Abstract
Purpose of Review
Recent studies of environmental chemicals and endometriosis were critically evaluated from the epidemiologic perspective to identify aspects of study design and analyses that may contribute to discrepant results across studies.
Recent Findings
Of the 29 studies reviewed, 12 studies used new approaches to population-based sampling. The remaining studies were conducted primarily among patients undergoing pelvic surgery; controls may not represent the exposure experience of the underlying study base, resulting in biased estimates of associations. Most studies used biologic specimens collected near diagnosis and varied in analytic approaches to minimize bias. Few studies investigated ovarian, deep-infiltrating, and peritoneal endometriosis presentations separately.
Summary
Recommendations to move the field forward include (1) control selection from a defined study base, (2) exposure characterization during the etiologically relevant window, (3) employment of best practices to minimize bias in analyses, and (4) separate consideration of endometriosis presentations that may be etiologically distinct entities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis is characterized by the presence of endometrial glands and stroma outside the uterus, usually in the peritoneal cavity. Endometriosis is associated with substantial morbidity; women with endometriosis frequently report pain symptoms, including dysmenorrhea, chronic pelvic pain, and dyspareunia [1]. For many women, these symptoms can be chronic and debilitating, substantially interfering with all aspects of life—daily activities, work productivity, school performance, and personal relationships [2,3,4,5]. This serious condition is estimated to affect approximately 10% of reproductive-age women globally, although reported prevalence estimates vary widely [6]. This is due to surgical visualization being required to definitively diagnose the disease.
The etiology of endometriosis is not well understood. Several theories have been hypothesized for disease pathogenesis which fall into two categories—in situ-based and transplantation-based theories (as reviewed by Lagana et al. [7••]). In situ-based theories hypothesize that endometrial-like stroma and glands originate from local tissues that undergo metaplasia or from cells of primitive endometrial tissue misplaced in utero, outside the expected area of Müllerian duct development. On the other hand, transplantation-based theories hypothesize that stroma and glands from the eutopic endometrium are displaced to locations outside the uterus. The most common transplantation-based theory is the retrograde menstruation theory introduced by Sampson in 1927 [8]. In that theory, endometriosis occurs from the reflux of endometrial tissue during menstruation. Although several theories have been proposed, one theory is not able to explain all manifestations of endometriosis.
It is additionally recognized that endometriosis is multifactorial, involving anatomical, hormonal, immunological, estrogenic, genetic, epigenetic, and environmental factors. Central to disease pathogenesis is estrogen. Estrogen regulates the key pathological processes in endometriosis, including immunologic, inflammatory, angiogenic, and antiapoptotic cellular and molecular mechanisms that promote the persistence and progression of endometriotic lesions [1]. Given that estrogen is the driver of disease, it is plausible that endometriosis risk could be affected by exposure to endocrine-disrupting chemicals.
An endocrine-disrupting chemical is defined as “an exogenous chemical, or mixture of chemicals, that interferes with any aspect of hormone action” [9]. In the past decade, the investigation into the human health effects of endocrine-disrupting chemicals has substantially grown, with a set of prototypical endocrine-disrupting chemicals being well established (as reviewed by Gore et al. [10••]). This set includes bisphenol A (BPA), phthalates, polychlorinated biphenyls (PCBs), polybrominated diphenyl ethers (PBDEs), the organochlorine pesticide p,p’-dichlorodiphenyltrichloroethane (DDT) and its metabolite dichlorodiphenyldichloroethylene (DDE), the perfluoroalkyl substance (PFAS), perfluorooctanoic acid (PFOA), and the dioxin 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD).
Over the past several decades, these endocrine-disrupting chemicals and others have been investigated in relation to endometriosis risk. Several comprehensive reviews have been conducted on these studies, all reporting a common conclusion: the results across studies are inconsistent [11,12,13,14,15,16,17]. The authors of these reviews, and of the individual studies themselves, have offered reasons for the disparate results. The reasons include differences between studies in study population characteristics (geographical, dietary, parity/lactation history), biologic media used for measurement of environmental chemicals, laboratory method for quantification of analytes, the specific compounds investigated, confounder adjustment, heterogeneity of disease, and undiagnosed disease among controls [11,12,13,14,15,16,17].
However, other aspects of study design and analyses may also contribute to the discrepant results. The approach to control selection can have a considerable impact on the validity of a case-control study. If controls are not sampled from the identified study base that gave rise to cases, they may not represent the distribution of exposure of the study base, resulting in biased estimates of associations [18]. Substantial bias can also be introduced from the approaches used in analyses to address samples with non-detectable concentrations of environmental chemicals [19,20,21] and to adjust for urinary dilution or lipid concentrations for environmental contaminants measured in urine or blood [22, 23].
Hence, the purpose of this review was to critically evaluate studies of environmental chemicals and endometriosis published in the past decade from the epidemiologic perspective, to identify overlooked aspects of study design and approaches to analyses that may contribute to discrepant results. In doing so, this review describes recently published studies not included in prior reviews. This review also highlights the important contributions made by studies in this field over the past decade and provides recommendations to move the field forward.
Article Search Approach and Criteria for Inclusion
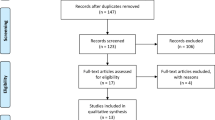
Although the environment encompasses an array of exposures, including those related to nutrition, pharmaceutics, smoking, alcohol, occupation, zoonotic and vector-borne diseases, radiation, water quality, and food safety, this review focuses on environmental chemicals, including those in air pollution, in relation to endometriosis risk. To identify articles in this area, a search was conducted using PubMed and the search terms environment*, air pollution, dioxin, metal*, cadmium, zinc, manganese, arsenic, mercury, lead, chromium, trace metals, trace elements, polychlorinated, PCB*, organochlorine, pesticide*, perfluoro, phthalate*, benzophenone, and bisphenol. Searches were conducted separately for each environmental search term, with the Boolean operator “AND” and search term endometrio*. The truncation (“wild card”) option was used to capture endometriosis, endometrioma, and endometriotic disease. All search terms were qualified with the [Title/Abstract] field tag. Articles were also identified from the reference list of reviewed articles.
Studies selected for inclusion in the review were observational human studies written in English and published in the past decade, between January 2010 and December 2019, reflecting the substantial expansion in endocrine disruptive chemical research after the publication of the first Endocrine Society Statement in 2009 [24]. Articles were further restricted to analytic studies in which endometriosis was the outcome of interest, and women with and without endometriosis were compared. Descriptive human studies, in vitro studies using endometrial stromal cell samples from women, and studies considering a combined outcome of endometriosis and adenomyosis were not included. Adenomyosis, characterized by the presence of endometrial stoma and glands within the myometrium, is generally considered a separate disease entity from that of endometriosis and the diagnosis of the two conditions substantially differ, with adenomyosis historically being diagnosed after hysterectomy [25]. Given the movement away from reliance on statistical significance testing and towards interpreting effect size and precision [26, 27], studies not reporting measures of association and precision (e.g., odds ratio and 95% confidence interval) were also excluded. For studies additionally examining gene-environment interactions, only the associations between environmental chemicals and endometriosis were evaluated.
The studies were reviewed with special attention to study design, including study population, outcome definition, and control/non-case selection (Table 1), as well as analyses, including covariate adjustment, modeling of the exposure-disease relationship, approach to handling values below the limit of detection, adjustment for urinary dilution or lipid concentration, and main findings (Table 2). To allow for the comparison of results across studies, the odds ratios (ORs) or hazard ratios (HRs) and accompanying 95% confidence intervals (CIs) are provided for each study in Table 2. For some chemical classes, a substantial number of analytes were investigated. Due to limited space, the ORs and 95% CIs are only provided for the environmental chemicals most frequently reported across studies for the following chemical classes: (1) organochlorine pesticides (OCPs): β-hexachlorocyclohexane (β-HCH), trans-nonachlor, hexachlorobenzene (HCB), oxychlordane, p,p’-DDE; (2) PCBs: congeners 118, 138, 153, 156; (3) PBDEs: congeners 47, 99, 100, 153, 154; (4) dioxins: 2,3,7,8-TCDD, 1,2,3,7,8-PeCDD, 1,2,3,4,7,8-HxCDD, 1,2,3,6,7,8-HxCDD; (5) furans: 2,3,4,7,8-PeCDF, 1,2,3,4,7,8-HxCDF, 1,2,3,4,7,8,9-HpCDF, OCDF; (6) PFAS: perfluoroalkyls perfluorooctane sulfonic acid (PFOS), perfluorooctanoic acid (PFOA), perfluorononanoic acid (PFNA), perfluorodecanoic acid (PFDA), perfluorohexane sulfonic acid (PFHxS); (7) metals: lead, cadmium, total mercury; and (8) phthalate metabolites: mono-n-butyl phthalate (MnBP), mono-benzyl phthalate (MBzP), mono-(2-ethylhexyl) phthalate (MEHP), mono-(2-ethyl-5-oxo-hexyl) phthalate (MEOHP), mono-(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP). The associations for summed chemicals are not provided.
Results
Twenty-four studies were included in the review (Tables 1 and 2) [28,29,30,31,32, 34,35,36,37,38,39,40,41,42,43,44, 46,47,48,49,50,51,52,53]. The studies were conducted in ten countries with the corresponding number of studies as follows: USA (n = 13), Taiwan (n = 2), Korea (n = 2), Belgium (n = 1), Italy (n = 1), Japan (n = 1), Spain (n = 1), France (n = 1), Iran (n = 1), and Brazil (n = 1) (Table 1). The studies evaluated the following environmental exposures: air pollution (n = 1), OCPs/PCBs/dioxins/furans/PBDEs/polybrominated biphenyls (PBB) (n = 9), PFAS (n = 2), metals (n = 2), BPA/phthalate metabolites (n = 9), and benzophenone-type ultraviolet (UV) filters (n = 1). Five studies used data from the Endometriosis: Natural History, Diagnosis and Outcomes (ENDO) study [28,29,30,31,32], and four studies used data from the Women’s Risk of Endometriosis (WREN) study [34,35,36,37]. The remaining 15 studies were conducted among unique study populations. In the ENDO study, results were reported for two cohorts, an operative cohort and population cohort [28,29,30,31,32]. Given the substantial differences in study participant sampling for these two cohorts, going forward, the two cohorts are considered separate studies. A revised total of 29 studies were reviewed.
Hospital or Clinic-Based Studies
Of the 29 studies, 17 studies (59%) were hospital- or clinic-based studies conducted among patients. A few of these studies were not defined as case-control studies, but since comparison groups were formed according to endometriosis case status, case-control study terminology is used to describe the studies. One study was conducted among patients of a gynecology and infertility center, with cases being patients referred with ovarian endometrioma and controls being patients who were previously seen at the center for a problem who were returning for routine care [52]. The remaining 16 studies were conducted among women undergoing laparoscopy, laparotomy, or other pelvic surgical procedures [28,29,30,31,32, 39,40,41,42,43,44, 47, 48, 50, 51, 53]. Five of these studies used data from the operative cohort of the ENDO study, which was composed of patients scheduled for laparoscopy or laparotomy at one of five hospital surgical centers in Salt Lake City, Utah, and nine clinical centers in San Francisco, CA. Across the 16 studies, the indications for surgery included pelvic pain, pelvic mass, menstrual irregularities, uterine fibroids, tubal ligation, infertility, Fallopian tube abnormalities/disease, ovarian cysts, hydrosalpinx, uterine cervical carcinoma, and genital prolapse.
Eight studies additionally applied exclusion rules to the control group that were not applied to the case group, such as requiring a laparoscopically normal pelvis [40]; no complaints of infertility or pelvic pain [42]; no history of pelvic surgery [43]; no clinical symptoms including chronic pelvic pain, dysmenorrhea, dyspareunia, or history of infertility [44]; no abdominal pain, diarrhea, dysmenorrhea, dyspareunia, or serum cancer agent 125 (CA-125) levels greater than 35 U/ml [47]; no laparoscopically confirmed leiomyoma or adenomyosis [48]; no adenomyosis, invasive cervix carcinoma or ovarian cancer [50]; and no past or present symptoms related to endometrioma [52].
Population-Based Studies
Twelve of the 29 studies used population-based sampling designs [28,29,30,31,32, 34,35,36,37,38, 46, 49]. Four studies used data from the WREN study, a population-based case-control study that was conducted among enrollees of an integrated healthcare system providing both insurance coverage and healthcare [34,35,36,37]. Premenopausal female enrollees ages 18–49 years with an intact uterus and at least one ovary enrolled in the healthcare system for ≥ 6 months in years 1996–2001 formed the study base; from this study base from this study base, from this study base, controls were directly and randomly sampled. Cases diagnosed for the first time with surgically visualized endometriosis were identified. ICD-9 codes were initially used to identify potential cases whose medical records, including operative notes and pathology reports, were then reviewed to confirm the surgical visualization of disease.
Five studies were conducted using data from the population cohort of the ENDO study [28,29,30,31,32]. Study participants in the population cohort were matched to the previously described operative cohort on age and residence within a 50-mi radius of the clinical centers which was the geographical residential area for ~ 90% of the operative cohort [33]. Since the operative cohort consisted of patients from one of 14 clinical centers in Utah and California, the population cohort was identified using a population database in Utah and telephone directory in California. Participants in the population cohort were screened by magnetic resonance imaging (MRI) to detect endometriosis. Using MRI, primarily ovarian endometriomas were visualized [33].
One study was conducted using data from the ongoing US-based prospective cohort study, Nurses’ Health Study II (NHSII) [38]. In the NHSII, 116,687 female registered nurses residing in the USA ages 25–43 years enrolled in the study in 1989. Since enrollment, the cohort has been followed every 2 years by questionnaire. Cases of endometriosis were identified by self-report of laparoscopically confirmed endometriosis.
Two studies used data from select cycles of the National Health and Nutrition Examination Survey (NHANES), which collects cross-sectional data on a sample representative of the US population [46, 49]. Cases of prevalent endometriosis were ascertained by self-report on whether a doctor or other health professional had ever told the study participant she had endometriosis.
Exposure Measurement
Most studies (n = 26) used biologic samples collected at or near the time of diagnosis for the measurement of environmental chemicals, although the timing of sample collection was not explicitly stated in eight studies [29, 31, 47, 48, 50, 53]. A single biologic sample was used to characterize past exposure. For two studies using data from cycles of NHANES, exposure measurement transpired a mean of 11.2 years after diagnosis in one study [46] and a median of 9 years in the other study [49].
In the prospective cohort study using NHS II data [38], exposure to air pollution over the years of participant follow-up until diagnosis or censoring was assessed by linking geocoded participant home addresses information to data from the US Census Topologically Integrated Geographic Encoding and Referencing System and US Environmental Protection Agency Air Quality System. From this data linkage, distance from roadways and exposure to particulate matter were estimated.
Outcome Definition
Many studies used a definition that required surgical visualization of endometriosis (n = 20). Four of these studies used data from the operative notes to further restrict cases to those meeting the definition of endometriotic disease [34,35,36,37]; three of these studies also used phenotype information on ovarian and non-ovarian peritoneal endometriosis [34, 35, 37]. Some studies additionally required histopathologic confirmation (n = 4) [40, 42, 47, 48], with one of these studies requiring an equal number of cases within each stage of the revised American Fertility Society (rAFS) staging system [40]. Four studies restricted endometriosis to surgical visualization of deep-infiltrating endometriosis (n = 1) [43], surgical visualization of deep-infiltrating endometriosis with rAFS staging III or IV (n = 1) [44], and surgical and histologic confirmation of ovarian endometriosis restricted to stages III and IV of the American Society of Reproductive Medicine revised (ASRMr) staging (n = 2) [50, 51]. For the remaining studies, endometriosis was detected by MRI (primarily ovarian endometriosis) (n = 5) [28,29,30,31,32], self-report of ever being told by a health provider they had endometriosis (prevalent disease) (n = 2) [46, 49], and sonographic evidence of ovarian endometriosis (n = 1) [52]. In one study, cases were those with histologic confirmation or MRI-detected endometriosis [53]. Twelve studies reported on the rAFS or ASRMr staging of endometriosis [28,29,30,31,32, 39,40,41,42, 44, 50, 51].
In terms of numbers of cases, ten studies involved < 50 endometriosis cases [28,29,30,31,32, 39, 41, 43, 48, 53] and ten studies involved 50–99 cases [36, 40, 42, 44, 46, 47, 49,50,51,52]. Nine studies had ≥ 100 cases [28,29,30,31,32, 34, 35, 37, 38].
Covariate Adjustment
Of the 29 studies included in this review, three did not adjust for confounding variables in the statistical analyses [41, 42, 53]. A few studies adjusted for parity status at the time of diagnosis or after [50,51,52], although infertility may be a consequence of disease. Four studies reported using directed acyclic graphs to select the variables for adjustment [35,36,37, 44].
Statistical Modeling that Allows for a Flexible Exposure-Disease Functional Form
Two studies did not state how environmental chemicals were modeled in the regression model [50, 52]. Five studies modeled the exposure both continuously and categorically [29, 32, 38, 39, 46]. A nearly equal number of studies modeled exposure continuously (most per 1-standard deviation change) (n = 9) [28, 30, 31, 43, 44, 51] and categorically (median, tertiles, or quartiles) (n = 11) [34,35,36,37, 40,41,42, 47,48,49, 53].
Approaches to Account for Lipids for Lipophilic Contaminants Measured in Blood
Of the 9 studies measuring lipophilic chemicals in serum or plasma, four studies lipid-standardized concentrations [40,41,42, 44] and five studies included lipids as a covariate in the regression model [28, 34, 35, 39].
Approaches to Account for Urinary Dilution for Environmental Contaminants Measured in Urine
Thirteen studies measured environmental chemicals in urine. Two studies (considering the population cohort and operative cohort as separate studies) did not report on the adjustment for urinary dilution for contaminants measured in urine [29], and one study reported that urinary creatinine was not measured [52]. The remaining studies measured urinary creatinine and either standardized concentrations (dividing the contaminant concentration by urinary creatinine concentration) (n = 6) [32, 48, 49, 51, 53] or included urinary creatinine as a covariate in the regression model (n = 4) [31, 36, 37].
Approaches to Handling Values Below Limit of Detection
Of the 29 studies reviewed, nearly a quarter of studies (n = 7) did not state how samples with concentrations below the limit of detection (LOD) were addressed in the analyses [31, 38, 42, 48, 50, 51]. Of those reporting approaches, the most commonly used were substitution (using 0, LOD, LOD/√2, LOD/2) (n = 8) [37, 41, 44, 46, 47, 49, 52, 53] and machine observed values (n = 7) [28, 29, 32, 39]. The remaining studies used imputation-based approaches (n = 2) [35, 36], recovery-adjusted values (n = 2) [30], deletion (n = 2) [40, 43], and inclusion of non-detects in lowest category of exposure (n = 1) [34]. Several studies did not investigate individual analytes with a substantial percent of non-detectable samples.
Consistencies in Results across Studies
The results across studies for the same environmental chemical appeared inconsistent. To understand whether studies employing similar approaches yielded similar results, the results for persistent environmental chemicals from studies with similar study population sampling, endometriosis phenotype, exposure measurement, and statistical approaches were compared. Two studies conducted in a similar manner were identified. These two studies were conducted in the USA and used a population-based sampling frame to investigate the OCPs β-HCH, γ-HCH, trans-nonachlor, HCB, oxychlordane, p,p’-DDE, and p,p’-DDT in relation to ovarian endometriosis—the population cohort in the ENDO study and the WREN population case-control study. Both studies measured the OCP analytes in serum, employed covariate adjustment to account for lipid concentrations, and had data on ovarian endometriosis. The directions of associations for ovarian endometriosis were similar for most of the OCP analytes in the two studies (Table 2). The results for PCBs could not be compared between the two studies as the ORs and 95% CIs between PCBs and ovarian endometriosis were not reported in the WREN study.
Comments
The study of environmental chemicals and endometriosis continues to be an active area of research. During the past decade, the range of environmental chemicals investigated in relation to endometriosis expanded, and now includes perfluoroalkyl substances, air pollution, and benzophenone-type UV filters. In addition, new population-based study designs were introduced. However, across studies, approaches to control selection and analyses to address issues related to studying environmental chemicals varied substantially. The following discussion describes how some approaches may result in biased estimates of the association and recommendations are provided to move the field forward.
Recommendation: Selection of Controls from a Defined Study Base
Over half of the studies in this review were clinic- or hospital-based studies in which controls were selected among patients undergoing laparoscopy or other pelvic surgery. The selection of controls in this manner allows for the identification of a disease-free comparison group using the same approach as that used to identify cases. However, this approach does not appear to follow a key principle of valid case-control study design: the identification of a study base from which the cases arose [54••]. The selection of controls from a study base allows controls to be selected independent of exposure. Violation of this key principle can yield wrong results [55]. Bias can be introduced when controls do not represent the exposure experience of the study base that gave rise to cases. Bias from the selection of surgical controls may be substantial when investigating exposures related to hormonal profiles [56••], such as endocrine-disrupting chemicals, as these exposures may be associated with the medical indications warranting surgery. In the studies reviewed, the indications for laparoscopy or other pelvic surgery included menstrual irregularities, uterine fibroids, infertility, and ovarian cysts. Associations between these conditions and exposure to endocrine-disrupting chemicals have been reported [10, 57,58,59,60,61]. Further support that the exposure distribution among surgical controls may differ from the underlying study base was provided in a population-based study of OCPs and endometriosis [35]. Among the population-based controls, those who had a history of undergoing laparoscopy had greater concentrations of oxychlordane, trans-nonachlor, HCB, and mirex compared to those without such a history.
The identification of a study base for a disease such as endometriosis which requires surgical visualization for diagnosis can be exceedingly difficult, particularly when the series of cases are identified first. The factors leading to surgical diagnosis can be complex and include the severity of symptoms, referral patterns, health care access, and agreeing to surgical evaluation [62, 63]. When controls cannot be randomly sampled from the study base that gave rise to cases, a non-random subset of hospital or clinic-based controls can be selected if a key assumption can be met: the non-random control subset represents the exposure distribution of the underlying study base [54••]. Using hospital controls as the example, Wacholder et al. posited that this assumption is reasonable when two conditions are satisfied: (1) hospital controls would have sought care at the same hospital for the case disease, and cases would have sought care at the same hospital for the control disease, and (2) the reason for hospital admission for the control is unrelated to exposure [54••]. Translating these conditions to the clinic-based controls undergoing pelvic surgery, the second condition is difficult to satisfy as the indications for surgery may be associated with exposure, as previously described.
Several studies in this review applied additional exclusion rules to surgical controls, including no complaints of infertility or pelvic pain, no history of pelvic surgery, and no symptoms of chronic pelvic pain, dysmenorrhea, and dyspareunia. Although the rationale for these rules was not provided, it appears that they were employed to minimize undiagnosed endometriosis among the controls, rather than select surgical patients with conditions not associated with exposure. The application of exclusion criteria to only controls violates the study base principle that rules should be applied equally to cases and controls, and could additionally contribute to biased estimates of associations [54••].
A common concern mentioned in hospital- or clinic-based studies in this review was the presence of undiagnosed endometriosis among controls who have not undergone laparoscopic evaluation—the gold standard in diagnosing endometriosis [63]. Three aspects of sampling from a study base alleviate this concern. First, as discussed previously, the selection of controls from an identified study base allows the controls to represent the exposure experience in the population that gave rise to cases. This provides for valid results. Second, the prevalence of undiagnosed disease among controls is likely to be low, particularly if a disease definition focused on progressive disease with interference of normal physiologic function is employed, such as the endometriotic disease definition proposed by Holt and Weiss [56••]. Using this definition, the prevalence of undiagnosed symptomatic disease is estimated to be < 2% [56••]. Third, the impact of systematic error on the estimate of association from case under-ascertainment and disease misclassification can be evaluated using quantitative bias analyses, considering different levels of case under-ascertainment [64, 65]. In this epidemiologist’s opinion, a valid case-control study design with some disease misclassification is preferable to a design that may not yield valid conclusions due to controls not representing the exposure experience of the source population.
Given these challenges, the introduction of new approaches to population-based sampling of study participants in the past decade has been an important advancement in study design for endometriosis research. This is exemplified by the population cohort of the ENDO study, the WREN study, and use of data from NHS II. For the population cohort of the ENDO study, participants were screened by MRI to detect cases of endometriosis. The WREN study employed the optimal approach to case-control study design; controls were directly sampled from a defined integrated health system population that gave rise to cases. By conducting the study among health plan enrollees, the financial barriers to accessing care were minimized and the likelihood that controls would seek care by the same providers as cases if they had symptoms was increased. The use of data from the large, epidemiologic NHS II cohort study shifted the paradigm for epidemiologic endometriosis research from case-control to prospective cohort study design.
Recommendation: Exposure Characterization During the Etiologically Relevant Window for Disease Onset
In the present review, most studies measured environmental chemical concentrations using a single sample collected at or near the time of endometriosis diagnosis. The measurement of environmental chemicals at diagnosis may not reflect body burden at the time of disease development. Reasons for this include (1) the documented long diagnostic delay, ranging on average 4 to 10 years between symptom onset and endometriosis diagnosis [5, 66,67,68]; (2) the measurement of less persistent environmental chemicals for which a single measurement may characterize more recent exposure. At the extreme end, exposure only over the past few hours or day may be characterized by the measurement of non-persistent chemicals such as bisphenol A and phthalates that are rapidly metabolized by the body after exposure [10••]; (3) the use of a biologic matrix (e.g., whole blood, serum, plasma, urine) that captures recent exposure. As one such example, cadmium measured in whole blood is considered a valid marker of recent exposure over the past few months, whereas its measurement in urine captures long-term exposure. The biologic half-life of cadmium in the kidneys is 10–30 years [69]; (4) the underestimation of body burden due to excretion factors. Body burden of persistent organic pollutants may be reduced in women who have given birth or breastfed [70,71,72,73,74,75]. PFAS body burden could also be underestimated in women with heavier menstrual flow as this has been reported to increase the elimination of PFAS [76]; (5) modifications to lifestyle habits after disease onset to manage symptoms. For example, to manage disease symptoms such as pain, women with endometriosis may change their diet. Since contaminated food and drink are important exposure sources for many environmental chemicals, changes to diet after disease onset could substantially affect environmental chemical concentrations measured at diagnosis; and (6) the potentially broad-range of the etiologically relevant window for disease susceptibility, which may include periods of development before menarche and symptom onset during the reproductive years. Although the specific windows are not known, several proposed theories for disease pathogenesis postulate aberrations in utero may contribute to disease [7••]. Exposures in utero and during infancy and childhood have also been associated with the increased risk of endometriosis in population-based epidemiologic studies [77,78,79,80]. It is also important to note that when the biologic specimen used for environmental chemical measurement is collected at or near the diagnosis of endometriosis, it is difficult to disentangle the involvement of environmental chemicals on disease progression from disease onset.
One approach to overcome this limitation is to use archived biologic samples collected over the life course. One novel example is the use of teeth lost during childhood. The development of deciduous teeth begins in utero and teeth accumulate environmental chemicals during formation. The analysis of childhood teeth allows for the reconstruction of past exposure to an array of environmental chemicals at specific periods of development, including in utero [81]. Another example is the use of newborn dried blood spots routinely collected at birth as part of state-based newborn screening programs in the USA. Several states archive the dried blood spots long-term for public health research use [82]. Although only a few drops of blood are collected from the newborn by heel stick, improvements in laboratory analytic methods now allow for the quantification of environmental chemicals in small amounts of biologic sample [83]. Other novel data linkages are possible, such as the geocoding of addresses and linkage to databases on air pollution as was done in the NHS II study [38].
Another approach to characterize exposure over the life course in relation to endometriosis is to build the capacity to collect data on incident endometriosis diagnosis in large, established cohort studies. A model for this approach has been the endometriosis research conducted using data from the NHS II study [84]. The identification of a cohort followed since preconception or in utero would be particularly valuable to understand early-life environmental exposures, collected in real time, that may contribute to endometriosis risk.
Recommendation: Employment of Best Practices to Minimize Bias in Analyses
In this review, it was observed that studies differed in the sophistication of analyses, with a few studies not adjusting for covariates in statistical analyses, not reporting on the approach to handle environmental chemical concentrations measured below the detection limit, and not accounting for urinary dilution when measuring environmental contaminants in urine. For the remaining studies that considered these issues, the analytic approaches varied.
For environmental contaminants measured in urine, the approach used to correct for urinary dilution may induce bias and affect the estimation of the association. O’Brien et al. suggested that two common approaches using urinary creatinine—standardization (dividing the environmental contaminant by the concentration of urinary creatinine) or covariate adjustment (including urinary creatinine as a covariate in the regression model)—may result in biased results in causal scenarios where disease risk factors (e.g., age) also affect creatinine concentrations [22•]. That study proposed another approach to minimize bias in which environmental contaminant concentrations are standardized by the estimated proportion of creatinine solely attributable to hydration. For similar reasons, bias may also be induced from the approach used to adjust for serum lipids for lipophilic environmental contaminants measured in blood. Consideration of the causal scenario using directed acyclic graphs is warranted to inform the selection of the most appropriate approach to adjust for urinary dilution and serum lipids [22, 23].
The method used to handle concentrations quantified below the detection limit can be another source of bias. Two simulation studies have reported that a common method, substitution with a single value (e.g., using values of LOD, LOD/2, LOD/√2), may introduce substantial bias if more than 10% of values are below the limit of detection [20, 21]. In these simulation studies, however, an approach such as multiple imputation that performed well with more than 30% missing began to degrade when > 50% of measurements were below the limit of detection [20, 21]. Hence, the approach selected should be appropriate for the percentage of values below the detectable level in the data.
Other aspects of analyses that may affect observed results include the modeling of the functional form of the exposure-disease relationship in the regression analyses. In the field of endocrine-disruption research, it is well recognized that the exposure-disease relationship may be non-monotonic [10, 85]. Imposing a linear relationship in regression modeling may result in associations being missed. In addition, results may be affected by the inclusion of variables in the regression model that do not operate as confounders. To aid the selection of variables for adjustment, a few studies in this review have used directed acyclic graphs. This allows one to avoid adjusting for variables that may not operate as confounder or whose adjustment may induce bias.
Not considered in this review is the movement in the past decade towards understanding the health effects from exposure to environmental chemical mixtures. This movement reflects the interest in understanding the impact of real-world simultaneous exposure to numerous environmental contaminants. Many approaches to studying chemical mixtures have been proposed, with several more in development. These approaches not only aid in understanding joint effects but may also help to identify “the bad actor” chemicals among highly correlated exposures [86, 87].
Recommendation: Separate Consideration of Endometriosis Presentations that May Be Etiologically Distinct Entities
Most studies in the review considered endometriosis as a single disease entity. This approach may reduce the sensitivity of a study to detect an association with environmental risk factors if endometriosis is comprised of separate etiologically distinct disease entities [18].
In 1997, it was proposed that three presentations of endometriosis—peritoneal endometriosis, ovarian endometriosis, and deep-infiltrating endometriosis of the rectovaginal septum—may indeed be etiologically distinct disease entities [88]. Nisolle et al. described the different pathogenic mechanisms for each phenotype as follows: menstrual transplantation into the pelvis for peritoneal endometriosis, metaplasia of coelomic epithelium for ovarian endometriosis, and metaplasia of Müllerian remnants in the rectovaginal septum for deep-infiltrating endometriosis. The possibility exists that environmental exposures may affect each endometriosis phenotype differently.
Hence, the study of the environmental origins of endometriosis may be aided by the investigation of individual endometriosis phenotypes, as was done in some of the studies in this review. Although 41% of studies in the present review collected data on rAFS and ASRMr staging of endometriosis, these staging systems are not correlated with endometriosis symptom severity and may not fully capture phenotype, since deep lesions are not captured in the staging system [89, 90]. The importance of disaggregating the heterogeneous endometriosis disease entity is recognized by the global effort of the World Endometriosis Research Foundation Endometriosis Phenome and Biobanking Harmonisation Project to promote the standardized collection of phenotype data, such as lesion location, color, and depth, in endometriosis research [89].
Conclusions
Endometriosis is common and is associated with substantial morbidity. Since endometriosis is an estrogen-driven condition, it is biologically plausible that exposure to endocrine-disrupting chemicals could contribute to the development of this serious condition. However, studies of environmental chemicals and endometriosis risk have yielded inconsistent results. This review, conducted from the epidemiologic perspective, identified several overlooked aspects of study design and analysis that may contribute to the disparate results across studies. Recommendations are provided to move the field of environmental origins of endometriosis research forward. If considered in concert, the recommendations have the potential to allow for the synthesis of findings across studies to further understand disease etiology and inform prevention efforts.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bulun SE. Chapter 25. Endometriosis. In: Strauss JF, 3rd, Baribieri RL, editors. Yen & Jaffe’s reproductive endocrinology. 8th ed. Philadelphia: Elsevier; 2019.
Fourquet J, Gao X, Zavala D, Orengo JC, Abac S, Ruiz A, et al. Patients’ report on how endometriosis affects health, work, and daily life. Fertil Steril. 2010;93(7):2424–8. https://doi.org/10.1016/j.fertnstert.2009.09.017.
Jones G, Jenkinson C, Kennedy S. The impact of endometriosis upon quality of life: a qualitative analysis. J Psychosom Obstet Gynaecol. 2004;25(2):123–33.
Moradi M, Parker M, Sneddon A, Lopez V, Ellwood D. Impact of endometriosis on women’s lives: a qualitative study. BMC Womens Health. 2014;14:123. https://doi.org/10.1186/1472-6874-14-123.
Nnoaham KE, Hummelshoj L, Webster P, d'Hooghe T, de Cicco NF, de Cicco NC, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011;96(2):366–73 e8. https://doi.org/10.1016/j.fertnstert.2011.05.090.
Ghiasi M, Kulkarni MT, Missmer SA. Is endometriosis more common and more severe than it was 30 years ago? J Minim Invasive Gynecol. 2019. https://doi.org/10.1016/j.jmig.2019.11.018.
•• Lagana AS, Garzon S, Gotte M, Vigano P, Franchi M, Ghezzi F, et al. The pathogenesis of endometriosis: molecular and cell biology insights. Int J Mol Sci. 2019;20(22):5615. https://doi.org/10.3390/ijms20225615Comprehensive summary of available evidence on what is known about endometriosis etiology and pathogenesis.
Sampson JA. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol. 1927;14:422–69.
Zoeller RT, Brown TR, Doan LL, Gore AC, Skakkebaek NE, Soto AM, et al. Endocrine-disrupting chemicals and public health protection: a statement of principles from the Endocrine Society. Endocrinology. 2012;153(9):4097–110. https://doi.org/10.1210/en.2012-1422.
•• Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, et al. EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals. Endocr Rev. 2015;36(6):E1–E150. https://doi.org/10.1210/er.2015-1010This Scientific Statement follows on the first statement published in 2009. Reviews the substantially larger body of literature on the health effects of endocrine disruption and describes the principles by which endocrine-disrupting chemicals act.
Bruner-Tran KL, Osteen KG. Dioxin-like PCBs and endometriosis. Syst Biol Reprod Med. 2010;56(2):132–46. https://doi.org/10.3109/19396360903381023.
Cano-Sancho G, Ploteau S, Matta K, Adoamnei E, Louis GB, Mendiola J, et al. Human epidemiological evidence about the associations between exposure to organochlorine chemicals and endometriosis: systematic review and meta-analysis. Environ Int. 2019;123:209–23. https://doi.org/10.1016/j.envint.2018.11.065.
Guo SW, Simsa P, Kyama CM, Mihalyi A, Fulop V, Othman EE, et al. Reassessing the evidence for the link between dioxin and endometriosis: from molecular biology to clinical epidemiology. Mol Hum Reprod. 2009;15(10):609–24. https://doi.org/10.1093/molehr/gap075.
Heilier JF, Donnez J, Lison D. Organochlorines and endometriosis: a mini-review. Chemosphere. 2008;71(2):203–10. https://doi.org/10.1016/j.chemosphere.2007.09.044.
Porpora MG, Resta S, Fuggetta E, Storelli P, Megiorni F, Manganaro L, et al. Role of environmental organochlorinated pollutants in the development of endometriosis. Clin Exp Obstet Gynecol. 2013;40(4):565–7.
Smarr MM, Kannan K, Buck Louis GM. Endocrine disrupting chemicals and endometriosis. Fertil Steril. 2016;106(4):959–66. https://doi.org/10.1016/j.fertnstert.2016.06.034.
Yao M, Hu T, Wang Y, Du Y, Hu C, Wu R. Polychlorinated biphenyls and its potential role in endometriosis. Environ Pollut. 2017;229:837–45. https://doi.org/10.1016/j.envpol.2017.06.088.
Koepsell TD, Weiss NS. Epidemiologic methods: studying the occurrence of illness. New York: Oxford University Press; 2003.
Dinse GE, Jusko TA, Ho LA, Annam K, Graubard BI, Hertz-Picciotto I, et al. Accommodating measurements below a limit of detection: a novel application of cox regression. Am J Epidemiol. 2014;179(8):1018–24. https://doi.org/10.1093/aje/kwu017.
• Lubin JH, Colt JS, Camann D, Davis S, Cerhan JR, Severson RK, et al. Epidemiologic evaluation of measurement data in the presence of detection limits. Environ Health Perspect. 2004;112(17):1691–6 Compared approaches to handling values measured below the limit of detection based on a simulation study and data example.
• Uh HW, Hartgers FC, Yazdanbakhsh M, Houwing-Duistermaat JJ. Evaluation of regression methods when immunological measurements are constrained by detection limits. BMC Immunol. 2008;9:59. https://doi.org/10.1186/1471-2172-9-59Compared six methods to address values below the limit of detection, using simulation studies.
• O’Brien KM, Upson K, Cook NR, Weinberg CR. Environmental chemicals in urine and blood: improving methods for creatinine and lipid adjustment. Environ Health Perspect. 2016;124(2):220–7. https://doi.org/10.1289/ehp.1509693Using simulations, adjustment methods for urinary dilution and serum lipids, including conventional and novel approaches are compared.
Schisterman EF, Whitcomb BW, Louis GM, Louis TA. Lipid adjustment in the analysis of environmental contaminants and human health risks. Environ Health Perspect. 2005;113(7):853–7. https://doi.org/10.1289/ehp.7640.
Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: an Endocrine Society scientific statement. Endocr Rev. 2009;30(4):293–342. https://doi.org/10.1210/er.2009-0002.
Struble J, Reid S, Bedaiwy MA. Adenomyosis: a clinical review of a challenging gynecologic condition. J Minim Invasive Gynecol. 2016;23(2):164–85. https://doi.org/10.1016/j.jmig.2015.09.018.
Schmidt M, Rothman KJ. Mistaken inference caused by reliance on and misinterpretation of a significance test. Int J Cardiol. 2014;177(3):1089–90. https://doi.org/10.1016/j.ijcard.2014.09.205.
Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31(4):337–50. https://doi.org/10.1007/s10654-016-0149-3.
Buck Louis GM, Chen Z, Peterson CM, Hediger ML, Croughan MS, Sundaram R, et al. Persistent lipophilic environmental chemicals and endometriosis: the ENDO Study. Environ Health Perspect. 2012;120(6):811–6. https://doi.org/10.1289/ehp.1104432.
Kunisue T, Chen Z, Buck Louis GM, Sundaram R, Hediger ML, Sun L, et al. Urinary concentrations of benzophenone-type UV filters in U.S. women and their association with endometriosis. Environ Sci Technol. 2012;46(8):4624–32. https://doi.org/10.1021/es204415a.
Louis GM, Peterson CM, Chen Z, Hediger ML, Croughan MS, Sundaram R, et al. Perfluorochemicals and endometriosis: the ENDO study. Epidemiology. 2012;23(6):799–805. https://doi.org/10.1097/EDE.0b013e31826cc0cf.
Buck Louis GM, Peterson CM, Chen Z, Croughan M, Sundaram R, Stanford J, et al. Bisphenol A and phthalates and endometriosis: the Endometriosis: Natural History, Diagnosis and Outcomes Study. Fertil Steril. 2013;100(1):162–9 e1–2. https://doi.org/10.1016/j.fertnstert.2013.03.026.
Pollack AZ, Louis GM, Chen Z, Peterson CM, Sundaram R, Croughan MS, et al. Trace elements and endometriosis: the ENDO study. Reprod Toxicol. 2013;42:41–8. https://doi.org/10.1016/j.reprotox.2013.05.009.
Buck Louis GM, Hediger ML, Peterson CM, Croughan M, Sundaram R, Stanford J, et al. Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertil Steril. 2011;96(2):360–5. https://doi.org/10.1016/j.fertnstert.2011.05.087.
Trabert B, De Roos AJ, Schwartz SM, Peters U, Scholes D, Barr DB, et al. Non-dioxin-like polychlorinated biphenyls and risk of endometriosis. Environ Health Perspect. 2010;118(9):1280–5. https://doi.org/10.1289/ehp.0901444.
Upson K, De Roos AJ, Thompson ML, Sathyanarayana S, Scholes D, Barr DB, et al. Organochlorine pesticides and risk of endometriosis: findings from a population-based case-control study. Environ Health Perspect. 2013;121(11–12):1319–24. https://doi.org/10.1289/ehp.1306648.
Upson K, Sathyanarayana S, De Roos AJ, Thompson ML, Scholes D, Dills R, et al. Phthalates and risk of endometriosis. Environ Res. 2013;126:91–7. https://doi.org/10.1016/j.envres.2013.07.003.
Upson K, Sathyanarayana S, De Roos AJ, Koch HM, Scholes D, Holt VL. A population-based case-control study of urinary bisphenol A concentrations and risk of endometriosis. Hum Reprod. 2014;29(11):2457–64. https://doi.org/10.1093/humrep/deu227.
Mahalingaiah S, Hart JE, Laden F, Aschengrau A, Missmer SA. Air pollution exposures during adulthood and risk of endometriosis in the Nurses’ Health Study II. Environ Health Perspect. 2014;122(1):58–64. https://doi.org/10.1289/ehp.1306627.
Cooney MA, Buck Louis GM, Hediger ML, Vexler A, Kostyniak PJ. Organochlorine pesticides and endometriosis. Reprod Toxicol. 2010;30(3):365–9. https://doi.org/10.1016/j.reprotox.2010.05.011.
Simsa P, Mihalyi A, Schoeters G, Koppen G, Kyama CM, Den Hond EM, et al. Increased exposure to dioxin-like compounds is associated with endometriosis in a case-control study in women. Reprod BioMed Online. 2010;20(5):681–8. https://doi.org/10.1016/j.rbmo.2010.01.018.
Cai LY, Izumi S, Suzuki T, Goya K, Nakamura E, Sugiyama T, et al. Dioxins in ascites and serum of women with endometriosis: a pilot study. Hum Reprod. 2011;26(1):117–26. https://doi.org/10.1093/humrep/deq312.
Vichi S, Medda E, Ingelido AM, Ferro A, Resta S, Porpora MG, et al. Glutathione transferase polymorphisms and risk of endometriosis associated with polychlorinated biphenyls exposure in Italian women: a gene-environment interaction. Fertil Steril. 2012;97(5):1143–51 e1–3. https://doi.org/10.1016/j.fertnstert.2012.02.027.
Martinez-Zamora MA, Mattioli L, Parera J, Abad E, Coloma JL, van Babel B, et al. Increased levels of dioxin-like substances in adipose tissue in patients with deep infiltrating endometriosis. Hum Reprod. 2015;30(5):1059–68. https://doi.org/10.1093/humrep/dev026.
Ploteau S, Cano-Sancho G, Volteau C, Legrand A, Venisseau A, Vacher V, et al. Associations between internal exposure levels of persistent organic pollutants in adipose tissue and deep infiltrating endometriosis with or without concurrent ovarian endometrioma. Environ Int. 2017;108:195–203. https://doi.org/10.1016/j.envint.2017.08.019.
Ploteau S, Antignac JP, Volteau C, Marchand P, Venisseau A, Vacher V, et al. Distribution of persistent organic pollutants in serum, omental, and parietal adipose tissue of French women with deep infiltrating endometriosis and circulating versus stored ratio as new marker of exposure. Environ Int. 2016;97:125–36. https://doi.org/10.1016/j.envint.2016.08.011.
Campbell S, Raza M, Pollack AZ. Perfluoroalkyl substances and endometriosis in US women in NHANES 2003-2006. Reprod Toxicol. 2016;65:230–5. https://doi.org/10.1016/j.reprotox.2016.08.009.
Lai GL, Yeh CC, Yeh CY, Chen RY, Fu CL, Chen CH, et al. Decreased zinc and increased lead blood levels are associated with endometriosis in Asian women. Reprod Toxicol. 2017;74:77–84. https://doi.org/10.1016/j.reprotox.2017.09.001.
Huang PC, Tsai EM, Li WF, Liao PC, Chung MC, Wang YH, et al. Association between phthalate exposure and glutathione S-transferase M1 polymorphism in adenomyosis, leiomyoma and endometriosis. Hum Reprod. 2010;25(4):986–94. https://doi.org/10.1093/humrep/deq015.
Weuve J, Hauser R, Calafat AM, Missmer SA, Wise LA. Association of exposure to phthalates with endometriosis and uterine leiomyomata: findings from NHANES, 1999-2004. Environ Health Perspect. 2010;118(6):825–32. https://doi.org/10.1289/ehp.0901543.
Kim SH, Chun S, Jang JY, Chae HD, Kim CH, Kang BM. Increased plasma levels of phthalate esters in women with advanced-stage endometriosis: a prospective case-control study. Fertil Steril. 2011;95(1):357–9. https://doi.org/10.1016/j.fertnstert.2010.07.1059.
Kim SH, Cho S, Ihm HJ, Oh YS, Heo SH, Chun S, et al. Possible role of phthalate in the pathogenesis of endometriosis: in vitro, animal, and human data. J Clin Endocrinol Metab. 2015;100(12):E1502–11. https://doi.org/10.1210/jc.2015-2478.
Rashidi BH, Amanlou M, Lak TB, Ghazizadeh M, Eslami B. A case-control study of bisphenol a and endometrioma among subgroup of Iranian women. J Res Med Sci. 2017;22:7. https://doi.org/10.4103/1735-1995.199086.
Moreira Fernandez MA, Cardeal ZL, Carneiro MM, Andre LC. Study of possible association between endometriosis and phthalate and bisphenol A by biomarkers analysis. J Pharm Biomed Anal. 2019;172:238–42. https://doi.org/10.1016/j.jpba.2019.04.048.
•• Wacholder S, McLaughlin JK, Silverman DT, Mandel JS. Selection of controls in case-control studies I. Principles. Am J Epidemiol. 1992;135(9):1019–28. https://doi.org/10.1093/oxfordjournals.aje.a116396A seminal paper on case-control study design in epidemiology. Part 1 of 3 papers jointly published on case-control study design in the American Journal of Epidemiology.
Rothman KJ, Greenland S, Lash TL. Modern Epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.
•• Holt VL, Weiss NS. Recommendations for the design of epidemiologic studies of endometriosis. Epidemiology. 2000;11(6):654–9 The review, written by two epidemiologists, proposed a standard definition of endometriotic disease and provided several strategies for selecting controls in clinic-based studies to increase validity and minimize bias.
Buck Louis GM. Persistent environmental pollutants and couple fecundity: an overview. Reproduction. 2014;147(4):R97–R104. https://doi.org/10.1530/REP-13-0472.
Cho YJ, Yun JH, Kim SJ, Kwon HY. Nonpersistent endocrine disrupting chemicals and reproductive health of women. Obstet Gynecol Sci. 2020;63(1):1–12. https://doi.org/10.5468/ogs.2020.63.1.1.
Minguez-Alarcon L, Gaskins AJ. Female exposure to endocrine disrupting chemicals and fecundity: a review. Curr Opin Obstet Gynecol. 2017;29(4):202–11. https://doi.org/10.1097/GCO.0000000000000373.
Rattan S, Zhou C, Chiang C, Mahalingam S, Brehm E, Flaws JA. Exposure to endocrine disruptors during adulthood: consequences for female fertility. J Endocrinol. 2017;233(3):R109–R29. https://doi.org/10.1530/JOE-17-0023.
Rutkowska AZ, Diamanti-Kandarakis E. Polycystic ovary syndrome and environmental toxins. Fertil Steril. 2016;106(4):948–58. https://doi.org/10.1016/j.fertnstert.2016.08.031.
Shafrir AL, Farland LV, Shah DK, Harris HR, Kvaskoff M, Zondervan K, et al. Risk for and consequences of endometriosis: a critical epidemiologic review. Best Pract Res Clin Obstet Gynaecol. 2018;51:1–15. https://doi.org/10.1016/j.bpobgyn.2018.06.001.
As-Sanie S, Black R, Giudice LC, Gray Valbrun T, Gupta J, Jones B, et al. Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol. 2019;221(2):86–94. https://doi.org/10.1016/j.ajog.2019.02.033.
Lash TL, Fox MP, Fink AK. Applying quantitative bias analysis to epidemiologic data. Statistics for biology and health. New York: Springer Science+Business Media, LLC; 2009.
Lash TL, Fox MP, MacLehose RF, Maldonado G, McCandless LC, Greenland S. Good practices for quantitative bias analysis. Int J Epidemiol. 2014. https://doi.org/10.1093/ije/dyu149.
Hudelist G, Fritzer N, Thomas A, Niehues C, Oppelt P, Haas D, et al. Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod. 2012;27(12):3412–6. https://doi.org/10.1093/humrep/des316.
Staal AH, van der Zanden M, Nap AW. Diagnostic delay of endometriosis in the Netherlands. Gynecol Obstet Investig. 2016;81(4):321–4. https://doi.org/10.1159/000441911.
Soliman AM, Fuldeore M, Snabes MC. Factors associated with time to endometriosis diagnosis in the United States. J Women's Health. 2017;26(7):788–97. https://doi.org/10.1089/jwh.2016.6003.
Jarup L, Akesson A. Current status of cadmium as an environmental health problem. Toxicol Appl Pharmacol. 2009;238(3):201–8. https://doi.org/10.1016/j.taap.2009.04.020.
Sarcinelli PN, Pereira AC, Mesquita SA, Oliveira-Silva JJ, Meyer A, Menezes MA, et al. Dietary and reproductive determinants of plasma organochlorine levels in pregnant women in Rio de Janeiro. Environ Res. 2003;91(3):143–50. https://doi.org/10.1016/s0013-9351(02)00053-1.
Soliman AS, Wang X, DiGiovanni J, Eissa S, Morad M, Vulimiri S, et al. Serum organochlorine levels and history of lactation in Egypt. Environ Res. 2003;92(2):110–7. https://doi.org/10.1016/s0013-9351(02)00056-7.
Wang RY, Jain RB, Wolkin AF, Rubin CH, Needham LL. Serum concentrations of selected persistent organic pollutants in a sample of pregnant females and changes in their concentrations during gestation. Environ Health Perspect. 2009;117(8):1244–9. https://doi.org/10.1289/ehp.0800105.
Thomsen C, Haug LS, Stigum H, Froshaug M, Broadwell SL, Becher G. Changes in concentrations of perfluorinated compounds, polybrominated diphenyl ethers, and polychlorinated biphenyls in Norwegian breast-milk during twelve months of lactation. Environ Sci Technol. 2010;44(24):9550–6. https://doi.org/10.1021/es1021922.
Needham LL, Grandjean P, Heinzow B, Jorgensen PJ, Nielsen F, Patterson DG Jr, et al. Partition of environmental chemicals between maternal and fetal blood and tissues. Environ Sci Technol. 2011;45(3):1121–6. https://doi.org/10.1021/es1019614.
Mondal D, Weldon RH, Armstrong BG, Gibson LJ, Lopez-Espinosa MJ, Shin HM, et al. Breastfeeding: a potential excretion route for mothers and implications for infant exposure to perfluoroalkyl acids. Environ Health Perspect. 2014;122(2):187–92. https://doi.org/10.1289/ehp.1306613.
Wong F, MacLeod M, Mueller JF, Cousins IT. Enhanced elimination of perfluorooctane sulfonic acid by menstruating women: evidence from population-based pharmacokinetic modeling. Environ Sci Technol. 2014;48(15):8807–14. https://doi.org/10.1021/es500796y.
Gao M, Scott K, Koupil I. Associations of perinatal characteristics with endometriosis: a nationwide birth cohort study. Int J Epidemiol. 2019. https://doi.org/10.1093/ije/dyz140.
Kvaskoff M, Bijon A, Clavel-Chapelon F, Mesrine S, Boutron-Ruault MC. Childhood and adolescent exposures and the risk of endometriosis. Epidemiology. 2013;24(2):261–9. https://doi.org/10.1097/EDE.0b013e3182806445.
Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Michels KB, Hunter DJ. In utero exposures and the incidence of endometriosis. Fertil Steril. 2004;82(6):1501–8. https://doi.org/10.1016/j.fertnstert.2004.04.065.
Upson K, Sathyanarayana S, Scholes D, Holt VL. Early-life factors and endometriosis risk. Fertil Steril. 2015;104(4):964–71 e5. https://doi.org/10.1016/j.fertnstert.2015.06.040.
Arora M, Austin C. Teeth as a biomarker of past chemical exposure. Curr Opin Pediatr. 2013;25(2):261–7. https://doi.org/10.1097/MOP.0b013e32835e9084.
Therrell BL Jr, Hannon WH, Bailey DB Jr, Goldman EB, Monaco J, Norgaard-Pedersen B, et al. Committee report: Considerations and recommendations for national guidance regarding the retention and use of residual dried blood spot specimens after newborn screening. Genet Med. 2011;13(7):621–4. https://doi.org/10.1097/GIM.0b013e3182147639.
Ma W, Kannan K, Wu Q, Bell EM, Druschel CM, Caggana M, et al. Analysis of polyfluoroalkyl substances and bisphenol A in dried blood spots by liquid chromatography tandem mass spectrometry. Anal Bioanal Chem. 2013;405(12):4127–38. https://doi.org/10.1007/s00216-013-6787-3.
Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160(8):784–96. https://doi.org/10.1093/aje/kwh275.
Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR Jr, Lee DH, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378–455. https://doi.org/10.1210/er.2011-1050.
Gibson EA, Goldsmith J, Kioumourtzoglou MA. Complex mixtures, complex analyses: an emphasis on interpretable results. Curr Environ Health Rep. 2019;6(2):53–61. https://doi.org/10.1007/s40572-019-00229-5.
Hamra GB, Buckley JP. Environmental exposure mixtures: questions and methods to address them. Curr Epidemiol Rep. 2018;5(2):160–5. https://doi.org/10.1007/s40471-018-0145-0.
Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil Steril. 1997;68(4):585–96. https://doi.org/10.1016/s0015-0282(97)00191-x.
Becker CM, Laufer MR, Stratton P, Hummelshoj L, Missmer SA, Zondervan KT, et al. World Endometriosis Research Foundation Endometriosis Phenome and Biobanking Harmonisation Project: I. Surgical phenotype data collection in endometriosis research. Fertil Steril. 2014;102(5):1213–22. https://doi.org/10.1016/j.fertnstert.2014.07.709.
Vercellini P, Fedele L, Aimi G, Pietropaolo G, Consonni D, Crosignani PG. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod. 2007;22(1):266–71. https://doi.org/10.1093/humrep/del339.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reproductive and Perinatal Epidemiology
Rights and permissions
About this article
Cite this article
Upson, K. Environmental Risk Factors for Endometriosis: a Critical Evaluation of Studies and Recommendations from the Epidemiologic Perspective. Curr Epidemiol Rep 7, 149–170 (2020). https://doi.org/10.1007/s40471-020-00236-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-020-00236-3