Abstract
Purpose of Review
We conducted a comprehensive and updated overview on complications occurring after transcatheter aortic valve implantation (TAVI) for severe aortic stenosis.
Recent Findings
Despite remarkable improvements in patient selection, devices, procedures, and ancillary management, complications may still occur in patients undergoing TAVI. On top of most commonly described adverse events such as death, myocardial infarction, stroke, bleeding, vascular complication, renal failure, pacemaker implantation and residual valve regurgitation, other less common but similarly severe complications may still occur. These may include events ranging from acute delirium to valve compression during cardiopulmonary resuscitation. Meticulous care should be applied to all screening and procedural steps for TAVI, and attentive follow-up should be implemented afterwards, especially in suboptimal TAVI candidates or those otherwise at high operative risk.
Summary
Despite recent remarkable improvements, additional research is warranted in order to further improve early and late outlook of TAVI, identify predictors of complications, and the best way to handle them.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
An expert is a man who has made all the mistakes which can be made, in a narrow field
Niels Bohr
Introduction
Transcatheter aortic valve implantation (TAVI) represents an appealing alternative for patients with severe symptomatic aortic stenosis and high surgical risk score. Indeed, surgical risk is typically appraised quantitatively with the EuroSCORE II, logistic EuroSCORE, or Society of Thoracic Surgery instruments. Otherwise, unsuitability for surgery is based on adverse features such as porcelain aorta, sequelae of chest radiation, or frailty [1•, 2,3,4].
Since the first pioneering cases, techniques and devices for TAVI have dramatically improved, and now, percutaneous transfemoral approach is considered the best option over transapical approach to minimize the risk of local as well as peripheral complications of TAVI procedures, even if other approaches are possible [5,6,7,8,9,10]. Indeed, several landmark randomized clinical trials have established the safety and efficacy of first and then current-generation TAVI devices, even in intermediate risk patients [10, 11••]. Most recent data are likely to expand indications for TAVI to include also subjects at low risk and those with pure aortic regurgitation [12].
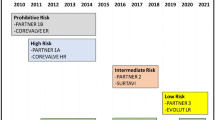
While TAVI has provided favorable early and mid-term results in selected patients, comparing favorably to surgery whenever risk was moderate, high, or prohibitive, there is uncertainty on the potential risk of adverse events associated acutely or chronically with TAVI, and this appraisal is further complicated by the ever increasing success of this procedure, and ensuing increase in the number of TAVI cases worldwide. Our primary objective was thus a systematic review of the TAVI literature focusing on potential complications (Fig. 1).
Methods
This work was designed as an umbrella review (i.e., overview of systematic reviews) in keeping with established recommendations for evidence synthesis [13]. Specifically, we searched PubMed in order to find pertinent systematic reviews or meta-analyses on of TAVI using the following string: systematic[sb] AND (TAVI OR TAVR OR ((transcatheter AND aortic AND valve) AND (implantation OR replacement))), restricting our search to studies published between January 2014 and January 2019 in order to inform on complications of currently available devices. Citations were first screened at the title/abstract level. Then, full texts were sought if potentially pertinent. We extracted salient features of included reviews, and then on type, timing, incidence and outlook of described complications, eventually summarizing the results in tabular form. Pragmatically, we differentiated complications in early and late ones. Specifically, in keeping with the Valve Academic Research Consortium (VARC)-2 recommendations, procedural and peri-procedural complications were defined as early, and the same applied to events occurring within 72 h after the procedure [14•]. Conversely, all other events were considered as late. Given the design of this work as a scoping review, we did not explicitly appraised methods or internal validity of included studies.
Results
The selection process is summarized in Fig. 1.
Early Complications
TAVI may be associated with several types of early complications, ranging, for instance, from arrhythmia to bleeding, dissection, myocardial infarction, perforation, or stroke, including fatal ones. Most can be easily anticipated and explained pathophysiologically given the need to gain vascular access, reach the aortic valve, and safely deliver there a bulky device (Fig. 2) [1]. Further acute adverse events can be easily anticipated given that TAVI is most often performed in elderly or otherwise at intermediate to high-risk patients [10, 11••]. Incidence of such events varies, and it may also depend on individualized device choice, operator experience, institution volume, and proactive multidisciplinary care (Table 1; Table 2). Briefly, death, myocardial infarction, stroke, bleeding, vascular complication, renal failure, permanent pacemaker implantation, and aortic regurgitation with or without paravalvular regurgitation should always be considered as potential early complications of TAVI [1, 11••, 15,16,17,18,19]. In addition, other less common acute complications of TAVI have been described, ranging from delirium, cognitive dysfunction, liver failure, endocarditis, and aseptic intracardiac shunt [20,21,22,23]. Similarly to more common events, these are more frequent or more worrisome in higher risk patients or when procedures entail more aggressive or time consuming approaches.
Proactive surveillance is thus required shortly after TAVI, possibly in an intensively monitored setting, with frequent checks of vital signs, and repeat measurements of laboratory tests capable of eliciting early signs of complications. In addition, periodic echocardiograms are useful to verify valve morphology and function, as well as other cardiac details. A low index of suspicion should be applied also to order magnetic resonance imaging for neurologic complications, computed tomography imaging for chest, abdominal, or access site complications, as well as duplex ultrasound imaging.
Late Complications
There are some clearly uniquely late adverse events that can occur after TAVI (Table 1; Table 2) [1]. As pertinent for acute complications, most late adverse events in patients with prior TAVI depend of course on baseline risk, which is typically high, and even when low or intermediate, is dominated by advanced age. Important albeit uncommon late events after TAVI include valve thrombosis, compression, or embolization caused by manual chest compression during cardiopulmonary resuscitation, valve deterioration, endocarditis, and coronary occlusion due to neointimal hyperplasia on valve struts [15, 16, 24•].
Periodic patient assessment with a detailed cardiac exam is mandatory after TAVI and should include transthoracic echocardiogram every 3 to 12 months, depending on timing since TAVI and clinical stability. A low index of suspicion should be applied to order transesophageal echocardiography or computed tomography imaging, whose greater diagnostic and prognostic accuracy result crucial for decision making (e.g., when considering repeat TAVI or surgical aortic valve replacement) in case of valve deterioration or compression.
Conclusions
Despite ongoing improvements in patient selection, procedural details, device features, and operator skill, complications may still occur in patients undergoing TAVI. On top of most commonly described events such as death, myocardial infarction, stroke, bleeding, vascular complication, renal failure, pacemaker implantation, and residual valve regurgitation, other less common but similarly dreadful conditions may impact on patient morbidity and mortality after TAVI. These may include heterogeneous events ranging from acute delirium to valve compression during cardiopulmonary resuscitation. Meticulous care should be applied to all the screening and procedural steps, and attentive follow-up with periodic clinical and imaging assessments should be implemented. This appears even truer given that TAVI to date is mostly offered to elderly patients at prohibitive, high or intermediate surgical risk, who by definition have an increased risk of complications, and may also have difficulties in facing clinical complications which would be less than life-threatening in fitter subjects.
Limitations of our work include those inherent to any umbrella review with scoping goals, thus avoiding accurate assessment of review validity and methods. In addition, most included reviews focused on first-generation devices, which are now considered outdated for TAVI.
In conclusion, despite ongoing improvements in early and long-term outcomes after TAVI, complications still occur. Thus, additional research is warranted in order to further improve early and late outlook of TAVI, better identify predictors of complications, and define the most effective way to handle them.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Giordano A, Biondi-Zoccai G, Frati G, editors. Transcatheter aortic valve implantation: clinical, interventional, and surgical perspectives. Cham: Springer International Publishing; 2019. Comprehensive textbook on transcatheter aortic valve implantation.
Gatto L, Biondi-Zoccai G, Romagnoli E, Frati G, Prati F, Giordano A. New-generation devices for transcatheter aortic valve implantation. Minerva Cardioangiol. 2018;66:747–61.
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38:2739–91.
Giordano A, Corcione N, Biondi-Zoccai G, Berti S, Petronio AS, Pierli C, et al. Patterns and trends of transcatheter aortic valve implantation in Italy: insights from RISPEVA. J Cardiovasc Med (Hagerstown). 2017;18:96–102.
Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002;106:3006–8.
Dewey TM, Walther T, Doss M, Brown D, Ryan WH, Svensson L, et al. Transapical aortic valve implantation: an animal feasibility study. Ann Thorac Surg. 2006;82:110–6.
Svensson LG, Dewey T, Kapadia S, Roselli EE, Stewart A, Williams M, et al. United States feasibility study of transcatheter insertion of a stented aortic valve by the left ventricular apex. Ann Thorac Surg. 2008;86:46–54.
Lichtenstein SV, Cheung A, Ye J, Thompson CR, Carere RG, Pasupati S, et al. Transapical transcatheter aortic valve implantation in humans: initial clinical experience. Circulation. 2006;114:591–6.
Webb JG, Pasupati S, Humphries K, Thompson C, Altwegg L, Moss R, et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation. 2007;116:755–63.
Zeeshan A, Tuzcu EM, Krishnaswamy A, Kapadia S, Mick S. Transcatheter aortic valve replacement: history and current indications. Cleve Clin J Med. 2015;82:S6–10.
•• Biondi-Zoccai G, Peruzzi M, Abbate A, Gertz ZM, Benedetto U, Tonelli E, et al. Network meta-analysis on the comparative effectiveness and safety of transcatheter aortic valve implantation with CoreValve or Sapien devices versus surgical replacement. Heart Lung Vessel. 2014;6:232–43. First ever network meta-analysis on transcatheter aortic valve implantation.
Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Søndergaard L, Mumtaz M, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017;376(14):1321–31.
Biondi-Zoccai G, editor. Umbrella reviews: evidence synthesis with overviews of reviews and meta-epidemiologic studies. Cham: Springer International Publishing; 2016.
• Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2012;33:2403–18. Key guideline on definitions for complications and adverse events in patients undergoing transcatheter aortic valve implantation.
Giordano A, Corcione N, Ferraro P, Morello A, Conte S, Bedogni F, et al. Impact of predilation before transcatheter aortic valve implantation with new-generation devices. Cardiovasc Revasc Med. https://doi.org/10.1016/j.carrev.2019.01.017.
Giordano A, Corcione N, Ferraro P, Pieri P, Avellino R, Frati G, et al. Propensity-score-adjusted comparison of Evolut vs. Portico devices for transcatheter aortic valve implantation. J Cardiovasc Med (Hagerstown). 2019;20:351–7. https://doi.org/10.2459/JCM.0000000000000764.
Sun Y, Liu X, Chen Z, Fan J, Jiang J, He Y, et al. Meta-analysis of predictors of early severe bleeding in patients who underwent transcatheter aortic valve implantation. Am J Cardiol. 2017;120:655–61.
Ma M, Gao WD, Gu YF, Wang YS, Zhu Y, He Y. Clinical effects of acute kidney injury after transcatheter aortic valve implantation: a systematic review and meta-analysis. Intern Emerg Med. 2019;14:161–75.
Auffret V, Regueiro A, Del Trigo M, Abdul-Jawad Altisent O, Campelo-Parada F, Chiche O, et al. Predictors of early cerebrovascular events in patients with aortic stenosis undergoing transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;68:673–84.
Abawi M, Pagnesi M, Agostoni P, Chiarito M, van Jaarsveld RC, van Dongen CS, et al. Postoperative delirium in individuals undergoing transcatheter aortic valve replacement: a systematic review and meta-analysis. J Am Geriatr Soc. 2018;66:2417–24.
Marullo AGM, Biondi-Zoccai G, Giordano A, Frati G. No guts, no glory for aortic stenosis: impact of liver function on patients undergoing trascatheter aortic valve implantation. J Cardiovasc Med (Hagerstown). 2019;20:245–7.
Ando T, Briasoulis A, Telila T, Afonso L, Grines CL, Takagi H. Does mild paravalvular regurgitation post transcatheter aortic valve implantation affect survival? A meta-analysis. Catheter Cardiovasc Interv. 2018;91:135–47.
Rojas P, Amat-Santos IJ, Cortés C, Castrodeza J, Tobar J, Puri R, et al. Acquired aseptic Intracardiac shunts following Transcatheter aortic valve replacement: A Systematic Review. JACC Cardiovasc Interv. 2016;9:2527–38.
• Mylotte D, Andalib A, Thériault-Lauzier P, Dorfmeister M, Girgis M, Alharbi W, et al. Transcatheter heart valve failure: a systematic review. Eur Heart J. 2015;36:1306–27. Comprehensive review on causes and mechanisms of transcatheter aortic valve implantation failure.
Acknowledgements
The authors would like to thank Dr. Robert Sherwin for reviewing their manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Prof. Biondi-Zoccai has consulted for Abbott Vascular and Bayer. Alberto Morello, Nicola Corcione, Paolo Farraro, Sirio Conte, Giacomo Frati, Barbara Antonazzo, Mariangela Peruzzi, Elena Cavarretta, Leonardo Roever, Antonio Popolo Rubbio, Magdalena Cuman, and Arturo Giordano declare interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiovascular Care
Rights and permissions
About this article
Cite this article
Morello, A., Corcione, N., Farraro, P. et al. Complications After Transcatheter Aortic Valve Implantation: an Updated Umbrella Review. Curr Emerg Hosp Med Rep 7, 227–233 (2019). https://doi.org/10.1007/s40138-019-00202-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-019-00202-4