Abstract
Hepatic clearance may be uptake rate limited by organic anion transporting polypeptides (OATPs) and organic cation transporter 1 (OCT1). While comparison of OATP activity has been investigated across species, little has been reported for OCT1. Additionally, while data on interspecies transporter expression in the liver exist, quantitative comparison of these transporters in multiple tissues is lacking. In the current research, the pharmacokinetics of OCT1 substrates (sumatriptan and metformin) were assessed in Oct knockout rats for comparison with previous Oct1/2−/− mice data and OCT1 pharmacogenetics in humans. Effect of OCT1 inhibitors verapamil and erlotinib on OCT1 substrate liver partitioning was also evaluated in rats. Expression of 18 transporters, including Oatps and Octs, in 9 tissues from mice and rats was quantitated using nanoLC/MS-MS, along with uptake transporters in hepatocytes from 5 species. Interspecies differences in OCT1 activity were further evaluated via uptake of OCT1 substrates in hepatocytes with corresponding in vivo liver partitioning in rodents and monkey. In Oct1−/− rats, sumatriptan hepatic clearance and liver partitioning decreased; however, metformin pharmacokinetics were unaffected. OCT1 inhibitor coadministration decreased sumatriptan liver partitioning. In rodents, Oatp expression was highest in the liver, although comparable expression of Oatps in other tissues was determined. Expression of Octs was highest in the kidney, with liver Oct1 expression comparably lower than Oatps. Liver partitioning of OCT1 substrates was lower in rodents than in monkey, in agreement with the highest OCT1 expression and uptake of OCT1 substrates in monkey hepatocytes. Species-dependent OCT1 activity requires consideration when translating preclinical data to the clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The role of hepatic uptake transporters in drug disposition has been confirmed in the clinic. For the organic anion transporting polypeptides (OATPs), the role of hepatic uptake has been established in hepatic clearance, drug-drug interactions (DDIs), pharmacodynamics, pharmacogenetics, and recently, liver drug exposure (1,2,3,4). Lately, the role of organic cation transporter 1 (OCT1) in the hepatic clearance of therapeutic agents has also become apparent. This has been demonstrated clinically by the effect of OCT1 variants on the exposure of several OCT1 substrates, including sumatriptan (5,6,7,8). Effect of the variants on the pharmacodynamics of the OCT1 substrate metformin has also been described (9, 10). There is one reported OCT1-mediated drug-drug interaction with the effect of OCT1 inhibitor verapamil on metformin pharmacodynamics (11). Interestingly, although many therapeutic agents have been identified as inhibitors of OCT1 (12, 13), there still remains a lack of reported drug-drug interactions affecting the exposure of OCT1 substrates in the clinic. OCT1 is primarily expressed in the liver and, to a lesser extent, in the intestine of humans (14), and it remains difficult to quantitate the specific role of OCT1 in the liver since most clinical studies assess pharmacokinetics of OCT1 substrates following oral administration. However, the proof of concept for altered hepatic uptake by OCT1 variants in humans has been demonstrated using 11C-metformin (15). In addition, the effect of OCT1 genotype on intravenous fenoterol has been recently demonstrated (5).
To substantiate the role of OCT1 in hepatic clearance as well as liver partitioning and to evaluate a potentially useful animal model, we previously assessed the pharmacokinetics of OCT1 substrates in Oct1/2−/− mice (16). These studies confirmed decreased hepatic clearance and liver partitioning of sumatriptan and fenoterol in mice lacking Oct1/2. In both mouse and human hepatocytes, uptake for both substrates could also be inhibited by an OCT1 inhibitor. In addition, previous evaluations have demonstrated decreased liver partitioning for metformin in these mice (17). However, we noticed differences in the hepatocyte uptake for other clinical OCT1 substrates, ondansetron and tropisetron, in that minimal inhibition in mouse hepatocytes was observed whereas it was significant in human hepatocytes. There was also a minimal effect of Oct1/2 knockout on the pharmacokinetics and tissue partitioning of these OCT1 substrates in mice, whereas significantly different plasma concentrations have been reported in subjects with null OCT1 variants (18).
Understanding of species differences in transporter expression/activity is necessary due to the use of preclinical species in assessing drug pharmacokinetics/pharmacodynamics in discovery and development. Additionally, animal models offer potential advantages over cell lines and overcome limitations in clinical evaluations such as measurement of tissue concentrations. For some transporters, including OATPs and P-gp, knockout mice have been shown to be particularly robust and therefore aid in identification of the role of transporters in their respective tissues (19,20,21). Due to the observed clinical relevance of OCT1 variants on pharmacokinetics of OCT1 substrates, tools for identifying the potential role of OCT1 in the pharmacokinetics of an investigational drug including understanding of OCT1 activity in preclinical species have become essential. In the current research, we offer a comprehensive evaluation on interspecies OCT1 activity in the liver, using in vitro and in vivo methods, including a novel knockout rat model. These activity data are compared with expression of uptake transporters in hepatocytes. The expression of hepatic uptake transporters and other transporters relevant to drug disposition is also characterized in various tissues from rat and mouse.
METHODS
Materials
Sumatriptan succinate was purchased from Thermo Fisher Scientific (Waltham, MA). Metformin hydrochloride was purchased from U.S. Pharmacopeia (Rockville, MD). 3H-sumatriptan and 14C-metformin were purchased from American Radiolabeled Chemicals (St. Louis, MO). InVitroGRO HT medium, Krebs-Henseleit buffer (KHB), cryopreserved male human hepatocytes (lot BRB), female human hepatocytes (lot JYS), male rat hepatocytes (lots TUX and OSO), male dog hepatocytes (Lot YVT), and male monkey hepatocytes (lot UQS) were purchased from BioreclamationIVT (Westbury, NY). Rodent hepatocyte thawing medium and mouse hepatocytes (lot MBL192) were purchased from Lonza (Walkersville, MD). Buffers for cell culture and uptake (Dulbecco’s PBS, HEPES, MES) were purchased from Thermo Fisher Scientific (Waltham, MA). Digitonin, Triton™ X-100, ammonium bicarbonate, dithiothreitol, β-casein, sodium deoxycholate, iodoacetamide, and formic, acetic, and trifluoroacetic acids were purchased from Sigma-Aldrich (St. Louis, MO). The Thermo Scientific™ Pierce™ BCA Protein Assay Kit was obtained from VWR International LLC. (Radnor, PA). Acetonitrile (HPLC grade) was from Fisher Scientific (Pittsburg, PA). Trypsin Gold mass spectrometry grade was purchased from Promega (Madison, WI) (product # V5280). Purified water was obtained from an in-house PicoPure® 2 system (Hydro Service and Supplies, Inc., Durham, NC). All other chemicals were reagent grade. Stable isotope-labeled (SIL) (13C and 15N) proteotypic tryptic peptide standards were purchased from JPT Peptide Technologies (Berlin, Germany) (SpikeTides™_TQL; purified and calibrated). The peptides are supplied with a tryptic linker, used for determining concentration at the time of manufacture, at the C-terminus and therefore are added to samples before digestion so that the linker is released. Solid-phase extraction (SPE) cartridges were Strata™-X 33u Polymeric Reversed Phase (10 mg/ml, part no. 8B S100 AAK) and obtained from Phenomenex (Torrance, CA).
In vivo Rat Studies
Wild-type, Oct1−/− (model TGRS5600), and Oct2−/− (model TGRS6580) male Sprague Dawley rats were purchased from Envigo (Hackensack, NJ). Studies were carried out at Covance (Greenfield, IN) and were approved by the Institutional Animal Care and Use Committee. To evaluate the effect of Oct knockout on the pharmacokinetics of known OCT1 substrates, groups of wild-type, Oct1−/−, and Oct2−/− rats (n = 3, 230–350 g, age 8–14 weeks) were administered sumatriptan succinate or metformin hydrochloride intravenously (1 mg/kg, 2 mg/kg, or 5 mg/kg, 1 ml/kg in normal saline) via the tail vein and orally (5 mg/kg or 10 mg/kg, 10 ml/kg in purified water) by gavage. Rats were fasted prior to oral drug administration. Pharmacokinetic experiments were performed in metabolism cages. In pharmacokinetic experiments, serial blood samples (via the jugular vein) and urine were collected for 24 h. At the end of blood pharmacokinetic studies, nine tissues (liver, spleen, kidney, duodenum, heart, lung, brain, muscle, and testes) were collected for transporter quantitation via LC-MS/MS. Additional groups of wild-type, Oct1−/−, and Oct2−/− rats were administered each compound intravenously then sacrificed at 2 h (sumatriptan) or 4 h (metformin) post-dose for tissue collection to determine tissue concentrations; the same nine tissues were collected and snap-frozen in liquid nitrogen. Plasma, urine, and tissue samples were stored at <60°C until drug or transporter concentration analysis by LC-MS/MS.
To assess the effect of OCT1 inhibitors on the liver partitioning of OCT1 substrates in rats, male Sprague Dawley rats (n = 4, 200–400 g, age 8–14 weeks) were administered sumatriptan and metformin to steady state with and without verapamil or erlotinib. Rats were cannulated via the femoral and arterial vein and by the vendor. Rats were dosed OCT1 substrate at 2 mg/kg, at an infusion rate of 3 ml/kg/h for 8 h via the femoral vein. For groups administered OCT1 inhibitors, verapamil or erlotinib, was co-infused with substrate at doses of 120 mg/kg and 24 mg/kg, respectively. Serial blood samples were taken via the femoral artery up to 8 h, to ensure steady state was reached. At 8 h post-dose, the animals were sacrificed, and liver, kidney, and spleen were collected and snap-frozen in liquid nitrogen. These tissues were chosen due to their differential expression of individual’s Oct isoforms, as shown in the “Results” below. Plasma and tissue samples were stored at <60°C until drug concentration analysis by LC-MS/MS.
In vivo Monkey Liver Biopsy Study
Male monkeys were chosen from a stock colony maintained at Covance (Madison, WI). Studies were carried out at Covance (Madison, WI) and were approved by the Institutional Animal Care and Use Committee. Monkeys were fasted overnight prior to dosing and liver biopsy. Monkeys (n = 8, 2–5 kg, young adult to adult) were administered 1 mg/kg of metformin over a 30-min infusion via the saphenous vein. Blood was collected at 0.25 h, 0.42 h, 0.58 h, 1 h, 1.5 h, 2 h, 3 h, 4 h, 6 h, and 8 h post-dose. Liver was collected via laparoscopic biopsy in a staggered schedule. Each monkey underwent 3 total biopsy procedures, for a total of 2–4 liver samples each at 1 h, 1.5 h, 2 h, 3 h, 4 h, 6 h, and 12 h post-dose. Animals were placed under general anesthesia using ketamine and sevoflurane. Antibiotics were administered according to study-specific procedures. The abdomen was insufflated with CO2, and two trocars were positioned through the abdominal wall to provide access for the laparoscope and biopsy forceps. A biopsy sample was taken from the liver margin, weighed, and snap-frozen in liquid nitrogen. Plasma and tissue samples were stored at <60°C until drug concentration analysis by LC-MS/MS.
In vitro Uptake of OCT1 Substrates in Hepatocytes of Various Species
Uptake of 3H-sumatriptan and 14C-metformin was evaluated in cryopreserved primary mouse, rat, monkey, and human hepatocytes in suspension using the oil-spin method, as previously reported (16, 22), in the presence of 4% bovine serum albumin (BSA). Uptake was evaluated in triplicate at 1 μM at 37°C in the absence and presence of 1 mM 1-methyl-4-phenylpyridinium (MPP+). Aliquots of cell suspension were taken up to 15 min. Inhibition of sumatriptan (1 μM) and metformin (10 μM) uptake in rat hepatocytes by 1 μM and 25 μM verapamil was also assessed to correspond with in vivo rat investigations.
Quantitation of Transporter Expression and Drug Concentrations in Tissues and Hepatocytes
Whole tissues of rats and mice were obtained frozen and kept at −80°C until thawed on ice for the preparation of membrane fractions. For rats, the entire tissues, or half of tissue sample if >1000 mg, were added to 2 ml PBS buffer on ice then homogenized briefly with a Polytron for 3 s. An aliquot of 150 ml representing approximately 35–75 mg wet tissue was added to 1.9 ml digitonin buffer as the initial step in preparing the membrane fraction using an adapted differential surfactant extraction method (23). Mouse tissues were from 20 to 60 mg; thus, the entire tissue was homogenized in 2 ml of the digitonin buffer. The sequential surfactant extraction method was also used to extract the membrane fraction from hepatocytes. Quantitation of transporter expression was performed by nanoLC-MS/MS using SIL peptide standards as previously described (16, 24). Peptides monitored for the transporters quantified are given in Supplemental Table 1. Concentrations of Na+/K+-ATPase measured by nanoLC-MS/MS were consistent across wild-type and knockout rats within a particular tissue type and provided support for the effective extraction of the membrane fraction from each tissue type.
LC-MS/MS methods for quantitation of sumatriptan and metformin from in vitro and in vivo samples were also as previously described (16, 17).
Data Analysis
In vivo pharmacokinetic parameters in rats were determined by non-compartmental analysis using Watson 7.2. The area under the plasma concentration-time curve (AUC) was determined using the trapezoidal method. Renal clearance (CLR) was determined as Ae/AUC, where Ae represents the amount recovered in urine and AUC represents the area under the plasma concentration-time curve. The renal clearance was then corrected for creatinine recovery; the calculated CLR values were divided by [calculated creatinine renal clearance/reported creatinine clearance]. Creatinine renal clearance was calculated as above, and 10 ml/kg/min was used as creatinine clearance in rats. Serum creatinine and calculated creatinine clearance values were not different between wild-type and knockout rats. Hepatic clearance was determined as total CL-CLR. Bioavailability (F) was calculated as AUCPO/AUCIV, after accounting for differences in dose. Total tissue partitioning coefficient (Kp) values for knockout rat studies and OCT inhibition studies were calculated as tissue/plasma concentration, at a single timepoint. One-way ANOVA was used to determine statistically significant differences in pharmacokinetic parameters and tissue partitioning in knockout rats compared to wild-type rats or in rats in the absence/presence of inhibitors, using GraphPad Prism 8.1.1. To estimate Kpuu for sumatriptan and metformin in rodents, Kp was normalized to that in Oct1−/− rats or Oct1/2−/− mice, assuming Kpuu = 1 in knockout animals. For these calculations, mouse partitioning data were used from previous Oct1/2−/− studies (16), as well additional Kp values at 1.5 h following metformin IV (5 mg/g) and PO (10 mg/kg) administration. Kp values for metformin from monkey were calculated as tissue/plasma concentrations, for each individual matched sample timepoint.
Active uptake of sumatriptan and metformin in hepatocytes over time was determined by subtracting that in the presence of MPP+ from that in its absence, for each timepoint assessed.
RESULTS
The pharmacokinetics of sumatriptan and metformin following IV and PO administration to wild-type and Oct knockout rats are given in Table I. The plasma profiles are shown in Fig. 1. Oct expression in wild-type and knockout rats is shown in Supplemental Fig. 1 and indicates deletion of the intended Oct protein. There was no change in knockout rats for any other transporters assessed (data not shown). As discussed in detail below, Oct1 was detected in the liver and kidney in rats, while Oct2 was limited to the kidney. For sumatriptan, a decrease in the hepatic and total clearance was observed in Oct1−/− rats compared to wild type, with a corresponding decrease in the liver Kp (Fig. 2). The renal clearance was unaffected, as was the partitioning in the kidney or any other tissue. The AUC following oral administration was also correspondingly increased, although the bioavailability was not significantly increased. There was no change in sumatriptan pharmacokinetics with knockout of Oct2. Conversely, the pharmacokinetics and tissue partitioning of metformin were not affected by single knockout of Oct1 or Oct2 in these rat models (Table I, Figs. 1 and 2).
Plasma concentrations of sumatriptan a and b and metformin c and d in wild-type and Oct1 or Oct2 knockout rats. Rats were administered 2 mg/kg (sumatriptan) or 5 mg/kg (metformin) intravenously a and c and 5 mg/kg (sumatriptan) or 10 mg/kg (metformin) orally b and d. Data are presented as mean ± SD, n = 3
Partitioning of sumatriptan and metformin in wild-type and Oct1 and Oct2 knockout rats. Rats administered sumatriptan 1 mg/kg IV were sacrificed at 2 h post-dose. Rats administered metformin 5 mg/kg IV were sacrificed at 4 h post-dose. Data are presented as mean ± SD, n = 3. Kp is the tissue partition coefficient
In rat hepatocytes, uptake of both sumatriptan and metformin was inhibited by verapamil (Fig. 3). For sumatriptan, inhibition was similar at 1 μM verapamil and 25 μM, indicating that even 1 μM was sufficient for complete OCT1 inhibition. However, for metformin, less inhibition was observed at 1 μM verapamil compared with that at 25 μM, indicating that 1 μM was insufficient for complete OCT1 inhibition of metformin uptake in rat hepatocytes. Correspondingly, in wild-type rats, the steady-state liver Kp of sumatriptan was decreased in the presence of OCT1 inhibitors verapamil and erlotinib (Fig. 3). In contrast, after infusion of the same doses of verapamil and erlotinib in wild-type rats, no effect on the steady-state liver partitioning of metformin was observed. The unbound steady-state concentrations of verapamil obtained were 0.58–0.97 μM in these studies, and those of erlotinib were 0.82–1.8 μM. Serial sampling up until the terminal timepoint confirmed both substrates and inhibitors reached steady state at the timepoint sampled.
Effect of OCT1 inhibitors on uptake into rat hepatocytes and on steady-state rat liver partitioning. Upper figures show uptake into rat hepatocytes, in the presence and absence of OCT1 inhibitor verapamil (25 μM). Experiments were performed in triplicate, data presented as mean ± SD. Lower 6 figures show partitioning in rat tissues after 8 h of infusion of 2 mg/kg substrate, with and without co-infusion of OCT1 inhibitors, verapamil (120 mg/kg) or erlotinib (24 mg/kg); n = 4, data shown as mean ± SD. Kp is the tissue partition coefficient
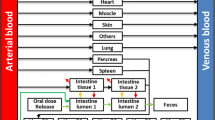
Protein expression levels of Oatps, Octs, and other transporters in tissues from wild-type mice and rats are shown in Figs. 4 and 5, respectively. Absolute concentrations determined are detailed in Supplemental Table 2. The concentrations of membrane marker protein Na+/K+-ATPase measured in each tissue are shown in Supplemental Fig. 2, indicating a wide range of values between tissues but little variability in the same tissue from different animals. Expression of multiple Oatps was high in the liver of both species. However, in both species, expression of Oatp1a and Oatp2a1 was high in other tissues. In contrast to the Oatps, a single Oct was predominant in single tissues. Oct1 was the only Oct detected in the liver of both rat and mouse. Oct2 expression in the kidney was highest of any uptake transporter, which is consistent with other functional studies demonstrating altered renal clearance of OCT2 substrates in Oct1/2−/− mice (16, 17, 25). Oct1 was also found in the kidney of both species, however at much lower levels than Oct2. Oct2 was also detected in the duodenum of mice, but not in rats, an observation we are unaware of having been previously reported. Although Oct1 protein has been determined present at least in mouse intestine (26), in our measurements, Oct1 was below the limit of quantitation in both species. Effect of Oct1 knockout on intestinal partitioning was also previously demonstrated (26), suggesting it may be present at concentrations below our current detection limit. Oct3 was expressed in tissues lacking Oct1 or Oct2, including the heart, lung, and spleen of both species, consistent with Oct3 messenger RNA (mRNA) expression data (27, 28). Liver Oct3 expression was below the limit of quantitation in both species, although others have reported Oct3 mRNA expression in mouse and rat liver, albeit low compared to Oct1 (27, 28).
Transporter expression in mouse tissues. Transporter measurement was performed using nanoLC/MS-MS, as described in the “METHODS,” on tissues from wild-type mice. Concentrations are in units of pmol per mg of membrane protein. Data are presented as mean ± SD, n = 4. Note: Oatp2b1 could not be detected in liver tissue extract possibly due to peak interference for both MRMs
Transporter expression in rat tissues. Transporter measurement was performed using nanoLC/MS-MS, as described in the “METHODS,” on tissues from wild-type rats. Concentrations are in units of pmol per mg of membrane protein. Data are presented as mean ± SD, n = 3. Note: Oatp2b1 could not be detected in liver tissue extract possibly due to peak interference for both MRMs
Expression of OATP/Oatp and OCT1/Oct1 protein in hepatocytes from varying species is shown in Fig. 6. As shown in Supplemental Fig. 2, the membrane marker protein Na+/K+-ATPase could be measured in hepatocytes from all 5 species. Direct interspecies comparison of OCT1/Oct1 protein is shown in Fig. 7, along with the corresponding uptake of OCT1 substrates in these hepatocytes and the in vivo liver partitioning of OCT1 substrates in rodents and monkey. High expression of OATPS/Oatps was found in the hepatocytes of every species, consistent with previous data (23, 24, 29). The distribution of individual OATPs in hepatocytes of each species is also in general agreement with distributions previously reported (29, 30). Oct1 expression was highest in monkey hepatocytes (Fig. 7a), in agreement with previous data (29). We determined human hepatocytes to have the next highest expression of OCT1, and Oct1 expression in hepatocytes of both rat and mice to be lower than OCT1 in human hepatocytes, which differs from other recent reports and is discussed below. With regard to OCT1 activity, the highest active intracellular accumulation for both sumatriptan and metformin was demonstrated in monkey hepatocytes, compared to that of other species (Fig. 7b and c). It was difficult to compare the initial active uptake rates given the very rapid accumulation of sumatriptan, particularly in monkey. It was apparent that active intracellular accumulation was lowest in human hepatocytes for both substrates, with activity in rodent species between that of human and that of monkey. We did attempt to evaluate OCT1-mediated uptake in dog hepatocytes and found no inhibition of sumatriptan uptake by MPP+. Previous results indicate low expression of Oct1 in dogs (29), which we also determined, along with negligible active uptake. Corresponding with activity in hepatocytes, the in vivo liver partitioning of sumatriptan and metformin was similar when compared between mice and rats (Fig. 7d and e). Metformin liver partitioning was higher in monkey than in either rodent species (Fig. 7f).
Expression of uptake transporters in hepatocytes from different species. Transporter measurement was performed using nanoLC/MS-MS, as described in the “METHODS.” Concentrations are in units of pmol per mg of membrane protein in each lot and were performed in duplicate; mean data are shown
Comparison of OCT1/Oct1 protein in hepatocytes a, active uptake of OCT1 substrates into hepatocytes b and c, and liver partitioning of OCT1 substrates d–f in different species. a Transporter measurement was performed using nanoLC/MS-MS, as described in the “METHODS.” Protein concentrations are presented as pmol per mg of membrane protein in each lot and were performed in duplicate; mean data are shown. Uppercase letters in parentheses indicate different lots of hepatocytes. b, c Experiments were performed in triplicate; data presented as mean ± SD. Data shown represent active uptake, after subtracting passive from total uptake at each timepoint. d Total partitioning (Kp) of sumatriptan was assessed in mice and rats administered 2 mg/kg IV and sacrificed at 2 h post-dose; data presented as mean ± SD. e Kpuu for sumatriptan was calculated by dividing Kp in wild-type animals with that in Oct1/2 or Oct1 knockout animals, for mouse and rat, respectively; data presented as mean ± SD. f Total partitioning (Kp) of metformin was assessed in mice and rats administered 5 mg/kg IV or 10 mg/kg PO and sacrificed at 1.5 or 4 h post-dose. Total partitioning (Kp) in monkey was assessed via liver biopsy sampling over 12 h following IV administration of 1 mg/kg
DISCUSSION
Transporter expression results from wild-type rat tissues indicate the potential role of Oct1 in the liver, and possibly both Oct1 and Oct2 in the kidney. Accordingly, the decrease in both hepatic clearance and partitioning of sumatriptan in Oct1−/− rats coincides with the uptake into the liver mediated by Oct1. The decrease in hepatic clearance in Oct1−/− rats is comparable to the 4-fold change observed in Oct1/2−/− mice, and the 2-fold change in oral clearance is similar to that observed in Oct1/2−/− mice and in human carriers of OCT1 null variants. Sumatriptan undergoes some degree of renal excretion in all 3 species. Although sumatriptan is an OCT2 substrate (16), no difference in the pharmacokinetics was observed in Oct2−/− rats, despite the renal clearance of sumatriptan in rats which suggests net secretion. Given the single knockout of individual Octs in the kidney, it is possible that Oct1 compensated for Oct2 deletion. Although the current data suggest Oct1 expression to be quantitatively lower than Oct2 and expression was not increased in the Oct2−/− rat, these results are, however, consistent with previous mouse data, in which sumatriptan also undergoes net secretion yet was not affected by complete deletion of Octs (1 and 2) in the kidney (16). Overall, these data support a mechanism other than Oct1/2 for renal secretion of sumatriptan in rodents. In contrast to sumatriptan, the pharmacokinetics of metformin were not different in Oct1−/− rats, compared to wild-type rats, nor affected in Oct2−/− rats. Renal clearance is the primary route of elimination for metformin, in rodents and humans. In the current study, it is again possible that one Oct compensated for deletion of the other in the kidney. This was observed in single Oct1−/− or Oct2−/− mouse, in which single knockout did not affect plasma pharmacokinetics whereas double knockout dramatically affected pharmacokinetics of metformin and other cations (17, 25, 31). The lack of change in Oct2−/− rats is still somewhat surprising given the much higher expression of Oct2 in the kidney compared to Oct1. Also unexpected is the lack of change in tissue partitioning, particularly in the liver of Oct1−/− rats, given the data with sumatriptan indicating functional OCT1 change in the liver. This may be an artifact of the single-timepoint, non-steady-state tissue assessment; however, the metformin liver Kp values in the knockout rat studies (Fig. 2) were similar to those obtained at steady state in the OCT1 inhibition experiments (Fig. 3) and it has been previously demonstrated that metformin liver partitioning in rats is similar at 4 h to earlier timepoints (32). Therefore, a more likely explanation may be that compensatory mechanisms are present in the rat knockout model, given that metformin is a substrate of multiple transporters in both the liver and kidney, all of which were not monitored for currently (33). These data contrast with that of altered metformin liver partitioning in Oct1−/− or Oct1/2−/− mice and in subjects carrying null OCT1 variants (15, 17, 26).
As mentioned above, there is a lack of reported clinical DDIs with known OCT1 substrates, although there are known inhibitors used in the clinic, some of which have been demonstrated to be quite potent (12, 34). One reason for this may simply be a lack of formal investigation. As the effects of complete knockout of OCT1 activity in subjects with null variants tend to be somewhat moderate, ~2-fold increase in plasma concentrations, OCT1-mediated DDIs may only manifest to minor changes in plasma concentrations or risk of adverse events/decreased efficacy. To assess the proof of concept that OCT1 could be inhibited in vivo, we chose to perform this assessment in rats due to the ability to reach high systemic concentrations of inhibitors. The one reported DDI attributed to hepatic OCT1 is that of verapamil on metformin, an indirect assessment of liver distribution through pharmacodynamic effects (11). Since both sumatriptan and metformin could be inhibited in rat hepatocytes in vitro, we assessed both substrates with verapamil and also evaluated infusion of erlotinib, a reportedly more specific OCT1 inhibitor (35). While the effect of the inhibitors on sumatriptan partitioning is not surprising, given the data in Oct1−/− rats (Fig. 3), it does represent one of the first direct measurements of in vivo liver OCT1 inhibition. The fact that the same inhibitors did not affect metformin partitioning was somewhat surprising, particularly with verapamil for which a clinical DDI is reported. The unbound steady-state concentration of verapamil reached just under 1 μM at the dose used. From in vitro experiments, it appears that maximal inhibition of sumatriptan uptake could be achieved at this concentration, but not that for metformin. Therefore, a plausible explanation is that the potency for verapamil against rat OCT1 is substrate dependent, which is consistent with previous reports for OCTs (36, 37), and that in vivo verapamil concentrations were insufficient to affect metformin liver uptake by rat Oct1 in vivo.
The expression of transporters in various tissues of various species has been separately reported, primarily by mRNA expression. More recently, protein quantitation using LC/MS-MS methods has been used to assess the expression of transporters in select cell types/tissues from human and rodents (23, 24, 29, 30, 38,39,40). However, we are unaware of any quantitative comparison of uptake and efflux transporter protein expression across multiple tissues even in any one species. Here, we report the expression of 18 transporters in 9 tissues from mice and rats. This aids in the interpretation of the current data regarding Oct1 activity and in the understanding of known pharmacokinetics/pharmacodynamics properties of many transporter substrates, including those in the many available transporter knockout and humanized animal/rodent models. While providing a broad comparison, a limitation of the current data should be noted in that expression in whole tissues was assessed, not that in specific functional cells of each organ. Therefore, samples for certain tissues may be diluted representations and lack of detection could be falsely negative and should not be overinterpreted. This is possibly why the expression of P-gp determined in many of the tissues is low and we did not determine Oct1 detectable in the intestine. In addition, the absence of Oatp2b1 in mouse and rat liver extracts (Figs. 4 and 5) could, we believe, be attributed to interference peaks for both MRMs used to quantitate Oatp2b1, obscuring the visibility of the representative peptide. Some tissues, particularly the liver, are made up primarily of their functional cells. Accordingly, and similar to what previously reported, we found high expression of Oatps in hepatocytes of all species, and data in rat and mouse hepatocytes correlated well with the expression determined in liver samples. Regarding the activity in the liver, the uptake of multiple OATP substrates in hepatocytes from preclinical species has been previously evaluated and compared to that in human. In these studies, uptake into rat hepatocytes was 7.1-fold higher than that in human hepatocytes, uptake into dog hepatocytes was as much as 5 times greater than that in human, and uptake in monkey hepatocytes was demonstrated generally similar to that in human (41,42,43,44).
The interspecies comparison of OCT1/Oct1 expression and activity appear to differ somewhat with that of the Oatps. We determined low comparable expression of Oct1 to Oatps in rodent liver/hepatocytes and somewhat comparable expression of OCT1 to OATPs in both human and monkey hepatocytes, results which are both similar to previously reported (23, 29). We also currently report lower expression of Oct1 in rodents compared to that in human, which is somewhat in contrast with other reports. Meyer et al. (45) just recently reported similar expression of OCT1 in the human and mouse liver. While our data in mouse hepatocytes are quantitatively similar to their report in mouse liver, we determined human hepatocytes to be higher than those in their study and more quantitatively consistent with that in the human liver reported by Wang et al. (29, 46). Wang et al. reported somewhat lower expression of Oct1 in the rat liver compared to human, albeit not as large of a difference as we currently report. In contrast, regarding OCT1 activity, we determined similar or greater active uptake of OCT1 substrates in both mouse and rat hepatocytes compared to human (Fig. 7). Meyer et al. (45) also reported the Km for metformin to be lower for mouse Oct1 than human OCT1, in overexpressing cells. Considering this, the expression of Oct1 may indeed be lower in rodents and the activity is maintained with increased affinity. A lower Km value for metformin in rat hepatocytes, compared to human, has also been previously reported (47). It is important to consider that the expression levels we report are in at most 2 lots of hepatocytes per species, with the aim to compare expression/activity in the same hepatocytes and may not quantitatively represent each species population as a whole. Conversely, the expression/activity we report in monkey is more clear, in that increased active accumulation of OCT1 substrates correlated well with the highest expression of OCT1 in monkey hepatocytes (Fig. 7). This is also in agreement with one previous assessment of transporter activity across hepatocytes of various species, demonstrating higher metformin uptake in monkey than rat or human hepatocytes (48). Here, we confirm this with an arguably more specific OCT1 probe, sumatriptan, for which decreased OCT1 function has been linked to decreased hepatic clearance in humans, mice, and now, rats. As a metabolically stable compound, the comparison of metformin in mice, rats, and monkey allows for a fair comparison of metformin partitioning in the liver due to active transport. Again, the high metformin liver Kp in monkey is consistent with the highest Oct1 expression and activity in monkey hepatocytes. High metformin partitioning in monkeys is also supported by previous data, in which a Kpuu value of 15 was reported (49).
CONCLUSIONS
As demonstrated with the OATPs, there exist species differences in OCT1 expression and activity in hepatocytes. While rodents are particularly a robust model for hepatic uptake via Oatps, considering the data for probe OCT1 substrate sumatriptan in hepatocytes and in knockout models, activity of OCT1 in rodents appears more comparable to that in human hepatocytes and carriers of null OCT1 variants. Monkeys appear the most robust preclinical species for assessing/confirming a role of OCT1 in vitro and in vivo, albeit come with certain limitations, including and not limited to availability and difficulty in assessing tissue partitioning compared to rodents.
References
Shitara Y, Maeda K, Ikejiri K, Yoshida K, Horie T, Sugiyama Y. Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: their roles in hepatic clearance and intestinal absorption. Biopharm Drug Dispos. 2013;34(1):45–78.
Maeda K, Ohnishi A, Sasaki M, Ikari Y, Aita K, Watanabe Y, et al. Quantitative investigation of hepatobiliary transport of [(11)C]telmisartan in humans by PET imaging. Drug Metab Pharmacokinet. 2019;34(5):293–9.
Billington S, Shoner S, Lee S, Clark-Snustad K, Pennington M, Lewis D, et al. Positron emission tomography imaging of [(11) C]rosuvastatin hepatic concentrations and hepatobiliary transport in humans in the absence and presence of cyclosporin A. Clin Pharmacol Ther. 2019;106(5):1056–66.
Yee SW, Giacomini MM, Shen H, Humphreys WG, Horng H, Brian W, et al. Organic anion transporter polypeptide 1B1 polymorphism modulates the extent of drug-drug interaction and associated biomarker levels in healthy volunteers. Clin Transl Sci. 2019;12(4):388–99.
Tzvetkov MV, Matthaei J, Pojar S, Faltraco F, Vogler S, Prukop T, et al. Increased Systemic exposure and stronger cardiovascular and metabolic adverse reactions to fenoterol in individuals with heritable OCT1 deficiency. Clin Pharmacol Ther. 2018;103(5):868–78.
Matthaei J, Seitz T, Jensen O, Tann A, Prukop T, Tadjerpisheh S, et al. OCT1 deficiency affects hepatocellular concentrations and pharmacokinetics of cycloguanil, the active metabolite of the antimalarial drug proguanil. Clin Pharmacol Ther. 2019;105(1):190–200.
Matthaei J, Kuron D, Faltraco F, Knoch T, Dos Santos Pereira JN, Abu Abed M, et al. OCT1 mediates hepatic uptake of sumatriptan and loss-of-function OCT1 polymorphisms affect sumatriptan pharmacokinetics. Clin Pharmacol Ther. 2015.
Tzvetkov MV, dos Santos Pereira JN, Meineke I, Saadatmand AR, Stingl JC, Brockmoller J. Morphine is a substrate of the organic cation transporter OCT1 and polymorphisms in OCT1 gene affect morphine pharmacokinetics after codeine administration. Biochem Pharmacol. 2013;86(5):666–78.
Shu Y, Leabman MK, Feng B, Mangravite LM, Huang CC, Stryke D, et al. Evolutionary conservation predicts function of variants of the human organic cation transporter, OCT1. Proc Natl Acad Sci U S A. 2003;100(10):5902–7.
Shu Y, Sheardown SA, Brown C, Owen RP, Zhang S, Castro RA, et al. Effect of genetic variation in the organic cation transporter 1 (OCT1) on metformin action. J Clin Invest. 2007;117(5):1422–31.
Cho SK, Kim CO, Park ES, Chung JY. Verapamil decreases the glucose-lowering effect of metformin in healthy volunteers. Br J Clin Pharmacol. 2014;78(6):1426–32.
Koepsell H. Organic cation transporters in health and disease. Pharmacol Rev. 2020;72(1):253–319.
Chen EC, Khuri N, Liang X, Stecula A, Chien HC, Yee SW, et al. Discovery of competitive and noncompetitive ligands of the organic cation transporter 1 (OCT1; SLC22A1). J Med Chem. 2017;60(7):2685–96.
Drozdzik M, Busch D, Lapczuk J, Muller J, Ostrowski M, Kurzawski M, et al. Protein abundance of clinically relevant drug transporters in the human liver and intestine: a comparative analysis in paired tissue specimens. Clin Pharmacol Ther. 2019;105(5):1204–12.
Jensen JB, Sundelin EI, Jakobsen S, Gormsen LC, Munk OL, Frokiaer J, et al. [11C]-Labeled metformin distribution in the liver and small intestine using dynamic positron emission tomography in mice demonstrates tissue-specific transporter dependency. Diabetes. 2016;65(6):1724–30.
Morse BL, Kolur A, Hudson LR, Hogan AT, Chen LH, Brackman RM, et al. Pharmacokinetics of organic cation transporter 1 (OCT1) substrates in Oct1/2 knockout mice and species difference in hepatic OCT1-mediated uptake. Drug Metab Dispos. 2020;48(2):93–105.
Higgins JW, Bedwell DW, Zamek-Gliszczynski MJ. Ablation of both organic cation transporter (OCT)1 and OCT2 alters metformin pharmacokinetics but has no effect on tissue drug exposure and pharmacodynamics. Drug Metab Dispos. 2012;40(6):1170–7.
Tzvetkov MV, Saadatmand AR, Bokelmann K, Meineke I, Kaiser R, Brockmoller J. Effects of OCT1 polymorphisms on the cellular uptake, plasma concentrations and efficacy of the 5-HT(3) antagonists tropisetron and ondansetron. Pharmacogenomics J. 2012;12(1):22–9.
Chen C, Liu X, Smith BJ. Utility of Mdr1-gene deficient mice in assessing the impact of P-glycoprotein on pharmacokinetics and pharmacodynamics in drug discovery and development. Curr Drug Metab. 2003;4(4):272–91.
Salphati L, Chu X, Chen L, Prasad B, Dallas S, Evers R, et al. Evaluation of organic anion transporting polypeptide 1B1 and 1B3 humanized mice as a translational model to study the pharmacokinetics of statins. Drug Metab Dispos. 2014;42(8):1301–13.
Higgins JW, Bao JQ, Ke AB, Manro JR, Fallon JK, Smith PC, et al. Utility of Oatp1a/1b-knockout and OATP1B1/3-humanized mice in the study of OATP-mediated pharmacokinetics and tissue distribution: case studies with pravastatin, atorvastatin, simvastatin, and carboxydichlorofluorescein. Drug Metab Dispos. 2014;42(1):182–92.
Morse BL, Cai H, MacGuire JG, Fox M, Zhang L, Zhang Y, et al. Rosuvastatin liver partitioning in cynomolgus monkeys: measurement in vivo and prediction using in vitro monkey hepatocyte uptake. Drug Metab Dispos. 2015;43(11):1788–94.
Qasem RJ, Fallon JK, Nautiyal M, Mosedale M, Smith PC. Differential detergent fractionation of membrane protein from small samples of hepatocytes and liver tissue for quantitative proteomic analysis of drug metabolizing enzymes and transporters. J Pharm Sci. 2020.
Khatri R, Fallon JK, Rementer RJB, Kulick NT, Lee CR, Smith PC. Targeted quantitative proteomic analysis of drug metabolizing enzymes and transporters by nano LC-MS/MS in the sandwich cultured human hepatocyte model. J Pharmacol Toxicol Methods. 2019;98:106590.
Jonker JW, Wagenaar E, Van Eijl S, Schinkel AH. Deficiency in the organic cation transporters 1 and 2 (Oct1/Oct2 [Slc22a1/Slc22a2]) in mice abolishes renal secretion of organic cations. Mol Cell Biol. 2003;23(21):7902–8.
Jonker JW, Wagenaar E, Mol CA, Buitelaar M, Koepsell H, Smit JW, et al. Reduced hepatic uptake and intestinal excretion of organic cations in mice with a targeted disruption of the organic cation transporter 1 (Oct1 [Slc22a1]) gene. Mol Cell Biol. 2001;21(16):5471–7.
Slitt AL, Cherrington NJ, Hartley DP, Leazer TM, Klaassen CD. Tissue distribution and renal developmental changes in rat organic cation transporter mRNA levels. Drug Metab Dispos. 2002;30(2):212–9.
Chen EC, Liang X, Yee SW, Geier EG, Stocker SL, Chen L, et al. Targeted disruption of organic cation transporter 3 attenuates the pharmacologic response to metformin. Mol Pharmacol. 2015;88(1):75–83.
Wang L, Prasad B, Salphati L, Chu X, Gupta A, Hop CE, et al. Interspecies variability in expression of hepatobiliary transporters across human, dog, monkey, and rat as determined by quantitative proteomics. Drug Metab Dispos. 2015;43(3):367–74.
Ishida K, Ullah M, Toth B, Juhasz V, Unadkat JD. Successful prediction of in vivo hepatobiliary clearances and hepatic concentrations of rosuvastatin using sandwich-cultured rat hepatocytes, transporter-expressing cell lines, and quantitative proteomics. Drug Metab Dispos. 2018;46(1):66–74.
Wang DS, Jonker JW, Kato Y, Kusuhara H, Schinkel AH, Sugiyama Y. Involvement of organic cation transporter 1 in hepatic and intestinal distribution of metformin. J Pharmacol Exp Ther. 2002;302(2):510–5.
Wilcock C, Wyre ND, Bailey CJ. Subcellular distribution of metformin in rat liver. J Pharm Pharmacol. 1991;43(6):442–4.
Liang X, Giacomini KM. Transporters involved in metformin pharmacokinetics and treatment response. J Pharm Sci. 2017;106(9):2245–50.
Minuesa G, Volk C, Molina-Arcas M, Gorboulev V, Erkizia I, Arndt P, et al. Transport of lamivudine [(-)-beta-L-2',3'-dideoxy-3'-thiacytidine] and high-affinity interaction of nucleoside reverse transcriptase inhibitors with human organic cation transporters 1, 2, and 3. J Pharmacol Exp Ther. 2009;329(1):252–61.
Minematsu T, Giacomini KM. Interactions of tyrosine kinase inhibitors with organic cation transporters and multidrug and toxic compound extrusion proteins. Mol Cancer Ther. 2011;10(3):531–9.
Koepsell H. Multiple binding sites in organic cation transporters require sophisticated procedures to identify interactions of novel drugs. Biol Chem. 2019;400(2):195–207.
Belzer M, Morales M, Jagadish B, Mash EA, Wright SH. Substrate-dependent ligand inhibition of the human organic cation transporter OCT2. J Pharmacol Exp Ther. 2013;346(2):300–10.
Uchida Y, Toyohara T, Ohtsuki S, Moriyama Y, Abe T, Terasaki T. Quantitative targeted absolute proteomics for 28 transporters in brush-border and basolateral membrane fractions of rat kidney. J Pharm Sci. 2016;105(2):1011–6.
Fallon JK, Houvig N, Booth-Genthe CL, Smith PC. Quantification of membrane transporter proteins in human lung and immortalized cell lines using targeted quantitative proteomic analysis by isotope dilution nanoLC-MS/MS. J Pharm Biomed Anal. 2018;154:150–7.
Fallon JK, Smith PC, Xia CQ, Kim MS. Quantification of four efflux drug transporters in liver and kidney across species using targeted quantitative proteomics by isotope dilution nanoLC-MS/MS. Pharm Res. 2016;33(9):2280–8.
Menochet K, Kenworthy KE, Houston JB, Galetin A. Simultaneous assessment of uptake and metabolism in rat hepatocytes: a comprehensive mechanistic model. J Pharmacol Exp Ther. 2012;341(1):2–15.
Menochet K, Kenworthy KE, Houston JB, Galetin A. Use of mechanistic modeling to assess interindividual variability and interspecies differences in active uptake in human and rat hepatocytes. Drug Metab Dispos. 2012;40(9):1744–56.
Matsunaga N, Ufuk A, Morse BL, Bedwell DW, Bao J, Mohutsky MA, et al. Hepatic organic anion transporting polypeptide-mediated clearance in the beagle dog: assessing in vitro-in vivo relationships and applying cross-species empirical scaling factors to improve prediction of human clearance. Drug Metab Dispos. 2019;47(3):215–26.
De Bruyn T, Ufuk A, Cantrill C, Kosa RE, Bi YA, Niosi M, et al. Predicting human clearance of organic anion transporting polypeptide substrates using cynomolgus monkey: in vitro-in vivo scaling of hepatic uptake clearance. Drug Metab Dispos. 2018;46(7):989–1000.
Meyer MJ, Tuerkova A, Romer S, Wenzel C, Seitz T, Gaedcke J, et al. Differences in metformin and thiamine uptake between human and mouse organic cation transporter 1: structural determinants and potential consequences for intrahepatic concentrations. Drug Metab Dispos. 2020;48(12):1380–92.
Wang L, Collins C, Kelly EJ, Chu X, Ray AS, Salphati L, et al. Transporter expression in liver tissue from subjects with alcoholic or hepatitis C cirrhosis quantified by targeted quantitative proteomics. Drug Metab Dispos. 2016;44(11):1752–8.
Umehara KI, Iwatsubo T, Noguchi K, Kamimura H. Functional involvement of organic cation transporter1 (OCT1/Oct1) in the hepatic uptake of organic cations in humans and rats. Xenobiotica. 2007;37(8):818–31.
Liao M, Zhu Q, Zhu A, Gemski C, Ma B, Guan E, et al. Comparison of uptake transporter functions in hepatocytes in different species to determine the optimal model for evaluating drug transporter activities in humans. Xenobiotica. 2019;49(7):852–62.
Morse BL, MacGuire JG, Marino AM, Zhao Y, Fox M, Zhang Y, et al. Physiologically based pharmacokinetic modeling of transporter-mediated hepatic clearance and liver partitioning of OATP and OCT substrates in cynomolgus monkeys. AAPS J. 2017;19(6):1878–89.
Author information
Authors and Affiliations
Contributions
Bridget L. Morse, Pharm.D./Ph.D., is a Principal Research Scientist in the Drug Disposition Department at Lilly Research Laboratories, Indianapolis, IN. She received her Pharm.D. from Butler University in Indianapolis and her Ph.D. from the University at Buffalo, followed by a postdoctoral fellowship at the University of Western Ontario. Dr. Morse worked in the transporter group within the Department of Metabolism and Pharmacokinetics at Bristol Myers-Squibb for 2 years prior to joining Eli Lilly in 2016. At Lilly, she serves as a subject matter expert in pharmacokinetics, transporters, and drug-drug interactions, particularly in the use of PBPK modeling for hepatic transporter substrates and interspecies translation of hepatic disposition. Dr. Morse has published over 20 journal articles and a chapter on Membrane Drug Transporters in both the 7th and 8th editions of Foye’s Principles of Medicinal Chemistry. She is currently Chair-elect of the AAPS Drug Transporter Community.
Kathleen M. Hillgren, Ph.D., is a Research Fellow in the Drug Disposition Department at Lilly Research Laboratories, Indianapolis, IN. She received her doctorate in Pharmaceutical Chemistry from the University of Kansas and then spent 2 years at the University of California at San Francisco as a postdoctoral fellow. After her fellowship, Dr. Hillgren worked at Rhone-Poulenc Rorer in the Department of Drug Metabolism and Pharmacokinetics where she was responsible for coordinating the preclinical development of drug candidates and in vitro drug absorption models. Dr. Hillgren joined Eli Lilly in 1999. At Lilly, she founded and developed the transporter research group within the Drug Disposition Department, developing assays to study the role of transporters and their pharmacogenomics in the absorption, distribution, and elimination of drugs and metabolites from early discovery through registration. Her research interests include prediction of clinical drug-drug interactions at transporters, transporter pharmacogenomics, and utilization of intestinal transporters for drug delivery. Dr. Hillgren is a charter member and an active participant of the International Transporter Consortium. She is also co-chair of the IQ Consortium’s Transporter Working Group.
Corresponding author
Additional information
Guest Editors: Diane Burgess, Marilyn Morris and Meena Subramanyam
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 116 kb)
Rights and permissions
About this article
Cite this article
Morse, B.L., Fallon, J.K., Kolur, A. et al. Comparison of Hepatic Transporter Tissue Expression in Rodents and Interspecies Hepatic OCT1 Activity. AAPS J 23, 58 (2021). https://doi.org/10.1208/s12248-021-00583-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-021-00583-z