Abstract
Purpose of Review
This review seeks to provide a summary of recent literature to help guide practitioners in the management of acute pain due to traumatic injury in patients with chronic pain as well as with pre-injury opioid use. It also seeks to illuminate areas in need of further investigation.
Recent Findings
There is a paucity of professional guidelines and clinical trials on this topic, despite the disproportionate rates of preexisting opioid use and chronic pain in trauma patients, and the contributions of these issues to inferior outcomes. The management of these patients is complex, requiring knowledge of opioid conversions, medication-assisted treatment (MAT), and non-opioid analgesic options.
Summary
Provider education, standardized assessments and screening tools, evolving multidisciplinary approach, careful management of pre-injury therapy, use of non-opioid adjuvant therapies, early discharge planning, and close follow-up are essential to achieving adequate acute pain control in these patients, which can contribute to better short- and long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Guidelines from both professional and governmental organizations for the treatment of chronic pain exist, but guidance for the treatment of acute pain due to trauma in patients with chronic pain as well as those with pre-injury opioid use—whether prescribed or secondary to opioid use disorder (OUD)—are limited, despite the fact that trauma patients have disproportionately high rates of preexisting substance use and chronic pain when compared to the general population [1, 2]. Up to 16–20% of trauma patients are using opioids at the time of injury, and approximately 40% of these patients also have issues with chronic pain [2,3,4]. Not only does pre-injury opioid use and chronic pain complicate the treatment of acute pain from a pharmacologic standpoint, but pre-injury opioid use is also associated with negative clinical outcomes, including increased number of days in the intensive care unit (ICU), increased hospital length of stay, and need for mechanical ventilation [1, 4]. Pre-injury opioid dependency was also found to be associated with a higher number of readmissions and of discharge to facilities [3]. Negative clinical outcomes have also separately been associated with inadequate control of acute pain, from increased cost and length of stay, to the development of post-injury chronic pain and psychological conditions [5, 6]. Ineffective acute traumatic pain control following discharge has also been associated with illicit opioid use [7]. Alternatively, aggressive management of acute post-surgical pain has been shown to reduce the risk of subsequent chronic pain [8]. Given the potential consequences of uncontrolled acute pain, effective management of acute pain is imperative for good clinical outcomes after traumatic injury. Unfortunately, the effective treatment of acute pain in patients with pre-injury opioid use and history of chronic pain is complicated by many biologic, pharmacologic, and psychosocial factors.
Chronic pain is characterized by a phenomenon known as central sensitization, defined as physical changes within the nervous system that alter the patient’s ability to perceive stimuli appropriately. These changes can lead to a variety of long-term effects, including “hyperalgesia, which is … a more intense experience of pain; allodynia, which is when previously non-painful stimuli are now painful; and spontaneous pain [9•].” To further complicate matters, both prescription opioid use, commonly employed in the treatment of both acute and chronic pain, and OUD can also each lead to opioid tolerance and opioid-induced hyperalgesia (OIH). OIH can muddle pain management by causing worsening pain perception with increasing opioid doses, limiting the effect that opioid medications can have in the management of acute pain in these patients [5•]. These effects can continue to be seen even after opioid use has stopped, and can lead to mistrust and distress in the patient, which can further contribute to poor pain control. All of this, coupled by the fact that chronic pain and opioid use disorders frequently co-occur, can make the care of these patients quite challenging [9, 10]. Management of acute pain in patients with pre-injury opioid use and chronic pain requires a delicate balance between pain control, side effects, and provider desire to avoid long-term use and misuse of analgesics or the development or exacerbation of chronic pain, making this a very demanding, yet vitally important, area of practice.
Search Techniques
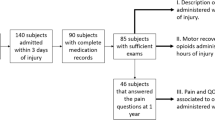
The PubMed MEDLINE database was searched for all abstracts and full-text articles, filtered by type to include clinical trial, meta-analysis, randomized controlled trial, review, and systematic reviews over the last 5 years. MeSH terms used included pain, management, chronic pain, acute on chronic pain, opioid dependence, opioid use, trauma, trauma patient, and traumatic injury. Each abstract was individually reviewed by the author to determine applicability to this narrative review. Articles focusing on pain related to chronic wounds, burn injuries, or athletic injuries were excluded. Articles focusing on acute pain management in the emergency department without a focus on trauma patients, or focusing on prehospital pain management, were also excluded. Articles focusing on management of chronic central pain after spinal cord injury or traumatic brain injury were also excluded, as many of these articles focus on spinal cord/brain stimulation, or other injury-specific treatment modalities, and thus would not be applicable to trauma patients without SCI/TBI.
Guidelines for Management
Provider Education
Given the complex physiological and psychological needs, as well as the varying socioeconomic statuses and resources of this wide variety of patients, the most important intervention to achieve adequate acute pain management following trauma in patients with pre-injury opioid use or chronic pain is provider education. Providers of all levels must be educated, not only in multimodal analgesic techniques and in the nuances of acute and chronic opioid maintenance therapies, but also in a variety of other topics crucial to the comprehensive care of this patient population.
Communication and Psychosocial Risk Factors
Good provider-patient communication, especially when tapering or de-escalating opioid therapy, is extremely important to a successful outcome. Patient anxiety or distress can lead to ineffective pain control, and patient expectations can alter the way pain is perceived [2, 9]. Setting expectations early and revisiting them often can help to increase the amount of control that these vulnerable patients feel and decrease overall anxiety regarding changes to the pain management plan. Although the conversation can be difficult, de-escalation or discontinuation of opioid therapy needs to be discussed with these patients before changes are made.
Psychosocial risk factors, such as preexisting mental health disorders, a lack of healthy coping mechanisms, and substance use, are associated with long-term opioid use and opioid misuse after trauma [11]. History of anxiety, depression, or alcoholism was also associated with chronic pain after trauma [6, 12]. Additionally, patients with chronic pain and those with OUD are both at a higher risk for issues like depression, especially in the setting of acute injury or trauma [13]. Given the complex relationship between OUD, chronic pain, and mental health, ensuring that psychosocial factors are addressed is essential to adequate acute pain control and to maintenance of pain control after discharge. Providers need to be trained to address these issues through validated screening tools and early involvement of medical social workers, chaplains, or psychiatry, when appropriate [14]. Socioeconomic concerns related to the patient’s injuries are also important to address, including clear communication of injuries and expected recovery course. Additionally, providing practitioners with education surrounding brief interventions and relaxation techniques gives them the tools to help mitigate the affect that anxiety related to the traumatic event has on achieving adequate acute pain control and, subsequently, improves patient outcomes [9, 15, 16]. Addressing patient anxiety or psychological distress after traumatic injury is not only important in caring for the patient but can also help to increase trust in the care team and help to achieve pain control goals.
Screening Tools and Pain Assessments
Screening for patients with current OUD as well as for those at high risk for OUD is important, as these can contribute to inferior outcomes if unrecognized. Providers should be educated on risks factors for both OUD and chronic pain, and on screening tools for the identification of high-risk patients, and these tools should be implemented into practice [9•]. There are many validated screening tools available, depending on the institution. One such tool is the Patient Medication Questionnaire (PMQ), which includes 26 questions designed to evaluate for certain drug-related behaviors, and can be helpful in identifying patients with OUD. As noted by Ducharme and Moore, the consistent and standardized implementation of screening tools is more important than the specific tool chosen. Standardized implementation helps improve detection rates by eliminating provider bias in screening [17]. This education about clinical patterns can help practitioners identify high-risk patients and implement appropriate interventions to help address uncontrolled pain or potential OUD. For example, pre-injury opioid use was found to be more common in female patients, and was also found to be associated with falls, especially in elderly patients [4]. Chronic pain after injury was also more likely in female patients and was more commonly associated with falls than any other mechanism of injury [12]. More severe injury, limb amputation, and a history of chronic pain are associated with long-term opioid use after trauma [18]. Nursing tools, like SBIRT (Screening, Brief Intervention and Referral to Treatment), have also been shown to identify at-risk patients and allow for a mechanism by which to connect high-risk patients with treatment and other resources. By identifying at-risk patients early in the hospital stay, providers can better tailor the pain management plan and begin early discharge planning. More research is needed to streamline the implementation of institution-wide, validated screening and referral techniques.
Prescription Drug Monitoring Programs (PDMPs) have been implemented widely across the USA in an attempt to improve inter-provider communication and reduce misuse of opioid prescriptions by providing a report of a patient’s recently filled scheduled prescriptions. Despite wide implementation, most states do not require providers to check reports prior to prescribing opioids and other scheduled substances, and so these programs have not been proven to reduce opioid complications [19, 20]. One study by Rasubala et al. was able to show a significant decrease in opioid prescriptions, as well as an increase in non-opioid analgesic prescriptions, when mandatory PDMP reports were required in a group of dentists [21]. This suggests that PDMP reports, when used consistently, can provide useful information both for identifying high-risk patients or patients with OUD and can aid in the discharge planning process. Practitioners should consider running a PDMP report on any patient receiving an opioid prescription.
Standardized pain assessments have also been shown to improve the treatment of acute pain [5, 16]. This is especially important in the chronic pain and opioid use disorder population, given the well-documented existence of provider bias against these patients [9•]. Provider beliefs about patient exaggerations of pain reports or perceived drug-seeking behavior and a lack of knowledge about tolerance or OIH can lead to undertreatment of acute pain and to patient distress, which can further contribute to inadequate pain management and, as discussed previously, worse outcomes [22•]. The use of standardized screening tools and provider training in pain assessment can help combat these biases and facilitate improvements in the treatment of acute traumatic pain.
Opioid Use and Management of Pre-injury Opioids and Medication-Assisted Treatment
Opioids are first-line treatment for acute traumatic and post-operative pain, and their use often cannot be avoided in patients with a history of pre-injury use (either illicit or prescribed) or in patients on medication-assisted treatment (MAT) for OUD. MAT involves use of an opioid agonist or antagonist to allow for the treatment of OUD without opiate withdrawal. Methadone and buprenorphine, two commonly utilized MAT medications, are safe and effective for the treatment of OUD, and are discussed in further detail below. Both methadone and buprenorphine can also be used in the management of chronic pain, though at different doses and intervals than those utilized during OUD treatment.
Mainstays of opioid use in these patients include assessment of usual daily morphine milligram equivalents (MMEs) with continuation of daily medications or an equivalent regimen, allowance for additional short-acting opioids as needed, and consistent and frequent assessments and reassessments of pain control to allow for the titration of doses. Other important principles include the use of or transition to enteral preparations as early as is clinically feasible and early involvement of the patient’s outpatient opioid or MAT prescribers. Early and ongoing conversations about patient and provider expectations, the care plan, and therapy tapers are also crucial to achieving adequate acute pain control [22•]. Patient expectations can dramatically affect the ability to achieve tolerable pain levels, so they should be discussed on admission and whenever pain goals are not being met [2]. Additionally, practitioners should be aware that these patients will often need higher and more frequent doses of opioid pain medication to achieve pain control than an opioid-naïve patient. Development of tolerance over time, concomitant MAT use, hyperalgesia, and the presence of chronic pain can all contribute to above-average opioid requirements [22, 23]. Involvement of multimodal therapies, discussed further below, is also key in decreasing overall opioid requirements and need for opioid prescriptions at discharge [15, 24]. The treatment of acute pain in these patients is complex and continually evolving, and the inpatient care plan needs to reflect this dynamic.
Heroin and Illicit Opioid Use
The management of patients using illicit opioids prior to a traumatic event can be challenging, as there is no way to definitively verify pre-injury daily doses. The practitioner must do her best job in assessing daily MMEs based on patient-reported use to help establish a baseline and set expectations about likely ongoing needs in the setting of acute pain. For those who misuse prescription opioid medications, self-reports should be considered accurate when calculating daily MME. Assumptions about patient reports can lead to undertreatment of pain which, as discussed above, contributes to worse outcomes. For those using heroin pre-injury, available data supports the conversion of 100 mg of heroin to 15–30 MME [22•]. Once daily MME has been estimated, an equivalent dose of short-acting opioid, with additional available for breakthrough pain as needed, should be provided for a 24-h period. This allows the practitioner to more accurately assess opioid requirements. The pain regimen should then be adjusted based on the balance between pain control and somnolence or respiratory depression. Once daily requirements can more accurately be assessed, a long-acting basal opioid can be initiated, with short-acting opioids remaining available as needed for breakthrough pain [22•]. Titrations should continue, weaning doses as the acute pain requirements decrease. It is important to monitor for signs of opiate withdrawal in these patients, considering daily MME calculations are often inaccurate. Clinical decision-making tools, like the Clinical Opiate Withdrawal Scale, can be utilized to monitor for opiate withdrawal, which can further complicate the management of acute pain following traumatic injury.
Methadone
Methadone is an opioid agonist, taken orally. When used for MAT, a daily maintenance dose allows for prevention of the symptoms of withdrawal and for reduction of opioid cravings without the euphoric effects of other opioids. When utilized in the management of chronic pain, it is often administered in lower doses more frequently (twice or three times daily) to allow for more consistent pain relief, again avoiding some of the psychological effects of other opioid medications.
In patients taking methadone pre-injury, daily dose should be confirmed with their provider, when able. Providers should note that if a patient receives methadone (or buprenorphine) from an Opioid Treatment Program (or “methadone clinic”), these prescriptions will NOT be available through PDMP reporting, and will need to be confirmed by contacting the program directly. This maintenance dose should be continued while inpatient, with additional short-acting opioids administered as needed for breakthrough acute pain. The practitioner should again note that higher and more frequent doses are often required in these patients [9, 22]. Plans to de-escalate opioid therapy should be created based on the clinical scenario and expected recovery time, as well as discussions with both the patient and his or her outpatient prescriber. Attempts should be made to discontinue opioid therapy prior to discharge whenever this is clinically feasible. When this is not feasible, discharge opioid prescriptions need to be communicated to the patient’s methadone prescriber to avoid delays in care to the patient. Additionally, the practitioner should confirm that the patient has access to their maintenance methadone after discharge.
Buprenorphine (ex. Subuxone, Subutex, Belbuca, Butrans)
Buprenorphine is another medication that is used commonly in MAT, with some formulations containing naloxone (ex. Suboxone) as a deterrent against misuse. Buprenorphine is also used in the management of chronic pain, often at higher doses than typically seen with MAT. Acute pain management in patients taking buprenorphine pre-injury is, unfortunately, more complicated than in those taking methadone due to the pharmacokinetic properties of buprenorphine. Buprenorphine is a partial agonist with a “ceiling effect” that has a very high affinity for mu opioid receptors, variable effects on other receptors, and a long half-life. This results in inhibition of the analgesic effects of other opioid medications due to a variable blockade of mu receptors that changes unpredictably over time and can last up to 72 h after cessation of buprenorphine [13, 22]. Patients who have recently stopped buprenorphine and are receiving opioids for acute pain require close monitoring for this time period. Metabolism of buprenorphine lifts the mu receptor blockade, allowing for additional opioid receptor-binding without administering any additional opioids. Given the high doses of opioid medication these patients often require, they are at high risk of respiratory depression until buprenorphine is fully metabolized [13].
There are a number of strategies for the management of acute pain in patients taking buprenorphine, all of which require vigilance due to the variable pharmacokinetics of buprenorphine. Whenever feasible, the patient’s outpatient provider or a practitioner with experience in buprenorphine prescribing should be involved in the care of the patient to help guide treatment decisions and to ensure continuity of care after discharge. Additionally, use of multimodal pain management, including non-opioid medications and regional anesthesia, when applicable, is again imperative to successful acute pain control in these patients [13].
The first management decision involves whether or not to continue the patient’s buprenorphine after injury. Although there is some evidence to suggest cessation of buprenorphine will improve post-operative and post-traumatic pain control, there are just as many case reports of difficulty with post-operative pain control despite pre-procedure cessation of buprenorphine. Additionally, given buprenorphine’s partial antagonism, it may provide some benefit to pain control in the setting of opioid-induced hyperalgesia. Lastly, the sudden cessation of buprenorphine, coupled with the anxiety and stress of an acute traumatic event, could potentially increase the risk of opioid use disorder relapse [13]. In situations where overall acute pain is expected to be relatively mild, or risks appear to outweigh the benefits, continuing buprenorphine dose is certainly reasonable [13]. It can be continued at the current dose, or divided to allow for more frequent dosing, depending upon the patient’s needs [9•]. If the patient is not on maximal therapy (24–32 mg daily), increasing the daily dose becomes an option, but this should be discussed with the patient’s outpatient provider first. Opioid therapy can be used as needed, but, again, a plan should be in place to taper these medications prior to discharge, when feasible [13].
If the plan is for buprenorphine to be discontinued upon admission, this should be discussed with the patient to minimize associated emotional distress and to set expectations moving forward. The practitioner must also remember that the patient will require higher than normal doses of short-acting opioid pain medications in order to compete with buprenorphine binding, and that this requirement will change over the first 72 h as buprenorphine is metabolized [13]. Use of high mu receptor-affinity opioids (hydromorphone, morphine, and fentanyl) may help to combat this effect [22•]. Buprenorphine dose can also be converted to an equivalent methadone dose, instead of continuing buprenorphine, with the addition of supplemental short-acting opioids to the regimen for breakthrough pain; however, this will require the assistance of either a physician or pharmacist who is very skilled at methadone prescribing [9•].
When severe pain is anticipated, a monitored setting should be considered due to the anticipated high opiate requirements and subsequent concerns for respiratory depression. PCA with end-tidal CO2 monitoring can be a useful adjunct in this population as it provides a way to closely monitor opiate use and adjust the pain regimen as needed, although routine use has not been shown to significantly affect clinical outcomes when compared to intermittent dosing [6, 25]. Dexmedetomidine or ketamine infusions, as discussed below, can also be useful adjuncts in these patients, depending on the clinical scenario and opioid requirements [13].
If buprenorphine has been discontinued, a plan for discontinuation of opioid therapy and resumption of buprenorphine should be implemented, either while hospitalized or under the supervision of their outpatient provider [22•].
Mixed Opioids
Tramadol and tapentadol are medications with activity at mu receptors, although less potent than other opioids, as well as reuptake inhibition of norepinephrine and serotonin. Although this unique mechanism of action can increase efficacy, these SNRI properties do carry the rare risk of serotonin syndrome, especially when used in conjunction with amine reuptake inhibitors in certain patients [26]. Their enteral formulations also pose some limits to their efficacy in the initial resuscitation period, and the cost of tapentadol can be a limiting factor for some patients. Additionally, tramadol’s efficacy can be limited by genetic variability in its metabolism, resulting in potentially increased side effects and/or inadequate pain control in certain patients. Furthermore, due to hepatic metabolism and renal excretion, tramadol is contraindicated in renal and hepatic dysfunction. However, these agents should be considered in certain patients who will be unable to wean from opioid medications entirely prior to discharge, as they are generally considered to be safer than higher affinity opioids, and have shown some efficacy in the treatment of various chronic pain syndromes, including fibromyalgia and neuropathic pain [27].
Non-narcotic Agents
Non-narcotic analgesics are essential in the treatment of acute pain, as they have consistently been shown to decrease opioid requirements and can be especially helpful in the management of opioid-induced hyperalgesia (OIH) [24]. They are also essential in continuing to treat acute pain after opioid medications have been weaned. However, their use must be balanced with their side effect profiles and can be limited by patient comorbidities.
Acetaminophen
Scheduled acetaminophen should be considered in all patients. IV formulations have not been shown to have superior outcomes compared to enteral formulations; however, they provide an option for patients in which enteral access for medication administration does not exist. Additionally, there is some suggestion in the literature that IV formulations are less likely to cause hepatotoxicity due to decreased peak hepatic concentration compared to the oral formulation [16]. According to the American College of Gastroenterology, acetaminophen should be limited to 1000 mg per dose and 3000 mg per 24-h period in healthy patients. Patients with liver disease should limit acetaminophen to 2000 mg per 24 h period. Attempts should be made to limit the duration of maximal doses to 3–5 days when clinically feasible. Clinical judgment should be utilized regarding acetaminophen and severe liver failure [28].
Non-steroidal Anti-inflammatory Drugs
Non-steroidal anti-inflammatory drugs (NSAIDs) can also be helpful in the management of acute pain, especially when paired with acetaminophen. A recent Cochrane review showed that the combination of 200 mg ibuprofen and 500 mg acetaminophen has a number needed to treat (NNT) to achieve a 50% reduction in pain of only 1.5, thus demonstrating that even low doses of these medications can lead to adequate pain control [29]. Centrally acting NSAIDs, such as celecoxib, have shown to be especially helpful in the management of OIH [9•]. Unfortunately, the use of these medications is limited by renal impairment, gastrointestinal side effects, history of gastric bypass, and potential concerns regarding platelet inhibition and effects on fracture healing [5, 30]. The minimal effective NSAID dose should be utilized, starting with a low dose and titrating up. High doses should be limited to short courses to help minimize side effects. NSAIDs should not be used in patients taking warfarin or other anticoagulation or antiplatelet medications. Care should also be used in patients taking SSRIs or glucocorticoids, as these medications are associated with increased gastrointestinal side effects. NSAIDs can also increase the efficacy of ACE inhibitors, resulting in hyperkalemia. NSAIDs should also be avoided in patients taking high-dose methotrexate [31].
Ketamine
Ketamine is unique in that it has both sedative-hypnotic and analgesic properties with minimal effects on hemodynamics and significantly lower risk of respiratory depression and/or hypoxia. Unfortunately, higher doses of ketamine have been associated with hallucinations and other psychotropic side effects [32]. Despite this, ketamine infusion can reduce opioid requirements at both high and low doses and has been shown to achieve more effective pain control than opioids alone [16, 30, 32, 33]. Additionally, more recent research suggests that low doses (0.1–0.4 mg/kg/h) have minimal psychotropic effects [5•]. Ketamine also may prevent the development of tolerance to opioids, in addition to decreasing overall opioid requirements [9•]. It has been shown to augment the perception of allodynia in patients with complex regional pain syndrome, suggesting particular efficacy in patients with chronic pain [27]. Additionally, it can be a useful adjunct in patients with OIH or recent buprenorphine ingestion, when opioids tend to be less effective [13]. Furthermore, it can reduce the risk for development of chronic post-surgical pain [8]. Institutions should consider developing a protocol for ketamine use in the management of acute pain, and practitioners should consider it if having difficulty achieving adequate control of acute pain.
Alpha-2 Agents (Dexmedetomidine and Clonidine)
Both clonidine and dexmedetomidine can be useful adjuncts in the management of acute pain, and clonidine has some off-label use in the treatment of opioid withdrawal [16, 30]. Both drugs have analgesic properties, in addition to sedative and anxiolytic properties, and have been shown to have opioid-sparing effects [5•]. Unfortunately, these medications can also lead to hypotension and bradycardia, so care must be taken if attempting to use early in the trauma resuscitation, and it is preferred to utilize these medications in the post-resuscitative phase. Dexmedetomidine use is limited to IV infusion, whereas clonidine can be administered enterally or transdermally [5•]. Cost of dexmedetomidine can also be a limiting factor; however, transition to clonidine early in the clinical course may help to offset this [30]. Additionally, dexmedetomidine may be of particular benefit in the management of critically ill trauma patients. It has been shown to provide non-inferior sedation when compared to both propofol and midazolam in multiple multi-center, randomized clinical trials, and was also associated with increased patient interaction and communication, as well as decreased duration of mechanical ventilation [34]. Due to these findings, it may be of particular use in mechanically ventilated patients who require frequent neurological assessments. More research needs to be performed to fully assess the potential for routine use in the management of acute pain due to traumatic injuries.
Methoxyflurane
Methoxyflurane is an inhalation hydrocarbon anesthetic that has been used in countries outside the USA for the management of acute pain. Methoxyflurane is ideal for acute pain management given its rapid onset and relative lack of prolonged adverse effects [35]. Borobia et al. demonstrated that inhaled methoxyflurane provided more rapid and better pain control compared with a standard analgesic group [36]. This medication has been withdrawn from the US market. However, more recent studies have been able to show some promise for use of this medication in the management of acute pain and may present a case for its reintroduction.
Amine Reuptake Inhibitors
Amine reuptake inhibitors (ARIs) such as duloxetine and amitriptyline are commonly used in the management of chronic pain. When feasible, these medications should be continued while patients are hospitalized, as long as there is not a high risk or clinical concern for serotonin syndrome. Practitioners should be aware that there have been case reports of serotonin syndrome in patients on these medications in conjunction with tramadol, especially in CYP2D6 poor metabolizers. Concomitant use of these medications should be avoided in known poor metabolizers, and closely monitored for signs/symptoms of serotonin syndrome in those who are not [26]. Practitioners can consider starting these medications as a part of the acute pain management plan, especially in patients with significant anxiety related to the traumatic event [9•]. However, discussion regarding the risks, benefits, and side effects should be undertaken with the patient, and the practitioner should note that these medications take a variable amount of time to reach full effect. Duloxetine in particular has shown efficacy in the treatment of chronic back pain and fibromyalgia, as well as neuropathic pain following spinal cord injury. Amitriptyline has also been studied in the management of chronic pain; however, it has a much larger and more severe side effect profile, including potential for lethal overdose [27, 30]. More research is needed to fully assess the potential efficacy of these medications in the management of acute traumatic pain.
GABA Analogs
Gabapentin and pregabalin are known to be effective in the treatment of neuropathic pain. They have also shown promise in the treatment of chronic pain conditions, especially when combined with anti-inflammatories [27]. There is some literature to suggest they can be useful in the management of hyperalgesia and they have been shown to reduce sensitization induced by surgery [8, 9, 30]. Pregabalin is absorbed more quickly than gabapentin, so it may be more efficacious in the management of acute pain. Either medication carries the risk for withdrawal, so they should be continued in patients taking these medications pre-injury, unless contraindicated [16]. Unfortunately, gabapentin and pregabalin are limited to patients with proximal enteral access due to their duodenal absorption and can also contribute to somnolence and ataxia [5•]. They also require dose adjustments in the setting of renal impairment [30]. These medications also have the potential for misuse or illicit use, and must be utilized with caution. Regardless, their use can be helpful in the management of acute traumatic pain, and should be considered, especially in patients with hyperalgesia.
Muscle Relaxants
Muscle relaxants, such as cyclobenzaprine or methocarbamol, can be useful adjuncts in the management of acute traumatic pain, especially in the setting of musculoskeletal injuries. These medications also have been shown to be efficacious in the treatment of chronic back and musculoskeletal pain, so they can help to address elements of chronic pain that may be contributing to inadequate acute pain control [27]. Caution must be exercised when utilizing these medications, however, as they do have some sedating effects and do carry potential for misuse [16, 30]. Routine use of benzodiazepines for their anti-spasmodic effects is not recommended given the risk for misuse and dependence.
Regional Anesthesia
Lidocaine patches have not been consistently shown to be efficacious in the management of acute or chronic pain. However, the side effect profile is relatively low, and some clinical trials do suggest efficacy in certain situations, such as neuropathic pain associated with traumatic injury, acute pain due to herpes zoster, and post-herpetic neuralgia. Additionally, there is some evidence to suggest efficacy as a part of a multimodal rib fracture treatment plan, although there is conflicting data in the literature [16, 27, 30]. Implementing their use over areas of point tenderness should be considered unless contraindicated, given the potential benefit and relatively low risk.
Fascial plane blocks are useful in the management of a wide variety of traumatic injuries and the management of post-operative pain. These include fascia iliaca, erector spinae plane (ESP), serratus anterior plane (SAP), and transversus abdominis plane (TAP) blocks [5•]. Given that these blocks do not involve a catheter that must remain in place, they can be utilized in patients with altered mental status or coagulopathy. Additionally, they have minimal effect on hemodynamics, and can potentially be performed in the emergency department (ED) to facilitate rapid control of acute pain, giving them some advantages over neuraxial anesthesia [16, 37, 38]. However, their utility is potentially limited by their limited duration of action. More research is needed in order to fully assess the routine use of these blocks for traumatic injury and to facilitate the creation of protocols for implementing their use, especially early in the hospitalization or in the ED.
Neuraxial anesthesia and peripheral nerve blocks have also been shown to reduce opioid use when used appropriately. Epidural anesthesia has shown great efficacy in pain management after rib fractures, and peripheral nerve blocks can be quite helpful in the management of extremity trauma [5, 39]. Unfortunately, catheter-based regional anesthesia is contraindicated in coagulopathy and in patients with altered mental status, and may have limited utility in some severe trauma patients. They also can affect hemodynamics, which can limit their effectiveness in certain patients. Despite this, neuraxial anesthesia can be very useful in the right patient and should be considered when appropriate [15].
Discharge Planning
Early discharge planning is essential in the success of patients with pre-injury opioid use and those with a history of chronic pain [22•]. The patient, their support system, and any outpatient providers should be involved in the discharge planning process whenever possible [23]. When feasible, additional opioids should be weaned prior to discharge, especially in patients at a high risk for becoming lost to follow-up or in patients with known, or high risk for, OUD. When this is not feasible, a concrete plan for tapering additional opioids should be implemented. Prescriptions for additional opioids should be limited to a week or less when possible and must be discussed with any outpatient opioid or MAT provider [22]. Education about safe storage and disposal practices should be provided to all patients receiving an opioid prescription on discharge [40]. Additionally, thorough discharge instructions that specifically describe the pain management plan should be given to all patients in order to minimize confusion regarding pain management following discharge [7, 41].
Any patient with known OUD or chronic pain, as well as those deemed to be high risk for the development of either condition, should also receive close hospital follow-up to monitor for effective pain control, as ineffective pain control after hospital discharge puts patients at higher risk for the development of chronic pain, long-term opioid use, and illicit substance use [9•]. Ineffective pain control after discharge can also be debilitating for patients and may prevent return to work or to normal life [7]. Trevino et al. found that a multidisciplinary trauma follow-up clinic focusing on quality of life 1 week after discharge helped improve follow-up rates substantially compared to traditional 2-week follow-up. They also incidentally identified an increase in psychology visits in the 1-week follow-up group [42]. This suggests that close follow-up is not only feasible, but increases patient-provider interactions and can help with early identification of barriers in the trauma patient’s return to normal life, in order to facilitate appropriate, multidisciplinary treatment.
In addition to close follow-up, patients with OUD should be referred to substance use treatment on hospital discharge. They should also be educated on the importance of clean needles and safe injecting practices. Opioid overdose education should also be provided, and strong consideration for intranasal naloxone prescription on discharge should be made [22•].
Conclusions
The management of acute pain in patients with chronic pain or pre-injury opioid dependence is complex. Provider education and the use of multimodal pain management in the acute setting are extremely important for achieving adequate pain control after a traumatic event. Additionally, providers need to take great care in standardized and frequent pain assessments to allow for titration and re-evaluation of the pain management regimen in order to balance adequate pain control with potential side effects. More research is needed in order to create an evidence-based, standardized approach to the management of acute pain due to traumatic injury in patients with chronic pain and/or opioid dependence.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cannon R, Bozeman M, Miller KR, Smith JW, Harbrecht B, Franklin G, et al. The prevalence and impact of prescription controlled substance use among injured patients at a level I trauma center. J Trauma Acute Care Surg. 2014;76:172–5. https://doi.org/10.1097/TA.0b013e3182ab10de.
Holman JE, Stoddard GJ, Higgins TF. Rates of prescription opiate use before and after injury in patients with orthopaedic trauma and the risk factors for prolonged opiate use. 2013. https://doi.org/10.2106/JBJS.L.00619
Hsiang WR, McGeoch C, Lee S, Cheung W, Becher R, Davis KA, et al. Opioid dependency is independently associated with inferior clinical outcomes after trauma. Injury. 2019;50:192–6. https://doi.org/10.1016/j.injury.2018.10.015.
Pandya U, Shay O’mara M, Wilson W, et al. Association for Academic Surgery Impact of preexisting opioid use on injury mechanism, type, and outcome. 2015. https://doi.org/10.1016/j.jss.2015.05.033.
• Karamchandani K, Klick JC, Linskey Dougherty M, et al. Pain management in trauma patients affected by the opioid epidemic: a narrative review. J. Trauma Acute Care Surg. 2019;87:430–9 Provides a recent and thorough review of multimodal pain management in critically-ill trauma patients.
Rockett M, Creanor S, Squire R, Barton A, Benger J, Cocking L, et al. The impact of emergency department patient-controlled analgesia (PCA) on the incidence of chronic pain following trauma and non-traumatic abdominal pain. Anaesthesia. 2019;74:69–73. https://doi.org/10.1111/anae.14476.
Goldsmith H, McCloughen A, Curtis K. The experience and understanding of pain management in recently discharged adult trauma patients: a qualitative study. Injury. 2018;49:110–6. https://doi.org/10.1016/j.injury.2017.09.027.
General M, Wang J, Fregoso G, et al. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. 2019.
• Dever C. Treating acute pain in the opiate-dependent patient. J Trauma Nurs. 2017;24:292–9. https://doi.org/10.1097/JTN.0000000000000309Provides an evidence-based guideline for the management of acute pain in patients with preexisting opioid dependence.
Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156:569–76. https://doi.org/10.1097/01.j.pain.0000460357.01998.f1.
Cragg A, Hau JP, Woo SA, Kitchen SA, Liu C, Doyle-Waters MM, et al. Risk factors for misuse of prescribed opioids: a systematic review and meta-analysis. Ann Emerg Med. 2019;74:634–46.
Daoust R, Paquet J, Moore L, Émond M, Gosselin S, Lavigne G, Choinière M, Boulanger A, Mac-Thiong JM, Chauny JM. Early factors associated with the development of chronic pain in trauma patients. Pain Res Manag. 2018. https://doi.org/10.1155/2018/7203218
Anderson A, Quaye ANA, Nalan Ward E, et al. To stop or not, that is the question acute pain management for the patient on chronic buprenorphine. Anesthesiology. 2017;126:1180–6.
Pagé MG, Kudrina I, Zomahoun HTV, Croteau J, Ziegler D, Ngangue P, et al. A systematic review of the relative frequency and risk factors for prolonged opioid prescription following surgery and trauma among adults. Ann Surg. 2020;271:845–54. https://doi.org/10.1097/sla.0000000000003403.
Ahmadi A, Bazargan-Hejazi S, Zadie ZH, et al. Pain management in trauma: a review study. J Inj Violence Res. 2016;8:89–98. https://doi.org/10.5249/jivr.v8i2.707.
Sullivan D, Lyons M, Montgomery R, Quinlan-Colwell A. Exploring opioid-sparing multimodal analgesia options in trauma: a nursing perspective. J Trauma Nurs. 2016;23:361–75.
Ducharme J, Moore S. Opioid use disorder assessment tools and drug screening. Mo Med. 2019;116:318–24.
Melcer T, Walker J, Sazon J, et al. Outpatient pharmacy prescriptions during the first year following serious combat injury: a retrospective analysis. Mil Med. 2020. https://doi.org/10.1093/milmed/usaa038.
D’Souza RS, Eldrige JS. Prescription drug monitoring program-StatPearls - NCBI Bookshelf. In: StatPearls. 2020. https://www-ncbi-nlm-nih-gov.ahecproxy.ncahec.net/books/NBK532299/. Accessed 13 Jun 2020
Rhodes E, Wilson M, Robinson A, et al. The effectiveness of prescription drug monitoring programs at reducing opioid-related harms and consequences: a systematic review. BMC Health Serv Res. 2019;19
Rasubala L, Pernapati L, Velasquez X, Burk J, Ren YF. Impact of a mandatory prescription drug monitoring program on prescription of opioid analgesics by dentists. PLoS One. 2015;10:e0135957. https://doi.org/10.1371/journal.pone.0135957.
• Raub JN, Vettese TE. Acute pain management in hospitalized adult patients with opioid dependence: a narrative review and guide for clinicians. J Hosp Med. 2017;12:375–9. https://doi.org/10.12788/jhm.2733Provides a review of available literature with subsequent recommendations for the management of acute pain in patient’s with preexisting opioid dependence.
Huxtable CA, Roberts LJ, Somogyi PM. Acute pain management in opioid-tolerant patients: a growing challenge. Anaesth Intensive Care. 2011;39:787–988.
Hamrick KL, Beyer CA, Lee JA, et al. Multimodal analgesia and opioid use in critically ill trauma patients. J Am Coll Surg. 2019;228:769–775.e1. https://doi.org/10.1016/j.jamcollsurg.2019.01.020.
Smith JE, Rockett M, Creanor S, et al. PAin SoluTions In the Emergency Setting (PASTIES)--patient controlled analgesia versus routine care in emergency department patients with pain from traumatic injuries: randomised trial. BMJ. 2015;350:h2988. https://doi.org/10.1136/bmj.h2988.
Nelson EM, Philbrick AM. Avoiding serotonin syndrome: the nature of the interaction between tramadol and selective serotonin reuptake inhibitors. Ann Pharmacother. 2012;46(12):1712–6 https://doi-org.ahecproxy.ncahec.net/10.1345/aph.1Q748.
Nicol AL, Hurley RW, Benzon HT. Alternatives to opioids in the pharmacologic management of chronic pain syndromes: a narrative review of randomized, controlled, and blinded clinical trials. Anesth Analg. 2017;125:1682–703.
Herrera JL. Medications and the Liver-American College of Gastroenterology. 2007, Updated 2012. https://gi.org/topics/medications-and-the-liver/. Accessed 20 Jul 2020
Moore RA, Derry S, Aldington D, Wiffen PJ. Single dose oral analgesics for acute postoperative pain in adults-an overview of Cochrane reviews. Cochrane Database Syst Rev. 2015;2017
Oyler DR, Parli SE, Bernard AC, Chang PK, Procter LD, Harned ME. Nonopioid management of acute pain associated with trauma: focus on pharmacologic options. J Trauma Acute Care Surg. 2015;79:475–83.
Solomon. NSAIDs: therapeutic use and variability of response in adults-UpToDate. 2020. https://www.uptodate.com/contents/nsaids-therapeutic-use-and-variability-of-response-in-adults?search=nsaids&source=search_result&selectedTitle=2~147&usage_type=default&display_rank=1#H8. Accessed 25 Jul 2020
Takieddine SC, Droege CA, Ernst N, Droege ME, Webb M, Branson RD, et al. Ketamine versus hydromorphone patient-controlled analgesia for acute pain in trauma patients. J Surg Res. 2018;225:6–14. https://doi.org/10.1016/j.jss.2017.12.019.
Häske D, Böttiger BW, Bouillon B, Fischer M, Gaier G, Gliwitzky B, et al. Analgesia in patients with trauma in emergency medicine-a systematic review and meta-analysis. Dtsch Arztebl Int. 2017;114:785–92. https://doi.org/10.3238/arztebl.2017.0785.
Jakob SM, Ruokonen E, Grounds RM, et al. Dexmedetomidine for Long-Term Sedation Investigators. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA. 2012;307(11):1151–60. https://doi.org/10.1001/jama.2012.304.
Porter KM, Dayan AD, Dickerson S, Middleton PM. The role of inhaled methoxyflurane in acute pain management. Open Access Emerg Med. 2018;10:149–64.
Borobia AM, Collado SG, Cardona CC, Pueyo RC, Alonso CF, Torres IP, et al. Inhaled methoxyflurane provides greater analgesia and faster onset of action versus standard analgesia in patients with trauma pain: InMEDIATE: a randomized controlled trial in emergency departments. Ann Emerg Med. 2020;75:315–28. https://doi.org/10.1016/j.annemergmed.2019.07.028.
Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: a retrospective cohort study. Anaesthesia. 2019;74:585–93. https://doi.org/10.1111/anae.14579.
Gadsden J, Warlick A. Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth. 2015;8:45–55.
Galvagno SM, Smith CE, Varon AJ, et al. Pain management for blunt thoracic trauma: a joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016;81:936–51. https://doi.org/10.1097/TA.0000000000001209.
Gregorian R, Marrett E, Sivathanu V, Torgal M, Shah S, Kwong WJ, et al. Safe opioid storage and disposal: a survey of patient beliefs and practices. J Pain Res Volume. 2020;13:987–95. https://doi.org/10.2147/jpr.s242825.
Goldsmith H, Curtis K, McCloughen A. Effective pain management in recently discharged adult trauma patients: identifying patient and system barriers, a prospective exploratory study. J Clin Nurs. 2017;26:4548–57. https://doi.org/10.1111/jocn.13792.
Trevino C, Geier T, Timmer-Murillo SC, Shawlin M, Milia DJ, Codner P, et al. Feasibility of a trauma quality of life follow up clinic. J Trauma Acute Care Surg. 2020;89:226–9. https://doi.org/10.1097/TA.0000000000002672.
Acknowledgements
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pain Management in Trauma
Rights and permissions
About this article
Cite this article
Fontaine, D., Hoffman, M.R. Management of Acute Pain Due to Traumatic Injury in Patients with Chronic Pain and Pre-injury Opioid Use. Curr Trauma Rep 7, 24–32 (2021). https://doi.org/10.1007/s40719-020-00207-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40719-020-00207-5