Abstract
Genetically engineered bacterial whole-cell biosensors are powerful tools that take advantage of bacterial proteins and pathways to allow for detection of a specific analyte. These biosensors have been employed for a broad range of applications, including the detection of bacterial quorum-sensing molecules (QSMs). Bacterial QSMs are the small molecules bacteria use for population density-dependent communication, a process referred to as quorum sensing (QS). Various research groups have investigated the presence of QSMs, including N-acyl homoserine lactones (AHLs) and autoinducer-2 (AI-2), in physiological samples in attempts to enhance our knowledge of the role of bacteria and QS in disease states. Continued studies in these fields may allow for improved patient care and therapeutics based upon QSMs. Furthermore, bacterial whole-cell biosensors have elucidated the roles of some antibiotics as QS agonists and antagonists.

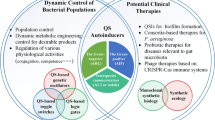
Graphical Abstract
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autoinducer-2 (AI-2)
- Cystic Fibrosis (CF)
- Inflammatory Bowel Disease (IBD)
- N-acyl homoserine lactones (AHLs)
- Quorum-sensing (QS)
- Quorum-sensing molecules (QSMs)
- Urinary Tract Infections (UTI)
- Whole-cell biosensors
1 Introduction
Quorum sensing (QS) is the population-dependent exchange of small chemical signaling molecules that allow bacteria to monitor their population density and regulate gene expression accordingly. The phenomenon was first described in the early 1970s with the microorganism Vibrio harveyi, which employs QS to control the emission of light (bioluminescence) [1, 2]. Traditionally, these signaling molecules have been classified into two subgroups: N-acyl homoserine lactones (AHLs, Fig. 1), which are used by Gram-negative bacteria, and oligopeptides, which are used by Gram-positive bacteria. In recent years, however, it has been found that quorum-sensing molecules (QSMs) are not limited to only these two subgroups, with the discovery of pseudomonas quinolone signal (PQS), autoinducer 2 (AI-2, Fig. 1), and autoinducer 3 (AI-3), among others; interestingly, some of these molecules, such as AI-2, can appear in both Gram-positive and Gram-negative bacteria [3, 4]. QSMs are estimated to influence 4–10 % of the bacterial genome and 20 % of the proteome, regulating myriad genes ranging from factors responsible for bacterial virulence to genes involved in basic metabolic processes [5]. For example, QSMs allow bacteria to communicate with each other to form biofilms, an extracellular matrix system that helps protect the bacteria: most bacteria reside in these three-dimensional matrix systems rather than existing in the planktonic form [6]. In order for bacteria to be able to respond to QSMs, quorum-sensing systems comprise recognition/regulatory proteins that are able to bind to the QSMs and regulate gene expression, as well as synthases which allow for production of QSMs. Table 1 provides examples of quorum-sensing organisms, their regulatory proteins, and QSMs.
Previously, studies on QS and the mechanism of action of the QSMs mostly relied on the native bacteria and examining growth rates and up- or down-regulation of specific genes. Although these methods would give qualitative information about the effects of QSMs on the microorganisms, the amount of quantitative information was limited. With the identification of QS regulatory proteins and their promoter binding regions, genetically engineered whole-cell bacterial biosensors (also called biosensing systems) have emerged as tools for detection of QSMs and understanding of the quorum-sensing mechanism [7]. These biosensing systems generate a detectable response under certain conditions, often times dose-dependent upon recognition of a specific analyte of interest. Whole-cell bacterial biosensors employ bacteria that have been genetically modified to contain a biological recognition agent coupled with a reporter. This genetic modification generally occurs in two ways: insertion of a genetically engineered plasmid and/or modification of the bacterial genome.
Developing a plasmid for use in a biosensing system allows for customization of a sensor depending upon the need, thus there is a large degree of variability. Several key elements that are required and/or commonly employed include genes for: a reporter protein, promoter region, antibiotic resistance, and over expression of the regulatory protein. The reporter plays a large role in the sensitivity of the biosensor, because it is the recognition agent for the assay. The reporter protein(s) selected for bacterial whole-cell biosensors are generally ones that can be detected optically, via an instrument or the naked eye (bioluminescence, chemiluminescence, fluorescence, and colorimetry), or electrochemically. Table 2 contains a list of a few common reporters, along with their detection methods and some advantages and disadvantages. The promoter region determines the production of the reporter protein, as well as playing a role in the specificity and selectivity of the system, thus it should be selected based upon the analyte of interest for the sensor. Including antibiotic resistance under a constitutive promoter allows for easy selection of bacteria expressing the plasmid, thus preventing the loss of plasmid as the bacterial culture grows. Overexpression of a regulatory protein increases the sensor’s ability to detect the analyte of interest: the more protein you have, the higher its chances of encountering the analyte. Once a plasmid has been genetically engineered, it is a relatively simple task to insert the DNA into electro- or chemically competent bacterial cells, thus creating a whole-cell bacterial biosensor.
In addition to genetically engineering a plasmid to employ in a whole-cell biosensor, it is possible to modify the bacterial genome to exploit the original organism itself as a whole-cell biosensor. Many bacterial strains generate QSMs through various synthesis pathways, thus modifications can be made to bacterial genomes to prevent the generation of and/or the response to QSMs. One such example is the V. harveyi strain BB170; native V. harveyi activates its bioluminescence in response to AHLs and AI-2 and can produce these QSMs. The BB170 strain was genetically modified to have its AHL detection pathway, as well as its ability to synthesize AHLs and AI-2, blocked. Thus BB170 was successfully engineered to only generate bioluminescence in response to exogenous AI-2, allowing it to function as a biosensing system.
Regardless of the method used to develop the sensing system, bacterial whole-cell biosensors are categorized into two general types based upon whether expression of the reporter protein is inducible or constitutive. Inducible expression systems employ cells that have been genetically modified to contain an inducible promoter fused to a reporter gene. In the absence of the analyte (inducer), the reporter gene is expressed at low basal levels, determining the “blank” level of the system. When the analyte (inducer) is present, the reporter gene is expressed in a dose-dependent manner within a certain range of concentrations, allowing for a standard curve to serve as a control for sample measurements. Reporter gene expression can be negatively or positively regulated, defined by how the analyte–protein complex interacts with the gene promoter. In negative regulation (Fig. 2a), the regulatory protein is bound to the operator/promoter region, thus preventing reporter and other downstream gene expression. The analyte can bind the regulatory protein, causing the complex to be released from the promoter region and allowing for gene expression to occur. In positive regulation (Fig. 2b), the unbound regulatory protein complexes with the analyte and this complex can then bind to the operator/promoter region to activate reporter gene expression.
Whole-cell-based biosensing system types. a In positive regulation of reporter gene expression, the regulatory protein is bound to the operon, preventing expression of the reporter gene. The analyte enters the cell and binds the regulatory protein, allowing for reporter gene expression. b In negative regulation of reporter gene expression, the analyte enters the cell and binds the regulatory protein. This analyte-regulatory protein complex can bind the operon and allow for expression of the reporter gene. c In constitutive expression, the reporter gene is constantly expressed
In contrast to inducible expression, constitutive expression systems are based upon generation of high basal levels of reporter expression (Fig. 2c). This approach is primarily employed in bacterial whole-cell biosensors as a measure of toxicity: however, nonspecific increased toxicity leads to cell death, reducing the amount of reporter protein and thus the overall signal. Therefore overall toxicity can be recorded, although it does not provide specific information about the nature and mode of action of the toxic agent(s) that is (are) killing the cells.
Bacterial whole-cell biosensors possess several advantages that have increased their popularity in recent years: they are relatively easy and inexpensive to prepare and store, are robust with a tendency to be stable to environmental changes such as pH or temperature fluctuations, can be engineered for multiplexing by using different recognition–reporter pairs, and can be integrated into various platforms allowing for high-throughput or on-site detection. In addition, regulatory proteins may prove difficult to express and purify, thus whole-cell biosensors provide an alternative route to investigating interactions with these proteins. Interestingly, bacterial whole-cell-based biosensors can provide physiologically relevant data and evaluate the bioavailability of the analyte of interest, inasmuch as the target chemical must be ingested by the cells in order to trigger a response. However, this requirement can also prove to be a limitation, as the bacteria rely primarily on diffusion, and thus may lack specific transport channels that may be necessary for the uptake of certain analytes.
2 QSMs in Physiological Samples via Bacterial Whole-Cell-Based Biosensing Systems
2.1 AHL Detection
Studies have shown that bacterial AHLs, such as 3-oxo-dodecanoyl-homserine lactone (3-oxo-C12-HSL), not only regulate bacterial virulence but can also stimulate cells important for inflammation and immune defense in the host [8]. It has been demonstrated that in burn wound mouse models infected with QS deficient bacterial strains, there was no production of mRNA for pro-inflammatory cytokines IL-6, TNFα, CGB, and TGFβ [9]. The opportunistic pathogen Pseudomonas aeruginosa, which employs QS to regulate virulence factor production and biofilm formation, plays an important role in chronic wounds, which are a large burden to the health system worldwide; P. aeruginosa is estimated to be present in up to 80 % of chronic wound cases. In addition, when P. aeruginosa is present, wounds are more severe and heal at a slower rate, which is thought to be caused by cell-to-cell communication with gram-positive bacteria, including Staphylococcus aureus [10–12].
The implications of bacteria in a variety of disorders have prompted researchers to investigate the role of QS in certain disease states by detecting QSMs in physiological samples. In an effort to elucidate the roles of QSMs in their natural environments, physico-chemical methods have been devised for their detection, including but not limited to high-performance liquid chromatography (HPLC), reversed phase HPLC mass spectrometry (RP-HPLC-MS), ultra-high-resolution mass spectrometry, and gas chromatography mass spectrometry (GC-MS) [13–15]. Additionally, work by Campagna et al. [16] and May et al. [17] has led to liquid chromatography–tandem mass spectrometry (LC-MS/MS) detection methods for AI-2 and AHLs in biologically relevant samples. Unfortunately, these methods require extensive sample extraction and/or preparation, large amounts of trained technician time, and expensive instrumentation, thus limiting their utility. Therefore we explore some of the findings from utilizing bacterial whole-cell-based biosensors for QSMs in physiological samples. The sensors employed for AHL detection are listed in Table 3. Please note, for the experiments and sensors described in the Table 3, short chain AHLs refer to AHLs with carbon chains of seven or less carbons, whereas long-chain AHLs refer to AHLs with carbon chains of eight or more carbons.
2.1.1 Cystic Fibrosis (CF)
Cystic fibrosis (CF) is an autosomal recessive genetic disorder that primarily affects the lungs, as well as the pancreas, liver, and intestine. Common symptoms include infertility, poor growth, sinus infections, and lung infections that lead to difficulty breathing. Although a large number of bacteria have been indicated to play a role in CF, the pathogenesis has yet to be fully elucidated [18]. Studies have shown that P. aeruginosa forms thick biofilms within the lungs of CF patients and uses QS extensively to modulate both biofilm formation and maturation [19, 20]. Of these bacteria, P. aeruginosa and Burkholderia cepacia, which are known to colonize the lungs of CF patients, both use AHL-dependent QS regulation [21].
In a study by Middleton et al. [22], sputum samples were collected from stable CF patients, extracted, and then analyzed by employing two E. coli whole-cell-based sensors bearing plasmids pSB401 and pSB1075, to detect short- and long-chain AHLs, respectively. For sputum samples colonized with P. aeruginosa, 71 % contained short-chain AHLs and 61 % contained long-chain AHLs (n = 42). Correspondingly, for sputum samples colonized with B. cepacia, 87 % contained short-chain AHLs and 50 % contained long-chain AHLs (n = 8). Another study published the same year by Erickson et al. [23] further confirmed the presence of AHLs in sputum samples from CF patients. Whole-cell sensors based on P. aeruginosa carrying plasmids pECP61.5 and pKDT17 were utilized to detect short- and long-chain AHLs, respectively. Short-chain AHLs were found in 26 % of the patient sputum samples and long-chain AHLs were found in 78 % of the samples (n = 29). This finding is in contrast to the results of Middleton et al. [22], however there are several possible explanations: small numbers of different patients were assessed, different sample processing/extraction methods were used, and different sensing systems, both the bacterial strains and the plasmids employed, were used. Unfortunately, the small number of patients assayed, the variability of the patient disease status, and the lack of an established range of AHLs in sputum, do not allow for conclusions to be drawn on how and if AHL levels fluctuate in CF patient samples.
These works were followed by Chambers et al. [24], which focused on identifying a broad range of AHLs within mucopurulent respiratory secretions from CF patients undergoing lung transplantation. Agrobacterium tumefaciens-based whole-cell sensor A136 was employed, which contains dual plasmids pCF218 and pMV26, allowing for detection of both short- and long-chain AHLs. Mucopurulent material was extracted, separated by reversed-phase fast pressure liquid chromatography (FPLC), and then analyzed by sensor A136. By combining the whole-cell-based sensor with FPLC, AHLs were found in 69 % of patient samples, with seven unique AHLs being identified. These studies have helped to establish bacterial whole-cell-based biosensors as important tools for QSM detection, as well as have provided researchers a focal point for further discoveries to improve the lives and care of patients with CF.
2.1.2 Inflammatory Bowel Disease (IBD)
IBD is an autoimmune disorder that is characterized by a group of chronic inflammatory conditions of the gastrointestinal tract (GI), commonly causing severe abdominal pain, vomiting, diarrhea, rectal bleeding, and weight loss. IBD can be further classified based upon the symptoms and the extent of the inflammation within the GI tract, with Crohn’s and Ulcerative Colitis being the two principal types. IBD is thought to be caused in genetically predisposed individuals by an overly aggressive immune response to commensal bacteria [25], thus research in this field has focused on the gut microbiome. The human gut is host to a broad range of bacteria, and although QS has been demonstrated for a limited number of intestinal bacteria, mainly pathogens, it is likely that a wide variety of enteric microorganisms, including commensal bacteria, communicate with each other and the host by means of QSMs.
Studies have shown that the bacteria of the gut play a role in IBD etiology, thus investigating QSMs in individuals may grant a greater understanding of the disease. To this end, work by Kumari et al. [15, 26] has led to the development and optimization of E. coli based whole-cell sensing systems, bearing plasmids pSB406 and pSB1075 [27], for quantitative detection of short- and long-chain AHLs (Fig. 3a, b), respectively, in human samples such as saliva and stool. By focusing on saliva and stool samples, this allows for a detection method that is completely non-invasive to patients. It is important to note that these methods do not require sample extraction or extensive sample preparation; simple centrifugation or dilution in water is all that is necessary to prepare samples. Additionally, these optimized systems allow for nanomolar limits of detection in physiological matrices, which makes these systems relevant, due to nanomolar levels of QSMs being necessary to initiate cellular communication [7]. Saliva from IBD and healthy individuals were assayed, revealing greatly varying levels of AHLs across individuals that were consistent for each individual for a period of time. Furthermore, stool samples from newborns admitted to a Neonatal Intensive Care Unit (NICU) also contained varying levels of AHLs. These results revealed for the first time that QSMs can be detected in human saliva and stool. These findings are of added interest, because it is well known that QSMs such as AHLs are subject to degradation by environmental factors, such as pH and temperature, and may be degraded by enzymes present in the gut [28, 29]. If a correlation can be established between the health of individuals and the levels of QSMs found in their samples, QSMs may develop into a biomarker for IBD, as well as other bacterial disorders. Current studies in the Daunert laboratory are in progress in which physiological samples from IBD patients, as well as matched controls, are being analyzed for their QSM levels, in order to investigate such correlation with disease status.
Dose response curves generated for N-hexanoyl-DL-homoserine lactone (red) and N-dodecanoyl-DL-homoserine lactone (blue) on E. coli whole-cell-based biosensor harboring plasmid a pSB406 or b pSB1075, indicating the selectivity of each sensor for short or long chain AHLs (adapted from Kumari et al. [26]). c Dose response curves of AI-2 generated in water (black), 1:100 (v/v) diluted saliva (red), and 1:750 (w/v) stool (blue) with the V. harveyi BB170 sensor, indicating optimized sample dilutions for use with the sensor. d Saliva from IBD patients (red) and healthy controls (blue) were then diluted and assayed with the sensor, n = 3 (adapted from Raut et al. [30])
2.1.3 Hospital-Acquired Urinary Tract Infections (UTI)
Nosocomial infections (NI), commonly known as hospital-acquired infections, include multiple types of fungal and bacterial infections that are aggravated by the weakened resistance of patients. With P. aeruginosa known as a common link among many types of NI, multiple groups have worked to characterize the AHL profile of this microorganism during infection [31–33]. Gupta et al. examined the role of QSMs for their ability to induce pro- and anti-inflammatory renal cytokines and inflammation in an experimental urinary tract infection (UTI) model [34]. Their results suggested that deficiency for production of QSMs in mutant strains of P. aeruginosa resulted in non-stimulation of a pro-inflammatory response. Kumar et al. [31] employed sensors pKDT17, A136, CV026, and pECP61.5 to detect a broad range of AHLs: long-chain, both long- and short-chain, short-chain, and short-chain, respectively. Analysis of P. aeruginosa isolates from catheter-associated UTI found AHL molecules of varying types in all samples, indicating that the virulence factors activated may vary between UTIs. These findings were verified in work by Lakshmana Gowda et al. [33], who applied sensors pKDT17 and A136, not only to UTI isolates, but to other nosocomial infection P. aeruginosa isolates as well. However, work by Senturk et al. [32], which utilized sensors CV026 and VIR07 for detection of short- and long-chain AHLs, respectively, revealed another side to P. aeruginosa infection; although the diversity of AHLs seen previously was detected in most UTI isolates, 7 % contained no detectable levels of AHLs. Sequence analysis revealed mutations within genes crucial to the AHL pathway; lasI, lasR, rhlR, and rhlI. The authors hypothesized that these findings signify that P. aeruginosa possess additional virulence pathways that are independent of AHLs. Continued analysis of QSM levels in UTI isolates may help to elucidate the mechanism of P. aeruginosa infection, allowing for greater patient care and treatment.
2.1.4 Paper Strip Detection of Quorum-Sensing Molecules
The previously mentioned research on AHL detection has been focused on assays performed in the laboratory, however, when developing sensors that may have relevance for diagnostics or environmental detection, it is important to utilize a type of sensor and detection method which can be portable, that is, applied in a bedside or field kit. Whole-cell biosensors are ideal candidates due to their ability to withstand a range of environmental conditions, requirement of minimal or no sample pretreatment, easy and rapid detection, and cost-effectiveness, to name a few [35, 36]. Due to the prevalence of QS in the pathogenesis of bacteria-related disorders, developing a fast, reliable, visual detection method for bacterial signaling molecules is of great interest. Work has been done to sense AHLs visually without instrumentation; however, these methods have shortcomings such as being time-consuming and not allowing detection in a dose-dependent manner [37]. To overcome these shortcomings, Struss et al. [38] designed a whole-cell biosensor that was amenable to paper strip incorporation for the semi-quantitative detection of bacterial quorum-signaling molecules. This whole-cell-based biosensor employed E. coli cells harbouring plasmid pSD908, which detects long-chain AHLs and contains the reporter gene lacZ, encoding β-galactosidase. β-galactosidase activity can be determined using a variety of substrates and, depending on the chosen substrate, detection of the analytical signal can be fluorescent, chemiluminescent, electrochemical, or colorimetric [26]. The E. coli cells harboring plasmid pSD908 were immobilized on the filter-paper-based strips by suspending the cells in a drying protectant solution and applying the suspension directly to filter-paper strips to allow them to dry via a liquid-drying method. This approach was used to help in the long-term preservation of cells. After the cells were dried on the filter-paper strips, they could then be immersed in liquid samples for detection of AHLs. After the sample immersion step, the strips were incubated in an 5-bromo-4-chloro-3-indolyl-β-D-galactoside (X-gal) solution to develop a blue color. The intensity of the blue color increased with an increasing concentration of AHL, thus allowing semi-quantitative naked-eye evaluation (Fig. 4a). The paper strip sensor was employed for detection of AHLs in saliva and AHL levels were found in both healthy and diseased individuals (Fig. 4b), mirroring previous findings and proving the paper strip sensor’s ability to detect AHLs in physiological samples. It is important to note that the assay was also performed at room temperature (RT), which demonstrates the applicability of the system for point-of-care diagnostics and field applications. Additionally, the paper strip sensors were found to be stable for at least three months at 4 °C without loss of analytical characteristics. Thus continued work with this and other bacterial whole-cell-based biosensors may allow for commercially available point-of-care and field tests for QSMs.
a Dose-response data in buffer using filter-paper-based strips. The color intensity increases with increasing concentration of AHL. b Detection of AHLs in healthy patients (1–5) and a patient with Crohn’s Disease (6). Reproduced with copyright permission from Struss et al. [38]
2.2 AI-2 Detection
In recent years, a group of molecules referred to as autoinducer-2 (AI-2) have been found in both Gram-positive and Gram-negative bacteria [39]. This finding is of great importance, as this indicates AI-2 molecules are used for interspecies communication. The production of these molecules from their common precursor, 4,5-dihydroxy-2,3-pentanedione (DPD), is catalyzed by the LuxS enzyme. In the organism V. harveyi, the AI-2 diffuses out of and into the cell and binds to a periplasmic binding protein, LuxP. This binding event starts a cascade of phosphorylation/dephosphorylation events and leads to the expression of luciferase for the production of light [40].
2.2.1 Inflammatory Bowel Disease (IBD)
As mentioned previously, AHLs are currently being investigated as a potential biomarker for IBD. As part of this research, Kumari et al. [26] and Raut et al. [30] hypothesized that monitoring the QSMs in physiological samples over time can give an idea of the amount of bacteria present, inflammation, and the progress of the disease. Specifically, as part of determining QSM profiles in patients, the interspecies communication molecule AI-2, which encompasses both Gram-negative and Gram-positive bacteria, could prove an ideal non-invasive biomarker for gastrointestinal disease.
Vibrio harveyi strain BB170 has been genetically modified to respond only to AI-2. Previously, this strain had only been used as a bioassay to screen cell cultures and identify bacteria able to produce AI-2. Raut et al. [30] developed and optimized a biosensing system based on V. harveyi BB170 and applied it for the quantitative detection of AI-2 in saliva, stool, and intestinal samples from IBD patients (Fig. 3c, d). As with their previous AHL research, a focus was placed on developing a non-invasive assay that did not require extensive sample preparation or extraction. With a similar process of simple centrifugation and dilution of samples in water, stool and saliva samples could be assayed for AI-2. Stool samples from IBD patients were then analyzed and found to exhibit considerably varied levels of AI-2. The authors hypothesized that these variations may reflect perturbations in the microflora of the inflamed intestines [41, 42]. AI-2 was also detectable in saliva samples from IBD patients via the BB170 biosensor in nanomolar concentrations, which correlates well with the levels of AI-2 previously detected in human saliva via LC-MS/MS (244-965 nM) [16]. Thus continued work with the universal signaling molecule AI-2 may help us better understand and diagnose IBD.
3 Quorum-Sensing Agonists and Antagonists
As our knowledge of QSMs and their potential roles as biomarkers of disease states has expanded, interest has focused on molecules that interfere with the quorum-sensing network, either by acting as agonists or antagonists [43]. By blocking or mimicking the native quorum-sensing molecule’s signal, more insight can be gained in the quorum-sensing molecular mechanism and it may be possible to interfere effectively with QS and modify the behavior of bacteria. These studies typically demonstrated that compounds analogous to the cognate quorum-sensing molecule (i.e. having a lactone ring but varying tail lengths, oxidation states, or saturation levels) induced weak to moderate gene expression [44]. Whole-cell biosensors have proven to be valuable tools to elucidate effects of structurally similar and dissimilar molecules on QS.
3.1 Antibiotics
Antibiotics are employed all over the world for the treatment and prevention of bacterial infection, however, their mechanisms of action are not fully elucidated. To this end, researchers have investigated the effects of antibiotics on QS pathways. Previous reports demonstrate that the antibiotic azithromycin was able to interfere with the regulation of the quorum-sensing network of P. aeruginosa, inhibiting virulence factors and biofilm formation [45]. These studies, however, only investigated the behavior changes of the native cells, such as motility and biofilm formation, but did little to investigate the mechanism of action of the antibiotic on the quorum-sensing system. To better understand how antibiotics are able to interact with the quorum-sensing network and screen for antibiotics that are able to interfere with QS, Struss et al. employed E. coli whole-cell biosensors harboring plasmids pSB406 and pSB1075 for the detection of short- and long-chain AHLs, respectively [26, 46]. The authors investigated three antibiotics that were commonly used in the treatment of IBD: ciprofloxacin, metronidazole, and tinidazole. Azithromycin was used as a control, in addition to exogenous AHL addition, as it has previously been shown to act as a quorum-sensing agonist/antagonist [47–49].
As expected, azithromycin was able to induce a dose-dependent response in both the pSB406- and pSB1075-based whole-cell sensors. Furthermore, this response occurred in both the presence and absence of exogenous cognate AHL. The antibiotics tested were also able to activate the systems in both whole-cell sensors, both in the presence and absence of the cognate AHL; however, the similarly structured tinidazole and metronidazole activated the pSB1075 sensor to a greater extent than the pSB406 system. It is important to note that when the authors performed the studies with the whole-cell biosensor, they normalized all of the results to cell viability. This was to ensure that the changes observed were due to the interaction of the compound with the regulatory protein and not other interactions with the other components in the cells or due to a decrease in signal due to a decrease in the number of live cells. Another important result to note is that the concentrations of antibiotic that initiated an agonistic response were clinically relevant and included the peak plasma concentrations of the antibiotics.
The authors point out that their results are in contrast to previous studies reported for ciprofloxacin [50]. However, the previous studies were performed in P. aeruginosa PAO1 cells whereas the current study was performed using E. coli cells. This is an important demonstration of how whole-cell biosensors can allow studying the effects of molecules on a specific protein/promoter system, and in the native cells the effect could be due to other cell components. This was proven by a study showing that azithromycin did not directly affect the expression of QS-related genes, but decreased AHL production by lowering expression of genes upstream to the synthase ones [45].
Whole-cell biosensors are powerful tools, specifically for quorum-sensing regulatory proteins that are difficult to purify and elucidate the structure. The ligand binding domain (LBD) of LasR was isolated and a crystal structure was solved [51]. A study was performed to screen antibiotics for inhibitory QS activity. Specifically, azithromycin and ciprofloxacin were docked against the LBD of LasR. It was shown that these antibiotics do not bind to the AHL binding site of LasR but rather to a different site [50]. By using a whole-cell biosensor, it was shown that although these molecules may not be binding to the LBD, they still bind in such a way that they can cause a conformational change and allow for LasR binding to its promoter region.
4 Conclusions and Future Perspectives
QS is communication between bacteria that allows for the regulation of genes which control certain behaviors such as formation of biofilms, expression of virulence factors, allows for mobility, and bioluminescence, to name a few. This intricate network of cellular communication is dictated by signaling molecules and their associated regulatory proteins. Although there have been continued efforts to develop QSM sensors using regulatory proteins [52], due to the difficulty to express and purify these regulatory proteins, whole-cell biosensors are important to assist in the understanding of the mechanism of QS. Many QS bacteria are implicated in diseases, therefore the studies we have discussed in this chapter have been performed to understand the QS and how it is involved in the disease state. Diagnosis and treatment of a disease are paramount, however, there are instances that could potentially be prevented altogether with proper methods of detection: annually, approximately 48 million people in the United States experience a foodborne illness, resulting in approximately 3000 deaths and an annual cost of illness estimated between US$51–77 billion [53]. Many of the agents involved in causing food borne illness are bacteria [54], with multiple studies having linked QSMs to food spoilage and activation of virulence factors [55]. By focusing on development and optimization of bacterial whole-cell-based biosensing systems for QSMs in foods, it may prove possible to prevent many cases of illness, as well as provide better diagnosis and treatment of severe cases.
Interspecies communication is a growing field of investigation as it plays an important role in large microbial communities. Work has been completed to detect AHLs in ecosystems where a range of bacteria would be present, such as in soil and the rhizosphere [56, 57]. As previously described, certain autoinducer molecules, such as AI-2, are used for interspecies communication. However, continued investigation of QSMs and QS networks is necessary as some organisms such as Salmonella, Shigella and E. coli cannot synthesize their own AHLs, yet these bacteria are able to communicate with other bacteria. It is hypothesized that this communication is facilitated via a receptor-like protein (SdiA) with amino acid sequences that are homologous to LuxR-type activators [58, 59]. The strain of E. coli, EHEC, which results in acute hemorrhagic diarrhea and can cause hemolytic uremic syndrome, appears to produce a thus far unidentified autoinducer termed AI-3. Clarke et al. identified the E. coli protein QseC that directly binds both AI-3 and epinephrine/norepinephrine [60]. This was one of the first studies demonstrating that mammalian signaling hormones can be detected by bacteria. AI-3 is thought to activate genes that are involved in intestinal colonization. Other organisms that produce AI-3 are Shigella, Salmonella, Klebsiella, Enterobacter and Citrobacter. Little is known about how these molecules interact with various quorum-sensing systems, thus whole-cell biosensors could lend insight about which regulatory proteins are important for this interspecies communication and the mechanism of action of these molecules.
Furthermore, QS has been implicated in interkingdom communication. In a novel 3-D co-culture model of epithelial cells and immune cells (monocytes/macrophages) it could be shown that the epithelial cells degrade the P. aeruginosa QSM 3-oxo-C12-HSL. This protective effect by the epithelial cells is thought to be caused through enzymatic degradation of these QSMs by the epithelial cells [61]. This study demonstrated that QSMs are sensed not only by bacteria, but also by eukaryocytes. Additionally, QSMs have been shown to cause an inflammatory response [8], which make them an attractive target for therapeutic interventions. Thus by continuing to employ bacterial whole-cell-based biosensors, research may be able to elucidate further how our bodies interact with our biome and affect disease.
Research employing bacterial whole-cell biosensors has proved great insight into the quorum-sensing mechanism. With these tools, it is possible to evaluate molecules and determine which chemical characteristics are important to agonize or antagonize quorum-sensing systems. This information will strongly impact the future of treatment for many of the diseases where QS is implicated, as well as broaden our knowledge of bacterial communication.
References
Uroz S, Dessaux Y, Oger P (2009) Quorum sensing and quorum quenching: the yin and yang of bacterial communication. Chembiochem: Eur J Chem Biol 10(2):205–216. doi:10.1002/cbic.200800521
Gonzalez JE, Keshavan ND (2006) Messing with bacterial quorum sensing. Microbiol Mol Biol Rev: MMBR 70(4):859–875. doi:10.1128/MMBR.00002-06
Waters CM, Bassler BL (2005) Quorum sensing: cell-to-cell communication in bacteria. Annu Rev Cell Dev Biol 21:319–346. doi:10.1146/annurev.cellbio.21.012704.131001
Kendall MM, Sperandio V (2014) Cell-to-cell signaling in and. EcoSal Plus 2014. doi:10.1128/ecosalplus.ESP-0002-2013
Sifri CD (2008) Healthcare epidemiology: quorum sensing: bacteria talk sense. Clin Infect Dis: Off Publ Infect Diseases Soc Am 47(8):1070–1076. doi:10.1086/592072
Sanchez CJ Jr, Mende K, Beckius ML, Akers KS, Romano DR, Wenke JC, Murray CK (2013) Biofilm formation by clinical isolates and the implications in chronic infections. BMC Infect Dis 13:47. doi:10.1186/1471-2334-13-47
Raut N, O’Connor G, Pasini P, Daunert S (2012) Engineered cells as biosensing systems in biomedical analysis. Anal Bioanal Chem 402(10):3147–3159. doi:10.1007/s00216-012-5756-6
Cohen TP, D Prince A (2015) Host Immune Evasion. Pseudomonas 3–23. doi:10.1007/978-94-017-9555-5_1
Rumbaugh KP, Hamood AN, Griswold JA (2004) Cytokine induction by the P. aeruginosa quorum sensing system during thermal injury. The Journal of surgical research 116(1):137–144
Gjodsbol K, Christensen JJ, Karlsmark T, Jorgensen B, Klein BM, Krogfelt KA (2006) Multiple bacterial species reside in chronic wounds: a longitudinal study. Int Wound J 3(3):225–231. doi:10.1111/j.1742-481X.2006.00159.x
Kirketerp-Moller K, Jensen PO, Fazli M, Madsen KG, Pedersen J, Moser C, Tolker-Nielsen T, Hoiby N, Givskov M, Bjarnsholt T (2008) Distribution, organization, and ecology of bacteria in chronic wounds. J Clin Microbiol 46(8):2717–2722. doi:10.1128/JCM.00501-08
Dalton T, Dowd SE, Wolcott RD, Sun Y, Watters C, Griswold JA, Rumbaugh KP (2011) An in vivo polymicrobial biofilm wound infection model to study interspecies interactions. PLoS ONE 6(11):e27317. doi:10.1371/journal.pone.0027317
Fekete A, Frommberger M, Rothballer M, Li X, Englmann M, Fekete J, Hartmann A, Eberl L, Schmitt-Kopplin P (2007) Identification of bacterial N-acylhomoserine lactones (AHLs) with a combination of ultra-performance liquid chromatography (UPLC), ultra-high-resolution mass spectrometry, and in-situ biosensors. Anal Bioanal Chem 387(2):455–467. doi:10.1007/s00216-006-0970-8
Struss AK, Nunes A, Waalen J, Lowery CA, Pullanikat P, Denery JR, Conrad DJ, Kaufmann GF, Janda KD (2013) Toward implementation of quorum sensing autoinducers as biomarkers for infectious disease states. Anal Chem 85(6):3355–3362. doi:10.1021/ac400032a
Kumari A, Pasini P, Daunert S (2008) Detection of bacterial quorum sensing N-acyl homoserine lactones in clinical samples. Anal Bioanal Chem 391(5):1619–1627. doi:10.1007/s00216-008-2002-3
Campagna SR, Gooding JR, May AL (2009) Direct quantitation of the quorum sensing signal, autoinducer-2, in clinically relevant samples by liquid chromatography-tandem mass spectrometry. Anal Chem 81(15):6374–6381. doi:10.1021/ac900824j
May AL, Eisenhauer ME, Coulston KS, Campagna SR (2012) Detection and quantitation of bacterial acylhomoserine lactone quorum sensing molecules via liquid chromatography-isotope dilution tandem mass spectrometry. Anal Chem 84(3):1243–1252. doi:10.1021/ac202636d
Ciofu O, Hansen CR, Hoiby N (2013) Respiratory bacterial infections in cystic fibrosis. Curr Opin Pulm Med 19(3):251–258. doi:10.1097/MCP.0b013e32835f1afc
Roy V, Meyer MT, Smith JA, Gamby S, Sintim HO, Ghodssi R, Bentley WE (2013) AI-2 analogs and antibiotics: a synergistic approach to reduce bacterial biofilms. Appl Microbiol Biotechnol 97(6):2627–2638. doi:10.1007/s00253-012-4404-6
Singh PK, Schaefer AL, Parsek MR, Moninger TO, Welsh MJ, Greenberg EP (2000) Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms. Nature 407(6805):762–764. doi:10.1038/35037627
Bjarnsholt T (2013) The role of bacterial biofilms in chronic infections. APMIS Suppl 136:1–58. doi:10.1111/apm.12099
Middleton B, Rodgers HC, Camara M, Knox AJ, Williams P, Hardman A (2002) Direct detection of N-acylhomoserine lactones in cystic fibrosis sputum. FEMS Microbiol Lett 207(1):1–7
Erickson DL, Endersby R, Kirkham A, Stuber K, Vollman DD, Rabin HR, Mitchell I, Storey DG (2002) Pseudomonas aeruginosa quorum-sensing systems may control virulence factor expression in the lungs of patients with cystic fibrosis. Infect Immun 70(4):1783–1790
Chambers CE, Visser MB, Schwab U, Sokol PA (2005) Identification of N-acylhomoserine lactones in mucopurulent respiratory secretions from cystic fibrosis patients. FEMS Microbiol Lett 244(2):297–304. doi:10.1016/j.femsle.2005.01.055
Sartor RB (2004) Therapeutic manipulation of the enteric microflora in inflammatory bowel diseases: antibiotics, probiotics, and prebiotics. Gastroenterology 126(6):1620–1633
Kumari A, Pasini P, Deo SK, Flomenhoft D, Shashidhar H, Daunert S (2006) Biosensing systems for the detection of bacterial quorum signaling molecules. Anal Chem 78(22):7603–7609. doi:10.1021/ac061421n
Winson MK, Swift S, Fish L, Throup JP, Jorgensen F, Chhabra SR, Bycroft BW, Williams P, Stewart GS (1998) Construction and analysis of luxCDABE-based plasmid sensors for investigating N-acyl homoserine lactone-mediated quorum sensing. FEMS Microbiol Lett 163(2):185–192
Yates EA, Philipp B, Buckley C, Atkinson S, Chhabra SR, Sockett RE, Goldner M, Dessaux Y, Camara M, Smith H, Williams P (2002) N-acylhomoserine lactones undergo lactonolysis in a pH-, temperature-, and acyl chain length-dependent manner during growth of Yersinia pseudotuberculosis and Pseudomonas aeruginosa. Infect Immun 70(10):5635–5646
Yang F, Wang LH, Wang J, Dong YH, Hu JY, Zhang LH (2005) Quorum quenching enzyme activity is widely conserved in the sera of mammalian species. FEBS Lett 579(17):3713–3717. doi:10.1016/j.febslet.2005.05.060
Raut N, Pasini P, Daunert S (2013) Deciphering bacterial universal language by detecting the quorum sensing signal, autoinducer-2, with a whole-cell sensing system. Anal Chem 85(20):9604–9609. doi:10.1021/ac401776k
Kumar R, Chhibber S, Gupta V, Harjai K (2011) Screening & profiling of quorum sensing signal molecules in Pseudomonas aeruginosa isolates from catheterized urinary tract infection patients. Ind J Med Res 134:208–213
Senturk S, Ulusoy S, Bosgelmez-Tinaz G, Yagci A (2012) Quorum sensing and virulence of Pseudomonas aeruginosa during urinary tract infections. J Infect Dev Countries 6(6):501–507
Lakshmana Gowda K, John J, Marie MA, Sangeetha G, Bindurani SR (2013) Isolation and characterization of quorum-sensing signalling molecules in Pseudomonas aeruginosa isolates recovered from nosocomial infections. APMIS: Acta Pathol Microbiol Immunol Scand. doi:10.1111/apm.12047
Gupta P, Gupta RK, Harjai K (2013) Quorum sensing signal molecules produced by Pseudomonas aeruginosa cause inflammation and escape host factors in murine model of urinary tract infection. Inflammation 36(5):1153–1159. doi:10.1007/s10753-013-9650-y
Daunert S, Barrett G, Feliciano JS, Shetty RS, Shrestha S, Smith-Spencer W (2000) Genetically engineered whole-cell sensing systems: coupling biological recognition with reporter genes. Chem Rev 100(7):2705–2738
Feliciano JP, Deo P, Daunert, S (2006) Photoproteins as reporters in whole-cell sensing. Wiley-VCH Verlag GmbH & Co KGaA 131–154
Yong YC, Zhong JJ (2009) A genetically engineered whole-cell pigment-based bacterial biosensing system for quantification of N-butyryl homoserine lactone quorum sensing signal. Biosens Bioelectron 25(1):41–47. doi:10.1016/j.bios.2009.06.010
Struss A, Pasini P, Ensor CM, Raut N, Daunert S (2010) Paper strip whole cell biosensors: a portable test for the semiquantitative detection of bacterial quorum signaling molecules. Anal Chem 82(11):4457–4463. doi:10.1021/ac100231a
Miller MB, Bassler BL (2001) Quorum sensing in bacteria. Annu Rev Microbiol 55:165–199. doi:10.1146/annurev.micro.55.1.165
Federle MJ (2009) Autoinducer-2-based chemical communication in bacteria: complexities of interspecies signaling. Contrib Microbiol 16:18–32. doi:10.1159/000219371
Manichanh C, Rigottier-Gois L, Bonnaud E, Gloux K, Pelletier E, Frangeul L, Nalin R, Jarrin C, Chardon P, Marteau P, Roca J, Dore J (2006) Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut 55(2):205–211. doi:10.1136/gut.2005.073817
Baumgart M, Dogan B, Rishniw M, Weitzman G, Bosworth B, Yantiss R, Orsi RH, Wiedmann M, McDonough P, Kim SG, Berg D, Schukken Y, Scherl E, Simpson KW (2007) Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn’s disease involving the ileum. ISME J 1(5):403–418. doi:10.1038/ismej.2007.52
Swift S, Throup JP, Williams P, Salmond GP, Stewart GS (1996) Quorum sensing: a population-density component in the determination of bacterial phenotype. Trends Biochem Sci 21(6):214–219
Reverchon S, Chantegrel B, Deshayes C, Doutheau A, Cotte-Pattat N (2002) New synthetic analogues of N-acyl homoserine lactones as agonists or antagonists of transcriptional regulators involved in bacterial quorum sensing. Bioorg Med Chem Lett 12(8):1153–1157
Kai T, Tateda K, Kimura S, Ishii Y, Ito H, Yoshida H, Kimura T, Yamaguchi K (2009) A low concentration of azithromycin inhibits the mRNA expression of N-acyl homoserine lactone synthesis enzymes, upstream of lasI or rhlI, in Pseudomonas aeruginosa. Pulm Pharmacol Ther 22(6):483–486. doi:10.1016/j.pupt.2009.04.004
Struss AK, Pasini P, Flomenhoft D, Shashidhar H, Daunert S (2012) Investigating the effect of antibiotics on quorum sensing with whole-cell biosensing systems. Anal Bioanal Chem 402(10):3227–3236. doi:10.1007/s00216-012-5710-7
Gillis RJ, Iglewski BH (2004) Azithromycin retards Pseudomonas aeruginosa biofilm formation. J Clin Microbiol 42(12):5842–5845. doi:10.1128/JCM.42.12.5842-5845.2004
Nalca Y, Jansch L, Bredenbruch F, Geffers, R, Buer J, Haussler S (2006) Quorum-Sensing Antagonistic Activities of Azithromycin in Pseudomonas aeruginosa PAO1: a Global Approach. Antimicrob. Agents Chemother 50:1680–1668
Bala A, Kumar R, Harjai K (2011) Inhibition of quorum sensing in Pseudomonas aeruginosa by azithromycin and its effectiveness in urinary tract infections. J Med Microbiol 60(Pt 3):300–306. doi:10.1099/jmm.0.025387-0
Skindersoe ME, Alhede M, Phipps R, Yang L, Jensen PO, Rasmussen TB, Bjarnsholt T, Tolker-Nielsen T, Hoiby N, Givskov M (2008) Effects of antibiotics on quorum sensing in Pseudomonas aeruginosa. Antimicrob Agents Chemother 52(10):3648–3663. doi:10.1128/AAC.01230-07
Bottomley MJ, Muraglia E, Bazzo R, Carfi A (2007) Molecular insights into quorum sensing in the human pathogen Pseudomonas aeruginosa from the structure of the virulence regulator LasR bound to its autoinducer. J Biol Chem 282(18):13592–13600. doi:10.1074/jbc.M700556200
Raut N, Joel S, Pasini P, Daunert S (2015) Bacterial autoinducer-2 detection via an engineered quorum sensing protein. Anal Chem 87(5):2608–2614. doi:10.1021/ac504172f
Scharff RL (2012) Economic burden from health losses due to foodborne illness in the United States. J Food Prot 75(1):123–131. doi:10.4315/0362-028X.JFP-11-058
Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM (2011) Foodborne illness acquired in the United States–unspecified agents. Emerg Infect Dis 17(1):16–22. doi:10.3201/eid1701.091101p2
Skandamis PN, Nychas GJ (2012) Quorum sensing in the context of food microbiology. Appl Environ Microbiol 78(16):5473–5482. doi:10.1128/AEM.00468-12
DeAngelis KM, Firestone MK, Lindow SE (2007) Sensitive whole-cell biosensor suitable for detecting a variety of N-acyl homoserine lactones in intact rhizosphere microbial communities. Appl Environ Microbiol 73(11):3724–3727. doi:10.1128/AEM.02187-06
Burmolle M, Hansen LH, Sorensen SJ (2005) Use of a whole-cell biosensor and flow cytometry to detect AHL production by an indigenous soil community during decomposition of litter. Microb Ecol 50(2):221–229. doi:10.1007/s00248-004-0113-8
Michael B, Smith JN, Swift S, Heffron F, Ahmer BM (2001) SdiA of Salmonella enterica is a LuxR homolog that detects mixed microbial communities. J Bacteriol 183(19):5733–5742. doi:10.1128/JB.183.19.5733-5742.2001
Smith JN, Ahmer BM (2003) Detection of other microbial species by Salmonella: expression of the SdiA regulon. J Bacteriol 185(4):1357–1366
Clarke MB, Hughes DT, Zhu C, Boedeker EC, Sperandio V (2006) The QseC sensor kinase: a bacterial adrenergic receptor. Proc Natl Acad Sci USA 103(27):10420–10425. doi:10.1073/pnas.0604343103
Crabbe A, Sarker SF, Van Houdt R, Ott CM, Leys N, Cornelis P, Nickerson CA (2011) Alveolar epithelium protects macrophages from quorum sensing-induced cytotoxicity in a three-dimensional co-culture model. Cell Microbiol 13(3):469–481. doi:10.1111/j.1462-5822.2010.01548.x
Acknowledgments
This work was supported in part by grants from the National Science Foundation, the Broad Foundation, Broad Medical Research Program, National Institute of Hometown Security, the Children’s Miracle Network, and the Department of Defense. S.D. is grateful for support from the Lucille P. Markey Chair in Biochemistry and Molecular Biology of the Miller School of Medicine of the University of Miami.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
O’Connor, G., Knecht, L.D., Salgado, N., Strobel, S., Pasini, P., Daunert, S. (2015). Whole-Cell Biosensors as Tools for the Detection of Quorum-Sensing Molecules: Uses in Diagnostics and the Investigation of the Quorum-Sensing Mechanism. In: Thouand, G., Marks, R. (eds) Bioluminescence: Fundamentals and Applications in Biotechnology - Volume 3. Advances in Biochemical Engineering/Biotechnology, vol 154. Springer, Cham. https://doi.org/10.1007/10_2015_337
Download citation
DOI: https://doi.org/10.1007/10_2015_337
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-27405-8
Online ISBN: 978-3-319-27407-2
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)