Abstract
Introduction
This article reviews evidence-based smoking cessation and prevention programs for Indigenous youth and young adults in Australia, Canada, New Zealand, and the USA.
Methods
A systematic review using PubMed and PsycINFO search engines was conducted to identify randomized controlled trials (RCTs) and quasi-experimental studies focusing on Indigenous youth and young adults.
Results
Beyond two Cochrane reviews (2012) of smoking cessation and prevention programs for Indigenous youth and young adults, we located only two additional studies post Cochrane review. Combined results from the articles in the Cochrane reviews and the more recent studies suggest that recruitment of young Indigenous populations is challenging. Only one study with the smoking cessation program using mobile phone text messaging among the Maori was shown effective.
Conclusions
Additional evidence-based programs are essential for Indigenous youth and young adults to reduce smoking initiation and prevalence rates. Further evaluations of commercial tobacco use prevention and cessation programs are needed to bridge the gap between tobacco-related health disparities in Indigenous and non-Indigenous populations. Additionally, qualitative research is encouraged to further understand the barriers to recruitment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Indigenous youth and young adult populations in Australia, Canada, New Zealand, and the USA have remarkably higher smoking rates than their non-Indigenous counterparts. Significant health disparities exist in these high-income countries where smoking prevalence is nearly double among Indigenous youth when compared to non-Indigenous youth populations. In Canada, daily smoking prevalence is 29.6% among First Nation youth compared to 18.1% of Canadians ages 12 and older [1, 2]. In Australia, 42% of Indigenous Australians are current smokers by early adulthood (15–24 years) [3]. In New Zealand, Maori youth male are almost twice as likely than non-Maori youth males to smoke (27% daily smoking prevalence rate for Maori youth males compared to 15% among non-Maori youth males), while Maori females are four times as likely as non-Maori youth female to smoke (34% daily smoking prevalence among female youth Maori compared to 8% non-Maori female youth) (New Zealand Health Survey, 2016). Similarly, in the USA, past-month smoking prevalence among 9th–12th graders (14–18 years) was 24.3% among AIs, as compared with 18.6% among Whites [4]. Unfortunately, indigenous populations will bear adverse health consequences of commercial tobacco use and lower life expectancy [5]. Obviously, more attention is needed to prevent smoking initiation and increase smoking cessation to reduce the morbidity and mortality, particularly among Indigenous youth and young adults.
Smoking initiation at an early age is a strong indicator of long-term nicotine addiction and subsequent smoking-related diseases [6]. Average smoking initiation age among on-reserve First Nations youth is 10 years, as compared with age 17 years among Canadian youth [7]. In US studies, AI youth initiated smoking at earlier ages than all other racial/ethnic groups [8]. Primary social factors influencing smoking initiation among adolescents include peer group pressure, positive attitudes towards smoking, and the observation of adult smoking [9]. Indigenous adolescents might experience additional risk factors including easy access to tobacco from smoking family members, introduction to tobacco at an early age through ceremonial tobacco use, and access to tobacco retailers on tribal lands, which typically have lower tobacco taxes and less-stringent enforcement of laws restricting tobacco sales to minors than tobacco retailers outside of tribal lands [10,11,12,13].
Efforts to prevent commercial tobacco use initiation and reduce the use of regular tobacco use are essential to curb the high tobacco use rates among Indigenous youth and young adults. Numerous tobacco prevention and cessation programs have been implemented in various Indigenous populations, but few of them have been evaluated rigorously. Identification of evidence-based programs can help program planners select and implement the most-effective programs for each population. This article summarizes tobacco prevention and cessation programs that have been rigorously evaluated among Indigenous youth worldwide. The Cochrane reviews undertook this task in 2012, publishing a review of prevention programs for Indigenous adults [14] and a review of cessation programs for Indigenous youth [15].
This article will briefly review and summarize the two Cochrane reviews and synthesize additional studies of smoking cessation among Indigenous youth and young adults (ages 18–27) that were conducted since 2012. This review only includes studies of youth and young adults. We use the same criteria that the Cochrane reviews used: RCTs and quasi-experimental studies.
Methods
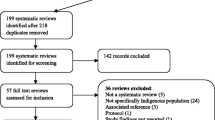
PubMed and PsycINFO search engines were used for the literature search. The term, “Indigenous,” can vary by region and population, but the use of the “Indigenous” term for this paper is to be consistent when describing “First Nations,” which are Indian populations Indigenous to Canada, “Australian Aboriginal” or “Torres Strait Islanders” for the Australian Indigenous, “Tangata Whenua” or “People of the land” for the Maori people of New Zealand, and “American Indian/Alaskan Natives” (AI/AN) for the US Indigenous populations. Each of these Indigenous populations has experienced colonization and removal from their motherland and culture after living in their country for thousands of years [16].
First, an overall search using the key terms “American Indian Tobacco Cessation Programs” or “Native Alaskan Tobacco Cessation Programs” yielded 13 peer-reviewed journal articles on tobacco cessation intervention. From these, only two articles met the inclusion criteria of being a RCT or quasi-experimental trial and having an age restriction (ages 18–27) on tobacco cessation interventions.
A more specialized search on tobacco prevention and cessation was conducted using a combination of 12 key terms. The search strategy for each country included the “name(s) of the “Indigenous population” AND (“Youth” OR “Emerging Adults”) AND (“Tobacco Cessation” OR “Smoking Prevention”). For example, a search for New Zealand included the following key terms: (“Tangata Whenua” OR “People of the land” OR “Maori”) AND (“Youth” OR “Emerging Adults” OR “Young Adults” OR “Adolescent”) AND (“Tobacco Cessation” OR “Smoking Prevention”). This search yielded no studies on commercial tobacco prevention.
Results
Prevention—Cochrane Review
The 2012 Cochrane review included two commercial tobacco use prevention studies among AI youth (Gilchrest, 1987; Schinke, 1994). Both studies were RCTs using a multi-component, community-based intervention tailored to the AI youth population (total N = 1505) to prevent commercial tobacco use. The Gilchrest study intervention (total N = 109 participants) included a 10-session skills enhancement program offered in the school setting compared to a test-only control group (three intervention sites, one urban and two rural, and four control sites, one urban and three rural). The Schinke study (n = 1396) was implemented at Tribal schools with three study arms: (1) skills only (15 classroom sessions along with booster sessions 6 months after initial intervention), (2) skills community (same as skills only, with annual intervention community involvement which included community activities for students to model to their parents and community the skills they learned from the classroom), and (3) control (no intervention).
Neither of these studies found a statistically significant difference in smoking between the intervention and control groups at the final follow-up timepoint. However, the Gilchrest study found a statistically significant difference in positive change in tobacco use at posttest (p < 0.05; change score of − 0.15 for intervention and − 0.01 for control), but it was not maintained at 6-month follow-up (p < 0.05). This study found no significant differences between the intervention and control groups on change in attitudes, self-esteem, or knowledge. The Schinke study found no significant differences between intervention and control groups at any follow-up.
Cessation—Cochrane Review
The Cochrane review titled, “Interventions for smoking cessation in Indigenous populations (review)” [15] included four studies. Of the four, only one study [17] met the target age range of young adults where the recruitment aim of the cessation program was to maximize participation of the young adult Maori population in New Zealand. The other three studies were among Indigenous adults, with mean ages of over 35 years.
The Bramley et al. [17] randomized controlled study involved a smoking cessation service (Stop Smoking by Mobile Phone—STOMP) using mobile phone text messaging targeting young smokers (16 years and older) to determine if STOMP was as effective for Maori as non-Maori populations. There were 355 Maori participants with 176 in the intervention group and 1705 non-Maori participants with 676 in the intervention group. The intervention included regular, personalized text messages to provide smoking cessation advice, support, and distraction for 6 weeks, with reduced messages thereafter until the end of the 26-week follow-up. The text messages were in English (over 1000 text messages) and in the Maori language (over 140 text messages), with information on Maori traditions. The control group received no smoking-related information but did receive text messages with reminders to complete follow-up surveys. Results indicated the Maori in the intervention group were more likely to report quitting at 6 weeks (26.1%) than those in the control group (11.2%) (RR 2.34, 95% CI: 1.44–3.79). There was no significant difference between the RR for Maori and that for non-Maori (RR 2.16, 95% CI 1.72–271), indicating that the STOMP program, when culturally targeted, is effective among Maori youth.
Prevention and Cessation Studies beyond Cochrane Review
Additional RCT studies on tobacco cessation intervention programs since the Cochrane review are limited (two additional peer-reviewed journal articles—see Table 1). For commercial tobacco prevention programs since the Cochrane review (2012b), no additional studies were found (Table 2).
Whittaker et al. [18] conducted a RCT to assess the effectiveness of a multimedia mobile phone intervention for smoking cessation among young adults (target age of 16–25 years), particularly among young Maori. The intervention was comprised of a series of chronologically sequenced video vignettes of former smokers acting as role models and sharing their quitting experience and coping strategies over a 6-month period. Participants were able to select their own role model from six different available role models, three of whom were ethnically Maori. The intervention group received one general health video message every 2 weeks and could receive specific messages when they texted key words to request additional support (for example, intervention participants could text “stress” and receive a video on how to cope with cravings in a text response). The control group received one video message every 2 weeks, with general health messages and reminders about the study for 6 months. However, the target sample size (n = 1300) was not achieved due to difficulty recruiting young adult quitters (n = 226, 110 assigned to intervention, of which 24% were Maori, and 116 assigned to control). There were no statistically significant differences in the six-month continuous self-reported abstinence rates for the intervention group, which had a 26.4% 6-month abstinence rate, compared to 27.6% in the control group (p value = 0.8). Strengths of the study include the use of the social cognitive theory to develop the intervention with technology-based health behavior change. Participants provided positive feedback on the use of video message technology to support further research.
Reasons for low recruitment were potentially due to participants perceiving the associated costs of using their personal mobile phone during the study to be high, even though the data used for texting and viewing videos were provided at no charge to their personal mobile phone accounts [18•]. Additionally, the advanced technology of the mobile phone was a concern, such as being unaware if their mobile phone could receive video messages when a text message with a universal resource locator (URL) was sent for participants to download the video message. Participant incentives of free data and other mobile phone perks were unattractive; therefore, vouchers were offered for mobile phone accessories, supermarkets, or gasoline until our study’s funding ran out. Lastly, the low recruitment and participation rates can be indicative that youth and young adults were not ready to commit to and participate in a smoking cessation program.
In the [19•]randomized two-group design study, a tobacco cessation program was designed for pregnant AN women of the Yukon-Kukokwim Delta region, with an average age of 25 years. The intervention group components included the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) cessation guide followed by a 15- to 25-min counseling session and viewing of a video sharing success stories of AN women who stopped tobacco use during pregnancy. Thereafter, a 10- to 15-min counseling session was held after the video viewing, and participants were provided with a copy of the video to share with their household. Telephone sessions were conducted at weeks 1, 2, 4, and 6 in which the participant’s tobacco use, self-efficacy, and problem-solving to barriers were discussed. The control group received a 5-min face-to-face counseling based on the 5 A’s and were provided with four culturally tailored brochures on pregnancy and tobacco use. Overall, enrollment into the program was low: 12% (35 out of 293 eligible), with 17 enrolled into the intervention group and 18 in the control. The biochemically confirmed abstinence rates at follow-up were 0% for the intervention group and 6% for the control.
The low recruitment rate was due to women having low interest and being not ready to quit smoking [19•]. Additionally, they lacked the time to complete the counseling visits because of flight schedules to return home. Even with phone counseling offered, this did not increase participation. Low rates of participation indicated a lack of acceptance or perceived feasibility among AN pregnant women to stop smoking. The social stigma of smoking during pregnancy and the method of recruitment in a large waiting area of a hospital could have acted as enrollment barriers. This was the first study of a smoking cessation intervention for AN pregnant women.
Project Stop the Use of Nicotine (SUN)
There is a clear need for evidence-based smoking cessation interventions that are culturally relevant and acceptable to Indigenous youth and young adults. To promote tobacco use cessation among AI teens, a RCT is currently underway, funded by the Tobacco-Related Disease Research Program (TRDRP) in California. The study will compare the efficacy of Project Stop the Use of Nicotine (SUN) (a modified version of Project EX, culturally targeted to AI teens) versus a control group [20]. Three hundred AI youth throughout California are being recruited from urban and rural/reservation areas. Hypotheses includes (1) AI youth who receive Project SUN will report less tobacco use at immediate posttest and 3- and 6-month follow-up compared to the control group, and (2) Project SUN program effects will be mediated by changes in knowledge, motivation to quit, and behavioral coping skills. Results will be available in 2019.
Main Findings—Analysis
While no meta-analysis will be conducted due to insufficient data being available, the following conclusion identifies trends in and barriers to creating a successful tobacco cessation intervention for AI/AN youth and discusses future research directions.
Conclusions
This review highlights the need for more studies that evaluate interventions to reduce and prevent the use of commercial tobacco use among young Indigenous populations around the world. Three studies (two prevention and one cessation) in two Cochrane reviews were summarized, and two additional cessation studies were found outside of the Cochrane reviews. Of the studies, only the smoking cessation program using mobile phone text messaging among the Maori was shown to be effective [17]. A funded RCT cessation intervention is mentioned to indicate some current work being implemented among AI youth.
All studies were RCTs which included school-based (Schinke et al., 1994; Gilchrest et al., 1987), mobile phone video/text messaging-based [18], and video-based types of interventions [19•]. These studies only included the AI/AN and Maori populations.
Of the five studies, the two studies had lower than expected recruitment [18, 19•] due to but not limited to cost, not being ready to quit, and social stigma to smoking while pregnant. Recruitment of youth for cessation programs has been shown to be a challenge because they may not be ready to commit to quit [21]. Not being able to achieve the recruitment goal within the trials can substantially under-power the results and hide any effects on the study findings.
Suggestions to increase future participation rates include examining additional approaches to maintaining higher retention and assess potential barriers and best practices for successful interventions. Finding out the best time to recruit (e.g. season of the year), offering incentives that are most valuable to the community, ensuring confidentiality, and including key stakeholders from within the Indigenous community are some essential ways to increase recruitment. Qualitative work can help determine the best time to enroll and where to recruit. Therefore, with larger sample sizes resulting in adequate power, an effect on quit rates between groups may be found.
Clearly, more evidence-based commercial tobacco use prevention and cessation services are needed to reduce tobacco use initiation and smoking prevalence among youth and young adults. This is particularly true of AI/AN adolescents, as they face a tremendous health disparity, with smoking rates being the highest among Indigenous youth when compared to the non-Indigenous populations.
References
Papers of particular interest, published recently, have been highlighted as:• Of importance
First Nations Information Governance Centre. First Nations Regional Health Survey (RHS) 2008/10: National Report on adults, Youth and Children Living in First Nations Communities 2012. (Accessed 1/12/2018).
Statistics Canada. Aboriginal Peoples Survey, 2012 (89–653-X). (Accessed 1/12/2018).
Australian Bureau of Statistics: National Aboriginal and Torres Strait Islander social survey 2008. 2009, Canberra: Australian Bureau of Statistics (No. 4714.0).
Centers for Disease Control and Prevention (CDC) (2013). 1991–2013 High School Youth Risk Behavior Survey Data. Available at http://nccd.cdc.gov/youthonline/. Accessed on December 28, 2017.
Cass A. Health outcomes in aboriginal populations. CMAJ Can Med Assoc J. 2004;171(6):597–8. https://doi.org/10.1503/cmaj.1041059.
Azagba S, Baskerville NB, Minaker L. A comparison of adolescent smoking initiation measures on predicting future smoking behavior. Prev Med Rep. 2015;2:174–7. https://doi.org/10.1016/j.pmedr.2015.02.015.
Lemstra M, Rogers M, Thompson A, Moraros J, Tempier R. Prevalence and risk indicators of smoking among on-reserve first nations youth. Paediatr Child Health. 2011;16(10):e71–7.
Clark TT, Doyle O, Clincy A. Age of first cigarette, alcohol, and marijuana use among US biracial/ethnic youth: a population-based study. Addict Behav. 2013;38(9):2450–4. https://doi.org/10.1016/j.addbeh.2013.04.005.
Liu J, Zhao S, Chen X, Falk E, Albarracín D. The influence of peer behavior as a function of social and cultural closeness: a meta-analysis of normative influence on adolescent smoking initiation and continuation. Psychol Bull. 2017;143(10):1082–115. https://doi.org/10.1037/bul0000113.
Johnston V, Thomas DP. Smoking behaviours in a remote Australian indigenous community: the influence of family and other factors. Soc Sci Med. 2008;67(11):1708–16. https://doi.org/10.1016/j.socscimed.2008.09.016.
Kegler MC, Cleaver VL, Yazzie-Valencia M. An exploration of the influence of family on cigarette smoking among American Indian adolescents. Health Educ Res. 2000;15(5):547–57. https://doi.org/10.1093/her/15.5.547.
Samuel KA, Ribisl KM, Williams RS. Internet cigarette sales and native American sovereignty: political and public health contexts. J Public Health Policy. 2012;33(2):173–87. https://doi.org/10.1057/jphp.2012.4.
Unger JB, Soto C, Baezconde-Garbanati L. Perceptions of ceremonial and nonceremonial uses of tobacco by American-Indian adolescents in California. J Adolesc Health. 2006;38(4):443–9.
Carson KV, Brinn MP, Labiszewski NA, Peters M, Veale A, Esterman, A.J.& Smith, B. J. Interventions for tobacco use prevention in indigenous youth. Cochrane Database Syst Rev. 2012a;1:1–51.
Carson KV, Brinn MP, Peters M, Veale A, Esterman AJ, Smith BJ. Interventions for smoking cessation in indigenous populations. Cochrane Database Syst Rev. 2012b;1:1–32.
Cunningham C, Stanley F. Indigenous by definition, experience, or world view: links between people, their land, and culture need to be acknowledged. BMJ: Br Med J. 2003;327(7412):403–4. https://doi.org/10.1136/bmj.327.7412.403.
Bramley D, Riddell T, Whittaker R, Corbett T, Lin RB, Wills M, et al. Smoking cessation using mobile phone text messaging is as effective in Maori as non-Maori. N Zealand Med J. 2005;118(1216):1–10.
• Whittaker R, Dorey E, Bramley D, Bullen C, Denny S, Elley R, et al. A theory-based video messaging mobile phone intervention for smoking cessation: randomized controlled trial. J Med Internet Res. 2011;13(1):e10. A randomized controlled trial to test the effectiveness of a social cognitive theory based smoking cessation intervention among the Maori population. https://doi.org/10.2196/jmir.1553.
• Patten CA, Windsor RA, Renner CC, Enoch C, Hochreiter A, Nevak C, et al. Feasibility of a tobacco cessation intervention for pregnant Alaska Native women. Nicotine Tob Res. 2009;12(2):79–87. This is an important randomized two-group designed with assessments at baseline and during pregnancy.
Sussman S, Dent CW, Lichtman KL. Project EX: outcomes of a teen smoking cessation program. Addict Behav. 2001;26(3):425–38. https://doi.org/10.1016/S0306-4603(00)00135-0.
Morphett K, Partridge B, Gartner C, Carter A, Hall W. Why don’t smokers want help to quit? A qualitative study of smokers’ attitudes towards assisted vs. unassisted quitting. Int J Environ Res Public Health. 2015;12(6):6591–607. https://doi.org/10.3390/ijerph120606591.
Chamberlain et al. (2017) Evidence for a comprehensive approach to Aborginial tobacco control to maintain the decline in smoking: an overview of reviews among indigenous peoples. Systematic Reviews.
Choi WS, Beebe LA, Nazir N, Kaur B, Hopkins M, Talawyma M, et al. All nations breath of life: a randomized controlled trial of smoking cessation for American Indians. Am J Prev Med. 2016;51(5):743–51. https://doi.org/10.1016/j.amepre.2016.05.021.
DiGiamcomo et al. (2011) Smoking cessation in indigenous populations of Australia, New Zealand, Canada, and the United States: elements of effective interventions. International Journal of Environmental Research and Public Health.
Gnich W, Sheehy C, Amos A, Bitel M, Platt S. A Scotland-wide pilot programme of smoking cessation services for young people: process and outcome evaluation. Addiction. 2008;103(11):1866–74. https://doi.org/10.1111/j.1360-0443.2008.02316.x.
High School Youth Risk Behavior Survey 1991–2015, Centers for Disease Control and Prevention.
Minichiello et al. (2016) Effective strategies to reduce commercial tobacco use in indigenous communities globally: a systematic review. BMC Public Health.
Ministry of Health. Annual update of key results 2015/16: New Zealand health survey. Wellington: Ministry of Health; 2016. https://www.health.govt.nz/system/files/documents/publications/annual-update-key-results-2015-16-nzhs-dec16-v2.pdf
Paavola M, Vartiainen E, Puska P. Smoking cessation between teenage years and adulthood. Health Educ Res. 2001;16(1):49–57. https://doi.org/10.1093/her/16.1.49.
Stevenson et al. (2017) Establishing smoke-free homes in the indigenous populations of Australia, New Zealand, Canada and United States: a systematic lit review. Int J Environ Res Public Health.
Van der Sterren, A., Greenhalgh, EM., Knoche, D., & Winstanley, MH. (2016) 8.3 prevalence of tobacco use among aboriginal and Torres Strait islander people. Tobacco in Australia: Facts and issues. Melbourne: Cancer Council Victoria.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Claradina Soto, Jennifer B. Unger, Steve Sussman, and Ingrid Zeledon declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Tobacco
Rights and permissions
About this article
Cite this article
Soto, C., Unger, J.B., Sussman, S. et al. International Approaches to Tobacco Use Cessation Programming and Prevention Interventions among Indigenous Adolescents and Young Adults. Curr Addict Rep 5, 35–41 (2018). https://doi.org/10.1007/s40429-018-0186-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-018-0186-y