Opinion Statement
Prevention of Clostridium difficile infection (CDI) is a complex task; adequate and sustained success is difficult to obtain. Focus on prevention has to start by analyzing the targeted patient population; the most important risk factors for development of CDI are previous exposure to antibiotics, hospitalization and advanced age. Thus, limiting antibiotic exposure and over exposure with an antibiotic stewardship program that employs combined strategies reducing the number of doses and spectrum is essential. Reducing hospital exposure by ambulatory care and short-stay procedures aids in this task, but, when hospitalized, patients rely solely on healthcare personnel commitment to hand hygiene to reduce transport of spores, and on environmental staff for providing a safe environment by proper decontamination of hospital surfaces and equipment. Age as a risk factor is not modifiable, but what is modifiable is the environment where elderly patients are cared for, in which individual rooms and proper disposal of bed pans, diapers and toilet disinfection are fundamental. Using contact precautions limits dissemination of potential infecting spores by reducing carriage to uninfected patients on hands and clothes of healthcare personnel. Probiotics studies are continuously providing more robust information on their role in primary and secondary prevention and are now more frequently used in hospitals. Vaccination will play a strong role in the near future by targeting key patients who are likely to be continuously exposed to a healthcare environment. A summarized message and approach of this text is shown in Table 1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clostridium difficile infection is currently the most frequent hospital-acquired infection worldwide [1••]. The burden of the disease is estimated to be more than 400,000 healthcare-related cases and up to [2] community-acquired events. The spectrum of the disease is variable, ranging from mild diarrhea to toxic megacolon and death. Over the past 15 years, cases of CDI have been characterized for a more aggressive course and higher mortality primarily associated with the appearance of hypervirulent strains, mainly NAP1/027, which are characterized by the production of high quantities of toxins A and B [3]. Multiple risk factors for the development of CDI have been described, although the three most important ones are hospitalization, prior antibiotic use and advanced age. Antibiotics generate dysbiosis in the colon which favors C. difficile survival and pathogenesis. Advanced age has been linked to a more severe course and higher risk of death and hospitalization, favoring colonization that can be as high as 40%. The first step in the treatment of CDI is discontinuing any unnecessary antibiotics or reducing the spectrum, and starting targeted antibiotic treatment with metronidazole, vancomycin and fidaxomicin, although recurrences are reported to be as high as 20% [4•]. Patients with CDI produce spores before symptoms appear, and for weeks after treatment with adequate clinical response, so they are a continuous source of potential environmental contamination. Clostridium difficile differs from other nosocomial pathogens by producing spores that are highly resistant to temperature, humidity and common disinfectants. These characteristic makes eradication of C. difficile from hospital and long-term care facilities (LTCF) environments cumbersome [5••]. Hand hygiene with soap and water is preferred to alcohol-based disinfectant since alcohol favors sporulation. Chlorine and peroxide are to date the only environmental disinfectants with substantial evidence of their sporicidal activity; thus, they are recommended for hospital use and outbreak scenarios. Other methods of disinfection such as UV light are used in some areas. The objective of this review is to synthesize the information regarding key interventions for the control and possible eradication of C. difficile from healthcare environments.
Hand hygiene
The cornerstone for infection control in healthcare environments has been hand hygiene, although compliance with proper hand hygiene is frequently difficult to accomplish since many factors influence adherence [6, 7, 8••]. Healthcare workers’ (HCW) hands are the most important vehicle for a microorganism to spread among patients. Clostridium difficile spores have been found not to be restricted to the patient but to also be found in high-touch surface areas surrounding the patient and medical equipment [9,10,11,12]. Therefore it is not necessary for the HCW to have direct contact with the infected patients in order to acquire spores. Contamination of clothing and hands can be found in over 50% of HCW while attending patients with CDI, even after symptom resolution [13, 14••].
Over the years, hand hygiene has shifted towards a more frequent use of alcohol-based solutions (ABS) that are more practical and less time consuming, and their use has been associated with a reduction of infections caused by Gram-positive cocci; Hospital infection rates of methicillin-resistant Staphylococcus aureus (MRSA) were significantly lower when ABS had a higher volume of use [15]. In addition, when a switch from soap and water to ABS was done [16], a noticeable decrease in MRSA and vancomycin-resistant enteroccoci (VRE) was noticed, but none of the former studies showed reduction in CDI rates with this association. Conversely, ethanol is used for enhancement of cultures for C difficile [17], and spores from C. difficile are unyielding to ABS. Thus, the question remains: are these ABS associated with spore survival and subsequently with the increase in CDI cases? To date, there have been no clinical trials providing robust evidence that this asseveration is true [18]. Although soap and water use compared to ABS has repeatedly demonstrated to be more effective for spore removal in healthcare personnel [19, 20, 21••, 22], no increase in transmission from HCW to patients has been documented. Other antiseptics such as chlorhexidine have not shown advantages over soap for spore removal [23].
Antibiotic stewardship
A cornerstone for controlling healthcare-related infections is the adequate prescription of antibiotics during patient care. Previous receipt of antibiotics is the main risk factor for developing CDI and, although fluoroquinolones and clindamycin have been predominantly linked to many outbreaks, virtually every antibiotic has been associated with CDI. Furthermore, approximately half of the patients with CDI received inappropriate antimicrobial therapy [24].
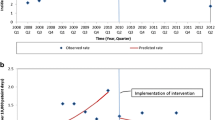
Restrictive strategies for antibiotics have been shown to have an association with the depletion of C. difficile burden in hospitals, showing a reduction in the CDI rate by up to 77% [25]. Fluoroquinolones restriction was associated with control of ribotype 027 strains in a multihospital outbreak [26]. Restriction of clindamycin has been shown to reduce rates of CDI in multiple hospital scenarios including medical wards, and has aided in the control of an outbreak in an orthopedic ward [27, 28]. Time series analysis showed that targeting reduction of four crucial antibiotics (clindamycin, ciprofloxacin, amoxacillin-clavulanate and cephalosporins) in large community hospitals was associated with a 68% reduction in hospital-acquired CDI and up to a 45% reduction in community-acquired CDI [29].
A meta-analysis reported the outcomes of several antibiotic stewardship programs (ASPs) that restricted exposure to certain high-risk antibiotics as a method for CDI prevention among hospitalized adult patients. The risk reduction in the rate of CDI was 52% (pooled risk ratio 0.48; 95% CI: 0.38–0.62), with the most significant protective effect for the acute geriatric wards and hip fracture surgery patients (56% reduction; pooled risk ratio 0.44; 95% CI: 0.35–0.56). Of note, when antimicrobial restrictive policies were compared to persuasive policies, only restrictive policies had a significant protective effect (pooled risk ratio 0.46; 95% CI: 0.38–0.56) [30••].
Antibiotic restrictive and non-restrictive approaches are not mutually exclusive, and on the majority of occasions these are combined. Prospective audit and feedback strategies are focused primarily on education providing sustained and prolonged results, and even when restrictive approaches are more useful in outbreak settings, both strategies are useful for CDI prevention [31].
Despite these encouraging results, only 52% of 398 surveyed hospitals in the U.S. reported regularly using their ASP to combat Clostridium difficile-associated disease [32].
Environmental cleaning and spore reduction
Spores of C. difficile have been found not to be restricted to the patient but have been isolated from the patient’s environment such as bed clothes and rails, toilets and nearby communal surfaces and nursing stations [33, 34].
Environmental contamination is a key factor for the transmission of C. difficile spores in healthcare settings. High levels of environmental contamination have been associated with CDI acquisition [35]. Adequate disinfection has been shown to decrease rates of C difficile infection, especially in wards where high environmental contamination with spores has been found [36]. In addition, medical devices such as portable bed commodes and electronic rectal thermometers have also been linked to transmission of C. difficile [37].
Clostridium difficile spores are not susceptible to the commonly used hospital disinfectants, such as phenolics and quaternary ammonium compounds, but they are inactivated by hypochlorites and peroxide. The use of hypochlorites for surface disinfection has been a key component of controlling outbreaks [38•, 39, 40]. Guidelines for the prevention of CDI suggest using a 1:10 dilution of sodium hypochlorite (household bleach) for environmental disinfection in outbreak settings and in settings of hyperendemicity, in addition to other infection prevention and control measures. [41]. Higher concentrations of chlorine within the range of 1000–5000 ppm have greater sporicidal activity than lower concentrations, but, due to their corrosive nature, high concentrations are limited for routine cleaning [40]. Chlorine-releasing agents have demonstrated the same effectiveness against newer methods of terminal disinfections, which is especially important when measuring the economic impact [42].
Dispersion of hydrogen peroxide by air is also used as a sporicidal agent [43]. When prospectively evaluated, hydrogen peroxide vapor room decontamination incidence of nosocomial CDI was significantly lower during the intervention than during the pre-intervention period (1.28 vs. 2.28 cases per 1,000 patient-days; P = .047).
In fact, sub-inhibitory concentrations of non-chlorine-based cleaning agents (detergent or hydrogen peroxide) significantly increased sporulation capacity; this effect was not seen with chlorine-based cleaning agents [44].
Regardless of the solution used for decontamination, inadequate training and wide variations in cleaning practices are the main obstacles for proper environmental control. [45]. Almost half of environmental surfaces were inadequately cleaned at baseline, and less than 15% of hospital environmental workers have the appropriate knowledge regarding the need for using bleach for C. difficile disinfection and contact duration for adequate disinfection [46]. Fluorescent and biological markers for terminal cleaning evaluation have aided in our understanding of cleaning thoroughness. Fluorescent markers are applied before cleaning and are assessed whether they were removed during cleaning; on the other hand, adenosine triphosphate (ATP) bioluminescence permits assessment of any remaining organic material after cleaning. However, despite using fluorescent or ATP bioluminescent markers, C. difficile is still frequently isolated in the environment. [47, 48]. Aside from the method used for environmental disinfection, every healthcare facility has to have its own operating procedure that needs to be frequently reassessed for adherence, along with continuous feedback to environmental workers. Also, ineffective cleaning may be due to insufficient time for cleaning, inadequate cleaning supplies, education, and poor communication [46].
Contact precautions
The hands of HCW are the main route for spore dissemination, frequently becoming contaminated with C. difficile spores during the routine care of individuals with CDI [49]. Contact precautions, individual rooms and individualized patient equipment are part of the isolation procedures used in patients with CDI or suspected CDI [50]. The adequate donning of gowns and gloves upon room entry and their removal before exiting may reduce transmission by focusing on the patient and the patient’s environment as the principal source of potential horizontal transmission [14••].
Improving availability of gloves and reminders for proper use has been shown to aid in reduction of infection rates, dropping from 7.7 to 1.5 per 1000 patient discharges [51]. Potential soiling of HCW clothing and subsequent dissemination is possible. Nurses’ clothing has been documented to become contaminated with C. difficile during a routine hospital shift, and although the study did not assess patient acquisition by this source, dissemination by clothes is feasible [52].
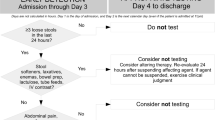
The duration of contact precautions is another important factor; current guidelines recommend continuous contact precautions until diarrhea resolution. In an outbreak setting, however, the spread of CDI is more difficult to control, and additional measures such as extending contact precautions until patient discharge, and empiric placement of patients in contact precautions while waiting for the results of C. difficile are important steps for the reduction of spore dissemination [50]. Delay in diagnosis is a big concern since the absence of prompt stool collection and of onsite laboratories may delay diagnosis and sometimes treatment; meanwhile, environmental contamination is occurring before the results of diagnostic tests for C. difficile are available [53]. Furthermore, environmental contamination with C. difficile continues to be found at the end of treatment in 14% of patients. Moreover, rebound in C. difficile colonization after a month was found in 56% of patients and environmental contamination found in 50% of rooms [14••, 54]. As a result, in the acute care setting, extended contact procedures have a role in preventing spore transmission. In LTCFs, implementation of some of this strategies is more cumbersome because of the long length of stay and the fact that these facilities try to provide a homelike environment with common areas, group therapy areas, etc. [55].
Isolation also includes medical equipment and devices that have to be disposable or need to be decontaminated before use; Single-use disposable thermometers compared with electronic thermometers reduce the likelihood of developing CDI (RR 0.44%; P = 0.026) [56]. Transfer of C. difficile by stethoscopes during simulation often seems to occur as well [57].
Probiotics as primary prevention
Maintaining microbiome homeostasis in the gut is fundamental for preventing C. difficile colonization and subsequent infections, and therefore many studies have looked at probiotics for this purpose.
A randomized trial investigated CDI incidence after administration of the probiotics lactobacilli and bifidobacteria in almost 3000 elderly patients and did not find any statistical reduction in CDI incidence. The rates in the probiotic and placebo groups were 0.8% and 1.2%, respectively; representing a relative risk associated with probiotic use of 0.71 with a 95% CI of 0.34–1.47 [58]. In a single-center, randomized, double-blind trial, Saccharomyces boulardii was not effective in preventing CDI compared to placebo (2.8% vs. 2%; OR 1.40, 95% CI 0.23–8.55) [59].
The longest study to date that has employed a combination of lactobacilli for hospital-wide prevention of CDI found a significant reduction in CDI rates after daily administration to all patients that were recipient of antibiotics. The study found a significant decrease in CDI rates from 18.0 cases per 10,000 patient-days, remaining at a mean level of 2.3 cases per 10,000 patient-days, which, compared to similar hospitals in the region, was significantly lower; furthermore, no complications were recorded after 10 years of daily administration [60•]. Compilation of results in a meta-analysis showed a favorable trend towards the prevention of CDI when probiotics are used [61,62,63]. One of those studies found that probiotics reduced the risk of CDI with a number needed to treat (NNT) of 29 (2% vs. 5.5%; RR 0.36, 95% CI 0.26–0.51) [64]. Another study reported that the risk reduction when probiotics were used persisted, whether the trials included adults or children, low or high doses of probiotics, or different probiotic species [65].
Patient placement, transferring and transition
Patient placement is also an important factor for acquiring C. difficile. Patients admitted to a room previously occupied by a patient with C. difficile have an increased risk for CDI [66]; in fact, the administration of antibiotics to the prior patients was associated with a 22% relative increased risk for the development of CDI in subsequent patients who occupied the same bed, meaning that antibiotics given to one patient may alter the local micro-environment influencing a different patient [67••].
A single room for CDI patients is preferred because it reduces the possibility of cross-contamination to other patients. When switched from double to single beds, patients in an ICU had a reduced rate for C. difficile acquisition 43% (95% CI, 7–65%) and a combined reduction of 54% (95% CI, 29–70%) when MRSA and VRE were taken into account. [68]. Cohorting patients is a strategy that should only be used when the hospital epidemiological condition leaves no other choice, since studies of the efficacy of these approaches exist in the outbreak setting, while no studies have shown that cohorting for endemic CDI is useful. On the other hand, cohorting can lead to up to 4 times more recurrence of CDI, probably due to reinfection [69].
Other factors such as adequate access to hand hygiene facilities are important for compliance and should be taken into account when deciding room accommodation [70••].
Transitions and transferring of patients are events that can lead to spore dissemination. Patients in long-term care or in nursing homes require multiple assistance during routine care and often have shared-space activities with other patients as part of their daily routine. Transferring a CDI patient to another ward or to routine procedures such as X-rays, endoscopy or to the operating room requires adequate communication in order to have a correct hand-over and to minimize risks, the more so when transfer is to another hospital. Regrettably, care transitions are often inadequately coordinated. Suboptimal communication is a major barrier to implementing appropriate prevention procedures [55]. Patients should be placed preferably in a single bedroom; when this is not possible, cohorting of CDI patients is recommended, while both patients and rooms must be effectively cleaned and disinfected before receiving the next patient.
Identifying asymptomatic carriers and treatment
When universal screening is performed on all hospitalized patients searching for asymptomatic carriers, one study showed that CDI was almost 2 times higher in patients exposed to asymptomatic carriers than in non-exposed patients (2.6% vs. 4.6% OR 1.79; 95% CI, 1.16-2.76) [71•].
Using multilocus variable number of tandem repeats analysis (MLVA), one study showed that out of 56 hospital-acquired cases of CDI, 17 (30%) were associated with other CDI patients, whereas 16 (29%) were associated with asymptomatic carriers. Asymptomatic carriers appear to play an important role in transmission. Identification and isolation of carriers may be necessary to further transmission reduction of C. difficile in such settings [72].
Treatment for asymptomatic C. difficile carriers was studied [73], with the absence of positive cultures after oral vancomycin therapy in 9 out of 10 patients, compared to 3 out of 10 patients treated by oral metronidazole (P = 0.02) and 2 out of 10 patients treated with placebo (P = 0.005). Nevertheless, within an average of 20 days after completing treatment, 8 out of 9 patients with transient clearance of fecal C. difficile carriage had positive cultures. Thus, there is no adequate evidence to support therapy in the routine management of fecal colonization by C. difficile.
Vaccines
Effective vaccination against nosocomial pathogens is imperative; currently, there are no FDA-approved vaccines that prevent infections acquired during medical care. Research for a C. difficile vaccine and development are underway.
Naturally occurring toxin A IgG antibodies seem to reduce recurrence [74]. In an animal study, previous toxoid B administration was effective in preventing disease occurrence after a challenge with toxigenic strains [75].
There is currently a phase 2 trial assessing the safety, tolerability and immunogenicity of a potential vaccine as well as a phase 3 trial which will assess the prevention of symptomatic PCR-confirmed primary CDI cases after 2 and 3 vaccine doses from 2 different pharmaceutical companies [76, 77•]. Based on different vaccination schemes, transmission modeling estimates that, when high-risk groups of patients are vaccinated around a 43% reduction in CDI cases is expected [78].
Conclusions
Difficile derives from Latin meaning “difficult” or “hard to deal with”, and in the sense of Clostridium difficile infection this is true for diagnosis since its anaerobic needs are complex. It is difficult to treat since it recurs often, but the same difficulty also applies to prevention on the basis that there is no single reliable strategy for the purpose of preventing Clostridium difficile infection. A quite of options for prevention has to be ensured for hospitalized patients in acute care or in long-term care, as well as a tailored approach for every institution. The backbone for prevention is composed of: adequate hand hygiene, a solid antibiotic stewardship program, continuous reinforcement of contact precautions, supervised environmental disinfection, and subsequently adding strategies such as probiotics, patient placement and, ultimately, vaccination.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Weiner LM, Fridkin SK, Aponte-Torres Z, et al. Vital signs: preventing antibiotic-resistant infections in hospitals - United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:235–41. Arecent article which addresses an extremely important issue.
Lessa FC, Winston LG, McDonald LC, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:2369–70.
McDonald LC, Killgore GE, Thompson A, Owens Jr RC, Kazakova SV, Sambol SP, et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353:2433–41.
• Soriano MM, Johnson S. Treatment of Clostridium difficile infections. Infect Dis Clin North Am. 2015;29:93–108. C. difficile is a common infection in hospital settings and it is important for physicians to be updated on its treatment.
•• Loo VG. Environmental interventions to control Clostridium difficile. Infect Dis Clin North Am. 2015;29:83–91. A recent article which addresses not only the already known medical treatment but also brings information regarding environmental interventions which are equally important, since they aim for prevention.
Sánchez-Carrillo LA, Rodríguez-López JM, Galarza-Delgado DÁ, Baena-Trejo L, Padilla-Orozco M, Mendoza-Flores L, et al. Enhancement of hand hygiene compliance among health care workers from a hemodialysis unit using video-monitoring feedback. Am J Infect Control. 2016;44:868–72.
Zellmer C, Blakney R, Van Hoof S, Safdar N. Impact of sink location on hand hygiene compliance for Clostridium difficile infection. Am J Infect Control. 2015;43(4):387–9. doi:10.1016/j.ajic.2014.12.016.
•• Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect. 2016;92(4):309–20. doi:10.1016/j.jhin.2015.11.012. Review. An updated report which emphasizes the importance of hand hygiene where compliance from the healthcare workers (nurses, medical staff) is still lacking.
Marinella MA, Pierson C, Chenoweth C. The stethoscope. a potential source of healthcare-associated infection? Arch Intern Med. 1997;157:786–90.
Manian FA, Meyer L, Jenne J. Clostridium difficile contamination of blood pressure cuff s: a call for a closer look at gloving practices in the era of universal precautions. Infect Control Hosp Epidemiol. 1996;17:180–2.
Kim KH, Fekety R, Batts DH, et al. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis. 1981;143:42–50.
Brooks SE, Veal RO, Kramer M, et al. Reduction in the incidence of Clostridium difficile-associated diarrhea in an acute care hospital and a skilled nursing facility following replacement of electronic thermometers with single-use disposables. Infect Control Hosp Epidemiol. 1992;13:98–103.
Guerrero DM, Becker JC, Eckstein EC, Kundrapu S, Deshpande A, Sethi AK, et al. Asymptomatic carriage of toxigenic Clostridium difficile by hospitalized patients. J Hosp Infect. 2013;85(2):155–8. doi:10.1016/j.jhin.2013.07.002.
•• Shrestha SK, Sunkesula VC, Kundrapu S, et al. Acquisition of Clostridium difficile on hands of healthcare personnel caring for patients with resolved C. difficile infection. Infect Control Hosp Epidemiol. 2016;37(4):475–7. Further reference to a very important issue, hand hygiene, explaining how healthcare personnel are often responsible for CDI among patients and again how to prevent it.
Kaier K, Hagist C, Frank U, Conrad A, Meyer E. Two time-series analyses of the impact of antibiotic consumption and alcohol-based hand disinfection on the incidences of nosocomial methicillin-resistant Staphylococcus aureus infection and Clostridium difficile infection. Infect Control Hosp Epidemiol. 2009;30(4):346–53. doi:10.1086/596605.
Gordin FM, Schultz ME, Huber RA, Gill JA. Reduction in nosocomial transmission of drug-resistant bacteria after introduction of an alcohol-based handrub. Infect Control Hosp Epidemiol. 2005;26(7):650–3.
Clabots CR, Bettin KM, Peterson LR, Gerding DN. Evaluation of cycloserine-cefoxitin-fructose agar and cycloserine-cefoxitin-fructose broth for recovery of Clostridium difficile from environmental sites. J Clin Microbiol. 1991;29(11):2633–5.
Boyce JM. Update on hand hygiene. Am J Infect Control. 2013;41(5 Suppl):S94–6. doi:10.1016/j.ajic.2012.11.008.
Jabbar U, Leischner J, Kasper D, Gerber R, Sambol SP, Parada JP, et al. Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol. 2010;31(6):565–70. doi:10.1086/652772.
Kundrapu S, Sunkesula V, Jury I, Deshpande A, Donskey CJ. A randomized trial of soap and water hand wash versus alcohol hand rub for removal of Clostridium difficile spores from hands of patients. Infect Control Hosp Epidemiol. 2014;35(2):204–6. doi:10.1086/674859.
•• Oughton MT, Loo VG, Dendukuri N, Fenn S, Libman MD. Hand hygiene with soap and water is superior to alcohol rub and antiseptic wipes for removal of Clostridium difficile. Infect Control Hosp Epidemiol. 2009;30(10):939–44. doi:10.1086/605322. It is important for healthcare personnel to know the difference between hand hygiene products when it comes to C. difficile, since a difference between the products has been shown.
Edmonds SL, Zapka C, Kasper D, Gerber R, McCormack R, Macinga D, et al. Effectiveness of hand hygiene for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol. 2013;34(3):302–5. doi:10.1086/669521.
Bettin K, Clabots C, Mathie P, Willard K, Gerding DN. Effectiveness of liquid soap vs. chlorhexidine gluconate for the removal of Clostridium difficile from bare hands and gloved hands. Infect Control Hosp Epidemiol. 1994;15(11):697–702.
Bui C, Zhu E, Donnelley MA, Wilson MD, Morita M, Cohen SH, et al. Antimicrobial stewardship programs that target only high-cost, broad-spectrum antimicrobials miss opportunities to reduce Clostridium difficile infections. Am J Infect Control. 2016;44:1684–6.
Dancer SJ, Kirkpatrick P, Corcoran DS, Christison F, Farmer D, Robertson C. Approaching zero: temporal effects of a restrictive antibiotic policy on hospital-acquired Clostridium difficile, extended-spectrum beta-lactamase-producing coliforms and meticillin-resistant Staphylococcus aureus. Int J Antimicrob Agents. 2013;41:137–42.
Aldeyab MA, Devine MJ, Flanagan P, et al. Multihospital outbreak of Clostridium difficile ribotype 027 infection: epidemiology and analysis of control measures. Infect Control Hosp Epidemiol. 2011;32(3):210–9.
Pear SM, Williamson TH, Bettin KM, et al. Decrease in nosocomial Clostridium difficile-associated diarrhea by restricting clindamycin use. Ann Intern Med. 1994;120(4):272–7.
Cruz-Rodríguez NC, Hernández-García R, Salinas-Caballero AG, Pérez-Rodríguez E, Garza-González E, Camacho-Ortiz A. The effect of pharmacy restriction of clindamycin on Clostridium difficile infection rates in an orthopedics ward. Am J Infect Control. 2014;42(6):e71–3. doi:10.1016/j.ajic.2014.02.018.
Lawes T, Lopez-Lozano JM, Nebot CA, Macartney G, Subbarao-Sharma R, Wares KD, Sinclair C, Gould IM. Effect of a national 4C antibiotic stewardship intervention on the clinical and molecular epidemiology of Clostridium difficile infections in a region of Scotland: a non-linear time-series analysis. Lancet Infect Dis. 2016; 4. doi: 10.1016/S1473-3099(16)30397-8.
•• Feazel LM, Malhotra A, Perencevich EN, Kaboli P, Diekema DJ, Schweizer ML. Effect of antibiotic stewardship programs on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother. 2014;69:1748–54. It is imperative for healthcare personnel to know and implement antibiotic stewardship programs in their own facilities to reduce not only CDI but also other antibiotic usage complications.
Wenzler E, Mulugeta SG, Danziger LH. The antimicrobial stewardship approach to combating clostridium difficile. Antibiotics (Basel). 2015;4(2):198–215. doi:10.3390/antibiotics4020198.
Saint S, Fowler KE, Krein SL, Ratz D, Flanders SA, Dubberke ER, et al. Clostridium difficile Infection in the United States: a national study assessing preventive practices used and perceptions of practice evidence. Infect Control Hosp Epidemiol. 2015. doi:10.1017/ice.2015.81.
Best EL, Sandoe JA, Wilcox MH. Best Potential for aerosolization of Clostridium difficile after flushing toilets: the role of toilet lids in reducing environmental contamination risk. J Hosp Infect. 2012;80(1):1–5. doi:10.1016/j.jhin.2011.08.010.
Best EL, Fawley WN, Parnell P, Wilcox MH. The potential for airborne dispersal of Clostridium difficile from symptomatic patients. Clin Infect Dis. 2010;50(11):1450–7. doi:10.1086/652648.
Fawley WN, Parnell P, Verity P, Freeman J, Wilcox MH. Molecular epidemiology of endemic Clostridium difficile infection and the significance of subtypes of the United Kingdom epidemic strain. J Clin Microbiol. 2005;43:2685–96.
Wilcox MH, Fawley WN, Wigglesworth N, Parnell P, Verity P, Freemen J. Comparison of the effect of detergent versus hypochlorite cleaning of environmental contamination and incidence of Clostridium difficile infection. J Hosp Infect. 2003;54:109–14.
Brooks S, Khan A, Stoica D, Griffith J, Friedeman L, Mukherji R, et al. Reduction in vancomycin-resistant Enterococcus and Clostridium difficile infections following change to tympanic thermometers. Infect Control Hosp Epidemiol. 1998;19(5):333–6.
• Weber DJ, Rutala WA, Miller MB, Huslage K, Sickbert-Bennett E. Role of hospital surfaces in the transmission of emerging health care-associated pathogens: norovirus, Clostridium difficile, and Acinetobacter species. Am J Infect Control. 2010;38:S25–33. Proper facilities’ cleaning is imperative and is not often taken into account as the culprit for the transmission of health care-associated pathogens; therefore, prompt and updated information and knowledge is needed.
Rutala WA, Gergen MF, Tande BM, Weber DJ. Room decontamination using an ultraviolet-C device with short ultraviolet exposure time. Infect Control Hosp Epidemiol. 2014;35(8):1070–2. doi:10.1086/677149.
Rutala WA, Weber DJ. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin Microbiol Rev. 1997;10(4):597–610.
Dubberke ER, Gerding DN, Classen D, et al. Strategies to prevent clostridium difficile infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29 Suppl 1:S81–92.
Doan L, Forrest H, Fakis A, Craig J, Claxton L, Khare M. Clinical and cost effectiveness of eight disinfection methods for terminal disinfection of hospital isolation rooms contaminated with Clostridium difficile 027. J Hosp Infect. 2012;82:114–21.
Boyce JM, Havill NL, Otter JA, et al. Impact of hydrogen peroxide vapor room decontamination on Clostridium difficile environmental contamination and transmission in a healthcare setting. Infect Control Hosp Epidemiol. 2008;29:723–9.
Wilcox MH. Hospital disinfectants and spore formation by Clostridium difficile. Lancet. 2006;356:1324.
Boyce JM, Havill NL, Lipka A, Havill H, Rizvani R. Variations in hospital daily cleaning practices. Infect Control Hosp Epidemiol. 2010;31(1):99–101. doi:10.1086/649225.
Jennings A, Sitzlar B, Jury L. A survey of environmental service workers’ knowledge and opinions regarding environmental cleaning. Am J Infect Control. 2013;41(2):177–9.
Boyce JM, Havill HL, et al. Comparison of fluorescent marker systems with 2 quantitative methods of assessing terminal cleaning practices. Infect Control Hosp Epidemiol. 2011;32(12):1187–93.
Deshpande A, Sitzlar B, Fertelli D, et al. Utility of an adenosine triphosphate bioluminescence assay to evaluate disinfection of Clostridium difficile isolation rooms. Infect Control Hosp Epidemiol. 2013;34(8):865–7.
Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Brun-Buisson C. Contamination of healthcare workers' hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10–5. doi:10.1086/674396.
Dubberke ER, Carling P, Carrico R, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(6):628–45.
Johnson S, Gerding DN, Olson MM, et al. Prospective, controlled study of vinyl glove use to interrupt Clostridium difficile nosocomial transmission. Am J Med. 1990;88(2):137–40.
Perry C, Marshall R, Jones E. Bacterial contamination of uniforms. J Hosp Infect. 2001;48(3):238–41.
Sunkesula VC, Kundrapu S, Jury LA, et al. Potential for transmission of spores by patients awaiting laboratory testing to confirm suspected Clostridium difficile infection. Infect Control Hosp Epidemiol. 2013;34(3):306–8.
Sethi AK, Al-Nassir WN, Nerandzic MM, et al. Persistence of skin contamination and environmental shedding of Clostridium difficile during and after treatment of C. difficile infection. Infect Control Hosp Epidemiol. 2010;31(1):21–7.
Ye Z, Mukamel DB, Huang SS, et al. Healthcare-associated pathogens and nursing home policies and practices: results from a national survey. Infect Control Hosp Epidemiol. 2015;36(7):759–66.
Jernigan JA, Siegman-Igra Y, Guerrant RC, et al. A randomized crossover study of disposable thermometers for prevention of Clostridium difficile and other nosocomial infections. Infect Control Hosp Epidemiol. 1998;19(7):494–9.
Vajravelu RK, Guerrero DM, Jury LA, et al. Evaluation of stethoscopes as vectors of Clostridium difficile and methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol. 2012;33(1):96–8.
Allen SJ, Wareham K, Wang D, et al. Lactobacilli and bifidobacteria in the prevention of antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in older inpatients (PLACIDE): a randomized, double-blind, placebo-controlled, multicenter trial. Lancet. 2013;382(9900):1249–57.
Pozzoni P, Riva A, Bellatorre AG, et al. Saccharomyces boulardii for the prevention of antibiotic-associated diarrhea in adult hospitalized patients: a single-center, randomized, double-blind, placebo-controlled trial. Am J Gastroenterol. 2012;107:922–31.
• Maziade PJ, Pereira P, Goldstein EJ. A decade of experience in primary prevention of clostridium difficile infection at a community hospital using the probiotic combination lactobacillus acidophilus CL1285, Lactobacillus casei LBC80R, and Lactobacillus rhamnosus CLR2 (Bio-K+). Clin Infect Dis. 2015 ;60 (Suppl 2):S144-7. doi: 10.1093/cid/civ178. This is important since it is a relatively recent prophylactic treatment.
Hempel S, Newberry SJ, Maher AR, et al. Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis. JAMA. 2012;307:1959–69.
Videlock EJ, Cremonini F. Meta-analysis: probiotics in antibiotic- associated diarrhoea. Aliment Pharmacol Ther. 2012;35:1355–69.
Johnston BC, Ma SS, Goldenberg JZ, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Ann Intern Med. 2012;157:878–88.
Goldenberg JZ, Ma SS, Saxton JD, et al. Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children. Cochrane Database Syst Rev. 2013;5, CD006095.
Pattani R, Palda VA, Hwang SW, Shah PS. Probiotics for the prevention of antibiotic-associated diarrhea and Clostridium difficile infection among hospitalized patients: systematic review and meta-analysis. Open Med. 2013;7:e56–67.
Shaughnessy MK, Micielli RL, DePestel DD, Arndt J, Strachan CL, Welch KB, et al. Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Infect Control Hosp Epidemiol. 2011;32(3):201–6. doi:10.1086/658669.
•• Freedberg DE, Salmasian H, Cohen B, Abrams JA, Larson EL. Receipt of antibiotics in hospitalized patients and risk for clostridium difficile. infection in subsequent patients who occupy the same bed. JAMA Intern Med. 2016;176(12):1801–8. doi:10.1001/jamainternmed.2016.6193. A recent article which provides new information concerning a different risk factor for CDI.
Teltsch DY, Hanley J, Loo VG, et al. Infection acquisition following intensive care unit room privatization. Arch Intern Med. 2011;171(1):32–8.
Islam J, Cheek E, Navani V, et al. Influence of cohorting patients with Clostridium difficile infection on risk of symptomatic recurrence. J Hosp Infect. 2013;85(1):17–21.
•• Deyneko A, Cordeiro F, Berlin L, Ben-David D, Perna S, Longtin Y. Impact of sink location on hand hygiene compliance after care of patients with Clostridium difficile infection: a cross-sectional study. BMC Infect Dis. 2016;16:203. doi:10.1186/s12879-016-1535-x. It is relevant to know sink placement for enhanced hand hygiene compliance.
• Blixt T, Gradel KO, Homann C, Seidelin JB, Schønning K, Lester A, et al. Asymptomatic carriers contribute to nosocomial Clostridium difficile infection: a cohort study of 4508 patients. Gastroenterology. 2017. doi:10.1053/j.gastro.2016.12.035. Relevant for screening patients.
Curry SR, Muto CA, Schlackman JL, Pasculle AW, Shutt KA, Marsh JW, et al. Use of multilocus variable number of tandem repeats analysis genotyping to determine the role of asymptomatic carriers in Clostridium difficile transmission. Clin Infect Dis. 2013;57(8):1094–102.
Johnson S, Homann SR, Bettin KM, Quick JN, Clabots CR, Peterson LR, et al. Treatment of asymptomatic Clostridium difficile carriers (fecal excretors) with vancomycin or metronidazole. A randomized, placebo-controlled trial. Ann Intern Med 1992;117:297e302. Clin Infect Dis. 2013;57(8):1094–102. doi:10.1093/cid/cit475.
Kyne L, Warny M, Qamar A, et al. Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhoea. Lancet. 2001;357(9251):189–93.
Siddiqui F, O’Connor JR, Nagaro K, et al. Vaccination with parenteral toxoid B protects hamsters against lethal challenge with toxin A-negative, toxin B-positive clostridium difficile, but does not prevent colonization. J Infect Dis. 2012;205(1):128–33.
A Study To Investigate A Clostridium Difficile Vaccine In Healthy Adults Aged 50 to 85 Years, Who Will Each Receive 3 Doses Of Vaccine. Available at https://clinicaltrials.gov/ct2/show/NCT02117570. Accessed January 9 2017
• Study of a Candidate Clostridium difficile Toxoid Vaccine (Cdiffense) in Subjects at Risk for C. difficile Infection. 2013. Available at: https://clinicaltrials.gov/ct2/show/NCT01887912. Accessed January 9 2017. It is relevant to know that new prevention measures are being developed.
van Kleef E, Deeny SR, Jit M, Cookson B, Goldenberg SD, Edmunds WJ. Robotham JV7.The projected effectiveness of Clostridium difficile vaccination as part of an integrated infection control strategy. Vaccine. 2016;34(46):5562–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors Adrián Camacho-Ortiz and Susana Chávez-Moreno declare having no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Treatment and Prevention of Hospital Infections
Rights and permissions
About this article
Cite this article
Camacho-Ortiz, A., Chavez-Moreno, S. Pearls in Infection Control for Clostridium difficile Infections in Healthcare Facilities. Curr Treat Options Infect Dis 9, 117–128 (2017). https://doi.org/10.1007/s40506-017-0114-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-017-0114-z