Abstract
Purpose of Review
The cardiovascular morbidity associated with obstructive sleep apnea (OSA) changes with aging. This review addresses unique aspects of OSA-associated hypertension and cardiovascular disease (CVD) in the elderly.
Recent Findings
The risk of hypertension and CVD in OSA diminishes with aging. The standard apnea hypopnea index cut-offs for OSA diagnosis and severity do not predict CVD or mortality in the elderly. Further, the impact of continuous positive airway pressure (CPAP) treatment on hypertension and mortality is inconsistent in this population. A therapeutic effect of CPAP is noted in some studies in subsets of elderly with high CPAP adherence.
Summary
Aging-related physiological changes in upper airway function and ventilatory control function modify the impact of OSA on hypertension and CVD. Future research should identify common endotypes of OSA and optimal OSA severity metrics from polysomnography to inform treatment algorithms for the elderly. Finally, promotion of CPAP adherence in this population may improve CVD outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of obstructive sleep apnea (OSA) increases with age. Despite a higher prevalence in the elderly, the impact of OSA and its treatment on hypertension and cardiovascular outcomes in this population is not well understood. The evidence supports OSA as a risk factor for hypertension and some forms of cardiovascular disease (CVD) in adults. However, this association remains controversial in the elderly. The role of potential moderators of CVD risk and treatment response in the elderly with OSA needs to be defined for optimal treatment strategy. Here, we provide a narrative review of (i) the changes in OSA and hypertension risk, (ii) potential mechanisms underlying this change, and (iii) the effectiveness of OSA treatment in improving systemic blood pressure (BP) and CVD in the elderly, comparing it to middle-aged adults when applicable.
Effect of Aging on Sleep Apnea
The prevalence of OSA, defined by AHI of 15/hour or more, increases with age, likely reaching a plateau of about 20% after 60 years [1,2,3,4]. In men, the AHI increases linearly with age, while in women, the AHI rises after 50 years, approximating the prevalence of OSA in men. This increase in OSA prevalence in women is hypothetically driven by post-menopausal changes and modified by hormone replacement therapy [5, 6]. Symptoms (snoring and witnessed apnea) and obesity or central fat distribution are less predictive of OSA risk in the elderly compared to middle-aged individuals [3, 7]. Aging increases the pharyngeal collapsibility due to anatomical [8, 9] and neuromuscular changes resulting in higher upper airway resistance and lower central reflex and ventilatory motor output during sleep [10,11,12,13,14]. This may explain the increased propensity for apnea expression in the elderly independent of obesity.
Sleep Apnea and Hypertension in Adults
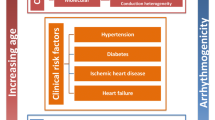
Pathophysiology
Chronic intermittent hypoxia, sleep fragmentation, and excessive intrathoracic pressure swings due to upper airway collapse during sleep cause perturbations in autonomic function, renin angiotensin system (RAS) activation, inflammation, and oxidative stress. The pathophysiological consequences include the development of systemic hypertension, as shown in Figure 1. There is significant cross-talk between the mechanistic pathways. For example, sympathetic hyperactivity exacerbates inflammation, RAS activation, and endothelial dysfunction. RAS activation, in turn, increases fluid retention with nocturnal fluid shifts and blunts nocturnal dipping of BP. Oxidative stress and inflammatory biomarkers, such as C-reactive protein, interleukins 1,2, and 6, tumor necrosis factor alpha, and interferon gamma, are upregulated leading to permanent remodeling of the systemic vasculature [15,16,17,18,19]. Potential effects of aging on these pathophysiological pathways are highlighted in Figure 1 (red font).
OSA and Hypertension: Epidemiologic and Clinical Studies in Adults
Multiple clinical and community-based cohort studies have demonstrated a relationship between OSA and the risk of hypertension (Table 1). These studies adjusted for age, obesity, and the severity of OSA showed a dose-response relationship with the risk of hypertension. Overall, the association of OSA with hypertension was stronger in clinical cohorts compared to community-based cohorts. An early report from the Wisconsin Sleep Cohort showed that moderate to severe OSA was associated with more than 2.5-fold increased adjusted risk of incident hypertension after 4 years [25]. In this cohort, REM sleep–related OSA has also been noted as a risk factor for incident hypertension [33]. However, few cohorts have failed to detect a significant association between OSA and incident hypertension. A community-based longitudinal study of more than 2000 participants, age 30–70 years and followed for 7.5 years, did not find an increase in the risk of incident hypertension after adjustment for age [34]. Notable differences between this Australian cohort and the Wisconsin cohort were OSA assessment methods (type III sleep apnea test vs. polysomnography, respectively) and obesity (body mass index 25.5±3.7 vs. 27±5 kg/m2). Hence, an underestimation of OSA and lower obesity rates may explain the negative findings reported in the study by Cano-Pumarega et al [34]. Another report on OSA and the risk of incident hypertension from the Sleep Heart Health Study found that the risk was not statistically significant after adjustment for BMI, even in the severe OSA group (odds ratio, OR=1.51, 95% confidence interval, CI=0.93–2.47) [35]. Notably, the participants’ mean age in this study was 60 years compared to a mean age of 45 years in the study by Peppard et al [25].
CPAP treatment lowers sympathetic and RAS activity, which mediates BP reduction [36, 37]. In an observational study of OSA patients who were continuous positive airway pressure (CPAP) treatment users vs. non-users, Marin et al. showed that untreated OSA increased (OR 1.33–1.96) and treated OSA decreased the risk of incident hypertension (OR 0.53–0.94) compared to a control group without OSA [38]. Several recent meta-analyses have been published on the treatment effects of OSA on hypertension, as summarized in Table 1. Besides severe OSA and higher CPAP adherence, CPAP treatment’s effectiveness in reducing BP is greater in symptomatic patients and those with resistant hypertension [39,40,41]. Some trials have failed to detect a BP response to CPAP treatment, likely due to the abovementioned moderators of CPAP treatment effects [42,43,44,45]. Overall, CPAP effects on BP are less than some antihypertension medications [46].
Sleep Apnea and Hypertension in Elderly
The strength of the evidence supporting OSA as an independent risk factor for hypertension is weaker in the elderly compared to middle-aged adults. In the Sleep Heart Health Study, the risk for hypertension in the severe OSA group (AHI ≥30) over 65 years of age was 23% higher but statistically insignificant compared to the control group without OSA. However, a significant 64% increased risk of hypertension was noted in the middle-aged severe OSA group [20]. Another report from the same cohort found no association of OSA with isolated systolic hypertension, which is more prevalent in the elderly [24]. In contrast, a study from France in the elderly found a significant increase in systolic ambulatory and diastolic nocturnal BP in the severe OSA group compared to those without OSA [47]. Follow-up reports from the same group found that severe OSA conferred an 80% higher risk of incident hypertension after 3 years [48], and the oxygen desaturation index (ODI) was a significant predictor of elevated daytime ambulatory BP [49]. Sex differences in the risk of hypertension related to OSA may exist, with studies suggesting a higher risk only in women [50, 51]. Population differences in sex, obesity, and other moderators of the OSA-hypertension association may account for the disparate findings in the elderly.
Few trials have examined the effects of CPAP intervention specifically in the elderly. CPAP improves the quality of life, symptoms, mood, and neurocognitive function and is cost-effective in this population [26, 27]. However, as summarized in Table 1, CPAP treatment does not significantly reduce BP in the elderly [26, 28].
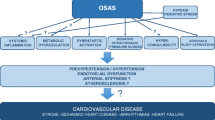
Does Sleep Apnea or CPAP Treatment Impact Cardiovascular Disease and Mortality in the Elderly?
Prospective cohorts have reported that severe OSA confers an increased risk of cerebrovascular disease (CVA) in the elderly, but not coronary heart disease (CHD) [52,53,54]. Further, sex differences are reported in the risk of CVD associated with OSA in the elderly. A prospective cohort of women aged 65 years or more with untreated OSA did not demonstrate a significant increase in CVA or CHD risk compared to those without OSA [55]. In a small, single-center study, OSA increased the risk of arrhythmia and cardiovascular events 6 months after acute myocardial infarction in the elderly [56]. Another report from a post-acute coronary syndrome sample of patients enrolled in a cardiac rehabilitation program found that OSA was associated with diastolic dysfunction in those less than 60 but not in the group over 60 years of age [57].
Similarly, early studies demonstrated that the association between OSA and mortality is attenuated with aging [58, 59]. In a study of over fourteen-thousand adult men, aged 20–93 years with suspected or diagnosed OSA, those aged ≥ 50 years did not have excess all-cause mortality compared to the general population [60]. Another study of over three-thousand men followed for 10 years reported an increase in overall and cardiovascular mortality in those with symptoms of OSA (versus those without symptoms) in the <60-year group but not in the ≥ 60-year group [61]. In the Sleep Heart Health Study, all-cause mortality in severe OSA was 46% higher than those without OSA. Further age and sex stratifications revealed that the increased mortality was driven by men ≤ 70 years (adjusted hazard ratio 2.09, CI 1.31–3.33) [62]. In contrast, OSA with daytime sleepiness was shown to increase the mortality risk 2.3-fold in an elderly cohort followed for more than 13 years, after adjustment for other risk factors such as sex and sleep duration [63]. Another factor that may impact the association of OSA with mortality in the elderly is the hypopnea definition used to diagnose OSA. When hypopnea is defined by oxygen desaturation alone, without considering arousals, severe OSA is associated with a significant and more than 2-fold increase in cardiovascular mortality in the elderly [64]. This is not surprising, since sleep fragmentation with aging is common and multifactorial.
Regarding CPAP treatment effects, a retrospective analysis of Medicare beneficiaries (≥ 65 years) with CPAP-treated OSA and followed for 25 months showed a 2% reduction in risk of CVA attributable to each month of CPAP use [65]. A prospective study on 166 CVA patients followed for 5 years (mean age 73 years, 96 with AHI≥20/hour) after hospitalization for ischemic CVA showed that patients with untreated OSA had increased mortality (HR, 1.58; 95% CI, 1.01–2.49) compared to those treated with CPAP [66]. In the elderly with moderate to severe OSA, CPAP treatment of more than 4 h nightly improves survival compared to untreated OSA [67, 68]. Many observational studies did not assess CPAP adherence, and low treatment adherence is a particular concern amongst the elderly [69, 70]. The importance of CPAP adherence is underscored in an observational study of 939 patients, 65 years or more of age with OSA, followed for 10 years. The mortality was significantly increased by 120% in the group with untreated severe OSA (AHI ≥30/hour) compared to those with AHI <15/hour [27]. Notably, CPAP adherence was a significant predictor of change in cardiovascular mortality in the treated group. Consistent with the results discussed above, a meta-analysis by Kim et al, showed that the observational studies suggested a significant reduction in the risk of CVA (Relative Risk, RR=0.27, CI 0.14-0.53) and cardiac events (RR=0.54, CI 0.38-0.75). Howwever, these trends were not confirmed by the randomized trials included in this meta-analysis, except in the subgroup with high CPAP adherence [71].
Conclusions
OSA appears to play a lesser role in propagating hypertension and CVD in the elderly compared to middle-aged adults. This may be due to survival bias or ischemic preconditioning of cardiovascular tissues caused by chronic intermittent hypoxia in OSA. Nevertheless, factors such as sex, obesity, symptoms, comorbidity, assessment methods, and definition of OSA influence the association of OSA with hypertension and CVD. These factors require systematic examination in adequately powered prospective studies. The endotypes of OSA may further affect CVD risk and treatment response in the elderly with OSA and merit further investigation [72]. Finally, CPAP adherence is a crucial determinant of CPAP treatment response in the elderly. Clinical trials in the elderly, promoting and controlling for CPAP adherence, are urgently needed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
McMillan A, Morrell MJ. Sleep disordered breathing at the extremes of age: the elderly. Breathe (Sheff). 2016;12(1):50–60.
Fietze I, Laharnar N, Obst A, Ewert R, Felix SB, Garcia C, et al. Prevalence and association analysis of obstructive sleep apnea with gender and age differences - results of SHIP-Trend. J Sleep Res. 2019;28(5):e12770.
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162(8):893–900.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Huang T, Lin BM, Redline S, Curhan GC, Hu FB, Tworoger SS. Type of menopause, age at menopause, and risk of developing obstructive sleep apnea in postmenopausal women. Am J Epidemiol. 2018;187(7):1370–9.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med. 2001;163(3 Pt 1):608–13.
Chung S, Yoon IY, Lee CH, Kim JW. Effects of age on the clinical features of men with obstructive sleep apnea syndrome. Respiration. 2009;78(1):23–9.
Shigeta Y, Enciso R, Ogawa T, Clark GT. Changes in three dimensional simulation models of the airway which are due to increases in age or body mass index. Stud Health Technol Inform. 2008;132:460–2.
Malhotra A, Huang Y, Fogel R, Lazic S, Pillar G, Jakab M, et al. Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med. 2006;119(1):72 e9–14.
Eikermann M, Jordan AS, Chamberlin NL, Gautam S, Wellman A, Lo YL, et al. The influence of aging on pharyngeal collapsibility during sleep. Chest. 2007;131(6):1702–9.
Kirkness JP, Schwartz AR, Schneider H, Punjabi NM, Maly JJ, Laffan AM, et al. Contribution of male sex, age, and obesity to mechanical instability of the upper airway during sleep. J Appl Physiol. 1985). 2008;104(6):1618–24.
Worsnop C, Kay A, Kim Y, Trinder J, Pierce R. Effect of age on sleep onset-related changes in respiratory pump and upper airway muscle function. J Appl Phys. 1985). 2000;88(5):1831–9.
Erskine RJ, Murphy PJ, Langton JA, Smith G. Effect of age on the sensitivity of upper airway reflexes. Br J Anaesth. 1993;70(5):574–5.
Klawe JJ, Tafil-Klawe M. Age-related response of the genioglossus muscle EMG-activity to hypoxia in humans. J Physiol Pharmacol. 2003;54(Suppl 1):14–9.
Jurado-Gamez B, Fernandez-Marin MC, Gomez-Chaparro JL, Munoz-Cabrera L, Lopez-Barea J, Perez-Jimenez F, et al. Relationship of oxidative stress and endothelial dysfunction in sleep apnoea. Eur Respir J. 2011;37(4):873–9.
Gottlieb DJ, Punjabi NM, Mehra R, Patel SR, Quan SF, Babineau DC, et al. CPAP versus oxygen in obstructive sleep apnea. N Engl J Med. 2014;370(24):2276–85.
Baessler A, Nadeem R, Harvey M, Madbouly E, Younus A, Sajid H, et al. Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers - a meta-analysis. J Inflamm (Lond). 2013;10:13.
Del Ben M, Fabiani M, Loffredo L, Polimeni L, Carnevale R, Baratta F, et al. Oxidative stress mediated arterial dysfunction in patients with obstructive sleep apnoea and the effect of continuous positive airway pressure treatment. BMC Pulm Med. 2012;12:36.
Paz YMHL, Hazen SL, Tracy RP, Strohl KP, Auckley D, Bena J, et al. Effect of continuous positive airway pressure on cardiovascular biomarkers: the sleep apnea stress randomized controlled trial. Chest. 2016;150(1):80–90.
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study JAMA. 2000;283(14):1829–36.
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Leiby BE, Vela-Bueno A, et al. Association of hypertension and sleep-disordered breathing. Arch Intern Med. 2000;160(15):2289–95.
Lavie P, Herer P, Hoffstein V. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. BMJ. 2000;320(7233):479–82.
Grote L, Ploch T, Heitmann J, Knaack L, Penzel T, Peter JH. Sleep-related breathing disorder is an independent risk factor for systemic hypertension. Am J Respir Crit Care Med. 1999;160(6):1875–82.
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111(5):614–21.
Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–84.
McMillan A, Bratton DJ, Faria R, Laskawiec-Szkonter M, Griffin S, Davies RJ, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Respir Med. 2014;2(10):804–12.
Martinez-Garcia MA, Chiner E, Hernandez L, Cortes JP, Catalan P, Ponce S, et al. Obstructive sleep apnoea in the elderly: role of continuous positive airway pressure treatment. Eur Respir J. 2015;46(1):142–51.
Ponce S, Pastor E, Orosa B, Oscullo G, Catalan P, Martinez A, et al. The role of CPAP treatment in elderly patients with moderate obstructive sleep apnoea: a multicentre randomised controlled trial. Eur Respir J. 2019;54(2).
Bakker JP, Edwards BA, Gautam SP, Montesi SB, Duran-Cantolla J, Aizpuru F, et al. Blood pressure improvement with continuous positive airway pressure is independent of obstructive sleep apnea severity. J Clin Sleep Med. 2014;10(4):365–9.
Fava C, Dorigoni S, Dalle Vedove F, Danese E, Montagnana M, Guidi GC, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea a systematic review and meta-analysis. Chest. 2014;145(4):762–71.
Iftikhar IH, Hays ER, Iverson MA, Magalang UJ, Maas AK. Effect of oral appliances on blood pressure in obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med. 2013;9(2):165–74.
Iftikhar IH, Valentine CW, Bittencourt LR, Cohen DL, Fedson AC, Gislason T, et al. Effects of continuous positive airway pressure on blood pressure in patients with resistant hypertension and obstructive sleep apnea: a meta-analysis. J Hypertens. 2014;32(12):2341–50 discussion 50.
Mokhlesi B, Finn LA, Hagen EW, Young T, Hla KM, Van Cauter E, et al. Obstructive sleep apnea during REM sleep and hypertension. results of the Wisconsin Sleep Cohort. Am J Respir Crit Care Med. 2014;190(10):1158–67.
Cano-Pumarega I, Duran-Cantolla J, Aizpuru F, Miranda-Serrano E, Rubio R, Martinez-Null C, et al. Obstructive sleep apnea and systemic hypertension: longitudinal study in the general population: the Vitoria Sleep Cohort. Am J Respir Crit Care Med. 2011;184(11):1299–304.
O'Connor GT, Caffo B, Newman AB, Quan SF, Rapoport DM, Redline S, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179(12):1159–64.
Lloberes P, Sampol G, Espinel E, Segarra A, Ramon MA, Romero O, et al. A randomized controlled study of CPAP effect on plasma aldosterone concentration in patients with resistant hypertension and obstructive sleep apnea. J Hypertens. 2014;32(8):1650–7 discussion 7.
Narkiewicz K, Kato M, Phillips BG, Pesek CA, Davison DE, Somers VK. Nocturnal continuous positive airway pressure decreases daytime sympathetic traffic in obstructive sleep apnea. Circulation. 1999;100(23):2332–5.
Marin JM, Agusti A, Villar I, Forner M, Nieto D, Carrizo SJ, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307(20):2169–76.
Bratton DJ, Stradling JR, Barbe F, Kohler M. Effect of CPAP on blood pressure in patients with minimally symptomatic obstructive sleep apnoea: a meta-analysis using individual patient data from four randomised controlled trials. Thorax. 2014;69(12):1128–35.
Navarro-Soriano C, Martinez-Garcia MA, Torres G, Barbe F, Caballero-Eraso C, Lloberes P, et al. Effect of continuous positive airway pressure in patients with true refractory hypertension and sleep apnea: a post-hoc intention-to-treat analysis of the HIPARCO randomized clinical trial. J Hypertens. 2019;37(6):1269–75.
Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359(9302):204–10.
Campos-Rodriguez F, Grilo-Reina A, Perez-Ronchel J, Merino-Sanchez M, Gonzalez-Benitez MA, Beltran-Robles M, et al. Effect of continuous positive airway pressure on ambulatory BP in patients with sleep apnea and hypertension: a placebo-controlled trial. Chest. 2006;129(6):1459–67.
Muxfeldt ES, Margallo V, Costa LM, Guimaraes G, Cavalcante AH, Azevedo JC, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension. 2015;65(4):736–42.
Robinson GV, Smith DM, Langford BA, Davies RJ, Stradling JR. Continuous positive airway pressure does not reduce blood pressure in nonsleepy hypertensive OSA patients. Eur Respir J. 2006;27(6):1229–35.
Barbe F, Duran-Cantolla J, Sanchez-de-la-Torre M, Martinez-Alonso M, Carmona C, Barcelo A, et al. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: a randomized controlled trial. JAMA. 2012;307(20):2161–8.
Pepin JL, Tamisier R, Barone-Rochette G, Launois SH, Levy P, Baguet JP. Comparison of continuous positive airway pressure and valsartan in hypertensive patients with sleep apnea. Am J Respir Crit Care Med. 2010;182(7):954–60.
Roche F, Pepin JL, Achour-Crawford E, Tamisier R, Pichot V, Celle S, et al. At 68 years, unrecognised sleep apnoea is associated with elevated ambulatory blood pressure. Eur Respir J. 2012;40(3):649–56.
Guillot M, Sforza E, Achour-Crawford E, Maudoux D, Saint-Martin M, Barthelemy JC, et al. Association between severe obstructive sleep apnea and incident arterial hypertension in the older people population. Sleep Med. 2013;14(9):838–42.
Monneret D, Barthelemy JC, Hupin D, Maudoux D, Celle S, Sforza E, et al. Serum lipid profile, sleep-disordered breathing and blood pressure in the elderly: a 10-year follow-up of the PROOF-SYNAPSE cohort. Sleep Med. 2017;39:14–22.
Sforza E, Chouchou F, Collet P, Pichot V, Barthelemy JC, Roche F. Sex differences in obstructive sleep apnoea in an elderly French population. Eur Respir J. 2011;37(5):1137–43.
Newman AB, Nieto FJ, Guidry U, Lind BK, Redline S, Pickering TG, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol. 2001;154(1):50–9.
Munoz R, Duran-Cantolla J, Martinez-Vila E, Gallego J, Rubio R, Aizpuru F, et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke. 2006;37(9):2317–21.
Catalan-Serra P, Campos-Rodriguez F, Reyes-Nunez N, Selma-Ferrer MJ, Navarro-Soriano C, Ballester-Canelles M, et al. Increased incidence of stroke, but not coronary heart disease, in elderly patients with sleep apnea. Stroke. 2019;50(2):491–4.
Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122(4):352–60.
Campos-Rodriguez F, Martinez-Garcia MA, Reyes-Nunez N, Caballero-Martinez I, Catalan-Serra P, Almeida-Gonzalez CV. Role of sleep apnea and continuous positive airway pressure therapy in the incidence of stroke or coronary heart disease in women. Am J Respir Crit Care Med. 2014;189(12):1544–50.
Wang LJ, Pan LN, Yan RY, Quan WW, Xu ZH. Obstructive sleep apnea increases heart rhythm disorders and worsens subsequent outcomes in elderly patients with subacute myocardial infarction. J Geriatr Cardiol. 2021;18(1):30–8.
Alonderis A, Raskauskiene N, Gelziniene V, Zaliunaite V, Brozaitiene J. Undiagnosed sleep apnoea in cardiac rehabilitation: age-dependent effect on diastolic function in coronary artery disease patients with preserved ejection fraction. Eur J Cardiovasc Nurs. 2020.
Ancoli-Israel S, Kripke DF, Klauber MR, Fell R, Stepnowsky C, Estline E, et al. Morbidity, mortality and sleep-disordered breathing in community dwelling elderly. Sleep. 1996;19(4):277–82.
Lavie P, Lavie L. Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res. 2009;18(4):397–403.
Lavie P, Lavie L, Herer P. All-cause mortality in males with sleep apnoea syndrome: declining mortality rates with age. Eur Respir J. 2005;25(3):514–20.
Lindberg E, Janson C, Svardsudd K, Gislason T, Hetta J, Boman G. Increased mortality among sleepy snorers: a prospective population based study. Thorax. 1998;53(8):631–7.
Punjabi NM, Caffo BS, Goodwin JL, Gottlieb DJ, Newman AB, O'Connor GT, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6(8):e1000132.
Gooneratne NS, Richards KC, Joffe M, Lam RW, Pack F, Staley B, et al. Sleep disordered breathing with excessive daytime sleepiness is a risk factor for mortality in older adults. Sleep. 2011;34(4):435–42.
Campos-Rodriguez F, Martinez-Garcia MA, Reyes-Nunez N, Selma-Ferrer MJ, Punjabi NM, Farre R. Impact of different hypopnea definitions on obstructive sleep apnea severity and cardiovascular mortality risk in women and elderly individuals. Sleep Med. 2016;27-28:54–8.
Wickwire EM, Bailey MD, Somers VK, Srivastava MC, Scharf SM, Johnson AM, et al. CPAP adherence is associated with reduced risk for stroke among older adult Medicare beneficiaries with obstructive sleep apnea. J Clin Sleep Med. 2021.
Martinez-Garcia MA, Soler-Cataluna JJ, Ejarque-Martinez L, Soriano Y, Roman-Sanchez P, Illa FB, et al. Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med. 2009;180(1):36–41.
Lopez-Padilla D, Alonso-Moralejo R, Martinez-Garcia MA, De la Torre CS. Diaz de Atauri MJ. Continuous positive airway pressure and survival of very elderly persons with moderate to severe obstructive sleep apnea. Sleep Med. 2016;19:23–9.
Ou Q, Chen YC, Zhuo SQ, Tian XT, He CH, Lu XL, et al. Continuous positive airway pressure treatment reduces mortality in elderly patients with moderate to severe obstructive severe sleep apnea: a cohort study. PLoS One. 2015;10(6):e0127775.
Dunietz GL, Chervin RD, Burke JF, Braley TJ. Obstructive sleep apnea treatment disparities among older adults with neurological disorders. Sleep Health. 2020;6(4):534–40.
Martinez-Garcia MA, Valero-Sanchez I, Reyes-Nunez N, Oscullo G, Garcia-Ortega A, Gomez-Olivas JD, et al. Continuous positive airway pressure adherence declines with age in elderly obstructive sleep apnoea patients. ERJ Open Res. 2019;5(1).
Kim Y, Koo YS, Lee HY, Lee SY. Can continuous positive airway pressure reduce the risk of stroke in obstructive sleep apnea patients? A systematic review and meta-analysis. PLoS One. 2016;11(1):e0146317.
Edwards BA, Redline S, Sands SA, Owens RL. More than the sum of the respiratory events: personalized medicine approaches for obstructive sleep apnea. Am J Respir Crit Care Med. 2019;200(6):691–703.
Funding
VA ORD (1IK2CX001026-01)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any conflict of interest.
Disclaimer
The findings reported in this article do not communicate the official position of the Veterans Affairs Office of Research and Development.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep Apnea in the Golden Age
Rights and permissions
About this article
Cite this article
Imayama, I., Sahni, A., Sunkara, S. et al. Sleep Apnea and Hypertension in the Elderly. Curr Sleep Medicine Rep 7, 80–86 (2021). https://doi.org/10.1007/s40675-021-00211-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-021-00211-4