Abstract
The manuscript presents a pilot study of the impact of orthodontic intervention on the brain electrical activity. The orthodontic treatment is a powerful factor of both physiological influence on the jaw system and the surrounding tissues of the head and stress influence. All practically healthy subjects of the same age category (18–25 years) were distributed among three groups based on the method of orthodontic treatment. Group 1 included patients using braces, groups 2 and 3 included patients using aligners in which pressure was applied to 3–5 or 1–2 teeth, respectively. Brain activity electroencephalographic data were collected twice during neurophysiological monitoring: before and after orthodontic correction. The collected data sets included EEG signals from the occipital region of the brain. Numerical processing was performed based on continuous wavelet analysis to estimate the number and duration of oscillatory patterns in narrow frequency bands from 1 to 50 Hz. An assessment of the oscillatory brain activity demonstrated that different grades of correction intensity, regarding the dentition and occlusion, lead to uniform changes in the oscillatory patterns assessed by the electroencephalography in the occipital lobe. Comparison of the number of oscillatory patterns in the groups showed significant changes in the high-frequency \(\bigcup _\textrm{HF} \ni \left\{ \left[ 16;18\right] , \left[ 20;28\right] , \left[ 32;34\right] , \left[ 42;50\right] \right\}\) Hz. The number of patterns in the \(\bigcup _\textrm{HF}\)-band increases when using the most intense bracket devices; while in cases of more gentle correction based on aligner systems, it remains unchanged or even decreases. The independent clustering procedure by assessing changes in oscillatory processes of \(\bigcup _\textrm{HF}\)-band occurring in a single occipital O1-canal made it possible to divide the data array into three clusters. The clusters of changes in brain activity correspond to clinical groups of patients. Thus, different types of dental exposure lead to significantly different changes in the brain activity of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
This manuscript is devoted to investigating changes in the oscillatory electrical activity of the brain under the impact of pronounced somatic stress caused by medical orthodontic procedures. Currently, the study of brain activity from the standpoint of nonlinear dynamics methodology and the theory of dynamic chaos is the mainstream of neuroscience.
Stress and noticeable pain effects almost always accompany orthodontic correction. Orthodontic pain and discomfort in some cases can be so significant that it leads patients to abandon orthodontic treatment without specialist supervision [1]. There are many papers investigating the effects of different psychological interventions on the duration and severity of this type of pain, a meta-review of which is given, for example, in Feng et al. [2]. Among such psychological practices considered were cognitive behavioral therapy (CPT) [3], music therapy [4], structured online and or telephone monitoring of patients, et al. Apparently, in the short term after initial orthodontic procedure, all psychological interventions significantly reduced the pain intensity without significant differences [2]. The understandable weaknesses of such studies are due to the inability to use of placebo control group and double-blind control to separate groups of patients make comparative studies of such techniques particularly challenging. Nevertheless, some studies of music therapy for pain demonstrate no differences in pain level reduction for different types of music [5], and even music exposure and CPT [6], but significant reductions compared to a control group without any therapy. At the same time, the level of pain sensation is a highly individual patient characteristic, perhaps more related to the patient’s neuropsychological status and even cognitive function states than to the severity of orthodontic effects [7]. At the same time, moving away from the subjective and poorly measurable concept of pain, it should be noted that the configuration of the dentoalveolar system in orthodontic patients in the course of treatment changes significantly objectively as a result of bone formation on the extension side and bone resorption in the pressure area. In the process of orthodontic treatment, there is also a partial transformation of the soft tissues of the face, as well as innervating nerve fibers and associated structures. Changes in facial structure, oral sensory experience modulate cortical neural networks, at least in the sensorimotor cortex region [8, 9]. Congenital bite abnormalities in children are known to result in significant changes in the spectral density of electroencephalographic signals (EEG) of the brain in theta (4–7 Hz) and alpha (8–12 Hz) bands compared with a conventionally normotypic structure, without anterior open bite [10]. Considering oral changes from the perspective of neuroplasticity, the oral cavity appears to be essentially an information-sensory system corresponding to the oral part of the sensorimotor cortex of the brain, and various oral functions, such as speech, mastication, deglutition, etc., are controlled by different parts of the brain [11, 12]. In this context, the corrective effects of orthodontic treatment may induce corresponding changes in brain structure and function [13,14,15]. Current research on brain activity changes during orthodontic corrections has mainly focused on finding and evaluating neural correlates associated with pain scores after orthodontic correction and its therapy [16,17,18]. Overall, it has been demonstrated that pain therapy leads to some changes in the electrical activity of the patients’ brain. However, it should be noted that the results of the analyses are somewhat contradictory. In particular, EEG analysis showed improved functional connectivity among different brain regions in patients using non-medication pain reduction methods compared to the control group without pain treatment [3, 6]. However, spectral power in theta, alpha and beta (14–30 Hz) bands for the groups with better pain treatment results in various studies showed both an increase [6] and a decrease [3], compared with the results of EEG analyses performed in the groups with more severe pain. We speculate that such different results may be related to the presence in patients of a process of changes in brain activity due to objective factors of pressure of orthodontic correction systems on the oral cavity. To determine these changes in our study, we examine the change in brain activity before and after the start of orthodontic correction in patients without significant pain syndromes. Thus, getting rid of subjective factors of pain and stress, we can focus on the changes caused directly by the transformation of the configuration of the dentoalveolar system.
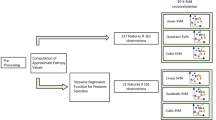
For the numerical processing of biomedical signals recorded in the cerebral cortex, we used the method for estimating oscillatory patterns based on the simultaneous assessment of energies, frequencies, and diagnostic time of continuous wavelet transform (CWT) skeletons. The method was described in our previous publication [19]. The use of this method makes it possible to distinguish the dynamics of various oscillatory components in a complex signal, as was shown for model systems [19] and tested for processing actual signals of living systems [20,21,22]. Our study, intended for the special issue, applied the above-mentioned method for identifying the effect of acute stress on the brain activity in patients during routine cognitive load. Surface recordings of the brain electrical activity in patients before and immediately after the orthodontic correction of their occlusion and/or dentition were used as experimental material.
In performed clinical studies, the dental anomalies observed in patients were local and were associated with a slight disorder of the occlusion. Patients did not complain of pain during the installation of braces or aligners. However, the beginning of the use of dentition correction systems imposes a substantial stress due to obvious awkwardness occurring in the facial area. Besides, the use of bracket systems inevitably entails some changes in the eating behavior of patients and in their sensations [23]. At the same time, the study participants hardly experienced significant changes in the blood supply and lymph flow of the brain andor activity of their facial muscles, at least at the starting time of using orthodontic systems for correcting the dentition.
Thus, this paper is devoted to the mathematical analysis of changes in brain activity under the influence of orthodontic correction. The Materials and methods section first describes the clinical studies in which EEG signals were recorded. Volunteers participated in the studies were divided into three groups according to the strength of the effects on the dentoalveolar system. Second, this section includes a description of the methods of digital processing of EEG signals. The processing based on oscillatory CWT patterns made it possible to thoroughly trace the dynamic characteristics of various EEG components. A description of the identified features of EEG signals in patients groups with different types of orthodontic correction is given in the Results section. The evaluation of brain activity differences before and after the start of orthodontic correction allowed independent clustering of the set of characteristics of EEG oscillatory patterns. The clusters detected by EEG characteristics coincide with the clinical groups of patients. Thus, the first results show that different levels of exposure to the dental system change brain activity in significantly different ways.
2 Materials and methods
The first part of this section provides the necessary information about clinical studies in which procedures for recording electrical activity of the brain were carried out. Our research was carried out in accordance with the requirements of Declaration of Helsinki [24] and was approved by the Ethics Committee at State Medical University of Saratov, Ministry of Healthcare of the Russian Federation. All participants provided written informed consent prior to their participation in the study. All research results, along with personal data regarding each volunteer, were used exclusively for the purposes of research implementation, without their transfer to third parties.
In the second part, all methods used for EEG processing are described. The use of these methods is aimed at searching for and quantifying differences in the oscillatory structure of the electrical activity of the brain before and after the start of orthodontic correction.
2.1 Clinical materials
2.1.1 Study subjects
We recruited volunteers without neurological disorders and signs of cognitive decline. The exclusion criteria were as follows: age under 18 and over 25 years, the value on the Hospital Anxiety and Depression Scale (HADS) \(\ge 10\), body mass index (BMI) value \(\ge 25\), chronic pain (head, back, pelvic area, etc) for over 6 months, history of serious neurological disorders (epilepsy, presence of acute cerebrovascular accident, etc.), psychiatric disorders (schizophrenia, dementia, severe cognitive impairment). The HADS was developed for the initial identification of depression and anxiety in general medical practice [25, 26]. This questionnaire was consisted of 7 questions with answer options ranging from 0 to 3 points; the sum 10 of the scores for all answers allowed a rough assessment of the presence of clinically and/or subclinically significant anxiety and depression in patients. BMI was estimated as the ratio of the patient’s body weight to the square of his or her height, i.e., \([\text {BMI}]=\text {kg/m}^2\), BMI value \(>25\) corresponds to overweight for adult patients according to the World Health Organization classification.
The inclusion criterion for the study group was the presence of dentoalveolar anomalies. When diagnosing the latter, such pathologies as distal occlusion (class 2 malocclusion in concordance with the classification of E. Angle [27, 28], here and below) and abnormal position of individual teeth (class 1 malocclusion) were identified. Patients were diagnosed using a standardized protocol that included the following: (a) patient complaints; (b) clinical examination of organs and tissues of the maxillofacial region; (c) instrumental examination of the dentition to exclude concomitant dental pathology; (d) determination of morphometric parameters of analog models of the jaws, as well as the analysis of virtual computer models of the jaws (control and diagnostic) to determine the parameters of the dentition. The photographs in Fig. 1a, b demonstrate examples of dentoalveolar disorders diagnosed as class 1 and class 2 malocclusion, respectively.
The morphometric characteristics were refined by comparing 3D models of dentition during scanning and creating virtual computer models on the iTero 2 scanner. We identified the type of dentoalveolar system anomaly in each patient and the lack of space in the dentition for teeth, the location of which was supposed to change during the treatment, to determine the degree of complexity of orthodontic correction (tooth movement). Group 1 patients were treated with G &H self-ligating bracket systems with 0.022 bracket slot and NiTi 0.014 archwires. When using bracket systems, pressure was applied to all teeth of both dentitions. The process of a typical treatment based on bracket systems is demonstrated in Fig. 1c.
The remaining patients received treatment based on materials and aligners manufactured by Align Technology [23, 29, 30]. The Fig. 1d demonstrates an example of aligners treatment. When exposed to aligners, pressure was applied locally, and the subjects were divided into two separate groups, namely Group 2 and Group 3, depending on the number of teeth that were affected. In these groups, only one jaw was subjected to orthodontic correction, and pressure was applied to 3–5 (Group 2) or 1–2 teeth (Group 3). Thus, the pressure on the patient’s dental system decreases from Group 1 to Group 3.
Figure 2a demonstrates two independent repeated neurophysiological monitoring sessions with each patient: prior to the orthodontic intervention (on the same day—experiment No. 1) and next day after it (experiment No. 2). This article presents the results of 16 neurophysiological monitoring sessions recorded in 8 patients with orthodontic correction.
2.1.2 Experimental design
As part of each experiment, the subjects underwent EEG monitoring. The multichannel surface EEG data were collected using the Encephalan-EEGR-19/26 recorder (Medicom MTD Ltd., Russia). Data were recorded at 250 Hz sampling rate using the conventional monopolar method of registration with two reference points and \(N=5\) electrodes, located according to the 10–20 scheme [31]. The adhesive Ag/AgCl electrodes in prewired head caps were used to detect EEG signals. Two reference electrodes, A1 and A2, were located on mastoids, while the ground electrode N was placed above the forehead. The EEG signals were filtered by a band-pass filter with cutoff points at 0.5 Hz (High Pass Filter) and 55.5 Hz (Low Pass Filter), and a 50 Hz notch filter. The position of the electrodes is shown in Fig. 2b, and examples of the signal in designated EEG channels are presented in Fig. 2c.
EEG was recorded during passive wakefulness, as shown in Fig. 2d. The volunteer was in a comfortable reclining position, could listen to arbitrary music of hisher choice andor view video clips on a fixed tablet.Patients were offered a choice of several long (about 60 min) recordings of classical and lounge music, as well as calm nature video with similar light music. During the first session, each patient made a choice of music or video, and during the second visit, EEG were recorded in the identical design as the first recording. Thus, the design of the first and second EEG recordings was completely repeated for each of the volunteers. All participants EEG were registered in the same way during the daytime, from 1 to 5 pm. The average duration of EEG registration was \(60\pm 3.35\) min.
2.2 EEG data processing
Numerical processing of EEG signals was carried out over the entire duration of the experimental recordings, without considering different stages of the experiment, in the range of \([t_\textrm{s}, t_\textrm{e}]\) s, as shown in Fig. 2d.
2.2.1 Assessment of the EEG oscillatory patterns
The initial stage of processing EEG signals was represented by improving the quality of records via reducing the confounding impact of oculomotor and muscular activities. Such improvement was based on standard methods [32, 33]. The signals of brain activity selected for analysis, recorded in the occipital region of the scalp, are naturally remote from the activity zones of the masticatory apparatus and the temporal joint, which makes it possible to assert that there was virtually no confounding effect of changes in the activity of the masticatory system. Then, for the EEG of each channel, the number and duration of oscillatory patterns were calculated on the CWT basis.
The procedure for estimating oscillatory patterns was proposed and described in Runnova, et al. [19]. First, CWT, \(\text {CWT}_\textrm{EEG}(f,t)\), was calculated for each EEG channel, \(x_\textrm{EEG}(t)\). Second, on each surface \(\text {CWT}_\textrm{EEG}(f,t)\), certain number, N, local maxima of CWT-amplitudes, \(\max [\text {CWT}_\textrm{EEG}^{1,2\ldots N}\left( f_{\max },t_{\max }\right) ]\) was detected. Third, for each EEG signal, \(x_\textrm{EEG}(t)\), we generated a corresponding array of coordinates \((f_{\max },t_{\max })^{1}, \ldots , (f_{\max },t_{\max })^{j}, \ldots , (f_{\max },t_{\max })^{N}\), for which CWT energy \(\text {CWT}_\textrm{EEG}\) exhibited local extrema. Next, the array of points \(\left( f_{\max },t_{\max }\right) ^{1 \ldots N}\) was sorted by time coordinate t: from start time, \(t_\textrm{s}\) to fin time, \(t_\textrm{e}\). Note that an arbitrary moment of time, \(t_0\), in the considered array of points \(\left( f_{\max }, t_{\max }\right) ^{1 \ldots N}\) could contain several corresponding coordinates \(\left( f_{\max }, t_{\max } = t_0\right) ^{j_1}\), \(\left( f_{\max },t_{\max } = t_0\right) ^{j_2}\), or none \(\left( f_{\max },t_{\max } \ne t_0\right) ^{\forall j}\). For any two points \(\left( f_{\max },t_{\max }\right) ^{j_1}\) and \(\left( f_{\max },t_{\max }\right) ^{j_2}\), we estimated the distance between them \(\delta ^{j_{1, 2}}\left( f_{\max },t_{\max }\right) =\left\| \left( f_{\max },t_{\max }\right) ^{j_1} - \left( f_{\max },t_{\max }\right) ^{j_2}\right\|\). If this distance was enough small, \(\delta ^{j_{1,2}}\left( f_{\max },t_{\max }\right) \le 4\cdot 10^{-6}\), the two points were considered to belong to the same oscillatory pattern P. This procedure was repeated for all points in the array, allowing the formation of sets of coordinates belonging to different patterns.
Thus, the all coordinates of each oscillatory pattern P were detected, consisting of sets \(\left[ f_{\max }, t_{\max }\right]\) forming continuous lines of the maxima of the CWT-surface (f, t). Time duration \(T_{P}\) and mean frequency \(F_P\) were estimated for each pattern P. We denote the coordinates of the beginning of pattern P registration as \(\left( f_{0}^P;t_0^P\right)\), and the coordinates of the end of its registration as \(\left( f_R^P;t_R^P\right)\), where R is the number of points belonging to this pattern P. Then, the registration time and average frequency of each pattern P were estimated as
All oscillatory activity was considered in the range [1; 50] Hz divided into 25 frequency bands: \(\Delta f_1 [1, 2]\), and 24 equal bands with a width of 2 Hz: \(\Delta f_2 \left[ 2, 4\right]\), \(\dots\), \(\Delta f_i\), \(\dots\), \(\Delta f_{25} [48, 50]\) Hz. For each frequency band \(\Delta f_i\) in a floating time interval of 30 s, we estimated the number of patterns \(N_P\) with a mean frequencies \(F_P\) belonging to the given \(\Delta f_i\) band, \(F_P \in \Delta f_i\). Also, for oscillatory patterns belonging to \(\Delta f_i\) band, average time duration of oscillatory patterns \(T_P\) was calculated in every 30-s time interval. As a result, for each EEG, two numerical characteristics \((N_P, T_P)\) of oscillatory patterns P of 25 \(\Delta f_i\) frequency bands were estimated for each time interval with duration of 30 s. Thus, the numerical processing of each EEG signal made it possible to obtain an array with a volume
The choice of averaging window was due to modern standards of EEG automatic processing during work with long-term monitoring, such as polysomnography. The time scale of about 30 s allows simultaneous assessment of brain activity rhythms, muscle movement artifacts, oculomotor oscillations, etc. The use of this time interval could provide a basis for further comparison of the results of pattern-based assessment in oscillatory brain activity with classical approaches of neurophysiology.
2.2.2 Assessing the difference of oscillatory patterns between experiments
Let us introduce the coefficients that characterize the differences in the brain electrical activity of the subjects before and after orthodontic treatment, modeling the stress effect of a significant force, in each \(\Delta f_i\) band:
where \(\left( N_P\right) _r, \left( T_P\right) _r\left\| _{EEG\#1,\Delta f_i}\right.\) and \(\left( N_P\right) _r, \left( T_P\right) _r\left\| _{EEG\#2,\Delta f_i}\right.\) are number and duration of oscillatory patterns P, calculated by time intervals \(\Delta t=30\) s in a frequency band \(\Delta f_i\) for the EEG, recorded in the first and second experiment, respectively; R, K and r, k are the total number of time intervals \(\Delta t\) and their serial numbers for the first and second experiments, correspondingly.
Coefficients \(\Theta _{N, \Delta f_i}\) (3) and \(\Theta _{T, \Delta f_i}\) (4) are estimates of the difference in the average values of the number \(N_P\) and the duration \(T_P\) of oscillatory patterns calculated in each frequency band \(\Delta f_i\) for the entire duration of experiments 1 and 2. These parameters describe the differences in electrical activity for a certain recording channel in different bands from experiment to experiment.
2.2.3 Cluster analysis
To group subjects based on electrical activity in their brain, we applied the cluster analysis based on the hierarchical clustering method [34]. This method allowed grouping the data into a tree of clusters [35]. Such hierarchical clustering is widely used by many researchers [36] because it allows higher quality clustering than other methods (e.g., k-means). To characterize electrical activity in subject’s brain, we performed the hierarchical clustering using difference variables \(\Theta _{N, \Delta f_i}\) and \(\Theta _{T, \Delta f_i}\) calculated according to Eqs. (3) and (4) for the number of patterns and transition of patterns. We used SPSS software to perform the clustering. To measure the distance between the clusters, used the Euclidean squared distance method (default) and the farthest neighbor clustering procedure.
2.2.4 Statistical data processing
Mean, median, and standard deviation were used in descriptive statistics of collected data. The Mann–Whitney U test for independent samples was performed for the comparison of quantitative data. Calculation and graphing of distributions of \(\textrm{Tr}\) coefficients made in OriginLab version 6.1. The results with a p-value \(\le 0.05\) were assumed statistically significant. Statistical analyses were conducted by SPSS version 22.0 software for Windows (IBM, Armonk, NY, USA).
3 Results and discussion
This section demonstrates the results of assessing objective quantitative characteristics of the EEG based on oscillatory patterns assessed in narrow bands. Further studies by the scientific group in this pioneering direction propose prolongation of clinical EEG recordings during the entire period of orthodontic correction and similar numerical processing to detect changes in brain activity throughout the entire cycle of changes in the patient’s dental system.
The first part of this section is devoted to a description of the N and T characteristics of oscillatory patterns calculated from EEG recorded in various groups of patients. In the second part, we demonstrate the identified differences in EEG patterns between the first and second experiments, i. e., before and after orthodontic correction. The third part describes the results of independent clustering of groups of patients according to the identified characteristics of differences between patterns in the frequency bands \(\Delta f_9 \left[ 16;18\right]\), \(\Delta f_{11} \left[ 20;22\right]\), \(\Delta f_{12} \left[ 22;24\right]\), \(\Delta f_{13} \left[ 24;26\right]\), \(\Delta f_{14} \left[ 26;28\right]\), \(\Delta f_{17} \left[ 32;34\right]\), \(\Delta f_{22} \left[ 42;44\right]\), \(\Delta f_{23} \left[ 44;46\right]\), \(\Delta f_{24} \left[ 46;48\right]\) and \(\Delta f_{25} \left[ 48;50\right]\) Hz. The final part is devoted to a short discussion of the results obtained.
3.1 EEG features
Figures 3 and 4 present a comparison of the number and duration of oscillatory patterns for four frequency bands: \(\Delta f_1 \left[ 1; 2\right]\), \(\Delta f_4 \left[ 6; 8\right]\), \(\Delta f_6 \left[ 10; 12\right]\) and \(\Delta f_11 \left[ 20; 22\right]\) Hz. The comparison is based on the results of calculations made from the recordings of four EEG channels in two typical participants of a clinical study: Sub.# 2 represents Group 1, while Sub. # 8 belongs to Group 3. Group 3 and Group 1 are characterized by the orthodontic exposure of a minimum and maximum intensity, respectively, occurring before experiment 2.
a–d Values of \(N_p\) (number of oscillatory patterns) and \(T_p\) (time duration of oscillatory pattern P) estimated in frequency bands \(\Delta f_1\) and \(\Delta f_4\), respectively. The diagrams of the characteristics calculated for the first and second experiments are shown in red and blue, correspondingly. The white background corresponds to participant Sub.# 2 representing Group 1, in which patients received orthodontic treatment based on braces. On the gray background, the EEG results are shown for participant Sub. # 8 representing Group 3, in which patients experienced the lowest exposure to aligners
Numerical estimates of the typical dynamics allow observing that the slow oscillation pattern in a low-frequency band remain virtually unchanged under the impact of orthodontic correction, as seen in Fig. 3. As seen in Fig. 3a, b, in the EEG recorded in the O1 channel in Group 1 patients (e.g., Sub. # 2,), the characteristics of patterns P in \(\Delta f_1\) band demonstrate the effect of switching in the number \(N_P\) and the duration \(T_P\). When moving from the first to the second experimental recording, the number of patterns (\(N_P\)) increases while their duration (\(T_P\)) decreases.
High-frequency activity changes to a greater extent, as shown in Fig. 4. The number of oscillatory patterns \(N_P\) measured in O1-channel in patients with brackets changes significantly from experiment 1 to experiment 2, which in blue and red for Sub. # 2 in Fig. 4c. At the same time, \(N_p\) in high-frequency bands for patients with aligners remains unchanged—e.g., in Sub. # 8, as seen in Fig. 4c. Also, the time duration \(T_P\) of alpha-patterns in \(\Delta f_6\) band exhibits specific dynamics: the range of such changes in patients of Group 1 significantly exceeds the analogous range in patients of Group 3 (Fig. 4b).
a–d Values of \(N_p\) (number of oscillatory patterns P) and \(T_p\) (time duration of oscillatory pattern P) estimated in frequency bands \(\Delta f_6 \left[ 6; 8\right]\) and \(\Delta f_{11} \left[ 20; 22\right]\) Hz, respectively. The diagrams of the characteristics calculated for the first and second experiments are shown in red and blue, correspondingly. The white background corresponds to participant Sub. # 2 representing Group 1, in which patients received orthodontic treatment based on braces. On the gray background, the EEG results are shown for participant Sub. # 8 representing Group 3, in which patients experienced the lowest exposure to aligners. Asterisks indicate significant differences between experiments according to the Mann–Whitney U test (p-value \(\le 0.05\))
3.2 EEG changes between experiments
Figure 5 presents the dependences of the coefficients \(\Theta _{N, \Delta f_i}\) and \(\Theta _{T, \Delta f_i}\) for several frequency bands in all subjects. Fast oscillations in beta-1 and gamma frequency bands, \(\Delta f_9 \left[ 16; 18 \right]\) and \(\Delta f_{22} \left[ 42; 44 \right]\) Hz, estimated for \(EEG_{O1}\), have characteristic features of changes in the \(N_P\) for each group of study subjects. In Group 1, the coefficient \(\Theta _{N, \Delta f_{\left( 9;22\right) }}\) has large negative values. In Group 2, \(\Theta _{N, \Delta f_{\left( 9;22\right) }}\) approaches zero. In Group 3, the values of the coefficient \(\Theta _{N, \Delta f_{\left( 9;22\right) }}\) are positive, as this is especially obvious in the graphs in the left panel of Fig. 5c, e. Oscillatory patterns, determined for low-frequency or slow activity, do not allow observing such regularities.
Estimating coefficients \(\Theta _{N, \Delta f_i}\) (3) and \(\Theta _{T, \Delta f_i}\) (4) for participants in clinical trials in frequency bands \(\Delta f_2 \left[ 2;4\right]\) Hz (a), \(\Delta f_5 \left[ 8;10\right]\) Hz (b), \(\Delta f_9 \left[ 16;18\right]\) Hz (c), \(\Delta f_{11} \left[ 20;22\right]\) Hz (d) and \(\Delta f_{22} \left[ 42;44\right]\) Hz (e). Different groups of patients are highlighted with different background colors
Preliminary estimates made it possible to isolate the occipital EEG recording channel corresponding to the O1 lead. An analysis of the activity in this channel allowed observing the most pronounced changes in the dynamics of oscillatory patterns in the high-frequency region. Further, for an independent assessment of changes in brain activity during orthodontic correction, we performed hierarchical clustering according to the values of the coefficient \(\Theta _{N, \Delta f_i}\) (3), estimated for the O1 channel in the following high-frequency bands: \(\bigcup _\textrm{HF}\) Hz:
The specified frequency ranges according to classical approaches of modern interdisciplinary brain electrophysiology are usually described as beta1, \(\beta _1, \left( 13; 21\right)\) Hz, and beta2, \(\beta _2,\left( 21; 30\right)\) Hz, and gamma, \(\gamma \left( 30; 50\right)\) Hz, rhythms of electrical activity. The activation of \(\beta\)-rhythms or \(\beta\)-synchronization in occipital cortical areas is observed in tasks involving the visual modality [37]. In the occipital area, beta synchronization occurs in response to neglected, so-called NOGO-stimuli, that is, stimuli that are accompanied by a “relaxation” of the subject, but not to stimuli (such as GO-stimuli) that require further processing or response. In the \(\gamma\)-range, a particular oscillatory activity is recorded that is independent of the traditional \(\beta\)-rhythm [38]. This activity, so-called “40 Hz rhythms”, may be directly related to cognitive operations, sensorimotor integration, recognition of tactile stimuli, and purposeful movements [39]. Assessments of the topical distribution and severity of \(\gamma\)-rhythms can serve to diagnose disorders of the normal organization of the corresponding higher mental functions [40].
3.3 Clustering according to changes in EEG patterns after orthodontic treatment
The dendrogram in Fig. 6 displays the results of clustering. The clustering procedure by assessing changes in oscillatory processes of \(\bigcup _\textrm{HF}\) bands occurring in a single occipital O1-canal made it possible to divide the data array into three clusters that matched the clinical groups of study participants. The quality of detection of patient clusters was the highest in the patient groups, where treatment was based on the use of braces and Invisalign orthodontic aligners. Classes based on EEG activity estimates for Group 2 and Group 3 patients (aligner groups) differed to a lesser extent, and this division was less reliable.
It should be noted that during numerical processing and further clustering, an extremely limited set of EEG signals of O1, O2, P3, P4 and Pz was used. The particular importance of the occipital region activity, associated with visual analyzers, as well as object recognition processes, mental imaginary motor activity and others, is well known [41,42,43]. In particular, as was shown in [44], the quality of stimuli detection observed by a test subject increases significantly when using exclusively occipital EEG channels. Besides, the occipital channels are preferred in practical use due to both the convenience of applying electrodes and the natural spatial remoteness from the powerful interference associated with the movements of eyes, facial muscles, mouth, etc.
It should be noted that we used continuous recording of neurophysiological activity over a fairly large set of samples without dividing into active and relaxation stages and additional evaluation of the special psychological tests. During a long recording \(\left[ t_s; t_e\right]\), the participants of the study could freely think or be in a state of conditionally “doing nothing”. An analysis of such complex voluntary cognitive activity with further averaging over a small time window makes it possible to identify the characteristic individual features of the dynamics of the occipital region of the brain.
The possibility of such average estimates of the oscillatory activity on the basis of brain EEG was facilitated, first of all, by the use of the CWT for pattern recognition procedure, which is highly sensitive to the variability of various components present in the time-frequency domain of complex signals. In particular, when detecting the CWT energy by conventional methods, it is be possible to track changes in the duration and number of oscillatory components when a stress factor is introduced.
Such approach to the evaluation of experimental records, based on averaging, allows solving the problem of developing clinical methods for EEG analysis without time marking of certain eventsactions that occur in a patient during neurophysiological monitoring. The need to create clear conditions for making records seems a serious limitation for introducing the experimental methods of neuroscience in clinical practice. Hence, in the future, development and accumulation of the experimental database will allow creating systems for monitoring the stressful impact at the very beginning of orthodontic corrections, i.e., to objectively identify patients with amplified sensitivity. For such patients, it is possible to change the process of orthodontic correction (e.g., to ensure a temporary reduction in the force of exposure). In addition, it is of interest to further evaluate the success of orthodontic correction in comparison with neurophysiological and neuropsychological assessments made in the course of a patient testing.
3.4 Discussion
In modern medicine, research and clinical work directly related to the oral cavity, namely the rehabilitation of occlusion, the restoration of esthetics, the functional assessment after rehabilitation and the development of orthodontic treatment approaches, belong exclusively to dentistry and are often of a narrow, purely applied nature. Such studies in scientific terms are somewhat behind modern medical approaches aimed at a comprehensive study of systemic interactions within the body. However, the applied possibilities of modern dentistry in restoring human health are currently reaching unprecedented heights and allow optimizing the occlusion of the dentition, normalizing the functions of the maxillofacial region, even in the most difficult cases.
Today, there is convincing practical evidence that dental treatment helps to reduce the risk of cardiovascular disease, the occurrence of dementia, and occlusal rehabilitation correlates with an increase in the duration and life quality [45,46,47]. In addition, human cognitive functions such as memory, gnosis, and praxis have been shown to decrease with loss of normal occlusion associated with tooth extraction andor masticatory dysfunction [48, 49]. Thus, the study of the direct effect of orthodontic treatment on the parameters of the electrical activity of the brain enriches the modern fundamental system of ideas about the integral nature of the dynamics of various biophysical systems of the body.
At the same time, the results obtained are also important from an applied point of view, since they allow us to confirm the possibilities of developing diagnostic systems for clinical diagnosis and monitoring of patient treatment. Such a breakthrough system, which allows a specialist to obtain an independent additional assessment of the state of the patient’s body, would be extremely interesting in the tasks of finding out the optimal duration of the total time of rehabilitation measures during orthodontic correction. Today, the duration of treatment can vary greatly: from several years in traditional orthodontics for adult patients to several months using innovative approaches, including surgical interventions (for example, osteotomy, corticotomy, etc.), supplemented by physiotherapeutic methods of influence [50,51,52]. Despite the clear advantage of reducing the time of wearing orthodontic appliances, associated with a decrease in their negative impact on the teeth and periodontal tissues, questions arise about the adaptive capabilities of the maxillofacial apparatus and its surrounding tissues for the rapid restructuring of this system while accelerating the correction [53]. Further studies of changes and variation of various functional signals of the body will be able to expand the range of diagnostic possibilities for specialists in this field in assessing the observation of the adaptation processes of patients. Of particular interest is the question of differentiating the effect of stress from braces or aligners and their direct impact on the patient’s dental system.
3.4.1 Future works
In further studies, the team of authors plans to conduct extended studies of the processes accompanying orthodontic treatment, including assessment of the status of cognitive functions during neuropsychological testing combined with EEG monitoring, supplemented by an electrocardiogram recording. In addition, during orthodontic treatment, monitoring data will be collected several times during the entire cycle. The development of this direction will be aimed at solving the problem of finding and quantifying the relationship between the health of the tissues of the maxillofacial region, the state of neurophysiological parameters under the control of the cognitive status and activity of the cardiac system.
4 Conclusion
The paper presents the first results of the study of changes in the electrophysiological activity of the brain of patients in the acute initial period of orthodontic correction. Eight healthy volunteers with detectable pathologies of distal occlusion (class 2 malocclusion) and abnormal position of individual teeth (class 1 malocclusion) participated in the collection of clinical material. Group 1 included volunteers using braces, groups 2 and 3 included volunteers using aligners in which pressure was applied to 3–5 or 1–2 teeth, respectively. Brain EEG data were collected twice during neurophysiological monitoring: at once before and after orthodontic correction. EEG signals from the occipital region of the brain were collected during quiet wakefulness, i.e., in a state of conditionally “doing nothing”. Numerical processing was performed based on continuous wavelet analysis to estimate the number and duration of oscillatory patterns in narrow frequency bands, dividing the entire band 1–50 Hz. An assessment of the oscillatory brain activity demonstrated that different grades of correction intensity, regarding the dentition and occlusion, lead to uniform changes in the oscillatory patterns assessed by the electroencephalography in the occipital lobe. Comparison of the number of oscillatory patterns in the groups showed significant changes in the high-frequency \(\bigcup _\textrm{HF}\) Hz. The number of patterns in the \(\bigcup _\textrm{HF}\)-band (5) increases when using the most intense bracket devices, while in cases of more gentle correction based on aligner systems, it remains unchanged or even decreases. The independent clustering procedure by assessing changes in oscillatory processes of \(\bigcup _\textrm{HF}\)-band (5) occurring in a single occipital O1-canal made it possible to divide the data array into three clusters. The clusters of changes in brain activity correspond to clinical groups of patients. Thus, different types of dental exposure lead to significantly different changes in the brain activity of patients. Our results are of certain interest for studying changes in stable oscillatory patterns of brain activity under the impact of orthodontic treatment procedures.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
H. Long, Y. Wang, F. Jian, L.-N. Liao, X. Yang, W.-L. Lai, Current advances in orthodontic pain. Int. J. Oral Sci. 8(2), 67–75 (2016)
C. Feng, C. Wu, Z. Jiang, L. Zhang, X. Zhang, Effectiveness of different psychological interventions in reducing fixed orthodontic pain: a systematic review and meta-analysis. Austral. Orthod. J. 35(2), 195–209 (2019)
J. Wang, D. Wu, Y. Shen, Y. Zhang, Y. Xu, X. Tang, R. Wang, Cognitive behavioral therapy eases orthodontic pain: EEG states and functional connectivity analysis. Oral Dis. 21(5), 572–582 (2015)
D. Wu, Hearing the sound in the brain: influences of different EEG references. Front. Neurosci. 12, 148 (2018)
A.E. Aly, I. Hansa, D.J. Ferguson, N.R. Vaid, The effect of alpha binaural beat music on orthodontic pain after initial archwire placement: a randomized controlled trial. Dental Press J. Orthod. 27, e2221150 (2023)
R. Huang, J. Wang, D. Wu, H. Long, X. Yang, H. Liu, X. Gao, R. Zhao, W. Lai, The effects of customised brainwave music on orofacial pain induced by orthodontic tooth movement. Oral Dis. 22(8), 766–774 (2016)
V. Legrain, D.M. Torta, Cognitive psychology and neuropsychology of nociception and pain, in Pain, Emotion and Cognition: A Complex Nexus (Springer, 2015), pp. 3–20
W. Liu, C. Cui, Z. Hu, J. Li, J. Wang, Changes of neuroplasticity in cortical motor control of human masseter muscle related to orthodontic treatment. J. Oral Rehabil. 49(2), 258–264 (2022)
M.Z. Pimenidis, Orthodontic avenues to neuroplasticity, in The Neurobiology of Orthodontics: Treatment of Malocclusion Through Neuroplasticity (2009), pp. 131–136
C. Restrepo, P. Botero, D. Valderrama, K. Jimenez, R. Manrique, Brain cortex activity in children with anterior open bite: A pilot study. Front. Hum. Neurosci. 14, 220 (2020)
I.B. Black, The Changing Brain: Alzheimer’s Disease and Advances in Neuroscience (Oxford University Press, USA, 2002)
I. Cioffi, Biological and psychological factors affecting the sensory and jaw motor responses to orthodontic tooth movement. Orthod. Craniofac. Res. 00, 1–9 (2023)
M. Novikov, M. Zhuravlev, A. Maksimova, R. Nasrullaev, D. Suetenkov, Effect of orthodontic correction characteristics in brain electrical activity. in Computational Biophysics and Nanobiophotonics, SPIE, vol. 12194 (2022), pp. 279–284
C.-S. Lin, Dental Neuroimaging: The Role of the Brain in Oral Functions (John Wiley & Sons, New York, 2021)
Y. Ariji, H. Kondo, K. Miyazawa, S. Sakuma, M. Tabuchi, Y. Kise, M. Nakayama, S. Koyama, A. Togari, S. Goto et al., Study on regional activities in the human brain caused by low-level clenching and tooth separation: investigation with functional magnetic resonance imaging. Oral Sci. Int. 16(2), 87–94 (2019)
F. Zhang, F. Li, H. Yang, Y. Jin, W. Lai, G.J. Kemp, Z. Jia, Q. Gong, Altered brain topological property associated with anxiety in experimental orthodontic pain. Front. Neurosci. 16, 907216 (2022)
H. Yang, X. Yang, H. Liu, H. Long, H. Hu, Q. Wang, R. Huang, D. Shan, K. Li, W. Lai, Placebo modulation in orthodontic pain: a single-blind functional magnetic resonance study. Radiol. Med. (Torino) 126(10), 1356–1365 (2021)
F. Zhang, F. Li, H. Yang, Y. Jin, W. Lai, N. Roberts, Z. Jia, Q. Gong, Effect of experimental orthodontic pain on gray and white matter functional connectivity. CNS Neurosci. Therapeut. 27(4), 439–448 (2021)
A. Runnova, M. Zhuravlev, R. Ukolov, I. Blokhina, A. Dubrovski, N. Lezhnev, E. Sitnikova, E. Saranceva, A. Kiselev, A. Karavaev et al., Modified wavelet analysis of ECoG-pattern as promising tool for detection of the blood–brain barrier leakage. Sci. Rep. 11(1), 1–8 (2021)
M. Simonyan, A. Fisun, G. Afanaseva, O. Glushkovskaya-Semyachkina, I. Blokhina, A. Selskii, M. Zhuravlev, A. Runnova, Oscillatory wavelet-patterns in complex data: mutual estimation of frequencies and energy dynamics. Eur. Phys. J. Spec. Top. 232(5), 595–603 (2023)
M.O. Zhuravlev, A.O. Kiselev, A.E. Runnova, Study of the characteristics of eeg frequency patterns: the automatic marking of sleep stage without additional physiological signals, in 2022 International Conference on Quality Management, Transport and Information Security, Information Technologies (IT &QM &IS) (IEEE, 2022), pp. 352–355
K. Sergeev, A. Runnova, M. Zhuravlev, O. Kolokolov, N. Akimova, A. Kiselev, A. Titova, A. Slepnev, N. Semenova, T. Penzel, Wavelet skeletons in sleep EEG-monitoring as biomarkers of early diagnostics of mild cognitive impairment. Chaos Interdiscip. J. Nonlinear Sci. 31(7), 073110 (2021)
G. Djeu, C. Shelton, A. Maganzini, Outcome assessment of invisalign and traditional orthodontic treatment compared with the American board of orthodontics objective grading system. Am. J. Orthod. Dentofac. Orthop. 128(3), 292–298 (2005)
World Medical Association, World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20), 2191–2194 (2013)
C. Brennan, A. Worrall-Davies, D. McMillan, S. Gilbody, A. House, The hospital anxiety and depression scale: a diagnostic meta-analysis of case-finding ability. J. Psychosom. Res. 69(4), 371–378 (2010)
A.S. Zigmond, R.P. Snaith, The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67(6), 361–370 (1983)
D.J. Rinchuse, D.J. Rinchuse, Ambiguities of Angle’s classification. Angle Orthod. 59(4), 295–298 (1989)
M.S. Alhammadi, E. Halboub, M.S. Fayed, A. Labib, C. El-Saaidi, Global distribution of malocclusion traits: a systematic review. Dental Press J. Orthod. 23, 40–1 (2018)
T. Weir, Clear aligners in orthodontic treatment. Aust. Dent. J. 62, 58–62 (2017)
M.O. Lagravere, C. Flores-Mir, The treatment effects of invisalign orthodontic aligners: a systematic review. J. Am. Dent. Assoc. 136(12), 1724–1729 (2005)
A. Morley, L. Hill, A. Kaditis, 10–20 System EEG Placement (European Respiratory Society, European Respiratory Society, 2016)
A. Runnova, M. Zhuravlev, A. Koronovskiy, A. Hramov, Mathematical approach to recover eeg brain signals with artifacts by means of Gram-Schmidt transform. In: Saratov Fall Meeting 2016: Laser Physics and Photonics XVII; and Computational Biophysics and Analysis of Biomedical Data III, SPIE, vol. 10337 (2017), pp. 254–259
C.S. Kim, J. Sun, D. Liu, Q. Wang, S.G. Paek, Removal of ocular artifacts using ICA and adaptive filter for motor imagery-based BCI. IEEE/CAA J. Automat. Sin. 1–8 (2017)
M.P. Milali, M.T. Sikulu-Lord, S.S. Kiware, F.E. Dowell, R.J. Povinelli, G.F. Corliss, Do NIR spectra collected from laboratory-reared mosquitoes differ from those collected from wild mosquitoes? PLoS One 13(5), 0198245 (2018)
S.C. Johnson, Hierarchical clustering schemes. Psychometrika 32(3), 241–254 (1967)
G. Karypis, V. Kumar, M. Steinbach, A comparison of document clustering techniques, in KDD Workshop on Text Mining (2000)
O. Jensen, P. Goel, N. Kopell, M. Pohja, R. Hari, B. Ermentrout, On the human sensorimotor-cortex beta rhythm: sources and modeling. Neuroimage 26(2), 347–355 (2005)
J.E. Desmedt, C. Tomberg, Transient phase-locking of 40 Hz electrical oscillations in prefrontal and parietal human cortex reflects the process of conscious somatic perception. Neurosci. Lett. 168(1–2), 126–129 (1994)
D.W. Loring, D.E. Sheer, J.W. Largen, Forty hertz eeg activity in dementia of the Alzheimer type and multi-infarct dementia. Psychophysiology 22(1), 116–121 (1985)
G. Pfurtscheller, C. Neuper, Simultaneous EEG 10 Hz desynchronization and 40 Hz synchronization during finger movements. Neuroreport 3(12), 1057–1060 (1992)
W.-L. Zheng, J.-Y. Zhu, B.-L. Lu, Identifying stable patterns over time for emotion recognition from EEG. IEEE Trans. Affect. Comput. 10(3), 417–429 (2017)
C. Babiloni, F. Vecchio, M. Miriello, G.L. Romani, P.M. Rossini, Visuo-spatial consciousness and parieto-occipital areas: a high-resolution EEG study. Cereb. Cortex 16(1), 37–46 (2006)
J. Williams, Frequency-specific effects of flicker on recognition memory. Neuroscience 104(2), 283–286 (2001)
A.E. Hramov, V.A. Maksimenko, S.V. Pchelintseva, A.E. Runnova, V.V. Grubov, V.Y. Musatov, M.O. Zhuravlev, A.A. Koronovskii, A.N. Pisarchik, Classifying the perceptual interpretations of a bistable image using EEG and artificial neural networks. Front. Neurosci. 11, 674 (2017)
F. Chiappelli, J. Bauer, S. Spackman, P. Prolo, M. Edgerton, C. Armenian, J. Dickmeyer, S. Harper, Dental needs of the elderly in the 21st century. Gen. Dent. 50(4), 358–363 (2002)
M.W.U. Khan, M. Azeem, Frequency of medical co-morbidities in oral surgery, prosthodontic and orthodontic patients. JPDA 29(1), 38–41 (2020)
N.C.F. Fagundes, R.S.D. Couto, A.P.T. Brandao, L.A. de Oliveira Lima, L. de Oliveira Bittencourt, R.D. de Souza-Rodrigues, M.A.M. Freire, L.C. Maia, R.R. Lima, Association between tooth loss and stroke: a systematic review. J. Stroke Cerebrovasc. Dis. 29(8), 104873 (2020)
M. Gutiérrez, S. Valenzuela, R. Miralles, C. Portus, H. Santander, A. Fuentes, I. Celhay, Does breathing type influence electromyographic activity of obligatory and accessory respiratory muscles? J. Oral Rehabil. 41(11), 801–808 (2014)
Y. Ono, T. Yamamoto, K.-Y. Kubo, M. Onozuka, Occlusion and brain function: mastication as a prevention of cognitive dysfunction. J. Oral Rehabil. 37(8), 624–640 (2010)
N.A. Parkin, S. Almutairi, P.E. Benson, Surgical exposure and orthodontic alignment of palatally displaced canines: can we shorten treatment time? J. Orthod. 46(1Suppl), 54–59 (2019)
N. Zimmo, M. Saleh, G. Mandelaris, H.-L. Chan, H.-L. Wang, Corticotomy-accelerated orthodontics: a comprehensive review and update. Compendium 38(1), 1–8 (2017)
G. Doshi-Mehta, W.A. Bhad-Patil, Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am. J. Orthod. Dentofac. Orthop. 141(3), 289–297 (2012)
S. Dab, K. Chen, C. Flores-Mir, Short-and long-term potential effects of accelerated osteogenic orthodontic treatment: a systematic review and meta-analysis. Orthod. Craniofac. Res. 22(2), 61–68 (2019)
Acknowledgements
The authors are very grateful to Dr. Sc. Alexander S. Fedonnikov, Vice-Rector for Research at V. I. Razumovsky Saratov State Medical University, for help in organization of the survey and clinical recordings of volunteers.
Funding
Study is carried out within the framework of the state task of the Russian Federation’s Ministry of Health #056-00030-21-01 dated 02052021 “Theoretical and experimental study of the integrative activity of various physiological systems of patient under stress” (the State registration number # 121030900357-3).
Author information
Authors and Affiliations
Contributions
Conceptualization MZ; funding acquisition AR, and AK; data curation DaS, MS, RN, RP, resources RP, DmS; project administration AR and MZ; supervision AR and AK; software MZ, RN; investigation RP, DaS, DmS; methodology MZ, AR; validation MS; visualization RN; writing—review and editing MZ, DaS, RP, AR, MS, RN, AK, and DmS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhuravlev, M., Suetenkova, D., Parsamyan, R. et al. Changes in EEG oscillatory patterns due to acute stress caused by orthodontic correction. Eur. Phys. J. Spec. Top. 233, 505–518 (2024). https://doi.org/10.1140/epjs/s11734-023-01064-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1140/epjs/s11734-023-01064-4