Abstract
In this article, we reviewed the association between depth of anesthesia and postoperative delirium. We also evaluated the evidence for intraoperative brain function monitoring to prevent delirium after surgery. Anesthetics produce profound neurochemical changes that may disrupt normal brain function and result in postoperative delirium. Brain function monitoring has emerged as a tool for titration of anesthetic delivery to avoid sedative drugs overdose and may prevent postoperative delirium. A meta-analysis of five existing trials showed that brain function monitoring significantly reduced the risk of delirium after surgery (odds ratio 0.56, 95 % confidence intervals: 0.40–0.77). However, the current evidence is still not definitive because of limited sample size and heterogeneity among studies. Future studies are required to evaluate different depths of anesthesia and postoperative delirium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative delirium is the state of acute confusion that occurs typically during the first few days after surgery [1, 2, 3•]. During an episode of delirium, there is fluctuation in consciousness with alternating periods of inattention and changes in cognitive function and perception [4]. It is commonly believed that delirious patients are hyperactive and are easily recognized. These patients may become violent, imposing self-injury, and producing harm to the attending healthcare workers. Other studies, however, have shown that the majority of patients are actually mute and quiet [5, 6]. These patients are only identified by careful examination using standardized instruments, such as the confusion assessment method [7]. It is the latter group of hypoactive patients, whom we often miss during routine ward assessment, that may contribute to the enormous variations in the incidence of postoperative delirium among studies [average (range) 37 % (0–74 %)] [2, 8, 9]. Postoperative delirium is also an independent risk factor for complications after surgery, leading to poor functional recovery and cognitive impairment [10–18].
Given the high incidence and significant impact on long-term outcome, a number of articles have highlighted the predisposing factors for postoperative delirium [8, 19–21]. Although age and pre-existing cognitive impairment are the most consistent risk factors, emerging data suggest that anesthetic per se may also contribute to the development of delirium after surgery. The purpose of this article was to review the association between anesthesia and delirium. We also evaluate the evidence for processed electroencephalogram (EEG) in guiding anesthetic administration to prevent postoperative delirium.
Anesthetics and Postoperative Delirium
The pathophysiology of postoperative delirium has not been fully elucidated; however, the prevailing mechanism suggests that delirium is primarily a consequence of the loss of connectivity between the various parts of the brain network. The failure of sensory integration and the loss of connection between sensory processing and motor responses, particularly within the thalamo-cortical system, may contribute to postoperative delirium [22–27]. In this regard, elderly patients and patients with pre-existing cognitive impairment have reduced baseline brain connectivity, and would be at risk of further network disconnection following surgery. At the receptor level, large doses of anesthetic agents would cause an increase in inhibitory tone by activation of gamma-aminobutyric acid receptors, rendering the brain network more vulnerable. Anesthetics also block central cholinergic receptors, producing further inhibitory effect on brain circuitry [28]. In animal experiments, standard doses of routine anesthetics have been shown to produce long-lasting neurochemical changes in the form of an increase in tau hyperphosphorylation [29–31], caspase-3 activation [32–35], and β amyloid deposition in the brain [33, 36–38]. Each of these processes may further reduce brain connectivity. It is therefore feasible that large doses of anesthetics might predispose patients to postoperative delirium.
There is another putative mechanism where anesthetics may disrupt brain connectivity. Large doses of anesthetic impair cerebral autoregulation [39, 40]. In this scenario, cerebral vasodilatation cannot compensate for any decrease in perfusion pressure below the lower limit of autoregulation. Progressive hypoperfusion beyond this point may therefore result in cerebral ischemia [41]. Among those who presented to the emergency room with acute stroke between 13 and 48 % of patients had an episode of delirium during the first week of hospitalization [42, 43]. Post-stroke delirium is associated with longer hospital stay and higher morbidity and mortality [odds ratio (95 %confidence intervals, CI): 3.83 (1.70–8.62)] [43–45]. Currently, there is no study demonstrating the association between delirium and stroke after surgery, owing to the fact that the incidence of postoperative stroke is low (0.1 %) [46, 47]. However, a recent observational study showed that new ischemic brain lesions on magnetic resonance imaging could be identified in 11.4 % (8/70 patients, 95 % CI 5.9–21.0 %) of patients following noncardiac surgery [48]. These lesions (covert stroke) may represent the underlying basis for postoperative delirium. Interestingly, delirium has been reported as the only manifestation of stroke in the non-operative setting [49]. The ongoing Neurological Impact of Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (NeuroVISION) study evaluates the epidemiology and clinical consequences of covert stroke in a representative sample of 1,500 patients undergoing noncardiac surgery (clinicaltrials.gov identifier NCT01980511). NeuroVISION has included postoperative delirium as a secondary endpoint and may help to clarify the missing link between postoperative covert stroke and delirium.
Currently, the literature suggests that postoperative delirium could be due to a direct inhibitory effect of anesthetics on the brain network. Alternatively, this may be the consequences of perioperative cerebral hypoxia and ischemia. Although there is no direct evidence to support these hypotheses, both mechanisms are likely to be dose-dependent, and therefore a technique that minimizes anesthetic exposure could be useful to prevent delirium after surgery.
Brain Function Monitoring and Anesthetic Administration
In order to tailor anesthetic delivery to the needs of individual patient, an accurate measure of anesthetic effect is required. For many years, anesthesiologists have routinely used clinical signs, such as blood pressure, heart rate, lacrimation, and sweating to indicate the depth of anesthesia. This is however unreliable. In patients with confirmed awareness during anesthesia, hypertension and tachycardia occurred in <15 % of cases [50]. In another study, intraoperative hemodynamic changes in patients with confirmed awareness during anesthesia were indistinguishable from the matched controls [51]. In order to prevent awareness, anesthetists have learned to give “a little extra” to ensure hypnosis during surgery, and this often results in deeper level of anesthesia.
Since anesthetic works primarily on the brain to produce loss of consciousness, it seems logical to monitor brain activity as a surrogate measure of anesthetic depth. In the past decade, a number of manufacturers have produced devices to measure depth of anesthesia. Table 1 summarizes the features of commercially available brain function monitors [52–62]. These devices are designed to collect (spontaneous or evoked) EEG signals from a specific (typically frontal) electrode montage. EEG data are extracted using specific algorithms. These are then correlated with clinical status (e.g., response to verbal command) in a reference population using a statistical model to generate a dimensionless linear index of anesthetic depth. Therefore, these indices are statistical functions that represent the likelihood of present depth of anesthesia [63]. Obviously, the accuracy of these indices will depend on the quality of the calibration dataset. It should be noted that measurements of entropy and auditory evoked potential have not undergone probability modeling, but the scales have been readjusted so that the values are comparable to other indices.
The advantage of brain function monitor is that it facilitates EEG interpretation by transforming the complex EEG signals into a single accessible number. When alarm settings are appropriately adjusted, it allows anesthesiologists to concentrate on the overall patient care without being distracted by the constantly changing raw EEG waveforms [64]. Based on the depth indices, anesthesiologist aims to titrate anesthetic administration so as to prevent periods of under-dosing and to avoid autonomic stimulation and unintentional awareness. Similarly, brain function monitoring facilitates anesthetic delivery to avoid periods of overdose and minimizes anesthetic exposure. In a meta-analysis of 20 studies involving a total of 2,557 patients, anesthesia guided by bispectral index (BIS) monitoring reduced propofol infusion rate by 17.8 % (95 % CI 9.9–25.8 %) and decreased volatile administration by 18.4 % (95 % CI 3.3–30.7 %), compared with standard patient care [65, 66]. This was associated with a decrease in time to tracheal extubation and recovery room discharge by 2.6 (95 % CI 1.8–3.5) min and 6.8 (95 % CI 2.3–11.2) min, respectively [65]. Although similar results were shown for other devices (entropy: 6 trials, 695 patients) and (narcotrend: 2 trials, 124 patients), study designs were different, and the sample size of the latter trials was relatively small [66].
Anesthetic Depth and Postoperative Delirium
Could monitoring of anesthetic depth prevent postoperative delirium? Currently, no study has evaluated the impact of varying anesthetic depth on postoperative delirium. Since brain function monitoring has been shown to reduce anesthetic exposure, studies that employ these monitors to target different ranges of anesthetic depths may be useful to highlight any effect of anesthetic depth on postoperative delirium.
Table 2 summarizes the findings of five existing trials that evaluate brain function monitoring and postoperative delirium [67, 68, 69•, 70•,71•]. The average age of patients in these trials was between 60 and 81.7 years. Jildenstål and colleagues studied the utility of auditory evoked potential (AEP) in patients undergoing eye surgery [67]. AEP-guided anesthesia reduced consumption of propofol and desflurane by 10.5 and 24.2 %, respectively. The decrease in anesthetic requirement was associated with a reduction in the risk of postoperative delirium by 88 %. All other trials used BIS monitoring to adjust anesthetic administration [68, 69•, 70•, 71•].
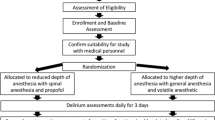
Sieber and coworkers randomized patients having hip fracture fixation to receive deep or light sedation using propofol infusion [68]. All patients received spinal anesthesia as the primary anesthetic. This trial actually tested two levels of sedation (BIS ≥ 80 vs. BIS 50), and reported that light sedation reduced the risk of postoperative delirium by 65 %. However, it should be noted that patients allocated in the deep sedation group (BIS 50) actually received less anesthetics than the other trials.
Two trials compared brain function monitoring with routine practice based on clinical signs [70•, 71•]. In the cognitive dysfunction after anesthesia (CoDA) trial, 902 patients, ≥60 years, undergoing noncardiac surgery were randomly assigned to receive BIS-guided anesthesia (keeping BIS between 40 and 60) or routine care [70•]. BIS monitoring decreased anesthetic exposure by 21–30 % and reduced duration of deep anesthesia (BIS <40) during the course of surgery and thus producing two levels of anesthetic depth, i.e., light anesthesia in the BIS group and deep anesthesia in the routine care group. BIS monitoring was associated with a lower risk of postoperative delirium (relative reduction 42 %). Similarly, Radtke and coworkers found that BIS monitoring reduced delirium after surgery compared with controls [odds ratio (95 % CI): 0.73 (0.54–0.98)]. Although the average BIS values were similar between groups, the trial showed that BIS monitoring was effective to reduce episodes of very deep anesthesia with BIS <20. It remains plausible that the very deep level of anesthesia is the trigger of postoperative delirium.
Using a subgroup of patients undergoing cardiothoracic surgery in the BIS or Anesthetic Gas to Reduce Explicit Recall (BAG-RECALL) trial [69•], Whitlock and coworkers compared the incidence of delirium between the patients who were randomize to BIS-guided anesthetic administration (targeted to a BIS value between 40 and 60) or maintenance of anesthesia at end-tidal volatile concentration of 0.7–1.3 minimum alveolar concentration (MAC). It was found that the rate of delirium tended to be lower in the BIS-monitoring group although the difference was not statistically significant. Surprisingly, low average anesthetic dose was identified as an independent predictor of delirium. In addition, the trial showed that larger volatile concentration appeared to reduce the risk of delirium [odds ratio (95 % CI): 0.70 (0.53–0.92)]. These findings may indicate that the delirious patients were more sensitive to anesthetics [72]. However, issues regarding post hoc study design, missing follow-up (3.8 % did not receive delirium assessment), and incomplete record (3.6 %) may have influenced these study results. Nevertheless, a pooled estimate for the 3 trials comparing the use of BIS monitoring and routine care or BIS monitoring and end-tidal anesthetic concentration demonstrated a significant risk reduction for postoperative delirium by 35 % (95 % CI 20–47 %), favoring BIS monitoring.
Overall, brain function monitoring reduced the risk of postoperative delirium and the treatment effect appeared to be substantial [odds ratio (95 % CI): 0.56 (0.40–0.77), p < 0.001)] (Fig. 1). However, these results warrant cautious interpretation. There are significant heterogeneity in the design and conduct of the various trials (I 2 = 48.5 %). It should be emphasized that these trials did not randomize patients into light or deep level of anesthesia, instead patients were allocated to have brain function monitoring or not. Although patients receiving brain function monitoring are likely to have less anesthetic exposure, we cannot exclude periods of deep anesthesia that may lead to postoperative delirium in these patients. Similarly, patients in the routine care group might not always result in deep anesthesia. These confounding factors would therefore obscure the association between anesthetic depth and postoperative delirium.
The ideal study should therefore randomize patients to two levels of anesthetic depth and measure postoperative delirium using a valid and standardized instrument at regular intervals. The Balanced Anesthesia Trial (Australian New Zealand Clinical Trials Registry No: ACTRN12612000632897) was recently initiated to recruit 6,500 high-risk patients of American Society of Anesthesiology physical status class 3 or 4, age ≥60 years, undergoing major surgery. Patients are randomly assigned to receive deep or light anesthesia with BIS target of 35 or 50, respectively. The primary outcome is all-cause mortality at one year after index surgery. A substudy has been planned to measure postoperative delirium using the confusion assessment method during the initial hospital stay. This substudy will provide clear evidence to establish the link between depth of anesthesia and postoperative delirium.
Conclusions
Postoperative delirium is common among elderly patients undergoing major surgery. Current studies have suggested that deep level of anesthesia may predispose patients to delirium after surgery. However, a definitive prospective trial is needed to establish the role of anesthetics in causing postoperative delirium.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Deiner S, Silverstein JH. Postoperative delirium and cognitive dysfunction. Br J Anaesth. 2009;103(suppl 1):i41–6.
Rudolph JL, Marcantonio ER. Postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112:1202–11.
• Hughes CG, Pandharipande PP. The effects of perioperative and intensive care unit sedation on brain organ dysfunction. Anesth Analg 2011;112:1212–7. An up-to-date review on postoperative delirum including topics on risk factors, patient outcomes, management and prevention stratgies.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM Jr. Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Arch Intern Med. 2001;161:2467–73.
Liptzin B, Levkoff SE. An empirical study of delirium subtypes. Br J Psychiatry. 1992;161:843–5.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8.
Gustafson Y, Berggren D, Brannstrom B, et al. Acute confusional states in elderly patients treated for femoral neck fracture. J Am Geriatr Soc. 1988;36:525–30.
Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium. A review of 80 primary data-collection studies. Arch Intern Med. 1995;155:461–5.
Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–9.
Rudolph JL, Marcantonio ER, Culley DJ, et al. Delirium is associated with early postoperative cognitive dysfunction. Anaesthesia. 2008;63:941–7.
Gottesman RF, Grega MA, Bailey MM, et al. Delirium after coronary artery bypass graft surgery and late mortality. Ann Neurol. 2010;67:338–44.
Franco K, Litaker D, Locala J, Bronson D. The cost of delirium in the surgical patient. Psychosomatics. 2001;42:68–73.
Rudolph JL, Inouye SK, Jones RN, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58:643–9.
Rudolph JL, Jones RN, Rasmussen LS, Silverstein JH, Inouye SK, Marcantonio ER. Independent vascular and cognitive risk factors for postoperative delirium. Am J Med. 2007;120:807–13.
Robinson TN, Raeburn CD, Tran ZV, Angles EM, Brenner LA, Moss M. Postoperative delirium in the elderly: risk factors and outcomes. Ann Surg. 2009;249:173–8.
Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48:618–24.
Koster S, Hensens AG, van der Palen J. The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thorac Surg. 2009;87:1469–74.
Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271:134–9.
Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119:229–36.
Williams-Russo P, Urquhart BL, Sharrock NE, Charlson ME. Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc. 1992;40:759–67.
Tononi G. An information integration theory of consciousness. BMC Neurosci. 2004;5:42.
Balduzzi D, Tononi G. Qualia: the geometry of integrated information. PLoS Comput Biol. 2009;5:e1000462.
Massimini M, Ferrarelli F, Huber R, Esser SK, Singh H, Tononi G. Breakdown of cortical effective connectivity during sleep. Science. 2005;309:2228–32.
Ferrarelli F, Massimini M, Sarasso S, et al. Breakdown in cortical effective connectivity during midazolam-induced loss of consciousness. Proc Natl Acad Sci USA. 2010;107:2681–6.
Sanders RD. Hypothesis for the pathophysiology of delirium: role of baseline brain network connectivity and changes in inhibitory tone. Med Hypotheses. 2011;77:140–3.
Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsiveness not equal unconsciousness. Anesthesiology. 2012;116:946–59.
Pratico C, Quattrone D, Lucanto T, et al. Drugs of anesthesia acting on central cholinergic system may cause post-operative cognitive dysfunction and delirium. Med Hypotheses. 2005;65(5):972–82.
Ikeda Y, Ishiguro K, Fujita SC. Ether stress-induced Alzheimer-like tau phosphorylation in the normal mouse brain. FEBS Lett. 2007;581:891–7.
Planel E, Richter KE, Nolan CE, et al. Anesthesia leads to tau hyperphosphorylation through inhibition of phosphatase activity by hypothermia. J Neurosci. 2007;27:3090–7.
Run X, Liang Z, Zhang L, Iqbal K, Grundke-Iqbal I, Gong CX. Anesthesia induces phosphorylation of tau. J Alzheimers Dis. 2009;16:619–26.
Fütterer CD, Maurer MH, Schmitt A, Feldmann RE Jr, Kuschinsky W, Waschke KF. Alterations in rat brain proteins after desflurane anesthesia. Anesthesiology. 2004;100:302–8.
Zhang B, Dong Y, Zhang G, et al. The inhalation anesthetic desflurane induces caspase activation and increases amyloid beta-protein levels under hypoxic conditions. J Biol Chem. 2008;283:11866–75.
Zhang G, Dong Y, Zhang B, et al. Isoflurane-induced caspase-3 activation is dependent on cytosolic calcium and can be attenuated by memantine. J Neurosci. 2008;28:4551–60.
Kalenka A, Gross B, Maurer MH, Thierse HJ, Feldmann RE Jr. Isoflurane anesthesia elicits protein pattern changes in rat hippocampus. J Neurosurg Anesthesiol. 2010;22:144–54.
Xie Z, Dong Y, Maeda U, et al. The common inhalation anesthetic isoflurane induces apoptosis and increases amyloid beta protein levels. Anesthesiology. 2006;104:988–94.
Abramov E, Dolev I, Fogel H, Ciccotosto GD, Ruff E, Slutsky I. Amyloid-beta as a positive endogenous regulator of release probability at hippocampal synapses. Nat Neurosci. 2009;12:1567–76.
Dong Y, Zhang G, Zhang B, et al. The common inhalational anesthetic sevoflurane induces apoptosis and increases beta-amyloid protein levels. Arch Neurol. 2009;66:620–31.
Summors AC, Gupta AK, Matta BF. Dynamic cerebral autoregulation during sevoflurane anesthesia: a comparison with isoflurane. Anesth Analg. 1999;88:341–5.
Strebel S, Lam AM, Matta B, Mayberg TS, Aaslid R, Newell DW. Dynamic and static cerebral autoregulation during isoflurane, desflurane, and propofol anesthesia. Anesthesiology. 1995;83:66–76.
Drummond JC. The lower limit of autoregulation: time to revise our thinking? Anesthesiology. 1997;86:1431–3.
Sheng AZ, Shen Q, Cordato D, Zhang YY, Chan DKY. Delirium within three days of stroke in a cohort of elderly patients. J Am Geriatr Soc. 2006;54:1192–8.
McManus J, Pathansali R, Stewart R, Macdonald A, Jackson S. Delirium post-stroke. Age Ageing. 2007;36:613–8.
Kostalova M, Bednarik J, Mitasova A, et al. Towards a predictive model for post-stroke delirium. Brain Inj. 2012;26:962–71.
Miu DK, Yeung JC. Incidence of post-stroke delirium and 1-year outcome. Geriatr Gerontol Int. 2013;13:123–9.
Mashour GA, Moore LE, Lele AV, Robicsek SA, Gelb AW. Perioperative care of patients at high risk for stroke during or after non-cardiac, non-neurologic surgery: consensus Statement from the Society for Neuroscience in Anesthesiology and Critical Care. J Neurosurg Anesthesiol. 2014;26:273–85.
Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, nonneurosurgical surgery. Anesthesiology. 2011;115:879–90.
Mrkobrada M, Hill MD, Chan MT, et al. The NeuroVISION pilot study: non-cardiac surgery carries a significant risk of acute covert stroke. Stroke 2013;44:ATMP9.
Stewart JT, Quijije N, Sheyner I, Stover KT. Delirium without focal signs related to a thalamic stroke. J Am Geriatr Soc. 2010;58:2433–4.
Domino KB, Posner KL, Caplan RA, Cheney FW. Awareness during anesthesia: a closed claims analysis. Anesthesiology. 1999;90:1053–61.
Moerman N, Bonke B, Oosting J. Awareness and recall during general anesthesia facts and feelings. Anesthesiology. 1993;79:454–64.
Sigl JC, Chamoun NG. An introduction to bispectral analysis for the electroencephalogram. J Clin Monit. 1994;10:392–404.
Drover DR, Lemmens HJ, Pierce ET, et al. Patient State Index: titration of delivery and recovery from propofol, alfentanil, and nitrous oxide anesthesia. Anesthesiology. 2002;97:82–9.
Schultz A, Grouven U, Beger FA, Schultz B. The narcotrend index: classification algorithm, correlation with propofol effect-site concentrations, and comparison with spectral parameters. Biomed Tech (Berl). 2004;49:38–42.
Aho AJ, Yli-Hankala A, Lyytikainen LP, Jantti V. Facial muscle activity, response entropy, and state entropy indices during noxious stimuli in propofol-nitrous oxide or propofol-nitrous oxide-remifentanil anaesthesia without neuromuscular block. Br J Anaesth. 2009;102:227–33.
Mantzaridis H, Kenny GN. Auditory evoked potential index: a quantitative measure of changes in auditory evoked potentials during general anaesthesia. Anaesthesia. 1997;52:1030–6.
Jensen EW, Lindholm P, Henneberg SW. Autoregressive modeling with exogenous input of middle-latency auditory-evoked potentials to measure rapid changes in depth of anesthesia. Methods Inf Med. 1996;35:256–60.
Jensen EW, Struys MMRF, Vazquez PM, Rodriguez B, Litvan H. An AEP/EEG hybrid index for monitoring the hypnotic depth during general anesthesia. In: International IEEE EMBS Conference on Neural Engineering 2003:268–70.
Jensen EW, Litvan H, Revuelta M, et al. Cerebral state index during propofol anesthesia: a comparison with the bispectral index and the A-line ARX index. Anesthesiology. 2006;105:28–36.
Jensen EW, Jospin M, Gambus PL, Vallverdu M, Caminal P. Validation of the index of consciousness (IoC) during sedation/analgesia for ultrasonographic endoscopy. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:5552–5.
Jensen EW, Valencia JF, LÓPez A, et al. Monitoring hypnotic effect and nociception with two EEG-derived indices, qCON and qNOX, during general anaesthesia. Acta Anaesthesiol Scand. 2014;58:933–41.
Wong CA, Fragen RJ, Fitzgerald P, McCarthy RJ. A comparison of the SNAP II and BIS XP indices during sevoflurane and nitrous oxide anaesthesia at 1 and 1.5 MAC and at awakening. Br J Anaesth. 2006;97:181–6.
Chan MT, Gin T. What does the bispectral EEG index monitor? Eur J Anaesthesiol. 2000;17:146–8.
Bennett C, Voss LJ, Barnard JP, Sleigh JW. Practical use of the raw electroencephalogram waveform during general anesthesia: the art and science. Anesth Analg. 2009;109:539–50.
Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;6:CD003843.
Shepherd J, Jones J, Frampton G, Bryant J, Baxter L, Cooper K. Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-entropy, bispectral index and narcotrend): a systematic review and economic evaluation. Health Technol Assess. 2013;17:1–264.
Jildenstål PK, Hallen JL, Rawal N, Gupta A, Berggren L. Effect of auditory evoked potential-guided anaesthesia on consumption of anaesthetics and early postoperative cognitive dysfunction: a randomised controlled trial. Eur J Anaesthesiol. 2011;28:213–9.
Sieber FE, Zakriya KJ, Gottschalk A, et al. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc. 2010;85:18–26.
• Whitlock EL, Torres BA, Lin N, et al. Postoperative delirium in a substudy of cardiothoracic surgical patients in the BAG-RECALL clinical trial. Anesth Analg 2014;118:809–17. A post hoc analysis of BAG-RECALL trial showing higher risk of postoperative delirium in patients who received lower doses of volatile anesthetics. This may reflect the role of anesthetic sensitivity on postoiperative delirium.
• Chan MTV, Cheng BC, Lee TM, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol 2013;25:33–42. A randomized controlled trial showing the utility of BIS monitoring for the prevention of postoprative cognitive dysfunction and delirium.
• Radtke FM, Franck M, Lendner J, Kruger S, Wernecke KD, Spies CD. Monitoring depth of anaesthesia in a randomized trial decreases the rate of postoperative delirium but not postoperative cognitive dysfunction. Br J Anaesth 2013;110 Suppl 1:i98–105. A randomized controlled trial showing that very deep anesthesia (BIS < 20) was associated with postoprative delirium.
Sessler DI, Sigl JC, Kelley SD, et al. Hospital stay and mortality are increased in patients having a “triple low” of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. Anesthesiology. 2012;116:1195–203.
Chan MTV, et al. Interventional neurophysiologic monitoring. Curr Opin Anaesthesiol. 2004;17(5):389–96.
Acknowledgments
The authors are site investigators for the Balanced Anesthesia Trial. Dr. Chan is a member of the steering committee of the NeuroVISION Study. The Balanced Anesthesia Trial is supported by a General Research Fund (461513), Research Grant Council, and the NeuroVISION Study is supported by a Health and Medical Research Fund (11120321), Food and Health Bureau, Hong Kong Special Administrative region.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Perioperative Delirium.
Rights and permissions
About this article
Cite this article
Luk, T.T.H., Jia, B., Pang, E.Y.T. et al. Depth of Anesthesia and Postoperative Delirium. Curr Anesthesiol Rep 5, 1–9 (2015). https://doi.org/10.1007/s40140-014-0088-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-014-0088-z