Abstract
Purpose of Review
Power outages, a common and underappreciated consequence of natural disasters, are increasing in number and severity due to climate change and aging electricity grids. This narrative review synthesizes the literature on power outages and health in communities.
Recent Findings
We searched Google Scholar and PubMed for English language studies with titles or abstracts containing “power outage” or “blackout.” We limited papers to those that explicitly mentioned power outages or blackouts as the exposure of interest for health outcomes among individuals living in the community. We also used the reference list of these studies to identify additional studies. The final sample included 50 articles published between 2004 and 2020, with 17 (34%) appearing between 2016 and 2020. Exposure assessment remains basic and inconsistent, with 43 (86%) of studies evaluating single, large-scale power outages. Few studies used spatial and temporal control groups to assess changes in health outcomes attributable to power outages. Recent research linked data from electricity providers on power outages in space and time and included factors such as number of customers affected and duration to estimate exposure.
Summary
The existing literature suggests that power outages have important health consequences ranging from carbon monoxide poisoning, temperature-related illness, gastrointestinal illness, and mortality to all-cause, cardiovascular, respiratory, and renal disease hospitalizations, especially for individuals relying on electricity-dependent medical equipment. Nonetheless the studies are limited, and more work is needed to better define and capture the relevant exposures and outcomes. Studies should consider modifying factors such as socioeconomic and other vulnerabilities as well as how community resiliency can minimize the adverse impacts of widespread major power outages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In August 2003, over 50 million Americans and Canadians lost power for up to 4 days due to a surge of electricity along faulty transmission lines [1]. In China, ice-coated transmission lines and towers collapsed during a severe winter storm in 2008, interrupting electric service to 200 million people [2]. Meanwhile, hot weather and related air conditioner use triggered a blackout affecting 8 million people in Baku, Azerbaijan, in July 2018 [1]. The largest blackout in history affected at least 600 million people across India in July 2012 [3]. The frequency and severity of these events will increase with population growth and climate change, as infrastructure damage from intense storms and floods, hydropower shortage from droughts, and increased demand as temperatures rise and strain an aging electricity grid [4,5,6].
Power Outages Worldwide
Today, South Asia has the highest system average interruption frequency index (SAIFI). The average business there experienced 26 outages per month in 2019 [7]. However, even businesses in Organisation for Economic Co-operation and Development (OECD) countries experienced one power outage every other month in 2019. Outages last longest, on average, in Latin America and the Caribbean (8 h) and Sub-Saharan Africa (7.5 h), compared to just 2.5 h in East Asia [8]. The US Energy Information Administration predicts that global electricity production will increase by 75%, from 20 trillion kilowatt-hours (kWh) in 2018 to 45 trillion kWh in 2050, driven in large part by demand in non-OECD countries [9]. This increased demand will result in more power outages, with unique economic, social, and health consequences, of which we review that latter.
Causes and Costs of US Power Outages
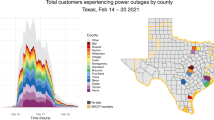
In the USA, major power outages increased 10-fold between 1984 and 2012 with the average household experiencing 470 min without power in 2017 [11, 12]. Large blackouts, disturbances that interrupt more than 300 MW (enough power for ~50,000 homes) or 50,000 customers and require reporting to the US Department of Energy [13], occur more commonly in the winter and summer and year-round during the mid-afternoon [14]. Electromagnetic events and intentional cyber-physical attacks caused > 25% of the total US power outages between 2000 and 2016 (Fig. 1a) [10, 15]. Such attacks present substantial risk to the electricity grid and could result in an outage that stretches for months across wide geographies, especially if timed after a natural disaster [16]. Most widespread power outages were caused by severe weather (Fig. 1b) and Florida, California, New York, and Michigan were hit hardest with 25.3 million, 22.2 million, 18.3 million, and 12.4 million affected customers, respectively [15].
Summary of large power outages in the USA from 2000 to 2016. a Number of large power outages by cause between 2000 and 2016. b Count of outages by primary cause type by state between 2000 and 2016. For example, Texas had 65 power outages caused by severe weather between 2000 and 2016. Data from Mukherjee et al. 2018 [10], which they assembled from publicly-available datasets. A large power outage is defined by the US Department of Energy as 50,000+ customers affected or an unplanned loss of 300 MW
Outages, particularly those related to weather, are almost always accompanied by intersecting and related phenomena that result in economic, social, and health damages (Fig. 2). Economically, they interrupt business, cripple the internet, and halt many forms of transportation [8]. The 2003 Northeast Blackout in Canada and the USA cost between $4 and 10 billion [17], and electricity infrastructure repairs alone cost $3.5 billion after Hurricane Sandy [18]. Social costs include increased crime, motor vehicle crashes, psychosocial stress, and interrupted communication between emergency services, delivery of clean water, and waste removal [3, 12, 19, 20•]. Although, altruistic acts, including providing assistance to others, donating money, assisting with traffic, may also increase during power outages [19, 20•, 21, 22]. Several factors influence the severity of economic, social, and health costs of power outages including outage frequency, duration, timing, and geographic range, as well as mitigation measures, population preparedness, and prior experience [19, 23].
Schematic showing hypothesized pathways between power outages and disease exacerbation. We illustrate co-occurring factors such as displacement, extreme temperatures, and air pollution, as well as vulnerability factors that might increase the risk of adverse health outcomes during power outages, including baseline health status, socioeconomic status, and social support
Medically High-Risk Groups During Power Outages
Certain subgroups have higher risk of adverse health outcomes during power outages. These include older adults; those reliant on electricity-dependent durable medical equipment (DME, e.g., oxygen concentrators); those unable to evacuate, including nursing home patients; those reliant on others to complete activities of daily living; the heat/cold susceptible; and those with underlying conditions exacerbated by the inciting events, such as respiratory, cardiovascular, and renal disease [23,24,25]. The number of electricity-dependent individuals is anticipated to grow in the coming years [23, 25]; numbers already trend upward, and rate of DME use appears higher among lower socioeconomic status individuals [26].
Documented Disparities in Power Outage Preparedness and Exposure
Evidence from the USA suggests older adults, poorer families, and individuals of non-Hispanic Black and Hispanic race/ethnicity are least likely to have a 3-day supply of food, drinking water, and medication, a preparedness measure for power outages [27,28,29]. In New York City, only 58% of 887 people surveyed were prepared for a disaster; preparedness dipped to 45% among households with income < $30,000 and to 28% among primary Spanish-speakers [29]. Generator cost ($2–5000) may price out lower socioeconomic status families and those living in public housing or apartment buildings that prohibit generators [21, 29]. Finally, power outages may last longer in lower socioeconomic status or communities of color [30••, 31,32,33,34], where impacts may already be greater. For example, in Florida after Hurricane Irma, higher income individuals evacuated farther and to destinations with lower power outage rates compared to their lower income counterparts [33]. After Hurricane Maria, satellite imagery of Puerto Rico suggested that households with power restored in stage 1 earned almost double the income of households with power restored in stages 2–3 [32]. After Hurricane Sandy in New Jersey, non-Hispanic White individuals had the longest duration outages (11.2 days compared to 8.2 days for African Americans) [34]. Such disparities put these already-vulnerable groups at increased risk of adverse power outage-related health outcomes.
Goal of this Review
This review focuses on blackouts—the unavailability of electric power in an area—and does not address issues of energy poverty, a separate and important predictor of health [35, 36]. In addition, we do not cover challenges faced by healthcare facilities during power outages. In this narrative review, we highlight themes in the current scholarship on power outages and community health and identify future avenues for research.
Methods
We conducted searches via Google Scholar and PubMed in spring 2020 for studies written in English with titles or abstracts containing “power outage” or “blackout.” We limited papers to those that explicitly mentioned power outages or blackouts as the exposure of interest for health outcomes among individuals living in the community. The reference lists of the identified studies were also examined to identify additional relevant articles. We screened the articles to include only original primary research published between January 2004 and June 2020 that explicitly mentioned power outage or blackout as an exposure of interest. The final sample included 50 articles spanning power outage events from 1977 to 2019 (Fig. 3). The majority (72%) of the studies evaluated health outcomes in the USA, but we collected literature from across the globe (Appendix Fig. 1). Non-US articles tended to focus on interrupted healthcare [37, 38], which was outside the scope of this review.
Timeline of the power outages evaluated by the epidemiologic literature between 2004 and 2020. Dashed outlines represent outages caused by technological failure and solid outlines those caused by severe weather. Numbers in square brackets denote the number of studies evaluating the specific outage and fill colors get closer to red with more studies evaluating the outage
Exposure Assessment
Single, Large-Scale Power Outages
Nearly all studies evaluated single, large-scale power outages. While the definition of large scale varied from study to study, many met the US Department of Energy criteria: 50,000+ customers affected or an unplanned loss of 300 MW [13]. Researchers assumed individuals experienced the outage if they lived or attended a healthcare facility in the region where the outage occurred. Most studies relied on pre-post outage temporal comparisons to draw inference [20•, 28, 39,40,41,42,43,44,45,46,47,48,49,50,51, 52•, 53] or only described health outcomes after the outage [54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71] (Fig. 4). Eight studies of single outages also incorporated geographic variability in outage distribution in the study design, in addition to using pre-post outage health measures [ 72,73,74,75, 76•, 77, 78, 79••].
Exposure definition and analytic comparison groups used in 50 reviewed epidemiologic studies, 2004–2020. Most studies evaluated a single outage by describing outcomes after the event among the exposed population (single outage, no temporal comparison). Eight studies evaluated a single outage but used both spatial and temporal comparison groups to make inference (single outage, temporal + spatial comparison). Three studies used measures of long-term exposure from multiple outages to assign levels of power outage exposure to the study population (multiple outages, measure of long-term exposure)
Multiple Power Outages
Seven studies evaluated multiple power outages [30••, 80••, 81••, 82, 83•, 84, 85 ], with three using outage frequency to characterize long-term exposure [82, 84, 85]. Others conducted longitudinal analyses. In South Africa, Gehringer and colleagues used a combination of government data, Facebook, and the local electric utility’s Twitter handle to track daily load shedding events (halted electricity distribution due to demand exceeding supply), including outage duration [30••]. Koroglu used standard electricity reliability data from the Maharashtra State Electricity Distribution Company in India to characterize monthly SAIFI and system average interruption duration indices (SAIDI) values statewide [83•]. Zhang and colleagues linked power outage records, including total number of customers affected, from the New York State Department of Public Service (NYSPS) between 2001 and 2013 to the power-operating division level (~ 1700 divisions exist in New York with an average population of ~ 11,000 people each). They created daily exposure metrics based on proportion of customers affected and duration (in days) of power outages. Likewise, Dominianni et al. used half-hourly NYSPS data to identify outages within each of New York City’s (NYC) 66 electricity grid networks [80••]. They defined the entire grid network area as exposed on a given day if > 1000 people were without power during the warm season and if > 75 people were without power during the cold season. Different cutpoints were used because fewer people experienced outages during the cold season.
Outcomes
Carbon Monoxide Poisoning
Twenty-three (48%) of studies included evaluated carbon monoxide (CO) poisoning [44, 45, 50, 51, 54, 55, 57,58,59,60,61,62, 64,65,66, 69,70,71,72, 76•, 77, 85, 86], a topic previously reviewed [87,88,89]. CO is a colorless, odorless, and tasteless gas, formed by incomplete combustion of carbon compounds. Because hemoglobin binds 250× more readily with CO than with oxygen, prolonged exposure leads to cellular hypoxia, ischemia, and death [90].
In the 23 reviewed articles, indoor use of charcoal and gasoline-powered generators caused the majority of CO poisonings. The most common symptoms of CO poisoning were headache, nausea, vomiting, dizziness, loss of consciousness, and death. The majority of studies identified CO poisoning using medical chart reviews including emergency department (ED) visits [50, 54, 55, 57, 60, 64,65,66, 69,70,71,72, 77], hospitalizations [58, 69,70,71, 76•], and emergency medical service (EMS) and poison control calls [28, 44, 45, 58, 59, 65, 69, 72] coded as CO poisoning-related; several studies used laboratory confirmation or reported serum carboxyhemoglobin (COHb) levels [44, 54, 55, 59,60,61, 64, 70, 91]. Many studies reported fatalities, particularly in the several days following storms [54, 55, 57, 59,60,61,62, 65, 69,70,71, 85]. Over 50% of CO poisoning studies reported the use of hyperbaric oxygen therapy [44, 54, 55, 58, 59, 61, 64, 65, 69,70,71,72, 91], and higher COHb levels may be related to persistent cognitive and psychiatric changes after CO poisoning [91]. In many cases, children [54, 55, 59, 72], older adults [61, 62, 65], immigrants [60, 65], and people of color [55, 60, 64, 65, 70] were disproportionately affected. Qualitative methods can provide key insights not otherwise captured. For example, Styles and colleagues also found that 62% of non-Hispanic White generator/charcoal grill/heater operators reported hearing warnings about CO poisoning in the year prior compared to just 30% of those in other racial/ethnic groups [70], and Van Sickle et al. determined fear of theft was the most common reason to place a generator indoors [71].
While most studies only catalogued CO poisoning events following power outages, a few employed a comparison time period [28, 45, 50, 72, 76•, 77], allowing authors to determine if more CO poisoning occurred than expected following power outages. After the Great East Japan Earthquake of 2011, Nakajima and colleagues found 13.5× the odds of CO poisoning among patients in the disaster area (including power outage exposure) from March 11 to April 9, 2011, compared to the same dates in 2012 [76•]. A spatial control also revealed higher counts of CO poisoning in the disaster area versus an unexposed region. Johnson-Arbor compared two major storms in Connecticut in 2011 and 2013, where the 2011 storm resulted in 11× the number of individuals losing power and 5× the number of CO poisonings [44].
All-Cause, Cardiovascular, Respiratory, and Renal Disease Healthcare Visits
In general, hospitals see fewer patients in the days leading up to storms [42], whereas more patients arrive during and after outages, often with respiratory, cardiovascular, or renal disease exacerbations [30, 40, 42, 46, 47, 53, 68, 80••, 81••]. In a comprehensive study, Dominianni et al. evaluated three major NYC outages (1999, 2003, 2006) and localized warm- and cold-weather outages within NYC [80••]. In models accounting for temperature, day of week, and seasonal and long-term trends, they confirmed prior findings of increased cardiovascular and respiratory disease hospitalizations during the 2003 outage and found new evidence of elevated risk of renal disease hospitalizations during warm-season power outages and cardiovascular disease hospitalizations during cold-season power outages. Zhang and colleagues also illustrated the utility of using daily sub-city level power outage data in their study of chronic obstructive pulmonary disease (COPD) hospitalizations statewide. They used power-operating division level (~ 11,000 residents per division) between 2001 and 2013 in New York and found the largest increases in COPD hospitalizations during the first 3 days after power outages, where 23% of COPD hospitalizations on power outages days could be attributed to the outage itself [81••]. Compared to non-power outage periods, COPD patients arriving for care during power outages had a higher number of comorbidities and healthcare costs. Interrupted use of nebulizers and oxygen and bilevel positive airway pressure machines, as well as sensitivity of COPD patients to changing indoor conditions (e.g., lack of air conditioning or dehumidifiers) likely explained the large increase in hospitalizations.
Many acute care visits related to cardiovascular and respiratory disease exacerbation during blackouts appear to result from failure of electricity-dependent medical devices [41, 42, 46, 50, 51, 63, 67, 68, 80••, 81••, 92]. For example, after the 2011 Great East Japan Earthquake, 75% of 24 new pediatric inpatients at Tohoku University Hospital relied on DME, including 13 children using ventilators [76•]. After Hurricane Sandy, ED visits at Beth Israel Medical Center related to respiratory device failure and “power outage” increased in all age groups and peaked the day following the disaster [41].
Older adults and children may be at particular risk during power outages. Unlike many other NYC hospitals in downtown Manhattan, Beth Israel Medical Center remained open after Hurricane Sandy, and their electronic health record (EHR) data revealed a 114% increase in ED use among patients aged 80+ and a 11% decline among those aged 18–64 compared to the 6 months prior [41]. In addition to power outage-related care, this increase reflects spillover from other closed hospitals. In South Africa, Gehringer and colleagues evaluated repeated, daily, temporary outages on pediatric hospital admissions, finding an average treatment effect of 6 additional admissions per day due to any power outage in the 2 days prior [30]. They found the largest effect sizes for respiratory outcomes, burns, and ear, eye, and gastrointestinal system outcomes in models that controlled for important factors like weather and seasonal and long-term trends.
Gastrointestinal Illness
Power outages can affect food refrigeration and water system supply and disinfection, potentially precipitating gastrointestinal illness as measured via poison control calls, prescription orders, and hospital admissions [30••, 45, 48, 78]. However, evidence is mixed, with several studies finding no increase in gastrointestinal illness after power outages [72, 78, 86]. Marx et al. employed methods from digital epidemiology to evaluate diarrheal illness after the 2003 Northeast Blackout finding that diarrheal syndrome ED visits, antidiarrheal medication sales, electrolyte sales, and worker absenteeism due to gastrointestinal illness all increased above expected in the days following the blackout [48].
Temperature-Related Illness
Power outages reduce individuals’ ability to control the indoor environment and may coincide with temperature extremes (both heatwaves and winter storms) resulting in illness [40, 42, 51, 53, 55, 68, 77, 80••] and disturbed sleep [49] related to heat and cold exposure. Racial, socioeconomic, and age disparities exist in response to extreme temperature exposures, owing to differences including baseline health, access to generators, the urban heat island effect, and occupation [93, 94].
Maternal and Neonatal Health
Four studies assessed the relationship between power outages and maternal healthcare utilization, measures of fertility, and birthweight [73, 74, 79••, 83•]. Using monthly power outage data from 2010 to 2015 in India’s Maharashtra state, Koroglu and colleagues evaluated the relationship between SAIFI (system average interruption frequency index) and SAIDI (duration) metrics and use of maternal health services [83•]. Increased monthly SAIFI but not SAIDI was associated with reduced odds of delivering in a healthcare institution (versus at home), both indices were associated with reduced odds of attendance of birth by skilled professional, and neither were related to cesarean section delivery. Outages may affect a woman’s ability to travel to a healthcare facility or reduce her perception of the quality of care she will receive there, encouraging her to stay at home.
Burlando exploited a month-long 2008 blackout that occurred on the island of Zanzibar, Tanzania, to study both measures of fertility (counts of live births) and birth weight [73, 74]. The outage caused both a transitory negative income shock, with those who used electricity at work reporting a decrease in earnings and hours worked, and individuals to spend more time at home. With data from the island’s main maternity hospital (500–900 births per month), Burlando used a difference-in-differences strategy to estimate the effect of the power outage on fertility and birthweight by comparing outcomes among mothers living in shehias (communities) with and without any electrification exposed and unexposed to the blackout at different times during pregnancy. They found that the blackout was associated with a 17% increase in live births (253 additional births) 8–10 months later [73]. The outage also appeared to reduce birthweights 7–10 months later, with the strongest associations among the lowest-percentile weights (e.g., 8th-percentile weight was reduced by 2 kg) [74].
Mental Health and Wellbeing
Qualitative studies identified worry, anxiety, stress, and reduced wellbeing among individuals exposed to power outages, generally tied to concerns about disrupted heating, food, water supplies, and healthcare [75, 82]. In the acute setting, healthcare seeking for mental health problems may actually decline, as was seen immediately after the 2003 Northeast Blackout in NYC [40]. Therefore, alternative data, such as Twitter, may supply valuable information about population health during an outage [20•]. Li et al. found a sharp drop in Twitter sentiment (i.e., more negative tweets) in the first hour of a NYC power outage in 2019. Other studies have evaluated longer term effects of power outages [56, 79••, 84] In Ghana, university students who experienced power outages ≥ 4 times per week had significantly higher levels of anxiety as measured by the generalized anxiety disorder 7-item scale [84]. After Hurricane Sandy, ED visits for mental health problems among pregnant women in New York increased gradually and peaked 8 months later at a level 33% higher than expected based on data from prior and subsequent years [79••].
Mortality
Three studies identified increased mortality after the 2003 Northeast Blackout in New York City (NYC), which affected 8 million NYC residents [39, 47, 80••]. Anderson and Bell found increased accidental (+ 122%) and non-accidental (+ 25%) mortality controlling for important environmental confounding variables such as temperature, air pollutants, day-of-week, and seasonal and long-term trends [39]. Dominianni and colleagues extended Anderson and Bell’s study to span major NYC blackouts in 1999, 2003, and 2006, as well as localized outages in 66 NYC electric-grid networks [80••], finding significant associations between localized cold weather, but not warm weather, outages, and all-cause and non-external mortality. Conversely, Imperato could not identify an effect of the 1977 NYC power outage on all-cause mortality as it coincided with and could not be disentangled from a heatwave [43]. Other studies have tied power outage-related mortality to CO poisoning (see prior section), falls [55, 62], fire [55, 62], heat [85], and cold exposure [55].
Other Outcomes
Several studies reported increases in healthcare visits for burns, lacerations, or other injuries [40, 42, 50, 68, 77], but attributing these events to power outages, rather than co-occurring exposures such as housing damage or motor vehicle crashes has been difficult. Further, two studies reported reduced prescription refills during power outages [42, 52•], and one found no change [50]. After Hurricane Maria, power outages lasted months in Puerto Rico, and prescription refills did not revert to normal levels even 1 year later [52•].
Review Summary and Recommendations
Recent studies point to a relationship between power outages and adverse health outcomes among community residents. Most have assessed single, large-scale power outages without linking events directly to patient residential addresses. New York has used data from electric utilities [80••, 81••, 83•] and social media [30••] to more accurately capture the temporal and spatial extent of outages. Consistent evidence from > 20 studies across a range of power outages from hurricanes to ice storms to earthquakes finds increased rates of CO poisoning during outages as individuals use alternative fuel sources, such a generators and charcoal. We also observed moderate evidence for an association between power outages and all-cause, cardiovascular, respiratory, and renal disease hospitalizations, except for the sub-group of individuals relying on electricity-dependent medical equipment where associations consistently pointed to elevated risk. In times and places where power outages corresponded to hot or cold ambient temperatures, we found moderate evidence of a relationship between power outage and temperature-related illness, gastrointestinal illness, and mortality. Recent studies have broadened their scope to consider additional outcomes such as mental health [19], maternal and child health [73, 74, 83•], prescription refills [42, 52•], and injuries [40, 42, 50, 68, 77]; future work should continue to explore these and other potentially important outcomes (Table 1).
Future Areas for Exposure Assessment
To date, most studies have focused on single power outages, which can allow better characterization of co-exposures but misses the larger burden of repeated outages and underestimates individual-level effects. Studies should consider factors such as duration (e.g., longer outages are likely much worse for health) and location (e.g., outages in San Diego likely have fewer impacts than outages in Maine in the winter). The lack of resolved spatial and temporal exposure data has also limited research. Attribution of adverse health outcomes directly to power outages will require exploiting variability in power outage locations, times, duration, and severity among populations. Zhang et al. successfully did this using NYSPS data [81••]. Such data are difficult to acquire and do not exist for many regions of the USA and the world. Therefore, borrowing from digital epidemiology [95], alternative strategies may be used, including remote sensing, internet-connected devices, and social media, to characterize spatiotemporal variability in power outages.
Remote Sensing
Researchers can use satellite or aircraft to measure reflected and emitted radiation of the earth. In particular, remote sensing of artificial lights at night [96] can be used to measure power outages [97]. In India, Min et al. created a Power Supply Irregularity (PSI) index using nighttime satellite imagery to compute the outage index in all 600,000 villages in India from 1993 to 2013 [97]. Likewise, Román et al. used globally available, daily nighttime light data from NASA’s Black Marble product to track electricity grid restoration in Puerto Rico after Hurricane Maria [32]. These data were used to create three metrics down to 902 barrios: [1] percent recovery; [2] number of days without electricity; and [3] number of customer-hours of interruption.
Internet Connected and Other Consumer Devices
Meier et al. used the power status of internet-connected thermostats, of which 6 million exist in the USA, to track outages at 15-min intervals during Hurricane Irma and severe windstorm [98]. Others have proposed using smartphones [99] or a host of internet-connected devices (e.g., alarm systems, ATM networks) to track power outages [100].
Social Media
Several researchers have used Twitter feeds to track power outages [20•, 101,104,105,104]. One option is to use geotagged tweets [101], but these make up < 1% of tweets as most users turn this function off [105]. Instead, researchers can search for location-specific terms within tweets, for example, “New York City” or obtain information from registered locations from the users’ accounts [20•, 104]. Khan et al. also attempted to extract power outage cause in four groups: manmade, natural (e.g., “storm”), wildlife, and faulty equipment [104]. This type of data may have increased utility in the future.
Co-exposures/Complex Disasters
One key and complicating feature of power outages is that they often occur alongside other disasters. Disentangling the impact of power outages from other physical destruction of infrastructure, such as landslides in Puerto Rico following Hurricane Maria [106, 107], fuel crises in Nepal after the 2015 earthquake [108], or windstorms in Ohio following Hurricane Ike [109] may not be possible. Bromet et al. noted a synergistic effect of multiple Sandy-related exposures, where participants experiencing 3–5 exposures (i.e., loss of power, extreme concern about finding gasoline, filing a FEMA claim, extensive home damage, and extensive possession damage) had > 6× the odds of PTSD and major depressive disorder compared to those experiencing 0 exposure [56]. Many studies implicitly include power outage as an exposure, but the researchers do not explicitly cite power outage as the main exposure of interest. Future work should consider the long-tail, ancillary impact of power outage-related health effects. Sustained power outages result in delayed or interrupted access to healthcare from infrastructure damage, access limitations, inability to pay (from disaster-related impoverishment), and loss of personnel [34, 83•, 110]. Such deferred care, from delayed treatments, unfilled prescriptions, or failure of DMEs impacts morbidity and mortality—as was in the case after Hurricane Maria in Puerto Rico, where nearly 4000 excess deaths occurred [111].
Future Areas for Outcome Assessment
Outcome assessment should increase in depth and breadth. Most studies only evaluated immediate effects of power outages. Future studies should expand the timescale to assess outcomes in the short-term and long-term. For example, Xiao et al. defined immediate impacts of Hurricane Sandy as the 30 days after and long-term impacts over the following year [79••]. They found immediate and long-term increases in ED visits for overall pregnancy complications among women in eight Sandy-exposed New York counties that exceeded increases in 54 less-exposed counties, highlighting the need to extend the relevant follow-up period. While studies have begun to assess perinatal health, future work should also consider children, another susceptible group. Additionally, studies must continue to evaluate the health of older adults, who rely more heavily on electricity-dependent medical equipment [26] and may have cognitive impairment or functional limitations [112], increasing their vulnerability to power outages.
The use of large insurance claims databases or EHRs [113], combined with better exposure assessment, will allow for investigating the impact of power outages on health in at least three important ways. First, it will allow for assessing a larger variety of health outcomes over a longer period of time. Many outcomes, such as maternal and child health or mental health, are known to be sensitive to power outages yet remained understudied. In addition to these outcomes, exploratory analyses of large claims databases may identify currently unknown outcomes impacted by power outages. Second, it will allow for identifying and studying particularly susceptible subpopulations, such as patients with temperature-sensitive comorbidities like multiple sclerosis or heart failure. Lastly, it will allow for a more complete description of the racial/ethnic, socioeconomic, and spatially patterned disparities in health response to power outages. Very few studies to date employ spatial and temporal control groups, rigorous statistical methods, and assess for effect modification by import socioeconomic and racial/ethnic sub-groups. This work can assist in identifying crucial points of intervention to allow for equitable allocation of preparedness, response and recovery activities, and resources to reduce disparities.
Building Resilience and Supporting Response
Resiliency spans from the individual to regional and global levels and encompasses individual skills, community health, and societal resources [114].
Preparedness
Individual and community preparedness, including access to alternative power sources, can influence the scope of effect of outages on population health. While baseline levels of individual preparedness appear low, a silver lining of repeated outages is that households become more prepared, buying additional supplies or equipment, over time [19]. In Florida, CO poisoning counts increased after the first, but not the second or third consecutive hurricanes, suggesting increased awareness, preparedness, or public health warnings during subsequent hurricanes of the season [50]. Personal preparedness can reduce the effect of power outages on health, but low socioeconomic status individuals have limited capacity to store food and water or own a generator [29], and marginalized groups may receive fewer disaster-related warnings [70]. Instead, emergency planners should focus on bolstering community resilience—physical, economic, and social—which can take many forms, from strengthening infrastructure to reducing baseline environmental exposure levels and socioeconomic inequities to expanding social capacities [21, 75]. Resilient communities deploy collective strategies such as community kitchens, checking on older adults, and providing each other with warmth, food, and shelter during outages [19, 115]. Government officials and utilities can further support health and safety by providing advanced warning of power outages as well as estimated duration once the outage has begun.
Electricity Infrastructure
Several steps can be taken to improve electricity grid resiliency and response. These might include better protection against cyber-attacks and tree maintenance [1, 16, 116], improved weather forecasting that allows utilities to prepare, decentralized power generation such as solar and battery storage [117, 118], smart grid technologies like advanced metering infrastructure and isolation, and service restoration to update and enhance grid reliability [1, 15]. Rather than increase access to generators, modest system upgrades could also allow for low-amperage service (e.g., 20A, which would keep lights or air conditioning on) during outages, possibly paid for via monthly backup insurance payments of < $1 per customer [119].
Supporting Health During Outages
In addition to primary prevention and building resilience, some specific actions can directly support power outage-related health maintenance, for example, notifying patients pre-disaster to refill prescriptions. Prior to a mid-Atlantic blizzard CVS pharmacy randomly notified 2.2 million patients to check their medication supply and found that they had a 9% increased odds of a refill within 48 h compared to the comparison group [120]. Pre-dialysis and other forms of pre-care at healthcare facilities can allow individuals to go safely without power for longer [121]. We also must further identify locations and comorbidities among those reliant on electricity-dependent medical equipment via patient registration with utility companies and information from EHRs or publicly available data sources like the emPOWER mapping tool [25, 26, 122] and provide community-based charging stations for medical equipment. In North Carolina, > 95% of severe CO poisoning after an ice storm occurred in households without CO detectors [123]. The benefit-to-cost ratio of installing a CO monitor may be as high as 7.2 to 1 [124]. Low-tech interventions, like paired CO monitor and generator purchases, or engineering controls like automatic generator shutoffs, low CO generators, or simply longer generator cords could reduce CO poisoning [125]. Finally, in low-resource settings where outages can limit ability to travel to hospitals or results in blackouts at hospitals themselves, mobile clinics can offer distributed access to care [126], and novel technologies, like solar and storage or oxygen reservoir systems, can support further continuity of care [127, 128].
Conclusion
As power outages increase in frequency and duration, researchers must expand efforts to understand their impact on individual and population health, refining methods of exposure assessment with attention to varied and disparate outcomes. There is urgent need for these data to inform disaster mitigation, preparedness, and response policies (and budgets) in an increasingly energy-reliant world.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Haes Alhelou H, Hamedani-Golshan ME, Njenda TC, Siano P. A survey on power system blackout and cascading events: research motivations and challenges. Energies. 2019;12(4):682.
Küfeoğlu S, Prittinen S, Lehtonen M. A summary of the recent extreme weather events and their impacts on electricity. Int Rev Electr Eng. 2014;9(4):821–8.
Matthewman S, Byrd H. Blackouts: a sociology of electrical power failure. Social Space (Przestrzeń Społeczna). 2013:31–55.
Auffhammer M, Baylis P, Hausman CH. Climate change is projected to have severe impacts on the frequency and intensity of peak electricity demand across the United States. Proc Natl Acad Sci U S A. 2017;114(8):1886–91.
Horton R, Rosenzweig C, Gornitz V, Bader D, O’Grady M. Climate risk information: climate change scenarios & implications for NYC infrastructure New York City panel on climate change. Ann N Y Acad Sci. 2010;1196(1):147–228.
Pachauri RK, Allen MR, Barros VR, Broome J, Cramer W, Christ R, et al. Climate change 2014: synthesis report. Contribution of Working Groups I, II and III to the fifth assessment report of the Intergovernmental Panel on Climate Change: IPCC; 2014.
The World Bank. Power Outages in Firms in a Typical Month 2020. Available from: https://data.worldbank.org/indicator/IC.ELC.OUTG. Accessed 4 Aug 2020.
Laghari J, Mokhlis H, Bakar A, Mohamad H. Application of computational intelligence techniques for load shedding in power systems: a review. Energy Convers Manag. 2013;75:130–40.
U.S. Energy Information Administration. EIA projects less than a quarter of the world’s electricity generated from coal by 2050. 2020 Available from: https://www.eia.gov/todayinenergy/detail.php?id=42555. Accessed 29 Jul 2020.
Mukherjee S, Nateghi R, Hastak M. Data on major power outage events in the continental. US Data Brief. 2018;19:2079–83.
U.S. Energy Information Administration. Average U.S. electricity customer interruptions totaled nearly 8 hours in 2017. 2018. Available from: https://www.eia.gov/todayinenergy/detail.php?id=37652. Accessed 4 June 2019.
Kenward A, Raja U. Blackout: Extreme weather, climate change, and power outages. Princeton; 2014.
U.S. Department of Energy. OE-417: Electric Emergency Incident and Disturbance Report. Available from: https://www.oe.netl.doe.gov/OE417/. Accessed 10 Aug 2020.
Hines P, Apt J, Talukdar S. Large blackouts in North America: historical trends and policy implications. Energ Policy. 2009;37(12):5249–59.
Eaton. Blackout Tracker United States Annual Report 2018. United States; 2019.
The President’s National Infrastructure Advisory Council. Surviving a catastrophic power outage: how to strengthen the capabilities of the nation 2018. Available from: https://www.cisa.gov/publication/niac-catastrophic-power-outage-study. Accessed 31 Jul 2020.
Eto J. Final report on the August 14, 2003 blackout in the United States and Canada: causes and recommendations. Washington, DC: US-Canada Power System Outage Task Force; 2004.
Aon Benfield. Hurricane Sandy Event Recap Report: Impact Forecasting. Available from: http://thoughtleadership.aonbenfield.com/Documents/20130514_if_hurricane_sandy_event_recap.pdf. Accessed 14 Aug 2020.
Rubin GJ, Rogers MB. Behavioural and psychological responses of the public during a major power outage: a literature review. Int J Disaster Risk Reduct. 2019;101226.
• Li L, Ma Z, Cao T. Leveraging social media data to study the community resilience of New York City to 2019 power outage. Int J Disaster Risk Reduct. 2020:101776 This study illustrated the utility of using Twitter data to track psychosocial stress during and after power outages.
Chakalian PM, Kurtz LC, Hondula DM. After the lights go out: household resilience to electrical grid failure following hurricane Irma. Nat Hazards Rev. 2019;20(4):05019001.
Lemieux F. The impact of a natural disaster on altruistic behaviour and crime. Disasters. 2014;38(3):483–99.
Klinger C, Landeg O, Murray V. Power outages, extreme events and health: a systematic review of the literature from 2011-2012. PLoS Curr. 2014;6.
Bean R, Snow S, Glencross M, Viller S, Horrocks N. Keeping the power on to home medical devices. PLoS One. 2020;15(7):e0235068.
Molinari NA, Chen B, Krishna N, Morris T. Who’s at risk when the power goes out? The at-home electricity-dependent population in the United States, 2012. J Public Health Manag Pract. 2017;23(2):152–9.
Casey JA, Mango M, Mullendore S, Kiang MV, Hernández D, Li BH, et al. Trends from 2008–2018 in electricity-dependent durable medical equipment rentals and sociodemographic disparities. Under Rev. 2020.
Bethel JW, Foreman AN, Burke SC. Disaster preparedness among medically vulnerable populations. Am J Prev Med. 2011;40(2):139–43.
Cox K, Kim B. Race and income disparities in disaster preparedness in old age. J Gerontol Soc Work. 2018;61(7):719–34.
Dominianni C, Ahmed M, Johnson S, Blum M, Ito K, Lane K. Power outage preparedness and concern among vulnerable New York City residents. J Urban Health. 2018;95(5):716–26.
•• Gehringer C, Rode H, Schomaker M. The effect of electrical load shedding on pediatric hospital admissions in South Africa. Epidemiology. 2018;29(6):841–7 Identified power outages using a combination of social media and government data and applied causal inference methods to estimate the public health-relevant average treatment effect.
Liévanos RS, Horne C. Unequal resilience: the duration of electricity outages. Energ Policy. 2017;108:201–11.
Roman MO, Stokes EC, Shrestha R, Wang Z, Schultz L, Carlo EAS, et al. Satellite-based assessment of electricity restoration efforts in Puerto Rico after Hurricane Maria. PLoS One. 2019;14(6):e0218883.
Yabe T, Ukkusuri SV. Effects of income inequality on evacuation, reentry and segregation after disasters. Transp Res D Transp Environ. 2020;82:102260.
Burger J, Gochfeld M, Lacy C. Ethnic differences in risk: experiences, medical needs, and access to care after hurricane Sandy in New Jersey. J Toxicol Environ Health A. 2019;82(2):128–41.
Jessel S, Sawyer S, Hernandez D. Energy, poverty, and health in climate change: a comprehensive review of an emerging literature. Front Public Health. 2019;7:357.
Irwin BR, Hoxha K, Grépin KA. Conceptualising the effect of access to electricity on health in low- and middle-income countries: a systematic review. Glob Public Health. 2020;15(3):452–73.
Adair-Rohani H, Zukor K, Bonjour S, Wilburn S, Kuesel AC, Hebert R, et al. Limited electricity access in health facilities of sub-Saharan Africa: a systematic review of data on electricity access, sources, and reliability. Glob Health Sci Pract. 2013;1(2):249–61.
Chawla S, Kurani S, Wren SM, Stewart B, Burnham G, Kushner A, et al. Electricity and generator availability in LMIC hospitals: improving access to safe surgery. J Surg Res. 2018;223:136–41.
Anderson GB, Bell ML. Lights out: impact of the August 2003 power outage on mortality in New York, NY. Epidemiology. 2012;23(2):189–93.
Freese J, Richmond NJ, Silverman RA, Braun J, Kaufman BJ, Clair J. Impact of a citywide blackout on an urban emergency medical services system. Prehosp Disaster Med. 2006;21(6):372–8.
Gotanda H, Fogel J, Husk G, Levine JM, Peterson M, Baumlin K, et al. Hurricane Sandy: impact on emergency department and hospital utilization by older adults in Lower Manhattan, New York (USA). Prehosp Disaster Med. 2015;30(5):496–502.
Greenstein J, Chacko J, Ardolic B, Berwald N. Impact of Hurricane Sandy on the Staten Island University hospital emergency department. Prehosp Disaster Med. 2016;31(3):335–9.
Imperato PJ. Public health concerns associated with the New York City blackout of 1977. J Community Health. 2016;41(4):707–16.
Johnson-Arbor KK, Quental AS, Li D. A comparison of carbon monoxide exposures after snowstorms and power outages. Am J Prev Med. 2014;46(5):481–6.
Klein KR, Herzog P, Smolinske S, White SR. Demand for poison control center services "surged" during the 2003 blackout. Clin Toxicol. 2007;45(3):248–54.
Kobayashi S, Hanagama M, Yamanda S, Satoh H, Tokuda S, Kobayashi M, et al. Impact of a large-scale natural disaster on patients with chronic obstructive pulmonary disease: the aftermath of the 2011 Great East Japan Earthquake. Respir Investig. 2013;51(1):17–23.
Lin S, Fletcher BA, Luo M, Chinery R, Hwang SA. Health impact in New York City during the northeastern blackout of 2003. Public Health Rep. 2011;126(3):384–93.
Marx MA, Rodriguez CV, Greenko J, Das D, Heffernan R, Karpati AM, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006;96(3):547–53.
Mizuno K, Okamoto-Mizuno K. Actigraphically evaluated sleep on the days surrounding the Great East Japan Earthquake. Nat Hazards. 2014;72(2):969–81.
Platz E, Cooper HP, Silvestri S, Siebert CF. The impact of a series of hurricanes on the visits to two Central Florida emergency departments. J Emerg Med. 2007;33(1):39–46.
Rand DA, Mener DJ, Lerner EB, DeRobertis N. The effect of an 18-hour electrical power outage on an urban emergency medical services system. Prehosp Emerg Care. 2005;9(4):391–7.
• Smith JY, Sow MM. Access to e-prescriptions and related technologies before and after Hurricanes Harvey, Irma, and Maria. Health Aff (Millwood). 2019;38(2):205–11 This retrospective study used a U.S. national health information network that transmits 1.7 billion e-prescriptions annually to assess the relationship between Hurricanes Harvey, Irma, and Maria and changes in provider prescribing activity.
Kearns RD, Wigal MS, Fernandez A, Tucker MA Jr, Zuidgeest GR, Mills MR, et al. The 2012 derecho: emergency medical services and hospital response. Prehosp Disaster Med. 2014;29(5):542–5.
Audin C. Carbon monoxide poisoning following a natural disaster: a report on Hurricane Rita. J Emerg Nurs. 2006;32(5):409–11.
Broder J, Mehrotra A, Tintinalli J. Injuries from the 2002 North Carolina ice storm, and strategies for prevention. Injury. 2005;36(1):21–6.
Bromet EJ, Clouston S, Gonzalez A, Kotov R, Guerrera KM, Luft BJ. Hurricane Sandy exposure and the mental health of World Trade Center responders. J Trauma Stress. 2017;30(2):107–14.
Cukor J, Restuccia M. Carbon monoxide poisoning during natural disasters: the Hurricane Rita experience. J Emerg Med. 2007;33(3):261–4.
Falise AM, Griffin I, Fernandez D, Rodriguez X, Moore E, Barrera A, et al. Carbon monoxide poisoning in Miami-Dade County following Hurricane Irma in 2017. Disaster Med Public Health Prep. 2019;13(1):94–6.
Fife CE, Smith LA, Maus EA, McCarthy JJ, Koehler MZ, Hawkins T, et al. Dying to play video games: carbon monoxide poisoning from electrical generators used after hurricane Ike. Pediatrics. 2009;123(6):e1035–8.
Gulati RK, Kwan-Gett T, Hampson NB, Baer A, Shusterman D, Shandro JR, et al. Carbon monoxide epidemic among immigrant populations: King County, Washington, 2006. Am J Public Health. 2009;99(9):1687–92.
Iseki K, Hayashida A, Shikama Y, Goto K, Tase C. An outbreak of carbon monoxide poisoning in Yamagata Prefecture following the Great East Japan Earthquake. Asia Pac J Med Toxicol. 2013;2(2):37–41.
Jani AA, Fierro M, Kiser S, Ayala-Simms V, Darby DH, Juenker S, et al. Hurricane Isabel-related mortality—Virginia, 2003. J Public Health Manag Pract. 2006;12(1):97–102.
Kile JC, Skowronski S, Miller MD, Reissman SG, Balaban V, Klomp RW, et al. Impact of 2003 power outages on public health and emergency response. Prehosp Disaster Med. 2005;20(2):93–7.
Klein JG, Alter SM, Paley RJ, Hughes PG, Clayton LM, Benda W, et al. Carbon monoxide poisoning at a Florida Hospital following Hurricane Irma. Am J Emerg Med. 2019;37(9):1800–1.
Lutterloh EC, Iqbal S, Clower JH, Spiller HA, Riggs MA, Sugg TJ, et al. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 2011;126(Suppl 1):108–15.
Muscatiello NA, Babcock G, Jones R, Horn E, Hwang SA. Hospital emergency department visits for carbon monoxide poisoning following an October 2006 snowstorm in western New York. J Environ Health. 2010;72(6):43–8.
Nakayama T, Tanaka S, Uematsu M, Kikuchi A, Hino-Fukuyo N, Morimoto T, et al. Effect of a blackout in pediatric patients with home medical devices during the 2011 eastern Japan earthquake. Brain Dev. 2014;36(2):143–7.
Prezant DJ, Clair J, Belyaev S, Alleyne D, Banauch GI, Davitt M, et al. Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med. 2005;33(1 Suppl):S96–101.
Schnall A, Law R, Heinzerling A, Sircar K, Damon S, Yip F, et al. Characterization of carbon monoxide exposure during Hurricane Sandy and subsequent Nor'easter. Disaster Med Public Health Prep. 2017;11(5):562–7.
Styles T, Przysiecki P, Archambault G, Sosa L, Toal B, Magri J, et al. Two storm-related carbon monoxide poisoning outbreaks-Connecticut, October 2011 and October 2012. Arch Environ Occup Health. 2015;70(5):291–6.
Van Sickle D, Chertow DS, Schulte JM, Ferdinands JM, Patel PS, Johnson DR, et al. Carbon monoxide poisoning in Florida during the 2004 hurricane season. Am J Prev Med. 2007;32(4):340–6.
Baer A, Elbert Y, Burkom HS, Holtry R, Lombardo JS, Duchin JS. Usefulness of syndromic data sources for investigating morbidity resulting from a severe weather event. Disaster Med Public Health Prep. 2011;5(1):37–45.
Burlando A. Power outages, power externalities, and baby booms. Demography. 2014;51(4):1477–500.
Burlando A. Transitory shocks and birth weights: evidence from a blackout in Zanzibar. J Dev Econ. 2014;108:154–68.
Moreno J, Shaw D. Community resilience to power outages after disaster: a case study of the 2010 Chile earthquake and tsunami. Int J Disaster Risk Reduct. 2019;34:448–58.
• Nakajima M, Aso S, Matsui H, Fushimi K, Yamaguchi Y, Yasunaga H. Disaster-related carbon monoxide poisoning after the Great East Japan Earthquake, 2011: a nationwide observational study. Acute Med Surg. 2019;6(3):294–300 This study used an inpatient database to compare counts carbon monoxide poisoning before and after among disaster-exposed and unexposed regions following the 2011 Japanese Earthquake.
Rajaram N, Hohenadel K, Gattoni L, Khan Y, Birk-Urovitz E, Li L, et al. Assessing health impacts of the December 2013 ice storm in Ontario, Canada. BMC Public Health. 2016;16:544.
Pirard P, Goria S, Nguengang Wakap S, Galey C, Motreff Y, Guillet A, et al. No increase in drug dispensing for acute gastroenteritis after Storm Klaus, France 2009. J Water Health. 2015;13(3):737–45.
•• Xiao J, Huang M, Zhang W, Rosenblum A, Ma W, Meng X, et al. The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Sci Total Environ. 2019;678:755–60 This time-series study used database contained 95% of New York hospitalizations and finds evidence of increased acute and chronic ED visits for pregnancy complications after Hurricane Sandy.
•• Dominianni C, Lane K, Johnson S, Ito K, Matte T. Health impacts of citywide and localized power outages in New York City. Environ Health Perspect. 2018;126(6):067003 Evaluated both large single outages and localized power outage in NYC and differentiated between warm- and cold-season power outages.
•• Zhang W, Sheridan SC, Birkhead GS, Croft DP, Brotzge J, Justino JG, et al. Power Outage: an ignored risk factor for COPD exacerbations. Chest. 2020; This retrospective cohort study assigned power outages by power-operating divisions in New York state from 2001–2013 and used distributed lag nonlinear models controlling for time-varying confounders.
Amadi HN. Impact of power outages on developing countries: evidence from rural households in Niger Delta, Nigeria. J Energy Resour Technol. 2015;5(3):27–38.
• Koroglu M, Irwin BR, Grépin KA. Effect of power outages on the use of maternal health services: evidence from Maharashtra, India. BMJ Glob Health. 2019;4(3):e001372 Data on SAIDI and SAIFI values from India’s largest distribution utility revealed a relationship between power outages and maternal healthcare.
Ibrahim A, Aryeetey GC, Asampong E, Dwomoh D, Nonvignon J. Erratic electricity supply (Dumsor) and anxiety disorders among university students in Ghana: a cross sectional study. Int J Ment Heal Syst. 2016;10:17.
Stoppacher R, Yancon AR, Jumbelic MI. Fatalities associated with the termination of electrical services. Am J Forensic Med Pathol. 2008;29(3):231–4.
Cox R, Amundson T, Brackin B. Evaluation of the patterns of potentially toxic exposures in Mississippi following hurricane Katrina. Clin Toxicol. 2008;46(8):722–7.
Hampson NB, Stock AL. Storm-related carbon monoxide poisoning: lessons learned from recent epidemics. Undersea Hyperb Med. 2006;33(4):257–63.
Iqbal S, Clower JH, Hernandez SA, Damon SA, Yip FY. A review of disaster-related carbon monoxide poisoning: surveillance, epidemiology, and opportunities for prevention. Am J Public Health. 2012;102(10):1957–63.
Waite T, Murray V, Baker D. Carbon monoxide poisoning and flooding: changes in risk before, during and after flooding require appropriate public health interventions. PLoS Curr. 2014;6.
Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva S, Tejero J, et al. Carbon monoxide poisoning: pathogenesis, management, and future directions of therapy. Am J Respir Crit Care Med. 2017;195(5):596–606.
Pages B, Planton M, Buys S, Lemesle B, Birmes P, Barbeau EJ, et al. Neuropsychological outcome after carbon monoxide exposure following a storm: a case-control study. BMC Neurol. 2014;14:153.
Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11(7):786–9.
Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep. 2014;1(3):165–73.
Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, et al. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ. 2017;586:241–54.
Salathe M, Bengtsson L, Bodnar TJ, Brewer DD, Brownstein JS, Buckee C, et al. Digital epidemiology. PLoS Comput Biol. 2012;8(7):e1002616.
Levin N, Kyba CCM, Zhang Q, Sánchez de Miguel A, Román MO, Li X, et al. Remote sensing of night lights: A review and an outlook for the future. Remote Sens Environ. 2020;237:111443.
Min B, O'Keeffe Z, Zhang F. Whose power gets cut? Using high-frequency satellite images to measure power supply irregularity: the World Bank; 2017.
Meier A, Ueno T, Pritoni M. Using data from connected thermostats to track large power outages in the United States. Appl Energy. 2019;256:113940.
Klugman N, Rosa J, Pannuto P, Podolsky M, Huang W, Dutta P, editors. Grid watch: Mapping blackouts with smart phones. Proceedings of the 15th Workshop on Mobile Computing Systems and Applications; 2014.
Simoes J, Blanquet A, Santos N, editors. Near real-time outage detection with spatio-temporal event correlation. CIRED Workshop 2016; 2016: IET.
Hultquist C, Simpson M, Cervone G, Huang Q. Using nightlight remote sensing imagery and Twitter data to study power outages. Proceedings of the 1st ACM SIGSPATIAL International Workshop on the Use of GIS in Emergency Management; Bellevue, Washington: Association for Computing Machinery; 2015. p. Article 6.
Mao H, Thakur G, Sparks K, Sanyal J, Bhaduri B. Mapping near-real-time power outages from social media. Int J Digit Earth. 2019;12(11):1285–99.
Sun H, Wang Z, Wang J, Huang Z, Carrington N, Liao J. Data-driven power outage detection by social sensors. IEEE Trans Smart Grid. 2016;7(5):2516–24.
Khan SS, Wei J, editors. Real-time power outage detection system using social sensing and neural networks. 2018 IEEE global conference on signal and information processing (GlobalSIP); 2018 26–29.
Huang B, Carley KM, editors. A large-scale empirical study of geotagging behavior on twitter. Proceedings of the 2019 IEEE/ACM International Conference on Advances in Social Networks Analysis and Mining; 2019.
Bessette-Kirton EK, Cerovski-Darriau C, Schulz WH, Coe JA, Kean JW, Godt JW, et al. Landslides triggered by Hurricane Maria: assessment of an extreme event in Puerto Rico. GSA Today. 2019;29(6):4–10.
Van Beusekom AE, Álvarez-Berríos NL, Gould WA, Quiñones M, González G. Hurricane Maria in the US Caribbean: disturbance forces, variation of effects, and implications for future storms. Remote Sens. 2018;10(9):1386.
Adhikari B, Mishra SR, Sujan Babu M, Kaehler N, Paudel K, Adhikari J, et al. Earthquakes, fuel crisis, power outages, and health care in Nepal: implications for the future. Disaster Med Public Health Prep. 2017;11(5):625–32.
Schmidlin TW. Public health consequences of the 2008 Hurricane Ike windstorm in Ohio, USA. Nat Hazards. 2011;58(1):235–49.
Ochi S, Leppold C, Kato S. Impacts of the 2011 Fukushima nuclear disaster on healthcare facilities: a systematic literature review. Int J Disaster Risk Reduct. 2020;42:101350.
Kishore N, Marques D, Mahmud A, Kiang MV, Rodriguez I, Fuller A, et al. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med. 2018;379(2):162–70.
Banks L. Caring for elderly adults during disasters: improving health outcomes and recovery. South Med J. 2013;106(1):94–8.
Casey JA, Schwartz BS, Stewart WF, Adler N. Using electronic health records for population health research: a review of methods and applications. Annu Rev Public Health. 2015;37:61–81.
The International Federation of Red Cross and Red Crescent Societies. IFRC Framework for Community Resilience Geneva 2014. Available from: https://media.ifrc.org/ifrc/wp-content/uploads/sites/5/2018/03/IFRC-Framework-for-Community-Resilience-EN-LR.pdf. Accessed 29 Aug 2020.
Helsloot I, Beerens R. Citizens' response to a large electrical power outage in the Netherlands in 2007. J Conting Crisis Manag. 2009;17(1):64–8.
Parent JR, Meyer TH, Volin JC, Fahey RT, Witharana C. An analysis of enhanced tree trimming effectiveness on reducing power outages. J Environ Manag. 2019;241:397–406.
Robinson M, Shapiro A. Home Healthcare in the Dark: Clean Energy Group and Meridian Institute; 2019.
Rosales-Asensio E, de Simón-Martín M, Borge-Diez D, Blanes-Peiró JJ, Colmenar-Santos A. Microgrids with energy storage systems as a means to increase power resilience: an application to office buildings. Energy. 2019;172:1005–15.
Baik S, Morgan MG, Davis AL. Providing limited local electric service during a major grid outage: a first assessment based on customer willingness to pay. Risk Anal. 2018;38(2):272–82.
Lurie N, Bunton A, Grande K, Margolis G, Howell B, Shrank WH. A public-private partnership for proactive pharmacy-based outreach and acquisition of needed medication in advance of severe winter weather. JAMA Intern Med. 2017;177(2):271–2.
Miles SB, Jagielo N, Gallagher H. Hurricane Isaac power outage impacts and restoration. J Infrastruct Syst. 2016;22(1):05015005.
DeSalvo KB. The health consequences of natural disasters in the United States: progress, perils, and opportunity. Ann Intern Med. 2018;168(6):440–1.
Use of carbon monoxide alarms to prevent poisonings during a power outage--North Carolina, December 2002. MMWR Morb Mortal Wkly Rep. 2004;53(9):189–92.
Ran T, Nurmagambetov T, Sircar K. Economic implications of unintentional carbon monoxide poisoning in the United States and the cost and benefit of CO detectors. Am J Emerg Med. 2018;36(3):414–9.
Henretig FM, Calello DP, Burns MM, O'Donnell KA, Osterhoudt KC. Predictable, preventable, and deadly: epidemic carbon monoxide poisoning after storms. Am J Public Health. 2018;108(10):1320–1.
Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania-findings from key informant interviews. PLoS One. 2018;13(9):e0203588.
Calderon R, Morgan MC, Kuiper M, Nambuya H, Wangwe N, Somoskovi A, et al. Assessment of a storage system to deliver uninterrupted therapeutic oxygen during power outages in resource-limited settings. PLoS One. 2019;14(2):e0211027.
Hawkes MT, Conroy AL, Namasopo S, Bhargava R, Kain KC, Mian Q, et al. Solar-oowered oxygen delivery in low-resource settings: a randomized clinical noninferiority trial. JAMA Pediatr. 2018;172(7):694–6.
Funding
Dr. Casey received funding from a National Institutes of Environmental Health Sciences R00 ES027023 and NIEHS P30 ES009089. Dr. Kiang received funding from National Institute on Drug Abuse K99 DA051534.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Environmental Disasters
Supplementary Information
ESM 1
(PDF 270 kb)
Rights and permissions
About this article
Cite this article
Casey, J.A., Fukurai, M., Hernández, D. et al. Power Outages and Community Health: a Narrative Review. Curr Envir Health Rpt 7, 371–383 (2020). https://doi.org/10.1007/s40572-020-00295-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-020-00295-0