acute inflammation status of the reperfused intestine is due to the production of reactive molecules caused by activation of the inflammatory cells (Fenoglio-Preiser et al. 2008). The reperfusion process with oxygen into anoxic tissue causes oxygen free radical cascades that secondarily increase mucosal and vascular permeability, with consequent potential mucosal damage that could also lead to bacterial sepsis (Fenoglio-Preiser et al. 2008). The microvascular injury from ischemia can result in a mucosal influx of neutrophil cells that also represents a source of reactive oxygen metabolites (Fenoglio-Preiser et al. 2008).
The small intestinal vasculature can respond to reduction of blood flow and of the oxygen content: occlusive arterial disease or significant reduction of inhaled oxygen causes a prompt but transient increase in spike potentials and contractions (Fondacaro 1984; Gilsdorf et al. 1983; Granger and Barrowman 1983; Kvietys et al. 1980; Wheaton et al. 1981). Quiescence of the musculature usually follows this intestinal hypermotility; segmental ischemia can cause alterations in motility of the entire small intestine through a reflex activity (Fondacaro 1984). In animal experimental data, it has been found that moderate ischemia can cause increased gastric emptying and decreased intestinal transit, however, 1 day later an active inflammation can occur at the ischemic site, with marked reduced motility of the entire intestine (Fondacaro 1984; Nylander and Wikstrom 1968). On the other hand, high-grade ischemia seems to stop the gastric emptying activity, with slowing of wave propagation in the visceral muscle (Fondacaro 1984). Restoration of a normal motor activity of the intestine after an ischemic event and reperfusion seems to be correlated with the temporal extent of the ischemia itself (Fondacaro 1984): the intestinal musculature seems to be less sensitive than the mucosa to ischemia, but if the ischemia is prolonged and severe, relevant damage to motility could occur (Fondacaro 1984).
In the large bowel, there is a complex network of intramural and extramural plexus of vascular supply from the superior and the inferior mesenteric arteries that can play an important role acting as collateral perfusion in the case of occlusion of an arterial major branch (Kvietys and Granger 1984). A lesser amount of epithelial desquamation and mild dilatation of blood vessels in the mucosa during the ischemic event represent damage to the colonic wall; after reperfusion, desquamation of the epithelium, cell necrosis, edema, and vascular dilatation can be observed (Kvietys and Granger 1984).
3 Clinical Findings
Abdominal pain represents the “core” symptoms underlying the acute disease caused by vascular disorder of the intestine. However, in the early phase of the disease severe pain could have no proportionate relationship to the physical signs, being due to an intense muscular spasm representing the immediate consequence of a decreased blood supply (Perko et al. 2002). Sudden symptoms of acute abdomen from mesenteric ischemia in patients apparently in good health is more frequently observed if the vascular disorder is related to embolism; in nonocclusive low-flow-state ischemia or in the case of mesenteric venous thrombosis, a gradual onset of symptoms with a more prolonged clinical course can be observed (Bartone et al. 2008). Typically, the mesenteric arterial embolism can clinically present different signs such as sudden abdominal pain, nausea, vomiting, hematochezia or melena, hypotension, peritonitis, whereas in the case of mesenteric arterial thrombosis it is usually evidenced as an insidious onset with progression of constant abdominal pain (Bartone et al. 2008). Nonocclusive ischemia can be correlated with acute or subacute symptoms, with abdominal tenderness and distension, muscular defense, hypotension, fever, decreased bowel sounds, nausea, and anorexia (Bartone et al. 2008). Patients with vascular disorders of the intestine related to impaired venous drainage from mesenteric vein thrombosis complain of a diffuse or localized long-standing abdominal pain associated with anorexia and diarrhea, or sometimes also fever and abdominal distension (Bartone et al. 2008). Patients with ischemic disease of the colon often present with left lower abdominal quadrant pain, with the descending colon being more commonly involved; a sudden, crampy abdominal pain is usually mentioned by the patient, accompanied by urgency to defecate; mild bleeding is common; abdominal distension, anorexia, nausea, and vomiting could also be present (Taourel et al. 2008). No specific laboratory parameter or biochemical or hematological combined marker seems to present sufficient sensitivity and specificity to allow diagnosis of acute mesenteric ischemia (Perko et al. 2002). The main laboratory findings correlated with mesenteric ischemia are hemoconcentration, acidosis with high anion gap, and alterations in the leukocyte count and lactate concentration (Bartone et al. 2008; Oldenburg et al. 2004). A diagnostic triad of acidosis, leukocytosis, and hyperphosphatemia has been reported as a useful tool in the clinical setting of a patient with acute mesenteric ischemia (Jamieson et al. 1982). Earlier, altered nonspecific laboratory parameters are high levels of serum amylase, aspartate aminotransferase, lactate dehydrogenate, and creatine phosphokinase; hyperphosphatemia and hyperkalemia are usually present at the late stage of ischemia, often associated with intestinal infarction and wall necrosis (Bartone et al. 2008; Oldenburg et al. 2004).
4 CT Findings
4.1 Small Intestine Vascular Disease from Arterial Supply Deficiency
The added value of the CT examination in a patient with acute abdomen related to mesenteric ischemia has been well established. This imaging method allows an efficient evaluation of the mesenteric vasculature as well as of the intestinal wall and other abdominal hollow and solid structures and related findings. The main problem in the imaging of the patient suspected of having an “intestinal ischemia” is related, on one hand, to “what” the CT findings are able to offer to us in term of diagnostic “specificity” and “sensitivity”. On the other hand, problems in interpretation of the imaging findings are due in most cases to the lack of knowledge of the ischemic disease progression and pathologic changes of the intestinal wall with respect to the timing of the disease itself. Common mistakes could also be represented by the confusion between ischemia (potentially reversible injury) and infarction (not-reversible injury with death of the intestinal segment involved) and errors in reporting the salient imaging findings that could help surgeons and clinicians in the management of the patient with acute disease. To support this process, it is imperative to be able to evaluate the endoluminal opacification and caliber of the superior mesenteric arterial district, to diagnose the ischemic disease when at early stage, to make a correct diagnosis of damage from reperfusion, to suggest a correct follow-up in terms of diagnostic imaging or interventional procedures, and to note the intestinal infarction signs, giving a comprehensive evaluation of the extent of damage. At the basis of interpreting the CT images of acute disease of the small intestine due to arterial supply deficiency is the knowledge of the early morphologic changes of the intestine due to the acute injury. It is important to note that the intestine is an “alive” structure able to react to injury, firstly with a neurogenic response by the spastic reflex ileus, in which the intestinal loops are collapsed with no endoluminal content, followed by the hypotonic state, in which the loops are distended by air (Romano et al. 2008). In these stages, the superior mesenteric artery can show defects in the endoluminal opacification by thrombosis or embolism or have a caliber reduction from low-flow nonocclusive disease. Parietal enhancement of the small bowel could be normal or in some cases it can appear higher and brighter than usual (Fig. 1). In the following stage, characterized by predominantly air distension of the small intestine, the wall could appear thinner than normal and an accurate evaluation of the parietal enhancement is mandatory. From this stage, in the absence of reperfusion, intestinal ischemia can progress to infarction (Fig. 2). When on CT examination in a patient with acute abdomen the presence of air-dilated small bowel loops is evident, occlusion of the superior mesenteric artery or a diminished caliber of the opacified vessel, in patients with suggestive clinical history for mesenteric vascular disorders, could be suggestive of intestinal ischemia. However, in the absence of vessel abnormalities and nonspecific clinical data, an alternative diagnostic hypothesis should be considered, with reflex spastic ileus and hypotonic ileus findings being nonspecific for intestinal ischemia but common as early reactions of different intestinal injuries (Romano et al. 2008). When the appearance of the small intestine is altered and the clinical symptoms are suggestive of intestinal ischemia in the absence of endoluminal vascular defects of opacification, low-flow-state conditions could be strongly considered (Romano et al. 2008). After an ischemic injury to the small intestine, when reperfusion occurs, blood plasma, contrast medium, or erythrocytes may extravasate through the disrupted vascular wall and mucosa, causing wall thickening and fluid filling of the lumen (Chou et al. 2004). CT findings in this stage of vascular disease of the small intestine could give us important information regarding the mesenteric arterial vasculature as well as the small bowel wall appearance, especially the presence of submucosa edema and possible moderate hyperdensity of the mucosa (Romano et al. 2008). In this stage it is important to differentiate between normal enhancement of the bowel wall and abnormal hyperdensity from mural hemorrhage. In fact, imaging findings on CT examination could be correlated with the histopathologic changes that occur in the intestine after an ischemic event, from the damage to the epithelium to inflammation, edema, and hemorrhage into the submucosa from reperfusion injuries (Romano et al. 2006) (Figs. 3, 4, 5, 6). At the same time, evidence from the CT findings of the late stage of intestinal vascular disease (intestinal infarction) with death, necrosis of the involved bowel, is correlated with the evidence of absent enhancement of the intestinal wall and the presence of pneumatosis (parietal, mesenteric, and portal) and free peritoneal air if perforation of the bowel has occurred (Romano et al. 2008). In this stage, attention to the endoluminal opacification of the mesenteric vessels could not be primary than a correct interpretation of the signs of intestinal necrosis (Romano et al. 2008).
Endoluminal defect of opacification from a thrombus in the superior mesenteric artery at the origin is appreciable on CT sagittal (a) and 3D (b) reconstructions. Signs of a spastic reflex ileus are evident, with normal enhanced and collapsed small bowel loops: this finding could represent the very early stage of ischemia, which requires accurate monitoring (c)
Extensive defects of endoluminal opacification from thrombosis were found in the inferior mesenteric artery and its aberrant branches that supply the distal ileum (arrow in a). Consequentely, small intestine ileal segmental infarction can be noted, with loops distended by gas and fluid, with thin nonenhanced wall with little air bubbles either in the wall (b) or in small venous mesenteric vessels (c); the colon shows extensive signs of infarction, with absence of enhancement of the wall, which appears not thickened, with evidence also of some little air bubbles from parietal pneumatosis (c, d). The intestinal wall feature could be related to the absence of reperfusion after ischemia, the fluid filling the lumen attesting also to a subsequent stasis to the intestinal transit
In a patient affected by cardiopathy, the acute abdominal pain occurred suddenly after an atrial fibrillation episode. Nonsignificant reduction of the caliber of the superior mesenteric artery and secondary branches could be observed, neither an endoluminal defect of opacification from embolism; however, some of the intestinal loop had parietal hyperemia from ischemic injury. The patient recovered without the need for surgical intervention
This case of a small endoluminal defect of opacification in the secondary branches of the superior mesenteric artery shows different stages of ischemic disease affecting the small intestine, with some segments characterized by parietal hyperdensity from an intermediate degree of ischemia, whereas others are in the late stage, infarcted, with no enhancement of the wall, which appears thin with fluid filling the lumen (a). The loops with infarction did not show signs of damage from reperfusion. The superior mesenteric artery at the origin was well opacified (b)
The extensive defect of endoluminal opacification of the superior mesenteric artery (a) caused ischemic damage to the intestine with evidence of most small bowel loops as well as the ascending colon showing submucosa edema as a sign of reperfusion (b), whereas other small intestinal segments show hyperdensity from transmural hemorrhagic phenomena (c)
Thrombosis of superior mesenteric artery branches (a) caused ischemic injury of the small intestine; ischemic area of the right kidney and spleen could also be noted (b). Reperfusion damage in the phase of healing could be observed with weak thickening and hypodensity of some intestinal segments, whereas others appear completely normal in features and wall enhancement (c, d)
4.2 Small Intestine Vascular Disease from Impaired Venous Drainage
Vascular disorders of the intestine due to mesenteric venous thrombosis in the acute forms differ from the acute conditions in terms of arterial origin, presenting a slow evolution on the order of days or weeks before an increased and persistent abdominal pain occurs (Laureano and Wade 1998). Frequently observed in patients with hepatopathy, cirrhosis, and/or portal hypertension (Fig. 7), thrombosis of the superior mesenteric vein can be also primary; however, other conditions such as polycytemia, systemic diseases, high level of plasmatic platelets, and an estrogen–progesterone therapy may all represent potential risk factors for mesenteric thrombosis (Jost and Gloviczki 2002; Kitchens 1992; Romano et al. 2006). CT examination to observe imaging findings of intestinal disorders related to mesenteric thrombosis is not rare (i.e., patients affected by chronic liver disease): difficulties can occur in discriminating between intestinal segments affected by injury from impaired venous drainage of medium–high stage and in diagnosing an intestinal infarction from venous origin. CT findings of vascular disorder due to impaired venous drainage from venous occlusions are related to the pathologic changes in the bowel wall, ranging from congestion and swelling of the bowel wall with edema to hemorrhage, with fluid flowing out from the bowel and the mesentery into the peritoneal cavity, as observed in animal experimental models (Friedberg 1965; Noer 1943; Polk 1966; Laureano and Wade 1998). Whereas in these models progression to infarction with bowel necrosis occurred in a few hours, in human clinical observations the entire process is longer, owing to the differences in collateral circulation (Laureano and Wade 1998). In radiologic clinical practice, on diagnostic imaging visualization of findings related to an early stage of intestinal disease from impaired venous drainage may be rare: although if the initial reaction of the small intestine to a superior mesenteric vein occlusion could be done by spasticity of the loops, due to the underlying slow pathophysiologic process related to thrombosis, a following progression of the disease with air distension of the involved intestine could be masked by intramural and mesenteric edema (Romano et al. 2006). In terms of CT findings, in a patient with acute abdomen and evidence of mesenteric venous thrombosis, the evidence of spastic intestine with a collapsed lumen or distended by air could be considered as an early stage of vascular disease of the bowel. However, in most cases it is common to find imaging signs of more advanced disease (Romano et al. 2008). With progression of mesenteric venous occlusion, the intravascular volume and the hydrostatic pressure increase and the arterial blood flows into capillaries and venules of the bowel and the mesentery, causing extravasation of plasma, red blood cells, and contrast material in the fenestrations of the arteriocapillary endothelium into the submucosa (Chou 2002, 2004). CT findings at this stage of disease are the evidence of mesenteric venous thrombosis, small bowel thickening, higher enhancement from intramural hemorrhage, and evidence of submucosa edema, with alternation of layers of different density, with hypodense submucosa (Romano et al. 2006) (Figs. 8, 9). From this stage, healing of the intestinal injury related to impaired venous drainage can be often achieved with a medical therapy; however, persistence of the disease causes a chronic alteration in the intestinal wall, and rarely progresses to intestinal infarction (Romano et al. 2006). In this case, the CT findings of intestinal infarction as the late stage of injury from impaired venous drainage (Fig. 9) are related to the evidence of mesenteric vein occlusion, peritoneal fluid, marked wall thickening, absence of parietal enhancement, and intramural and/or portal-mesenteric pneumatosis (Romano et al. 2008).
Extensive splenic-portal venous thrombosis (asterisk in a), with infarction of some jejunal loops (b, c). Note the feature of the distal jejunum, presenting parietal enhancement and damage from impaired venous drainage; note the appearance of the ileum, with most loops collapsed, spastic (d). Different appearance of the intestine with the presence of infarcted segments (asterisk in e) and damage from impaired venous drainage in the following tract; ileum is collapsed. Note also the appearance of the large intestine, with tristratification of the wall and hyperenhanced mucosa
4.3 Colonic Ischemia
Vascular disorders of the colon include various pathologic and clinical findings of different grades of severity from self-limiting and transient ischemia to bowel infarction (Marston 1986; Robert et al. 1993; Balthazar et al. 1999; Romano et al. 2006). Ischemic colitis was considered as a form of nonocclusive ischemic disease, with no correlations between the site and extension of the intestinal involvement and the distribution of the superior or inferior mesentery artery or vein (Eisenberg et al. 1979; Brandt and Boley 1993; Balthazar et al. 1999; Zimmermann and Granger 1992; Romano et al. 2006). The colonic regions pertinent to Griffith’s point (the junction between the distribution of the superior and inferior mesenteric arteries closed to the colonic splenic flexure) and Sudeck’s point (the anastomotic plexus between the inferior mesenteric and the hypogastric arteries at the rectosigmoid junction) have been reported as most commonly involved by ischemic injuries (Balthazar et al. 1999; Rogers and David 1995; Romano et al. 2006). Regarding the various degrees of injury from ischemia affecting the colon, the damage could range from mucosal ulcerations to submucosa edema and hemorrhage to transmural infarction (Balthazar et al. 1999). CT findings of ischemic disease of the colon could be considered in a disease–progression grading scale (Romano et al. 2006), from early injury to late evidence of infarction. Acute ischemic damage to the colon can be segmental or diffuse, with the typical pattern consisting in hemorrhage in the lamina propria associated with superficial epithelial necrosis (Whitehead 1972; Petras 2004) that could progress to full-thickness ulceration of the mucosa (Petras 2004). At this stage CT could be a useful tool to evaluate the colonic wall feature and injury: mural thickening with hyperdensity of the mucosa from hemorrhage associated with submucosal edema has the typical sign of the “little rose” (Romano et al. 2006, 2007), appreciable on the axial scan especially at the level of the descending colon (Fig. 10). A small amount of peritoneal fluid with evidence of pericolic streakiness and shaggy contour of the involved intestine are additional findings to note (Romano et al. 2006). The inferior artery vascular tree could be easily evaluated on the multiplanar reformation in the arterial phase of the study. Persistence of the ischemic injury without reperfusion causes a concentric, symmetric, mild mural thickening with homogeneous density of the large bowel wall, offering a well-defined edge (Fig. 11); pericolic streakiness could be present as well as a moderate amount of peritoneal fluid (Romano et al. 2006). If the ischemia persists longer, infarction could develop, with necrosis of the involved colonic segment. Reperfusion after the ischemic event causes marked submucosal edema (Fig. 12), wall thickening and inhomogeneous parietal enhancement, loss of colonic haustra, and pericolic streakiness of different degrees (Romano et al. 2006). Progression of the colonic ischemia to infarction leads to imaging findings related to bowel necrosis with the absence of enhancement and the presence of parietal pneumatosis and free peritoneal or retroperitoneal air if perforation occurs (Fig. 2, 13).
Infarction of the distal descending and sigmoid colon infarction (a–c) in a patient submitted to abdominal aortic surgery (d) after rupture of an aneurysm (e). Note the complete absence of enhancement of the involved colonic segment and the presence of a bubble of gas from parietal pneumatosis due to the late stage of ischemia with infarction
4.4 CT Pitfalls
Diagnosis of intestinal ischemia is not easy, especially if the CT examination is not performed adequately (i.e., administration of intravenous contrast medium, multiphase examination, thin slice thickness with back reconstructions less than 1 mm). Evaluation of the intestinal trophism is not easy without knowledge of the physiopathologic changes that occur in the bowel wall as a consequence of deficiency in blood supply or impaired venous drainage. Reperfusion damage to the intestine from an arterial cause, mainly represented on CT by evidence of submucosal hypodensity from edema, has to be differentiated with the target sign from venous occlusive disease or stratification of the bowel from inflammation related to enteritis of other origin (Figs. 14, 15). Again, evaluation of parietal enhancement of a segment affected by disease from impaired venous drainage is not easy in some cases for experienced radiologists not well trained in emergency intestinal disease imaging. Other aspects to consider as potential pitfalls are the enhancement and features of the colon in ischemic injury: weak hyperdensity of the bowel wall from hemorrhage could be erroneously considered a “normal finding,” or a mistake could be made in evaluating a thin colonic segment from infarction, described as “ischemic” and not irreversible death. Appropriate definition of “pneumatosis” and evaluation of any eventual different benign cause of this findings (such as the presence of parietal air from damage related to overdistension of the lumen, not related to wall infarction) is mandatory (Fig. 16). To limit any potential error in diagnosis in the case of CT examination for clinical suspicion of vascular intestinal disorder, it should be mandatory to evaluate the imaging findings related to the bowel wall and to other abdominal structures considering the clinical history of the patient, the laboratory parameters, the type of abdominal pain, and the results of any eventual recent diagnostic imaging examination performed.
Intestinal ischemia has to be differentiated from other findings of intestinal wall abnormality. In this case a diffuse enteritis in a young patient with bone marrow transplant is shown (a, b). Note the diffuse “target sign” with hyperenhancement of the mucosa and stratification of the wall. Mesenteric vessels were well opacified
Parietal pneumatosis is not related to intestinal infarction. Presence of gas in the wall of the ascending colon (a, b) distended by fluid in a patient with large bowel obstruction caused by a proximal sigmoid colon neoplasm (b). The wall of the ascending colon shows normal parietal enhancement with no sign of infarction. The concept of “benign” pneumatosis is related to the presence of this finding in conditions other than intestinal ischemia; in this case the parietal pneumatosis was caused by overdistension of the gut with damage to the mucosa and spread in the wall of some amount of gas
5 CT Impact on Management
Advances in technology of the CT equipment with the introduction of multidetector-row machines contributed to improvement in the diagnostic imaging using CT, with a positive gain in time needed and efficacy in response to clinical questions, especially in emergency patients. The use of multiphasic evaluation of anatomic structures with the added value of some software to reduce the overall radiation doses administered to patients during examinations improved the number and type of clinical requests for this imaging method. Actually, the use of CT is widespread in the main emergency department and diagnostic efficacy in numerous and different diseases, traumatic and nontraumatic, is attested by multiple scientific publications from large series of patients. The impact of CT on the management of the acute abdominal pain from mesenteric ischemic affection is high: the use of this method as a first-line or immediate second-line examination, because of the diagnostic support provided by the imaging findings, could be of extreme importance either to indicate in what phase or stage of ischemic disease (if any) the patient is or to allow a prompt diagnosis of vascular disease of the intestine that could require interventional procedures or surgery.
6 Diagnostic Strategy
Despite the current widespread use of CT as the first-line examination in patients with acute abdominal pain, there is still a role for the basic imaging methods (conventional radiograph and ultrasonography), represented by detection of gross abdominal findings underlying an acute disease, such as the evidence on conventional radiography of fluid or gaseous distension of the intestine and bowel loop features or the presence of free peritoneal air. Using ultrasonography of the abdomen it is possible to document the presence of peritoneal fluid as well as the evaluation of the intestinal peristalsis, the fluid-filled lumen, and the features of the bowel wall and plicae. Findings from basic imaging methods could help in selecting patients who could benefit from an immediate CT examination, evaluating firstly the cause and potential stage of the disease. Detection of an endoluminal defect of opacification of mesenteric vessels by CT could suggest the type of disease to be subjected to angiographic procedures or to be clinically treated with medical therapy. The most important role of CT is to provide diagnostic information for a correct interpretation of the findings in order to select patients who require immediate surgical intervention. Follow-up examination of the intermediate stage of ischemia could be done with CT if no specific radiation risks are present. Serial ultrasonography examination could help in monitoring any abnormality in the bowel wall detected by CT, especially the damage from reperfusion characterized by parietal thickening and edema, suggesting a relapse in injury or recovery from an ischemic event. The combination of findings from different imaging methods could be added value for an efficient diagnostic strategy for patients affected by vascular disorders of the intestine.
References
Acosta S (2010) Epidemiology of mesenteric vascular disease: clinical implications. Semin Vasc Surg 23(1):4–8
Balthazar EJ, Yen BC, Gordon RB (1999) Ischemic colitis: CT evaluation of 54 cases. Radiology 211:381–388
Bartone G et al (2008) Clinical symptoms of intestinal vascular disorders. Radiol Clin North Am 46:887–889
Brandt LJ, Boley SJ (1993) Ischemic and vascular lesions of the bowel. In: Sleisenger MH, Fordtran JS (eds) Gastrointestinal disease: pathophysiology, diagnosis, management, 5th edn. Saunders, Philadelphia, pp 1940–1945
Bulkley GB et al (1985) Relationship of blood flow and oxygen consumption to ischemic injury in the canine small intestine. Gastroenterology 89:852–857
Chou CK (2002) CT manifestation of bowel ischemia. AJR Am J Roentgenol 178:87–91
Chou CK et al (2004) CT of small bowel ischemia. Abdom Imaging 29:18–22
Eisenberg RL, Montgomery CK, Margulis AR (1979) Coltis in the elderly: ischemic colitis mimicking ulcerative and granulomatous colitis. AJR Am J Roentgenol 133:1113–1118
Fenoglio-Preiser CM et al (2008) The nonneoplastic small intestine. In: Fenoglio-Preiser CM (ed) Gastrointestinal pathology. An atlas and text, 3rd edn. Wolters Kluwer, Lippincott, Williams & Wilkins, Philadelphia, pp 326–339
Fondacaro JD (1984) Intestinal blood flow and motility. In: Shepherd AP, Granger DN (eds) Physiology of the intestinal circulation. Raven Press, New York, pp 107–119
Friedberg MJ, Polk HC Jr (1965) Superior mesenteric arteriography in experimental mesenteric venous thrombosis. Radiology 85:38–45
Gilsdorf RB et al (1983) Posterior hypothalamic effects on gastrointestinal blood flow in the conscious cat. Proc Soc Exp Biol Med 143:329–334
Gore RM et al (2008) Imaging in intestinal ischemic disorders. Radiol Clin North Am 46:845–875
Granger DN, Barrowman JA (1983) Microcirculation of the alimentary tract. II. Pathophysiology of edema. Gastroenterology 84:1035–1049
Herbert GS, Steele SR (2007) Acute and chronic mesenteric ischemia. Surg Clin North Am 87:1115–1134
Jamieson WG et al (1982) The early diagnosis of massive acute intestinal ischemia. Br J Surg 69(Suppl):552–553
Jost CJ, Gloviczki P (2002) Mesenteric vein thrombosis. In: Geroulakos G, Cherry KJ (eds) Disease of the visceral circulation. Arnold, London, pp 145–157
Klatte EC et al (1982) Angiographic studies of the upper gastrointestinal tract. In: Scott HW, Sawyers JL (eds) Surgery of the stomach, duodenum and small intestine. pp 194–197
Kitchens CS (1992) Evolution of our understanding of the pathophysiology of primary mesenteric venous thrombosis. Am J Surg 163:346–348
Kvietys PR, Granger DN (1984) Physiology, pharmacology and pathology of the colonic circulation. In: Shepherd AP, Granger DN (eds) Physiology of the intestinal circulation. Raven Press, New York, pp 131–142
Kvietys PR et al (1980) Intrinsic control of colonic blood flow and oxygenation. Am J Physiol 238:478–484
Laureano BA, Wade TP (1998) Mesenteric venous disease. In: Longo WE, Peterson GJ, Jacobs DL (eds) Intestinal ischemia disorders. Quality Medical Publishing, St Louis, pp 207–219
Martinez JP, Hogan GJ (2004) Mesenteric ischemia. Emerg Med Clin North Am 22(4):909–928
Marston A (1986) Vasular disease of the gastrointestinal tract. William and Wilkins, Baltimore, pp 152–173
Noer RJ (1943) The blood vessels of the jejunum and ileum: a comparative study of man and certain laboratory animals. Am J Anat 73:293–334
Nylander G, Wikstrom S (1968) Propulsive gastrointestinal motility in regional and graded ischemia of the small bowel. An experimental study in rats. I. Immediate results. Acta Chir Scand 385(Suppl) :1–67
Oldenburg WA et al (2004) Acute mesenteric ischemia: a clinical review. Arch Intern Med 164(10):1054–1062
Paterno F, Longo WE (2008) The etiology and pathogenesis of vascular disorders of the intestine. Radiol Clin North Am 46:877–885
Perko MJ et al (2002) Management of acute visceral ischemia. In: Geroulakos G, Cherry KJ (eds) Diseases of the visceral circulation. Arnold, London, pp 80–87
Petras RE (2004) Acute ischemic colitis. In: Mills SE (ed) Sternberg’s diagnostic surgical pathology. Lippincott Williams & Wilkins, Philadelphia, p 1495
Polk HC Jr (1966) Experimental mesenteric venous occlusion. III. Diagnosis and treatment of induced mesenteric venous thrombosis. Ann Surg 163:432–444
Robert JH, Mentha G, Rohner A (1993) Ischaemic colitis: two distinct patterns of severity. Gut 34:4–6
Rogers AI, David S (1995) Intestinal blood flow and diseases of vascular impairement. In: Haubrich WS, Schaffner F, Berck JE (eds) Gastroenterology, 5th edn. Saunders, Philadelphia, pp 1212–1234
Romano S et al (2006) Ischemia and infarction of the small bowel and colon: spectrum of imaging findings. Abdom Imaging 31(3):277–292
Romano S et al (2007) Multidetector row computed tomography findings from ischemia to infarction of the large bowel. Eur J Rad 61(3):433–441
Romano S et al (2008) Small bowel vascular disorders from arterial etiology and impaired venous drainage. Radiol Clin North Am 46:891–908
Taourel P et al (2008) Imaging of ischemic colitis. Radiol Clin North Am 46:909–924
Wheaton GB et al (1981) Gross anatomy of the splanchnic vasculature. In: Granger DN, Bulkley GB (ed) Measurement of blood flow: applications to the splanchnic circulation. Williams and Wilkins, Baltimore, pp 9–45
Whitehead R (1972) The pathology of intestinal ischemia. Clin Gastroenterol 1:613–637
Zimmermann BJ, Granger DN (1992) Reperfusion injury. Surg Clin North Am 72:65–83
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Romano, S., Romano, L. (2010). Ischemia (Acute Mesenteric Ischemia and Ischemic Colitis). In: Taourel, P. (eds) CT of the Acute Abdomen. Medical Radiology(). Springer, Berlin, Heidelberg. https://doi.org/10.1007/174_2010_82
Download citation
DOI: https://doi.org/10.1007/174_2010_82
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-89231-1
Online ISBN: 978-3-540-89232-8
eBook Packages: MedicineMedicine (R0)