Abstract
Over the last decade, there has been a steady increase in the use of fixed dose combinations for the treatment of a range of diseases, including cancer, AIDS, tuberculosis and other infectious diseases. It is now evident that patients with asthma or chronic obstructive pulmonary disease (COPD) can also benefit from the use of fixed dose combinations, including combinations of a long-acting β2-agonist (LABA) and an inhaled corticosteroid (ICS), and combinations of LABAs and long-acting muscarinic receptor antagonists (LAMAs). There are now also “triple inhaler” fixed dose combinations (containing a LABA, LAMA and ICS) under development and already being made available in clinical practice, with the first such triple combination having been approved in India. The use of combinations containing drugs with complementary pharmacological actions in the treatment of patients with asthma or COPD has led to the discovery and development of drugs having two different primary pharmacological actions in the same molecule that we have called “bifunctional drugs”. In this review we have discussed the state of the art of bifunctional drugs that can be categorized as bifunctional bronchodilators, bifunctional bronchodilator/anti-inflammatory drugs, bifunctional anti-inflammatory drugs and bifunctional mucolytic and anti-inflammatory drugs.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Background
Asthma and COPD are common complex inflammatory diseases of the respiratory tract that usually require treatment with multiple drug classes (Boulet et al. 2012; Vestbo et al. 2013). Over the last decade, there has been a steady increase in the use of fixed dose combinations of two or more drugs for the treatment of a range of diseases including cancer (van Meir et al. 2014), AIDS (Flexner and Saag 2013), tuberculosis (Dawson and Diacon 2013) and other infectious diseases (Huang et al. 2013).
It is now recognized that the treatment of asthma and COPD can benefit from the use of fixed dose combinations of two or more drug classes (Cazzola et al. 2012a). Today the treatment of asthma and COPD globally is dominated by the use of inhaled fixed dose combinations of a LABA and an ICS, although the wide usage of ICS in the treatment of patients with COPD is being questioned because of a potential increased risk of pneumonia (Kew and Seniukovich 2014) and because of recent observations questioning their efficacy (Magnussen et al. 2014). Nonetheless many fixed dose combinations of ICS/LABA and ICS/LAMA and indeed triple inhalers containing fixed doses of LABA/LAMA and ICS are in development.
However, the use of fixed dose combinations for the treatment of asthma and COPD is not a new concept with inhaled fixed dose combinations of both short-acting β2-agonists (SABAs) and short-acting muscarinic receptor antagonists (SAMAs) having been used for many years in the treatment of patients with asthma or COPD (Goodman & Gilman 2005), and such combinations are particularly used in the treatment of acute exacerbations of these diseases. The success of these medicines has stimulated the development of longer-acting β2-agonists (LABAs) and ultra-LABAs and longer-acting muscarinic receptor antagonists (LAMAs). These drugs are now widely used as bronchodilators for the treatment of patients with COPD and more severe asthma (Cazzola et al. 2012a).
These developments in treatment using fixed dose combinations reflect our growing understanding that there is a need to treat both the underlying inflammation and the symptoms of airway obstruction that characterize asthma and COPD. Moreover, the use of multiple drugs in a single inhaler is thought to improve the adherence to treatment, as it is well recognized that patients prescribed a bronchodilator and an anti-inflammatory drug as monoinhalers will often stop the anti-inflammatory drug when symptoms improve (Stempel et al. 2005), despite current understanding suggesting that regular use of ICS (at least in patients with asthma) may be necessary to optimize lung function and reduce exacerbations of the disease in the long term (Bateman et al. 2008).
However, the development of formulations to allow the use of more than one drug class in a single inhaler is sometimes challenging, as there are often differences in duration of action of the mono-components and issues concerning chemical compatibility and stability as well as gallenic challenges relating to the different physiochemical properties of the different drug classes (Cazzola et al. 2012a). This is especially so with the development of triple inhalers, and to date only one such medicine containing tiotropium bromide, ciclesonide and formoterol fumarate has been approved in India, although others are in late-stage clinical development (Cazzola and Matera 2014).
However, an alternative approach to delivering complementary pharmacological activities for the treatment of patients with asthma or COPD is to develop molecules designed to have two distinct primary pharmacological actions, which we will term bifunctional drugs. In this article we review the current status of bifunctional drugs in development or currently in use for the treatment of respiratory diseases.
2 Bifunctional Bronchodilator Drugs
It has long been recognized that β2-agonists and muscarinic receptor antagonists improve lung function by distinct pharmacological mechanisms, β2-agonists acting to relax airway smooth muscle irrespective of the cause of the bronchoconstriction and muscarinic receptor antagonists by blocking M3 receptors on airway smooth muscle to limit the actions of the neurotransmitter acetylcholine (ACh) released from parasympathetic nerves innervating the lung (Cazzola et al. 2012a; Cazzola and Molimard 2010).
Moreover, β2-agonists can amplify the bronchial smooth muscle relaxation caused by a muscarinic receptor antagonist by decreasing the release of ACh via a modulation of cholinergic neurotransmission that involves calcium-activated potassium (KCa) channels rather than adenylyl cyclase and subsequent increases in intracellular levels of cyclic adenosine monophosphate (c-AMP). Activation of KCa channels is thought to hyperpolarize the cell membrane, thus causing reductions in the concentration of intracellular Ca2+ and ACh release in prejunctional parasympathetic nerves (Cazzola and Molimard 2010; Cazzola et al. 2013a) and thus potentially providing additional bronchodilation above the effects seen with antagonism of muscarinic receptors alone on the airway smooth muscle. However, this mechanism seems unlikely to contribute in a significant way in clinical practice as there is evidence clearly indicating that β2-agonists facilitate, rather than inhibit release of Ach from airway parasympathetic nerves (Meurs and Dekkers 2013; Meurs et al. 2013). Therefore, it has been suggested that crosstalk between the signalling mechanisms arising from antagonism of muscarinic receptors and activation of β2 adrenoceptors within airway smooth muscle provides a more plausible explanation of the additional bronchodilation seen when both classes of drug are used together rather than individually (Meurs and Dekkers 2013; Meurs et al. 2013). Indeed, crosstalk between Gq-coupled M3 receptors and Gs-coupled β2 adrenoceptors may have a major influence on β2-agonist-induced relaxation, presumably by activation of protein kinase C (PKC) and subsequent phosphorylation of the β2 adrenoceptor and/or Gs protein (Meurs and Dekkers 2013; Meurs et al. 2013). Moreover, at postsynaptic level β2AR signalling limits M3 receptor-mediated inositol triphosphate (IP3) production by several distinct mechanisms, most presumed to involve protein kinase A (PKA) (Pera and Penn 2014).
Recent findings have also demonstrated that β2 adrenoceptors and muscarinic receptors mediate opposing effects on endothelin-1 expression in human lung fibroblasts (Ahmedat et al. 2012). Since muscarinic receptor-mediated upregulation of endothelin-1 contributes to profibrotic effects induced by muscarinic agonists, inhibition of endothelin-1 expression by a muscarinic receptor antagonist could contribute to long-term beneficial effects of these drugs. Moreover, β2-agonists and muscarinic receptor antagonists have been demonstrated to provide additive control of transforming growth factor (TGF)-β1-mediated neutrophilic inflammation in patients with COPD (Profita et al. 2012) that has implications also for the use of such drugs in the treatment of patients with neutrophilic asthma. LABAs and anticholinergic drugs might also contribute to control the ACh-induced increased levels of Th17 cells in systemic inflammation of COPD (Profita et al. 2014).
These complementary pharmacological actions have led to LABAs and LAMAs often being used together, particularly in the treatment of patients with COPD (van der Molen and Cazzola 2012), but they are also now being investigated for the treatment of asthma where combinations of SABAs and SAMAs have been widely used for several decades (Goodman & Gilman 2005). These observations have led to the development of a number of new drugs referred to as MABAs, which have both β2-agonist activity and muscarinic receptor antagonism in the same molecule, some of which have now reached early clinical development (Cazzola et al. 2012a). These bifunctional (or dual pharmacophore) muscarinic antagonist β2-agonist (MABA) agents are exemplified by the drugs GSK 961081 (batefenterol) and THR 200495 which have recently been shown to induce bronchodilation in patients with COPD that lasts for up to 24 h and that is comparable to a combination of salmeterol and tiotropium (Bateman et al. 2013; Norris and Ambery 2013). Other examples include AZD 2115, LAS 190792, TEI3252, PF-3429281 and PF-4348235 (Hughes and Jones 2011; McNamara et al. 2012).
The MABA approach circumvents the potential problems associated with formulating different drugs in one inhaler yet still providing a fixed ratio of muscarinic antagonism and β2 agonism compared with combination therapy (Cazzola et al. 2013b). However, what is not yet clear is the relative contribution of the two different pharmacological activities to the overall improvement in lung function and indeed on which pharmacological action such drugs should be optimally dosed, as some examples of MABAs have different pharmacodynamic half-lives for their β2-agonist activity and the muscarinic receptor antagonist activity within the same molecule (Bateman et al. 2013; Norris and Ambery 2013). A recent clinical study has demonstrated that treatment with 3 separate doses of GSK 961081 showed superior improvements in lung function in patients with COPD compared with a standard dose of salmeterol suggesting that the MABA provides a better treatment than monotherapy with a β2-agonist (Wielders et al. 2013), although a similar trial has not yet been performed comparing a MABA with monotherapy with a muscarinic receptor antagonist. Thus, whilst MABAs show promise, there is a lot that still needs to be understood as to how to best use this class of drug and how they will compare to existing fixed dose combination inhalers (Cazzola et al. 2013b).
3 Bifunctional Bronchodilator/Anti-inflammatory Drugs
Xanthines such as theophylline have been widely used as treatments for both asthma and COPD for more than 100 years, and whilst early clinical studies with such drugs have stressed their bronchodilator activity, they were originally introduced into clinical practice to treat an inflammatory renal disease, glomerular nephritis (Persson 1985). It has been recognized for some time that xanthines could exhibit anti-inflammatory activity experimentally in the lung, additional to their bronchodilator activity (Persson 1985; Spina et al. 1998), an observation that has been confirmed clinically in patients with asthma (Crescioli et al. 1991; Sullivan et al. 1994; Jaffar et al. 1996; Evans et al. 1997; Lim et al. 2001) or COPD (Culpitt et al. 2002; Ford et al. 2010). Such observations provided some of the earliest evidence that it was possible to have both bronchodilator and anti-inflammatory activity in a single molecule. The problem with xanthines is their very narrow therapeutic window (Boswell-Smith et al. 2006a) that has limited their wider use. Furthermore, the advent of newer inhaled bronchodilator and anti-inflammatory drugs, particularly inhaled β2-agonists and ICS, has seen a progressive decline in the use of xanthines (that are usually administered systemically), even though there is clear evidence that withdrawal of theophylline from patients with asthma or COPD leads to worsening of airways inflammation and symptoms, even in patients taking glucocorticosteroids and other classes of bronchodilator drug (Baba et al. 2001; Minoguchi et al. 1998; Kidney et al. 1995). Such observations suggest that xanthines possess other useful pharmacological properties not shared with glucocorticosteroids and other classes of bronchodilator.
This has led at least one pharmaceutical company to develop a combination inhaler using theophylline and an ICS (Barnes et al. 2010). Other pharmaceutical companies have tried to find safer xanthines and a number of been investigated in the clinic, including bamiphylline (Spinelli et al. 1991), enprophylline (Pauwels et al. 1985), isbuphylline (Manzini et al. 1993), acebrophylline (Tapadar et al. 2014) and doxophylline (Page 2010; van Mastbergen et al. 2012), some of which have been approved for the treatment of asthma and COPD. Like theophylline, each of these drugs has been shown to possess anti-inflammatory and bronchodilator actions to varying degrees and, in the case of doxophylline, a wider therapeutic window than theophylline (Page 2010).
Theophylline and the related xanthine isobutyl methylxanthine (IBMX), in particular, have often been described as the archetypal non-selective phosphodiesterase (PDE) inhibitors as a possible mechanism of action of these drugs (Nicholson et al. 1991), although of course it is now recognized that this is probably not the only molecular mechanism contributing to their therapeutic benefit in the treatment of patients with asthma or COPD (Boswell-Smith et al. 2006a). Thus, another approach to try and improve the therapeutic window of xanthines has been to develop more selective inhibitors of the growing family of PDEs, as it is now recognized that PDE 3 and 4 are found in airway smooth muscle, whilst PDE 3, 4 and 7 are found in the majority of inflammatory cells thought to be involved in the pathogenesis of asthma and COPD (Spina et al. 1998; Page 2014). Specifically, the PDE3 isoenzyme is considered to predominate in airway smooth muscle, and inhibition of this enzyme, rather than PDE4 inhibition, leads to airway smooth muscle relaxation, whereas the PDE4 isoenzyme is the predominant isoenzyme in the majority of inflammatory cells, including neutrophils, which are implicated in the pathogenesis of COPD and severe asthma, and in eosinophils, which characterize inflammation in patients with asthma (Page 2014).
Recently the selective PDE4 inhibitor roflumilast-n-oxide has been approved for the treatment of severe COPD, although the side effect profile of this drug still limits the wider use of this agent (Calverley et al. 2009; Fabbri et al. 2009). This clinical benefit of roflumilast is thought to arise from the anti-inflammatory action of this selective PDE4 inhibitor (Grootendorst et al. 2007), as whilst PDE4 is found in human airway smooth muscle, it is now clear from a number of clinical studies with a variety of PDE4 inhibitors administered either orally (Grootendorst et al. 2003; Harbinson et al. 1997) or by inhalation (Singh et al. 2010), that this drug class is not able to induce acute bronchodilation.
In contrast, a number of selective PDE3 inhibitors have been shown to elicit acute bronchodilation in man (Bardin et al. 1998; Myou et al. 1999), and indeed recently PDE3 has been documented to be upregulated in airway smooth muscle obtained from patients with asthma (Yick et al. 2013). These observations have led to the development of drugs having dual inhibitory activity for both PDE3 and PDE4 in order to obtain both bronchodilator and anti-inflammatory activity in the same molecule. The first such drug was zardaverine, which clearly exhibited bronchodilation in patients with asthma but unfortunately was halted during clinical development because of gastrointestinal side effects (Brunnée et al. 1992). Another example was benzafentrine (AH 21-132) (Foster et al. 1992), which clinically elicited bronchodilation but was later discontinued from clinical development, as was another dual PDE 3/4 inhibitor, pumafentrine (Rieder et al. 2013).
Other compounds having both PDE3 and 4 inhibitory activities have been described by Kyorin Pharmaceuticals in Japan, but these have also been stopped at the preclinical stage because of unwanted gastrointestinal side effects (Ochiai et al. 2013). However, another inhaled dual PDE3/4 inhibitor, RPL 554 (Boswell-Smith et al. 2006b), has been shown in early clinical studies to have both bronchodilator and anti-inflammatory actions at the same dose, without having significant side effects (Franciosi et al. 2013), representing potentially a new class of drug for the treatment of patients with asthma or COPD (Wedzicha 2013). Furthermore, recent data investigating this drug in combination with either a muscarinic receptor antagonist or a β2-agonist has shown synergistic interactions on the relaxation of human bronchi (Calzetta et al. 2013) or human small airways (Calzetta et al. 2015). If such findings translate into the clinical setting, such observations raise the distinct possibility of combination of dual PDE 3/4 inhibitors with other drug classes. Furthermore, PDE5 inhibitors such as sildenafil are also able to induce bronchodilation in addition to their well-documented effects on pulmonary vascular smooth muscle (Charan 2001) as well as suppress the pulmonary inflammation and airway hyperreactivity that follow allergen and lipopolysaccharide (LPS) challenge (Toward et al. 2004). Thus, it has been suggested that a new molecule that inhibits both PDE4 and PDE5 could act at multiple levels in patients with COPD, reducing lung inflammation and, possibly, remodelling, as well as decreasing arterial pulmonary hypertension, and improving lung function (Giembycz 2005). One such example is LASSBio596, designed as a hybrid of thalidomide and aryl sulfonamide, which is a drug that exhibits potent inhibitory effects on both PDE4 and PDE5 (Rocco et al. 2003). In a murine model of elastase-induced emphysema, LASSBio596 reduced lung inflammation and remodelling as well as being able to improve lung mechanics (Guimaraes et al. 2014). Interestingly, it has also been documented that LASSBio596 has the potential to block proliferation of fibroblasts (Campos et al. 2006).
Another approach to combining anti-inflammatory and bronchodilator actions in a single molecule has been to combine the bronchodilator actions of nitric oxide (NO) with the anti-inflammatory actions of an ICS. NO-budesonide (TPI 1020) (Boulet et al. 2009; Turner et al. 2010) was the first example of such a drug, although this drug has been dropped from further development. Others have attempted to combine NO and salbutamol into a single molecule (NCX 950) to obtain both bronchodilator and anti-inflammatory actions, and this approach has shown some promise preclinically (Lagente et al. 2004). Another innovative approach is the use of a mutual prodrug designed to allow local metabolism to the active forms of the parent constituents at the site of action, thus reducing unwanted systemic side effects. GS424020, a novel mutual prodrug of salmeterol and desisobutrylciclesonide, exhibited intriguing pharmacological activity in preclinical studies (Barrett et al. 2010).
GS-5759 is a novel bifunctional PDE4 inhibitor/LABA drug that displays PDE4 inhibition and β2 agonism comparable to roflumilast and indacaterol, respectively (McDonald et al. 2012). More recently a series of molecules that combine the anti-inflammatory drug roflumilast with the LABA salmeterol (Barrett et al. 2010; Huang et al. 2014; Liu et al. 2013) or formoterol (Tannheimer et al. 2012) have been described that are other potential examples of a new drug class that combine anti-inflammatory and bronchodilator actions into a single molecule, although to date there are very limited biological data with these molecules. A potential advantage of these compounds is that both β2-agonists and PDE4 inhibitors rely on modulation of the secondary messenger cyclic AMP to elicit their effects, and it is possible that such a bifunctional drug could provide additive or even potentially synergistic anti-inflammatory activity in the lungs (Tannheimer et al. 2012). Also bifunctional compounds in which a PDE4 inhibitor is connected to a muscarinic receptor antagonist have been described (Phillips and Salmon 2012) that utilize a pyrazolopyridine as the PDE4 inhibitor and a biaryl-containing muscarinic antagonist but differ in the linker used to combine these two activities into the same molecule. Another example of such an approach is UCB-101333-3, a 4,6-diaminopyrimidine (Provins et al. 2007).
RO 50-24118, a stable analogue of vasoactive intestinal peptide (VIP) that is highly selective for the VPAC2 receptor, has been shown to have dual bronchodilatory and anti-inflammatory effects, in that it relaxes airway smooth muscle cells, inhibits bronchoconstriction and attenuates the influx of neutrophils and CD8+ T cells in inflammatory lung disease (Tannu et al. 2010) suggesting another potential approach to combining anti-inflammatory and bronchodilator actions into a single molecule.
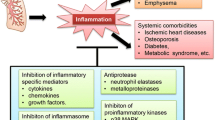
4 Bifunctional Anti-inflammatory Drugs
Glucocorticosteroids are currently recognized as the gold standard anti-inflammatory drugs for the treatment of inflammatory airway diseases such as asthma and COPD, in part because they exhibit polypharmacy via a range of actions, such as reducing the activation and recruitment of inflammatory cells into the lung (Adcock et al. 2008). However, this drug class can also be associated with significant side effects when they enter the systemic circulation as well as having local side effects when applied topically. Nonetheless, given the success of glucocorticosteroids as anti-inflammatory drugs, it is perhaps not surprising that the “holy grail” of the pharmaceutical industry for many years in the respiratory field has been to find an alternative anti-inflammatory drug to glucocorticosteroids that retain the efficacy but that have a better safety profile (Adcock et al. 2008). There have been many new classes of anti-inflammatory drug developed (Adcock et al. 2008; Cazzola et al. 2012b), most of which have failed, except in the treatment of a subset of more severe patients with asthma (Nair et al. 2009) or COPD (Calverley et al. 2009; Fabbri et al. 2009). Many of these have been drugs or biologics directed against a single inflammatory mediator, and these failures (Adcock et al. 2008; Cazzola et al. 2012b; Bryan et al. 2000; Leckie et al. 2000; Nair et al. 2012; Gauvreau et al. 2014) perhaps suggest that the complexity of the inflammatory response in both asthma and COPD requires drugs that have actions at more than one biological target.
Thus, a number of drugs have been developed having bifunctional anti-inflammatory activity, including drugs exhibiting antagonism for the receptors for platelet-activating factor (PAF) and histamine, and also mast cell secretion-blocking effects in the same molecule such as rupatadine (Saint-Martin et al. 2004; Church 2010), as well as drugs behaving as thromboxane receptor antagonists and cys-LT antagonists in the same molecule (Arakida et al. 1998). However, both of these classes of drug have to date only shown limited efficacy, at least in the treatment of allergic airways disease.
Dual targeting of IL-13 and IL-4 is another approach that holds promise for achieving great efficacy. Persistence of asthma symptoms despite high-dose corticosteroids has been linked to increased IL-13 levels in the lungs, suggesting that IL-13 expression might contribute to corticosteroid resistance in some patients. IL-4 shares functional redundancy with IL-13 because of a shared receptor, the type 2 IL-4R; however, IL-4 can also signal exclusively through the type 1 IL-4R (composed of IL-4Rls in the lungs, suggest) (Kasaian et al. 2013; Kau and Korenblat 2014 Dec). A biotherapeutic agent targeting both murine IL-4 and IL-13 was generated by combining well-characterized binding domains in an optimal configuration, using appropriate linker regions (Kasaian et al. 2013). This bifunctional IL-4 and IL-13 antagonist demonstrated high affinity for both cytokines and reduced the IL-4-dependent rise in serum IgE and reduced IL-13-dependent BHR, lung inflammation, mucin gene expression and serum chitinase responses in mice. Effective dual blockage of IL-13 and IL-4 resulted in greater therapeutic benefit than could be achieved by targeting either cytokine alone raising the possibility of bifunctional biologics. Other multiple agents that target both IL-4 and IL-13 have entered into clinical development, including AMG-317, dupilumab and pitrakinra. Pitrakinra, a recombinant IL-4 mutein that blocks the effects of both IL-4 and IL-13, improved the exacerbation incidence in response to medication withdrawal in asthmatic patients with high peripheral blood eosinophil counts (>350 cells/mm3) (Wenzel et al. 2010). In patients with persistent, moderate-to-severe asthma and elevated eosinophil levels who used ICS and LABAs, therapy with dupilumab, a fully humanized mAb to the IL-4Rα receptor that inhibits both IL-4 and IL-13, as compared with placebo, was associated with fewer asthma exacerbations when LABAs and inhaled glucocorticoids were withdrawn, with improved lung function and reduced levels of Th2-associated inflammatory markers (Wenzel et al. 2013). Bispecific antibodies, antibodies that are able to inhibit the action of two targets simultaneously, have been designed for IL-4 and anti IL-13 and could be an additional therapeutic option in individuals with an unfavourable IL-4Rα polymorphism (Spiess et al. 2013).
The co-expression of PDE4 and PDE7 in most immunoinflammatory cells and the synergistic effects of PDE7- and PDE4-selective drugs in the suppression of inflammation in cell-based studies have fuelled speculation that dual inhibition of PDE7 and PDE4 could be an effective strategy to treat COPD (Page and Spina 2012). IR-284 is a dual PDE4–PDE7 inhibitor, but there is no published study that has documented its effects in patients with COPD (Matera et al. 2014). Nonetheless, TPI 1100, which comprises two antisense oligonucleotides targeting the messenger RNA (mRNA) for the PDE4B/4D and PDE7A isoforms, has been shown to reduce neutrophil influx and key cytokines in an established smoking mouse model (Seguin and Ferrari 2009).
Since pathological airway remodelling is mediated by PDE1 and PDE1 inhibitors that block smooth muscle mitogenesis (Chan and Yan 2011), combined PDE1 and PDE4 inhibitors could have utility in the treatment of patients with COPD (Giembycz and Maurice 2014). The dual PDE1/4 inhibitor KF19514 is also reported to be able to suppress inflammation and arrest airway remodelling, at least in a murine model of chronic asthma (Kita et al. 2009).
5 Bifunctional Anti-inflammatory/Mucolytic/Antioxidant Drugs
Carbocysteine (Rahman and MacNee 2012), N-acetyl cysteine (NAC) (Rahman and MacNee 2012) and erdosteine (Cazzola et al. 2010) are all drugs that have been used for many years in the treatment of COPD. They have been variously described as antioxidants or mucolytic drugs and continue to be prescribed in many countries. However, recent data with NAC (Zheng et al. 2014) has reported significant effects on exacerbations in patients with COPD which suggest that this class of drug may need to be used more widely. It is of interest that both NAC (Zheng et al. 2014) and erdosteine (Cazzola et al. 2010) have both been shown to be anti-inflammatory, as well as mucolytic, activities which would both be expected to contribute to the clinical efficacy observed with these drugs in reducing exacerbations. As such they provide templates for the development of novel bifunctional drugs exhibiting both anti-inflammatory and mucolytic activities and have the distinct advantage over many existing drugs in being orally active and well tolerated.
6 Conclusions
It is clear that there is a growing trend to develop drugs with bifunctional activity for the treatment of respiratory diseases that have the potential benefit of being easier to formulate than combinations of multiple drugs in a single inhaler, thus improving adherence and potentially being able to offer additive or even synergistic benefit, as such drugs may target different cellular compartments than when individual drugs are presented to cells individually. It is also likely that the development of bifunctional drugs may serve as a basis for improved “triple-therapy” combinations through coformulation that could deliver three complementary therapeutic effects for patients with asthma or COPD using only two drugs; an example is provided by the recent evidence that the use of the dual PDE3/4 inhibitor, RPL554 in combination with an M3 muscarinic antagonist, may provide synergistic activity on the relaxation of human airway smooth muscle which suggests that if this drug was combined with an anticholinergic drug this could translate into further clinical benefit (Franciosi et al. 2013). Furthermore, the MABA, GSK961081, has recently been evaluated as twice daily fixed combination with fluticasone propionate (Cazzola et al. 2012a).
It is evident therefore that bifunctional drugs offer an exciting new approach to the treatment of respiratory diseases where there remains significant unmet need, and we anticipate that bifunctional drugs will have a significant role to play in the future treatment of patients with asthma or COPD.
References
Adcock IM, Caramori G, Chung KF (2008) New targets for drug development in asthma. Lancet 372:1073–1087
Ahmedat AS, Warnken M, Juergens UR et al (2012) β2-adrenoceptors and muscarinic receptors mediate opposing effects on endothelin-1 expression in human lung fibroblasts. Eur J Pharmacol 691:218–224
Arakida Y, Suwa K, Ohga K et al (1998) In vitro pharmacologic profile of YM158, a new dual antagonist for LTD4 and TXA2 receptors. J Pharmacol Exp Ther 287:633–639
Baba K, Sakakibara A, Yagi T et al (2001) Effects of theophylline withdrawal in well-controlled asthmatics treated with inhaled corticosteroid. J Asthma 38:615–624
Bardin PG, Dorward MA, Lampe FC et al (1998) Effect of selective phosphodiesterase 3 inhibition on the early and late asthmatic responses to inhaled allergen. Br J Clin Pharmacol 45:387–391
Barnes N, Grape S, Fox JC, Fitzgerland M, Snell N, Pavord ID, Jeffery P, Qui Y, Singh D, Antczak A, Nizankowska-Mogilnicka E (2010) Effects of low dose inhaled theophylline (ADC 4022) co-administered with budesonide on inflammatory markers and lung function in patients with COPD. American Thoracic Society Abstract, Annual Conference
Barrett EG, Rudolph K, Royer C et al (2010) A novel mutual prodrug of salmeterol and desisobutrylciclesonide attenuates acute bronchoconstriction in the absence of cardiovascular side-effects in ragweed sensitized and naive dogs [abstract]. Am J Respir Crit Care Med 181:A4249
Bateman ED, Hurd SS, Barnes PJ et al (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31:143–178
Bateman ED, Kornmann O, Ambery C et al (2013) Pharmacodynamics of GSK961081, a bi-functional molecule, in patients with COPD. Pulm Pharmacol Ther 26:581–587
Boswell-Smith V, Cazzola M, Page CP (2006a) Are PDE4 inhibitors just more theophylline? J Allergy Clin Immunol 117(6):1237–1243
Boswell-Smith V, Spina D, Oxford AW et al (2006b) The pharmacology of two novel long-acting phosphodiesterase 3/4 inhibitors, RPL554 [9,10-dimethoxy-2(2,4,6-trimethylphenylimino)-3-(n-carbamoyl-2-aminoethyl)-3,4,6,7-tetrahydro-2H-pyrimido[6,1-a]isoquinolin-4-one] and RPL565 [6,7-dihydro-2-(2,6-diisopropy. J Pharmacol Exp Ther 318:840–848
Boulet L-P, Lemière C, Gauvreau G et al (2009) Safety, pharmacodynamics and pharmacokinetics of TPI 1020 in smokers with asthma. Respir Med 103:1159–1166
Boulet L-P, FitzGerald JM, Levy ML et al (2012) A guide to the translation of the Global Initiative for Asthma (GINA) strategy into improved care. Eur Respir J 39:1220–1229
Brunnée T, Engelstätter R, Steinijans VW, Kunkel G (1992) Bronchodilatory effect of inhaled zardaverine, a phosphodiesterase III and IV inhibitor, in patients with asthma. Eur Respir J 5:982–985
Bryan SA, O’Connor BJ, Matti S et al (2000) Effects of recombinant human interleukin-12 on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet 356:2149–2153
Calverley PMA, Rabe KF, Goehring U-M et al (2009) Roflumilast in symptomatic chronic obstructive pulmonary disease: two randomised clinical trials. Lancet 374:685–694
Calzetta L, Page CP, Spina D et al (2013) Effect of the mixed phosphodiesterase 3/4 inhibitor RPL554 on human isolated bronchial smooth muscle tone. J Pharmacol Exp Ther 346:414–423
Calzetta L, Cazzola M, Page CP, Rogliani P, Facciolo F, Matera MG (2015) Pharmacological chemochestion of the interaction between the dual PDE 3 / 4 inhibitor RPL554 and glycopyronim on human isolated bronchi and small airways. Pulm Pharmacol Ther 32:15–23
Campos HS, Xisto DG, Oliveira MB et al (2006) Protective effects of phosphodiesterase inhibitors on lung function and remodelling in a murine model of chronic asthma. Braz J Med Biol Res 39:283–287
Cazzola M, Matera MG (2014) Triple combinations in chronic obstructive pulmonary disease – is three better than two? Expert Opin Pharmacol 15:2475–2478
Cazzola M, Molimard M (2010) The scientific rationale for combining long acting β2 agonists and muscarinic antagonists in COPD. Pulm Pharmacol Ther 23:257–267
Cazzola M, Floriani I, Page CP (2010) The therapeutic efficacy of erdosteine in the treatment of chronic obstructive bronchitis: a meta analysis of induced patient data. Pulm Pharm Ther 23:135–144
Cazzola M, Page CP, Calzetta L, Matera MG (2012a) Pharmacology and therapeutics of bronchodilators. Pharmacol Rev 64:450–504
Cazzola M, Page CP, Calzetta L, Matera MG (2012b) Emerging anti-inflammatory strategies for COPD. Eur Respir J 40:724–741
Cazzola M, Segreti A, Matera MG (2013a) New developments in the combination treatment of COPD: focus on umeclidinium/vilanterol. Drug Des Devel Ther 7:1201–1208
Cazzola M, Lopez-Campos JL, Puente-Maestu L (2013b) The MABA approach: a new option to improve bronchodilator therapy. Eur Respir J 42:885–887
Chan S, Yan C (2011) PDE1 isozymes, key regulators of pathological vascular remodeling. Curr Opin Pharmacol 11:720–724
Charan NB (2001) Does sildenafil also improve breathing? Chest 120:305–306
Church MK (2010) Efficacy and tolerability of rupatadine at four times the recommended dose against histamine- and platelet-activating factor-induced flare responses and ex vivo platelet aggregation in healthy males. Br J Dermatol 163:1330–1332
Crescioli S, Spinazzi A, Plebani M et al (1991) Theophylline inhibits early and late asthmatic reactions induced by allergens in asthmatic subjects. Ann Allergy 66:245–251
Culpitt SV, de Matos C, Russell RE et al (2002) Effect of theophylline on induced sputum inflammatory indices and neutrophil chemotaxis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 165:1371–1376
Dawson R, Diacon A (2013) PA-824, moxifloxacin and pyrazinamide combination therapy for tuberculosis. Expert Opin Investig Drugs 22:927–932
Evans DJ, Taylor DA, Zetterstrom O et al (1997) A comparison of low-dose inhaled budesonide plus theophylline and high-dose inhaled budesonide for moderate asthma. N Engl J Med 337:1412–1418
Fabbri LM, Calverley PMA, Izquierdo-Alonso JL et al (2009) Roflumilast in moderate-to-severe chronic obstructive pulmonary disease treated with long acting bronchodilators: two randomised clinical trials. Lancet 374:695–703
Flexner C, Saag M (2013) The antiretroviral drug pipeline: prospects and implications for future treatment research. Curr Opin HIV AIDS 8:572–578
Ford PA, Durham AL, Russell REK et al (2010) Treatment effects of low-dose theophylline combined with an inhaled corticosteroid in COPD. Chest 137:1338–1344
Foster RW, Rakshi K, Carpenter JR, Small RC (1992) Trials of the bronchodilator activity of the isoenzyme-selective phosphodiesterase inhibitor AH 21–132 in healthy volunteers during a methacholine challenge test. Br J Clin Pharmacol 34:527–534
Franciosi LG, Diamant Z, Banner KH et al (2013) Efficacy and safety of RPL 554, a dual PDE3 and PDE4 inhibitor, in healthy volunteers and in patients with asthma or chronic obstructive pulmonary disease: findings from four clinical trials. Lancet Respir Med 1:714–727
Gauvreau GM, Boulet L-P, Cockcroft DW et al (2014) OX40L blockade and allergen-induced airway responses in subjects with mild asthma. Clin Exp Allergy 44(1):29–37. doi:10.1111/cea.12235
Giembycz MA (2005) Life after PDE4: overcoming adverse events with dual-specificity phosphodiesterase inhibitors. Curr Opin Pharmacol 5:238–244
Giembycz MA, Maurice DH (2014) Cyclic nucleotide-based therapeutics for chronic obstructive pulmonary disease. Curr Opin Pharmacol 16:89–107
Goodman & Gilman (2005) The pharmacological basis of therapeutics. In: Brunton LL, Lazo JS, Parker KL (eds), 11th edn. McGraw Hill, pp 717–736
Grootendorst DC, Gauw SA, Benschop N et al (2003) Efficacy of the novel phosphodiesterase 4 inhibitor BAY 19–8004 on lung function and airway inflammation in asthma and chronic obstructive pulmonary disease (COPD). Pulm Pharmacol Ther 16:115–120
Grootendorst DC, Gauw SA, Verhoosel RM et al (2007) Reduction in sputum neutrophil and eosinophil numbers by the PDE4 inhibitor roflumilast in patients with COPD. Thorax 62:1081–1087
Guimaraes IH, Padilha GDA, Lopes-Pacheco M et al (2014) Therapy with a new phosphodiesterase 4 and 5 inhibitor in experimental elastase-induced emphysema (abstract). Am J Respir Crit Care Med 189:A6557
Harbinson PL, MacLeod D, Hawksworth R et al (1997) The effect of a novel orally active selective PDE4 isoenzyme inhibitor (CDP840) on allergen-induced responses in asthmatic subjects. Eur Respir J 10:1008–1014
Huang Z-B, Zhao S-S, Huang Y et al (2013) Comparison of the efficacy of lamivudine plus adefovir versus entecavir in the treatment of lamivudine-resistant chronic hepatitis B: a systematic review and meta-analysis. Clin Ther 2013 35(12):1997–2006. doi:10.1016/j.clinthera.2013.10.002
Huang L, Shan W, Zhou Q et al (2014) Design synthesis and evaluation of dual pharmacology β2-adrenoceptor agonists and PDE4 inhibitors. Bioorg Med Chem Lett 24:249–253
Hughes AD, Jones LH (2011) Dual-pharmacology muscarinic antagonist and β2-agonist molecules for the treatment of chronic obstructive pulmonary disease. Future Med Chem 3:1585–1605
Jaffar ZH, Sullivan P, Page C, Costello J (1996) Low-dose theophylline modulates T-lymphocyte activation in allergen-challenged asthmatics. Eur Respir J 9:456–462
Kasaian MT, Marquette K, Fish S et al (2013) An IL-4/IL-13 dual antagonist reduces lung inflammation, airway hyperresponsiveness, and IgE production in mice. Am J Respir Cell Mol Biol 49:37–46
Kau AL, Korenblat PE (2014) Anti-interleukin 4 and 13 for asthma treatment in the era of endotypes. Curr Opin Allergy Clin Immunol 14(6):570–575
Kew KM, Seniukovich A (2014) Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database Syst Rev (3):CD010115
Kidney J, Dominguez M, Taylor M et al (1995) Immunomodulation by theophylline in asthma. Demonstration by withdrawal of therapy. Am J Respir Crit Care Med 151:1907–1914
Kita T, Fujimura M, Myou S et al (2009) Effects of KF19514, a phosphodiesterase 4 and 1 inhibitor, on bronchial inflammation and remodeling in a murine model of chronic asthma. Allergol Int 58:267–275
Lagente V, Naline E, Guenon I et al (2004) A nitric oxide-releasing salbutamol elicits potent relaxant and anti-inflammatory activities. J Pharmacol Exp Ther 310:367–375
Leckie MJ, ten Brinke A, Khan J et al (2000) Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet 356:2144–2148
Lim S, Tomita K, Caramori G et al (2001) Low-dose theophylline reduces eosinophilic inflammation but not exhaled nitric oxide in mild asthma. Am J Respir Crit Care Med 164:273–276
Liu A, Huang L, Wang Z et al (2013) Hybrids consisting of the pharmacophores of salmeterol and roflumilast or phthalazinone: dual β2-adrenoceptor agonists-PDE4 inhibitors for the treatment of COPD. Bioorg Med Chem Lett 23:1548–1552
Magnussen H, Disse B, Rodriguez-Roisin R, Kirsten A, Waltz H, Tetzlaff K, Towse L, Finnegan H, Dahl R, Decramer M, Chanez P, Wouters EFM, Calverley PMA (2014) Withdrawal of inhibited glucocorticosteroids of COPD. N Engl J Med 371(14):1285–1294
Manzini S, Perretti F, Abelli L et al (1993) Isbufylline, a new xanthine derivative, inhibits airway hyperresponsiveness and airway inflammation in guinea pigs. Eur J Pharmacol 249:251–257
Matera MG, Rogliani P, Calzetta L, Cazzola M (2014) Phosphodiesterase inhibitors for chronic obstructive pulmonary disease: what does the future hold? Drugs 74:1983–1992
McDonald JD, Doyle-Eisele M, Kuehl PJ et al (2012) GS-5759, a novel bi-functional phosphodiesterase 4 inhibitor and long-acting β2-adrenoreceptor agonist: evaluation of its bronchodilator and anti-inflammatory pharmacology in non-human primates [abstract]. Am J Respir Crit Care Med 185:A5698
McNamara A, Steinfeld T, Pulido-Rios MT et al (2012) Preclinical efficacy of THRX-200495, a dual pharmacology muscarinic receptor antagonist and β2-adrenoceptor agonist (MABA). Pulm Pharmacol Ther 25:357–363
Meurs H, Dekkers BG, Maarsingh H et al (2013a) Muscarinic receptors on airway mesenchymal cells: novel findings for an ancient target. Pulm Pharmacol Ther 26:145–155
Meurs H, Oenema TA, Kistemaker LE, Gosens R (2013b) A new perspective on muscarinic receptor antagonism in obstructive airways diseases. Curr Opin Pharmacol 13:316–323
Minoguchi K, Kohno Y, Oda N et al (1998) Effect of theophylline withdrawal on airway inflammation in asthma. Clin Exp Allergy 28(Suppl 3):57–63
Myou S, Fujimura M, Kamio Y et al (1999) Bronchodilator effect of inhaled olprinone, a phosphodiesterase 3 inhibitor, in asthmatic patients. Am J Respir Crit Care Med 160:817–820
Nair P, Pizzichini MM, Kjarsgaard M et al (2009) Mepolizumab for prednisone-dependent asthma with sputum eosinophilia. N Engl J Med 360:985–993
Nair P, Gaga M, Zervas E et al (2012) Safety and efficacy of a CXCR2 antagonist in patients with severe asthma and sputum neutrophils: a randomized, placebo-controlled clinical trial. Clin Exp Allergy 42:1097–1103
Nicholson CD, Challiss RA, Shahid M (1991) Differential modulation of tissue function and therapeutic potential of selective inhibitors of cyclic nucleotide phosphodiesterase isoenzymes. Trends Pharmacol Sci 12:19–27
Norris V, Ambery C (2013) Bronchodilation and safety of supratherapeutic doses of salbutamol or ipratropium bromide added to single dose GSK961081 in patients with moderate to severe COPD. Pulm Pharmacol Ther 26:574–580
Ochiai K, Takita S, Kojima A et al (2013) Phosphodiesterase inhibitors. Part 5: hybrid PDE3/4 inhibitors as dual bronchorelaxant/anti-inflammatory agents for inhaled administration. Bioorg Med Chem Lett 23:375–381
Page CP (2010) Doxophylline: a “novophylline”. Pulm Pharmacol Ther 23:231–234
Page CP (2014) Phosphodiesterase inhibitors for the treatment of asthma and COPD. Int Arch Allergy Immunol 165:152–164
Page CP, Spina D (2012) Selective PDE inhibitors as novel treatments for respiratory diseases. Curr Opin Pharmacol 12:275–286
Pauwels R, Van Renterghem D, Van der Straeten M et al (1985) The effect of theophylline and enprofylline on allergen-induced bronchoconstriction. J Allergy Clin Immunol 76:583–590
Pera T, Penn RB (2014) Crosstalk between beta 2-adrenoceptor and muscarinic acetylcholine receptors in the airway. Curr Opin Pharmacol 16:72–81
Persson CG (1985) On the medical history of xanthines and other remedies for asthma: a tribute to HH Salter. Thorax 40:881–886
Phillips G, Salmon M (2012) Bifunctional compounds for the treatment of COPD. Annu Rep Med Chem 47:209–222
Profita M, Bonanno A, Montalbano AM et al (2012) β2 long-acting and anticholinergic drugs control TGF-β1-mediated neutrophilic inflammation in COPD. Biochim Biophys Acta 1822:1079–1089
Profita M, Albano GD, Riccobono L, Di Sano C, Montalbano AM, Gagliardo R, Anzalone G, Bonanno A, Pieper MP, Gjomarkaj M (2014) Increased levels of Th17 cells are associated with non-neuronal acetylcholine in COPD patients. Immunobiology 219:392–401
Provins L, Christophe B, Danhaive P et al (2007) Dual M3 antagonists–PDE4 inhibitors. Part 2: synthesis and SAR of 3-substituted azetidinyl derivatives. Bioorg Med Chem Lett 17:3077–3080
Rahman I, MacNee W (2012) Anti oxidant pharmacological therapies for COPD. Curr Opin Pharmacol 12:256–265
Rieder F, Siegmund B, Bundschuh DS et al (2013) The selective phosphodiesterase 4 inhibitor roflumilast and phosphodiesterase 3/4 inhibitor pumafentrine reduce clinical score and TNF expression in experimental colitis in mice. PLoS One 8:e56867
Rocco PR, Momesso DP, Figueira RC et al (2003) Therapeutic potential of a new phosphodiesterase inhibitor in acute lung injury. Eur Respir J 22:20–27
Saint-Martin F, Dumur JP, Pérez I, Izquierdo I (2004) A randomized, double-blind, parallel-group study, comparing the efficacy and safety of rupatadine (20 and 10 mg), a new PAF and H1 receptor-specific histamine antagonist, to loratadine 10 mg in the treatment of seasonal allergic rhinitis. J Investig Allergol Clin Immunol 14:34–40
Seguin RM, Ferrari N (2009) Emerging oligonucleotide therapies for asthma and chronic obstructive pulmonary disease. Expert Opin Investig Drugs 18:1505–1517
Singh D, Petavy F, Macdonald AJ et al (2010) The inhaled phosphodiesterase 4 inhibitor GSK256066 reduces allergen challenge responses in asthma. Respir Res 11:26
Spiess C, Bevers J III, Jackman J et al (2013) Development of a human IgG4 bispecific antibody for dual targeting of interleukin-4 (IL-4) and interleukin-13 (IL-13) cytokines. J Biol Chem 288:26583–26593
Spina D, Landells LJ, Page CP (1998) The role of theophylline and phosphodiesterase isoenzyme inhibitors as anti-inflammatory drugs. Clin Exp Allergy 28(Suppl 3):24–34
Spinelli A, Fanelli A, Gorini M et al (1991) Control of breathing in patients with chronic pulmonary obstructive disease: response to bamiphylline. Respiration 58:241–248
Stempel DA, Stoloff SW, Carranza Rosenzweig JR et al (2005) Adherence to asthma controller medication regimens. Respir Med 99:1263–1267
Sullivan P, Bekir S, Jaffar Z et al (1994) Anti-inflammatory effects of low-dose oral theophylline in atopic asthma. Lancet 343:1006–1008
Tannheimer SL, Sorensen EA, Haran AC et al (2012) Additive anti-inflammatory effects of beta 2 adrenoceptor agonists or glucocorticosteroid with roflumilast in human peripheral blood mononuclear cells. Pulm Pharmacol Ther 25:178–184
Tannu SA, Renzetti LM, Tare N et al (2010) Dual bronchodilatory and pulmonary anti-inflammatory activity of RO5024118, a novel agonist at vasoactive intestinal peptide VPAC2 receptors. Br J Pharmacol 161:1329–1342
Tapadar SR, Das M, Chaudri AD, Basak S, Mahopatra AR (2014) The effect of acebrofylline vs sustained release theophylline in patients with COPD – A comparative study. J Clin Diagn Res 8(9):MC11–MC14
Toward TJ, Smith N, Broadley KJ (2004) Effect of phosphodiesterase-5 inhibitor, sildenafil (Viagra), in animal models of airways disease. Am J Respir Care Med 169:227–234
Turner DL, Ferrari N, Ford WR et al (2010) TPI 1020, a novel anti-inflammatory, nitric oxide donating compound, potentiates the bronchodilator effects of salbutamol in conscious guinea-pigs. Eur J Pharmacol 641:213–219
van der Molen T, Cazzola M (2012) Beyond lung function in COPD management: effectiveness of LABA/LAMA combination therapy on patient-centred outcomes. Prim Care Respir J 21:101–108
van Mastbergen J, Jolas T, Allegra L, Page CP (2012) The mechanism of action of doxofylline is unrelated to HDAC inhibition, PDE inhibition or adenosine receptor antagonism. Pulm Pharmacol Ther 25:55–61
van Meir H, Kenter GG, Burggraaf J et al (2014) The need for improvement of the treatment of advanced and metastatic cervical cancer, the rationale for combined chemo-immunotherapy. Anticancer Agents Med Chem 14(2):190–203. doi:10.2174/18715206113136660372
Vestbo J, Hurd SS, Agustí AG et al (2013) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187:347–365
Wedzicha JA (2013) Dual PDE3/4 inhibition: a novel approach to airway disease? Lancet Respir Med 1:669–670
Wenzel S, Ind PW, Otulana BA et al (2010) Inhaled pitrakinra, an IL-4/IL-13 antagonist, reduced exacerbations in patients with eosinophilic asthma [abstract]. Eur Respir J 36:P3980
Wenzel S, Ford L, Pearlman D et al (2013) Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med 368:2455–2466
Wielders PL, Ludwig-Sengpiel A, Locantore N et al (2013) A new class of bronchodilator improves lung function in COPD: a trial with GSK961081. Eur Respir J 42:972–981
Yick CY, Zwinderman AH, Kunst PW et al (2013) Transcriptome sequencing (RNA-Seq) of human endobronchial biopsies: asthma versus controls. Eur Respir J 42:662–670
Zheng JP, Wenb FQ, Bai CX, Wan HY, Kang J, Chen P, Yao WJ, Ma LJ, Xia L, Raitieri L, Sardina M, Gao Y, Wang BS, Zhong NS, On Behalf of the PANTHEON Study Group (2014) Twice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trial. Lancet Respir Med 2(3):187–194. doi:10.1016/S2213-2600(13)70286-8
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Page, C., Cazzola, M. (2016). Bifunctional Drugs for the Treatment of Respiratory Diseases. In: Page, C., Barnes, P. (eds) Pharmacology and Therapeutics of Asthma and COPD. Handbook of Experimental Pharmacology, vol 237. Springer, Cham. https://doi.org/10.1007/164_2016_69
Download citation
DOI: https://doi.org/10.1007/164_2016_69
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52173-2
Online ISBN: 978-3-319-52175-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)