Abstract
The focus on drug delivery for the pediatric population has been steadily increasing in the last decades. In terms of developing in vitro models simulating characteristics of the targeted pediatric population, with the purpose of predicting drug product performance after oral administration, it is important to simulate the gastro-intestinal conditions and processes the drug will encounter upon oral administration. When a drug is administered in the fed state, which is commonly the case for neonates, as they are typically fed every 3 h, the digestion of the milk will affect the composition of the fluid available for drug dissolution/solubilization. Therefore, in order to predict the solubilized amount of drug available for absorption, an in vitro model simulating digestion in the gastro-intestinal tract should be utilized. In order to simulate the digestion process and the drug solubilization taking place in vivo, the following aspects should be considered; physiologically relevant media, media volume, use of physiological enzymes in proper amounts, as well as correct pH and addition of relevant co-factors, e.g., bile salts and co-enzymes. Furthermore, physiological transit times and appropriate mixing should be considered and mimicked as close as possible. This paper presents a literature review on physiological factors relevant for digestion and drug solubilization in neonates. Based on the available literature data, a novel in vitro digestion model simulating digestion and drug solubilization in the neonate and young infant pediatric population (2 months old and younger) was designed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
During the past decades, the focus on drug delivery for the pediatric population has increased considerably (1). As an outcome of the increased focus created by the pediatric community in collaboration with pediatric organizations, regulatory agencies and the government, specific guidelines and requirements on children’s medicine was introduced by both the United States Food and Drug Administration (FDA) and the European Medicines Agency (EMA) in the mid 1990s (2–8). The key objectives of these regulations are to ensure high-quality information about medicines administered to children, as well as high-quality research into the development of medicines for children (9). As a direct result, the development plan of any new medicinal product must include an initial Pediatric Study Plan (iPSP) in the US and a Pediatric Investigation Plan (PIP) in the EU (2,10). The iPSP and the PIP emphasize a developmental plan including timing of studies in clinical, non-clinical, and technical aspects. It contains details of the measures planned to demonstrate quality, safety, and efficacy in the entire pediatric population (birth to adolescents) (2). In addition, organizations like the European Paediatric Formulation Initiative (EUPFI) assist the pediatric formulation development by creating knowledge repositories and promoting dialogue through their website, organizing conferences, and writing reflection papers (11–13).
With respect to the pediatric population, as well as the adult population, the oral route is commonly preferred due to convenience and compliance aspects (2). During the early stages of drug development, in vitro models are widely used to forecast the oral drug performance and identify compounds and drug delivery systems displaying unfavorable absorption profiles (14–16). To facilitate in vitro–in vivo correlations (IVIVC), the in vitro models should reflect the complex human gastro-intestinal (GI) tract in terms of, e.g., fluid composition and volumes, hydrodynamics, presence of enzymes and transit times. Presently, a large number of different in vitro models are utilized to predict the oral drug performance estimating one or more of the critical factors, including tablet disintegration, dissolution, drug solubilization, digestion of excipients, and drug absorption. These models vary greatly in complexity including, e.g., relatively simple dissolution models, as well as multifaceted combined dissolution-absorption models (14,17–19). In order not to overcomplicate the models, the general concept is to simulate the rate limiting processes to absorption. As this process is drug and drug delivery system specific, the use of diverse in vitro models is justified. In the case of poorly water-soluble drugs (BCS class II), presently constituting the vast majority of drugs in development, dissolution and solubilization are generally considered rate limiting to drug absorption (16). However, if the drug is administrated in the presence of food, the type of food and GI digestion of this food will presumable also affect the drug solubilization.
Most established in vitro models have been designed to simulate the specific processes taking place within an adult human. However, as pediatric patients are different from adults in many aspects, including physiology, feeding and sleep patterns, as well as diet, an in vitro model developed to simulate the adult human will not accurately reflect processes occurring in neonates, infants, or children (13,20,21). The aim of the present study is to develop an in vitro digestion model simulating the digestion in the pediatric GI tract, in order to predict the in vivo performance of drugs and drug delivery systems administered orally to the pediatric patient. In order to do so, it was essential to gather existing information of the physiology and GI fluid composition of the pediatric patients during a feeding cycle, i.e., in the fasted (3 h postprandial) and the fed state. Furthermore, it was relevant to define the differences between the pediatric patient groups and the adult patient group with focus on aspects important for digestion and drug solubilization and absorption. Based on a thorough literature review, it was possible to design physiologically relevant simulated pediatric gastric and intestinal fluids. A full in vitro digestion model setup was suggested, including relevant enzyme levels, fluid volumes, and transfer rates. The in vitro model was designed to mimic the GI tract of neonates defined as preterm and term newborns at the age from birth to 2 months.
METHOD
The search for relevant publications was conducted using EMBASE and PubMed. Additional articles were found as references in the initial search. In the present study, three segments of the pediatric population were considered, i.e., neonates aged from 0 to 1 months, infants from 1 to 12 months, and children from 12 months to 16 years; however, as limited data was available for older infants and children, the focus was placed on the 0–2-month-old neonate and young infant population, which will be referred to as neonates for brevity throughout the manuscript. Only results obtained of healthy (pre- and full-term) individuals were included. The suggested in vitro digestion model was designed to mimic the neonate population.
RESULTS AND DISCUSSION
Drug Solubilization and Absorption Processes in the Human GI Tract
The rate and extent of drug absorption are governed by the physicochemical characteristics of the drug substance, drug delivery system properties, as well as the nutritional state, and a number of physiological factors (22,23). As many physiological factors are altered with growth and maturation (age), drug absorption after oral administration must also be altered with age (21). In the next sections, age specific information regarding the following physiological factors are described: gastric and intestinal transit rates, GI fluid volumes and composition including pH, osmolality, bile salts (BSs), and digestive enzymes.
GI Transit
Upon oral administration, a given drug needs to dissolve and be absorbed across the intestinal barrier to reach the systemic circulation. The time available for these processes to occur is defined by the gastric emptying (GE) and the intestinal transit time. Whereas the intestinal transit time is considered to be fairly constant, the GE is affected by several factors including the type of drug delivery system administrated and the prandial state (24,25). In relation to the prandial state, it is worth mentioning that the diet and feeding pattern of neonates and infants are very different from that of children and adults, consisting solely of milk and/or infant formula typically being fed every third hour.
Gastric Emptying
Aside from affecting the rate at which a drug is presented to the small intestinal mucosa for absorption, the GE affects the time a meal is exposed to the various digestive enzymes in the stomach which, e.g., affects the amount of triglycerides hydrolyzed by the human gastric lipase (HGL) (26). Furthermore, it determines the necessary duration of a fast for a particular pediatric group in order to be considered in a fasted state.
During the last 40 years, the GE of neonates, infants, and children has been studied by several research groups (24, 27–34). The studies have been conducted using various analytical techniques, as well as in the fasted and various types of fed state. For example, Cavell et al. (1981) studied the GE of breast milk and infant formula in full-term neonates and infants (aged 4 weeks to 6 months) using a marker dilution technique with polyethylene glycol as an inert marker. The results showed a significant difference in the gastric half-emptying time (GHET) after administration of equal volumes of breast milk compared to infant formula, with GHET values of 48 ± 15 min, and 78 ± 14 min, respectively (29). Ewer et al. (1994) studied 14 preterm (mean GA 33 weeks) neonates with a mean age of 11 days (4–26 days); they performed a total of 46 ultrasound measurements with the antral cross sectional area imaged continuously after a feed consisting of 21 mL/kg expressed breast milk or infant formula. Investigating the effect of the type of feed administrated, they found a similar result to Cavell et al. (1981), a significantly shorter GHET in neonates receiving breast milk compared to infants receiving infant formula (28). Bode et al. (2004) measured the GE in 10 preterm neonates (mean gestational age (GA) 29 weeks) fed expressed breast milk by a nasogastric tube. The neonates were imaged using scintigraphy before, at 0, 15, 30, 45, and 60 min after the test meal, and thereafter hourly until 12 h. Gastric activity was measured until residual contents were less than 10%. The results proposed a median GHET of 1.0 h (range 0.5–3.0 h) (27). Signer et al. (1975) investigated the gastric patterns of 28 neonates (25 full-term and three preterm), fed adapted cow’s milk formula, using a radio-isotopic method. They observed two different gastric emptying patterns: a monophasic exponential pattern observed in 24 out of 28 neonates with a GHET of 87 min ± 29 min (SD) and a biphasic pattern consisting of an initial phase with retention of gastric contents followed by an exponential phase observed in 4 out of 28 neonates. The initial retention phase in the biphasic pattern resulted in very long half-lives (32). Cavell (1979) also reported that the GE of breast milk followed a biphasic emptying pattern (35); however, most studies support the monophasic exponential pattern (24,28,34,36). Also, supporting the later pattern, Armand et al. (1996) measured the gastric volume after administration of a meal, in 28 neonates fed either breast milk or infant formula (same volume and similar nutrient composition). The gastric volumes determined by Armand et al. (1996) are depicted in Fig. 1, where the volume at time zero resembles the feeding volume (24). The measurements were done by gastric aspiration into a syringe. The figure illustrates the exponential emptying pattern described above. Figure 2 shows the average values of the GHET in neonates following a feed of either breast milk or infant formula (22–33 mL/kg bodyweight) found in the literature (27–35,37,38). The figure illustrates the significant difference in GHET caused by a difference in the type of diet (breast milk vs infant formula), described by several studies (28,29,33,38). The overall mean GHET were 0.7 ± 0.2 h and 1.0 ± 0.4 h, for breast milk and infant formula, respectively.
Gastric volume as a function of time after feed. Data from Armand et al. (1996) (24)
Small Intestinal Transit Time
In general, very few studies concerning the small intestinal transit in pediatric patients were found. Specifically, no research studies were found stating the intestinal transit time in neonates and infants; however, in other reviews, it has been stated that the intestinal transit time of full-term infants are comparable to adults (approximately 4 h), whereas that of preterm infants generally is considered four times longer (20,39).
GI Fluids
The volume and composition of the fluids present in the GI tract is the main determinants for the dissolution of orally administrated drugs as they will determine the soluble dose.
GI Fluid Volume
The available volume for drug dissolution present in the stomach and small intestine is governed by the GI resting fluid volumes, fluid secretion and absorption, as well as the liquid volume administrated with the drug, i.e., as part of the drug delivery system or food and drinks taken with the medicine. For neonates and infants, orally administrated drugs are commonly given with breast milk or infant formula or in between a meal (fasted for up to 3 h).
Fasted State Gastric Volume
The fasted state GI fluid volumes have only been estimated in a few studies, though many studies have been conducted with fluid being aspirated from the stomach and duodenum of neonates and infants, in order to measure, e.g., pH, BS levels, or enzyme activity (25,26,34,40–45). In 1951, Thompson passed a sterile catheter into the stomach of 154 unfed newborn neonates and aspirated the gastric fluid to determine its volume and acidity (46). A mean volume of 2.65 ± 2.05 mL was recorded, with no relation between birth weight (range 2.0–4.8 kg) and the recorded volume of the gastric contents (46). Widstrom et al. (1988) also investigated the fasting gastric volume in newborn full-term neonates immediately after birth (n = 25). They reported a median fasting gastric volume of 4 mL (range 0–11 mL) (40). Pooling the data from available studies (n = 189), the mean fasted state gastric volume in neonates is 2.9 ± 0.3 mL (34,40,46,47).
Gastric Secretions
The feeding volume will clearly have the biggest impact on the fed state gastric volume; however, the volume of gastric secretions should be incorporated in the total volume as it has been shown to have a significant contribution (34). In a study by Roman et al. (2007), it was shown that the gastric secretion contribution to the total volume was 32, 28, and 43% v/v at time point 30, 60, and 90 min postprandial, respectively (34). The results were obtained from gastric aspirates comparing the residual meal and the total gastric volume, with the volume of the residual meal indirectly determined from the GHET found using total fatty acids as markers (34). Cavell (1983) reported that gastric secretions during the first hour postprandial were 2.0 ± 1.4 mL/kg body weight (mean ± SD) (42). Somewhat conflicting these results, Siegel et al. (1982) reported that secretions only have a small contribution to the overall gastric volume, approximately 1 mL or less per kg bodyweight within 30-min postprandial (48).
Feeding Volume
The feeding volume has been reported in various studies, with some variation (range 14.5–33.0 mL/kg body weight). Based on 13 different studies corresponding to 176 neonates, the mean feeding volume, disregarding type of food (breast milk of infant formula) and GA at birth, neither of which was shown to affect the administrated volume, was 23.5 ± 4.2 mL/kg body weight (24,27–32,34,41,47–49).
pH
The GI pH is very important in relation to drug ionization affecting drug release, solubility, and absorption. Furthermore, it affects drug stability as well as the activity of various digestive enzymes, e.g., HGL (47,50). The pH of the pediatric GI tract has been measured in a series of studies using various techniques, i.e., gastric aspirates (25,26,34,40–43), intestinal aspirates (44,45), intragastric monitoring using a pH probe (31, 47), and a pH-sensitive capsule (51). Figure 3 displays the mean pH values measured in the stomach and small intestine of the neonate pediatric population, in the fasted state (measured just before a feeding) and fed state (measured within 30 min after a feeding), respectively.
Gastric pH
At birth, the gastric pH has been reported to be ∼7 caused by the presence of amniotic fluid which has a pH of 9.2 (40). Within a few hours after birth, the gastric pH value is seen to drop to approximately 1.5–3 as the amniotic fluid is emptied from the stomach. After the quite steep pH drop, the pH increases again as an effect of feeding (20,39).
As for adults, the gastric pH follows a characteristic pattern during a feeding cycle; when food enters the stomach, the pH is increased followed by a gradual decrease caused by secretion of gastric acid (25,31). Figure 4 shows a gastric pH profile obtained during a 4-h feeding cycle (25). The study was conducted with 25 healthy, full-term neonates aged 5–13 days and breast fed at 4 h intervals. The pH values were measured from gastric aspirate using narrow-range pH meter paper. The study reported variability in the rate of gastric emptying intra-, as well as inter-infants. The pH of gastric aspirates was measured over 240 min. The fasting pH value was 3.5 ± 1.0, whereas the fed state pH value was 6.4 ± 0.6 (30 min after a feeding) (25).
Continuous pH measurements in infants following a meal. The figure is made from data obtained from Mason et al. (1962); every point represents mean ± SD (n ≥ 5) (25)
As it can be seen from Figs. 3 and 4, the fasted state gastric pH is considerably lower than the fed state pH; the overall mean values were 2.8 ± 0.9 and 6.4 ± 0.6 in the fasted and fed state, respectively. Comparing these values to those of an adult, it is important to remember the different fasting times for pediatric patients vs adults, i.e., infants are considered to be fasted 3 h postprandial and adults commonly after an overnight fast. Aside from varying with age and nutritional state, it has been reported that the measured gastric pH varies with the position of the utilized pH sensor (31); Omari et al. (2003) reported a regional variation between three different pH sensor positions; 3, 6, and 9 cm below the lower esophageal sphincter, respectively. Furthermore, significant variation in the time it takes to reach a pH < 4 according to the position was observed. The pH was measured to be 2.6, 1.8, and 2.1 pre-prandial at the different locations and 7.3, 6.8, and 6.6, in the fed state, respectively (31). The observed regional pH differences may have a large impact on drug solubilization and enzyme activity, as a microclimate displaying a different pH may affect drug solubilization possibly causing supersaturation or drug precipitation. The differences in microclimate may, furthermore, lead to altered digestion rates of, e.g., lipids, which in turn may also affect drug solubilization.
Duodenal and Intestinal pH
Only two studies were found regarding the intestinal pH of neonates. In the first study, Barbero et al. (1952) reported a fed state duodenal pH of 6.5 ± 0.5 measured on intestinal aspirates from 7 full-term neonates/infants aging between 2 weeks and 3 months. The pH of jejunum and ileum was reported to be 6.6 ± 0.4 and 6.8 ± 0.7, respectively (44). In the second study, Fredrikzon et al. (1978) tested the pH of neonates under the age of 25 days and reported a fasted state pH of ∼7 based on 7 observations. Postprandial, the intestinal pH decreased to 6.5 (30 min after feeding). The neonatal pre- and postprandial pH values were generally slightly higher compared to the adults, who were investigated in the same study (45).
Osmolality
The osmolality of the gastric and duodenal contents has been investigated in 15 low birth weight neonates (age 8 ± 4 days) fed breast milk (52). Measurements were carried out in breast milk as well as in both gastric and intestinal aspirates taken at time points 45, 90, 135, and 180 min after a feeding. The osmolality of breast milk was measured to be 291 ± 4 mosmol/kg. During the 180-min study, the average osmolality of the gastric and intestinal contents ranged from 291 to 298 mosmol/kg and 296 to 308 mosmol/kg, respectively (52). Assuming the neonate population is in a fasted state 3 h after a feed, the fasted and fed state values were 298 and 291 mosmol/kg, in the gastric phase and 308 and 296 mosmol/kg, in the intestinal phase, and thus there was basically no difference between the fasted and the fed state.
Bile Salts
In the GI lumen, BSs and phospholipids (PLs) are secreted as part of the bile. BSs are very important during lipid digestion, as they facilitate the emulsification of chyme and the catalytic activity of lipases by removing lipolysis products from the emulsion interface via formation of mixed micelles (53). Mixed micelles, in turn, play an important role in the solubilization of neutral drug compounds, as they can increase the apparent solubility of the drug by incorporation into the micelles (54).
The composition and concentration of BSs have been shown to vary significantly with age, i.e., compared to adults, the BS level is very low in neonates (55,56). The duodenal concentration of BSs has been measured several times in aspirates of neonates, infants, and children. In these studies, various effects have been investigated, e.g., type of food (38,57,58), prandial state (56,57), GA (55,56), and postnatal age (38,55,57–59). Furthermore, the specific BSs have been quantitated, and the ratios between cholic acid (CA) and chenodeoxycholic acid (CDCA), as well as ratio between taurine and glycine conjugation, determined (38,55,57). As an example, Boehm et al. (1997) measured the total pre-prandial concentration of BSs in duodenal aspirates of 41 neonates during the first 60 days of life. The results showed a continuous increase in the BS concentration throughout the study, going from approximately 2 to 8 mM during the 60 days (mean 4.4 ± 2.0 mM). The neonates were grouped according to their GA (27–34w); however, the results showed no difference related to the GA (55). The same study also investigated the CA/CDCA ratio, as well as the taurine/glycine conjugation ratio. Both ratios were seen to decrease with postnatal age from ∼6 to ∼2, with mean ratios of 2.8 ± 1.5 and 2.7 ± 1.3 for CA/CDCA and taurine/glycine, respectively (55). With a similar study setup, Järvenpäa et al. (1983) studied the effects of type of feeding, comparing the pre-prandial concentration of BSs in duodenal aspirates of 65 preterm neonates fed breast milk and three different infant formulas enriched with various amounts of taurine and cholesterol, respectively (38). The study showed no consistent difference in the total concentration of BS between the neonates fed the different infant formula; however, the total BS concentration was significantly higher in those fed breast milk (38). Correlating well with the data by Boehm et al. (1997), the total BS concentration in neonates fed breast milk increased from 4.8 mM 1 week postnatal to 7.8 mM 5 weeks postnatal; however, the difference was not statistically significant (38). Mainly primary BSs were found in the duodenal aspirates of neonates (38,55). In comparison to the adult population, neonates and infants have a very small pool of BSs. Furthermore, the secondary BSs are lacking, as the bacterial flora of the large intestine, which converts the primary BSs to secondary BSs, is not established in the neonate population (55).
Based on the inconsistency in terms of effect of postnatal age on the level of BSs in the neonatal population, a mean total BS concentration was estimated by pooling the data from six studies and a total of 255 neonates. The mean BS concentration for the fasted and fed state was calculated to be 4.7 ± 1.4 mM and 1.0 ± 0.3 mM, respectively (38,55–58,60). The difference between the fasted and the fed state corresponds to the dilution taken place in the presence of food, as the BS pool of infants is very small (55). Figure 5 displays the total BS concentrations in neonates in the fasted and fed state, respectively.
Halpern et al. (1996) determined the contents of cholesterol, BSs, and PLs in the gallbladder bile of neonates, infants, and children (59). Based on the results of that study, the BS:PL ratio was 4.8 ± 2.0 in neonates (n = 3).
Digestive Enzymes
The presence of digestive enzymes in the GI tract will inherently facilitate the hydrolysis of ingested food components (61,62). During digestion of breast milk or infant formula, macronutrients are hydrolyzed and several different digestion products form (34,63,64). The digestion will affect the stability of the fat globules present in milk or formula, and new colloidal structures (e.g., mixed micelles and vesicles) will assemble from the lipid digestion products (65). Milk’s solubilizing capacity towards poorly water-soluble drugs can subsequently be reduced, as it has been observed previously during several in vitro digestion studies of lipid-based drug delivery systems (66–74). The decreased drug solubilization will reduce the driving force for drug absorption through the epithelial cells lining the small intestine, as the solubilized fraction of drug is believed to be the only fraction available for absorption (53,67,75). Infants and especially neonates are fed frequently, typically every third hour, and can therefore be assumed to be in a fed or semi-fed state most of the time. Thus, in order to conduct an in vitro assessment of dosage forms intended for oral administration to neonates or infants, one needs to take milk digestion into account.
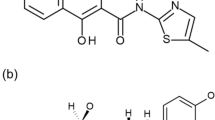
Several studies have investigated the activity of specific enzymes in the gastric and duodenal fluids of the pediatric population (24,34,63,74–79). The enzymes receiving most focus are HGL, pancreatic lipase (and colipase), pepsin and trypsin, which are responsible for the degradation of lipids and proteins throughout the GI tract (24,63,77–79). Although these enzymes are the most investigated, several enzymes are responsible for the hydrolysis of lipids and proteins (80–82). According to Abrahamse et al. (2012), the following four lipases should be present in order to obtain a physiologically relevant lipolysis: GL, pancreatic triglyceride lipase (PTL) (and colipase), carboxylester hydrolase (CEH), and pancreatic lipase-related protein 2 (PLRP2) (83). Furthermore, bile salt stimulated lipase should be present, if the infants are fed with non-pasteurized breast milk (84).
The following section will try to elucidate the role the different enzymes play in the digestion of breast milk or infant formula and how this potentially can affect drug solubilization. Carbohydrate digestion will not be covered in this section as it believed to have limited effect on the solubilization of poorly water-soluble drugs.
Lipases
Gastric Lipase
HGL is the only preduodenal lipase in man and is solely responsible for the intragastric lipolysis in neonates (80,85). HGL is sn-1 and an-3 regioselective and stereoselective but has a preference for the sn-3 position (86,87). Thus, the major digestion products following digestion of triacylglycerides (TAGs) facilitated by HGL are 1,2-diacylglycerides (predominantly), 2,3-diacylglycerides, and free fatty acids (FAs) (86,88). HGL is active at pH 1 to 7 and has a pH optimum of 3 to 5 (50). In adults, the moderately acidic pH optimum makes HGL more active in the fed stomach compared to the small intestine, where higher pH levels are expected. However, in the case of neonates who display very similar pH values in the fed stomach and small intestine, the HGL activity is expected to be similar as it retains some of its activity throughout the GI tract (89). HGL is furthermore stable towards the proteolytic activity of pepsin above pH 1, but is denaturated and hydrolyzed below pH 1 (90). These unique characteristics make HGL suitable for digestion even in the harsh environment of the stomach.
In neonates, the intragastric digestion of breast milk or infant formula is responsible for approximately 10% of the total TAG digestion, which corresponds well with intragastric lipolysis levels reported in adults (34,63,88). HGL expression is fully matured at birth, which has been investigated by biopsy samples from the fundic mucosa of infants, children, and adults showing the same level and activity of HGL (78). This indeed suggests that HGL activity in gastric content is comparable in neonates and adults, which has been confirmed in a study by Roman et al. (2007) (34). The authors reported fasted HGL levels of 77 vs 100 μg/mL (corresponding to HGL activity in infants of approximately 100 tributyrin units (TBU)/mL, assuming the specific activity of HGL is 1300 TBU/mL) in neonates and adults, respectively (34). Nenonate’s gastric juice is typically diluted 1:6 by milk during a meal resulting in a HGL activity of 17 TBU/mL. HGL activity in fed adults has been reported to be approximately 18 TBU/mL and is therefore very similar to the estimated neonate HGL activity (88,91–94). Many different studies have been studying HGL activity in the stomach of fed neonates but have been using different substrates and assay conditions (24,63,77,95). Due to the difficulties in comparing data from such studies, only a few studies provide data that enable a direct comparison between HGL activity in neonates and adults. Still, the activity is generally believed to be comparable (34,39,89).
The quantitative hydrolysis of TAG (approximately 10%) by HGL is relatively low, as digestion is hampered by lipolysis product build-up at the fat globules interphase, due to limited absorption through the gastric mucosa (96). Indeed, short and medium chain FAs can be absorbed, but they are only a small fraction (<10%) of the FAs present in breast milk (34,80). HGL’s importance during milk digestion is attributed to its ability to initiate hydrolysis of breast milk TAGs in the stomach, without requiring BSs or other co-factors, making it unique compared to the other lipases in the GI tract (80). HGL’s catalytic activity towards milk fat globules is interesting since milk fat globules are stabilized by the apical side of plasma membranes and do primarily consist of PLs and glycoproteins, for which HGL has no affinity (80). HGL is nevertheless able to digest TAGs and thus making the fat globules available for enzymatic degradation by other lipases in the small intestine, as explained in the next sections (97).
Pancreatic Lipases
PTL, CEH, and PLRP2 are secreted from the exocrine pancreas into the intestinal lumen and their relative contribution to the hydrolysis of TAG present in breast milk and infant formula has been discussed over the years (80,82,98). In adults, PTL has been shown to be the key enzyme in the lipolysis of TAG, but the secretion of PTL has been shown to be lower in neonates compared to in adults (45,88). The lower levels of PTL has been confirmed both by protein expression levels through the concentration of mRNA encoding for the PTL but also by determining lipase activity in duodenal aspirates (45,82,99). Based on mRNA levels, the expression of CEH and PLPR2 in infants is, however, not fully matured at birth (99). Thus, it has been hypothesized that CEH and PLRP2 might be the key enzymes in the intestinal lipolysis in infants (82), which is supported by studies in knock-out mice where the two enzymes have been shown to have a major impact on lipolysis (100). Although CEH and PLRP2 most likely are important for lipid digestion in infants, PTL hydrolysis should be neglected and may in fact still be instrumental in infant digestion, as further explained in the following.
Pancreatic Triglyceride Lipase and Colipase
As mentioned above, PTL levels have been reported to be lower in infants than in adults (45,82,99). The fasted state activity of PTL was shown in a study by Frederikzon et al. (1978) to have a median activity of 250 TBU/mL in neonates (149–586 TBU/mL) and 580 TBU/mL (84–1124 TBU/mL) in adults (45). In neonates, the PTL activity has been shown to decrease in the fed state by dilution of the meal (45). This is contrary to what is observed in adults, where the pancreas is stimulated by the presence of macronutrients and hence secretes more enzymes (101). The postprandial PTL activity is therefore higher in adults than the fasted state level, despite dilution by the meal (101). A possible explanation for this discrepancy between neonates and adults could be the regular feeding of neonates resulting in continuous stimulation of pancreas, leaving the remaining enzyme reservoir in the pancreas low (45). The fed state PTL activity has been determined by Frederikzon et al. (1978) to be approximate 50 TBU/mL in average during the first 2 h after feeding (45). It should be noted that lipase activities are often measured in duodenal aspirates and thus might contain CEH and PLRP2 additionally to PTL, which will be reflected in a higher lipase activity as these also contribute to the total activity (45). In adults, CEH and PLRP2 only accounts for 4 and 0.5% of the total pancreatic proteins, whereas PTL accounts for approximately 10% (102,103). The specific activity towards tributyrin is 100-fold and 40-fold higher for PTL compared to CEH and PLRP2, respectively (102). Thus, it is plausible that the majority of lipolytic activity recorded in the intestinal juice of neonates originates from PTL, even though PLRP2 and CEH expression has been reported to be fully matured at birth, it cannot account for the lipase activity level reported in neonate intestinal juice (250 TBU/mL) (45). Hence, PTL hydrolysis should not be neglected when conducted in vitro lipolysis experiments.
PTL is sn-1 and 3 specific, as HGL, and is inhibited in the presence of BSs, if pancreatic colipase is not present (86,89). Thus, the major lipolysis products following digestion facilitated by HGL and PTL are 2-monoacylglyceride (MAG) and FAs which are readily absorbed in the small intestine in the presence of BSs (80). PTL is active in the pH interval 5–11 and has an optimum between pH 6.5 and 9 (104). Thus, it is highly active throughout the small intestine. Interestingly, PTL has been shown in vitro not to have any activity on breast milk, even in the presence of colipase and BSs, despite its believed role as lead enzyme in milk fat digestion (80,97,98). PTL does, however, facilitate massive hydrolysis if breast milk fat has been exposed to gastric digestion beforehand, which is the case in the infant (80,97). Thus, in order to obtain complete digestion of breast milk in vivo and in vitro, both gastric and pancreatic digestions are necessary.
Pancreatic Lipase-Related Protein 2
PLRP2 is a lipase with similar digestive characteristics as PTL. In vitro studies have shown that PLRP2 is able to hydrolyze the fat in breast milk in the presence of colipase without prior incubation with HGL (82). Even though the rate of TAG digestion in heat-treated breast milk is detectable, it is very limited (82). The activity is, as observed for PTL, markedly increased when milk fat globules has been pre-incubated with HGL (82). Thus, the level of lipolysis catalyzed by PLRP2 is still dependent on HGL activity. PLRP2 is sn-1 and 3 specific as HGL and PTL, thus the major lipolysis products are again 2-MAGs and FAs (103).
Carboxylester Hydrolase and Bile Salt Stimulated Lipase
CEH (also known as cholesterol ester lipase (CEL) or bile salt dependent lipase) and bile salt stimulated lipase (BSSL) are structurally the same lipases, but differ in site of expression (105,106). Some authors do not even differentiate between the nomenclature of the two enzymes and just call them both CEL (103). CEH is secreted by the exocrine pancreas, whereas BSSL is secreted by mammary glands, and is therefore present in non-pasteurized breast milk (106). The lipase is stable in an environment with a pH as low as 3.5 and is, in the presence of BSs, not affected by the proteolytic enzymes present in the GI tract (107). As the name indicates, this lipase is dependent on the presence of BSs to be active and specifically primary BSs (39,84). BSSL is unable to hydrolyze native milk fat globule triacylglycerol on its own, even in the presence of BSs (80,82). Only when HGL has hydrolyzed some TAGs is BSSL able to continue hydrolysis (80). Contrary to the above-mentioned lipases, CEL is able to hydrolyze both primary and secondary ester bonds on TAGs (80,84). As a result of this lack of stereospecificity, 2-MAGs can be hydrolyzed by CEL to glycerol and FAs (80). In adults, 2-MAGs are readily absorbed, due to the high levels of BSs, which are essential for a quantitative uptake of MAGs (80). Neonates do, however, have lower levels of BSs, and absorption of MAGs and FAs might therefore be hampered (80). Thus, it is advantageous to have complete hydrolysis of the TAG to free glycerol and FAs for dietary fat uptake in neonates (80).
Infant formulas do not contain CEH (BSSL) and a lower level of intragastric lipolysis has been reported for infant formulas compared to breast milk (34). This could, however, also be attributed to the nature of the fat globules. Where breast milk fat globules are stabilized by a plasma membrane, fat globules from infant formulas are stabilized by proteins or phospholipids (80). Thus, HGL might have a higher affinity for the fat globules in breast milk than infant formula (34,39,108).
Proteases
Pepsin
Pepsin is secreted by the chief cells in the fundus region of the stomach along with HGL (109). It has a pH optimum between 1.8 and 3.5 making it well suited for proteolysis in the stomach (103). In neonates, pepsin expression is not fully developed and matures over time (39). Thus pepsin, activity in neonates is often expressed as U/mL/kg bodyweight, to account for the maturation of pepsin expression as a function of neonate growth. Gastric aspirates of neonates were investigated by Armand et al. (1996) to determine pepsin activity (24). The authors found the postprandial pepsin activity to be approx. 50–65 U/mL/kg bodyweight, 30 min after feeding (24).
In a study by Bourlieu et al. (2015), an in vitro lipolysis model for infants using a pepsin activity of 63 U/mL/kg body weight was developed (64). This is in line with the values reported by Armand et al. (1996) (24). At this pepsin level, the authors found that the lipolysis rate of bovine milk fat globules facilitated by rabbit GL was not influenced by the proteolytic activity (64). Bovine milk fat globules are very similar to breast milk fat globules and rabbit GL has been shown to mimic the digestive properties of HGL well (110). Thus, pepsin could be expected to have little effect on the gastric lipolysis of breast milk and hence the solubilization of drug in the lipid phase. Bourlieu et al. (2015) did, however, observe an increased lipolysis of processed bovine milk, when the fat globules were stabilized by proteins, which is the case for most infant formulas (64). Thus, pepsin could potentially alter lipid digestion in neonates and infants and hence affect drug solubilization and should therefore be incorporated in in vitro digestion models.
Trypsin
Trypsin is expressed in the exocrine pancreas and is the most abundant protein (20% of the pancreatic proteins are trypsin) in pancreatic juice in adults (103). Trypsin levels in neonates have been reported to be lower than in children and adults (111). In a study by Zoppi et al. (1972) the trypsin activity was determined to be approximately 7-fold higher in children compared to neonates (76). In a review by McClean et al. (1993), they found that the trypsin activity in neonates was 90% that of the adult value (111). Thus, different trypsin levels in neonates have been reported in literature, but most of them have shown trypsin activity to be within the same order of magnitude as in adults (39,111). Not a lot is known about trypsin’s effect on lipolysis of fat from breast milk or infant formula, but it could potentially have an effect similar to the effect pepsin has on GL. Thus, trypsin should be present when conducting in vitro lipolysis of both breast milk and infant formula. Other proteases such as chymotrypsin might also be present in the GI tract of neonates and can also contribute to the proteolysis occurring in the GI tract of neonates.
In Vitro Model Setup
When developing an in vitro model with the purpose of predicting drug performance after oral administration, it is important to simulate the GI conditions and processes the drug will encounter. When a drug is administered in the fed state, which is commonly the case for neonates as they are typically feed every third hour, the digestion of the milk will affect the composition of the fluid available for drug dissolution/solubilization. Therefore, in order to predict the solubilized amount of drug available for absorption, an in vitro model including digestion should be utilized. In order to simulate the digestion process and the drug solubilization taking place in vivo, the following aspects should be considered: physiological relevant media volume, use of physiological enzymes in proper amounts, as well as correct pH and addition of relevant co-factors, e.g., BSs and co-enzymes. Furthermore, physiological transit times and appropriate mixing should be considered and mimicked as close as possible. In order to get the full picture, the model should optimally include an absorption module; however, this may complicate the model substantially.
Different in vitro models have been developed to simulate the digestion process in the stomach, duodenum, and small intestine. The in vitro pediatric digestion model suggested in the present study is based on the lipolysis model originally developed by Zangenberg et al. (2001) (66). Figure 6 shows a schematic representation of a one-compartment in vitro lipolysis model with continuous pH measurement and addition of NaOH to maintain a predefined pH, stirring, and temperature control. The in vitro digestion takes place in a temperature controlled reaction vessel where the tested formulation is added to dissolve or disperse in a medium resembling fasted or fed state GI fluids. Digestion is initiated by manual addition of enzymes. The amount digested can be estimated based on the amount of NaOH added during lipolysis in order to neutralize the pH drop caused by fatty acids released from enzymatic hydrolysis of triglycerides and other digestible excipients. The exact composition and concentration of digested lipids can also be determined by lipid analyses (34,63,64). During a digestion experiment, samples should be taken and centrifuged to separate the three possible phases: an oil phase, an aqueous phase containing micelles and vesicles, and a pellet phase. The amount of drug solubilized in the aqueous phase is commonly used as an estimate for the amount of drug available for absorption (112).
To mimic the drug solubilization in the stomach and the small intestine, the model should be designed as a two-step model comprising a gastric phase and an intestinal phase. The duration of each phase and the transfer between the two phases should be designed to correlate with the GHET and intestinal transit time in neonates. Using a pump to transfer the gastric media to the intestinal phase, Table I shows suggested flow rates to mimic the GE pattern described by Armand et al. (1996) (Figure 1; 24). As several studies showed a difference in the GE of breast milk and infant formula, two separate flow rates are suggested for doing studies with breast milk and infant formula, respectively. As discussed previously, the gastric emptying pattern is best fit by a monophasic exponential pattern; however, to reproduce this in vitro will require a programmable pump or multiple flow rate adjustments during a single run. Flow rate values are suggested for a simplified exponential setup with three different flow settings. Alternately, the model may be simplified by using a constant transfer rate, which is also suggested in Table I.
In a system where a pump is used, it is important to consider drug adhesion to the extended surface area produced by the tubing. Furthermore, when setting flow rates, a possible difference in viscosity should be taken into account, as it may affect the effective flow rate. In the interest of simplifying the in vitro model further, and avoiding adhesion to tubing, the transfer can also be done simply by adding a concentrated simulated intestinal media designed to reach final concentrations relative to the physiological values of pH, BSs, and PLs (method depicted in Fig. 6).
In Vitro Model Media Composition
Based on the results of the literature study, Table II summarizes the important physiological parameters, as described above that should be considered in an in vitro digestion model. The specific volumes and concentrations are calculated based on an infant weighing 2.0 kg, as this was the mean birth weight of all the neonates (n = 482) from which data were used in the present review.
Due to the uniformity of the neonate diet (breast milk and/or infant formula), it is possible to simulate the fed state quite accurately. However, as breast milk and infant formula differ in many ways including, e.g., lipid composition, presence of BSSL and effect on GHET, it is important to keep in mind that the choice of meal can affect the result in terms of predicting the oral drug performance. With respect to the digestion of the different types of meals, the choice and activity levels of the used digestive enzymes will also be of great importance.
In contrast to the studies investigating GE, pH levels and BS concentration, which were measured in absolute numbers, despite varying analytical techniques, the level of digestive enzymes have been reported in activity levels determined in non-standardized assays. Thus, pooling of data from the different studies is not possible and the selection of enzyme levels for an in vitro digestion model corresponding to what is observed in neonates is therefore based on a few studies (Table II). CEL and PLRP2 have been shown to have a synergetic effect when added to breast milk, which has been pre-incubated with HGL (82). Thus, in order to simulate fat digestion of breast milk in vitro, it is needed to include HGL, PTL, PLRP2, and CEL. PTL and CEL are both present in porcine pancreatin, which is commonly used as digestive extract for the intestinal digestion, as it has been shown to simulate the digestive properties of human pancreatic juice well. PLRP2 is present in pigs, but has not yet been proven to be present in porcine pancreatin, although indications of its presence in low quantities have been shown (102,113). Thus, due to the non-physiological levels of PLRP2 in porcine pancreatin, PLPR2 needs to be added independently, if biorelevant levels of the enzyme should be achieved during an in vitro digestion. Unfortunately, neither PLRP2 nor HGL are easily obtained commercially, which complicates the development of in vitro models simulating neonate digestion.
Both trypsin and chymotrypsin are present in the porcine pancreatin extract commonly used for in vitro lipolysis, ensuring that proteolysis is occurring during the digestion experiment.
As emphasized by the last section, developing a simple (or even a complex) in vitro model simulating the very multifaceted in vivo processes taken place in the human GI tract is very difficult. It is generally problematic to fix any values (e.g., pH, GE and enzyme activity), as all in vivo processes are dynamic displaying many variations over time and location in the GI tract, and as a function of the prandial state. Furthermore, despite the many studies described in the present review, the general level of information characterizing the age based changes in physiology of the pediatric population is still relatively low. As stated by Batchelor et al. (2016), there is need for additional research to cover the knowledge gabs regarding, e.g., the understanding of drug transporters and metabolizing enzymes along the GI tract, understanding of drug permeability in pediatric populations, and further characterization of pediatric GI fluids (12,13). Still, an in vitro model based on representative mean values and physiological relevant conditions may well be used for, e.g., early predictions of in vivo outcome, learning studies by providing standard conditions for comparing formulations during development of drug delivery systems.
CONCLUSIONS
The literature review showed that several studies have been conducted to characterize the basic physiology of neonates and young infants. Due to various differences in study designs, some of the results were very difficult to compare. Furthermore, the authors found very few studies characterizing the fluid volumes and transit times in the small intestine of neonates.
Based on available literature data, it was possible to design an in vitro model simulating the GI digestion in the neonate pediatric population. Using mean values, the model simulated neonate GI transit times, GI fluid composition, and volumes including pH, osmolality, and BSs. However, in terms of digestive enzymes, mean values were hard to determine as most of the studies were done using various activity assays producing results which are difficult to compare. Therefore, estimated enzyme levels only represent data from a few studies. Furthermore, the lack of commercial availability of PLRP2 and HGL adds to the difficulties of mimicking in vivo conditions in vitro. Thus, a relatively simple in vitro model design was considered as an informative starting point instead of a complex model.
References
Bar-Shalom D, Rose K. In: Bar-Shalom D, Rose K, editors. Pediatric Formulations. 1st ed. New York: Springer; 2014.
Zisowsky J, Krause A, Dingemanse J. Drug Development for Pediatric Populations: Regulatory Aspects. Pharmaceuticals. 2010;2(4):364–88. doi:10.3390/pharmaceutics2040364.
EC Regulation No 1901/2006 of the European Parliament and of the council of 12 December 2006 on medicinal products for paediatric use and amending Regulation (EEC) No 1768/92, directive 2001/20/EC, Directive 2001/83/EC and Regulation (EC) No 726/2004. Official Journal of the European Union, L378-1-L378/19. European Medicines Agency. 2006. http://ec.europa.eu/health/files/eudralex/vol-1/reg_2006_1901/reg_2006_1901_en.pdf
European Medicines Agency. Paediatric Regulations. 2016. http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/document_listing/document_listing_000068.jsp. Accessed 18 July 2016.
European Medicines Agency. The European paediatric initiative: History of the Paediatric Regulation. Doc. Ref: EMEA/17967/04 Rev 1. 2007. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2009/09/WC500003693.pdf
U.S.Department of Health and Human Services Food and Drug Administration. Guidance for Industry. How to Comply with the Pediatric Research Equity Act. Draft guidance. 2005. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm079756.pdf
U.S.Department of Health and Human Services Food and Drug Administration. General Clinical Pharmacology Considerations for Pediatric Studies for Drugs and Biological Products. Guidance for Industry. Draft guidance. 2014. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm425885.pdf
U.S.Department of Health and Human Services Food and Drug Administration. Pediatric Product Development.2015. http://www.fda.gov/Drugs/DevelopmentApprovalProcess/DevelopmentResources/ucm049867.htm. Accessed 18 July 2016.
The European Commision. Better Medicines for Children From Concept to Reality. Progress report on the paediatric regulation (EC) N°1901/2006. Com (2013) 443. 2013. http://ec.europa.eu/health/files/paediatrics/2013_com443/paediatric_report-com(2013)443_en.pdf
U.S.Department of Health and Human Services Food and Drug Administration. Pediatric Study Plans: Content of and Process for Submitting Initial Pediatric Study Plans and Amended Initial Study Plans. Guidance for Industry. Draft Guidance. Draft guidance. March 2016 Revision 1. 2016. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm360507.pdf
European Paediatric Formulation Initiative (EuPFI). Formulating better medicines. 2015. http://www.eupfi.org/
Batchelor HK, Kendall R, Desset-Bretches S, Alex R, Ernest TB, on behalf of the European Paediatric Formulation Initiative (EUPFI). Application of in vitro biopharmaceutical methods in development of immediate release oral dosage forms intended for paediatric patients. EurJPharmBiopharm. 2013;85:833–42.
Batchelor HK, Fotaki N, Klein S. Paediatric oral biopharmaceutics: Key considerations and current challenges. Adv Drug Deliv Rev. 2014;73:102–26.
Kostewicz ES, Abrahamsson B, Brewster M, Brouwers J, Butler J, Carlert S, et al. In vitro models for the prediction of in vivo performance of oral dosage forms. Eur J Pharm Sci. 2014;57:342–66. doi:10.1016/j.ejps.2013.08.024.
Kalantzi L, Goumas K, Kalioras V, Abrahamsson B, Dressman JB, Reppas C. Characterization of the human upper gastrointestinal contents under conditions simulating bioavailability/bioequivalence studies. Pharm Res. 2006;23(1):165–76. doi:10.1007/s11095-005-8476-1.
Dressman JB, Amidon GL, Reppas C, Shah VP. Dissolution testing as a prognostic tool for oral drug absorption: immediate release dosage forms. Pharm Res. 1998;15(1):11–22.
Kataoka M, Masaoka Y, Yamazaki Y, Sakane T, Sezaki H, Yamashita S. In vitro system to evaluate oral absorption of poorly water-soluble drugs: simultaneous analysis on dissolution and permeation of drugs. Pharm Res. 2003;20(10):1674–80.
Frank KJ, Locher K, Zecevic DE, Fleth J, Wagner KG. In vivo predictive mini-scale dissolution for weak bases: Advantages of pH-shift in combination with an absorptive compartment. Eur J Pharm Sci. 2014;61:32–9. doi:10.1016/j.ejps.2013.12.015.
Kostewicz ES, Brauns U, Becker R, Dressman JB. Forecasting the oral absorption behavior of poorly soluble weak bases using solubility and dissolution studies in biorelevant media. Pharm Res. 2002;19(3):345–9.
Kaye JL. Review of paediatric gastrointestinal physiology data relevant to oral drug delivery. Int J Clin Pharm. 2011;33(1):20–4.
Mooij MG, de Koning BA, Huijsman ML, de Wildt SN. Ontogeny of oral drug absorption processes in children. Expert Opin Drug Metab Toxicol. 2012;8(10):1293–303. doi:10.1517/17425255.2012.698261.
Ashford M. Bioavailability - physiochemical and dosage form factors. In: Aulton M, Taylor K, editors. Aulton’s Pharmaceutics, The Design amd Manufacture of Medicines. 4th ed. Edinburgh: Elsevier Ltd; 2013. p. 314–33.
Mudie DM, Amidon GL, Amidon GE. Physiological parameters for oral delivery and in vitro testing. Mol Pharm. 2010;7(5):1388–405. doi:10.1021/mp100149j.
Armand M, Hamosh M, Mehta NR, Angelus PA, Philpott JR, Henderson TR, et al. Effect of human milk or formula on gastric function and fat digestion in the premature infant. Pediatr Res. 1996;40(3):429–37. doi:10.1203/00006450-199609000-00011.
Mason S. Some aspects of gastric function in the newborn. Arch Dis Child. 1962;37:387–91.
Fredrikzon B, Hernell O. Role of feeding on lipase activity in gastric contents. Acta Paediatr Scand. 1977;66(4):479–84.
Bode S, Dreyer M, Greisen G. Gastric emptying and small intestinal transit time in preterm infants: a scintigraphic method. J Pediatr Gastroenterol Nutr. 2004;39(4):378–82.
Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1994;71(1):F24–7.
Cavell B. Gastric emptying in infants fed human milk or infant formula. Acta Paediatr Scand. 1981;70(5):639–41.
Staelens S, Van Den Driessche M, Barclay D, Carrie-Faessler AL, Haschke F, Verbeke K, et al. Gastric emptying in healthy newborns fed an intact protein formula, a partially and an extensively hydrolysed formula. Clin Nutr. 2008;27(2):264–8. doi:10.1016/j.clnu.2007.12.009.
Omari TI, Davidson GP. Multipoint measurement of intragastric pH in healthy preterm infants. Arch Dis Child Fetal Neonatal Ed. 2003;88(6):F517–20.
Signer E. Gastric emptying in newborns and young infants. Measurement of the rate of emptying using indium-113m-microcolloid. Acta Paediatr sScand. 1975;64(3):525–30.
Van Den Driessche M, Peeters K, Marien P, Ghoos Y, Devlieger H, Veereman-Wauters G. Gastric emptying in formula-fed and breast-fed infants measured with the 13C-octanoic acid breath test. J Pediatr Gastroenterol Nutr. 1999;29(1):46–51.
Roman C, Carriere F, Villeneuve P, Pina M, Millet V, Simeoni U, et al. Quantitative and qualitative study of gastric lipolysis in premature infants: do MCT-enriched infant formulas improve fat digestion? Pediatr Res. 2007;61(1):83–8. doi:10.1203/01.pdr.0000250199.24107.fb.
Cavell B. Gastric emptying in preterm infants. Acta Paediatr Scand. 1979;68(5):725–30.
Billeaud C, Guillet J, Sandler B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur J Clin Nutr. 1990;44(8):577–83.
Cavell B. Reservoir and emptying function of the stomach of the premature infant. Acta Paediatr Scand Suppl. 1982;296:60–1.
Jarvenpaa AL, Rassin DK, Kuitunen P, Gaull GE, Raiha NC. Feeding the low-birth-weight infant. III. Diet influences bile acid metabolism. Pediatrics. 1983;72(5):677–83.
Bourlieu C, Menard O, Bouzerzour K, Mandalari G, Macierzanka A, Mackie AR, et al. Specificity of infant digestive conditions: some clues for developing relevant in vitro models. Crit Rev Food Sci Nutr. 2014;54(11):1427–57. doi:10.1080/10408398.2011.640757.
Widstrom AM, Christensson K, Ransjo-Arvidson AB, Matthiesen AS, Winberg J, Uvnas-Moberg K. Gastric aspirates of newborn infants: pH, volume and levels of gastrin- and somatostatin-like immunoreactivity. Acta Paediatr Scand. 1988;77(4):502–8.
Smith LJ, Kaminsky S, D’Souza SW. Neonatal fat digestion and lingual lipase. Acta Paediatr Scand. 1986;75(6):913–8.
Cavell B. Postprandial gastric acid secretion in infants. Acta Paediatr Scand. 1983;72(6):857–60.
Litman RS, Wu CL, Quinlivan JK. Gastric volume and pH in infants fed clear liquids and breast milk prior to surgery. Anesth Analg. 1994;79(3):482–5.
Barbero GJ, Runge G, Fischer D, Crawford MN, Torres FE, Gyorgy P. Investigations on the bacterial flora, pH, and sugar content in the intestinal tract of infants. J Pediatr. 1952;40(2):152–63.
Fredrikzon B, Olivecrona T. Decrease of lipase and esterase activities in intestinal contents of newborn infants during test meals. Pediatr Res. 1978;12(5):631–4. doi:10.1203/00006450-197805000-00004.
Thomson J. The volume and acidity of the gastric contents in the unfed newborn infant. Arch Dis Child. 1951;26(130):558–65.
Sondheimer JM, Clark DA, Gervaise EP. Continuous gastric pH measurement in young and older healthy preterm infants receiving formula and clear liquid feedings. J Pediatr Gastroenterol Nutr. 1985;4(3):352–5.
Siegel M, Lebenthal E, Topper W, Krantz B, Li PK. Gastric emptying in prematures of isocaloric feedings with differing osmolalities. Pediatr Res. 1982;16(2):141–7.
Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying and gastro-oesophageal reflux in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1996;75(2):F117–21.
Gargouri Y, Pieroni G, Riviere C, Sauniere JF, Lowe PA, Sarda L, et al. Kinetic assay of human gastric lipase on short- and long-chain triacylglycerol emulsions. Gastroenterology. 1986;91(4):919–25.
Fallingborg J, Christensen LA, Ingeman-Nielsen M, Jacobsen BA, Abildgaard K, Rasmussen HH, et al. Measurement of gastrointestinal pH and regional transit times in normal children. J Pediatr Gastroenterol Nutr. 1990;11(2):211–4.
Billeaud C, Senterre J, Rigo J. Osmolality of the gastric and duodenal contents in low birth weight infants fed human milk or various formulae. Acta Paediatr Scand. 1982;71(5):799–803.
Porter CJ, Trevaskis NL, Charman WN. Lipids and lipid-based formulations: optimizing the oral delivery of lipophilic drugs. Nat Rev Drug Discov. 2007;6(3):231–48. doi:10.1038/nrd2197.
Bakatselou V, Oppenheim RC, Dressman JB. Solubilization and wetting effects of bile salts on the dissolution of steroids. Pharm Res. 1991;8(12):1461–9.
Boehm G, Braun W, Moro G, Minoli I. Bile acid concentrations in serum and duodenal aspirates of healthy preterm infants: effects of gestational and postnatal age. Biol Neonate. 1997;71(4):207–14.
Watkins JB, Szczepanik P, Gould JB, Klein P, Lester R. Bile salt metabolism in the human premature infant. Preliminary observations of pool size and synthesis rate following prenatal administration of dexamethasone and phenobarbital. Gastroenterology. 1975;69(3):706–13.
Encrantz JC, Sjovall J. On the bile acids in duodenal contents of infants and children. Bile acids and steroids 72. Clin Chim Acta. 1959;4:793–9.
Glasgow JF, Dinsmore H, Molla A, Macfarlane T. A comprehensive study of duodenal bile salts in newborn infants and their relationship to fat absorption. Ir J Med Sci. 1980;149(9):346–56.
Halpern Z, Vinograd Z, Laufer H, Gilat T, Moskowitz M, Bujanover Y. Characteristics of gallbladder bile of infants and children. J Pediatr Gastroenterol Nutr. 1996;23(2):147–50.
Challacombe DN, Edkins S, Brown GA. Duodenal bile acids in infancy. Arch Dis Child. 1975;50(11):837–43.
Carey MC, Small DM, Bliss CM. Lipid digestion and absorption. Annu Rev Physiol. 1983;45:651–77. doi:10.1146/annurev.ph.45.030183.003251.
Patton JS, Carey MC. Watching fat digestion. Science. 1979;204(4389):145–8.
Hamosh M, Bitman J, Liao TH, Mehta NR, Buczek RJ, Wood DL, et al. Gastric lipolysis and fat absorption in preterm infants: effect of medium-chain triglyceride or long-chain triglyceride-containing formulas. Pediatrics. 1989;83(1):86–92.
Bourlieu C, Menard O, De La Chevasnerie A, Sams L, Rousseau F, Madec MN, et al. The structure of infant formulas impacts their lipolysis, proteolysis and disintegration during in vitro gastric digestion. Food Chem. 2015;182:224–35.
Small DM. A classification of biologic lipids based upon their interaction in aqeous systems. J Am Oil Chem Soc. 1968;45(3):108–19.
Zangenberg NH, Mullertz A, Kristensen HG, Hovgaard L. A dynamic in vitro lipolysis model. II: Evaluation of the model. Eur. J Pharm Sci. 2001;14(3):237–44.
Larsen A, Holm R, Pedersen ML, Mullertz A. Lipid-based formulations for danazol containing a digestible surfactant, Labrafil M2125CS: in vivo bioavailability and dynamic in vitro lipolysis. Pharm Res. 2008;25(12):2769–77. doi:10.1007/s11095-008-9641-0.
Porter CJ, Kaukonen AM, Boyd BJ, Edwards GA, Charman WN. Susceptibility to lipase-mediated digestion reduces the oral bioavailability of danazol after administration as a medium-chain lipid-based microemulsion formulation. Pharm Res. 2004;21(8):1405–12.
Porter CJ, Kaukonen AM, Taillardat-Bertschinger A, Boyd BJ, O’Connor JM, Edwards GA, et al. Use of in vitro lipid digestion data to explain the in vivo performance of triglyceride-based oral lipid formulations of poorly water-soluble drugs: studies with halofantrine. J Pharm Sci. 2004;93(5):1110–21. doi:10.1002/jps.20039.
Williams HD, Sassene P, Kleberg K, Bakala-N’Goma JC, Calderone M, Jannin V, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 1: method parameterization and comparison of in vitro digestion profiles across a range of representative formulations. J Pharm Sci. 2012;101:3360–80. doi:10.1002/jps.23205.
Sassene PJ, Knopp MM, Hesselkilde JZ, Koradia V, Larsen A, Rades T, et al. Precipitation of a poorly soluble model drug during in vitro lipolysis: characterization and dissolution of the precipitate. J Pharm Sci. 2010;99(12):4982–91. doi:10.1002/jps.22226.
Mosgaard MD, Sassene P, Mu H, Rades T, Mullertz A. Development of a high-throughput in vitro intestinal lipolysis model for rapid screening of lipid-based drug delivery systems. Eur J Pharm Biopharm. 2015;94:493–500. doi:10.1016/j.ejpb.2015.06.028.
Sassene PJ, Mosgaard MD, Lobmann K, Mu H, Larsen FH, Rades T, et al. Elucidating the Molecular Interactions Occurring during Drug Precipitation of Weak Bases from Lipid-Based Formulations: A Case Study with Cinnarizine and a Long Chain Self-Nanoemulsifying Drug Delivery System. Mol Pharm. 2015;12(11):4067–76. doi:10.1021/acs.molpharmaceut.5b00498.
Thomas N, Holm R, Mullertz A, Rades T. In vitro and in vivo performance of novel supersaturated self-nanoemulsifying drug delivery systems (super-SNEDDS). J Control Release. 2012;160(1):25–32. doi:10.1016/j.jconrel.2012.02.027.
Larsen AT, Sassene P, Mullertz A. In vitro lipolysis models as a tool for the characterization of oral lipid and surfactant based drug delivery systems. Int J Pharm. 2011;417(1-2):245–55. doi:10.1016/j.ijpharm.2011.03.002.
Zoppi G, Andreotti G, Pajno-Ferrara F, Njai DM, Gaburro D. Exocrine pancreas function in premature and full term neonates. Pediatr Res. 1972;6(12):880–6. doi:10.1203/00006450-197212000-00005.
Hamosh M, Scanlon JW, Ganot D, Likel M, Scanlon KB, Hamosh P. Fat digestion in the newborn. Characterization of lipase in gastric aspirates of premature and term infants. J Clin Invest. 1981;67(3):838–46.
DiPalma J, Kirk CL, Hamosh M, Colon AR, Benjamin SB, Hamosh P. Lipase and pepsin activity in the gastric mucosa of infants, children, and adults. Gastroenterology. 1991;101(1):116–21.
Boehm G, Bierbach U, Senger H, Jakobsson I, Minoli I, Moro G, et al. Activities of lipase and trypsin in duodenal juice of infants small for gestational age. J Pediatr Gastroenterol Nutr. 1991;12(3):324–7.
Bernback S, Blackberg L, Hernell O. The complete digestion of human milk triacylglycerol in vitro requires gastric lipase, pancreatic colipase-dependent lipase, and bile salt-stimulated lipase. J Clin Invest. 1990;85(4):1221–6. doi:10.1172/JCI114556.
Bernback S, Blackberg L, Hernell O. Fatty acids generated by gastric lipase promote human milk triacylglycerol digestion by pancreatic colipase-dependent lipase. Biochim Biophys Acta. 1989;1001(3):286–93.
Johnson K, Ross L, Miller R, Xiao X, Lowe ME. Pancreatic lipase-related protein 2 digests fats in human milk and formula in concert with gastric lipase and carboxyl ester lipase. Pediatr Res. 2013;74(2):127–32. doi:10.1038/pr.2013.90.
Abrahamse E, Minekus M, van Aken GA, van de Heijning B, Knol J, Bartke N, et al. Development of the Digestive System-Experimental Challenges and Approaches of Infant Lipid Digestion. Food Dig. 2012;3(1-3):63–77. doi:10.1007/s13228-012-0025-x.
Blackberg L, Hernell O. The bile-salt-stimulated lipase in human milk. Purification and characterization. Eur J Biochem. 1981;116(2):221–5.
Moreau H, Laugier R, Gargouri Y, Ferrato F, Verger R. Human preduodenal lipase is entirely of gastric fundic origin. Gastroenterology. 1988;95(5):1221–6.
Rogalska E, Ransac S, Verger R. Stereoselectivity of lipases. II. Stereoselective hydrolysis of triglycerides by gastric and pancreatic lipases. J Biol Chem. 1990;265(33):20271–6.
Jensen RG, DeJong FA, Clark RM, Palmgren LG, Liao TH, Hamosh M. Stereospecificity of premature human infant lingual lipase. Lipids. 1982;17(8):570–2.
Carriere F, Barrowman JA, Verger R, Laugier R. Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Gastroenterology. 1993;105(3):876–88.
Sams L, Paume J, Giallo J, Carriere F. Relevant pH and lipase for in vitro models of gastric digestion. Food Funct. 2016;7(1):30–45. doi:10.1039/c5fo00930h.
Ville E, Carriere F, Renou C, Laugier R. Physiological study of pH stability and sensitivity to pepsin of human gastric lipase. Digestion. 2002;65(2):73–81.
Armand M, Borel P, Dubois C, Senft M, Peyrot J, Salducci J, et al. Characterization of emulsions and lipolysis of dietary lipids in the human stomach. Am J Physiol. 1994;266(3 Pt 1):G372–81.
Armand M, Borel P, Pasquier B, Dubois C, Senft M, Andre M, et al. Physicochemical characteristics of emulsions during fat digestion in human stomach and duodenum. Am J Physiol. 1996;271(1 Pt 1):G172–83.
Armand M, Pasquier B, Andre M, Borel P, Senft M, Peyrot J, et al. Digestion and absorption of 2 fat emulsions with different droplet sizes in the human digestive tract. Am J Clin Nutr. 1999;70(6):1096–106.
Carriere F, Renou C, Lopez V, De CJ, Ferrato F, Lengsfeld H. de, C.A.; Laugier, R.; Verger, R. The specific activities of human digestive lipases measured from the in vivo and in vitro lipolysis of test meals. Gastroenterology. 2000;119(4):949–60.
Abrams CK, Hamosh M, Lee TC, Ansher AF, Collen MJ, Lewis JH, et al. Gastric lipase: localization in the human stomach. Gastroenterology. 1988;95(6):1460–4.
Pafumi Y, Lairon D, de la Porte PL, Juhel C, Storch J, Hamosh M, et al. Mechanisms of inhibition of triacylglycerol hydrolysis by human gastric lipase. J Biol Chem. 2002;277(31):28070–9. doi:10.1074/jbc.M202839200.
Gargouri Y, Pieroni G, Riviere C, Lowe PA, Sauniere JF, Sarda L, et al. Importance of human gastric lipase for intestinal lipolysis: an in vitro study. Biochim Biophys Acta. 1986;879(3):419–23.
Jensen RG, Clark RM, DeJong FA, Hamosh M, Liao TH, Mehta NR. The lipolytic triad: human lingual, breast milk, and pancreatic lipases: physiological implications of their characteristics in digestion of dietary fats. J Pediatr Gastroenterol Nutr. 1982;1(2):243–55.
Yang Y, Sanchez D, Figarella C, Lowe ME. Discoordinate expression of pancreatic lipase and two related proteins in the human fetal pancreas. Pediatr Res. 2000;47(2):184–8.
Lowe ME, Kaplan MH, Jackson-Grusby L, D’Agostino D, Grusby MJ. Decreased neonatal dietary fat absorption and T cell cytotoxicity in pancreatic lipase-related protein 2-deficient mice. J Biol Chem. 1998;273(47):31215–21.
Carriere F, Grandval P, Renou C, Palomba A, Prieri F, Giallo J, et al. Quantitative study of digestive enzyme secretion and gastrointestinal lipolysis in chronic pancreatitis. Clin Gastroenterol Hepatol. 2005;3(1):28–38.
Fernandez S, Jannin V, Rodier JD, Ritter N, Mahler B, Carriere F. Comparative study on digestive lipase activities on the self emulsifying excipient Labrasol, medium chain glycerides and PEG esters. Biochim Biophys Acta. 2007;1771(5):633–40. doi:10.1016/j.bbalip.2007.02.009.
Whitcomb DC, Lowe ME. Human pancreatic digestive enzymes. Dig Dis Sci. 2007;52(1):1–17. doi:10.1007/s10620-006-9589-z.
Gargouri Y, Moreau H, Verger R. Gastric lipases: biochemical and physiological studies. Biochim Biophys Acta. 1989;1006(3):255–71.
Armand M. Lipases and lipolysis in the human digestive tract: where do we stand? Curr Opin Clin Nutr Metab Care. 2007;10(2):156–64. doi:10.1097/MCO.0b013e3280177687.
Nilsson J, Blackberg L, Carlsson P, Enerback S, Hernell O, Bjursell G. cDNA cloning of human-milk bile-salt-stimulated lipase and evidence for its identity to pancreatic carboxylic ester hydrolase. Eur J Biochem. 1990;192(2):543–50.
Fredrikzon B, Hernell O, Blackberg L, Olivecrona T. Bile salt-stimulated lipase in human milk: evidence of activity in vivo and of a role in the digestion of milk retinol esters. Pediatr Res. 1978;12(11):1048–52. doi:10.1203/00006450-197811000-00004.
JH, Nejrup RG, Frøkjær H, Nilsson Å, Ohlsson L, Hellgren LI. Emulsifying triglycerides with dairy phospholipids instead of soy lecithin modulates gut lipase activity. Eur J Lipid Sci Technol. 2015;117:1522–39.
Moreau H, Bernadac A, Gargouri Y, Benkouka F, Laugier R, Verger R. Immunocytolocalization of human gastric lipase in chief cells of the fundic mucosa. Histochemistry. 1989;91(5):419–23.
Capolino P, Guérin C, Paume J, Giallo J, Ballester JM, Cavalier JF, et al. In Vitro Gastrointestinal Lipolysis: Replacement of Human Digestive Lipases by a Combination of Rabbit Gastric and Porcine Pancreatic Extracts. Food Dig. 2011;2:43–51. doi:10.1007/s13228-011-0014-5.
McClean P, Weaver LT. Ontogeny of human pancreatic exocrine function. Arch Dis Child. 1993;68:62–5.
Thomas N, Holm R, Rades T, Mullertz A. Characterising lipid lipolysis and its implication in lipid-based formulation development. AAPS J. 2012;14(4):860–71. doi:10.1208/s12248-012-9398-6.
Xiao X, Ross LE, Sevilla WA, Wang Y, Lowe ME. Porcine pancreatic lipase related protein 2 has high triglyceride lipase activity in the absence of colipase. Biochim Biophys Acta. 2013;1831(9):1435–41. doi:10.1016/j.bbalip.2013.06.002.
Acknowledgments
This work is a research collaboration with the United States Food and Drug Administration, Center for Drug Evaluation and Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The approaches and conclusions in this manuscript have not been formally disseminated by the United States Food and Drug Administration and should not be construed to represent any agency determination or policy.
Additional information
Guest Editors: Maren Preis and Jorg Breitkreutz
Rights and permissions
About this article
Cite this article
Kamstrup, D., Berthelsen, R., Sassene, P.J. et al. In Vitro Model Simulating Gastro-Intestinal Digestion in the Pediatric Population (Neonates and Young Infants). AAPS PharmSciTech 18, 317–329 (2017). https://doi.org/10.1208/s12249-016-0649-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-016-0649-1