Abstract
Purpose of Review
Sequestration of Plasmodium-infected cells in the placenta causes significant adverse effects on mothers and their fetuses. With progress in understanding placental malaria and associated adverse consequences, this review addresses the situation in an area with high prevalence, in Blue Nile State, Sudan, where protective interventions are not adequately provided.
Recent Findings
Several studies have confirmed that malaria infection during pregnancy with parasites in the placenta, even at sub-patent level detected by molecular techniques, can result in maternal morbidity, fetal growth restriction, and reduced birth weight. Thus, malaria protection measures and antenatal care are vital for pregnant women in endemic areas.
Summary
Falciparum and vivax-infected erythrocytes are able to sequester in the placenta and not easily detected in peripheral blood during antenatal period. Recently, several biological biomarkers associated with malaria infection during pregnancy were detected. Such biomarkers could be used as indicators for identifying women at risk of placental infection complications, particularly when pre-eclampsia may occur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria remains a major health problem in endemic areas among children and pregnant women. Between 2015 and 2017, the global number of malaria cases increased from 211 million to 219 million and is related to an increase in deaths [1]. It has been estimated that 200,000 infants and 10,000 maternal deaths occur per year in Africa caused by malaria-related morbidity [2]. Pregnant women are more susceptible to Plasmodium infections than the general population with 2- to 3-fold increased risk of malaria infection [1, 3, 4], due to hormonal alterations [5], pregnancy-related immune suppression, and cell sequestration in the placenta [6, 7]. In addition, there is increased attractiveness of pregnant women to mosquitoes due to increased abdomen temperature [8, 9]. Among the five known Plasmodium species that infect humans, only Plasmodium falciparum (P. falciparum) and Plasmodium vivax (P. vivax) have been linked with pregnancy-associated malaria (PAM) resulting in placental malaria (PM) with pronounced maternal and fetal health consequences. PM increases the risk of maternal anemia, pregnancy loss, and low birth weight (LBW) (defined as birth weight < 2500 g) which is related to a high risk for infant death [10,11,12]. Different mechanisms are alleged to be tangled depending on the infecting species [13, 14].
This review provides an overview about the mechanisms by which placental infections by Plasmodium species could lead to adverse pregnancy outcomes and consequences in the fetus and during childhood. It also attempts to highlight the situation in a neglected area, i.e., Blue Nile State, Sudan, with a high seasonal malaria transmission, and discusses how the use of the host biomarkers as indicator for PM can guide control strategies for optimizing the malaria prevention and intervention measures so as to minimize the consequence of placental sequestration that results in poor birth outcomes.
Burden of Placental Plasmodium Infections
Placental malaria is more common in areas where malaria is endemic [15,16,17,18], and almost exclusively due to P. falciparum which is the most prevalent and virulent human malaria species, in sub-Saharan Africa [17,18,19], while the burden of P. vivax is significant in the regions of the South East Asia and South America [20, 21].
It has been documented that nearly a third of 10,032 women enrolled without evidence of malaria infection at delivery time for 20 studies conducted in nine sub-Saharan African countries were infected with PM [18], and prevalence of 26.5% and 38% for PM was reported in East and Southern Africa and West and Central Africa, respectively [15, 22]. The median proportion of women with PM has been estimated at 11% in the Asia-Pacific region [23], and 26% prevalence of PM has been found using PCR in Colombia [24], and was an important contributor to maternal mortality in Thailand [25].
Moreover, the prevalence and severity of PM are affected by malaria transmission intensity, geographical region and socio-economic situation of populations, highest in rural ones, and the use of malaria prevention tools [16, 17]. In areas of high malaria transmission, the prevalence of PM is highest in young primigravidae women as they lack the placental parasite-specific immunity which develop with subsequent pregnancies [7, 19, 26], while women of all gravidities are susceptible to symptomatic and severe maternal disease associated with adverse outcomes in low transmission areas [27, 28]. Furthermore, the susceptibility to PM infection increases in women with HIV infection compared with healthy ones [29, 30].
In the case of P. falciparum, the placenta provides an ideal environment for the development of a subpopulation of malaria parasites capable of sequestration in infected erythrocytes (IEs), hemozoin deposition in the intervillous space of the placenta, and leads to placental pathophysiological changes [31,32,33]. Although P. vivax was not considered to sequester in the microcirculation and placental inflammation was not observed [14], recent studies showed that P. vivax-infected erythrocytes (PvIE) do have the potential to cyto-adhere to glycosaminoglycans and may contribute to the pathophysiological effect of vivax malaria in pregnancy [21, 34]. Likewise, P. chabaudi infection was reported to lead to poor pregnancy outcomes in B6 mice as a result of accumulation of IEs in the placenta [35].
Detection of Placental Plasmodium Infections
Diagnosis of Plasmodium infections during pregnancy remains challenging due to sequestration of the mature parasites or parasite products such as hemozoin in the placenta, while circulating at low-density levels in peripheral blood which do not correlate with the infection in the placenta [10, 36, 37]. Although light microscopy remains the standard of practice for malaria diagnosis in clinical settings, microscopy of peripheral blood films fails to identify a considerable proportion of placental infections [13, 37, 38]. Even though placental histology can diagnose active on past PM infections by detecting the malaria pigment hemozoin within fibrin [31, 39, 40], when taken as a reference test for P. falciparum infections, lower sensitivity was reported compared with peripheral microscopy [41]. Additionally, performing placental histology examination is costly and its use is possible only for research studies. However, sensitive diagnostic methods are needed to assess placental malaria before delivery for both clinical and epidemiological reasons. Alternatives to light microscopy include rapid diagnostic tests (RDTs), which are easy to use and have facilitated access to malaria diagnosis outside health facilities in peripheral communities. Nonetheless, sensitivity of conventional RDTs in pregnant women ranges between 78 and 95% if compared with placental blood microscopy as reference standard and between 57 and 81% if compared with placental thick smear histology [41, 42]. Furthermore, RDTs cannot detect the low-level blood stage malaria infections that can otherwise be identified by molecular methods [41, 43], such as nucleic acid amplification techniques, e.g., loop-mediated isothermal amplification (LAMP) that displays similar sensitivity to PCR (down to one parasite/μl of blood) and is an optimal alternative to PCR-based tests for screening malaria in peripheral and placental blood as it can be relatively easily deployed outside reference laboratories [44]. Although molecular detection methods of Plasmodium have been shown to be sensitive in detecting low-level parasitemia and sub-microscopic infections associated with LBW [14, 44,45,46] and maternal anemia at delivery for P. falciparum [47] and P. vivax infections [43, 48], its operational limitations such as the demand for high technical expertise and the high cost drive for the need of other diagnostic methods to increase proportion detection of placental infection before delivery.
Placental Changes Associated with Plasmodium Infections
The crucial experience underlying PM pathogenesis is the sequestration of IEs and immune cell infiltrates in the placental syncytiotrophoblasts triggering an inflammatory reaction known as intervillitis [6, 18, 36, 49]. This inflammation is mediated by parasite expression of a pregnancy-specific variant surface antigen (VAR2CSA) coded for by the var2csa gene, which appears only in pregnancy on the red blood cell surface and is capable of binding to the placental target chondroitin sulfate A (CSA) existing in the intervillous spaces [16, 50,51,52].
Placental changes associated with PM have been documented for stable and unstable malaria transmission settings [33] and for both P. falciparum and P. vivax. It is well known that the sequestration of P. falciparum-infected erythrocytes (PfIE) has been shown to contribute to a high rate of severe PM [6, 7, 17, 37, 53]. Some evidences currently support that PvIE also undergo cyto-adherence events [21, 54] to induce PM associated with maternal anemia and fetal LBW [23, 55, 56], while no placental changes are reported in other species.
Placental inflammation and damage as a result of IE sequestration can lead to thickening of the trophoblast layer syncytial knotting and fibrinoid deposits [39], decreased in placental weight [57], focal necrosis fibrin deposition, and clumping of syncytiotrophoblast cells, reduction of their microvilli basal membrane, and lesions [31, 37]. Sequestration of P. falciparum expressing VAR2CSA in the immune-privileged placenta favors parasite survival as a result of evasion to any previously acquired immunity [6, 58, 59]. In highly endemic areas, where women are assumed to have protection from the sever syndrome and to acquire IgG-mediated protective immunity directed against the pregnancy-specific target VAR2CSA [51, 59], the frequency and severity of the infection are highest in women in their first and second pregnancies because they lack the acquired immunity to parasites expressing this specific variant surface antigen [33, 49, 58]. Moreover, the levels of anti-VAR2CSA-specific IgGs increase with parity and are associated with encouraging pregnancy outcome [51].
IE binding promotes intense infiltration of immune cells in the intervillous spaces and shifts the balance between Th1/Th2 immune responses toward the Th1 pathway resulting in an important pro-inflammatory cytokine production and attraction of mononuclear inflammatory cells necessary to parasite elimination but disturbing the immunological balance both in the peripheral and in the placental blood [17, 37, 60]. Elevated levels of pro-inflammatory cytokines, such as IFN-γ, IL-2, TNF-α, and IL-6 in the peripheral and/or placental blood of malaria-infected primigravidae, are responsible for the observed placental pathology and adverse pregnancy outcomes [58, 60, 61]. Moreover, the accumulation of the maternal immune cells with increased levels of inflammatory cytokines may trigger a local immune response at the maternal-fetal zone in the placenta [62] and affect maternal-fetal transfer of nutrients, oxygen, and waste products by mechanical blockage and inflammatory cells [40, 63]. Furthermore, high levels of parasitemia and chronic parasite infection in the placental intervillous space can lead to consumption of nutritive blood substances due to slow and small venous flow which affect the nutrient transport function of the placenta [64], which leads to increased rates of maternal morbidity which results in a worsening of perinatal outcomes and death [65].
Additionally, inflammation and abnormal utero-placental blood flow in the placenta have been associated with fetal growth restriction [53, 66], maternal anemia [13, 67], and with reduced birth weight [68, 69]. Walker and colleagues [70], using modeling studies, reported that high proportions of placental infections might have been started by the end of the first trimester, and in the absence of malaria prevention methods such as intermittent preventive treatment (IPTp), placental inflammation might begin in early pregnancy and persist for months. Although cumulative evidence shows that at least some women remain at increased risk of malaria infection following delivery [19, 71], peripheral parasitemia is commonly cleared naturally within 1–2 days of delivery [7].
Consequences of PM in the Fetus and During Childhood
Published data has demonstrated perinatal complications associated with PAM and PM in the fetus which involved abortion and still birth [68], IUGR, premature delivery, and LBW [23, 53] which is indirectly associated with increased infant morbidity and mortality in Africa [7, 72]. Although it is still unclear what are the reasons that affect fetal growth and the exact period of infection during pregnancy is the most harmful for the growth, in utero infection has been related to stillbirth [7], and infections in the first or second trimester lead to an increased risk of LBW in some studies [53, 73, 74]. Moreover, PM increases the risk of vertical transmission of Plasmodium parasite from maternal circulation through the placenta into fetal circulation and result in congenital malaria [75, 76], which can contribute to infant morbidity and mortality [77].
PM has also been linked with the high burden of infant and childhood malaria [78] and with the risk of fetal and infant anemia [37]. Moreover, exposure of the immature fetus to malaria parasite antigens transmitted across the placenta during pregnancy can lead to an alteration of immune development of the fetus [79], resulting in a malaria-specific immuno-tolerant phenotype in the infant due to induction of protection prior to primary natural infection which may affect malaria vaccine immunogenicity [80]. Furthermore, in utero immune experience can affect transplacental transference of antibodies to antigens of other pathogens such as measles, Streptococcus pneumonia, and tetanus [7, 81, 82] and may increase the risk of congenital cytomegalovirus infections [83].
It has been documented that in utero variations in nutrient transfer from mother to child are associated to reduced birth weight, ultimately increased rates of cardiovascular disease, type 2 diabetes, and osteoporosis later in life [84], Moreover, PAM and PM may mediate neuropathology via immune activation and inflammation in the placenta [85].
Use of Host Biomarkers as Indicator of PM
Despite the contradicting findings for the association between PM and the risk for hypertension and pre-eclampsia reported [65, 86, 87], several biomarkers indicative of placenta dysfunction that may indicate PM have been studied to differentiate from pre-eclampsia which shares numerous pathophysiological features with placental malaria [42, 88]. Moreover, sequestered PfIEs and monocytes in the placenta induce inflammation and dysregulated angiogenesis offering the possibility of detecting pro- and anti-inflammatory molecules and angiogenic factors such as soluble fms-like tyrosine kinase-1 (sFLT1) or soluble endoglin (sEng) involved in blood vessel remodeling in peripheral and placental blood [62] and has a role in preterm birth, LBW, and perinatal death [65]. Elevation of plasma sEng levels has been shown to precede the onset of pre-eclampsia [89]; its elevated circulating concentrations have been associated with PM and increased severity of malaria infection in children in Gabon [90]. Angiopoietins (ANG-1 and ANG-2) are critical regulators of vascular development, which were reported to be clinically informative biomarkers for cerebral malaria in children [91, 92]. They are also disrupted by the sequestered PfIEs resulting in placental various histopathological changes associated with poor pregnancy outcomes and the inability of the placenta to support rapid fetal growth in the third trimester, ultimately leading to LBW [93]. Moreover, complement component factor 5, particularly C5a, which has been associated with altered angiogenesis parameters and with babies small for gestational age [94], was significantly elevated in placental malaria infection, and reduced IGF-1 levels in infected pregnant women when compared with non-infected controls were correlated with decreased birth weight [69].
Although PM may contribute to the development of pre-eclampsia by placental inflammatory processes with increased cytokine secretion [86], indication from pre-eclampsia and other causes of adverse pregnancy outcomes suggests that interventions to promote placental angiogenesis may improve birth outcomes [95, 96].
Using combination of multiple biomarkers for screening of PAM in longitudinal cohort studies could have diagnostic value. This would help to determine the timing of the parasite placental infections and to identify at risk group of women for developing PM and consequently poor pregnancy outcomes. At risk patient’s identification can guide malaria control strategies and help the initiation of an effective anti-malarial treatment during the antenatal period to optimize the prevention of the consequences of placental sequestration in inhabitants of malaria endemic areas.
PAM and PM in Sudan
Malaria is one of the virulent and epidemic diseases in Sudan, with P. falciparum as the most dominant species and Anopheles arabiensis as the main vector. Malaria during pregnancy has been documented as a long-standing health problem in different parts of the country and pregnant women are more susceptible to malaria infection during pregnancy [97, 98]. Moreover, P. vivax has been reported among pregnant women in Eastern Sudan [99].
Maternal mortality ratio for Sudan in 2017 was 295 deaths /100,000 live birth [1]. Infants’ health is also at risk as a result of PM and maternal anemia resulting from malaria with high burden to LBW [45], which is the leading cause of perinatal and infant mortality [100]. Moreover, it has been reported that sub-patent antenatal and placental malaria infections, detected by molecular techniques, contribute to adverse pregnancy outcomes [45, 101].
In many African countries, decline of placental malaria associated with substantial reductions in neonatal mortality and LBW has been linked with malaria prevention and control, such as use of sulfadoxine/pyrimethamine intermittent preventive treatment (SP-IPTp) after the first trimester, mass distribution of insecticide-treated bednets (ITNs), and effective case management of malarial sickness and anemia [15, 17, 102,103,104]. However, coverage of these interventions is limited in the antenatal care program in Sudan with complete absence of IPTp treatment due to the spread of resistance to SP in East Africa [17, 105].
PM in the Blue Nile State of Sudan
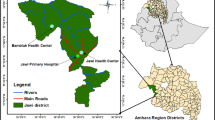
Blue Nile State lies in the tropical climate zone in the South-east of Sudan bordering South Sudan Ethiopia where Blue Nile River enters Sudan from the Ethiopian Highland. This area remains the worst among the central Sudan states in health indicators, particularly in primary health care accompanied by the role of migration due to political unrest. Infant and child mortality rate are higher when compared with other neighboring states. Inhabitants are mixed with Ethiopian and South Sudanese people where other plasmodium infections exist. Malaria illness caused by P. falciparum is one of the major health problems which increase mortality rates in the region. The surveillance system of Blue Nile State showed that malaria remains the top communicable disease that causes common morbidity and mortality in the area [106]. Few published studies investigate the prevalence of PM and its associated adverse outcome in the Blue Nile State. A cross-sectional study involving 1149 women who delivered in the three main hospitals of the State between 2012 and 2015 was conducted. A high prevalence of PM with P. falciparum as the only species was detected in the study population, particularly among younger age and primiparae women [41]. In a subsequent investigation for the role of submicroscopic parasitemia at time of delivery, a clear association has been found between sub-patent infections with maternal anemia and low birth weight in women of all parities irrespective of age [49]. In addition, investigating congenital malaria at time of delivery using real-time PCR proved malaria-infected placenta caused infants and cord blood infections [82].
Probable reasons of the above-mentioned findings in the Blue Nile area include lack of the recommended control polices and the poor implementation of optimal coverage of preventive tools. Moreover, documentation on the prevalence of PAM in the area is not separated from the overall prevalence of malaria in the population so as to reflect about the burden and severity of infection in pregnant women as compared with the general population. Additionally, the usage of the ITNs is not extensively practiced as poor pregnant women might not use the ITNs distributed by the ANC program free of charge and prefer to cover their young children with them, or even to sell the nets in the market to gain money. In addition to many other behavioral factors, women are not familiar with ANC attendance and drug use during pregnancy as they are afraid of the toxic effects of drugs in general and antimalarial treatment in particular. As such, there is a low enrollment of pregnant women in antenatal care.
Notably, due to traditional and cultural constraints, the majority of women in the area prefer to deliver at home, in addition to the economic and logistic requirements related to hospital delivery such as the charges to be paid for delivery even in public hospitals and other indirect costs such as expensive transportation and stay near the hospitals. Consequently, most of those women; who were never examined by a qualified physician, come to the health centers for delivery with many serious morbidities difficult to be diagnosed as PM or preeclampsia.
In order to reduce the risk of placental Plasmodium infections in areas such as Blue Nile State, there is an urgent need for raising the awareness at the community level about the detrimental effects of PAM and PM for the mothers and their fetuses. Moreover, the available malaria control measures in the area need to be reviewed with emphasis on sufficient sensitization of ITNs usage with coverage of all family members. Government and NGO efforts of health education of pregnant women for early ANC attendance and WHO recommended and focused number of visits are very essential, to avoid late attendance, particularly in rural areas where political stability and socioeconomic development are required.
Moreover, efforts to effectively address the limitations in the use of the antimalarial prevention measures by the population, beside the awareness for safety of medication intake during pregnancy, targeting women of childbearing age through community approaches and at educational and social meetings to improve the handling and usage of malaria prevention measures are vital. There is a need of more malaria control policies to screen for asymptomatic Plasmodium infection among pregnant women in the ANC service followed by immediate effective anti-malarial treatment to enhance the prevention of placental sequestration and decrease probabilities of suffering from adverse pregnancy outcomes and improve the benefits for the women’s health.
In such population where PM and pre-eclampsia may interact to drive adverse pregnancy outcomes, it would be interesting to measure placental biomarkers in peripheral blood during pregnancy that could help determine the timing of peripheral infections which lead to placental sequestration. Also, to assess the ability of treatment during pregnancy to clear the placenta and lead for the development of more effective interventions to decrease the burden of PAM and PM so as to improve the fetal and maternal outcome. Availability and increased use of obstetric ultrasound examination in maternity hospitals and units throughout pregnancy to improve understanding of the effect of malaria in pregnancy on fetal health is needed.
Subsequent to the findings of the above study, a longitudinal study is in progress following pregnant women throughout the course of pregnancy. The objectives of the study are characterization of genetic complexity of placental Plasmodium infections by sequence analysis of complete var2csa and to assess multiple biomarkers during pregnancy that can indicate PM and help to determine women at increasing risk for developing poor pregnancy outcomes.
Conclusion
Several studies have indicated that the detrimental effects of placental Plasmodium infections to the mother, fetus, and the child are accumulative effects of cellular damage. Although P. vivax interactions were believed to be milder than those due to P. falciparum, pathophysiological effects occur in both infections.
There are still challenges in the prompt diagnosis and treatment of PM infections. Measuring placental biomarkers within the framework of pre-eclampsia and associated to severe malaria in children and in infected pregnant women will allow optimizing the prevention of the consequences of placental sequestration and can provide information about disease pathophysiology and may improve the detection of PM in the absence of peripheral parasitemia.
Although var2csa has been identified as a major target for a vaccine against P. falciparum malaria during pregnancy, efforts to identify the different genetic variants and conserved epitopes of this protein from different geographical areas are still needed. Understanding maternal immune responses in the placenta as a result of Plasmodium infections is critical for management of pregnancy failures and poor birth outcomes.
Change history
17 October 2020
The article The Placenta and <Emphasis Type="Italic">Plasmodium</Emphasis> Infections: a Case Study from Blue Nile State, Sudan, written by Samia A. Omer and Suad M. Sulaiman, was originally published electronically on the publisher’s internet portal (currently SpringerLink) on October 03, 2020, with open access.
References
Organization WH. World malaria report. 2017.
Schantz-Dunn J, Nour NM. Malaria and pregnancy: a global health perspective. Rev Obstet Gynecol. 2009;2(3):186–92.
Huynh B-T, Cottrell G, Cot M, Briand V. Burden of malaria in early pregnancy: a neglected problem? Clin Infect Dis. 2015;60(4):598–604.
Dellicour S, Tatem AJ, Guerra CA, Snow RW, Ter Kuile FO. Quantifying the number of pregnancies at risk of malaria in 2007: a demographic study. PLoS Med. 2010;7(1).
Robinson DP, Klein SL. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm Behav. 2012;62(3):263–71.
Rogerson SJ, Pollina E, Getachew A, Tadesse E, Lema VM, Molyneux ME. Placental monocyte infiltrates in response to Plasmodium falciparum malaria infection and their association with adverse pregnancy outcomes. Am J Trop Med Hyg. 2003;68(1):115–9.
Rogerson SJ, Hviid L, Duffy PE, Leke RF, Taylor DW. Malaria in pregnancy: pathogenesis and immunity. Lancet Infect Dis. 2007;7(2):105–17.
Lindsay S, Ansell J, Selman C, Cox V, Hamilton K, Walraven G. Effect of pregnancy on exposure to malaria mosquitoes. Lancet. 2000;355(9219):1972.
Ansell J, Hamilton K, Pinder M, Walraven G, Lindsay S. Short-range attractiveness of pregnant women to Anopheles gambiae mosquitoes. Trans R Soc Trop Med Hyg. 2002;96(2):113–6.
Brabin B. An assessment of low birth weight risk in primiparae as an indicator of malaria control in pregnancy. Int J Epidemiol. 1991;20(1):276–83.
Umbers AJ, Aitken EH, Rogerson SJ. Malaria in pregnancy: small babies, big problem. Trends Parasitol. 2011;27(4):168–75.
Walker PG, ter Kuile FO, Garske T, Menendez C, Ghani AC. Estimated risk of placental infection and low birthweight attributable to Plasmodium falciparum malaria in Africa in 2010: a modelling study. Lancet Glob Health. 2014;2(8):e460–e7.
Tako EA, Zhou A, Lohoue J, Leke R, Taylor DW, Leke RF. Risk factors for placental malaria and its effect on pregnancy outcome in Yaounde, Cameroon. Am J Trop Med Hyg. 2005;72(3):236–42.
Mayor A, Bardají A, Felger I, King CL, Cisteró P, Dobaño C, et al. Placental infection with Plasmodium vivax: a histopathological and molecular study. J Infect Dis. 2012;206(12):1904–10.
Takem EN, D’Alessandro U. Malaria in pregnancy. Mediterr J Hematol Infect Dis. 2013;5 (1).
Sharma L, Shukla G. Placental malaria: a new insight into the pathophysiology. Front Med. 2017;4:117.
Rogerson SJ, Desai M, Mayor A, Sicuri E, Taylor SM, van Eijk AM. Burden, pathology, and costs of malaria in pregnancy: new developments for an old problem. Lancet Infect Dis. 2018;18(4):e107–e18.
Clark RL. Genesis of placental sequestration in malaria and possible targets for drugs for placental malaria. Birth Defects Res. 2019;111(10):569–83.
Desai M, Ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7(2):93–104.
Chaikitgosiyakul S, Rijken MJ, Muehlenbachs A, Lee SJ, Chaisri U, Viriyavejakul P, et al. A morphometric and histological study of placental malaria shows significant changes to villous architecture in both Plasmodium falciparum and Plasmodium vivax infection. Malar J. 2014;13(1):4.
Totino PR, Lopes SC. Insights into the cytoadherence phenomenon of Plasmodium vivax: the putative role of phosphatidylserine. Front Immunol. 2017;8:1148.
Chico RM, Mayaud P, Ariti C, Mabey D, Ronsmans C, Chandramohan D. Prevalence of malaria and sexually transmitted and reproductive tract infections in pregnancy in sub-Saharan Africa: a systematic review. JAMA. 2012;307(19):2079–86.
Rijken MJ, McGready R, Boel ME, Poespoprodjo R, Singh N, Syafruddin D, et al. Malaria in pregnancy in the Asia-Pacific region. Lancet Infect Dis. 2012;12(1):75–88.
Campos IM, Uribe ML, Cuesta C, Franco-Gallego A, Carmona-Fonseca J, Maestre A. Diagnosis of gestational, congenital, and placental malaria in Colombia: comparison of the efficacy of microscopy, nested polymerase chain reaction, and histopathology. Am J Trop Med Hyg. 2011;84(6):929–35.
McGready R, Lee S, Wiladphaingern J, Ashley E, Rijken M, Boel M, et al. Adverse effects of falciparum and vivax malaria and the safety of antimalarial treatment in early pregnancy: a population-based study. Lancet Infect Dis. 2012;12(5):388–96.
Kane EG, Taylor-Robinson AW. Prospects and pitfalls of pregnancy-associated malaria vaccination based on the natural immune response to Plasmodium falciparum VAR2CSA-expressing parasites. Malar Res Treat. 2011;2011:1–21.
Nosten F, Ter Kuile F, Maelankirri L, Decludt B, White N. Malaria during pregnancy in an area of unstable endemicity. Trans R Soc Trop Med Hyg. 1991;85(4):424–9.
Menendez C. Malaria during pregnancy. Curr Mol Med. 2006;6(2):269–73.
Ter Kuile FO, Parise ME, Verhoeff FH, Udhayakumar V, Newman RD, Van Eijk AM, et al. The burden of co-infection with human immunodeficiency virus type 1 and malaria in pregnant women in sub-saharan Africa. Am J Trop Med Hyg. 2004;71(2_suppl):41–54.
Perrault SD, Hajek J, Zhong K, Owino SO, Sichangi M, Smith G, et al. Human immunodeficiency virus co-infection increases placental parasite density and transplacental malaria transmission in Western Kenya. Am J Trop Med Hyg. 2009;80(1):119–25.
Bulmer J, Rasheed F, Francis N, Morrison L, Greenwood B. Placental malaria. I Pathological classification. Histopathology. 1993;22(3):211–8.
Ordi J, Ismail MR, Ventura PJ, Kahigwa E, Hirt R, Cardesa A, et al. Massive chronic intervillositis of the placenta associated with malaria infection. Am J Surg Pathol. 1998;22(8):1006–11.
McGready R, Davison BB, Stepniewska K, Cho T, Shee H, Brockman A, et al. The effects of Plasmodium falciparum and P. vivax infections on placental histopathology in an area of low malaria transmission. Am J Trop Med Hyg. 2004;70(4):398–407.
Chotivanich K, Udomsangpetch R, Suwanarusk R, Pukrittayakamee S, Wilairatana P, Beeson JG, et al. Plasmodium vivax adherence to placental glycosaminoglycans. PLoS One. 2012;7(4).
Poovassery J, Moore JM. Murine malaria infection induces fetal loss associated with accumulation of Plasmodium chabaudi AS-infected erythrocytes in the placenta. Infect Immun. 2006;74(5):2839–48.
Rogerson SJ, Mkundika P, Kanjala MK. Diagnosis of Plasmodium falciparum malaria at delivery: comparison of blood film preparation methods and of blood films with histology. J Clin Microbiol. 2003;41(4):1370–4.
Brabin B, Romagosa C, Abdelgalil S, Menendez C, Verhoeff FH, McGready R, et al. The sick placenta—the role of malaria. Placenta. 2004;25(5):359–78.
Omer SA, Idress HE, Adam I, Abdelrahim M, Noureldein AN, Abdelrazig AM, et al. Placental malaria and its effect on pregnancy outcomes in Sudanese women from Blue Nile State. Malar J. 2017;16(1):374.
Walter PR, Garin Y, Blot P. Placental pathologic changes in malaria. A histologic and ultrastructural study. Am J Pathol. 1982;109(3):330.
Ismail MR, Ordi J, Menendez C, Ventura PJ, Aponte JJ, Kahigwa E, et al. Placental pathology in malaria: a histological, immunohistochemical, and quantitative study. Hum Pathol. 2000;31(1):85–93.
Kattenberg JH, Ochodo EA, Boer KR, Schallig HD, Mens PF, Leeflang MM. Systematic review and meta-analysis: rapid diagnostic tests versus placental histology, microscopy and PCR for malaria in pregnant women. Malar J. 2011;10(1):321.
Ruizendaal E, Van Leeuwen E, Mens PF. Peripheral and placental biomarkers in women with placental malaria: a systematic review. Biomark Med. 2015;9(3):217–39.
Arango EM, Samuel R, Agudelo OM, Carmona-Fonseca J, Maestre A, Yanow SK. Molecular detection of malaria at delivery reveals a high frequency of submicroscopic infections and associated placental damage in pregnant women from Northwest Colombia. Am J Trop Med Hyg. 2013;89(1):178–83.
Kapisi J, Kakuru A, Jagannathan P, Muhindo MK, Natureeba P, Awori P, et al. Relationships between infection with Plasmodium falciparum during pregnancy, measures of placental malaria, and adverse birth outcomes. Malar J. 2017;16(1):400.
Mohammed AH, Salih MM, Elhassan EM, Mohmmed AA, Elzaki SE, El-Sayed BB, et al. Submicroscopic Plasmodium falciparum malaria and low birth weight in an area of unstable malaria transmission in Central Sudan. Malar J. 2013;12(1):172.
Omer SA, Noureldein AN, Eisa H, Abdelrahim M, Idress HE, Abdelrazig AM, et al. Impact of submicroscopic Plasmodium falciparum parasitaemia on maternal anaemia and low irth weight in Blue Nile State, Sudan J Trop Med 2019;2019.
Arango E, Maestre A, Carmona-Fonseca J. Effect of submicroscopic or polyclonal Plasmodium falciparum infection on mother and gestation product: systematic review. Rev Bras Epidemiol. 2010;13(3):373–86.
Rijken M, Rijken J, Papageorghiou A, Kennedy S, Visser G, Nosten F, et al. Malaria in pregnancy: the difficulties in measuring birthweight. BJOG. 2011;118(6):671–8.
Fried M, Duffy PE. Adherence of Plasmodium falciparum to chondroitin sulfate A in the human placenta. Science. 1996;272(5267):1502–4.
Fried M, Muga RO, Misore AO, Duffy PE. Malaria elicits type 1 cytokines in the human placenta: IFN-γ and TNF-α associated with pregnancy outcomes. J Immunol. 1998;160(5):2523–30.
Salanti A, Dahlbäck M, Turner L, Nielsen MA, Barfod L, Magistrado P, et al. Evidence for the involvement of VAR2CSA in pregnancy-associated malaria. J Exp Med. 2004;200(9):1197–203.
Pehrson C, Mathiesen L, Heno KK, Salanti A, Resende M, Dzikowski R, et al. Adhesion of Plasmodium falciparum infected erythrocytes in ex vivo perfused placental tissue: a novel model of placental malaria. Malar J. 2016;15(1):292.
Seitz J, Morales-Prieto DM, Favaro RR, Schneider H, Markert UR. Molecular principles of intrauterine growth restriction in Plasmodium falciparum infection. Front Endocrinol (Lausanne). 2019;10.
Souza RM, Ataíde R, Dombrowski JG, Ippólito V, Aitken EH, Valle SN, et al. Placental histopathological changes associated with Plasmodium vivax infection during pregnancy. PLoS Negl Trop Dis. 2013;7(2).
Luxemburger C, Ricci F, Nosten F, Raimond D, Bathet S, White NJ. The epidemiology of severe malaria in an area of low transmission in Thailand. Trans R Soc Trop Med Hyg. 1997;91(3):256–62.
Poespoprodjo JR, Fobia W, Kenangalem E, Lampah DA, Warikar N, Seal A, et al. Adverse pregnancy outcomes in an area where multidrug-resistant Plasmodium vivax and Plasmodium falciparum infections are endemic. Clin Infect Dis. 2008;46(9):1374–81.
Uneke CJ. Impact of placental Plasmodium falciparum malaria on pregnancy and perinatal outcome in sub-Saharan Africa: II: effects of placental malaria on perinatal outcome; malaria and HIV. Yale J Biol Med. 2007;80(3):95–103.
Fried M, Nosten F, Brockman A, Brabin BJ, Duffy PE. Maternal antibodies block malaria. Nature. 1998;395(6705):851–2.
Hviid L, Salanti A. VAR2CSA and protective immunity against pregnancy-associated Plasmodium falciparum malaria. Parasitology. 2007;134(13):1871–6.
Fievet N, Moussa M, Tami G, Maubert B, Cot M, Deloron P, et al. Plasmodium falciparum induces a Th1/Th2 disequilibrium, favoring the Th1-type pathway, in the human placenta. J Infect Dis. 2001;183(10):1530–4.
Davison BB, Kaack MB, Rogers LB, Rasmussen KK, Rasmussen TA, Henson EW, et al. The role of soluble tumor necrosis factor receptor types I and II and tumor necrosis factor–α in malaria during pregnancy. J Infect Dis. 2006;194(1):123–32.
Suguitan AL Jr, Leke RG, Fouda G, Zhou A, Thuita L, Metenou S, et al. Changes in the levels of chemokines and cytokines in the placentas of women with Plasmodium falciparum malaria. J Infect Dis. 2003;188(7):1074–82.
Boeuf P, Aitken EH, Chandrasiri U, Chua CLL, McInerney B, McQuade L, et al. Plasmodium falciparum malaria elicits inflammatory responses that dysregulate placental amino acid transport. PLoS Pathog. 2013;9(2).
Zamudio S, Baumann M, Illsley N. Effects of chronic hypoxia in vivo on the expression of human placental glucose transporters. Placenta. 2006;27(1):49–55.
Dorman E, Shulman C, Kingdom J, Bulmer J, Mwendwa J, Peshu N, et al. Impaired uteroplacental blood flow in pregnancies complicated by falciparum malaria. Ultrasound Obstet Gynecol. 2002;19(2):165–70.
Davison BB, Cogswell FB, Baskin GB, Falkenstein KP, Henson EW, Krogstad DJ. Placental changes associated with fetal outcome in the Plasmodium coatneyi/rhesus monkey model of malaria in pregnancy. Am J Trop Med Hyg. 2000;63(3):158–73.
Boeuf P, Tan A, Romagosa C, Radford J, Mwapasa V, Molyneux ME, et al. Placental hypoxia during placental malaria. J Infect Dis. 2008;197(5):757–65.
Menendez C, Ordi J, Ismail M, Ventura P, Aponte J, Kahigwa E, et al. The impact of placental malaria on gestational age and birth weight. J Infect Dis. 2000;181(5):1740–5.
Umbers AJ, Boeuf P, Clapham C, Stanisic DI, Baiwog F, Mueller I, et al. Placental malaria-associated inflammation disturbs the insulin-like growth factor axis of fetal growth regulation. J Infect Dis. 2011;203(4):561–9.
Walker PG, Griffin JT, Cairns M, Rogerson SJ, Van Eijk AM, Ter Kuile F, et al. A model of parity-dependent immunity to placental malaria. Nat Commun. 2013;4(1):1–11.
Ramharter M, Grobusch MP, Kießling G, Adegnika AA, Möller U, Agnandji ST, et al. Clinical and parasitological characteristics of puerperal malaria. J Infect Dis. 2005;191(6):1005–9.
Guyatt HL, Snow RW. Impact of malaria during pregnancy on low birth weight in sub-Saharan Africa. Clin Microbiol Rev. 2004;17(4):760–9.
Cottrell G, Mary J-Y, Barro D, Cot M. The importance of the period of malarial infection during pregnancy on birth weight in tropical Africa. Am J Trop Med Hyg. 2007;76(5):849–54.
Huynh B-T, Fievet N, Gbaguidi G, Dechavanne S, Borgella S, Guézo-Mévo B, et al. Influence of the timing of malaria infection during pregnancy on birth weight and on maternal anemia in Benin. Am J Trop Med Hyg. 2011;85(2):214–20.
Poespoprodjo JR, Fobia W, Kenangalem E, Hasanuddin A, Sugiarto P, Tjitra E, et al. Highly effective therapy for maternal malaria associated with a lower risk of vertical transmission. J Infect Dis. 2011;204(10):1613–9.
Omer SA, Adam I, Noureldien A, Elhaj H, Guerrero-Latorre L, Silgado A, et al. Congenital malaria in newborns delivered to mothers with malaria-infected placenta in Blue Nile State, Sudan J Trop Pediatr 2020; 0, 1–7. doi: https://doi.org/10.1093/tropej/fmz083.
Bardají A, Sigauque B, Sanz S, Maixenchs M, Ordi J, Aponte JJ, et al. Impact of malaria at the end of pregnancy on infant mortality and morbidity. J Infect Dis. 2011;203(5):691–9.
Borgella S, Fievet N, Huynh B-T, Ibitokou S, Hounguevou G, Affedjou J, et al. Impact of pregnancy-associated malaria on infant malaria infection in southern Benin. PLoS One. 2013;8(11).
Broen K, Brustoski K, Engelmann I, Luty AJ. Placental Plasmodium falciparum infection: causes and consequences of in utero sensitization to parasite antigens. Mol Biochem Parasitol. 2007;151(1):1–8.
Malhotra I, Dent A, Mungai P, Wamachi A, Ouma JH, Narum DL, et al. Can prenatal malaria exposure produce an immune tolerant phenotype?: a prospective birth cohort study in Kenya. PLoS Med. 2009;6(7).
de Moraes-Pinto MI, Verhoeff F, Chimsuku L, Milligan PJ, Wesumperuma L, Broadhead RL, et al. Placental antibody transfer: influence of maternal HIV infection and placental malaria. Arch Dis Child Fetal Neonatal Ed. 1998;79(3):F202–F5.
Okoko BJ, Wesuperuma LH, Ota MO, Banya WA, Pinder M, Gomez FS, et al. Influence of placental malaria infection and maternal hypergammaglobulinaemia on materno-foetal transfer of measles and tetanus antibodies in a rural west African population. J Health Popul Nutr 2001:59–65.
van der Sande MA, Kaye S, Miles DJ, Waight P, Jeffries DJ, Ojuola OO, et al. Risk factors for and clinical outcome of congenital cytomegalovirus infection in a peri-urban West-African birth cohort. PLoS One. 2007;2(6).
Christensen DL, Kapur A, Bygbjerg IC. Physiological adaption to maternal malaria and other adverse exposure: low birth weight, functional capacity, and possible metabolic disease in adult life. Int J Gynecol Obstet. 2011;115:S16–S9.
Tran V, Weckman A, Kain K. Malaria in pregnancy: an unrecognized risk factor for neuropsychiatric disease in offspring. Pediatr Infect Dis. 2016;1(17):2573–0282.100017.
Muehlenbachs A, Mutabingwa TK, Edmonds S, Fried M, Duffy PE. Hypertension and maternal–fetal conflict during placental malaria. PLoS Med. 2006;3(11).
Ndao CT, Dumont A, Fievet N, Doucouré S, Gaye A, Lehesran J-Y. Placental malarial infection as a risk factor for hypertensive disorders during pregnancy in Africa: a case-control study in an urban area of Senegal, West Africa. Am J Epidemiol. 2009;170(7):847–53.
Gueneuc A, Deloron P, Bertin GI. Usefulness of a biomarker to identify placental dysfunction in the context of malaria. Malar J. 2017;16(1):11.
Agarwal I, Karumanchi SA. Preeclampsia and the anti-angiogenic state. Pregnancy Hypertens. 2011;1(1):17–21.
Dietmann A, Helbok R, Lackner P, Fischer M, Reindl M, Lell B, et al. Endoglin in African children with Plasmodium falciparum malaria: a novel player in severe malaria pathogenesis? J Infect Dis. 2009;200(12):1842–8.
Lovegrove FE, Tangpukdee N, Opoka RO, Lafferty EI, Rajwans N, Hawkes M, et al. Serum angiopoietin-1 and-2 levels discriminate cerebral malaria from uncomplicated malaria and predict clinical outcome in African children. PLoS One. 2009;4(3).
Jain V, Lucchi NW, Wilson NO, Blackstock AJ, Nagpal AC, Joel PK, et al. Plasma levels of angiopoietin-1 and-2 predict cerebral malaria outcome in Central India. Malar J. 2011;10(1):383.
Silver KL, Conroy AL, Leke RG, Leke RJ, Gwanmesia P, Molyneux ME, et al. Circulating soluble endoglin levels in pregnant women in Cameroon and Malawi—associations with placental malaria and fetal growth restriction. PLoS One. 2011;6(9).
Conroy AL, Bangirana P, Muhindo MK, Kakuru A, Jagannathan P, Opoka RO, et al. Case report: birth outcome and neurodevelopment in placental malaria discordant twins. Am J Trop Med Hyg. 2019;100(3):552–5.
Silasi M, Cohen B, Karumanchi SA, Rana S. Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin N Am. 2010;37(2):239–53.
McDonald CR, Cahill LS, Gamble JL, Elphinstone R, Gazdzinski LM, Zhong KJ, et al. Malaria in pregnancy alters l-arginine bioavailability and placental vascular development. Sci Transl Med. 2018;10(431).
Adam I, Khamis AH, Elbashir MI. Prevalence and risk factors for Plasmodium falciparum malaria in pregnant women of eastern Sudan. Malar J. 2005;4(1):18.
Omer SA, Khalil EAG, Sharief AH, Ali HA. Pregnancy-associated malaria in Sudan: prevalence and possible risk factors. Open Trop Med J. 2011;4(1).
Rayis DA, Ahmed MA, Omer EM, Adam I. Plasmodium vivax malaria among pregnant women in Eastern Sudan. Asian Pacific J Trop Dis. 2016;6:2021–3.
Hassan AA, Abubaker MS, Radi EA, Adam I. Education, prenatal care, and poor perinatal outcome in Khartoum, Sudan. Int J Gynecol Obstet. 2009;105(1):66–7.
Omer S, Khalil E, Ali H, Sharief A. Submicroscopic and multiple Plasmodium falciparum infections in pregnant Sudanese women. N Am J Med Sci. 2011;3(3):137–41.
Kayentao K, Kodio M, Newman RD, Maiga H, Doumtabe D, Ongoiba A, et al. Comparison of intermittent preventive treatment with chemoprophylaxis for the prevention of malaria during pregnancy in Mali. J Infect Dis. 2005;191(1):109–16.
Hommerich L, Von Oertzen C, Bedu-Addo G, Holmberg V, Acquah PA, Eggelte TA, et al. Decline of placental malaria in southern Ghana after the implementation of intermittent preventive treatment in pregnancy. Malar J. 2007;6(1):144.
Bouyou-Akotet M, Mawili-Mboumba D, Kendjo E, Moutandou Chiesa S, Tshibola Mbuyi M, Tsoumbou-Bakana G, et al. Decrease of microscopic Plasmodium falciparum infection prevalence during pregnancy following IPTp-SP implementation in urban cities of Gabon. Trans R Soc Trop Med Hyg. 2016;110(6):333–42.
Okell LC, Griffin JT, Roper C. Mapping sulphadoxine-pyrimethamine-resistant Plasmodium falciparum malaria in infected humans and in parasite populations in Africa. Sci Rep. 2017;7(1):1–15.
Health FMo. Blue Nile state emerging profile. Khartoum: Federal Ministiry of Health; 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The article The Placenta and Plasmodium Infections: a Case Study from Blue Nile State, Sudan, written by Samia A. Omer and Suad M. Sulaiman, was originally published electronically on the publisher’s internet portal (currently SpringerLink) on October 03, 2020 with open access. With the author(s)’ decision to step back from Open Choice, the copyright of the article changed on October 12, 2020 to © Springer Nature Switzerland AG 2020 and the article is forthwith distributed under the terms of copyright.
This article is part of the Topical Collection on The Placenta, Tropical Diseases, and Pregnancies
Rights and permissions
About this article
Cite this article
Omer, S.A., Sulaiman, S.M. The Placenta and Plasmodium Infections: a Case Study from Blue Nile State, Sudan. Curr Trop Med Rep 7, 153–160 (2020). https://doi.org/10.1007/s40475-020-00214-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-020-00214-1