Abstract
Purpose of review
The purpose of this manuscript is to review preventive strategies for surgical site infection (SSI) in low- and middle-income countries (LMIC) and how the recent World Health Organization (WHO) guidelines, along with the Centers for Disease Control (CDC) recommendations on SSI prevention, may be implemented on these settings, considering frequent limitations and possible solutions.
Recent findings
Surgical site infection (SSI) is the most common postoperative complication and in LMIC is the first cause among healthcare-associated infections (HAI). SSIs are largely preventable if there is a standardized process of care throughout the operative and perioperative period. SSIs, especially clean procedures, are considered a marker of quality in healthcare.
Summary
Education and cultural aspects have an enormous influence on the correct performance of SSI preventive measures. Getting patients and healthcare professionals engaged with prevention is the first step to make policies work properly in LMIC, no matter how this might take a lot of time and effort to be accomplished. Infection control professionals are not a luxury in any setting and efforts to support HAI control should be a priority. Surveillance is one of the most important and difficult tasks in SSI prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Importance, background, and problem magnitude: in limited resource countries
Surgical site infection (SSI) is the most common postoperative complication and in many settings, the first cause among healthcare-associated infections (HAI) [1••, 2••]. SSIs are expensive as they increase morbidity and mortality, direct and indirect healthcare-associated costs, pain, and patients’ suffering. In addition, when patients are required to pay for their own treatment, catastrophic health expenditure and impoverishment can also result [3•].
Low-, middle-, and high-income economies are defined according to their per capita national income using the World Bank Atlas methods. Sixty-three percent of the world’s nations are classified as low- and middle-income countries (LMIC), and they represent more than 75% of the world’s population [4].
In 2010, the World Health Organization (WHO) reported that the prevalence of HAI in LMIC was 20 times higher than that observed in high-income countries. SSIs were the most prevalent HAI and affected up to one-third of patients undergoing surgery, demonstrating a marked disparity compared with SSI rates from high-income countries [2••]. Furthermore, data from the GlobalSurg Collaborative study reported more resistant infections in LMIC, consistent with other reports from Latin America and Asia [3•, 5, 6].
SSIs are largely preventable if there is a standardized process of care throughout the operative and perioperative period. SSIs (especially clean procedures) are considered a marker of quality in healthcare, and thus, the efforts targeted to reduce these infections through the surgical process standardization, and introduction of evidence-based preventive measures, represents a major accomplishment for healthcare institutions.
The practice of surgery in limited resources settings is often surrounded by medical and non-medical factors that interfere with best surgical practice, as equipment, surgical facilities, supplies, and standards of operations need to be improved. In LMIC, it is a well-known fact the reuse of medical equipment that is designed for single use is a common practice with non-optimal reprocessing protocols and sterilization, as these protocols are frequently non-regulated and insufficient to guarantee sterility of supplies [7]. Another problem faced in the surgical practice is the constant availability of supplies. Antibiotics for surgical prophylaxis, antiseptics, properly fitted gloves, and a wide variety of other resources are not always available because of economic constrains and administrative policies, creating a non-safe environment for surgery and surgical care, which in turn, increases the risk of SSIs and other adverse events [8].
Most of the guidelines on SSI prevention come from high-income countries, and despite its proficient quality and reasonable adherence in such countries, the implementation and compliance of these recommendations in LMIC may be unrealistic due to the inherent limitations on infrastructure, financial support, logistics, and human capital. To overcome part of these problems, in 2016, the WHO published a series of recommendations that could be used worldwide, with a certain focus on LMIC [9]. Shortly after their publication, the Centers for Disease Control (CDC) updated their current guidelines and recommendations [10••].
In this literature review, we analyze the policies on SSI prevention throughout the process of surgical care, considering the most recent recommendations by WHO and the CDC guidelines, with special emphasis in the process of care and practices in LMIC; we also review some common limitations and possible solutions in these settings. For host-related factors, and those targeted to special surgeries, we encourage the readers to review the WHO and CDC guidelines and specialized literature.
What are the current recommendations on SSI prevention?
For a long time, SSI prevention has been a serious concern among surgeons, hospital epidemiologists, and infection control practitioners, not to mention patients. With the increasing complexity of surgery and more comorbid patients, safe surgical care must be a priority.
There is compelling evidence of preventive measures that reduce SSIs; however, their implementation varies according to the type of medical center and within countries. In LMIC, many of the preventive strategies to reduce SSIs are still lacking or might be difficult to utilize despite the most current recommendations.
The cause of an SSI is usually multi-causal (Fig. 1) and depends on the interaction of host and microbial and environment/extrinsic factors. Process standardization and compliance to the most basic infection control measures may prevent up to 50% of SSI, but preventing those infections in LMIC facilities is still difficult to achieve.
Actions against SSI must be taken before, during, and after the surgical procedure. Relevant aspects of the process will be discussed in the following part of this manuscript.
Preoperative preventive strategies
Perioperative antimicrobial prophylaxis
Administration of parenteral antimicrobial prophylaxis (PAP) is widely accepted as an efficacious preventive strategy for SSI in clean-contaminated and several clean procedures (e.g., cardiovascular, neurological, orthopedic with prosthetic implant, hernioplasty, and breast procedures). It is strongly recommended by most guidelines worldwide and is an accepted practice. Antimicrobial agents for perioperative antibiotic prophylaxis should be administered within 60 min of the skin incision (strong recommendation) and no additional prophylactic agent doses are needed after the surgical incision is closed in the operating room, even in the presence of a drain (strong recommendation; high quality of evidence). Some research gaps remain related to weight-adjusted parenteral administration of antibiotics and intraoperative redosing in long surgeries [9••, 10••].
Gaps and opportunities in limited resources countries
Despite that recommendations in the use of PAP regarding the most appropriate antibiotics and number of doses are widely accepted, in limited resources settings, it is not infrequent to choose antibiotics for prophylaxis based on availability or surgeons’ preferences. In many hospitals, there is no continuous supply of antibiotics or restricted amount of them, which frequently ends up on choosing antibiotics according to their availability and not based on the best practice. The use of low-quality generic drugs that deliver suboptimal concentrations seems to be an increasing problem with negative consequences.
In limited resources medical facilities, extended prescription of antibiotics after surgery prevails, with the belief that sanitary conditions in the hospitals and the hygiene of patients are inferior to that of high-income countries. Other factors such as the wide use of quinolones for PAP in environments with high resistance not only make PAP inappropriate but also increase selective pressure with the risk of infections caused by resistant pathogens [11].
The introduction of stewardship programs for reducing the inappropriate use of antibiotics in surgery is still lacking in most hospitals in LMIC. The use of centralized pharmacy delivery of antibiotics is also absent in many institutions, and there is a big opportunity to improve and standardize its prescription; we strongly recommend this strategy. Education to nurses, surgeons, and anesthesiologists, coupled with electronic systems that favor a rational use of antibiotics during the surgical process of care, should be promoted. For policy makers and investors, the introduction of affordable information technology that can be available to all prescribers is a huge necessity.
Screening for extended-spectrum beta-lactamase colonization and surgical antibiotic prophylaxis
The prevalence of extended-spectrum beta-lactamase (ESBL)–producing Enterobacteriaceae, mainly Escherichia coli, has increased over the past 10 years both in the community and healthcare facilities. As other Enterobacteriaceae, ESBL strains reside in the gastrointestinal tract. Gastrointestinal tract colonization varies, but it is considered to be high if there is a prevalence > 10%. In two recent studies, preoperative carriage of ESBL Enterobacteriaceae was higher than 10% [12, 13]. In the study by Dubinsky-Pertzov conducted in three cities, Geneva, Serbia, and Tel Aviv, in patients undergoing colorectal surgery, the prevalence in each city was 12%, 9%, and 29%, respectively [12]. For the patients in Mexico, the prevalence in gynecological and gastrointestinal surgeries was 17.5% [13]. In both studies, being colonized by an ESBL Enterobacteriaceae duplicated the risk of an SSI [12, 13].
Gaps and opportunities in limited resources countries
In LMIC, E. coli and other enterobacteria are frequently associated to SSI [14, 15•]. Considering the high prevalence of ESBL-colonizing strains, although there is no any recommendation regarding perioperative antibiotic prophylaxis if the patient is colonized by ESBL strains, adjusting PAP might be necessary in some procedures. An individualized approach should be considered in high-risk patients, such as patients with cancer or those undergoing complex procedures such as liver transplant or pancreatic surgery. The authors do not recommend routine screening, nor a particular scheme for prophylaxis, but we encourage the reader to evaluate the local conditions and make the best choice of antibiotics for the patient and the type of surgery.
Decolonization with mupirocin in nasal carriers of Staphylococcus aureus
S. aureus is one of the most common pathogens associated with healthcare infections. In SSIs, it is the microorganism most frequently isolated, especially in clean procedures, such as cardiothoracic and orthopedic surgeries [16].
S. aureus nasal carriage has been identified as a risk factor for subsequent infection in several groups of patients, with increased morbidity, mortality, and costs, particularly if there is methicillin resistance. Despite that very few SSIs are caused by methicillin-resistant S. aureus, preoperative nasal decolonization with mupirocin 2% ointment, with or without chlorhexidine soap body wash in cardiothoracic and orthopedic surgeries, is recommended (strong recommendation, moderate quality of evidence) [17, 18]. For other high-risk surgeries, it can also be considered [9••, 10••].
Gaps and opportunities in limited resources countries
Screening for S. aureus nasal colonization is a well-accepted, efficient, and cheap preoperative practice in high-risk procedures; in high-income countries, it is also cost-effective. In LMIC, implementation of this strategy is feasible and it is probably cost-effective as well, but considering that in many hospitals from limited resources countries, the prevalence of S. aureus is lower compared with other settings, we recommend to evaluate the prevalence of S. aureus nasal colonization in each setting prior to the implementation of a decontamination program [19]. It is also important to mention that many LMIC microbiology laboratories are not always available on site, and if available, they usually have scarce resources.
Considering all of the above, the authors recommend to shape a screening and decontamination protocol based on each hospital and patient’s prevalence of S. aureus colonization and infections.
Antiseptic prophylaxis
For this section, three practices will be reviewed, preoperative bathing, preoperative surgical skin preparation, and surgical hand preparation, as these preventive measures are related to skin antisepsis and represent a key element to SSI prevention.
Preoperative bathing
It is a good clinical practice for patients to bathe or shower prior to surgery (the same day or the night before), and most medical societies and organizations endorse this measure as it helps to keep the skin clean and reduce the burden of microorganisms. There is inconclusive evidence regarding the optimal timing of preoperative shower or bath, the total number of soap or antiseptic applications, and the use or not of chlorhexidine washcloths. The US Institute for Healthcare Improvement (IHI) bundle for hip and knee arthroplasty recommends the use of chlorhexidine soap for preoperative bathing [20].
Gaps and opportunities in limited resources countries
Bathing or showering should be encouraged in all patients undergoing surgery, but in LMIC, the availability and access to clean water may be a problem in some areas. Another potential problem is the conditions and long journeys patients take prior to their arrival into the hospital. Considering the increasing number of patients admitted the same day of surgery, the medical centers should have the facilities for the patients to shower, and nurses and medical assistants should encourage the patients to do so.
Despite that the quality of water can be a problem in limited resources settings, and that there is inconclusive evidence on the use of impregnated chlorhexidine wash-clothes to prevent SSIs, as they increase costs and potentially bacterial tolerance and resistance, we do not recommend this as an alternative to patients showering and use of plain or antiseptic soap prior to surgery.
Surgical skin preparation
The aim of the surgical site skin preparation is to reduce the patient’s skin microbial load prior to the surgical incision. It should always be performed inside the operating room, prior to the initiation of surgery. For a long time, the most common agents used include chlorhexidine gluconate (CHG) and povidone-iodine, alone or in combination with alcohol-based solutions. The current evidence supports the use of alcohol-based antiseptic solution based on CHG for surgical skin preparation, unless contraindicated (strong recommendation, moderate quality of evidence) [9••, 10••]. Alcohol-based solutions should not be used on neonates or come into contact with mucosa or eyes. Because of its flammable nature, caution should be exercised. Chlorhexidine should not get in contact with the brain meninges, eyes, or middle ear.
Gaps and opportunities in limited resources countries
In LMIC, it is not an extended practice to use alcohol-based solutions for surgical site skin preparation as they are usually more expensive, and in distant places, procurement is also more difficult. In most LMIC, povidone-iodine is extensively available. Despite that the current recommendations favor alcohol-based CHG antiseptic solutions, it is not inappropriate to use povidone-iodine or chlorhexidine for skin preparation [21]. What is more important is the quality and availability of antiseptics, and we strongly recommend that in LMIC, healthcare providers and administrators verify the quality and acquisition of antiseptics because it is not uncommon that administrators buy cheaper products that do not comply with quality standards [14].
Another frequent problem with the antiseptics in LMIC is that they are not single use preparations. Operating room staff should also comply with a prespecified and regular disposal of antiseptics in small volumes in order to avoid contamination and ensure that the containers used are cleaned and sterilized on regular basis.
Surgical hand preparation
It is widely accepted and strongly recommended that surgical hand preparation of staff on the sterile field is performed either by scrubbing with a suitable antimicrobial soap and water, or using alcohol-based hand rub before donning the sterile gloves. Surgical hand preparation is of utmost importance to maintain the lowest possible contamination of the surgical field, especially if we consider that glove micropunctures are frequent during surgery. Surgical hand preparation is clearly acknowledged and recommended in 2009 WHO Guidelines [22].
Gaps and opportunities in limited resources countries
As for the surgical site skin preparation, in LMIC, the quality of antiseptics and safety of the running water pose a risk, and operating room and infection control staff should warranty the quality of both. Regular checking of water chlorine and the quality of antiseptics are highly encouraged, along with appropriate sinks for hand cleaning and antisepsis, and/or alcohol-based hand rub dispensers as per international standards. In places with limited availability of antiseptics, the local production of alcohol-based formulation as specified in the WHO Hand Hygiene Guidelines is highly encouraged [22].
Hair removal
In patients undergoing surgery, removal of hair has been traditionally a part of the preoperative preparation; however, evidence strongly supports not to remove the hair, unless if it is absolutely necessary. Hair removal can be achieved by shaving, clipping, or depilatory creams. Although clipping is preferred over shaving because SSIs rates are 50% lower, both have the potential to cause microscopic skin trauma and should be discouraged. When necessary, the use of the clipper is preferred and should always be conducted as close as possible to the incision time. Removing the hair the night before is strongly discouraged as this practice increases the skin colonization by hospital bacteria.
Gaps and opportunities in limited resources countries
In busy hospitals from LMIC, clippers are usually not available because of their cost, and shaving razors remain the most frequent method for hair removal. Although some studies found an increased risk of SSI with shaving, when using this method, razors should be single use [23, 24]. We also encourage to perform the hair removal as close as possible to the incision time to avoid colonization of skin micro-abrasions after shaving. In LMIC, physicians and nurses are advised to verify the current practice of hair removal in their hospitals and write clear policies on this practice, as important variations may occur within hospitals and healthcare workers beliefs.
Intraoperative and immediate postoperative period
In general, according to the CDC guidelines, the priority during surgery to reduce SSI is to maintain a correct surgical technique and proper aseptic precautions. During the postoperative period, it is important to emphasize that wound closed by first intention must be covered by a sterile dressing at least for the next 24 h after the surgery, and dressing must be changed using sterile technique [25•].
It is important to explain in a more detailed fashion the following concepts during the intraoperative period:
Normothermia
Hypothermia is a common phenomenon that usually occurs during and after surgery in procedures lasting more than 2 h because of impairment of thermoregulation by anesthesia, combined with exposure to cold environment in the operating room [26••, 27]. Unintended hypothermia might be associated with an increased risk of cardiac complications, blood loss due to impaired coagulation, impaired wound healing, decreased drug metabolism, decreased immune function, and an increased risk of SSI [26••, 28]. There are several studies that have demonstrated the effect of body warming with 50–70% reductions in SSIs, regardless the warming method [29] (Wong, 2007).
Gaps and opportunities in limited resources countries
Although there is a good amount of evidence to support the use of warming devices to avoid hypothermia during surgery, in low resources settings, these devices are usually not available because of their cost and maintenance. Several alternatives as warming the solutions in conventional microwaves or using simple blankets can help to reduce hypothermia, but a note of caution is advised, especially with fluid warming. We encourage the readers to adopt the best practice considering a reduction of risks to patients (e.g., fluid contamination). Another problem in some of these settings is the lack of sensors to measure core body temperature, with the consequence of no records on body temperature. We encourage the reader to establish a program of body temperature measurement during surgery and shortly after, balancing efficiency, cost, and risks of the available warming devices.
Perioperative oxygenation
Several studies have suggested that providing high FiO2 (80%) compared with the usual 30–35% FiO2 is beneficial in adult patients undergoing general anesthesia with tracheal intubation, especially in colorectal surgeries, based on the fact that the surgical incision might receive higher oxygen if there is a higher partial pressure of oxygen in the blood. There is also the notion that higher oxygenation improves the neutrophil oxidative killing, decreasing several adverse events, including SSIs. [30]. Although perioperative oxygenation through a facemask or nasal cannula may optimize oxygenation during and immediately after surgery and that this preventive measure has been endorsed by different professional associations, the 2018 updated WHO Global Guidelines for the Prevention of Surgical Site Infection and the CDC SSI 2017 guideline give to this preventive strategy a conditional recommendation with moderate quality of evidence [9••, 10••]. There are some concerns on pulmonary adverse events, such as atelectasis; critically ill patients may increase mortality and there is scarce information on the pediatric population [31].
Gaps and opportunities in limited resources countries
Considering the available information and that in remote areas, oxygen supply might be restricted, we suggest to prioritize its use in procedures (e.g., colorectal surgery) in which hyperoxia has shown more benefits, in order to have a rational use of resources.
Glycemic control
Control of blood glucose during surgery and the immediate postoperative period in diabetic and non-diabetic is desirable and sounds a physiological and a medical measure that should be done in all surgical patients. This has been recommended by many professional associations, but some confusion has arisen regarding intensive perioperative blood glucose control and more strict target levels, as more adverse events, such as hypoglycemia, may occur. The current WHO Global Guidelines for the Prevention of Surgical Site Infection left the intensive protocols for blood glucose control as a conditional recommendation with low-quality evidence. Opposite to the WHO recommendation, the 2017 CDC SSI guideline strongly recommends to implement perioperative glycemic control and use of blood glucose target levels less than 200 mg/dL, regardless if the patient has diabetes or not [9••, 10••]. From our point of view, and considering that approximately 3.42% of patients undergoing non-cardiac surgery do not know that they are diabetic, and that levels > 200 mg/dL have been associated to SSIs and other adverse events, we support the control of blood glucose during surgery and the immediate postoperative period in all major in-hospital surgeries with targets not higher than 180–200 mg/dL [32].
Gaps and opportunities in limited resources countries
Most of the studies published on glycemic control in surgical patients come from high-income countries, and cost-effectiveness of this preventive measure is lacking. The latter issue is an important gap to consider when planning to implement this policy in constrained resources environments; we encourage to conduct such analysis in LMIC. There are also some practical aspects to acknowledge when doing glycemic control in the surgical patient in limited resources centers:
-
1.
The resources available. Capillary blood glucose measurement is easy and inexpensive, but the availability of these supplies varies from site to site and we must make sure that the implementation of a more intensive blood glucose program in surgical patients does not compromise the resources for other patients, such as the diabetics.
-
2.
A clear policy must be introduced, stating the surgeries in which this policy will operate, along with a clear and safe insulin program delivery for patients with glucose levels > 200 mg/dL during surgery or the immediate postoperative period.
From our perspective, a written program on glucose measurement and control for surgical patients in LMIC is a priority, since there are many patients with unknown diabetes or pre-diabetes, overweight, and obesity who could benefit from the test itself and to reduce SSIs, which have been shown to be increased in patients with both diabetes and obesity. Considering these facts, a surgical glycemic control program is probably cost-effective in most cases, but more studies in these settings are needed.
Postoperative period
Wound care and dressings
The surgical wound refers to the incision made with a scalpel or other sharp cutting device and then closed by approximation of the skin edges in the operating room by suture, staples, adhesive tape, or glue. These incisions are regularly covered by a dressing that acts as a physical barrier to protect the wound from the external environment until it becomes impermeable to microorganisms. The dressing may also serve to absorb exudate and keep the wound dry. A surgical wound closed in the operating room is usually impermeable 48 h after the incision, and covering the incision is a common and an appropriate practice in surgery [9••].
There are a wide variety of dressings, from gauzes to advanced dressings that can be used to cover the surgical incision. From the most recent evidence, it is uncertain whether one dressing or other reduces the risk of developing an SSI. It is also uncertain that covering the surgical wounds healing by primary intention for longer periods than 48–72 h reduces the risk of SSI [9••, 33].
Despite the controversies, the UK-based NICE clinical guideline on SSI prevention recommends the use of an appropriate interactive dressing at the end of the procedure over the traditional gauze [34]. Nowadays, several transparent film dressings for postoperative use are available to cover surgical wounds, and their use depends a lot on surgeon preferences. They are usually cheap, easy to use, and comfortable for patients, with the advantage of being semipermeable with better adhesion than a gauze.
Gaps and opportunities in limited resources countries
Despite that there are some controversies on the use of dressings to prevent SSIs, in LMIC, several issues must be addressed. In many hospitals, it is a common practice to use a simple gauze as an occlusive dressing because of its low cost, but in most settings, there is a lack of a protocol of care of the surgical wounds during the postoperative period. It is not uncommon that as a standard practice, the gauzes are changed once or twice daily, regardless of the time since surgery or the condition of the wound. Moreover, in limited resources settings, overcrowding and unsafe delivery of care are common, and due to the low risk perception of dressing change by most healthcare workers, poor hand hygiene compliance and incorrect use of gloves increase the risk of wound contamination and cross-transmission. Exposure during the first 48 h to unsafe water may also increase the risk of wound contamination.
We strongly recommend that a written protocol on surgical wound care is written and used at each institution. Recommending one dressing over another depends on the resources available and preferences, but having the wound occluded for the first 48 h without manipulation or exposure to water, if no complication occurs, sounds cost-effective and a safe preventive measure. Transparent semipermeable post-op films may be a good and cost-effective dressing. We suggest the reader to evaluate the most appropriate dressing in each practice.
Implementation and strengthening of a good surveillance program to detect and prevent surgical infections
Surveillance is one of the most important and difficult tasks in SSI prevention. It consumes more time and resources compared with other hospital infections and it is labor-intensive. It has been demonstrated that surveillance, regular auditing, and feedback to surgeons on their SSI rates contribute to SSI reduction. It can also help to strengthen compliance of bundles on SSI prevention [35•, 36].
Several modalities of surveillance are accepted, with various degrees of sensitivity. For SSI surveillance, a combination of methods is usually used. Electronical patient, microbiology, and pharmacy records seem to be effective in high-income countries while the patient is in-hospital; however, the most challenging part of surveillance is post-discharge surveillance, as should be as long as 30 days after surgery, or even 1 year when prosthetic material has been inserted. For post-discharge surveillance, information usually relies on surgeon reports of infection, questionnaires or telephone calls to the patient, or a follow-up visit by healthcare workers to patients’ “home” [37]. The combined use of chart reviews, microbiology reports, and re-admissions to the hospital within the 30 days of surgery is also an accepted method for SSI surveillance. The combination of different strategies usually gives best results.
Ideally, surveillance on surgical patients should create necessary data for developing statistical models to predict SSI in specific populations, as has been proven accurate and relevant for assisting high-risk patients in certain groups [38]. Nevertheless, this reality is far from being implemented in the majority of LMIC, but some similar and simpler measures might be helpful.
Gaps and opportunities in limited resources countries
Surveillance as a hallmark on SSI is also vulnerable in LMIC. Although successful development of HAI National Surveillance Programs has been implemented in various LMIC, lack of resources and continuity still remains [39]. Pressure to report SSI data and more strict regulations are not enforced as strictly as in high-income countries, and not infrequently there is a low risk perception of surgical-related infections by most actors. Furthermore, the importance of surveillance, audit, and feedback becomes crucial at the moment of asking for new government funds. If no surveillance in SSI is made, no data is obtained, which misses the opportunity to identify the problem. If the problem is not identified, then there is no evidence of it and therefore no way to prove the importance of this issue as a priority and the need of more resources to deal with it [40]. A fact usually left unadvertised is that prevention results in savings, which is appealing for all HAI in LMIC [41].
Also, poor attendance to follow-up visits has been identified as a common problem in LMIC [42]. Therefore, some strategies have been proposed to overcome this problem. In LMIC with high penetration of mobile phone services, telephone calls to patients after discharge have been considered a reasonable method for SSI detection. Some studies have described a sensitivity ranging from 70 to 83%, and a specificity of 100% for this modality, when compared with direct clinical evaluation [37, 43, 44]. When phone call is made, there is consensus regarding the good negative predictive value of the self-diagnosis of purulent drainage by patients, which ranges from 95 to 99%. [37, 44, 45]. Although more information is needed, the use of these technologies and friendly and appropriate applications for patients that live in remote areas may be attractive.
What else can we do to prevent SSIs? Think on multimodal improvement strategy
SSI’s prevention is complex and it is possibly underestimated because of the challenges around complete ascertainment of these infections, especially for the SSIs that are diagnosed after hospital discharge or are related to ambulatory procedures.
In the WHO Global Infection Prevention and Control Unit, a multimodal improvement strategy with the aim of reducing SSIs was established. This multimodal strategy is targeted to system change, training and education, evaluation and feedback, communication for awareness raising, and creating an institution safety climate and culture. All of these should allow for steps to be taken to prevent SSIs based on known modifiable risk factors [46].
With a similar approach, in the USA, the Centers for Medicare and Medicaid Services and the Centers for Disease Control and Prevention established the Surgical Care Improvement Project (SCIP) with the support of multiple agencies and organizations, and with the aim of improving SSI outcomes by increasing adherence to established evidence-base performance measures. Although with the same objectives as the WHO multimodal strategy, these measures are more specific and some of them require more than a system change in LMIC. The measures proposed by SCIP regarding SSI prevention are as follows: prophylactic antibiotic started within 1 h prior to surgical incision; antibiotic prophylaxis consistent with recommendations; prophylactic antibiotics discontinued within 24 h after surgery end time; cardiac surgery patients with controlled postoperative glucose; surgery patients with appropriate hair removal; urinary catheter removed on postoperative day 1 or postoperative day 2 with day of surgery being day zero; and surgery patients with perioperative temperature management. Most hospitals in the USA have rapidly adopted these measures during the last decade, but as has been discussed, these practices probably reflect the minimum requirement for SSI prevention; for true SSI reduction, simultaneous adherence to additional interventions is needed.
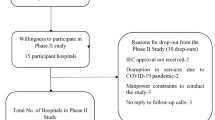
In Fig. 2, we provide a flowchart of evidence-based risk factors for SSIs throughout the process of surgical care that may be reduced if addressed properly.
Closing remarks on SSI prevention in LMIC
Education and cultural aspects have an enormous influence on the correct performance of SSI preventive measures. A lack of culture in infection prevention, no awareness of guidelines, and non-expectancy to implement and follow up them, deficient audit systems, deviations in application of policies to protect patients’ rights, lack of motivation, and deficient communication to health professionals and patients are reported as regular cultural and educational limitations to prevent SSI in LMIC [47•].
Fear to change is also common and resistance to the introduction of new policies is frequent in some hospitals. Healthcare staff is generally satisfied with their status quo and they would be unlikely to accept changes. As their performance is continuously evaluated, they might feel it as a threat and a lot needs to be done in this regard [48]. Getting patients and healthcare professionals engaged with prevention is the first step to make policies work properly in LMIC, no matter how this might take a lot of time and effort to be accomplished [49]. Although it is a long and a difficult task, there are successful examples that should encourage other hospitals, infection control personnel, surgeons, and other HCWs and administrators to embrace in these activities.
Infection control professionals are not a luxury in any setting [26••] and efforts to support the programs should be a priority. Academic and professional cooperation among developed countries and LMIC should be encouraged as a tool for training high-quality professionals, so they can return to their native countries and implement the state of art on SSI prevention on precarious settings.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Allegranzi B, Kubilay NZ, Zayed B, Atema JJ, Gans S, Boermeester MA, et al. Surgical site infections 1 New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis. 2016;16:e276–87. https://doi.org/10.1016/S1473-3099(16)30398-X Key reference for preventing surgical infections. Up-to-date information from the WHO guidelines.
•• Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet (London, England). 2011;377(9761):228–41. https://doi.org/10.1016/S0140-6736(10)61458-4 Key reference for preventing surgical infections. Up-to-date information from the WHO guidelines.
• Bhangu A, Ademuyiwa AO, Aguilera ML, Alexander P, Al-Saqqa SW, Borda-Luque G, et al. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 2018;18(5):516–25. https://doi.org/10.1016/S1473-3099(18)30101-4 Manuscript that describes some of the current problems and the impact of surgical site infections in low-, middle-, and high-income countries. Although it only provides information regarding gastrointestinal, it clearly exemplifies the impact of multi-drug-resistant infections and the risk of infection between regions according to income country.
The World Bank. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups Accessed 6 Feb 2019
Figueroa-Padilla J, Soto-Perez-de-Celis E, Maciel-Miranda A, Vargas-Salas D, Santamaria E, Esparza-Arias N, et al. Implementation of a microsurgical breast reconstruction program in Mexico. Microsurgery. 2018;38(8):831–3. https://doi.org/10.1002/micr.30383.
Kamat U, Ferreira A, Savio R, Motghare D. Antimicrobial resistance among nosocomial isolates in a teaching hospital in Goa. Indian J Community Med 2008;33(2):89–92. https://doi.org/10.4103/0970-0218.40875.
Tessarolo F, Caola I, Caciagli P, Guarrera GM, Nollo G. Sterility and microbiological assessment of reused single-use cardiac electrophysiology catheters. Infect Control Hosp Epidemiol. 2006;27(12):1385–92. https://doi.org/10.1086/508829.
Rönnerstrand B, Lapuente V. Corruption and use of antibiotics in regions of Europe. Health Policy (Amsterdam, Netherlands). 2017;121(3):250–6. https://doi.org/10.1016/j.healthpol.2016.12.010.
••Global Guidelines for the prevention of surgical site infection. Geneva: World health organization; 2016.The WHO guideline is a comprehensive review of preventive measures targeted to a wide and general audience.
•• Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784. https://doi.org/10.1001/jamasurg.2017.09041 This paper contains the most current prevention recommendations from the CDC in the USA.
Murillo Llanes J, Varon J, Velarde Félix JS, González-Ibarra FP. Antimicrobial resistance of Escherichia coli in Mexico: how serious is the problem. J Infect Dev Ctries. 2012;6(2):126–31 https://doi.org/10.3855/jidc.1525.
Dubinsky-Pertzov, B., Temkin, E., Harbarth, S., Fankhauser-Rodriguez, C., Carevic, B., Radovanovic, I, Carmeli, Y. (2019). Carriage of extended-spectrum beta-lactamase–producing Enterobacteriaceae and the risk of surgical site infection after colorectal surgery: a prospective cohort study. Clin Infect Dis, 68(10), 1699–1704. https://doi.org/10.1093/cid/ciy768
Golzarri MF, Silva-Sánchez J, Cornejo-Juárez P, Barrios-Camacho H, Chora-Hernández LD, Velázquez-Acosta C, et al. Colonization by fecal extended-spectrum β-lactamase-producing Enterobacteriaceae and surgical site infections in patients with cancer undergoing gastrointestinal and gynecologic surgery. Am J Infect Control. 2019. 2019 Mar 6. pii: S0196-6553(19)30061-6.https://doi.org/10.1016/j.ajic.2019.01.020.
Cornejo-Juárez P, Velásquez-Acosta C, Díaz-González A, Volkow-Fernández P. Trend of antimicrobial drug-susceptibility of blood isolates at an oncological center (1998–2003). Salud Publica Mex. 2005;47(4):288–93 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16259290. Accessed 21 Mar 2019.
• Shah KH, Singh SP, Rathod J. Surgical site infections: incidence, bacteriological profiles and risk factors in a tertiary care teaching hospital, western India. International Journal of Medical Science and Public Health. 2017;6:173. https://doi.org/10.5455/ijmsph.2017.14082016597 This is one of the few papers containing microbiology information from surgical site infections during the last decade.
Humphreys, H., Becker, K., Dohmen, P. M., Petrosillo, N., Spencer, M., van Rijen, M., … Garau, J. (2016). Staphylococcus aureus and surgical site infections: benefits of screening and decolonization before surgery. J Hosp Infect, 94(3), 295–304. https://doi.org/10.1016/j.jhin.2016.06.011.
Kalra L, Camacho F, Whitener CJ, Du P, Miller M, Zalonis C, et al. Risk of methicillin-resistant Staphylococcus aureus surgical site infection in patients with nasal MRSA colonization. Am J Infect Control. 2013;41(12):1253–7. https://doi.org/10.1016/j.ajic.2013.05.021.
Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, et al. The burden of Staphylococcus aureus infections on hospitals in the United States: an analysis of the 2000 and 2001 Nationwide Inpatient Sample Database. Arch Intern Med. 2005;165(15):1756–61. https://doi.org/10.1001/archinte.165.15.1756.
Chen C-J, Huang Y-C. New epidemiology of Staphylococcus aureus infection in Asia. Clin Microbiol Infect. 2014;20(7):605–23. https://doi.org/10.1111/1469-0691.12705.
How-to guide: prevent surgical site infection for hip and knee arthroplasty. (2012). Cambridge (MA): Institute for Healthcare Improvement. Retrieved from www.ihi.org Accessed 19 Mar 2019.
Hadiati DR, Hakimi M, Nurdiati DS, da Silva Lopes K, Ota E. Skin preparation for preventing infection following caesarean section. Cochrane Database Syst Rev. 2018;10:CD007462. https://doi.org/10.1002/14651858.CD007462.pub4.
WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care: World Health Organization; 2009. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23805438 Accessed 16 May 2019.
Hamilton HW, Hamilton KR, Lone FJ. Preoperative hair removal. Can J Surg. 1977;20(3):269–71–5 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/870157. Accessed 1 Apr 2019.
Seropian R, Reynolds BM. Wound infections after preoperative depilatory versus razor preparation. Am J Surg. 1971;121(3):251–4 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/5546329. Accessed 16 May 2019.
• Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27(2):97–132 quiz 133–4; discussion 96. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10196487. Accessed 16 May 2019.A must-read manuscript. Contains definitions and recommendations on surgical site infection prevention.
•• Allegranzi, B., Zayed, B., Bischoff, P., Kubilay, N. Z., de Jonge, S., de Vries, F., … WHO Guidelines Development Group. (2016). New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12), e288–e303. https://doi.org/10.1016/S1473-3099(16)30402-9. World Health Organization publication guidelines that review the best evidence on surgical site infection prevention. Contains an extensive and evidence-based review on the most important risk factors for surgical site infections.
Sessler DI. Perioperative thermoregulation and heat balance. Lancet. 2016;387(10038):2655–64. https://doi.org/10.1016/S0140-6736(15)00981-2.
Melling AC, Ali B, Scott EM, Leaper DJ. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet. 2001;358(9285):876–80. https://doi.org/10.1016/S0140-6736(01)06071-8.
Wong PF, Kumar S, Bohra A, Whetter D, Leaper DJ. Randomized clinical trial of perioperative systemic warming in major elective abdominal surgery. Br J Surg. 2007;94(4):421–6. https://doi.org/10.1002/bjs.5631.
Allen, D. B., Maguire, J. J., Mahdavian, M., Wicke, C., Marcocci, L., Scheuenstuhl, H., Hunt, T. K.. Wound hypoxia and acidosis limit neutrophil bacterial killing mechanisms. Arch Surg 1997; 132 (9): 991–6 https://doi.org/10.1001/archsurg.1997.01430330057009.
Ni Y-N, Wang Y-M, Liang B-M, Liang Z-A. The effect of hyperoxia on mortality in critically ill patients: a systematic review and meta-analysis. BMC Pulm Med. 2019;19(1):53. https://doi.org/10.1186/s12890-019-0810-1.
Abdelmalak B, Abdelmalak JB, Knittel J, Christiansen E, Mascha E, Zimmerman R, et al. The prevalence of undiagnosed diabetes in non-cardiac surgery patients, an observational study. Can J Anesth. 2010;57(12):1058–64. https://doi.org/10.1007/s12630-010-9391-4.
Dumville JC, Gray TA, Walter CJ, Sharp CA, Page T, Macefield R, et al. Dressings for the prevention of surgical site infection. Cochrane Database Syst Rev. 2016;12:CD003091. https://doi.org/10.1002/14651858.CD003091.pub4.
Leaper D, Burman-Roy S, Palanca A, Cullen K, Worster D, Gautam-Aitken E, et al. Prevention and treatment of surgical site infection: summary of NICE guidance. BMJ (Clinical Research Ed). 2008;337(oct28 1):a1924. https://doi.org/10.1136/bmj.a1924.
• Manivannan B, Gowda D, Bulagonda P, Rao A, Raman SS, Natarajan SV. Surveillance, auditing, and feedback can reduce surgical site infection dramatically: toward zero surgical site infection. Surg Infect. 2018;19(3):313–20. https://doi.org/10.1089/sur.2017.272 An interesting perspective for surgical site infection surveillance and prevention. Review the importance of surveillance, auditing, and providing feedback to surgeons.
Fakih MG, Heavens M, Ratcliffe CJ, Hendrich A. First step to reducing infection risk as a system: evaluation of infection prevention processes for 71 hospitals. Am J Infect Control. 2013;41(11):950–4. https://doi.org/10.1016/j.ajic.2013.04.019.
Guerra J, Isnard M, Guichon C. Postdischarge surveillance of surgical site infections using telephone calls and a follow-up card in a resource-limited setting. J Hosp Infect. 2017;96(1):16–9. https://doi.org/10.1016/j.jhin.2017.02.019.
Fukuda H, Kuroki M. The development of statistical models for predicting surgical site infections in Japan: toward a statistical model–based standardized infection ratio. Infect Control Hosp Epidemiol. 2016;37(03):260–71. https://doi.org/10.1017/ice.2015.302.
Vilar-Compte D, Camacho-Ortiz A, Ponce-de-León S. Infection control in limited resources countries: challenges and priorities. Curr Infect Dis Rep. 2017;19(5):20. https://doi.org/10.1007/s11908-017-0572-y.
Swaminathan, S., Prasad, J., Dhariwal, A. C., Guleria, R., Misra, M. C., Malhotra, R, … Srikantiah, P. (2017). Strengthening infection prevention and control and systematic surveillance of healthcare associated infections in India. BMJ (Clinical Research Ed), 358, j3768. https://doi.org/10.1136/bmj.j3768
Wenzel RP. The Lowbury Lecture. The economics of nosocomial infections. J Hosp Infect. 1995;31(2):79–87 https://doi.org/10.1016/0195-6701(95)90162-0.
Fehr, J., Hatz, C., Soka, I., Kibatala, P., Urassa, H., Smith, T, Widmer, A. (2006). Risk factors for surgical site infection in a Tanzanian district hospital: a challenge for the traditional National Nosocomial Infections Surveillance System Index. Infect Control Hosp Epidemiol 27(12), 1401–1404. https://doi.org/10.1086/509855
Nguhuni B, De Nardo P, Gentilotti E, Chaula Z, Damian C, Mencarini P, et al. Reliability and validity of using telephone calls for post-discharge surveillance of surgical site infection following caesarean section at a tertiary hospital in Tanzania. Antimicrob Resist Infect Control. 2017;6(1):43. https://doi.org/10.1186/s13756-017-0205-0.
Aiken, A. M., Wanyoro, A. K., Mwangi, J., Mulingwa, P., Wanjohi, J., Njoroge, J., … Hall, A. J. (2013). Evaluation of surveillance for surgical site infections in Thika Hospital, Kenya. J Hosp Infect, 83(2), 140–145. https://doi.org/10.1016/j.jhin.2012.11.003
Whitby M, McLaws M-L, Doidge S, Collopy B. Post-discharge surgical site surveillance: does patient education improve reliability of diagnosis? J Hosp Infect. 2007;66(3):237–42. https://doi.org/10.1016/j.jhin.2007.04.014.
Preventing surgical site infections: implementation approaches for evidence-based recommendations (2018). Geneva, World Health Organization. https://apps.who.int/iris/handle/10665/273154.
•Ayub Khan MN, Verstegen DML, Bhatti ABH, Dolmans DHJM, van Mook WNA. Factors hindering the implementation of surgical site infection control guidelines in the operating rooms of low-income countries: a mixed-method study. Eur J Clin Microbiol. 2018;37(10):1923–9. https://doi.org/10.1007/s10096-018-3327-2 Provides some insights on the difficulties to implement evidence-based prevention strategies in the operating room. Reviews some new aspects on the OR functioning and the implementation of preventive strategies among the anesthesia group.
Huskins WC, Soule BM, O’Boyle C, Gulácsi L, O’Rourke EJ, Goldmann DA. Hospital infection prevention and control: a model for improving the quality of hospital care in low- and middle-income countries. Infect Control Hosp Epidemiol. 1998;19(2):125–35. https://doi.org/10.2307/30142003.
Licker, M., Bădiţoiu, L., Lungeanu, D., Dobrevska, R., Szilagy, E., Raka, L, … Brusaferro, S. (2017). Infection control capacity building in European countries with limited resources: issues and priorities. J Hosp Infect, 96(1), 85–88. https://doi.org/10.1016/J.JHIN.2016.12.024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Eduardo Rojas-Gutierrez declares that he has no conflict of interest. Diana Vilar-Compte declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Treatment and Prevention of Hospital Infections
Rights and permissions
About this article
Cite this article
Rojas-Gutierrez, E., Vilar-Compte, D. An Overview of Surgical Site Infection in Low- and Middle-Income Countries: the Role of Recent Guidelines, Limitations, and Possible Solutions. Curr Treat Options Infect Dis 11, 300–316 (2019). https://doi.org/10.1007/s40506-019-00198-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-019-00198-1